Professional Documents
Culture Documents
NATURE - Sex-Related Similarities and Differences in Responses To Heart Failure Therapies (Chyou Et Al., 2024)
NATURE - Sex-Related Similarities and Differences in Responses To Heart Failure Therapies (Chyou Et Al., 2024)
Uploaded by
Marcelo TrCopyright:
Available Formats
You might also like
- Boylan - The Spiritual Life of The PriestDocument63 pagesBoylan - The Spiritual Life of The Priestpablotrollano100% (1)
- Module 2 1 Math 10 Graphs of Polynomial Functions FinalDocument29 pagesModule 2 1 Math 10 Graphs of Polynomial Functions FinalJacob Sanchez100% (1)
- Update On Psychotropic Medication Use in Renal DiseaseDocument15 pagesUpdate On Psychotropic Medication Use in Renal DiseaseMartinaNo ratings yet
- 2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in CarDocument16 pages2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in CarAngie OvandoNo ratings yet
- Chapter 69Document8 pagesChapter 69ingbarragan87No ratings yet
- Importance of Pharmacogenomics in The Personalized MedicineDocument6 pagesImportance of Pharmacogenomics in The Personalized MedicineJames AustinNo ratings yet
- Adv Pharmacology - AnswerDocument7 pagesAdv Pharmacology - AnswerMEHATHI SUBASHNo ratings yet
- Patel 2017Document11 pagesPatel 2017Imanuel CristiantoNo ratings yet
- 2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in Ca1Document17 pages2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in Ca1Angie OvandoNo ratings yet
- Pharmacogenetics of Cardiovascular Drug TherapyDocument11 pagesPharmacogenetics of Cardiovascular Drug Therapybalaji5563No ratings yet
- Adrs For WomenDocument9 pagesAdrs For WomenFajar PutraNo ratings yet
- Gender Differences in Disease Manifestation and PresentationDocument5 pagesGender Differences in Disease Manifestation and PresentationGustavo Anzola100% (1)
- Cubała W. (ZOLPIDEM) 0Document2 pagesCubała W. (ZOLPIDEM) 0Antonio SanchezNo ratings yet
- Combination Medical Therapy For Lower Urinary Tract Symptoms and Benign Prostatic HyperplasiaDocument9 pagesCombination Medical Therapy For Lower Urinary Tract Symptoms and Benign Prostatic HyperplasiaganangahimsaNo ratings yet
- Erectile Dysfunction and HypertensionDocument8 pagesErectile Dysfunction and HypertensionILham SyahNo ratings yet
- 2017 - Behavioral Emergencies - Geriatric Psychiatric PatientDocument14 pages2017 - Behavioral Emergencies - Geriatric Psychiatric PatientAna María Arenas DávilaNo ratings yet
- Prescribing Pattern of Antihypertensive Drugs in A Tertiary Care Hospital in Jammu-A Descriptive StudyDocument4 pagesPrescribing Pattern of Antihypertensive Drugs in A Tertiary Care Hospital in Jammu-A Descriptive StudyMahantesh NyayakarNo ratings yet
- Key Points To RememberDocument37 pagesKey Points To RememberheikalNo ratings yet
- AJGP 0102 2023 Focus Chung Male Sexual Dysfunction WEBDocument5 pagesAJGP 0102 2023 Focus Chung Male Sexual Dysfunction WEBrisang akrima fikriNo ratings yet
- Pharmacotherapy For Cardiovascular Disorders EditedDocument5 pagesPharmacotherapy For Cardiovascular Disorders Editedhutwriters2No ratings yet
- Piis2050052117300744 PDFDocument15 pagesPiis2050052117300744 PDFRichu UhcirNo ratings yet
- Diet and Men 'S Sexual Health: Rates of Male Sexual DysfunctionsDocument15 pagesDiet and Men 'S Sexual Health: Rates of Male Sexual DysfunctionsHoa VânNo ratings yet
- Heart Failure With Preserved Ejection Fraction - JAMA (2023)Document12 pagesHeart Failure With Preserved Ejection Fraction - JAMA (2023)cheve glzNo ratings yet
- Redfield Margaret M Heart Failure With PreservedDocument12 pagesRedfield Margaret M Heart Failure With PreservedNathan Kulkys MarquesNo ratings yet
- Solomon 2006Document5 pagesSolomon 2006Ottofianus Hewick KalangiNo ratings yet
- Erectile Dysfunction and Comorbid Diseases, Androgen Deficiency, and Diminished Libido in MenDocument7 pagesErectile Dysfunction and Comorbid Diseases, Androgen Deficiency, and Diminished Libido in MenAfif Al FatihNo ratings yet
- Captura de Pantalla 2022-08-15 A La(s) 17.37.40 PDFDocument11 pagesCaptura de Pantalla 2022-08-15 A La(s) 17.37.40 PDFMatias PadillaNo ratings yet
- Pharmaceutics 15 01002 v3Document20 pagesPharmaceutics 15 01002 v3YASH BNo ratings yet
- Chew Et Al-2008-Journal of The American Geriatrics Society PDFDocument9 pagesChew Et Al-2008-Journal of The American Geriatrics Society PDFChrysoula GkaniNo ratings yet
- JNC8Document21 pagesJNC8ZakisyarifudintaqiyNo ratings yet
- Pharmacological and Parenteral Therapies in Older Adult PopulationDocument5 pagesPharmacological and Parenteral Therapies in Older Adult PopulationNDINDA GODYFREEY NATTOHNo ratings yet
- Geriatric Drug TherapyDocument48 pagesGeriatric Drug Therapywalt65No ratings yet
- AndrologyDocument298 pagesAndrologyPrakash JanakiramanNo ratings yet
- Hulley 1998Document9 pagesHulley 1998junta.propietarios.1456No ratings yet
- Variation of Drug Response-1Document26 pagesVariation of Drug Response-1كسلان اكتب اسميNo ratings yet
- Management of Constipation in Patients With Schizophrenia - A Case Study and Review of LiteratureDocument7 pagesManagement of Constipation in Patients With Schizophrenia - A Case Study and Review of LiteratureRimayNo ratings yet
- Hormone Replacement HerapyDocument5 pagesHormone Replacement HerapyCindy HartNo ratings yet
- Cfs 8 PDFDocument9 pagesCfs 8 PDFDaniel Fernando Mendez CarbajalNo ratings yet
- Risk Related To Hormone Therapy and Cardiovascular Disease in WomenDocument44 pagesRisk Related To Hormone Therapy and Cardiovascular Disease in Womenosama saeedNo ratings yet
- Pharmacogenetics and The Concept of Individualized Medicine: BS ShastryDocument6 pagesPharmacogenetics and The Concept of Individualized Medicine: BS Shastrykunalprabhu148No ratings yet
- Cardiology PDFDocument9 pagesCardiology PDFFC Mekar AbadiNo ratings yet
- Ultrafiltration Therapy For Cardiorenal Syndrome Physiologic Basis and Contemporary OptionsDocument9 pagesUltrafiltration Therapy For Cardiorenal Syndrome Physiologic Basis and Contemporary Optionsfernando.suarez.mtzNo ratings yet
- Cancer-Relatedfatiguein Cancersurvivorship: Chidinma C. Ebede,, Yongchang Jang,, Carmen P. EscalanteDocument13 pagesCancer-Relatedfatiguein Cancersurvivorship: Chidinma C. Ebede,, Yongchang Jang,, Carmen P. EscalanteMahdhun ShiddiqNo ratings yet
- Reversibledementias: Milta O. LittleDocument26 pagesReversibledementias: Milta O. LittleLUCAS IGNACIO SANCHEZNo ratings yet
- Interacciones Medicamentos en Odontologia 2017 PDFDocument35 pagesInteracciones Medicamentos en Odontologia 2017 PDFDANIELA PARRA BOTERONo ratings yet
- 1 s2.0 S0735109723003686 MainDocument19 pages1 s2.0 S0735109723003686 MainArunNo ratings yet
- Hudmon 2007Document4 pagesHudmon 2007ARAFAT MIAHNo ratings yet
- Preventive Cardiology For WomenDocument5 pagesPreventive Cardiology For WomenninataniaaaNo ratings yet
- CollegePharmacy BHRT Abstracts ReviewsDocument46 pagesCollegePharmacy BHRT Abstracts ReviewsJoyce IpadNo ratings yet
- Ethn 15 01 116Document8 pagesEthn 15 01 116Bot AINo ratings yet
- Gerotological Care IssuesDocument21 pagesGerotological Care IssuesOdey GodwinNo ratings yet
- Case StudiesDocument5 pagesCase Studiespragna novaNo ratings yet
- Prescribing For The ElderlyDocument8 pagesPrescribing For The ElderlykarladeyNo ratings yet
- Comparative Effectiveness of Diuretic Regimens: EditorialDocument2 pagesComparative Effectiveness of Diuretic Regimens: EditorialFabio Luis Padilla AvilaNo ratings yet
- Geriatric Pharmacology. Journal of The American Podriatric Medical AssociationDocument8 pagesGeriatric Pharmacology. Journal of The American Podriatric Medical AssociationJose Fernando Díez ConchaNo ratings yet
- Examining The Effects of Herbs On TestosteroneDocument22 pagesExamining The Effects of Herbs On TestosteroneKelson dos SantosNo ratings yet
- Evidence Based Care For All Patients - AjmDocument3 pagesEvidence Based Care For All Patients - Ajmdaniel martinNo ratings yet
- Consenso IccDocument15 pagesConsenso IccMaida Martinez AngelesNo ratings yet
- David J. Greenblatt D. (ZOLPIDEM) 2Document9 pagesDavid J. Greenblatt D. (ZOLPIDEM) 2Antonio SanchezNo ratings yet
- Top 5 - Considerations For Anesthesia of A Geriatric PatientDocument5 pagesTop 5 - Considerations For Anesthesia of A Geriatric PatientMabe AguirreNo ratings yet
- The Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianFrom EverandThe Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 4: VascularFrom EverandComplementary and Alternative Medical Lab Testing Part 4: VascularNo ratings yet
- Hprocedure of Export or ImportDocument96 pagesHprocedure of Export or ImportHiren RatnaniNo ratings yet
- IntroductionDocument15 pagesIntroductionAhinurNo ratings yet
- Star Holman 210HX Conveyor OvenDocument2 pagesStar Holman 210HX Conveyor Ovenwsfc-ebayNo ratings yet
- Global Warming (Word Formation)Document2 pagesGlobal Warming (Word Formation)EvaNo ratings yet
- Bba 400 Module Revised 2017 April To DsvolDocument68 pagesBba 400 Module Revised 2017 April To DsvolKafonyi JohnNo ratings yet
- IfDocument44 pagesIfSean RoxasNo ratings yet
- The Wall Street Journal - Vol. 277 No. 075 (01 Apr 2021)Document32 pagesThe Wall Street Journal - Vol. 277 No. 075 (01 Apr 2021)Andrei StrăchinescuNo ratings yet
- Islam Articles of FaithDocument1 pageIslam Articles of Faithapi-247725573No ratings yet
- AlgecirasDocument7 pagesAlgecirasEvrenNo ratings yet
- NavAid Module 2.0Document21 pagesNavAid Module 2.0Kiel HerreraNo ratings yet
- Putra, 003 - 3035 - I Wayan Adi Pranata - GalleyDocument7 pagesPutra, 003 - 3035 - I Wayan Adi Pranata - Galleyeunike jaequelineNo ratings yet
- Beyond Risk - Bacterial Biofilms and Their Regulating ApproachesDocument20 pagesBeyond Risk - Bacterial Biofilms and Their Regulating ApproachesVictor HugoNo ratings yet
- Måttblad Bauer BK P7112BGM CatalogueB2010 0312 en A4 Chapter12Document54 pagesMåttblad Bauer BK P7112BGM CatalogueB2010 0312 en A4 Chapter12earrNo ratings yet
- Physics 158 Final Exam Review Package: UBC Engineering Undergraduate SocietyDocument22 pagesPhysics 158 Final Exam Review Package: UBC Engineering Undergraduate SocietySpam MailNo ratings yet
- Crawling Under A Broken Moon 05Document28 pagesCrawling Under A Broken Moon 05Maxim BorisovNo ratings yet
- Soil Pollution: Causes, Effects and Control: January 2016Document15 pagesSoil Pollution: Causes, Effects and Control: January 2016Nagateja MondretiNo ratings yet
- 520SL SLB Guide en USDocument2 pages520SL SLB Guide en USBruce CanvasNo ratings yet
- CASE REPORT On OsteomyelitisDocument30 pagesCASE REPORT On OsteomyelitisNirbhay KatiyarNo ratings yet
- TCS Ninja English Questions and AnswersDocument16 pagesTCS Ninja English Questions and AnswersVijayPrajapatiNo ratings yet
- DER Vol III DrawingDocument50 pagesDER Vol III Drawingdaryl sabadoNo ratings yet
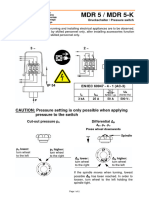
- Pressure Switch MDR5Document4 pagesPressure Switch MDR5Fidelis NdanoNo ratings yet
- User'S Manual: Questions?Document32 pagesUser'S Manual: Questions?gorleanosNo ratings yet
- 04 Vikram Pawar Volume 3 Issue 2Document18 pages04 Vikram Pawar Volume 3 Issue 2Juwan JafferNo ratings yet
- Composite EbookDocument285 pagesComposite Ebooksunilas218408100% (1)
- L-s20 Specification For Road Lighting InstallationDocument82 pagesL-s20 Specification For Road Lighting Installationzamanhuri junidNo ratings yet
- Equivalent Length Calculator - RevADocument10 pagesEquivalent Length Calculator - RevArkrajan1502No ratings yet
- (M. J. Edwards) The ''Epistle To Rheginus'' ValenDocument17 pages(M. J. Edwards) The ''Epistle To Rheginus'' ValenGlebMatveevNo ratings yet
- Bristow Part B EC155B1 Section 2 LimitationsDocument4 pagesBristow Part B EC155B1 Section 2 LimitationsrobbertmdNo ratings yet
NATURE - Sex-Related Similarities and Differences in Responses To Heart Failure Therapies (Chyou Et Al., 2024)
NATURE - Sex-Related Similarities and Differences in Responses To Heart Failure Therapies (Chyou Et Al., 2024)
Uploaded by
Marcelo TrOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NATURE - Sex-Related Similarities and Differences in Responses To Heart Failure Therapies (Chyou Et Al., 2024)
NATURE - Sex-Related Similarities and Differences in Responses To Heart Failure Therapies (Chyou Et Al., 2024)
Uploaded by
Marcelo TrCopyright:
Available Formats
nature reviews cardiology https://doi.org/10.
1038/s41569-024-00996-1
Review article Check for updates
Sex-related similarities and
differences in responses to
heart failure therapies
Janice Y. Chyou1,6, Hailun Qin 2,6
, Javed Butler3,4, Adriaan A. Voors 2
& Carolyn S. P. Lam 5
Abstract Sections
Although sex-related differences in the epidemiology, risk factors, Introduction
clinical characteristics and outcomes of heart failure are well known, Response to pharmacological
investigations in the past decade have shed light on an often overlooked therapy for HF
aspect of heart failure: the influence of sex on treatment response. Response to device therapy
for HF
Sex-related differences in anatomy, physiology, pharmacokinetics,
pharmacodynamics and psychosocial factors might influence the Response to cardiac
rehabilitation in HF
response to pharmacological agents, device therapy and cardiac
Challenges and opportunities
rehabilitation in patients with heart failure. In this Review, we discuss
the similarities between men and women in their response to heart Conclusions
failure therapies, as well as the sex-related differences in treatment
benefits, dose–response relationships, and tolerability and safety
of guideline-directed medical therapy, device therapy and cardiac
rehabilitation. We provide insights into the unique challenges faced
by men and women with heart failure, highlight potential avenues for
tailored therapeutic approaches and call for sex-specific evaluation
of treatment efficacy and safety in future research.
1
Cardiovascular Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA. 2Department of Cardiology,
University of Groningen, University Medical Centre Groningen, Groningen, Netherlands. 3Department of Medicine,
University of Mississippi School of Medicine, Jackson, MS, USA. 4Baylor Scott and White Research Institute, Dallas,
TX, USA. 5National Heart Centre Singapore and Duke-NUS Medical School, Singapore, Singapore. 6These authors
contributed equally: Janice Y. Chyou and Hailun Qin. e-mail: carolyn.lam@duke-nus.edu.sg
Nature Reviews Cardiology
Review article
Key points patients with HF. By examining studies focused on the efficacy and
safety of pharmacological interventions, device-based therapies
and cardiac rehabilitation (Fig. 1), we provide insights into the unique
•• Men and women with heart failure with reduced ejection challenges faced by male and female patients with HF and highlight
fraction derive similar benefits from pharmacotherapy with potential avenues for tailored therapeutic approaches.
renin–angiotensin system inhibitors, angiotensin receptor–neprilysin
inhibitors, β-blockers, mineralocorticoid receptor antagonists and Response to pharmacological therapy for HF
sodium–glucose cotransporter 2 inhibitors. The cornerstone of HF guideline-directed medical therapy (GDMT) in
both men and women includes renin–angiotensin system (RAS) inhibi-
•• In patients with heart failure with preserved ejection fraction, tors or angiotensin receptor–neprilysin inhibitors (ARNI), β-blockers,
treatment heterogeneity by sex has been observed with angiotensin mineralocorticoid receptor antagonists (MRAs) and sodium–glucose
receptor–neprilysin inhibitors and spironolactone, whereby women cotransporter 2 (SGLT2) inhibitors18–20. Sex-specific differences in
seem to derive greater benefit than men. anatomy and physiology can influence the pharmacokinetics and
pharmacodynamics of these HF medications21,22.
