Professional Documents
Culture Documents
Safetyof Peripheral Administrationof 3 Hypertonic Salinein Critically Ill Patients ALiterature Review
Safetyof Peripheral Administrationof 3 Hypertonic Salinein Critically Ill Patients ALiterature Review
Uploaded by
YoelOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Safetyof Peripheral Administrationof 3 Hypertonic Salinein Critically Ill Patients ALiterature Review
Safetyof Peripheral Administrationof 3 Hypertonic Salinein Critically Ill Patients ALiterature Review
Uploaded by
YoelCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/348940355
Safety of Peripheral Administration of 3% Hypertonic Saline in Critically Ill
Patients: A Literature Review
Article in Critical Care Nurse · February 2021
DOI: 10.4037/ccn2021400
CITATIONS READS
10 929
4 authors, including:
Ahmed Alenazi
National Guard Health Affairs
20 PUBLICATIONS 58 CITATIONS
SEE PROFILE
All content following this page was uploaded by Ahmed Alenazi on 29 September 2021.
The user has requested enhancement of the downloaded file.
Feature
Safety of Peripheral
Administration of 3%
Hypertonic Saline in
Critically Ill Patients:
A Literature Review
Ahmed O. Alenazi, PharmD, BSc, CACP
Zahra M. Alhalimi, PharmD
Manar H. Almatar, PharmD
Taha A. Alhajji, BS Pharm
Background Hyponatremia and neurocritical injury are life-threatening conditions requiring immediate
management with consideration of the safety concerns related to peripheral intravenous administration
of hypertonic solutions. Although a central intravenous catheter is the preferred route of administration,
central intravenous catheters have many complications and can potentially delay medication administra-
tion in urgent situations.
Objective To evaluate the safety and efficacy of continuous infusion of 3% hypertonic saline via peripheral
intravenous administration in critically ill adult patients.
Methods Data were collected from PubMed and Web of Science from database inception to April 7, 2019.
Included studies involved adult patients with hyponatremia and/or neurocritical situations and compared
administration of 3% hypertonic saline via peripheral administration with standard supportive care (admin-
istration through a central intravenous catheter).
Results Of 502 articles identified, 7 were included in the review. Three articles were retrospective studies,
2 were prospective studies, 1 was a case series, and 1 was a case report. Infusion-related adverse events
and electrolyte abnormalities due to 3% hypertonic saline administration through a peripheral intravenous
catheter were minimal and were limited to phlebitis, erythema, edema, hyperchloremia, and hypokalemia
with administration at a high infusion rate (83.3 mL/h) and for a prolonged duration (≥ 6 hours). Infusion
rate, duration, catheter gauge, and catheter placement may have a role in infusion-related adverse events.
Conclusions Current recommendations to administer continuous infusions of 3% hypertonic saline
through a central intravenous catheter should be reassessed. Peripheral intravenous administration can
be used safely and effectively in patients in critical situations. (Critical Care Nurse. 2021;41[1]:25-31)
H
yponatremia, defined as a serum sodium concentration of less than 135 mEq/L, is one of
the most prevalent electrolyte abnormalities in clinical practice.1 Hyponatremia occurs in
15% to 30% of hospitalized patients.2 The incidence and prevalence vary because the sodium
level can be affected by factors such as patient population, laboratory methods, and diagnostic criteria.2
Hyponatremia can increase morbidity, mortality, and length of hospital stay for a variety of high-risk
disorders or diseases such as heart failure, liver cirrhosis, and critical illness.3,4
©2021 American Association of Critical-Care Nurses doi:https://doi.org/10.4037/ccn2021400
www.ccnonline.org CriticalCareNurse Vol 41, No. 1, FEBRUARY 2021 25
Table 1 Classification and common disorders of hyponatremia according to volume status5-7
Hypovolemia Euvolemia Hypervolemia
Gastrointestinal fluid loss (eg, Medications (see Table 2) Acute kidney injury/chronic
severe diarrhea or vomiting) Syndrome of inappropriate antidiuretic hormone resulting kidney disease
Third spacing of fluids (eg, from malignancy, central nervous system disorders (eg, Congestive heart failure
pancreatitis, severe subarachnoid hemorrhage, meningitis, encephalitis), Liver cirrhosis
hypoalbuminemia) pulmonary disease (eg, pneumonia), or idiopathic origin Nephrotic syndrome
