Professional Documents
Culture Documents
Renal and Urinary Tract Problems
Renal and Urinary Tract Problems
Uploaded by
Rubie T. Igdalino0 ratings0% found this document useful (0 votes)
6 views6 pagesOriginal Title
Renal And Urinary Tract Problems
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
6 views6 pagesRenal and Urinary Tract Problems
Renal and Urinary Tract Problems
Uploaded by
Rubie T. IgdalinoCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 6
Hyponatremia
Serum sodium level lower than 135 mEq/L.
Sodium imbalances are mostly associate with fluid volume imbalances.
Causes
Loss of Sodium
Excessive Diaphoresis
Diuretics
Serum Dilution
Diarrhea
Kidney Problems
Hypoaldosteronism
Lack of Sodium
Fasting
NPO
Low Sodium Diet
Serum Dilution
Syndrome of Inappropriate Anti-Diuretic Hormone (SIADH)
Overhydration
Hyperglycemia
Fresh Water Drowning
Assessments
Increased Heart Rate
Shallow Breathing (Weak Respiratory Muscles)
Generalized Body Weakness
Negative Deep Tendon Reflex
Headache
Confusion, Seizures, Coma
Increased Motility
Diarrhea
Polyuria
Dry Mucous Membrane
Interventions
Monitor Vital Signs
If hyponatremia is accompanied by Fluid Volume Deficit:
Start IV Sodium Chloride Infusion (PNSS)
If hyponatremia is accompanied by Fluid Volume Excess:
Give Osmotic Diuretics (Mannitol IV)
If hyponatremia is accompanied by SIADH
Give ADH Antagonizers (Tolvaptan or Conivaptan)
High Sodium Diet
Processed Food
Bacon
Milk
Snacks
Cheese
Special Nursing Considerations
If the client is taking Lithium, monitor the Lithium Level.
Hyponatremia can cause Diminished Lithium Excretion.
Hence, Hyponatremia causes Lithium Toxicity.
Hypernatremia
Serum sodium level higher than 145 mEq/L.
Causes
Decreased Sodium Excretion
Corticosteroids
Cushing’s Syndrome
Kidney Disease
Hyperaldosteronism
Increased Sodium Intake
Excessive Oral Sodium Intake
Excessive Administration of Sodium-Containing IV Fluids
Decreased Water Intake
Fasting
NPO
Increased Water Loss
Assessments
Increased Blood Pressure
Tachycardia
Pulmonary Edema (If hypervolemia is present)
Twitches (Early)
Weakness (Late)
Altered Cerebral Function (Most Common)
Extreme Thirst
Dry Skin, Mucous Membranes, Sticky Tongue
Interventions
Monitor Vital Signs
If has fluid loss: Prepare IV Infusions
If caused by inadequate renal excretion: Administer Diuretics
Restrict sodium and fluid intake
Hypocalcemia
Serum calcium level lower than 9.0 mg/dL
Causes
Low calcium absorption in GI Tract
Calcium is absorbed in the GI Tract
Low Calcium Intake
Lactose Intolerance
o Milk is rich source of calcium
Malabsorption Syndromes:
o Celiac Disease
Lack of villous area in GI Tract
o Crohn Disease
Inflamed lower GI Tract
Inadequate intake of Vitamin D (Calciferol)
o Vitamin D increases absorption of calcium in GI Tract
End-Stage Kidney Disease
o CKD causes Hyperphosphatemia and decreased production of
Vitamin D
Increased Calcium Excretion
Polyuric Phase of Kidney Disease
Diarrhea
Steatorrhea
o Depletion of fat-soluble vitamin D may cause calcium deficiency
Wound Drainage
Decreased Ionized Fraction of Calcium
Ionized fraction of calcium is those that freely circulating the body.
Hyperproteinemia
Alkalosis
o It promotes the binding of calcium to albumin, which reduce the
fraction of ionized calcium in the blood.
Steatorrhea
Calcium Binders
Acute Pancreatitis
o Calcium is saponified by release of pancreatic lipase.
Hyperphosphatemia
o Inversely proportional with Calcium
Removal of Parathyroid Gland
o This gland regulates calcium levels in the blood.