•• Optimal doses of renin–angiotensin–aldosterone system
inhibitors and β-blockers might be lower in women than in men, Sex-related differences in pharmacokinetics and
whereas adverse effects, such as dry cough and angio-oedema with pharmacodynamics
angiotensin-converting enzyme inhibitors, might be more common in Sex-related differences exist in the pharmacokinetics of HF medica-
women than in men. tions, including drug absorption, distribution, metabolism and elimina-
tion (Fig. 2). For drug absorption, women have a higher gastric pH and
•• Among patients with left bundle branch block, women derive greater slower gastric emptying time than men, which can delay and/or reduce
benefit from cardiac resynchronization therapy at a shorter QRS the absorption of drugs that require an acidic environment21. Body
duration for reducing mortality than men. composition, organ blood flow, plasma volume and protein binding all
influence how drugs are distributed throughout the body. In general,
•• In relation to the patient-oriented outcomes of quality of life and women have lower body weight, lower total body water (intracellular
functional status, women derive similar benefits from baroreceptor and extracellular) content, lower plasma volume and smaller organ
activation therapy but less benefit from mitral valve intervention size than men, but have a higher proportion of body fat23. These differ-
compared with men. ences might contribute to a larger volume of distribution, faster onset
and longer duration of action for lipophilic drugs in women than in
•• Women with heart failure might derive greater benefit from cardiac men (and, conversely, a smaller volume of distribution and relatively
rehabilitation than men but have lower rates of enrolment and higher concentrations for hydrophilic drugs in women than in men).
adherence. Sex-related differences in the activity of hepatic enzymes might also
influence treatment responses, given that many HF drugs are metab
olized by cytochrome P450 (CYP) isoenzymes, and some CYP isoen-
Introduction zymes have been shown to differ by sex (particularly CYP3A4, which
The sex-related differences in heart failure (HF) are well known1,2. Tra- has higher activity levels in women)24,25. Women generally have lower
ditional risk factors such as hypertension, diabetes mellitus, obesity renal blood flow, estimated glomerular filtration rate, and tubular secre-
and smoking have a more potent influence on the risk of HF in women tion, transport and reabsorption than men26,27. Therefore, drugs that
than in men3–7. Additional sex-specific risk factors in women are related are primarily inactivated or excreted by the kidneys might be cleared
to sex hormones, pregnancy and gestational complications, propen- more slowly in women than in men.
sity and treatment for breast cancer, as well as autoimmune diseases In healthy volunteers given a single oral dose (5 mg) of the RAS inhib-
and the associated inflammatory and immune system milieu8. HF in itor ramipril, women showed a higher area under the concentration–
women is marked by pathophysiological predominance of endothelial time curve (AUC/kg) of the active metabolite ramiprilat than men28.
inflammation and microvascular dysfunction compared with HF in Plasma concentrations of the RAS inhibitor losartan were approxi-
men9–11. The epidemiology of HF is notable for a higher prevalence of mately two times higher in women than in men with hypertension,
HF with preserved ejection fraction (HFpEF) in women, higher preva- but the concentrations of the active metabolites of losartan were
lence of non-ischaemic cardiomyopathy among women with HF, female similar across both sexes29. Although the pharmacokinetics of the
preponderance in Takotsubo cardiomyopathy, and the sex-specific RAS inhibitor irbesartan were not affected by sex in healthy partici-
entity of peripartum cardiomyopathy12–14. Compared with men with pants, women with hypertension had higher plasma irbesartan lev-
HF, women with HF are generally older, more likely to be physically els than men29,30. Among healthy young men and women receiving
frail, more symptomatic and have worse self-reported health status, irbesartan 75 mg for 4 weeks, which increased to 150 mg for a further
yet better survival15,16. Therefore, although among patients with HF, 4 weeks, women had increased sensitivity to RAS modulation and
women outlive men, their additional years of life are of poorer quality17. thus might require lower dosages of irbesartan than men to achieve
Extensive research has been dedicated to understanding these a similar response31.
sex-related differences in epidemiology, risk factors, clinical char- Compared with men, women have a lower activity of the CYP2D6
acteristics and outcomes in HF, but investigations in the past decade enzyme, which metabolizes the β-blocker metoprolol, and thus a slower
have shed light on an often-overlooked aspect: the influence of sex on body clearance, greater exposure and higher plasma levels of metopro-
treatment responses. In this Review, we comprehensively evaluate the lol after normalizing for body weight32–34. In healthy individuals receiv-
current literature on sex-related differences in treatment response in ing metoprolol 100 mg twice daily for a total of nine doses, women had
Nature Reviews Cardiology
Review article
a Pharmacological therapy b Device therapy c Cardiac rehabilitation
Counselling
Autonomic Electrical conduction Mental health Education
Medication
• ACE inhibitors, nervous system • Defibrillation
ARBs, ARNI • Modulation • Pacing
• β-Blockers • Resynchronization
• MRAs Stress Physical activity
• SGLT2 inhibitors
Anatomical remodelling
• Modification Lifestyle modification
• Haemodynamic support
Women have: Anatomy: Cardiac electrical system: • Lower self-reported physical function
• Lower body weight • Narrower QRS complexes • Increased prevalence of frailty
• Lower total body water content • Longer QTc interval • Increased fear of exercise
• Greater body fat percentages Anatomy: • More comorbidities
• Smaller organ size • Smaller LV mass and volume • Older age at heart failure diagnosis
• Smaller body surface area • Thinner myocardial walls • Greater psychological burdens
Pharmacokinetics and pharmacodynamics: • Predisposition to LV concentric remodelling
• Higher gastric pH Cardiac autonomic nervous system:
• Slower gastric emptying time • Higher resting heart rates
• Different enzyme activity levels • Lower sympathetic activities
Fig. 1 | Sex-specific considerations in heart failure therapy. Women are under- inhibitors. Sex-related differences in anatomy and physiology can influence the
represented in randomized clinical trials and some therapies for heart pharmacokinetics and pharmacodynamics of heart failure medications.
failure are underutilized in women. Encouragingly, these gaps have gradually b, The three major domains of therapeutic targets for device therapies in heart
narrowed over time. In approximately 70% of trials on heart failure therapies, failure are the electrical conduction system, anatomical remodelling and the
outcome data were reported by sex, and only a minority (5%) of the trials autonomic nervous system. Therapeutic interventions have primary targets
detected significant variation in treatment effects by sex. a, The cornerstone but can have additional effects on other domains. c, Cardiac rehabilitation is a
of heart failure guideline-directed medical therapy in both men and women comprehensive non-pharmacological intervention that is underutilized among
includes loop diuretics, renin–angiotensin system inhibitors, angiotensin women and adherence is particularly low in women. ACE, angiotensin-converting
receptor–neprilysin inhibitors (ARNI), β-blockers, mineralocorticoid enzyme; ARB, angiotensin-receptor blocker; LV, left ventricular.
receptor antagonists (MRAs) and sodium–glucose cotransporter 2 (SGLT2)
higher maximum plasma concentrations (146 ng/ml versus 85.5 ng/ml) from treatment with the ARB candesartan up to a higher left ventricular
and AUC values (867 µg/h/l versus 417 µg/h/l) of metoprolol than men32. ejection fraction (LVEF) range than men57.
Similarly, a clinical trial simulation model found that, after receiving A significant differential treatment response between men and
100 mg of metoprolol, healthy men had a faster metoprolol absorption women was found in two trials in patients with HF with LVEF ≥45%. In the
and clearance rates than women35. The pharmacokinetics of 100 mg of PARAGON-HF trial36, sex was an independent treatment effect modifier
metoprolol in men were roughly similar to the pharmacokinetics (unadjusted P for interaction 0.017), wherein women derived greater
of 50 mg of metoprolol in women35. benefit from sacubitril–valsartan versus valsartan for the primary com-
Importantly, in prospective, randomized, controlled trials (RCTs) posite outcome of total HF hospitalizations and cardiovascular death
assessing GDMT in patients with HF, achieved doses of ARNI 36,37, (rate ratio for the primary outcome 0.73, 95% CI 0.59–0.90) compared
β-blockers38 and vericiguat39 were similar between men and women. with men (rate ratio 1.03, 95% CI 0.84–1.25). However, men had a greater
Therefore, pharmacokinetic and pharmacodynamic differences improvement in the Kansas City Cardiomyopathy Questionnaire clini-
between men and women do not seem to translate into clinically mean- cal summary score than women in response to sacubitril–valsartan
ingful differences in achievable doses of GDMT for HF, at least in the treatment, and similar improvements in New York Heart Association
context of prospective clinical trials. (NYHA) class and renal function were observed between women and
men36. No sex-related differences in the effect of spironolactone on
Sex-related differences in treatment benefit with GDMT the primary composite outcome (death from cardiovascular causes,
Although sex differences in the response to pharmacological HF ther- aborted cardiac arrest or HF hospitalization) were found in the overall
apy are important to consider, the similarities are equally important. TOPCAT population (P for interaction 0.99)58. However, when restricted
In the big picture, GDMT for HF with reduced ejection fraction (HFrEF) to the TOPCAT-Americas cohort (which included only the participants
is strongly indicated in both men and women on the basis of consist- from Argentina, Brazil, Canada and the USA), sex was found to signifi-
ent overall treatment benefits in both sexes demonstrated in large cantly modify the treatment effect of spironolactone on all-cause death
outcomes trials40–47, including for angiotensin-converting enzyme (P for interaction 0.024); when compared with placebo, spironolactone
(ACE) inhibitors47, angiotensin-receptor blockers (ARBs)48, ARNI42, reduced all-cause death in women (by 34%), but not in men59.
β-blockers49, MRAs50, SGLT2 inhibitors44,51 and ivabradine52. Similarly, In the PARAGON-HF trial36, sex-specific spline analyses of treat-
in patients with HFpEF, no significant treatment heterogeneity by sex ment effect across the LVEF spectrum showed that the benefit of
has been observed for the primary outcomes in large clinical trials sacubitril–valsartan treatment seemed to extend to a higher LVEF
of ACE inhibitors or ARBs53–55, or SGLT2 inhibitors56 (Fig. 3; Table 1). range in women than in men, both for the primary composite end point
However, in the CHARM programme, women seemed to derive benefit and for total HF hospitalizations (Table 1). By contrast, in men, the
Nature Reviews Cardiology
Review article
Higher in men Fig. 2 | Sex-related differences in
Factors affecting drug distribution pharmacokinetics. In general, compared
and metabolism Drug with men, women have lower body weight,
• Body surface area, organ size and therapy total body water content and cardiac output,
blood flow
• Total body water content and higher gastric pH and slower gastric emptying
plasma volume time, smaller organ size and body surface
• Volume of distribution for area, and greater body fat percentages, all of
water-soluble drugs
which affect the absorption and distribution
Factors affecting drug distribution of drugs. The sex-specific differences in the
and metabolism Higher in women activity of metabolizing enzymes in the liver
• Cardiac output, lung volume
Factors affecting drug metabolism and the lower glomerular filtration rate in
• Functional capacity
• Levels of CYP1A2, CYP2D6, CYP2E1 • CYP2A6, CYP2B6, CYP3A4 women might also affect drug elimination.
enzyme activity enzyme activity
• Xanthine oxidase,
CYP, cytochrome P450; eGFR, estimated
• Levels of UGTs, methyltransferase,
N-acetyltransferases glomerular filtration rate; UGTs, uridine
sulfotransferase
diphosphate glucuronosyltransferases.
Factors affecting drug elimination Factors affecting drug elimination
• Liver metabolism • Elimination half-life
• Renal blood flow, eGFR
• Tubular secretion and reabsorption Factors affecting drug distribution
• Body fat content
Factors affecting drug absorption • Volume of distribution for
• Gastric acid secretion and gastric lipophilic drugs
emptying
• Gastrointestinal transit time and rate
drug was only beneficial in those with a lower LVEF36. In the TOPCAT of patients in the DIG study, among whom only 20% were women, and
trial60, the interaction between treatment and LVEF (stronger benefit thus statistical power was insufficient for further sex-specific analyses.
in patients with a lower LVEF) for the primary outcome also seemed to Although the sex-related differences described above are nota-
differ by sex, wherein women across the LVEF spectrum benefited from ble, some of these findings are from post hoc subgroup analyses of
spironolactone treatment, whereas in men, the benefit was limited trials that had neutral results for their primary outcome analyses
to those with a lower LVEF (P for interaction 0.077). A similar pattern (PARAGON-HF, TOPCAT and CHARM-Preserved)36,57,58. Furthermore,
was observed in the CHARM-Preserved trial with candesartan for the the overwhelming evidence from large clinical trials of neurohormonal
primary composite outcome of first occurrence of HF hospitalization agents in patients with HF across the LVEF spectrum indicate similar
or cardiovascular death57. These observed sex-related differences in effect modification by LVEF in men and women (greater benefit at
treatment response across the LVEF spectrum in patients with HF, which lower LVEF) for the primary end point, calling into question the clini-
were consistent across different neurohormonal drugs (ARNI, MRAs cal significance of sex-related differences in component or secondary
and ARBs), have been postulated to be related to known sex differences end points. Conversely, the under-representation of women in clinical
in cardiac remodelling with age and risk factors such as hypertension. trials, especially in smaller HF studies (CONSENSUS68, US Carvedilol
Greater concentric cardiac remodelling in women resulted in smaller HF study69 and RALES70) might limit the ability to detect sex-related
left ventricular volumes and higher LVEF (higher stroke volume for a differences by interaction testing.
given left ventricular end-diastolic volume) in women than in men61. In aggregate, the evidence suggests that sex modifies the response
Indeed, in the general population, the distribution of LVEF is shifted to ARNI and spironolactone in patients with HFpEF. Indeed, there are
towards higher values in women than in men16,62,63, with a normal LVEF in now sex-specific considerations for GDMT in patients with HFpEF in
older women being closer to 60% compared with 55% in men. Therefore, the most recent American College of Cardiology Expert Consensus
women with HF and a LVEF of 50% have more adverse cardiac remodel- statement19, which recommends that the use of ARNI and spirono-
ling or contractile dysfunction than men, and thus might derive more lactone be considered across the entire LVEF spectrum in women
benefit from neurohormonal inhibitor therapies whose mechanism with HFpEF.
of action is promoting reverse cardiac remodelling64. Indeed, in the
PARAMOUNT trial65, women with HFpEF had greater systolic dysfunc- Sex-related differences in dose–response relationships with
tion (lower tissue S′ velocity), despite having a higher LVEF, than men GDMT
with HFpEF. In a large, prospective, multinational, observational HF study con-
Important sex-related differences in the response to pharma- ducted in patients across Europe, the lowest risk of the composite of
cological HF therapy have also been shown with digoxin. A post hoc, hospitalization for HF or all-cause death was observed in women with
sex-specific subgroup analysis of the DIG study66 found that treatment HFrEF who had received ~40% of the recommended target doses of
with digoxin significantly increased all-cause mortality among women ACE inhibitors and ARB, whereas in men with HFrEF, the lowest risk
but not among men (P for interaction 0.034). Women had greater serum was found in those who achieved 100% of the recommended target
digoxin concentrations than men at 1 month after treatment initiation doses71. For β-blockers, women with HFrEF had the lowest risk of the
(1.05 ng/ml versus 0.96 ng/ml; P = 0.003), and serum digoxin concen- composite outcome at ~60% of the recommended target doses, whereas
trations exceeding the upper limit of therapeutic range (>2.0 ng/ml) the lowest risk in men with HFrEF was observed at 100% of the target
were found in 4% of women, twice the percentage found in men67. How- doses71. These findings were validated in a separate prospective, mul-
ever, the serum digoxin concentration was only tested in a subgroup tinational, observational HF study in patients across Asia71. Although
Nature Reviews Cardiology
Review article
hypothesis-generating, these observational, non-randomized results adverse drug reactions in women might be attributable to sex-related
should be interpreted with caution. differences in the pharmacokinetics and pharmacodynamics of the
Two RCTs compared the effects of a low dose versus a high dose of drug treatments, resulting in higher doses of drugs per kilogram of
an ACE inhibitor and an ARB on clinical outcomes in patients with HFrEF. body weight in women than in men; to biological differences, such as
The ATLAS trial72 compared a low dose (2.5–5.0 mg per day) versus a longer corrected QT interval in women or differences in circulating
high dose (32.5–35 mg per day) of lisinopril in patients with HFrEF. hormone levels; or to greater polypharmacy in women, with the asso-
Patients receiving the higher dose had a significant 12% lower risk of ciated increased potential for drug–drug interactions76,78. Indeed, a
death or hospitalization for any reason and 24% fewer hospitalizations report published in 2023 highlighted that more women than men with
for HF. Interestingly, no additional benefit of the high dose of lisinopril HF were prescribed medications that might cause or exacerbate HF
was found in women compared with the low dose, and the positive (such as inhaled sympathomimetics, diltiazem and antidepressants)79.
results were completely driven by the effects seen in men. The HEAAL Despite a 1.5 to 1.7 times higher likelihood of adverse drug reactions
trial73 compared the effects of losartan 50 mg versus losartan 150 mg in women than in men80, only 11 (7%) clinical trials of pharmacological HF
on death or HF hospitalization in patients with HFrEF. Patients who therapies have found sex-specific adverse drug reactions21,74,81. Among
were assigned to the higher dose had a significantly lower event rate them, three studies found that women have a higher risk of adverse reac-
than those assigned to the lower dose, and this result was completely tions with ACE inhibitors81. In a post hoc analysis from the SOLVD trial82,
driven by a beneficial effect of the higher dose in men but not in women dry cough after taking enalapril occurred approximately 1.4 times more
(P for interaction 0.018)73. frequently in women than in men. In a retrospective cohort study from
In aggregate, these data suggest that the optimal doses of ACE the USA, the cumulative incidence of new-onset angio-oedema with
inhibitors or ARBs and β-blockers might be lower in women than in ACE inhibitor treatment in patients with HF was more than twofold
men with HF. However, given that the trials that formed the evidence higher in women than in men83. No sex-related differences in adverse
base for HF management guideline recommendations used the same drug reactions were observed in clinical trials of ARBs and β-blockers81.
target doses for men and for women, sex-specific target doses cannot A pooled analysis of three landmark trials of MRAs (RALES, EMPHASIS-HF
be recommended at this time. Nonetheless, future trials should be and TOPCAT) showed no sex-specific differences in adverse drug reac-
designed with the consideration of potential sex-specific differences tions (all P for interaction >0.1), including worsening renal function and
in target doses to best optimize the benefit–risk ratio in both women hyperkalaemia43. Moreover, a small study including 134 patients with HF
and men with HF. found that a comparable number of men and women treated with
spironolactone withdrew from the study because of hyperkalaemia or
Tolerability of GDMT in men and women worsening renal function (and gynaecomastia in men)84. In the DAPA-HF
Women are known to experience more adverse effects from cardiovas- and DELIVER trials, which assessed SGLT2 inhibitors, men treated with
cular medications and generally have a higher rate of hospital admis- dapagliflozin were more likely to experience severe adverse events,
sions for adverse drug reactions than men74–77. The increased risk of but women were more likely to experience adverse events leading to
Men Similarities between men and women Women
• Sacubitril–valsartan reduced the risk • Similar response to ACE inhibitors, • Higher mortality with digoxin
of hospitalization for heart failure to a ARBs, ARNI, β-blockers, MRAs and • Lower optimal dose for ACE inhibitors,
lesser degree in men with HFpEF SGLT2 inhibitors in HFrEF ARBs and β-blockers
than in women with HFpEF • Similar response to ACE inhibitors, • Higher incidence of dry cough and
• Spironolactone did not reduce ARBs and SGLT2 inhibitors in HFpEF angio-oedema with ACE inhibitors
all-cause death in men with HFpEF, • Largely similar in achieved dose and • Lower rate of enrolment and adherence
but reduced all-cause death in adherence in cardiac rehabilitation
women with HFpEF • Predominantly similar in adverse • Might benefit more from cardiac
drug reactions rehabilitation
Fig. 3 | Sex-based considerations in the response to pharmacological and and spironolactone therapies in men and women with HFpEF are different.
non-pharmacological therapies for heart failure. Men and women with The achieved dose and adherence to heart failure guideline-directed medical
heart failure with reduced ejection fraction (HFrEF) have similar treatment therapies are largely similar in men and women. Women have lower optimal
response to angiotensin-converting enzyme (ACE) inhibitors or angiotensin- doses of ACE inhibitors, ARBs and β-blockers than men. Adverse drug reactions
receptor blockers (ARBs), angiotensin receptor–neprilysin inhibitors (ARNI), are predominantly similar in both sexes. However, women have a higher
β-blockers, mineralocorticoid receptor antagonists (MRAs) and sodium–glucose incidence of dry cough and angio-oedema with ACE inhibitors than men.
cotransporter 2 (SGLT2) inhibitors. No evidence of treatment heterogeneity In general, women have lower rates of enrolment into clinical trials and treatment
by sex has been observed for the primary outcomes of large clinical trials of adherence than men, but women might derive more benefit from cardiac
ACE inhibitors or ARBs and SGLT2 inhibitors in patients with heart failure rehabilitation than men.
