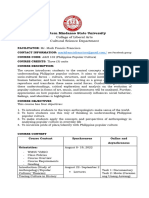
Professional Documents
Culture Documents
Brain Hematoma
Brain Hematoma
Uploaded by
bellaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Brain Hematoma
Brain Hematoma
Uploaded by
bellaCopyright:
Available Formats
A brain hematoma, also known as an intracranial hematoma, is a serious medical condition characterized
by the accumulation of blood within the skull, either within the brain tissue itself or in the space
between the brain and the skull. This accumulation of blood can lead to increased pressure on the brain,
potentially causing severe neurological symptoms and even life-threatening complications if not
promptly treated.
There are several types of brain hematomas, each with its own causes, symptoms, and treatments:
1. **Epidural Hematoma:** An epidural hematoma occurs when blood collects between the dura mater
(the outermost layer of the brain's protective covering) and the skull. It is often caused by a traumatic
head injury, such as a skull fracture, which ruptures an artery, leading to bleeding. Epidural hematomas
can develop rapidly and cause symptoms such as headache, confusion, dizziness, nausea, and loss of
consciousness. Immediate medical intervention, typically surgical evacuation of the hematoma, is
necessary to relieve pressure on the brain.
2. **Subdural Hematoma:** A subdural hematoma occurs when blood accumulates between the dura
mater and the arachnoid membrane (the middle layer of the brain's protective covering). Subdural
hematomas are commonly caused by head trauma, particularly in older adults with age-related brain
atrophy or individuals with a history of repeated head injuries. Symptoms may include headache,
confusion, drowsiness, slurred speech, and seizures. Treatment may involve close monitoring,
medication to reduce swelling, or surgical evacuation depending on the size and severity of the
hematoma.
3. **Intracerebral Hematoma:** An intracerebral hematoma occurs when blood pools within the brain
tissue itself, usually due to trauma, ruptured blood vessels, or conditions such as hemorrhagic stroke or
arteriovenous malformations (abnormal connections between arteries and veins). Symptoms vary
depending on the location and size of the hematoma but may include weakness, numbness, difficulty
speaking or understanding speech, vision changes, and loss of consciousness. Treatment may involve
surgery to remove the hematoma, medication to control symptoms, and rehabilitation to address any
neurological deficits.
4. **Subarachnoid Hemorrhage:** Although technically not a hematoma, a subarachnoid hemorrhage
refers to bleeding into the space between the arachnoid membrane and the pia mater (the innermost
layer of the brain's protective covering). It is often caused by the rupture of a cerebral aneurysm (a
weakened, bulging blood vessel), head trauma, or other vascular abnormalities. Subarachnoid
hemorrhage presents with sudden, severe headache ("thunderclap headache"), nausea, vomiting, neck
stiffness, and altered mental status. Emergency treatment is essential to prevent complications such as
cerebral vasospasm and hydrocephalus.
Diagnosis of a brain hematoma typically involves a combination of medical history, physical examination,
imaging studies (such as CT scans or MRI), and possibly additional tests to assess neurological function.
Treatment varies depending on the type, location, and severity of the hematoma but may include
surgical intervention, medication to control symptoms and reduce swelling, and supportive care to
manage complications.
Overall, brain hematomas are serious medical emergencies that require prompt recognition and
intervention to minimize the risk of permanent brain damage or death. Early diagnosis and appropriate
treatment can significantly improve outcomes and reduce the likelihood of long-term neurological
deficits.