Assessment
Bradycardia
Hypotension
Bradypnea
Twitches (Part of Triple T)
Tetany (Part of Triple T)
Watch out for signs of respiratory arrest.
+ Trousseau’s Sign (Part of Triple T)
Taas ng Kamay
+ Chvostek’s Sign
Cheeks
Hyperactive Bowl & Diarrhea
Interventions
Monitor Vital Signs
Place the patient on a Cardiac Monitor
Administer Calcium: Oral or Intravenous
For IV Administration, warm the injection solution to body temperature.
Administer slowly
Monitor ECG Changes
Monitor for Hypercalcemia
Administer medications that increase Calcium absorption
Aluminum Hydroxide
o Reduces Phosphorus Levels
o Increases Calcium Levels
Vitamin D (Calciferol)
o Aids in absorption of Calcium in the GI Tract
Provide a quiet environment
Initiate seizure precautions
Be careful when moving the patient
At risk for Pathologic Fracture
Standby Calcium Gluconate
Increase calcium in the diet
Dairy Products
Milk
Green Leafy Vegetables
Hypercalcemia
Serum calcium level higher than 10.5 mEq/L
Causes
Increased Calcium Absorption in GI Tract
Excessive Oral Intake of Calcium
Excessive Oral Intake of Vitamin D
Decreased Calcium Excretion
Kidney Disease
Use of Thiazide Diuretics
o It increases renal reabsorption of Calcium
Increased Bone Resorption of Calcium
Hyperparathyroidism
Hyperthyroidism
Malignancy
o Bone Destruction from Metastatic Tumor
Immobility
Glucocorticoids
Hemoconcentration
Dehydration
Use of Lithium
o It causes Hyperplasia of Parathyroid Gland
Increases Parathyroid Hormone
PTH increases Calcium
Adrenal Insufficiency
o Reduced Calcium Excretion by the Kidney
This increases calcium entry into the circulation.
Assessments
Tachycardia
Hypertension
Bradypnea
Due to Skeletal Muscle Weakness
PROFOUND MUSCLE WEAKNESS
Lethargy, Coma, Death
ECG Changes
Shortened ST Interval
Widened T Wave
Interventions
Monitor Vital Signs
Place the patient on a Cardiac Monitor
Discontinue IVF/Meds containing Calcium and Vitamin D
Discontinue Thiazide Diuretics
It can be replaced with Loop Diuretics
*At risk for Pathologic Fracture*
o Bumetanide (Bumex)
o Furosemide (Lasix)
o Ethacrynic Acid (Edecrin) If all fails to
Administer drugs that inhibit calcium resorption: lower down
Phosphorus calcium, prepare
Calcitonin (Miacalcin) the patient for
Biphosphonates Dialysis.
o Alendronate (Fosamax)
o Residronate (Actonel)
Prostaglandin Synthesis Inhibitor (Acetylsalicylic acid)
NSAID’s
Monitor the patient for Flank Pain
To check for presence of Urinary Stones
Monitor for signs of Pathologic Fracture
You might also like
- CPR ScriptDocument13 pagesCPR ScriptMary Benjie BandelariaNo ratings yet
- Delusions: Presenter: DR Srinivas Chair Person: Dr.V.V.SESHAMMADocument42 pagesDelusions: Presenter: DR Srinivas Chair Person: Dr.V.V.SESHAMMANirmal QwertyNo ratings yet
- Fluid Electrolyte Balances and ImbalanceDocument157 pagesFluid Electrolyte Balances and ImbalanceManisha Shakya0% (1)
- EndocrinologyDocument34 pagesEndocrinologymiyuchix100% (2)
- Renal Tubular Acidosis SlideshareDocument31 pagesRenal Tubular Acidosis Slidesharehector100% (1)
- Med Micro AlgorithmsDocument2 pagesMed Micro Algorithmsgregoryvo100% (11)
- Electrolyte ImbalanceDocument54 pagesElectrolyte ImbalanceJEM93No ratings yet