with preserved ejection fraction (HFpEF). However, the responses to ARNI
Nature Reviews Cardiology
Review article
Table 1 | Landmark clinical trials of drug therapy in men and women with HF
Trial (year) Drug Number Mean Mean Primary end point RR or HR (95% CI) P for interaction
of patients age LVEF
(% women) (years) (%) Men Women Sex Treatment Treatment,
or sex and sex and
LVEF LVEF
ACE inhibitors
CONSENSUS (1987)a Enalapril 253 (30) 71 ≤35 Mortality 0.41 (0.16–0.58) 1.01 (0.59–1.73) NA NA NA
(refs. 68,231)
SOLVD-Treatment Enalapril 2,569 (20) 61 25 Mortality Favourable treatment outcomes in NA NA
(1991)232,233 both sexes, but the effect seemed
to be greater in men
Meta-analysis of ACE inhibitors 7,105 (22) NA NA Mortality 0.76 (0.65–0.88) 0.79 NA NA NA
32 RCTs (1995)47 (0.59–1.06)
Mortality or 0.63 (0.55–0.73) 0.78 NA NA NA
hospitalization (0.59–1.04)
Angiotensin-receptor blockers
Val-HeFT (2005)234 Valsartan 5,010 (20) 63 27 Mortality and 0.84 (0.67–1.06) 0.87 NS NA NA
morbidity (0.78–0.98)
Non-fatal morbidity 0.74 (0.56–0.99) 0.72 NS NA NA
(0.61–0.84)
Hospitalization 0.78 (0.59–1.04) 0.71 NS NA NA
for HF (0.60–0.83)
CHARM Candesartan 7,599 (32) 66 39 Cardiovascular 0.84 (0.76–0.92) 0.84 0.9939 0.0146b; 0.0649
programme death (0.73–0.97) 0.73c
(2007)53,57
Hospitalization Reference 0.83
for HF group (0.76–0.91)
Mortality Reference 0.77 NA 0.65c NA
group (0.69–0.86)
I-PRESERVE Irbesartan 4,128 (60) 71 60 Mortality or 0.96 (0.83–1.12) 0.94 0.78 NA NA
(2008)54,235 hospitalization (0.82–1.08)
for specified
cardiovascular cause
Angiotensin receptor–neprilysin inhibitors
PARADIGM-HF Sacubitril– 8,399 (22) 64 29 Cardiovascular Significant Significant 0.63 NA NA
(2014)42 valsartan death or benefitd benefitd
hospitalization
for HF
Cardiovascular Significant Trend towards 0.92 NA NA
death benefitd benefitd
PARAGON-HF Sacubitril– 4,769 (52) 72 57 Cardiovascular 1.02 (0.83–1.24) 0.73 0.0225 NA NA
(2020)36 valsartan death or (0.60–0.90)
hospitalization
for HF
Mortality 0.95 (0.77–1.17) 0.99 0.8703 NA NA
(0.79–1.24)
Pooled analysis Sacubitril– 13,195 (33) 67 39.7 Cardiovascular 0.86 (0.79–0.93) 0.79 0.3452 0.0424b 0.032
(PARADIGM and valsartan death or (0.70–0.91)
PARAGON-HF) hospitalization
(2020)57,236 for HF
β-Blockers
US Carvedilol HF Carvedilol 1,094 (23) 58 22 Mortality 0.41 (0.22–0.80) 0.23 NS NA NA
Study (1996)69 (0.07–0.69)
CIBIS II (2001)237 Bisoprolol 2,647 (19) 61 28 Mortality Reference 0.64 NA NA NA
group (0.47–0.86)
MERIT-HF Metoprolol 3,991 (22.5) 64 28 Mortality Risk reduction Risk reduction NS NA NA
(1999)49,238 18% 21%
COPERNICUS Carvedilol 2,289 (20) 63 20 Mortality 0.65 0.65 NS NA NA
(2001)239
Nature Reviews Cardiology
Review article
Table 1 (continued) | Landmark clinical trials of drug therapy in men and women with HF
Trial (year) Drug Number Mean Mean Primary end point RR or HR (95% CI) P for interaction
of patients age LVEF
(% women) (years) (%) Men Women Sex Treatment Treatment,
or sex and sex and
LVEF LVEF
β-Blockers (continued)
Pooled data β-Blockers 8,927 (NA) NA NA Mortality Similar survival benefit in men and women
(CIBIS II, MERIT-HF
and COPERNICUS)
(2002)49
MRAs
RALES (1999)70 Spironolactone 1,663 (27) 65 25 Mortality Significant Significant NS NA NA
reductiond reductiond
EMPHASIS-HF Eplerenone 2,737 (22) 69 26 Cardiovascular Significant Significant 0.36 NA NA
(2011)50 death or hospitaliza reductiond reductiond
tion for HF
TOPCAT- Spironolactone 1,767 (49.9) 71 58 Cardiovascular 0.85 (0.67–1.08) 0.81 0.84 NA NA
Americas (2019)59 death, aborted (0.63–1.05)
cardiac arrest, or
hospitalization
for HF
Mortality 1.06 (0.81–1.39) 0.66 0.024 NA NA
(0.48–0.90)
Pooled analysis MRAs 6,167 (31) 69 35.3 Cardiovascular 0.70 (0.63–0.77) 0.71 0.8089 0.0074b 0.0682
(RALES, death or (0.60–0.84)
EMPHASIS-HF hospitalization
and TOPCAT- for HF
Americas) (2020)57
SGLT2 inhibitors
DAPA-HF Dapagliflozin 4,744 (23) 66 31 Cardiovascular 0.73 (0.63–0.85) 0.79 0.67 NA NA
(2019)44,240 death or (0.59–1.06)
worsening HF
EMPEROR- Empagliflozin 3,730 (24) 67 27 Cardiovascular 0.80 0.59 NS NA NA
Reduced (2020)51 death or (0.68–0.93) (0.44–0.80)
hospitalization
for worsening HF
EMPEROR- Empagliflozin 5,988 (45) 72 54 Cardiovascular 0.81 (0.69–0.96) 0.75 0.536 Men, 0.878
Preserved (2022)241 death or (0.61–0.92) 0.402b;
hospitalization women,
for worsening HF 0.587b
DELIVER (2022)242 Dapagliflozin 6,263 (44) 71 54 Cardiovascular 0.82 (0.71–0.96) 0.81 NS NA NA
death or (0.67–0.97)
worsening HF
Pooled analysis Dapagliflozin 11,007 (35) 70 44 Cardiovascular 0.78 (0.70–0.86) 0.80 0.77 0.71b 0.86
(DAPA-HF death or (0.68–0.94)
and DELIVER) worsening HF
(2022)85,243
Meta-analysis (five SGLT2 20,725 (36) NA NA Cardiovascular 0.78 (0.73–0.85) 0.74 0.45 NA NA
RCTs) (2022)56 inhibitors death or (0.66–0.84)
hospitalization
for HF
Digoxin
DIG (1997)66,244 Digoxin 6,800 (22) 63 28 Mortality 0.93 (0.85–1.02) 1.23 0.014 NA NA
(1.02–1.47)
DIG-PEF (2006)245 Digoxin 988 (41) 67 55 Mortality Reference 0.59 NA NA NA
group (0.43–0.82)
Hospitalization Reference 1.06 NA NA NA
for HF group (0.75–1.51)
ACE, angiotensin-converting enzyme; HF, heart failure; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid receptor antagonist; NA, not available; NS, not significant; RCT,
randomized controlled trial; RR, relative risk; SGLT2, sodium–glucose cotransporter 2. aAt 6 months, 66 of the 178 men and 22 of the 75 women had died; enalapril reduced mortality by 51%
in men and 6% in women (small number of women and wide confidence intervals). bInteraction between treatment and LVEF. cInteraction between sex and LVEF. dResults of sex subgroup
analyses were reported in forest plots; quantitative data were not provided.
Nature Reviews Cardiology
Review article
study drug cessation as well as study drug cessation for any reason85. Anatomical size and anatomical remodelling. Sex-related differences
No sex-related differences in adverse events were observed in the exist in anatomical size and anatomical remodelling. In the general pop-
dapagliflozin group (all P for interaction >0.1)85. ulation, women have smaller left ventricular cavities, greater diastolic
Notably, for the vast majority of HF clinical trials, sex-stratified dysfunction, and more concentric hypertrophy on echocardiography
adverse events were not reported, and this aspect has not improved studies than men95–97. Cardiac MRI data reveal that left ventricular vol-
over time81. Data safety monitoring in future clinical trials in patients umes indexed to body surface area are smaller in women than in men,
with HF should account for potential sex-related differences in adverse and that women have higher LVEF due to a higher stroke volume for a
events and they should be reported in a sex-disaggregated manner86. given left ventricular end-diastolic volume61. Cardiac remodelling in
the setting of HF is also influenced by older age and higher proportions
Response to device therapy for HF of non-ischaemic aetiology in women than in men12.
Sex-related differences in device therapies for HF might relate to dif-
ferences in biology, prevalence of associated conditions, therapeutic Cardiac autonomic nervous system. Premenopausal women have
responses, adverse procedural events and systemic barriers in thera- higher resting heart rates than men, consistently seen between the ages
peutic adoption. Therapeutic targets for device-based therapies for HF of 20 and 50 years and attenuating thereafter93,98. In healthy volunteers
fall into three major domains: the cardiac electrical system, anatomical aged <40 years, women had lower sympathetic activity (quantified
remodelling and the autonomic nervous system (Fig. 1). Sex-based by low-frequency component of heart rate variability) than men99.
considerations in HF device therapy incorporate domain-specific bio- In a middle-aged population (age 50 ± 6 years), baroreflex sensitivity
logical differences as well as cross-domain differences in risk factors, was lower in women without oestrogen therapy than in men, but was
pathophysiology, epidemiology, outcomes, symptoms, quality of life not significantly different between women taking oestrogen therapy
(QoL), functional capacity and challenges in clinical trial representation and men100,101.
and therapeutic adoption (Fig. 4).
Sex-related differences in response to device therapies
Sex-related biological differences Implantable cardioverter–defibrillator. Implantable cardioverter–
Cardiac electrical conduction system. Sex differences exist in cellular defibrillators (ICDs) are indicated for primary and secondary preven-
electrophysiology and in surface electrocardiography. On the cellular and tion of sudden cardiac death102,103. Among eligible patients with HF,
tissue level, sex differences exist in the expression of ion channels, ICDs are underutilized in all sexes104,105, but even more so in women16,
which are further modulated by sex hormones. Human cardiac tissues even after accounting for age39 and comorbidities106–111. Low referral
from donor hearts revealed reduced expression of potassium channel rates, financial concerns and inadequate knowledge about ICDs have
subunits involved in cardiac repolarization in the heart of female indi- been reported as potential reasons for ICD underutilization104,112,113. ICD
viduals compared with the heart of male individuals87. Sex hormones counselling and strategies to improve referral might help to address
(most notably oestradiol and testosterone) differentially influence sex-related differences in utilization. Among patients with HF who are
the ion channels, with implications for cardiac repolarization and eligible for an ICD, women received ICD counselling less frequently
excitability88. On surface electrocardiography, women have a shorter than men (19.3% versus 24.6%; P < 0.001); however, among those who
PR interval, a shorter effective refractory period of the atrioventricular received counselling, women and men received an ICD at similar
node, and a narrower QRS complex than men89–91. QT intervals cor- rates (63.1% versus 62.3%)114, suggesting that equitable ICD counsel-
rected for resting heart rates are approximately 20 ms longer in women ling might be a potential tool to address sex-related disparities in
than in men92. Significant sex differences in the QTc interval start to be ICD utilization. The use of a screening tool115 or electronic health
seen after puberty, persist through adulthood but attenuate in older record alert116 has been shown to improve referral of ICD-eligible
age, suggestive of the influence of sex hormones92–94. patients, among whom point-of-care alerts through electronic health
ain differe
-dom nc
oss es
Cr Cardiac electrical conduction Anatomical Autonomic modulation
ic al differe
g nc
olo es • Cardiac resynchronization therapy • LV assist device • Baroreflex activation therapy
Bi • Implantable cardioverter–defibrillator • Mitral valve procedure • Vagal nerve stimulation
i ce the rap
ev ie
D
• Narrower QRS complexes • Smaller LV mass • Higher resting heart rates
Domains of • Longer QTc (premenopause) • Smaller LV volume (premenopause)
therapeutic • Thinner myocardial walls • Lower sympathetic activity
target • Predisposition to LV concentric (healthy volunteers,
remodelling premenopause)
• Risk factors • Pathophysiology • Symptoms • Therapeutic adoption
• Epidemiology • Outcomes • Quality of life • Clinical trial representation
Fig. 4 | Factors influencing sex-related differences in device therapies for well as cross-domain differences in risk factors, pathophysiology, epidemiology,
heart failure. Sex-based considerations in response to device therapy for heart outcomes, symptoms, quality of life, functional capacity and challenges in
failure incorporate considerations of domain-specific baseline differences as clinical trial representation and therapeutic adoption. LV, left ventricular.
Nature Reviews Cardiology
Review article
records had a modestly greater effect in improving referral rates in Landmark RCTs evaluating CRT for HFrEF collectively established
women than in men, mitigating the sex-based gap otherwise seen the benefits of CRT in improving clinical outcomes and reducing mor-
with under-referral of women (in the study comparison group without tality, HF hospitalizations and HF symptoms, and improving QoL,
electronic alert)116. 6-min walking distance (6MWD)138–142 and left ventricular reverse
In landmark studies of the efficacy and indication for ICD thera- remodelling143 (Table 3). However, definitive RCT-level evidence for
pies for primary prevention in patients with HFrEF, women comprised sex-specific treatment response to CRT is not feasible because none of
only 10–29% of the study populations117–123 (Table 2). Sex-specific data the studies was powered to assess treatment response by sex specifi-
from the MADIT II trial118 and secondary analyses of the MUSTT124, cally given that women were under-represented (17–33% of the study
SCD-HeFT125 and DEFINITE126 trials found no significant sex-specific population in the landmark CRT trials)138–144. Although men and women
differences in the benefit derived from ICD. Although pooled analyses both benefit from CRT, data from post hoc analyses and registry studies
of several landmark studies have questioned the benefit of ICDs for suggest that women might derive more benefit than men, in terms of
reducing all-cause mortality in women127–129, a definitive interpreta- both clinical outcomes145–147 and left ventricular reverse remodelling148.
tion of findings from these pooled analyses127–129 has been difficult Baseline patient characteristics in trials of CRT are notable, with women
given the heterogeneity of the included trials, particularly with regard having shorter stature, smaller left ventricular end-diastolic diameter,
to the length of follow-up and the study population composition more LBBB and more non-ischaemic cardiomyopathy (less often ischae-
(especially concerning ischaemic versus non-ischaemic aetiology and mic cardiomyopathy) than men144,145,149. An analysis of the MADIT-CRT
concomitant use of cardiac resynchronization therapy (CRT)). study148 identified six baseline characteristics predictive of a favourable
A retrospective analysis of 14 European registries of ICD use for CRT response: female sex, LBBB, no previous myocardial infarction,
primary prevention revealed that women had lower mortality and fewer BMI <30 kg/m2 and smaller left atrial volume index. However, in a
appropriate ICD shocks than men after adjusting for age, ischaemic meta-analysis of five RCTs (CARE-HF, MIRACLE, REVERSE, MIRACLE
cardiomyopathy, LVEF ≤25% and concomitant CRT130. In a comparison ICD and RAFT), QRS duration was the only independent predictor
of an older US patient population from the National Cardiovascular of a reduction in all-cause mortality with CRT, and QRS duration and
Data Registry of ICD for primary prevention with propensity-matched height were independent predictors of CRT benefits in the composite
patients from the GWTG-HF registry without ICD, similar rates of reduc- outcome of all-cause mortality or HF hospitalization149.
tion in mortality were found in men and women with ICDs compared The extent and mitigation of left ventricular electrical delay are
with matched counterparts without ICDs, highlighting the similar central to the considerations for CRT150,151. Longer QRS duration in
benefit of ICD treatment in both sexes131. Appropriate shock was a LBBB (especially ≥150 ms) is associated with increased survival with
strong predictor of mortality in both men (HR 2.61, 95% CI 1.82–3.74; CRT-D in both sexes147. Among recipients of CRT-D in large national
P < 0.0001) and women (HR 5.99, 95% CI 2.75–13.02; P <0.0001)132. databases, women with LBBB had even greater mortality reduction
Of note, women received fewer inappropriate therapies than men than men with LBBB147,152. Women with LBBB derive benefit at a shorter
(9.2% versus 13.5%; P = 0.006)132. QRS duration than men with LBBB153,154, prompting ongoing discus-
Finally, although the initial RCTs establishing efficacy of ICDs sions for further sex-specific considerations for recommendations
as primary prevention therapy in patients with HF were based on for CRT155,156. The AdaptResponse RCT utilized sex-specific inclusion
transvenous ICD systems, the subcutaneous ICD system is a contem- criteria for QRS duration, which is likely to have contributed to the high
porary alternative for ICD therapy in individuals without need for portion of women (43.4%) in the trial157, paving the way for utilization
pacing. Data from the PRAETORIAN trial133 established that the sub- of sex-specific criteria158 in future clinical trials and in clinical practice.
cutaneous ICD was non-inferior to the transvenous ICD with respect With regard to the aetiology of the cardiomyopathy, a meta-
to device-related complications and the number of inappropriate analysis revealed that, whereas no sex-based differences were seen in
shocks. The UNTOUCHED trial134 demonstrated high safety and effi- CRT recipients with ischaemic cardiomyopathy, among CRT recipients
cacy, and a low rate of inappropriate shocks with contemporary with non-ischaemic cardiomyopathy, women had greater observed
second-generation and third-generation subcutaneous ICD systems. benefit than men149. A retrospective analysis of CRT recipients with
No significant differences in survival or inappropriate shock rates were non-ischaemic cardiomyopathy and LBBB suggests that the com-
seen between men and women in the IDE or EFFORTLESS registries135. plex interplay between QRS duration and heart size might explain
the observed sex-based differences in CRT response, in which a more
Cardiac resynchronization therapy. CRT can be part of a pacemaker favourable CRT response (defined in this study as an increase in LVEF,
system (CRT-P) or part of a defibrillator system (CRT-D). Guideline as determined by echocardiography) was seen in women, but women
recommendations for CRT are currently sex-neutral. In HFrEF, CRT also had a larger baseline index of QRS duration to heart size (with
is indicated in patients with NYHA class II, III or ambulatory IV HF generally smaller heart size than men), such that normalization of QRS
despite optimal pharmacological treatment, LVEF ≤35%, left bundle duration for heart size resolved the sex-based differences associated
branch block (LBBB) with a prolonged QRS duration of ≥150 ms, and in with the response to CRT159. A subsequent study extended this concept,
sinus rhythm as a class I recommendation in both the American136 and noting that normalization of QRS duration to left ventricular dimension
European137 guidelines. Class IIa recommendations in the American improved the prediction of survival after CRT implantation160.