You might also like
- Pathophysiology of StrokeDocument3 pagesPathophysiology of StrokeAqeel Al-Mahdaly0% (1)
- Epidural HematomaDocument33 pagesEpidural HematomaRupak GhimireNo ratings yet
- Case Presentation of Hemorrhagic Stroke Subarachnoid HemorrhageDocument69 pagesCase Presentation of Hemorrhagic Stroke Subarachnoid HemorrhageShin FerranculloNo ratings yet
- Soal Ujian Neurotrauma Full - JWBDocument22 pagesSoal Ujian Neurotrauma Full - JWBTina HerreraNo ratings yet
- Lecture Note On Intracrenial HemorrhageDocument4 pagesLecture Note On Intracrenial HemorrhageLionel EmmanuelNo ratings yet
- Head InjuryDocument6 pagesHead InjuryHurrinazilla AwaliaNo ratings yet
- Pa Tho Physiology of Hemorrhagic StrokeDocument2 pagesPa Tho Physiology of Hemorrhagic StrokeMerlash MerlaNo ratings yet
- Disorders of The Nervous SystemDocument100 pagesDisorders of The Nervous SystemnipoNo ratings yet
- Stroke: C or Brain Attack) Results From Sudden Interruption of Blood Supply ToDocument3 pagesStroke: C or Brain Attack) Results From Sudden Interruption of Blood Supply ToFlorence Hadap-EndrinaNo ratings yet
- Brain 2Document2 pagesBrain 2bambangNo ratings yet
- Cerebral HemorrhageDocument2 pagesCerebral HemorrhageGian TejadaNo ratings yet
- Head InjuryDocument13 pagesHead InjuryMay NitayakulNo ratings yet
- Head Trauma Is The Most Commone Epidural and Subdural HematomaDocument5 pagesHead Trauma Is The Most Commone Epidural and Subdural HematomaBereket ShimelisNo ratings yet
- Hemorrhagic StrokeDocument18 pagesHemorrhagic StrokeNdan RahmaNo ratings yet
- Intracranial Hemorrhage IntroDocument5 pagesIntracranial Hemorrhage IntroPat Vierneza-CalalangNo ratings yet
- Cerebrovascular Accident or StrokeDocument3 pagesCerebrovascular Accident or StrokeJohn DNo ratings yet
- Classification of Hemorrhagic StrokesDocument7 pagesClassification of Hemorrhagic StrokesRavinr9No ratings yet
- Week 6 Craniotomy Part IIDocument27 pagesWeek 6 Craniotomy Part IIkatherinerance331No ratings yet
- LP StrokeDocument33 pagesLP StrokeMiskan FebrianiNo ratings yet
- Signs and Symptoms: Epidural HematomaDocument2 pagesSigns and Symptoms: Epidural HematomaRein VillanuevaNo ratings yet
- Stroke: Etiology, Classification, and EpidemiologyDocument34 pagesStroke: Etiology, Classification, and EpidemiologySteffNo ratings yet
- Journal 222Document1 pageJournal 222Gabriela CuestaNo ratings yet
- Journal 1111Document1 pageJournal 1111Gabriela CuestaNo ratings yet
- Stroke: Etiology, Classification, and EpidemiologyDocument34 pagesStroke: Etiology, Classification, and EpidemiologySteffNo ratings yet
- Ppt. Patho Head InjuryDocument56 pagesPpt. Patho Head Injurybermejomelody6877100% (3)
- Brain Injury: Closed (Blunt) Brain Injury Occurs When The Head Accelerates and ThenDocument7 pagesBrain Injury: Closed (Blunt) Brain Injury Occurs When The Head Accelerates and Thencute_tineeNo ratings yet
- Stroke MsDocument57 pagesStroke MsAishwarya ShahNo ratings yet
- A Brain Hemorrhage Is A Type of StrokeDocument2 pagesA Brain Hemorrhage Is A Type of StrokeuzmajbnNo ratings yet
- Subdural HematomaDocument3 pagesSubdural HematomaFaadela Ali-BissessarNo ratings yet
- Traumatic Brain Injury: Department of Neurosurgery, The First Affiliated Hospital of Zhengzhou University Xu BinDocument95 pagesTraumatic Brain Injury: Department of Neurosurgery, The First Affiliated Hospital of Zhengzhou University Xu Binapi-19916399No ratings yet
- Stroke: By: Georgina Vega Period 4 AnatomyDocument8 pagesStroke: By: Georgina Vega Period 4 AnatomyGina VegaNo ratings yet