- Hyperparathyroidsm HANDOUTDocument2 pagesHyperparathyroidsm HANDOUTmendellianNo ratings yet
- Electrolyte ImbalancesDocument8 pagesElectrolyte Imbalancesdonna mae junioNo ratings yet
- Calcium ImbalancesDocument7 pagesCalcium ImbalancesLorelyn Santos CorpuzNo ratings yet
- F18 N320 FE and ABG PowerpointDocument41 pagesF18 N320 FE and ABG Powerpointfetalposition00No ratings yet
- Hypercalcemia (F&e)Document3 pagesHypercalcemia (F&e)Sarah Grace CajucomNo ratings yet
- Hyperparathyroidism and HypoparathyroidismDocument44 pagesHyperparathyroidism and Hypoparathyroidismshweta singhNo ratings yet
- Hypocalcemia: Dept of Nephrology PsriDocument40 pagesHypocalcemia: Dept of Nephrology Psriind78No ratings yet
- FLUIDS AND ELECTROLYTES MNGTDocument44 pagesFLUIDS AND ELECTROLYTES MNGTremerose100% (1)
- ElectrolytesDocument60 pagesElectrolytesnmukila2No ratings yet
- Calcium Regulation: 800-1200 Mg/dayDocument3 pagesCalcium Regulation: 800-1200 Mg/dayclarheenaNo ratings yet
- Management For HypoparathyroidismDocument6 pagesManagement For Hypoparathyroidismansherina100% (1)
- Fluids and Electrolytes, Acid-Base ImbalancesDocument15 pagesFluids and Electrolytes, Acid-Base ImbalancesJherome FernandoNo ratings yet
- HypercalcemiaDocument50 pagesHypercalcemiaEvelyn EdgarNo ratings yet
- Drug StudyDocument20 pagesDrug StudyBrylle CapiliNo ratings yet
- Wk8 - Electrolyte Imbalances & Acid-Base ImbalancesDocument65 pagesWk8 - Electrolyte Imbalances & Acid-Base ImbalancesPotato PceeNo ratings yet
- Electrolye CheatDocument6 pagesElectrolye CheatKatie RoyNo ratings yet
- Alteration in Fluid and Electrolyte ImbalanceDocument118 pagesAlteration in Fluid and Electrolyte ImbalanceRenuga SureshNo ratings yet
- Electrolytes & FluidimbalancesDocument80 pagesElectrolytes & FluidimbalancesDennis Nyambane MomanyiNo ratings yet
- Electrolytes Slide 21Document111 pagesElectrolytes Slide 21Elaisha Mae C. CarsulaNo ratings yet
- Electrolyte ChartDocument8 pagesElectrolyte ChartCharli SlodovNo ratings yet
- English Comp Electrolytes Mdb-AnalytesDocument11 pagesEnglish Comp Electrolytes Mdb-AnalytesaxmedjiinjeaxmedNo ratings yet
- Function Maintain Homeostatic Balance With Respect To Fluids, Electrolytes, and Organic SolutesDocument8 pagesFunction Maintain Homeostatic Balance With Respect To Fluids, Electrolytes, and Organic SolutesNikki SalivioNo ratings yet
- Electrolytes SummaryDocument3 pagesElectrolytes SummaryMutya XDNo ratings yet
- Common ElectrolyteDocument48 pagesCommon ElectrolytemekuriawNo ratings yet
- Electrolyte ImbalancesDocument41 pagesElectrolyte ImbalancesReignallienn Inocencio MartinNo ratings yet
- Disturbances of Fluid and Electrolyte BalanceDocument3 pagesDisturbances of Fluid and Electrolyte BalanceJezel B. AnadonNo ratings yet
- Renal Disease of Small AnimalsDocument46 pagesRenal Disease of Small AnimalsTahir KasimNo ratings yet
- FE2 OutlineDocument9 pagesFE2 Outlineapi-3697326No ratings yet
- Biochemisty Cheat SheetsDocument4 pagesBiochemisty Cheat SheetsNatalie KingNo ratings yet
- Electrolytes Imbalances: Prepared By: Mr. Charlie C. Falguera, RNDocument35 pagesElectrolytes Imbalances: Prepared By: Mr. Charlie C. Falguera, RNJarvin RenomeronNo ratings yet