guidelines136 include a QRS duration of 120–149 ms in sinus rhythm, Despite the benefits and indications, CRT is under-implemented
or atrial fibrillation that requires ventricular pacing or meets CRT in both men and women161–166. Estimates of European inhabitants with
criteria; atrioventricular nodal ablation or pharmacological rate con- HFrEF and LBBB167 qualifying for CRT and statistics of utilization of
trol will allow near complete ventricular pacing with CRT. Class IIa cardiac implantable electronic devices (CIED)168 suggest that up to
recommendations in the European guidelines137 include a QRS duration two-thirds of CRT-eligible patients are not receiving CRT166. The multi-
of 130–149 ms in sinus rhythm or ≥130 ms in atrial fibrillation with a national ESC CRT survey II noted that referral from non-implanting cen-
strategy in place to ensure biventricular pacing. tres accounted for only 25% of CRT referrals, suggesting that patients
Nature Reviews Cardiology
Review article
Table 2 | Clinical trials of implantable cardioverter–defibrillators in men and women with HF
Trial (year) Device Patient cohort Number of Mean Follow-up Primary Main results Interaction by sex or end
therapy patients age (months) end point point data
(% women) (years)
MUSTT EPS-guided LVEF ≤40%, CAD, 704 (10) 67 39 Cardiac EPS-guided therapy with ICD Primary end point in
(1999)117,124 antiarrhythmic NSVT and inducible arrest or reduced cardiac arrest or death comparator groups did not
therapy sustained VT at EPS death from from arrhythmia compared differ by sex; the interaction
(AAD or ICD arrhythmia with EPS-guided therapy between treatment and
if failed AAD) without defibrillator (HR 0.24, sex was not significant for
versus no 95% CI 0.13–0.45; P < 0.001) the secondary end point of
antiarrhythmic and compared with no all-cause death (P = 0.12)
therapy antiarrhythmic therapy (HR 0.27,
95% CI 0.15–0.47; P < 0.001)
EPS-guided therapy with
ICD reduced all-cause death
compared with EPS-guided
therapy without defibrillator
(HR 0.40, 95% CI 0.27–0.59;
P < 0.001) and compared with no
antiarrhythmic therapy (HR 0.45,
95% CI 0.32–0.63; P < 0.001)
MADIT II ICD or medical LVEF ≤30%, 1,232 (16) 64 20 All-cause Compared with medical No significant interaction by
(2002)118 therapy ischaemic death therapy, ICD reduced the sex for primary end point
cardiomyopathy, rate of the primary end point
previous MI (HR 0.69, 95% CI 0.51–0.93;
P = 0.016)
SCD-HeFT Placebo or LVEF ≤35%, 2,521 (23) 52 45.5 All-cause Compared with placebo, ICD P for interaction by sex for
(2005)121,125 amiodarone or ischaemic or death reduced the primary end point primary end point 0.54; ICD
ICD (on top of non-ischaemic (HR 0.77, 95% CI 0.62–0.96; versus placebo adjusted HR
conventional cardiomyopathy, P = 0.007) 0.71 (95% CI 0.57–0.88) in men
therapy) NYHA class II–III and 0.90 (95% CI 0.56–1.43)
in women; lower mortality in
women than in men; the
differences in mortality were
most accentuated in the
placebo group
DINAMIT ICD or medical LVEF ≤35%, recent 674 (24) 62 30 All-cause Similar rates of the primary end P for interaction by sex for
(2004)120 therapy MI (6–40 days), death point in the ICD and medical primary end point 0.82
heart rate ≥80 bpm, therapy groups (HR 1.08, 95%
SDNN ≤70 ms CI 0.76–1.55; P = 0.66)
IRIS ICD or medical LVEF ≤40%, recent 898 (23) 63 37 All-cause Similar rates of the primary end P for interaction by sex for
(2009)122 therapy MI (5–31 days), death point in the ICD and medical primary end point 0.85
heart rate ≥90 bpm, therapy groups (HR 1.04, 95%
with or without CI 0.81–1.35; P = 0.78)
Holter monitoring
with NSVT
≥150 bpm
DEFINITE ICD or medical LVEF ≤35%, 458 (29) 58 29 All-cause Similar rates of the primary end P for interaction by sex
(2004)119,126 therapy non-ischaemic death point in the ICD and medical (univariate) 0.11; primary
cardiomyopathy, therapy groups (HR 0.65, 95% end point HR 0.49 (95% CI
NYHA class I–III, CI 0.40–1.06; P = 0.08) 0.27–0.90; P = 0.018) in men
Holter monitoring and 1.14 (95% CI 0.50–2.64;
NSVT ≥120 bpm or P = 0.75) in women; sex
≥10 PVC/h was not an independent
predictor of primary end
point in multivariable
analysis adjusting for NYHA
class, LVEF, age and race
(P = 0.18)
DANISH ICD or no ICD LVEF ≤35%, 1,116 (27.5) 63 67.6 All-cause Similar rates of the primary P for interaction by sex 0.66;
(2016)123 non-ischaemic death end point in the ICD and primary end point HR 0.85
cardiomyopathy, non-ICD groups (HR 0.87, 95% (95% CI 0.64–1.12; P = 0.24)
NYHA class II–IV CI 0.68–1.22; P = 0.28); there in men and 1.03 (95% CI
was high background cardiac 0.57–1.87; P = 0.92) in women
resynchronization therapy (58%)
AAD, antiarrhythmic drug; CAD, coronary artery disease; EPS, electrophysiology studies; HF, heart failure; ICD, implantable cardioverter–defibrillator; LVEF, left ventricular ejection fraction;
MI, myocardial infarction; NSVT, non-sustained ventricular tachycardia; NYHA, New York Heart Association; PVC, premature ventricular complexes; SDNN, standard deviation of normal-to-
normal RR intervals (a measure of heart rate variability); VT, ventricular tachycardia.
Nature Reviews Cardiology
Review article
Table 3 | Clinical trials of cardiac resynchronization therapy in men and women with HF
Trial (year) Device Patient cohort Number Mean Follow- Primary end Main results Interaction by sex or
therapy of patients age up point end point data
(% women) (years)
MIRACLE CRT-P LVEF ≤35%, ischaemic 453 (32) 64 6 months 6MWD, QoL, Compared with no pacing, CRT Interaction with CRT
(2002)138 randomized or non-ischaemic NYHA class improved 6MWD (P = 0.005), by sex not reported in
to CRT cardiomyopathy, QoL (P = 0.001) and NYHA main manuscript
on or no NYHA class III–IV, class (P < 0.001) and reduced
pacing QRS ≥130 ms, LVEDD hospitalizations for worsening
≥55 mm, 6MWD HF (HR 0.5, 95% CI 0.28–0.88;
≤450 m P = 0.02)
COMPANION CRT-P, LVEF ≤35%, ischaemic 1,520 (33) 67 11.9–16.2 All-cause Reduced 12-month rate of the Interaction with CRT
(2004)139 CRT-D or or non-ischaemic months death or primary end point with CRT-P by sex not reported in
OMT cardiomyopathy, all-cause (HR 0.81, 95% CI 0.69–0.96; main manuscript
NYHA class III–IV, hospitalization P = 0.014) or CRT-D (HR 0.80,
QRS ≥120 ms, sinus 95% CI 0.68–0.95; P = 0.010)
rhythm, PR ≥150 ms compared with OMT
CARE-HF CRT-P or LVEF ≤35%, ischaemic 813 (27) 66 29 months All-cause CRT-P reduced the rate of the Primary end point HR
(2005)140 OMT or non-ischaemic death or primary end point compared 0.62 (95% CI 0.49–0.79)
cardiomyopathy, hospitalization with OMT (HR 0.63, 95% CI in men and 0.64 (95%
NYHA class III–IV; for cardio 0.51–0.77; P < 0.001) CI 0.42–0.07) in women
QRS ≥120 ms, LVEDDi vascular
≥30 mm causes
REVERSE CRT (± ICD) LVEF ≤40%, 610 (21) 63 12 months HF clinical CRT-on did not significantly Primary end point OR
(2008)143 randomized ischaemic or composite reduce the rate of the primary 0.69 (95% CI 0.43–1.11)
to CRT on non-ischaemic response end point compared with in men and 0.75 (95% CI
or off cardiomyopathy, CRT-off (OR 0.70, 95% CI 0.26–2.19) in women
NYHA class I–II, QRS 0.45–1.07; P = 0.10); CRT-on
≥120 ms, LVEDD reduced LVESVI (P < 0.0001) and
>55 mm time to first HF hospitalization
(HR 0.47; P = 0.03) compared
with CRT-off
MADIT-CRT CRT-D or LVEF ≤30%, ischaemic 1,820 (25) 65 2.4 years All-cause CRT-D reduced the rate of the P for interaction by
(2009)141 ICD cardiomyopathy death or primary end point compared sex 0.01; primary end
(NYHA class I–II) non-fatal with ICD-only (HR 0.66, 95% CI point HR 0.76 (95% CI
or non-ischaemic HF event 0.52–0.84; P = 0.001) 0.59–0.97) in men and
cardiomyopathy 0.37 (95% CI 0.22–0.61)
(NYHA class II), QRS in women
≥130 ms, sinus rhythm
RAFT CRT-D or LVEF ≤30%, ischaemic 1,798 (17) 66 40 months All-cause CRT-D reduced the rate of the P for interaction by sex
(2010)142 ICD or non-ischaemic death or HF primary end point compared 0.09
cardiomyopathy, hospitalization with ICD-only (HR 0.75, 95% CI
NYHA class II–III, 0.64–0.87; P < 0.001)
intrinsic QRS ≥120 ms
(or paced QRS
≥200 ms)
Pooled CRT-P or MIRACLE, MIRACLE 3,782 (22) 66 See All-cause Compared with no CRT (OMT, All-cause death HR 0.68
analysis CRT-D ICD, CARE-HF, individual death; ICD, back-up pacing), CRT (95% CI 0.57–0.80) in
(2013)246 versus OMT REVERSE, RAFT; trials all-cause (CRT-P or CRT-D) reduced men and 0.58 (95% CI
or ICD or see individual death or HF all-cause death (HR 0.66, 0.41–0.84) in women;
back-up trials; excluded hospitalization 95% CI 0.57–0.77) and the all-cause death or HF
pacing NYHA class I, atrial composite of all-cause death hospitalization HR 0.69
fibrillation, existing or HF hospitalization (HR 0.65, (95% CI 0.60–0.79) in
pacemaker 95% CI 0.58–0.74) men and 0.50 (95% CI
0.37–0.66) in women
Pooled CRT-D or REVERSE, MADIT-CRT, 4,076 (22) 65 See Death or HF; With LBBB and QRS ≥150 ms, CRT-D reduced clinical
analysis ICD RAFT individual death end points compared with ICD-alone in women (death
(2014)153 trials or HF, HR 0.33, 95% CI 0.21–0.52; death, HR 0.36,
95% CI 0.16–0.82) and men (death or HF, HR 0.47, 95% CI
0.37–0.59; death, HR 0.65, 95% CI 0.47–0.91)
With LBBB and QRS 130–149 ms, CRT-D reduced clinical
end points compared with ICD-alone in women (death
or HF, HR 0.24, 95% CI 0.11–0.53; death, HR 0.24, 95% CI
0.06–0.89), but not in men (death or HF, HR 0.85, 95% CI
0.60–1.21; death, HR 0.86, 95% CI 0.49–1.52)
6MWD, 6-min walking distance; CRT, cardiac resynchronization therapy; CRT-D, CRT plus defibrillator; CRT-P, CRT plus pacemaker; HF, heart failure; ICD, implantable cardioverter–defibrillator;
LBBB, left bundle branch block; LVEDD, left ventricular end-diastolic diameter; LVEDDi, LVEDD indexed for height; LVEF, left ventricular ejection fraction; LVESVI, left ventricular
end-systolic volume index; NYHA, New York Heart Association; QoL, quality of life; OMT, optimal medical therapy.
Nature Reviews Cardiology
Review article
outside university or teaching hospital settings have more limited Interventions for mitral valve regurgitation. Sex-related differences
access to CRT169. In an analysis of a HF registry from Sweden, female in outcomes exist after mitral valve intervention for mitral regurgita-
sex and advanced age were independent predictors of non-referral tion in patients with HF (Table 4). In a secondary analysis of sex-based
for CRT161. Strategies to improve implementation of CRT are needed, differences177 from the Cardiothoracic Surgical Trials Network SIMR
especially in eligible women in light of the evidence showing that they trial178,179, women had a smaller left ventricular volume and a smaller
derive greater benefit than men. Such strategies include overcoming mitral valve effective regurgitant orifice area (EROA) but proportionally
barriers in referral166,170, which includes increasing awareness of the larger EROA-to-left ventricular end-diastolic volume ratio than men177. At
indications and benefits of CRT among clinicians169, leveraging elec- 2 years after mitral valve surgery, although the degree of reverse left ven-
tronic health records for identification of eligible patients, and engag- tricular remodelling was similar in both sexes, women had higher rates
ing patients and support organizations to address misconceptions, of all-cause death and major adverse cardiovascular and cerebrovascular
promote information dissemination and increase therapeutic uptake166. events and worse QoL and functional status than men177.
Together with advances in pharmacological therapies for HF, A sex-specific analysis of the COAPT trial assessed the influence of sex
new approaches to pacing and resynchronization are also emerging. on the response to device therapy in patients with HF and severe secondary
In particular, conduction system pacing171–174 (targeting the His bun- mitral regurgitation. Although transcatheter mitral valve repair with the
dle or the left bundle branch area) as a form of cardiac physiological MitraClip resulted in improved clinical outcomes compared with GDMT
pacing175 is emerging as an alternative to conventional resynchroni- alone for both sexes, the relative reduction in HF hospitalizations was less
zation (with placement of a coronary sinus lead to pre-excite the left pronounced in women (HR 0.78, 95% CI 0.57–1.05) than in men (HR 0.43,
ventricle). The RCT funded by the Patient-Centered Outcomes Research 95% CI 0.34–0.54; P for interaction 0.002), especially beyond the first year
Insitute176 will evaluate the comparative effectiveness of His bundle of treatment. Women also derived less benefit from transcatheter mitral
or left bundle branch pacing in patients with a LVEF ≤50% and with valve repair than men with regard to QoL scores and 6MWD180.
either a wide QRS (≥130 ms), or with an anticipated pacing of >40% who
are already receiving current standard HF pharmacological therapy. Mechanical circulatory support. With respect to left ventricular
Sex-specific data in conduction system pacing will be needed to guide assist device (LVAD) therapy, female sex was independently associated
further consideration. with higher inpatient mortality after implantation in those implanted
Table 4 | Select clinical trials of mitral valve interventions and neuromodulation in men and women with HF
Trial (year) Device Patient cohort Number Mean Follow-up Primary end Main results Interaction by sex or end point data
therapy of patients age (months) point
(% women) (years)
Mitral valve interventions
COAPT TMVR LVEF 20–50%, 614 (36) 72 24 HF TMVR reduced the P for interaction by sex 0.05; primary
(2018)180,247 plus ischaemic or hospitalization primary end point of end point HR 0.44 (95% CI 0.32–0.61)
GDMT or non-ischaemic HF hospitalization in men and 0.77 (95% CI 0.49–1.21) in
GDMT cardiomyopathy, (HR 0.53, 95% CI women
alone moderate-to- 0.40–0.70; P < 0.001)
severe or severe as well as all-cause
secondary mitral death (HR 0.62, 95% CI
regurgitation, 0.46–0.82; P < 0.001)
NYHA class II–IV
Autonomic nervous system modulation
BeAT-HF BAT plus LVEF ≤35%, 264 (20) 62 6 6MWD, QoL, BAT improved No significant interaction by sex for
(2020)187,248 GDMT NYHA class II–III NT-proBNP 6MWD (P < 0.001), 6MWD, QoL and NYHA; BAT showed
or GDMT QoL (P < 0.001) and benefits in women and men; significant
alone NT-proBNP (P < 0.001) interaction by sex for NT-proBNP (P for
at 6 months of interaction 0.05), significant reduction
follow-up in plasma NT-proBNP levels with BAT in
women (P < 0.01) but less pronounced
and not significant in men (P = 0.08)
INOVATE-HF VNS plus LVEF ≤40%, NYHA 707 (21) 61 16 All-cause Similar rates of the P for interaction by sex 0.03; primary
(2016)188 GDMT or class III, mortality or HF primary end point in end point HR 0.99 (P = 0.93) in men
GDMT LVEDD 50–80 mm event the VNS and control and 2.43 (P = 0.02) in women; sex was
groups (HR 1.14, 95% no longer an independent predictor
CI 0.86–1.53; P = 0.37); of outcome (P = 0.17) in multivariate
compared with analysis incorporating sex-based
control, VNS improved differences (women were younger, with
6MWD (P < 0.01), QoL smaller left ventricular volume, shorter
(P < 0.01) and NYHA QRS duration and more likely to have
class (P < 0.01) non-ischaemic cardiomyopathy)
6MWD, 6-min walking distance; BAT, baroreflex activation therapy; GDMT, guideline-directed medical therapy; HF, heart failure; LVEDD, left ventricular end-diastolic diameter; LVEF, left
ventricular ejection fraction; NT-proBNP, amino‐terminal pro‐B‐type natriuretic peptide; NYHA, New York Heart Association; QoL, quality of life; TMVR, transcatheter mitral valve repair;
VNS, vagal nerve stimulation.
Nature Reviews Cardiology
Review article
during the pulsatile-flow LVAD era, but not in those implanted during new CIED in Australia and New Zealand reported more 90-day major
the continuous-flow LVAD era181. However, although the number of device-related complications in women than in men, and the difference
women undergoing LVAD implantation has increased, a utilization gap remained significant after adjusting for age, procedural acuity and
remains, with less utilization in women than in men182. Women have comorbidities (OR 1.10, 95% CI 1.04–1.16; P < 0.001)194. Multivariable
greater left ventricular reverse remodelling after implantation of LVAD analyses of the population-based Danish Pacemaker and ICD Register
than men183. A retrospective analysis of 355 patients who underwent similarly found that female sex was a predictor of increased risk of
LVAD implantation (167 with a HeartMate II and 188 a HeartMate VAD) complications after device implantation195. The postulated reasons
revealed that, compared with men, women had a greater reduction in for the higher implant-related complications observed in women with
left ventricular dimensions and a greater increase in LVEF in response transvenous CIEDs than in men include more difficult vascular access,
to unloading by the LVAD early after implantation and up to 5 years of thinner myocardial walls and smaller coronary sinus diameter196,197. In
follow-up, regardless of LVAD type183. contrast to this higher rate of implant-related complications associated
Extending the consideration of mechanical circulatory sup- with transvenous CIED systems192–194, an analysis of the IDE and EFFORT-
port to patients with cardiogenic shock in the setting of acute myo- LESS registries involving recipients of subcutaneous ICD systems found
cardial infarction, women derived greater benefit than men from no sex-related differences in 360-day complications with these devices,
early mechanical circulatory support (in this study, percutaneous which do not require vascular access for implantation198.
mechanical circulatory support before the percutaneous coronary
intervention)184. Adverse procedural events related to mitral valve procedures. In
patients with severe ischaemic mitral valve regurgitation undergoing
Neuromodulation in HF. Baroreflex activation therapy (BAT), via mitral valve surgery, the rate of 2-year major adverse cardiac and cer-
stimulation of the carotid baroreceptor by an implanted impulse gen- ebrovascular events (stroke, worsening HF, rehospitalization for HF and
erator, results in a centrally mediated decrease in sympathetic activity mitral valve reoperation) was higher in women than in men (49.0% ver-
and an increase in parasympathetic flow185,186. Sex-specific data from sus 38.1%; HR 1.58, 95% CI 1.06–2.37; P = 0.02)177. In patients with HF and
the randomized BeAT-HF study187, which compared BAT combined with severe secondary mitral regurgitation undergoing transcatheter mitral
GDMT versus GDMT alone, showed that women undergoing BAT had a valve repair, procedural success rates were high and device-related
significant improvement in 6MWD, QoL and NYHA functional class at complications were infrequent, irrespective of sex180,199,200.