- Types of Brain HemorrhageDocument2 pagesTypes of Brain HemorrhageRichie Marie BajaNo ratings yet
- Stroke: Joan Marie Amamio BSN IV Report byDocument35 pagesStroke: Joan Marie Amamio BSN IV Report byAnjo Marie AmamioNo ratings yet
- Neurological System DisordersDocument41 pagesNeurological System DisordersJoanna Ephraim CruzNo ratings yet
- Stroke: DefinitionDocument8 pagesStroke: DefinitionKasuganti koteshwar raoNo ratings yet
- Cerebro Vascular AccidentDocument16 pagesCerebro Vascular Accidentaldrich_muncalNo ratings yet
- Traumatic Brain InJuryDocument21 pagesTraumatic Brain InJuryShara SampangNo ratings yet
- REPORTDocument34 pagesREPORTClaire GidoNo ratings yet
- Lecture 3Document41 pagesLecture 3issrafil mussaNo ratings yet
- Cerebrovascular DiseasesDocument15 pagesCerebrovascular DiseaseskiflomNo ratings yet
- Cerebrovascular DiseasesDocument15 pagesCerebrovascular DiseaseskiflomNo ratings yet
- Head InjuryDocument11 pagesHead InjurypertinenteNo ratings yet
- PBL 2 - StrokeDocument14 pagesPBL 2 - StrokeKong Pei IngNo ratings yet
- LP SHDocument14 pagesLP SHLara larantikaNo ratings yet
- Disusun Oleh: Ichtiyar Rizki Zerniansyah Tingkat IV / Semester VIII P27820714019Document20 pagesDisusun Oleh: Ichtiyar Rizki Zerniansyah Tingkat IV / Semester VIII P27820714019RaniauliaNo ratings yet
- Pathophysiology Ischemic Stroke - VinaDocument2 pagesPathophysiology Ischemic Stroke - VinaDevi Astri KusumawardaniNo ratings yet
- What Is StrokeDocument2 pagesWhat Is StrokeFatma Sari MasithaNo ratings yet
- Subarachnoid Hemorrhage - Stroke (CVA) - Merck Manual Home Edition2Document8 pagesSubarachnoid Hemorrhage - Stroke (CVA) - Merck Manual Home Edition2Noval LiadyNo ratings yet
- Ronny Yusyanto. Head InjuryDocument12 pagesRonny Yusyanto. Head InjuryFerdyNo ratings yet
- Askep Stroke Periode AkutDocument19 pagesAskep Stroke Periode AkutRusma WitwickyNo ratings yet
- Attack, Also Called A TIA or "Mini-Stroke." A TIA Occurs IfDocument12 pagesAttack, Also Called A TIA or "Mini-Stroke." A TIA Occurs IfMary Rose F. MalaluanNo ratings yet
- Head Trauma: George Ayoub - Med3Document23 pagesHead Trauma: George Ayoub - Med3Joe KhdeirNo ratings yet
- Anaphysio 9b Cva Bleed Vs InfarctDocument5 pagesAnaphysio 9b Cva Bleed Vs InfarctAngayan, Merry GraceNo ratings yet
- Subdural HematomaDocument54 pagesSubdural HematomaNuzhat Noor Ayesha100% (1)
- Disease of Nervous System Lect 2Document62 pagesDisease of Nervous System Lect 2Monirul IslamNo ratings yet
- LP Stroke Hemoragik OkDocument18 pagesLP Stroke Hemoragik OkramidahNo ratings yet
- Stroke 1Document51 pagesStroke 1fatmaabdelazizNo ratings yet
- Stroke (Brain Attack) : Frontal Lobe (Blue)Document6 pagesStroke (Brain Attack) : Frontal Lobe (Blue)Pauline ChanNo ratings yet
- Impact of StrokeDocument2 pagesImpact of StrokeFauziah eka santiNo ratings yet
- Neurology LecturesDocument348 pagesNeurology LecturesRaj DeepakNo ratings yet
- STROKE: Handbook with activities, exercises and mental challengesFrom EverandSTROKE: Handbook with activities, exercises and mental challengesNo ratings yet
- Cerebral Edema, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCerebral Edema, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Crafts of Eastern Asia Are A Testament To The RegionDocument1 pageCrafts of Eastern Asia Are A Testament To The RegionbellaNo ratings yet
- 5es Revised FinalDocument10 pages5es Revised FinalbellaNo ratings yet
- Popular Culture Course OutlineDocument5 pagesPopular Culture Course OutlinebellaNo ratings yet