- NCM 112 Fluid and Electrolytes: Hyperkalemia or Potassium ExcessDocument2 pagesNCM 112 Fluid and Electrolytes: Hyperkalemia or Potassium ExcessAngeline NavarroNo ratings yet
- 2 DiureticsDocument23 pages2 DiureticsAudrey Beatrice ReyesNo ratings yet
- Hepatic Cirrhosis: de Los Santos, Kristine Bernadette R. Usana, Noah Billy D.RDocument26 pagesHepatic Cirrhosis: de Los Santos, Kristine Bernadette R. Usana, Noah Billy D.RBernadette De Los SantosNo ratings yet
- Fluid N Electrolyte BalanceDocument60 pagesFluid N Electrolyte BalanceAnusha Verghese67% (3)
- Chronic Renal FailureDocument3 pagesChronic Renal FailureirismgallNo ratings yet
- Fluid Electrolyte Imbalance n132 160210135651Document100 pagesFluid Electrolyte Imbalance n132 160210135651Shahan FarooqNo ratings yet
- Hypokalemia: Presented By: Group 4 Dolfo, Dominise, Ejercito, FloraldeDocument20 pagesHypokalemia: Presented By: Group 4 Dolfo, Dominise, Ejercito, FloraldeKyle De Sagun OtedaNo ratings yet
- Fluid ImbalancesDocument43 pagesFluid ImbalancesHarold DiasanaNo ratings yet
- Fluidandelectrolyte TodayDocument76 pagesFluidandelectrolyte TodayPrithvi MagarNo ratings yet
- CHF Drug StudyDocument4 pagesCHF Drug StudyAiza Apelada-NievaNo ratings yet
- Mark Billy L. Perpetua, Man RN: Fluids, Electrolytes andDocument96 pagesMark Billy L. Perpetua, Man RN: Fluids, Electrolytes andMaica LectanaNo ratings yet
- Hipokalsemia WikiDocument5 pagesHipokalsemia Wikiagee_quakerNo ratings yet
- Drugs For Maintaining Calcium Homeostasis:: ParathormoneDocument4 pagesDrugs For Maintaining Calcium Homeostasis:: Parathormonenafiul islamNo ratings yet
- WEEK 9 Disorders of The Parathyroid GlandsDocument2 pagesWEEK 9 Disorders of The Parathyroid GlandsJiro MarianoNo ratings yet
- Chronic Renal FailureDocument3 pagesChronic Renal FailureJashine DajayNo ratings yet
- Parathyroid GlandsDocument3 pagesParathyroid GlandsStrong Woman Bong SoonNo ratings yet
- Hypercalcemia: Bibek Ghimire 3 Batch, PAHSDocument25 pagesHypercalcemia: Bibek Ghimire 3 Batch, PAHSBibek GhimireNo ratings yet
- 3A - BOLDIOS Electrolytes Tabular ComparisonDocument20 pages3A - BOLDIOS Electrolytes Tabular ComparisonPsyche Valerie BoldiosNo ratings yet
- Calcium (HypoHypercalcemia) ImbalanceDocument13 pagesCalcium (HypoHypercalcemia) ImbalanceReabetsoe LebesaNo ratings yet
- Hypocalcaemia - Wikipedia PDFDocument4 pagesHypocalcaemia - Wikipedia PDFYvonne WongNo ratings yet
- 2.3 HYPOCALCEMIA and HYPERCALCEMIADocument7 pages2.3 HYPOCALCEMIA and HYPERCALCEMIABooz Waief CaluzaNo ratings yet
- ATI Med Surg TipsDocument17 pagesATI Med Surg Tipsmike Gee100% (5)
- Fluidandelectrolyteimbalance2 220412174955Document39 pagesFluidandelectrolyteimbalance2 220412174955. anil dev.No ratings yet
- Prometric Medical Surgical TipsDocument11 pagesPrometric Medical Surgical TipstmanareNo ratings yet
- Liver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesFrom EverandLiver Cirrhosis, A Simple Guide To The Condition, Treatment And Related DiseasesNo ratings yet
- Impaired Gas ExchangeDocument3 pagesImpaired Gas ExchangePaul VincentNo ratings yet
- The Bethesda System For Reporting Cervical Cytolog PDFDocument359 pagesThe Bethesda System For Reporting Cervical Cytolog PDFsurekhaNo ratings yet