6 months, similar to men, and that women had an additional benefit of
significant reduction in plasma amino‐terminal pro‐B‐type natriuretic Adverse procedural events related to mechanical circulatory sup-
peptide (NT-proBNP) levels (Table 4). port. An analysis of 966 LVAD recipients (815 men and 151 women,
The INOVATE-HF trial188, which is the largest trial on vagal nerve median follow-up 1.26 years) from the European EUROMACS registry
stimulation (VNS)188–191, compared high-amplitude, low-frequency (which includes a broad range of LVAD types) found that women expe-
VNS plus GDMT versus GDMT alone in patients with chronic, symp- rienced significantly more major bleeding events (P = 0.0012), arrhyth-
tomatic HFrEF. A significant treatment-by-subgroup interaction was mias (P = 0.022) and right ventricular failure with need for additional
seen for sex (HR 0.99 in men versus HR 2.43 in women for the primary right ventricular support (P < 0.001) than men201. Although the rates
efficacy end point of a composite of death from any cause or first event of pump thrombosis were not significantly different between men and
for worsening HF; P for interaction by sex 0.03). However, sex was no women, the occurrence of pump thrombosis was even more strongly
longer an independent predictor of the primary efficacy end point in a related to mortality in women than in men (HR 10.01 in women (95% CI
multivariate analysis incorporating sex-based differences (women were 4.44–22.55; P < 0.001) and HR 3.27 in men (95% CI 2.07–5.16; P < 0.001);
younger, more likely to have a non-ischaemic aetiology of HF and had a P for interaction for sex 0.028)201. An analysis of the US National Inpa-
smaller left ventricular volume and a shorter QRS duration than men), tient Sample including 3,511 patients with HF who received an LVAD
underscoring the importance of considering underlying sex-related between 2009 and 2014 found no sex-related differences in periproce-
differences in epidemiology, pathophysiology and electroanatomical dural complications182; however, the National Inpatient Sample dataset
remodelling. Further sex-specific analyses are needed to assess whether is primarily an administrative dataset that is not specifically developed
the optimal dose, intensity and duration of stimulation vary by sex. for HF (in contrast to the EUROMACS registry) and does not specifically
capture INTERMACS (Interagency Registry for mechanically assisted
Sex-related differences in adverse procedural events circulatory support) profiles or the need for right ventricular support.
Adverse procedural events related to CIEDs. Among US Medicare-
covered recipients of single-chamber or dual-chamber transvenous Adverse procedural events related to neuromodulation. In the
ICDs for primary prevention, women had more comorbidities, more BeAT-HF trial187, high rates of freedom from system-related and
advanced HF at the time of ICD implantation and higher odds of procedure-related major adverse neurological and cardiovascular
6-month procedural complications than men (OR 1.39, 95% CI 1.26–1.53; events were seen in the 125 patients (101 men and 24 women) who
P < 0.001), even after adjusting for differences in baseline characteris- underwent BAT with an implanted impulse generator, with no appar-
tics and device type192. Among recipients of a transvenous ICD device ent sex-specific differences (97% in men and 96% in women; P = 0.57).
(including for a primary or secondary prevention indication, and with With regard to VNS, the rate of freedom from procedure-related and
device systems ranging from single-chamber to dual-chamber, to system-related adverse events in the INOVATE-HF trial188 was 90.6%
CRT-D systems) from the Ontario ICD Database, women were more (95% CI 87.7–93.5%), without specification by sex.
likely than men to experience 45-day and 1-year implant-related com-
plications, after adjusting for baseline characteristics, comorbid con- Response to cardiac rehabilitation in HF
ditions and prevention indication, regardless of ICD type or implant HF guidelines strongly recommend non-pharmacological interven-
site193. Beyond recipients of ICDs, an analysis of adult recipients of a tions, including multidisciplinary team care, exercise training and
Nature Reviews Cardiology
Review article
associated with a non-significant overall reduction in the primary
Box 1 end point of all-cause mortality or hospitalizations (HR 0.93, 95% CI
0.84–1.02), with 64% of women and 68% of men experiencing the pri-
mary outcome (hazard ratios adjusted only for cause 0.83 (95% CI
Challenges and opportunities 0.68–1.00) in women and 0.97 (95% CI 0.87–1.09) in men; P for interac-
tion 0.17). A further analysis that adjusted for baseline covariates found
in sex-based considerations sex-related differences in outcomes, wherein women with LVEF ≤35%
for HF therapies in the exercise training group had a significant 26% reduction in the
primary composite outcome compared with no reduction in men with
LVEF ≤35% (adjusted HR 0.74 (95% CI 0.59–0.92) in women and 0.99
Challenges and opportunities exist when addressing sex-related (95% CI 0.86–1.13) in men; P for interaction 0.027)212,213. Although the
considerations in the design and conduct of clinical trials and the mechanisms behind this preferential benefit of exercise training in
implementation of heart failure therapies (see the table). Complex women are still unclear, these results are consistent with the findings
interactions of sex with other sociodemographic characteristics of other trials in patients with coronary conditions and patients with
pose additional challenges and opportunities for the optimization HF214,215. Among US Medicare beneficiaries who were hospitalized
of clinical trials and therapeutic adoption. for coronary conditions or cardiac revascularization procedures,
the reduction in 5-year mortality among cardiac rehabilitation users
Areas Challenges and Complex interaction (versus non-users) was greater in women than in men214. Moreover, in
opportunities between sex and
sociodemographic
the REHAB-HF trial215 in 349 older patients (52% women) hospitalized
characteristics with HF, an early, tailored and multidomain physical rehabilitation
programme clearly improved physical function among women, with
Clinical trial Study population, inclusion Gender
design and exclusion criteria an increase in the primary end point of Short Physical Performance
Race and ethnicity
Dose selection Battery score by a mean of 1.9 (95% CI 1.1–2.7) compared with 1.0 (95% CI
Urbanity versus rurality
Powered to detect 0.1–1.8) among men. A post hoc analysis of the REHAB-HF trial showed
Psychological factors
sex-specific effects that compared with patients with HFrEF, those with HFpEF were more
Social determinants of
At each stage of the therapy health often women (43% versus 61%) and had more frailty and depression and
development process, the worse baseline physical function and QoL216. The benefits of the multi-
influence of sex on the safety
domain physical rehabilitation intervention were numerically larger in
and efficacy of the treatment
should be assessed patients with HFpEF than in those with HFrEF, although the P values for
interaction for the 3-month outcomes were not significant216.
Conduct of Trial leadership
clinical trials Recruitment to ensure
representation of both sexes Challenges and opportunities
Participant engagement and Numerous opportunities exist to address sex-related differences in clin-
retainment during the study ical trials and therapeutic adoption, but they are not without challenges
Implementation Counselling and education (Box 1). In clinical trial design, sex-related considerations are relevant in
Shared decision-making the determination of inclusion and exclusion criteria, treatment dose
Adherence selection, protocol design, sample size calculation (ideally powered to
generate sex-specific data), and data and safety monitoring plan (cog-
nizant of potential sex-related differences in biological response and
adverse events)86. Women remain under-represented in clinical trials217.
cardiac rehabilitation18,202,203. Cardiac rehabilitation is safe, reduces Addressing this challenge calls for a multilevel approach, including
the rate of HF-related hospitalizations and improves functional capac- ensuring representation of women in clinical trial leadership218, educa-
ity, QoL and psychosocial wellbeing204,205. However, cardiac rehabili- tion of recruiting personnel on the importance of enrolling women and
tation is remarkably underutilized, particularly in women206,207. An of sharing their experience on enrolling women86, tailored recruitment
analysis of data from two meta-analyses showed that women were 36% (including outreach to community settings frequented by women and
less likely to enrol in cardiac rehabilitation programmes than men, and the involvement of family members and primary care providers)86
adherence was 3.6% lower among women than among men207,208. The and retention strategies that take into account logistical barriers to
reasons for these sex-related differences might be because women participation (such as offering flexible hours and at-home follow-up
with HF tend to be older, have more comorbidities and have lower and provision or reimbursement for concomitant childcare or family
levels of social support and functional capacity, and have greater care-giving responsibilities)86.
psychological burden than men with HF209. Up to 30% of patients Therapeutic adoption has been hindered by differential access
with HF have depression, and even more patients have depressive and counselling among women in particular. Approaches to improve
symptoms, particularly women with HFpEF210,211. Paradoxically, these the implementation of HF therapies will need to assess and address
challenges faced by women make it all the more necessary to encour- systemic and individual barriers to access as well as adherence to thera-
age participation and increase adherence to cardiac rehabilitation pies, and further consider differences in decision-making. Digital
among women with HF. health tools might have increasing roles in facilitating remote interac-
In the large HF-ACTION trial212, 2,331 outpatients (28% women) with tions between patients and clinicians, improving standardization of
HFrEF were randomly assigned to receive standard care or standard HF care, and promoting adherence to evidence-based guidelines219.
care with supervised aerobic exercise training. Exercise training was Electronic health record alerts can improve referral of ICD-eligible
Nature Reviews Cardiology
Review article
patients, thereby mitigating the observed sex-based gaps, with References
1. Lam, C. S. P. et al. Sex differences in heart failure. Eur. Heart J. 40, 3859–3868c (2019).
under-referral in women116. Decision support tools (such as with order
2. Vaduganathan, M. et al. Do women and men respond similarly to therapies in
sets and triggered alerts) serve as opportunities to increase adher- contemporary heart failure clinical trials? JACC Heart Fail. 7, 267–271 (2019).
ence to GDMT220–222. Increasing the readability and comprehensibility 3. Butler, J. et al. Systolic blood pressure and incident heart failure in the elderly. The
Cardiovascular Health Study and the Health, Ageing and Body Composition Study.
of patient-facing guideline materials has been helpful in promoting
Heart 97, 1304–1311 (2011).
patient partnership and empowering patients to make decisions 4. He, J. et al. Risk factors for congestive heart failure in US men and women: NHANES I
regarding their own therapies223. Given the known sex-related differ- epidemiologic follow-up study. Arch. Intern. Med. 161, 996–1002 (2001).
5. Magnussen, C. et al. Sex-specific epidemiology of heart failure risk and mortality in
ences in the decision-making processes (women might take longer to
Europe: results from the biomarCaRE consortium. JACC Heart Fail. 7, 204–213 (2019).
make decisions, require more sources of input and be more susceptible 6. Savji, N. et al. The association of obesity and cardiometabolic traits with incident HFpEF
to external influences than men)224, such patient-facing tools can be and HFrEF. JACC Heart Fail. 6, 701–709 (2018).
7. Uijl, A. et al. Risk factors for incident heart failure in age- and sex-specific strata: a
tailored for optimal sex-specific decision-making. Multi-stakeholder population-based cohort using linked electronic health records. Eur. J. Heart Fail. 21,
engagement (patients, care-givers, health-care practitioners, payers 1197–1206 (2019).
and public-health and policy makers, across multiple cultures)225 will 8. Lala, A. et al. Sex differences in heart failure. J. Card. Fail. 28, 477–498 (2022).
9. Ho, J. E. et al. Predicting heart failure with preserved and reduced ejection fraction: the
be important to promote implementation and sustainability among international collaboration on heart failure subtypes. Circ. Heart Fail. 9, e003116 (2016).
both women and men. 10. Paulus, W. J. & Tschope, C. A novel paradigm for heart failure with preserved ejection
Additionally, the exploration of how sex (biological domain), fraction: comorbidities drive myocardial dysfunction and remodeling through coronary
microvascular endothelial inflammation. J. Am. Coll. Cardiol. 62, 263–271 (2013).
gender (psychosocial domain) and sex hormones and exogenous 11. Sorimachi, H. et al. Pathophysiologic importance of visceral adipose tissue in women
hormones contribute to HF are needed in future research. Gender with heart failure and preserved ejection fraction. Eur. Heart J. 42, 1595–1605 (2021).
interacts with sex, and its properties are fluid and not binary terms226. 12. Stolfo, D. et al. Sex-based differences in heart failure across the ejection fraction
spectrum: phenotyping, and prognostic and therapeutic implications. JACC Heart Fail.
Traits of masculinity or femininity coexist and are expressed to vary- 7, 505–515 (2019).
ing degrees in the general population. Gender has been related to the 13. Templin, C. et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy.
development and progression of cardiovascular diseases227. Feminine N. Engl. J. Med. 373, 929–938 (2015).
14. Sliwa, K. et al. Clinical characteristics of patients from the worldwide registry on
gender, independent of sex, has been shown to be a strong predictor peripartum cardiomyopathy (PPCM): EURObservational Research Programme in
of recurrent acute coronary syndrome, and patients with feminine conjunction with the Heart Failure Association of the European Society of Cardiology
personality traits have poorer access to care than patients with mas- Study Group on PPCM. Eur. J. Heart Fail. 19, 1131–1141 (2017).
15. Denfeld, Q. E. et al. Characterizing sex differences in physical frailty phenotypes in heart
culine traits228,229. In a large cohort study, feminine characteristics were failure. Circ. Heart Fail. 14, e008076 (2021).
associated with an increased risk of cardiovascular diseases, especially 16. Dewan, P. et al. Differential impact of heart failure with reduced ejection fraction on men
in men230. However, much less is known about the association between and women. J. Am. Coll. Cardiol. 73, 29–40 (2019).
17. Ravera, A. et al. Quality of life in men and women with heart failure: association with
gender and HF. Notably, no gold standard exists for gender assessment. outcome, and comparison between the Kansas City Cardiomyopathy Questionnaire and
The measurement of gender in a reliable way (for example, current the EuroQol 5 dimensions questionnaire. Eur. J. Heart Fail. 23, 567–577 (2021).
18. McDonagh, T. A. et al. 2021 ESC guidelines for the diagnosis and treatment of acute and
theory-driven methods include the Bem Sex-Role Inventory and the
chronic heart failure. Eur. Heart J. 42, 3599–3726 (2021).
Masculine Gender Role Stress scale, and data-driven methods include 19. Kittleson, M. M. et al. 2023 ACC expert consensus decision pathway on management
the gender index) is the first challenging step for future research. of heart failure with preserved ejection fraction: a report of the American College of
Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 81, 1835–1878 (2023).
20. McDonagh, T. A. et al. 2023 Focused update of the 2021 ESC guidelines for the diagnosis
Conclusions and treatment of acute and chronic heart failure. Eur. Heart J. 44, 3627–3639 (2023).
Sex differences in anatomy, physiology, pharmacokinetics, pharma- 21. Soldin, O. P. & Mattison, D. R. Sex differences in pharmacokinetics and
pharmacodynamics. Clin. Pharmacokinet. 48, 143–157 (2009).
codynamics and psychosocial factors might influence the response to
22. Tamargo, J. et al. Gender differences in the effects of cardiovascular drugs. Eur. Heart
pharmacological agents, device therapy and cardiac rehabilitation in J. Cardiovasc. Pharmacother. 3, 163–182 (2017).
patients with HF (Fig. 1). The response to pharmacological therapies 23. Soldin, O. P., Chung, S. H. & Mattison, D. R. Sex differences in drug disposition. J. Biomed.
Biotechnol. 2011, 187103 (2011).
for HF in men and women are generally similar, except the response to
24. Anderson, G. D. Sex differences in drug metabolism: cytochrome P-450 and uridine
ARNI and spironolactone in those with higher LVEF (Fig. 3). Sex-related diphosphate glucuronosyltransferase. J. Gend. Specif. Med. 5, 25–33 (2002).
differences and similarities in clinical outcomes in response to device 25. Greenblatt, D. J. & von Moltke, L. L. Gender has a small but statistically significant effect
on clearance of CYP3A substrate drugs. J. Clin. Pharmacol. 48, 1350–1355 (2008).
therapies for HF have been reported. CRT is associated with a reduction 26. McDonough, A. A., Harris, A. N., Xiong, L. I. & Layton, A. T. Sex differences in renal
in mortality at a shorter QRS duration in women with LBBB than in men transporters: assessment and functional consequences. Nat. Rev. Nephrol. 20, 21–36
with LBBB. For the patient-oriented outcomes of QoL and functional (2023).
27. Bairey Merz, C. N. et al. Sex and the kidneys: current understanding and research
status, women derive similar benefits from BAT to men, but less benefit opportunities. Nat. Rev. Nephrol. 15, 776–783 (2019).
from mitral valve interventions. Women might also be more prone to 28. Vree, T. B. et al. Lack of male-female differences in disposition and esterase hydrolysis of
adverse effects of some HF medications (such as ACE inhibitors) and ramipril to ramiprilat in healthy volunteers after a single oral dose. ScientificWorldJournal
3, 1344–1358 (2003).
to procedural complications than men. Conversely, cardiac rehabilita- 29. Michel, M. C., Foster, C., Brunner, H. R. & Liu, L. A systematic comparison of the
tion might be particularly beneficial among women with HF. In general, properties of clinically used angiotensin II type 1 receptor antagonists. Pharmacol. Rev.
however, sex-specific evidence on therapeutic efficacy and safety in 65, 809–848 (2013).
30. Vachharajani, N. N., Shyu, W. C., Smith, R. A. & Greene, D. S. The effects of age and
patients with HF is still limited given the historical under-representation of gender on the pharmacokinetics of irbesartan. Br. J. Clin. Pharmacol. 46, 611–613 (1998).
women in clinical trials, as well as the lack of sex-specific evaluation 31. Miller, J. A. et al. Gender differences in the renal response to renin-angiotensin system
of therapeutic efficacy and safety in these trials. Such deficiencies also blockade. J. Am. Soc. Nephrol. 17, 2554–2560 (2006).
32. Luzier, A. B. et al. Gender-related effects on metoprolol pharmacokinetics and
represent opportunities to address sex-related disparities in HF and pharmacodynamics in healthy volunteers. Clin. Pharmacol. Ther. 66, 594–601 (1999).
develop tailored approaches to improve outcomes for both women 33. Thurmann, P. A. et al. Tolerability of β-blockers metabolized via cytochrome P450 2D6 is
and men with HF. sex-dependent. Clin. Pharmacol. Ther. 80, 551–553 (2006).
34. Labbe, L. et al. Effect of gender, sex hormones, time variables and physiological urinary
pH on apparent CYP2D6 activity as assessed by metabolic ratios of marker substrates.
Published online: xx xx xxxx Pharmacogenetics 10, 425–438 (2000).
Nature Reviews Cardiology
Review article
35. Eugene, A. R. Metoprolol dose equivalence in adult men and women based on gender 64. Benedict, C. R. et al. Comparative neurohormonal responses in patients with preserved
differences: pharmacokinetic modeling and simulations. Med. Sci. 4, 18 (2016). and impaired left ventricular ejection fraction: results of the Studies of Left Ventricular
36. McMurray, J. J. V. et al. Effects of sacubitril-valsartan versus valsartan in women Dysfunction (SOLVD) Registry. The SOLVD Investigators. J. Am. Coll. Cardiol. 22,
compared with men with heart failure and preserved ejection fraction: insights from 146A–153A (1993).