- Lesson Plan Earth and SpaceDocument4 pagesLesson Plan Earth and SpacebellaNo ratings yet
- Development of The Periodic Table Lesson PlanDocument9 pagesDevelopment of The Periodic Table Lesson Planbella100% (1)
- Cerebral AneurysmDocument6 pagesCerebral AneurysmNavjot BrarNo ratings yet
- Neurology Passmedicine & Onexamination Notes 2016Document158 pagesNeurology Passmedicine & Onexamination Notes 2016Muhammad Haneef100% (2)
- Neurological Impact of Coronavirus Disease, Practical Considerations For The Neuroscience CommunityDocument33 pagesNeurological Impact of Coronavirus Disease, Practical Considerations For The Neuroscience CommunityArtur Cordeiro100% (1)
- Neonatal Neurosonography: A Pictorial Essay: Venkatraman Bhat, Varun BhatDocument19 pagesNeonatal Neurosonography: A Pictorial Essay: Venkatraman Bhat, Varun BhatHeitor Bittencourt Netto0% (1)
- Hemorrhagic Cerebro Vascular DiseaseDocument37 pagesHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- Cerebrovascular Accident (Cva) : DescriptionDocument12 pagesCerebrovascular Accident (Cva) : DescriptionAbeera AhmadNo ratings yet
- Subarachnoid Hemorrhage: Beyond Aneurysms: Carrie P. Marder Vinod Narla James R. Fink Kathleen R. Tozer FinkDocument13 pagesSubarachnoid Hemorrhage: Beyond Aneurysms: Carrie P. Marder Vinod Narla James R. Fink Kathleen R. Tozer FinkDaylamiNo ratings yet
- AHA ASA-AV Malformation 2017Document25 pagesAHA ASA-AV Malformation 2017Kym DominguezNo ratings yet
- Neuromuscular System: Med SurgDocument25 pagesNeuromuscular System: Med Surgp23bhatiaNo ratings yet
- Basic Approch To CT BrainDocument62 pagesBasic Approch To CT BrainS B SayedNo ratings yet
- Diagnosing Secondary and Primary Headache Disorders: Review ArticleDocument14 pagesDiagnosing Secondary and Primary Headache Disorders: Review ArticleMD IurieNo ratings yet
- Neurology SyllabusDocument42 pagesNeurology SyllabusCHALAPATHI ENJAPURINo ratings yet
- DjlnknekjecDocument7 pagesDjlnknekjecRafaelNo ratings yet
- Cerebrospinal Fluid Dynamics in Non-Acute Post-Traumatic VentriculomegalyDocument10 pagesCerebrospinal Fluid Dynamics in Non-Acute Post-Traumatic VentriculomegalyDespina Aphroditi LalouNo ratings yet
- What Is A Brain Aneurysm?Document2 pagesWhat Is A Brain Aneurysm?shinNo ratings yet
- Hemorragia SubaracnoideaDocument40 pagesHemorragia SubaracnoideaEdwin Jofred Torres HuamaniNo ratings yet
- Stroke 1Document43 pagesStroke 1n&t3000No ratings yet
- CCRN Cert Review Neuro 2Document15 pagesCCRN Cert Review Neuro 2Giovanni MictilNo ratings yet
- Initial Assessment and Management of Acute StrokeDocument49 pagesInitial Assessment and Management of Acute StrokeIrina DuceacNo ratings yet
- Kasus Perdarahan Intrakranial Pada Bayi Baru LahirDocument58 pagesKasus Perdarahan Intrakranial Pada Bayi Baru LahirSilvia PAgitta TariganNo ratings yet
- Intracranial HemorrhageDocument41 pagesIntracranial Hemorrhagedoctormussieaberra100% (1)
- Acute Stroke CaseDocument19 pagesAcute Stroke CaseAsep BageurNo ratings yet
- External HydrocephalusDocument6 pagesExternal HydrocephalusJorge VergaraNo ratings yet
- Askep StrokeDocument46 pagesAskep Strokesybilla17No ratings yet
- Stroke and Subarachnoid HaemorrhageDocument69 pagesStroke and Subarachnoid HaemorrhagePrincewill SmithNo ratings yet
- Raised Intracranial PressureDocument6 pagesRaised Intracranial PressureindihimmakhairaniNo ratings yet
- Neuropathology PDFDocument205 pagesNeuropathology PDFNarendraNo ratings yet
- Cerebrospinal Fluid (CSF) AnalysisDocument8 pagesCerebrospinal Fluid (CSF) AnalysisVidhya.MNo ratings yet