- PolioDocument4 pagesPolioShambhu NathNo ratings yet
- A Case of Beauvieux'S Syndrome and Its EvolutionDocument7 pagesA Case of Beauvieux'S Syndrome and Its EvolutionAndrea ModestieNo ratings yet
- Enterobiasis (Pinworm) and Trichuriasis (Whipworm) - UpToDateDocument23 pagesEnterobiasis (Pinworm) and Trichuriasis (Whipworm) - UpToDateFrank Harry LampardNo ratings yet
- Pregnancy: Signs/Symptoms and Common Health ConcernsDocument5 pagesPregnancy: Signs/Symptoms and Common Health ConcernsTracy50% (2)
- Latest Packages Ayushman Bharat and HIMCARE 3-CompressedDocument630 pagesLatest Packages Ayushman Bharat and HIMCARE 3-Compressedlove gumberNo ratings yet
- The 4 Stages of Habituation (2018)Document1 pageThe 4 Stages of Habituation (2018)Joe BlowNo ratings yet
- Config 10Document9 pagesConfig 10Lindsey K. AliceaNo ratings yet
- Alere Cholestech LDX System: Complete Lipid ProfileDocument2 pagesAlere Cholestech LDX System: Complete Lipid ProfileRoberto NutiNo ratings yet
- A Prospective Study in Analgesic Effect of Distal Sodium Channel Blockers (DSCB) in Patients With SciaticaDocument5 pagesA Prospective Study in Analgesic Effect of Distal Sodium Channel Blockers (DSCB) in Patients With SciaticaInternational Journal of Innovative Science and Research Technology100% (1)
- RCH PALS Study Guide - Web-121514Document5 pagesRCH PALS Study Guide - Web-121514Ryan N Brandy CooperNo ratings yet
- Supercillin™Document2 pagesSupercillin™Samuel BallouNo ratings yet
- Oral Minoxidil 2023Document10 pagesOral Minoxidil 2023maat1No ratings yet
- NCPDocument3 pagesNCPLeslie PaguioNo ratings yet
- Topic 1: Molecules, Transport and Health Chapter 1B: Mammalian Transport SystemsDocument4 pagesTopic 1: Molecules, Transport and Health Chapter 1B: Mammalian Transport SystemsMariam El KhatibNo ratings yet
- Instructions For Use: Read Carefully Before UseDocument36 pagesInstructions For Use: Read Carefully Before UseCorey EasleyNo ratings yet
- Daftar Pasien Neurologi SELASA, 02 MARET 2021: Lontara 3 Saraf Kamar 1Document5 pagesDaftar Pasien Neurologi SELASA, 02 MARET 2021: Lontara 3 Saraf Kamar 1Louis MailuhuNo ratings yet
- Trastuzumab MonographDocument11 pagesTrastuzumab MonographAmeliaNo ratings yet
- Nursing Care Plan: Assessment Explanation of The Problem Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Assessment Explanation of The Problem Objectives Interventions Rationale EvaluationNelly CruzNo ratings yet
- Latihan Amali: Wja 102:balutan Ringkas 9 NOVEMBER 2020Document19 pagesLatihan Amali: Wja 102:balutan Ringkas 9 NOVEMBER 2020pei yeu tehNo ratings yet
- PRO Post Natal AssessmentDocument9 pagesPRO Post Natal AssessmentMali KanuNo ratings yet
- Zamle Mock Exam 2019 2Document44 pagesZamle Mock Exam 2019 2ct303 uuuNo ratings yet
- African Swine Fever: Now in WidespreadDocument2 pagesAfrican Swine Fever: Now in WidespreadMariaGlenda Dellosa Guevara-YusonNo ratings yet
- Virology LecturesDocument72 pagesVirology LecturesKrishma GuptaNo ratings yet
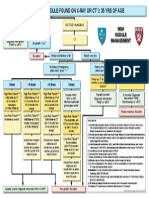
- Algorithm For Solitary Lung NoduleDocument1 pageAlgorithm For Solitary Lung NoduleMargaretDeniseDelRosarioNo ratings yet
- 450 Midterm AdimeDocument2 pages450 Midterm Adimeapi-384372769No ratings yet