PARAGON-HF. Circulation 141, 338–351 (2020). 65. Gori, M. et al. Sex-specific cardiovascular structure and function in heart failure with
37. Berg, D. D. et al. Efficacy and safety of sacubitril/valsartan by dose level achieved in the preserved ejection fraction. Eur. J. Heart Fail. 16, 535–542 (2014).
PIONEER-HF Trial. JACC Heart Fail. 8, 834–843 (2020). 66. Rathore, S. S., Wang, Y. & Krumholz, H. M. Sex-based differences in the effect of digoxin
38. Wikstrand, J. et al. Dose of metoprolol CR/XL and clinical outcomes in patients with heart for the treatment of heart failure. N. Engl. J. Med. 347, 1403–1411 (2002).
failure: analysis of the experience in metoprolol CR/XL randomized intervention trial in 67. Adams, K. F. et al. Relationship of serum digoxin concentration to mortality and morbidity
chronic heart failure (MERIT-HF). J. Am. Coll. Cardiol. 40, 491–498 (2002). in women in the digitalis investigation group trial: a retrospective analysis. J. Am. Coll.
39. Lam, C. S. P. et al. Age, sex, and outcomes in heart failure with reduced EF: insights from Cardiol. 46, 497–504 (2005).
the VICTORIA trial. JACC Heart Fail. 11, 1246–1257 (2023). 68. Group, C. T. S. Effects of enalapril on mortality in severe congestive heart failure. Results
40. Granger, C. B. et al. Effects of candesartan in patients with chronic heart failure and of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N. Engl.
reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme J. Med. 316, 1429–1435 (1987).
inhibitors: the CHARM-Alternative trial. Lancet 362, 772–776 (2003). 69. Packer, M. et al. The effect of carvedilol on morbidity and mortality in patients with
41. McMurray, J. J. et al. Effects of candesartan in patients with chronic heart failure and chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N. Engl. J. Med. 334,
reduced left-ventricular systolic function taking angiotensin-converting-enzyme 1349–1355 (1996).
inhibitors: the CHARM-Added trial. Lancet 362, 767–771 (2003). 70. Pitt, B. et al. The effect of spironolactone on morbidity and mortality in patients with
42. McMurray, J. J. V. et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. severe heart failure. Randomized Aldactone Evaluation Study Investigators. N. Engl.
N. Engl. J. Med. 371, 993–1004 (2014). J. Med. 341, 709–717 (1999).
43. Rossello, X. et al. Sex differences in mineralocorticoid receptor antagonist trials: 71. Santema, B. T. et al. Identifying optimal doses of heart failure medications in men
a pooled analysis of three large clinical trials. Eur. J. Heart Fail. 22, 834–844 (2020). compared with women: a prospective, observational, cohort study. Lancet 394,
44. Butt, J. H. et al. Efficacy and safety of dapagliflozin in men and women with heart 1254–1263 (2019).
failure with reduced ejection fraction: a prespecified analysis of the dapagliflozin 72. Packer, M. et al. Comparative effects of low and high doses of the angiotensin-converting
and prevention of adverse outcomes in heart failure trial. JAMA Cardiol. 6, 678–689 enzyme inhibitor, lisinopril, on morbidity and mortality in chronic heart failure. ATLAS
(2021). Study Group. Circulation 100, 2312–2318 (1999).
45. Zannad, F. et al. SGLT2 inhibitors in patients with heart failure with reduced ejection 73. Ferreira, J. P. et al. Dosing of losartan in men versus women with heart failure with
fraction: a meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. Lancet 396, reduced ejection fraction: the HEAAL trial. Eur. J. Heart Fail. 23, 1477–1484 (2021).
819–829 (2020). 74. Rosano, G. M. C. et al. Gender differences in the effect of cardiovascular drugs: a position
46. Shekelle, P. G. et al. Efficacy of angiotensin-converting enzyme inhibitors and document of the Working Group on Pharmacology and Drug Therapy of the ESC.
beta-blockers in the management of left ventricular systolic dysfunction according to Eur. Heart J. 36, 2677–2680 (2015).
race, gender, and diabetic status: a meta-analysis of major clinical trials. J. Am. Coll. 75. Zopf, Y. et al. Women encounter ADRs more often than do men. Eur. J. Clin. Pharmacol.
Cardiol. 41, 1529–1538 (2003). 64, 999–1004 (2008).
47. Garg, R. & Yusuf, S. Overview of randomized trials of angiotensin-converting enzyme 76. Kando, J. C., Yonkers, K. A. & Cole, J. O. Gender as a risk factor for adverse events to
inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group medications. Drugs 50, 1–6 (1995).
on ACE Inhibitor Trials. JAMA 273, 1450–1456 (1995). 77. Rodenburg, E. M., Stricker, B. H. & Visser, L. E. Sex differences in cardiovascular
48. Young, J. B. et al. Mortality and morbidity reduction with candesartan in patients with drug-induced adverse reactions causing hospital admissions. Br. J. Clin. Pharmacol. 74,
chronic heart failure and left ventricular systolic dysfunction: results of the CHARM 1045–1052 (2012).
low-left ventricular ejection fraction trials. Circulation 110, 2618–2626 (2004). 78. Hreiche, R., Morissette, P. & Turgeon, J. Drug-induced long QT syndrome in women:
49. Ghali, J. K., Piña, I. L., Gottlieb, S. S., Deedwania, P. C. & Wikstrand, J. C. Metoprolol CR/XL review of current evidence and remaining gaps. Gend. Med. 5, 124–135 (2008).
in female patients with heart failure: analysis of the experience in Metoprolol Extended- 79. Tromp J, E. J. et al. Global variations according to sex in patients hospitalized for heart
Release Randomized Intervention Trial in Heart Failure (MERIT-HF). Circulation 105, failure in the REPORT-HF registry. JACC: Heart Fail. 11, 1262–1271 (2023).
1585–1591 (2002). 80. Rademaker, M. Do women have more adverse drug reactions? Am. J. Clin. Dermatol. 2,
50. Zannad, F. et al. Eplerenone in patients with systolic heart failure and mild symptoms. 349–351 (2001).
N. Engl. J. Med. 364, 11–21 (2011). 81. Bots, S. H. et al. Adverse drug reactions to guideline-recommended heart failure drugs in
51. Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. women: a systematic review of the literature. Jacc. Heart Fail. 7, 258–266 (2019).
N. Engl. J. Med. 383, 1413–1424 (2020). 82. Kostis, J. B. et al. Adverse effects of enalapril in the studies of left ventricular dysfunction
52. Swedberg, K. et al. Ivabradine and outcomes in chronic heart failure (SHIFT): (SOLVD). SOLVD investigators. Am. Heart J. 131, 350–355 (1996).
a randomised placebo-controlled study. Lancet 376, 875–885 (2010). 83. Do, T. P. et al. A database cohort study to assess the risk of angioedema among patients
53. O’Meara, E. et al. Sex differences in clinical characteristics and prognosis in a broad with heart failure initiating angiotensin-converting enzyme inhibitors in the USA.
spectrum of patients with heart failure: results of the Candesartan in Heart failure: Am. J. Cardiovasc. Drugs 18, 205–211 (2018).
Assessment of Reduction in Mortality and morbidity (CHARM) program. Circulation 115, 84. Lopes, R. J., Lourenço, A. P., Mascarenhas, J., Azevedo, A. & Bettencourt, P. Safety of
3111–3120 (2007). spironolactone use in ambulatory heart failure patients. Clin. Cardiol. 31, 509–513
54. Lam, C. S. P. et al. Sex differences in clinical characteristics and outcomes in elderly (2008).
patients with heart failure and preserved ejection fraction: the Irbesartan in Heart Failure 85. Wang, X. et al. Sex differences in characteristics, outcomes, and treatment response with
with Preserved Ejection Fraction (I-PRESERVE) trial. Circulation. Heart Fail. 5, 571–578 dapagliflozin across the range of ejection fraction in patients with heart failure: insights
(2012). from DAPA-HF and DELIVER. Circulation 147, 624–634 (2023).
55. Cleland, J. G. F. et al. The perindopril in elderly people with chronic heart failure 86. Lam, C. S. P. How to incorporate sex and gender into the design of cardiovascular clinical
(PEP-CHF) study. Eur. Heart J. 27, 2338–2345 (2006). trials. Circulation 145, 499–501 (2022).
56. Vaduganathan, M. et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive 87. Gaborit, N. et al. Gender-related differences in ion-channel and transporter subunit
meta-analysis of five randomised controlled trials. Lancet 400, 757–767 (2022). expression in non-diseased human hearts. J. Mol. Cell Cardiol. 49, 639–646 (2010).
57. Dewan, P. et al. Interactions between left ventricular ejection fraction, sex and effect 88. Odening, K. E. & Koren, G. How do sex hormones modify arrhythmogenesis in long QT
of neurohumoral modulators in heart failure. Eur. J. Heart Fail. 22, 898–901 (2020). syndrome? Sex hormone effects on arrhythmogenic substrate and triggered activity.
58. Pitt, B. et al. Spironolactone for heart failure with preserved ejection fraction. N. Engl. Heart Rhythm. 11, 2107–2115 (2014).
J. Med. 370, 1383–1392 (2014). 89. Liu, S., Yuan, S., Kongstad, O. & Olsson, S. B. Gender differences in the
59. Merrill, M., Sweitzer, N. K., Lindenfeld, J. & Kao, D. P. Sex differences in outcomes electrophysiological characteristics of atrioventricular conduction system and their
and responses to spironolactone in heart failure with preserved ejection fraction: clinical implications. Scand. Cardiovasc. J. 35, 313–317 (2001).
a secondary analysis of TOPCAT trial. Jacc. Heart Fail. 7, 228–238 (2019). 90. Macfarlane, P. W., McLaughlin, S. C., Devine, B. & Yang, T. F. Effects of age, sex, and race
60. Solomon, S. D. et al. Influence of ejection fraction on outcomes and efficacy of on ECG interval measurements. J. Electrocardiol. 27, 14–19 (1994).
spironolactone in patients with heart failure with preserved ejection fraction. Eur. Heart J. 91. Hnatkova, K., Smetana, P., Toman, O., Schmidt, G. & Malik, M. Sex and race differences
37, 455–462 (2016). in QRS duration. Europace 18, 1842–1849 (2016).
61. Chung, A. K. et al. Women have higher left ventricular ejection fractions than men 92. Rautaharju, P. M. et al. Sex differences in the evolution of the electrocardiographic QT
independent of differences in left ventricular volume: the Dallas Heart Study. Circulation interval with age. Can. J. Cardiol. 8, 690–695 (1992).
113, 1597–1604 (2006). 93. Rautaharju, P. M., Mason, J. W. & Akiyama, T. New age- and sex-specific criteria for QT
62. Poppe, K. K. et al. Ethnic-specific normative reference values for echocardiographic LA prolongation based on rate correction formulas that minimize bias at the upper normal
and LV size, LV mass, and systolic function: the EchoNoRMAL study. JACC: Cardiovasc. limits. Int. J. Cardiol. 174, 535–540 (2014).
Imaging 8, 656–665 (2015). 94. Kurokawa, J., Kodama, M., Clancy, C. E. & Furukawa, T. Sex hormonal regulation of
63. Dewan, P. et al. Sex-related differences in heart failure with preserved ejection fraction. cardiac ion channels in drug-induced QT syndromes. Pharmacol. Ther. 168, 23–28
Circulation. Heart Fail. 12, e006539 (2019). (2016).
Nature Reviews Cardiology
Review article
95. Okura, H. et al. Age- and gender-specific changes in the left ventricular relaxation: 123. Køber, L. et al. Defibrillator implantation in patients with nonischemic systolic heart
a Doppler echocardiographic study in healthy individuals. Circ. Cardiovasc. Imaging 2, failure. N. Engl. J. Med. 375, 1221–1230 (2016).
41–46 (2009). 124. Russo, A. M. et al. Influence of gender on arrhythmia characteristics and outcome in the
96. Krumholz, H. M., Larson, M. & Levy, D. Sex differences in cardiac adaptation to isolated Multicenter UnSustained Tachycardia Trial. J. Cardiovasc. Electrophysiol. 15, 993–998
systolic hypertension. Am. J. Cardiol. 72, 310–313 (1993). (2004).
97. Cheng, S. et al. Correlates of echocardiographic indices of cardiac remodeling over 125. Russo, A. M. et al. Primary prevention with defibrillator therapy in women: results from
the adult life course: longitudinal observations from the Framingham Heart Study. the Sudden Cardiac Death in Heart Failure Trial. J. Cardiovasc. Electrophysiol. 19, 720–724
Circulation 122, 570–578 (2010). (2008).
98. Umetani, K., Singer, D. H., McCraty, R. & Atkinson, M. Twenty-four hour time domain heart 126. Albert, C. M. et al. Sex differences in outcome after implantable cardioverter defibrillator
rate variability and heart rate: relations to age and gender over nine decades. J. Am. Coll. implantation in nonischemic cardiomyopathy. Am. Heart J. 156, 367–372 (2008).
Cardiol. 31, 593–601 (1998). 127. Ghanbari, H. et al. Effectiveness of implantable cardioverter-defibrillators for the
99. Ramaekers, D., Ector, H., Aubert, A. E., Rubens, A. & Van de Werf, F. Heart rate variability primary prevention of sudden cardiac death in women with advanced heart failure:
and heart rate in healthy volunteers. Is the female autonomic nervous system a meta-analysis of randomized controlled trials. Arch. Intern. Med. 169, 1500–1506
cardioprotective? Eur. Heart J. 19, 1334–1341 (1998). (2009).
100. Huikuri, H. V. et al. Sex-related differences in autonomic modulation of heart rate in 128. Santangeli, P. et al. Gender differences in clinical outcome and primary prevention
middle-aged subjects. Circulation 94, 122–125 (1996). defibrillator benefit in patients with severe left ventricular dysfunction: a systematic
101. Liao, D. et al. Age, race, and sex differences in autonomic cardiac function measured review and meta-analysis. Heart Rhythm. 7, 876–882 (2010).
by spectral analysis of heart rate variability – the ARIC study. Atherosclerosis risk in 129. Barra, S. et al. Do women benefit equally as men from the primary prevention
communities. Am. J. Cardiol. 76, 906–912 (1995). implantable cardioverter-defibrillator? Europace 20, 897–901 (2018).
102. Al-Khatib, S. M. et al. 2017 AHA/ACC/HRS guideline for management of patients with 130. Sticherling, C. et al. Sex differences in outcomes of primary prevention implantable
ventricular arrhythmias and the prevention of sudden cardiac death: a report of the cardioverter-defibrillator therapy: combined registry data from eleven European
American College of Cardiology/American Heart Association Task Force on Clinical countries. Europace 20, 963–970 (2018).
Practice Guidelines and the Heart Rhythm Society. Circulation 138, e272–e391 (2018). 131. Zeitler, E. P. et al. Primary prevention implantable cardioverter-defibrillators and survival
103. Zeppenfeld, K. et al. 2022 ESC guidelines for the management of patients with in older women. JACC Heart Fail. 3, 159–167 (2015).
ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 43, 132. Tompkins, C. M. et al. Sex differences in inappropriate ICD device therapies: MADIT-II and
3997–4126 (2022). MADIT-CRT. J. Cardiovasc. Electrophysiol. 28, 94–102 (2017).
104. Chia, Y. M. F. et al. Disparity between indications for and utilization of implantable 133. Knops, R. E. et al. Subcutaneous or transvenous defibrillator therapy. N. Engl. J. Med.
cardioverter defibrillators in Asian patients with heart failure. Circ. Cardiovasc. Qual. 383, 526–536 (2020).
Outcomes 10, e003651 (2017). 134. Gold, M. R. et al. Primary results from the understanding outcomes with the S-ICD in
105. Camm, A. J. & Nisam, S. European utilization of the implantable defibrillator: has 10 years primary prevention patients with low ejection fraction (UNTOUCHED) trial. Circulation
changed the ‘enigma’? Europace 12, 1063–1069 (2010). 143, 7–17 (2021).
106. Curtis, L. H. et al. Sex differences in the use of implantable cardioverter-defibrillators 135. Han, J. K. & Russo, A. M. Underrepresentation of women in implantable cardioverter
for primary and secondary prevention of sudden cardiac death. JAMA 298, 1517–1524 defibrillator trials. Am. Heart J. Plus 14, 100120 (2022).
(2007). 136. Epstein, A. E. et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/
107. Hernandez, A. F. et al. Sex and racial differences in the use of implantable AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities:
cardioverter-defibrillators among patients hospitalized with heart failure. JAMA 298, a report of the American College of Cardiology Foundation/American Heart Association
1525–1532 (2007). Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation 127,
108. MacFadden, D. R., Tu, J. V., Chong, A., Austin, P. C. & Lee, D. S. Evaluating sex e283–e352 (2013).
differences in population-based utilization of implantable cardioverter-defibrillators: 137. Glikson, M. et al. 2021 ESC guidelines on cardiac pacing and cardiac resynchronization
role of cardiac conditions and noncardiac comorbidities. Heart Rhythm. 6, 1289–1296 therapy. Eur. Heart J. 42, 3427–3520 (2021).
(2009). 138. Abraham, W. T. et al. Cardiac resynchronization in chronic heart failure. N. Engl. J. Med.
109. Mezu, U., Ch, I., Halder, I., London, B. & Saba, S. Women and minorities are less likely 346, 1845–1853 (2002).
to receive an implantable cardioverter defibrillator for primary prevention of sudden 139. Bristow, M. R. et al. Cardiac-resynchronization therapy with or without an implantable
cardiac death. Europace 14, 341–344 (2012). defibrillator in advanced chronic heart failure. N. Engl. J. Med. 350, 2140–2150 (2004).
110. Al-Khatib, S. M. et al. Trends in use of implantable cardioverter-defibrillator therapy 140. Cleland, J. G. et al. The effect of cardiac resynchronization on morbidity and mortality in
among patients hospitalized for heart failure: have the previously observed sex and racial heart failure. N. Engl. J. Med. 352, 1539–1549 (2005).
disparities changed over time? Circulation 125, 1094–1101 (2012). 141. Moss, A. J. et al. Cardiac-resynchronization therapy for the prevention of heart-failure
111. Patel, N. J. et al. Gender, racial, and health insurance differences in the trend of events. N. Engl. J. Med. 361, 1329–1338 (2009).
implantable cardioverter-defibrillator (ICD) utilization: a United States experience over 142. Tang, A. S. et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure.
the last decade. Clin. Cardiol. 39, 63–71 (2016). N. Engl. J. Med. 363, 2385–2395 (2010).
112. Bradfield, J., Warner, A. & Bersohn, M. M. Low referral rate for prophylactic implantation 143. Linde, C. et al. Randomized trial of cardiac resynchronization in mildly symptomatic
of cardioverter-defibrillators in a tertiary care medical center. Pacing Clin. Electrophysiol. heart failure patients and in asymptomatic patients with left ventricular dysfunction and
32, S194–S197 (2009). previous heart failure symptoms. J. Am. Coll. Cardiol. 52, 1834–1843 (2008).
113. Johnson, A. E., Bell, Y. K., Hamm, M. E., Saba, S. F. & Myaskovsky, L. A qualitative 144. Linde, C., Gold, M., Abraham, W. T. & Daubert, J. C. Baseline characteristics of patients
analysis of patient-related factors associated with implantable cardioverter defibrillator randomized in the resynchronization reverses remodeling in systolic left ventricular
acceptance. Cardiol. Ther. 9, 421–432 (2020). dysfunction (REVERSE) study. Congest. Heart Fail. 14, 66–74 (2008).
114. Hess, P. L. et al. Response by Hess et al. to letter regarding article, “Sex and race/ethnicity 145. Arshad, A. et al. Cardiac resynchronization therapy is more effective in women than in
differences in implantable cardioverter-defibrillator counseling and use among patients men: the MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial with Cardiac
hospitalized with heart failure: findings from the Get With The Guidelines-Heart Failure Resynchronization Therapy) trial. J. Am. Coll. Cardiol. 57, 813–820 (2011).
Program”. Circulation 135, e22–e23 (2017). 146. Zabarovskaja, S. et al. Women have better long-term prognosis than men after cardiac
115. Gravelin, L. M. et al. Use of a screening tool improves appropriate referral to an resynchronization therapy. Europace 14, 1148–1155 (2012).
electrophysiologist for implantable cardioverter-defibrillators for primary prevention of 147. Zusterzeel, R. et al. Sex-specific mortality risk by QRS morphology and duration in
sudden cardiac death. Circ. Cardiovasc. Qual. Outcomes 4, 152–156 (2011). patients receiving CRT: results from the NCDR. J. Am. Coll. Cardiol. 64, 887–894 (2014).
116. Thalappillil, A. et al. Impact of an automated best practice alert on sex and race 148. Hsu, J. C. et al. Predictors of super-response to cardiac resynchronization therapy and
disparities in implantable cardioverter-defibrillator therapy. J. Am. Heart Assoc. 11, associated improvement in clinical outcome: the MADIT-CRT (multicenter automatic
e023669 (2022). defibrillator implantation trial with cardiac resynchronization therapy) study. J. Am.
117. Buxton, A. E. et al. A randomized study of the prevention of sudden death in patients with Coll. Cardiol. 59, 2366–2373 (2012).
coronary artery disease. Multicenter Unsustained Tachycardia Trial investigators. N. Engl. 149. Linde, C. et al. The interaction of sex, height, and QRS duration on the effects of cardiac
J. Med. 341, 1882–1890 (1999). resynchronization therapy on morbidity and mortality: an individual-patient data
118. Moss, A. J. et al. Prophylactic implantation of a defibrillator in patients with myocardial meta-analysis. Eur. J. Heart Fail. 20, 780–791 (2018).
infarction and reduced ejection fraction. N. Engl. J. Med. 346, 877–883 (2002). 150. Ali, N. et al. Comparison of methods for delivering cardiac resynchronization therapy:
119. Kadish, A. et al. Prophylactic defibrillator implantation in patients with nonischemic an acute electrical and haemodynamic within-patient comparison of left bundle branch
dilated cardiomyopathy. N. Engl. J. Med. 350, 2151–2158 (2004). area, His bundle, and biventricular pacing. Europace 25, 1060–1067 (2023).
120. Hohnloser, S. H. et al. Prophylactic use of an implantable cardioverter-defibrillator after 151. Ezzeddine, F. M. et al. Outcomes of conduction system pacing for cardiac
acute myocardial infarction. N. Engl. J. Med. 351, 2481–2488 (2004). resynchronization therapy in patients with heart failure: a multicenter experience.
121. Bardy, G. H. et al. Amiodarone or an implantable cardioverter-defibrillator for congestive Heart Rhythm. 20, 863–871 (2023).
heart failure. N. Engl. J. Med. 352, 225–237 (2005). 152. Loring, Z. et al. Left bundle branch block predicts better survival in women than men
122. Steinbeck, G. et al. Defibrillator implantation early after myocardial infarction. N. Engl. receiving cardiac resynchronization therapy: long-term follow-up of ∼ 145,000 patients.
J. Med. 361, 1427–1436 (2009). JACC Heart Fail. 1, 237–244 (2013).
Nature Reviews Cardiology
Review article
153. Zusterzeel, R. et al. Cardiac resynchronization therapy in women: US Food and Drug 183. Kenigsberg, B. B. et al. Sex-associated differences in cardiac reverse remodeling in
Administration meta-analysis of patient-level data. JAMA Intern. Med. 174, 1340–1348 patients supported by contemporary left ventricular assist devices. J. Card. Fail. 26,
(2014). 494–504 (2020).
154. Woods, B. et al. Individual patient data network meta-analysis of mortality effects of 184. Joseph, S. M. et al. Women with cardiogenic shock derive greater benefit from early
implantable cardiac devices. Heart 101, 1800–1806 (2015). mechanical circulatory support: an update from the cVAD registry. J. Interv. Cardiol. 29,
155. Lee, N. S., Lin, F. & Birgersdotter-Green, U. Should women have different ECG criteria for 248–256 (2016).
CRT than men? J. Cardiol. 70, 1–6 (2017). 185. Abraham, W. T. et al. Baroreflex activation therapy for the treatment of heart failure with
156. Zusterzeel, R. et al. Toward sex-specific guidelines for cardiac resynchronization therapy? a reduced ejection fraction. JACC Heart Fail. 3, 487–496 (2015).
J. Cardiovasc. Transl. Res. 9, 12–22 (2016). 186. Georgakopoulos, D., Little, W. C., Abraham, W. T., Weaver, F. A. & Zile, M. R. Chronic
157. Wilkoff, B. L. et al. Adaptive versus conventional cardiac resynchronisation therapy baroreflex activation: a potential therapeutic approach to heart failure with preserved
in patients with heart failure (AdaptResponse): a global, prospective, randomised ejection fraction. J. Card. Fail. 17, 167–178 (2011).
controlled trial. Lancet 402, 1147–1157 (2023). 187. Lindenfeld, J. et al. Response by sex in patient-centered outcomes with baroreflex
158. Linde, C. Will the results from the AdaptResponse trial boost CRT use? Lancet 402, activation therapy in systolic heart failure. JACC Heart Fail. 9, 430–438 (2021).
1110–1112 (2023). 188. Gold, M. R. et al. Vagus nerve stimulation for the treatment of heart failure: the
159. Varma, N. et al. Sex-specific response to cardiac resynchronization therapy: effect of left INOVATE-HF trial. J. Am. Coll. Cardiol. 68, 149–158 (2016).
ventricular size and QRS duration in left bundle branch block. JACC Clin. Electrophysiol. 189. Premchand, R. K. et al. Autonomic regulation therapy via left or right cervical vagus
3, 844–853 (2017). nerve stimulation in patients with chronic heart failure: results of the ANTHEM-HF trial.
160. Zweerink, A. et al. Size matters: normalization of QRS duration to left ventricular J. Card. Fail. 20, 808–816 (2014).
dimension improves prediction of long-term cardiac resynchronization therapy 190. Zannad, F. et al. Chronic vagal stimulation for the treatment of low ejection fraction heart
outcome. Circ. Arrhythm. Electrophysiol. 11, e006767 (2018). failure: results of the NEural Cardiac TherApy foR Heart Failure (NECTAR-HF) randomized
161. Lund, L. H. et al. Association between demographic, organizational, clinical, and controlled trial. Eur. Heart J. 36, 425–433 (2015).
socio-economic characteristics and underutilization of cardiac resynchronization 191. Anand, I. S. et al. Comparison of symptomatic and functional responses to vagus nerve
therapy: results from the Swedish Heart Failure Registry. Eur. J. Heart Fail. 19, 1270–1279 stimulation in ANTHEM-HF, INOVATE-HF, and NECTAR-HF. Esc. Heart Fail. 7, 75–83 (2020).
(2017). 192. Russo, A. M. et al. Gender and outcomes after primary prevention implantable
162. Chatterjee, N. A. et al. Increasing sex differences in the use of cardiac resynchronization cardioverter-defibrillator implantation: findings from the National Cardiovascular Data
therapy with or without implantable cardioverter-defibrillator. Eur. Heart J. 38, 1485–1494 Registry (NCDR). Am. Heart J. 170, 330–338 (2015).
(2017). 193. MacFadden, D. R. et al. Sex differences in implantable cardioverter-defibrillator
163. Gadler, F., Valzania, C. & Linde, C. Current use of implantable electrical devices in outcomes: findings from a prospective defibrillator database. Ann. Intern. Med. 156,
Sweden: data from the Swedish pacemaker and implantable cardioverter-defibrillator 195–203 (2012).
registry. Europace 17, 69–77 (2015). 194. Moore, K. et al. Sex differences in acute complications of cardiac implantable electronic
164. Linde, C. et al. Gender, underutilization of cardiac resynchronization therapy, and devices: implications for patient safety. J. Am. Heart Assoc. 8, e010869 (2019).
prognostic impact of QRS prolongation and left bundle branch block in heart failure. 195. Kirkfeldt, R. E., Johansen, J. B., Nohr, E. A., Jørgensen, O. D. & Nielsen, J. C. Complications
Europace 17, 424–431 (2015). after cardiac implantable electronic device implantations: an analysis of a complete,
165. Dickstein, K. et al. The European cardiac resynchronization therapy survey. Eur. Heart J. nationwide cohort in Denmark. Eur. Heart J. 35, 1186–1194 (2014).
30, 2450–2460 (2009). 196. Amuthan, R. & Curtis, A. B. Sex-specific considerations in drug and device therapy
166. Mullens, W. et al. Optimized implementation of cardiac resynchronization therapy: a call of cardiac arrhythmias: JACC focus seminar 6/7. J. Am. Coll. Cardiol. 79, 1519–1529
for action for referral and optimization of care: a joint position statement from the Heart (2022).
Failure Association (HFA), European Heart Rhythm Association (EHRA), and European 197. Blendea, D. et al. Variability of coronary venous anatomy in patients undergoing cardiac
Association of Cardiovascular Imaging (EACVI) of the European Society of Cardiology. resynchronization therapy: a high-speed rotational venography study. Heart Rhythm. 4,
Eur. J. Heart Fail. 22, 2349–2369 (2020). 1155–1162 (2007).
167. Baldasseroni, S. et al. Left bundle-branch block is associated with increased 1-year 198. Russo, A. M. et al. Impact of gender on clinical outcomes associated with subcutaneous
sudden and total mortality rate in 5517 outpatients with congestive heart failure: a report implantable cardioverter defibrillators [abstract]. Circulation 134, A19607 (2016).
from the Italian network on congestive heart failure. Am. Heart J. 143, 398–405 (2002). 199. Werner, N. et al. Gender-related differences in patients undergoing transcatheter mitral
168. Raatikainen, M. J. et al. Statistics on the use of cardiac electronic devices and valve interventions in clinical practice: 1-year results from the German TRAMI registry.
electrophysiological procedures in the European Society of Cardiology countries: 2014 Catheter. Cardiovasc. Interv. 95, 819–829 (2020).
report from the European Heart Rhythm Association. Europace 17, i1–i75 (2015). 200. Estévez-Loureiro, R. et al. Effect of gender on results of percutaneous edge-to-edge
169. Dickstein, K. et al. CRT Survey II: a European Society of Cardiology survey of cardiac mitral valve repair with MitraClip system. Am. J. Cardiol. 116, 275–279 (2015).
resynchronisation therapy in 11 088 patients – who is doing what to whom and how? 201. Magnussen, C. et al. Gender differences and outcomes in left ventricular assist device
Eur. J. Heart Fail. 20, 1039–1051 (2018). support: the European Registry for Patients with Mechanical Circulatory Support.
170. Thorvaldsen, T. & Lund, L. H. Focusing on referral rather than selection for advanced J. Heart Lung Transpl. 37, 61–70 (2018).
heart failure therapies. Card. Fail. Rev. 5, 24–26 (2019). 202. Bozkurt, B. et al. Cardiac rehabilitation for patients with heart failure: JACC expert panel.
171. Salden, F. et al. Short-term hemodynamic and electrophysiological effects of cardiac J. Am. Coll. Cardiol. 77, 1454–1469 (2021).
resynchronization by left ventricular septal pacing. J. Am. Coll. Cardiol. 75, 347–359 203. Heidenreich, P. A. et al. 2022 AHA/ACC/HFSA guideline for the management of heart
(2020). failure: a report of the American College of Cardiology/American Heart Association Joint
172. Liang, Y. et al. Left bundle branch pacing versus biventricular pacing for acute cardiac Committee on Clinical Practice Guidelines. Circulation 145, e895–e1032 (2022).
resynchronization in patients with heart failure. Circ. Arrhythm. Electrophysiol. 15, 204. Alter, D. A., Oh, P. I. & Chong, A. Relationship between cardiac rehabilitation and
e011181 (2022). survival after acute cardiac hospitalization within a universal health care system.
173. Arnold, A. D. et al. His resynchronization versus biventricular pacing in patients with Eur. J. Cardiovasc. Prev. Rehabil. 16, 102–113 (2009).
heart failure and left bundle branch block. J. Am. Coll. Cardiol. 72, 3112–3122 (2018). 205. Anderson, L. et al. Exercise-based cardiac rehabilitation for coronary heart disease:
174. Diaz, J. C. et al. Left bundle branch area pacing versus biventricular pacing as initial Cochrane systematic review and meta-analysis. J. Am. Coll. Cardiol. 67, 1–12 (2016).
strategy for cardiac resynchronization. JACC Clin. Electrophysiol. 9, 1568–1581 (2023). 206. Colella, T. J. et al. Sex bias in referral of women to outpatient cardiac rehabilitation?
175. Chung, M. K. et al. 2023 HRS/APHRS/LAHRS guideline on cardiac physiologic pacing for A meta-analysis. Eur. J. Prev. Cardiol. 22, 423–441 (2015).
the avoidance and mitigation of heart failure. Heart Rhythm. 20, e17–e91 (2023). 207. Oosenbrug, E. et al. Sex differences in cardiac rehabilitation adherence: a meta-analysis.
176. US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/ Can. J. Cardiol. 32, 1316–1324 (2016).
NCT05650658 (2023). 208. Samayoa, L. et al. Sex differences in cardiac rehabilitation enrollment: a meta-analysis.
177. Giustino, G. et al. Sex-based differences in outcomes after mitral valve surgery for severe Can. J. Cardiol. 30, 793–800 (2014).
ischemic mitral regurgitation: from the cardiothoracic surgical trials network. JACC Heart 209. Khadanga, S., Savage, P. D., Gaalema, D. E. & Ades, P. A. Predictors of cardiac
Fail. 7, 481–490 (2019). rehabilitation participation: opportunities to increase enrollment. J. Cardiopulm. Rehabil.
178. Acker, M. A. et al. Mitral-valve repair versus replacement for severe ischemic mitral Prev. 41, 322–327 (2021).
regurgitation. N. Engl. J. Med. 370, 23–32 (2014). 210. Sbolli, M., Fiuzat, M., Cani, D. & O’Connor, C. M. Depression and heart failure: the lonely
179. Goldstein, D. et al. Two-year outcomes of surgical treatment of severe ischemic mitral comorbidity. Eur. J. Heart Fail. 22, 2007–2017 (2020).
regurgitation. N. Engl. J. Med. 374, 344–353 (2016). 211. Hsich, E. M. et al. Sex differences in in-hospital mortality in acute decompensated heart
180. Kosmidou, I. et al. Sex-specific outcomes of transcatheter mitral-valve repair and failure with reduced and preserved ejection fraction. Am. Heart J. 163, 430–437.e3
medical therapy for mitral regurgitation in heart failure. JACC Heart Fail. 9, 674–683 (2012).
(2021). 212. O’Connor, C. M. et al. Efficacy and safety of exercise training in patients with chronic
181. Joshi, A. A. et al. Sex-based differences in left ventricular assist device utilization: insights heart failure: HF-ACTION randomized controlled trial. JAMA 301, 1439–1450 (2009).
from the nationwide inpatient sample 2004 to 2016. Circ. Heart Fail. 12, e006082 (2019). 213. Pina, I. L. et al. Effects of exercise training on outcomes in women with heart failure:
182. Ahmed, A. et al. Gender differences in outcomes after implantation of left ventricular analysis of HF-ACTION (Heart Failure–A Controlled Trial Investigating Outcomes of
assist devices. Ann. Thorac. Surg. 109, 780–786 (2020). Exercise TraiNing) by sex. JACC Heart Fail. 2, 180–186 (2014).
Nature Reviews Cardiology
Review article
214. Suaya, J. A., Stason, W. B., Ades, P. A., Normand, S. L. & Shepard, D. S. Cardiac 240. McMurray, J. J. V. et al. Dapagliflozin in patients with heart failure and reduced ejection
rehabilitation and survival in older coronary patients. J. Am. Coll. Cardiol. 54, 25–33 fraction. N. Engl. J. Med. 381, 1995–2008 (2019).
(2009). 241. Butler, J. et al. Effects of empagliflozin in women and men with heart failure and
215. Kitzman, D. W. et al. Physical rehabilitation for older patients hospitalized for heart failure. preserved ejection fraction. Circulation 146, 1046–1055 (2022).
N. Engl. J. Med. 385, 203–216 (2021). 242. Solomon, S. D. et al. Dapagliflozin in heart failure with mildly reduced or preserved
216. Mentz, R. J. et al. Rehabilitation intervention in older patients with acute heart failure with ejection fraction. N. Engl. J. Med. 387, 1089–1098 (2022).
preserved versus reduced ejection fraction. JACC Heart Fail. 9, 747–757 (2021). 243. Jhund, P. S. et al. Dapagliflozin across the range of ejection fraction in patients with heart
217. Jin, X. et al. Women’s participation in cardiovascular clinical trials from 2010 to 2017. failure: a patient-level, pooled meta-analysis of DAPA-HF and DELIVER. Nat. Med. 28,
Circulation 141, 540–548 (2020). 1956–1964 (2022).
218. Van Spall, H. G. C. et al. Ending gender inequality in cardiovascular clinical trial 244. Digitalis Investigation Group The effect of digoxin on mortality and morbidity in patients
leadership: JACC review topic of the week. J. Am. Coll. Cardiol. 77, 2960–2972 (2021). with heart failure. N. Engl. J. Med. 336, 525–533 (1997).
219. Kao, D. P., Trinkley, K. E. & Lin, C. T. Heart failure management innovation enabled by 245. Deswal, A. & Bozkurt, B. Comparison of morbidity in women versus men with heart failure
electronic health records. JACC Heart Fail. 8, 223–233 (2020). and preserved ejection fraction. Am. J. Cardiol. 97, 1228–1231 (2006).
220. Riggio, J. M. et al. Effectiveness of a clinical-decision-support system in improving 246. Cleland, J. G. et al. An individual patient meta-analysis of five randomized trials assessing
compliance with cardiac-care quality measures and supporting resident training. the effects of cardiac resynchronization therapy on morbidity and mortality in patients
Acad. Med. 84, 1719–1726 (2009). with symptomatic heart failure. Eur. Heart J. 34, 3547–3556 (2013).
221. Ballard, D. J. et al. Impact of a standardized heart failure order set on mortality, 247. Stone, G. W. et al. Transcatheter mitral-valve repair in patients with heart failure. N. Engl.
readmission, and quality and costs of care. Int. J. Qual. Health Care 22, 437–444 (2010). J. Med. 379, 2307–2318 (2018).
222. Krive, J., Shoolin, J. S. & Zink, S. D. Effectiveness of evidence-based congestive heart 248. Zile, M. R. et al. Baroreflex activation therapy in patients with heart failure with reduced
failure (CHF) CPOE order sets measured by health outcomes. AMIA Annu. Symp. Proc. ejection fraction. J. Am. Coll. Cardiol. 76, 1–13 (2020).
2014, 815–824 (2014).
223. Stromberg, A. The crucial role of patient education in heart failure. Eur. J. Heart Fail. 7, Author contributions
363–369 (2005). The authors contributed substantially to all aspects of the article.
224. Lobato, L. et al. Impact of gender on the decision to participate in a clinical trial:
a cross-sectional study. BMC Public. Health 14, 1156 (2014). Competing interests
225. Concannon, T. W. et al. A systematic review of stakeholder engagement in comparative J.B. has received consultancy and/or research fees from Abbott, American Regent, Amgen,
effectiveness and patient-centered outcomes research. J. Gen. Intern. Med. 29, Applied Therapeutics, AskBio, Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Boston
1692–1701 (2014). Scientific, Bristol Myers Squibb, Cardiac Dimension, Cardiocell, Cardior, CSL Behring, CVRx,
226. Shannon, G. et al. Gender equality in science, medicine, and global health: where are we Cytokinetics, Daxor, Edwards, Element Science, Faraday, Foundry, G3P, Innolife, Impulse
at and why does it matter? Lancet 393, 560–569 (2019). Dynamics, Imbria, Inventiva, Ionis, Lexicon, Eli Lilly, LivaNova, Janssen, Medtronics, Merck,
227. van Diemen, J. et al. The importance of achieving sex- and gender-based equity in Occlutech, Owkin, Novartis, Novo Nordisk, Pharmacosmos, Pharmain, Pfizer, Prolaio,
clinical trials: a call to action. Eur. Heart J. 42, 2990–2994 (2021). Regeneron, Renibus, Roche Diagnostics, Salamandra, Sanofi, SC Pharma, Secretome,
228. Pelletier, R. et al. Sex-related differences in access to care among patients with Sequana, SQ Innovation, Tenex, Tricog, Ultromics, Vifor, and Zoll. A.A.V. has received
premature acute coronary syndrome. CMAJ 186, 497–504 (2014). consultancy and/or research fees from Anacardio, AstraZeneca, Bayer, Bristol Myers Squibb,
229. Pelletier, R. et al. Sex versus gender-related characteristics: which predicts outcome Boehringer Ingelheim, Cytokinetics, Corteria, Eli Lilly, Moderna, Novartis, Novo Nordisk,
after acute coronary syndrome in the young? J. Am. Coll. Cardiol. 67, 127–135 (2016). Pfizer and Roche Diagnostics. C.S.P.L. is supported by a Clinician Scientist Award from the
230. Ballering, A. V., Bonvanie, I. J., Olde Hartman, T. C., Monden, R. & Rosmalen, J. G. M. National Medical Research Council of Singapore; has received research support from Novo
Gender and sex independently associate with common somatic symptoms and lifetime Nordisk and Roche Diagnostics; has served as consultant or on the Advisory Board/Steering
prevalence of chronic disease. Soc. Sci. Med. 253, 112968 (2020). Committee/Executive Committee for Alleviant Medical, Allysta Pharma, Amgen, AnaCardio
231. Ghali, J. K. Sex-related differences in heart failure and beta-blockers. Heart Fail. Rev. 9, AB, Applied Therapeutics, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific,
149–159 (2004). Bristol Myers Squibb, CardioRenal, Cytokinetics, Darma Inc., EchoNous Inc, Eli Lilly, Impulse
232. SOLVD Investigators Effect of enalapril on survival in patients with reduced left Dynamics, Intellia Therapeutics, Ionis Pharmaceutical, Janssen Research & Development
ventricular ejection fractions and congestive heart failure. N. Engl. J. Med. 325, 293–302 LLC, Medscape/WebMD Global LLC, Merck, Novartis, Novo Nordisk, Prosciento, Quidel
(1991). Corporation, Radcliffe Group, Recardio, ReCor Medical, Roche Diagnostics, Sanofi, Siemens
233. Wenger, N. K., Speroff, L. & Packard, B. Cardiovascular health and disease in women. Healthcare Diagnostics and Us2.ai; and serves as co-founder and non-executive director of
N. Engl. J. Med. 329, 247–256 (1993). Us2.ai. J.Y.C. has received consultancy fees from Medtronic. H.Q. has no competing interests.
234. Majahalme, S. K. et al. Comparison of treatment benefit and outcome in women versus
men with chronic heart failure (from the Valsartan Heart Failure Trial). Am. J. Cardiol. 95, Additional information
529–532 (2005). Peer review information Nature Reviews Cardiology thanks Harriette Van Spall, Theresa
235. Massie, B. M. et al. Irbesartan in patients with heart failure and preserved ejection McDonagh, and the other, anonymous, reviewer(s) for their contribution to the peer review
fraction. N. Engl. J. Med. 359, 2456–2467 (2008). of this work.
236. Solomon, S. D. et al. Sacubitril/valsartan across the spectrum of ejection fraction in heart
failure. Circulation 141, 352–361 (2020). Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in
237. Simon, T., Mary-Krause, M., Funck-Brentano, C. & Jaillon, P. Sex differences in the published maps and institutional affiliations.
prognosis of congestive heart failure: results from the Cardiac Insufficiency Bisoprolol
Study (CIBIS II). Circulation 103, 375–380 (2001). Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this
238. MERIT-HF Study Group Effect of metoprolol CR/XL in chronic heart failure: Metoprolol article under a publishing agreement with the author(s) or other rightsholder(s); author
CR/XL Randomised Intervention Trial-in Congestive Heart Failure (MERIT-HF). Lancet self-archiving of the accepted manuscript version of this article is solely governed by the
353, 2001–2007 (1999). terms of such publishing agreement and applicable law.
239. Packer, M. et al. Effect of carvedilol on survival in severe chronic heart failure. N. Engl.
J. Med. 344, 1651–1658 (2001). © Springer Nature Limited 2024
Nature Reviews Cardiology
You might also like
- Boylan - The Spiritual Life of The PriestDocument63 pagesBoylan - The Spiritual Life of The Priestpablotrollano100% (1)
- Module 2 1 Math 10 Graphs of Polynomial Functions FinalDocument29 pagesModule 2 1 Math 10 Graphs of Polynomial Functions FinalJacob Sanchez100% (1)
- Update On Psychotropic Medication Use in Renal DiseaseDocument15 pagesUpdate On Psychotropic Medication Use in Renal DiseaseMartinaNo ratings yet
- 2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in CarDocument16 pages2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in CarAngie OvandoNo ratings yet
- Chapter 69Document8 pagesChapter 69ingbarragan87No ratings yet
- Importance of Pharmacogenomics in The Personalized MedicineDocument6 pagesImportance of Pharmacogenomics in The Personalized MedicineJames AustinNo ratings yet
- Adv Pharmacology - AnswerDocument7 pagesAdv Pharmacology - AnswerMEHATHI SUBASHNo ratings yet
- Patel 2017Document11 pagesPatel 2017Imanuel CristiantoNo ratings yet
- 2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in Ca1Document17 pages2021 Sexual Activity After Myocardial Revascularizat 2021 Current Problems in Ca1Angie OvandoNo ratings yet
- Pharmacogenetics of Cardiovascular Drug TherapyDocument11 pagesPharmacogenetics of Cardiovascular Drug Therapybalaji5563No ratings yet
- Adrs For WomenDocument9 pagesAdrs For WomenFajar PutraNo ratings yet
- Gender Differences in Disease Manifestation and PresentationDocument5 pagesGender Differences in Disease Manifestation and PresentationGustavo Anzola100% (1)
- Cubała W. (ZOLPIDEM) 0Document2 pagesCubała W. (ZOLPIDEM) 0Antonio SanchezNo ratings yet
- Combination Medical Therapy For Lower Urinary Tract Symptoms and Benign Prostatic HyperplasiaDocument9 pagesCombination Medical Therapy For Lower Urinary Tract Symptoms and Benign Prostatic HyperplasiaganangahimsaNo ratings yet
- Erectile Dysfunction and HypertensionDocument8 pagesErectile Dysfunction and HypertensionILham SyahNo ratings yet
- 2017 - Behavioral Emergencies - Geriatric Psychiatric PatientDocument14 pages2017 - Behavioral Emergencies - Geriatric Psychiatric PatientAna María Arenas DávilaNo ratings yet
- Prescribing Pattern of Antihypertensive Drugs in A Tertiary Care Hospital in Jammu-A Descriptive StudyDocument4 pagesPrescribing Pattern of Antihypertensive Drugs in A Tertiary Care Hospital in Jammu-A Descriptive StudyMahantesh NyayakarNo ratings yet
- Key Points To RememberDocument37 pagesKey Points To RememberheikalNo ratings yet
- AJGP 0102 2023 Focus Chung Male Sexual Dysfunction WEBDocument5 pagesAJGP 0102 2023 Focus Chung Male Sexual Dysfunction WEBrisang akrima fikriNo ratings yet
- Pharmacotherapy For Cardiovascular Disorders EditedDocument5 pagesPharmacotherapy For Cardiovascular Disorders Editedhutwriters2No ratings yet
- Piis2050052117300744 PDFDocument15 pagesPiis2050052117300744 PDFRichu UhcirNo ratings yet
- Diet and Men 'S Sexual Health: Rates of Male Sexual DysfunctionsDocument15 pagesDiet and Men 'S Sexual Health: Rates of Male Sexual DysfunctionsHoa VânNo ratings yet
- Heart Failure With Preserved Ejection Fraction - JAMA (2023)Document12 pagesHeart Failure With Preserved Ejection Fraction - JAMA (2023)cheve glzNo ratings yet
- Redfield Margaret M Heart Failure With PreservedDocument12 pagesRedfield Margaret M Heart Failure With PreservedNathan Kulkys MarquesNo ratings yet
- Solomon 2006Document5 pagesSolomon 2006Ottofianus Hewick KalangiNo ratings yet
- Erectile Dysfunction and Comorbid Diseases, Androgen Deficiency, and Diminished Libido in MenDocument7 pagesErectile Dysfunction and Comorbid Diseases, Androgen Deficiency, and Diminished Libido in MenAfif Al FatihNo ratings yet
- Captura de Pantalla 2022-08-15 A La(s) 17.37.40 PDFDocument11 pagesCaptura de Pantalla 2022-08-15 A La(s) 17.37.40 PDFMatias PadillaNo ratings yet
- Pharmaceutics 15 01002 v3Document20 pagesPharmaceutics 15 01002 v3YASH BNo ratings yet
- Chew Et Al-2008-Journal of The American Geriatrics Society PDFDocument9 pagesChew Et Al-2008-Journal of The American Geriatrics Society PDFChrysoula GkaniNo ratings yet
- JNC8Document21 pagesJNC8ZakisyarifudintaqiyNo ratings yet
- Pharmacological and Parenteral Therapies in Older Adult PopulationDocument5 pagesPharmacological and Parenteral Therapies in Older Adult PopulationNDINDA GODYFREEY NATTOHNo ratings yet
- Geriatric Drug TherapyDocument48 pagesGeriatric Drug Therapywalt65No ratings yet
- AndrologyDocument298 pagesAndrologyPrakash JanakiramanNo ratings yet
- Hulley 1998Document9 pagesHulley 1998junta.propietarios.1456No ratings yet
- Variation of Drug Response-1Document26 pagesVariation of Drug Response-1كسلان اكتب اسميNo ratings yet
- Management of Constipation in Patients With Schizophrenia - A Case Study and Review of LiteratureDocument7 pagesManagement of Constipation in Patients With Schizophrenia - A Case Study and Review of LiteratureRimayNo ratings yet
- Hormone Replacement HerapyDocument5 pagesHormone Replacement HerapyCindy HartNo ratings yet
- Cfs 8 PDFDocument9 pagesCfs 8 PDFDaniel Fernando Mendez CarbajalNo ratings yet
- Risk Related To Hormone Therapy and Cardiovascular Disease in WomenDocument44 pagesRisk Related To Hormone Therapy and Cardiovascular Disease in Womenosama saeedNo ratings yet
- Pharmacogenetics and The Concept of Individualized Medicine: BS ShastryDocument6 pagesPharmacogenetics and The Concept of Individualized Medicine: BS Shastrykunalprabhu148No ratings yet
- Cardiology PDFDocument9 pagesCardiology PDFFC Mekar AbadiNo ratings yet
- Ultrafiltration Therapy For Cardiorenal Syndrome Physiologic Basis and Contemporary OptionsDocument9 pagesUltrafiltration Therapy For Cardiorenal Syndrome Physiologic Basis and Contemporary Optionsfernando.suarez.mtzNo ratings yet
- Cancer-Relatedfatiguein Cancersurvivorship: Chidinma C. Ebede,, Yongchang Jang,, Carmen P. EscalanteDocument13 pagesCancer-Relatedfatiguein Cancersurvivorship: Chidinma C. Ebede,, Yongchang Jang,, Carmen P. EscalanteMahdhun ShiddiqNo ratings yet
- Reversibledementias: Milta O. LittleDocument26 pagesReversibledementias: Milta O. LittleLUCAS IGNACIO SANCHEZNo ratings yet
- Interacciones Medicamentos en Odontologia 2017 PDFDocument35 pagesInteracciones Medicamentos en Odontologia 2017 PDFDANIELA PARRA BOTERONo ratings yet
- 1 s2.0 S0735109723003686 MainDocument19 pages1 s2.0 S0735109723003686 MainArunNo ratings yet
- Hudmon 2007Document4 pagesHudmon 2007ARAFAT MIAHNo ratings yet
- Preventive Cardiology For WomenDocument5 pagesPreventive Cardiology For WomenninataniaaaNo ratings yet
- CollegePharmacy BHRT Abstracts ReviewsDocument46 pagesCollegePharmacy BHRT Abstracts ReviewsJoyce IpadNo ratings yet
- Ethn 15 01 116Document8 pagesEthn 15 01 116Bot AINo ratings yet
- Gerotological Care IssuesDocument21 pagesGerotological Care IssuesOdey GodwinNo ratings yet
- Case StudiesDocument5 pagesCase Studiespragna novaNo ratings yet
- Prescribing For The ElderlyDocument8 pagesPrescribing For The ElderlykarladeyNo ratings yet
- Comparative Effectiveness of Diuretic Regimens: EditorialDocument2 pagesComparative Effectiveness of Diuretic Regimens: EditorialFabio Luis Padilla AvilaNo ratings yet
- Geriatric Pharmacology. Journal of The American Podriatric Medical AssociationDocument8 pagesGeriatric Pharmacology. Journal of The American Podriatric Medical AssociationJose Fernando Díez ConchaNo ratings yet
- Examining The Effects of Herbs On TestosteroneDocument22 pagesExamining The Effects of Herbs On TestosteroneKelson dos SantosNo ratings yet
- Evidence Based Care For All Patients - AjmDocument3 pagesEvidence Based Care For All Patients - Ajmdaniel martinNo ratings yet
- Consenso IccDocument15 pagesConsenso IccMaida Martinez AngelesNo ratings yet
- David J. Greenblatt D. (ZOLPIDEM) 2Document9 pagesDavid J. Greenblatt D. (ZOLPIDEM) 2Antonio SanchezNo ratings yet
- Top 5 - Considerations For Anesthesia of A Geriatric PatientDocument5 pagesTop 5 - Considerations For Anesthesia of A Geriatric PatientMabe AguirreNo ratings yet
- The Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianFrom EverandThe Prevention and Treatment of Disease with a Plant-Based Diet Volume 2: Evidence-based articles to guide the physicianNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 4: VascularFrom EverandComplementary and Alternative Medical Lab Testing Part 4: VascularNo ratings yet
- Hprocedure of Export or ImportDocument96 pagesHprocedure of Export or ImportHiren RatnaniNo ratings yet
- IntroductionDocument15 pagesIntroductionAhinurNo ratings yet
- Star Holman 210HX Conveyor OvenDocument2 pagesStar Holman 210HX Conveyor Ovenwsfc-ebayNo ratings yet
- Global Warming (Word Formation)Document2 pagesGlobal Warming (Word Formation)EvaNo ratings yet
- Bba 400 Module Revised 2017 April To DsvolDocument68 pagesBba 400 Module Revised 2017 April To DsvolKafonyi JohnNo ratings yet
- IfDocument44 pagesIfSean RoxasNo ratings yet
- The Wall Street Journal - Vol. 277 No. 075 (01 Apr 2021)Document32 pagesThe Wall Street Journal - Vol. 277 No. 075 (01 Apr 2021)Andrei StrăchinescuNo ratings yet
- Islam Articles of FaithDocument1 pageIslam Articles of Faithapi-247725573No ratings yet
- AlgecirasDocument7 pagesAlgecirasEvrenNo ratings yet
- NavAid Module 2.0Document21 pagesNavAid Module 2.0Kiel HerreraNo ratings yet
- Putra, 003 - 3035 - I Wayan Adi Pranata - GalleyDocument7 pagesPutra, 003 - 3035 - I Wayan Adi Pranata - Galleyeunike jaequelineNo ratings yet
- Beyond Risk - Bacterial Biofilms and Their Regulating ApproachesDocument20 pagesBeyond Risk - Bacterial Biofilms and Their Regulating ApproachesVictor HugoNo ratings yet
- Måttblad Bauer BK P7112BGM CatalogueB2010 0312 en A4 Chapter12Document54 pagesMåttblad Bauer BK P7112BGM CatalogueB2010 0312 en A4 Chapter12earrNo ratings yet
- Physics 158 Final Exam Review Package: UBC Engineering Undergraduate SocietyDocument22 pagesPhysics 158 Final Exam Review Package: UBC Engineering Undergraduate SocietySpam MailNo ratings yet
- Crawling Under A Broken Moon 05Document28 pagesCrawling Under A Broken Moon 05Maxim BorisovNo ratings yet
- Soil Pollution: Causes, Effects and Control: January 2016Document15 pagesSoil Pollution: Causes, Effects and Control: January 2016Nagateja MondretiNo ratings yet
- 520SL SLB Guide en USDocument2 pages520SL SLB Guide en USBruce CanvasNo ratings yet
- CASE REPORT On OsteomyelitisDocument30 pagesCASE REPORT On OsteomyelitisNirbhay KatiyarNo ratings yet
- TCS Ninja English Questions and AnswersDocument16 pagesTCS Ninja English Questions and AnswersVijayPrajapatiNo ratings yet
- DER Vol III DrawingDocument50 pagesDER Vol III Drawingdaryl sabadoNo ratings yet
- Pressure Switch MDR5Document4 pagesPressure Switch MDR5Fidelis NdanoNo ratings yet
- User'S Manual: Questions?Document32 pagesUser'S Manual: Questions?gorleanosNo ratings yet
- 04 Vikram Pawar Volume 3 Issue 2Document18 pages04 Vikram Pawar Volume 3 Issue 2Juwan JafferNo ratings yet
- Composite EbookDocument285 pagesComposite Ebooksunilas218408100% (1)
- L-s20 Specification For Road Lighting InstallationDocument82 pagesL-s20 Specification For Road Lighting Installationzamanhuri junidNo ratings yet
- Equivalent Length Calculator - RevADocument10 pagesEquivalent Length Calculator - RevArkrajan1502No ratings yet
- (M. J. Edwards) The ''Epistle To Rheginus'' ValenDocument17 pages(M. J. Edwards) The ''Epistle To Rheginus'' ValenGlebMatveevNo ratings yet
- Bristow Part B EC155B1 Section 2 LimitationsDocument4 pagesBristow Part B EC155B1 Section 2 LimitationsrobbertmdNo ratings yet