Salt-wasting nephropathy High fluid intake
Cerebral salt-wasting syndrome Intense/prolonged physical activity (eg, marathon running)
Mineralocorticoid deficiency Primary polydipsia (also referred to as psychogenic polydipsia)
The different causes and comorbidities associated
with a low sodium level pose major challenges in the Table 2 Mechanisms of hyponatremia caused
by drugs6,7
management of hyponatremia. Hyponatremia is primar-
ily a water imbalance and is associated with a disturbance Medication Mechanism of hyponatremia
Desmopressin Vasopressin analogues; pro-
in the hormone vasopressin (antidiuretic hormone). The Oxytocin motes water reabsorption
causes of hyponatremia are classified according to reduced, in kidney and return of
normal, or increased extracellular fluid volume (Table 1).5-7 water to blood circulation
Antidepressants Stimulate release or potentiate
Drugs cause hyponatremia through various mechanisms Opioids the effects of vasopressin
(Table 2). The most frequent mechanism is an increase 3,4-Methylenedioxymetham
in vasopressin release, increasing the inhibition of sodium phetamine (ecstasy)
reabsorption at the kidneys. Diuretics prevent sodium Diuretics Impaired urine dilution
Carbamazepine Uncertain mechanism of
reabsorption in the kidney tubules, resulting in a higher Vincristine action
level of sodium elimination.8 Antipsychotics
Signs and symptoms of hyponatremia vary depending Cyclophosphamide
Nonsteroidal anti-
on the acuity and severity of the hyponatremia (Table 3).5-7 inflammatory drugs
Severe neurological symptoms occur when the hypona-
tremia develops acutely (usually in less than 48 hours)
because the brain cannot adapt to this rapid change in Table 3 Hyponatremia signs and symptoms5,7
the sodium level. Cerebral edema develops subsequent
Severe acute Severe headache, obtundation, frank
to the water shift in the brain cells. In mild to moderate symptoms ataxia, seizures, cerebral edema,
chronic hyponatremia, brain cells adapt to the change, brainstem herniation, coma, death
and the patient remains asymptomatic or has mild cog- Mild symptoms Nausea, mild headache, mild ataxia,
mild cognitive impairment
nitive signs.5-7
Hyponatremia classifications are not mutually
Authors
exclusive. Clinical correlation and the possibility of
Ahmed O. Alenazi is a critical care clinical pharmacist, Al Imam multiple causes of hyponatremia should be considered.5
Abdulrahman Bin Faisal Hospital, Dammam, Saudi Arabia.
The different classifications are based on the serum
Zahra M. Alhalimi was a PharmD student at Al Imam Abdulrahman
Bin Faisal University, Dammam, at the time of writing this article. sodium concentration, symptoms, duration and rapid-
Manar H. Almatar was a PharmD student at Al Imam Abdulrah- ity of development, serum osmolality, and body volume
man Bin Faisal University, at the time of writing this article. status (Table 4).5-7
Taha A. Alhajji is an inpatient pharmacist, Al Imam Abdulrahman The management of hyponatremia depends on the
Bin Faisal Hospital. acuity and severity of the symptoms, volume status, and
Corresponding author: Ahmed O. Alenazi, PharmD, BSc, CACP, Al Imam Abdulrahman underlying cause. Rapid correction in severely symptom-
Bin Faisal Hospital, Ministry of National Guard-Health Affairs, PO Box 4616, atic patients is important to prevent serious neurological
Dammam, Saudi Arabia 31412 (email: alenaziah5@ngha.med.sa).
sequelae. Evidence indicates that the therapeutic limit of
To purchase electronic or print reprints, contact the American Association of Critical-
Care Nurses, 27071 Aliso Creek Rd, Aliso Viejo, CA 92656. Phone, (800) 899-1712 sodium correction with hypertonic saline (HTS) ranges
or (949) 362-2050 (ext 532); fax, (949) 362-2049; email, reprints@aacn.org. from 8 to 12 mEq/L in the first 24 hours.3,9 Too-rapid
26 CriticalCareNurse Vol 41, No. 1, FEBRUARY 2021 www.ccnonline.org
Table 4 Classifications of hyponatremia criteria5,7
Criteria Classification
Serum sodium concentration Mild: serum sodium concentration of 130 to 135 mEq/L
Moderate: serum sodium concentration of 125 to 129 mEq/L
Severe: serum sodium concentration less than 125 mEq/L
Symptoms Symptomatic: mild, moderate, or severe symptoms
Asymptomatic
Onset Acute: duration less than 48 hours
Chronic: duration greater than 48 hours
Osmolality (tonicity) Hypotonic: low plasma osmolality less than 280 mOsm/kg H2O
Isotonic: plasma osmolality within reference range (280-295 mOsm/kg H2O)
Hypertonic: plasma osmolality greater than 295 mOsm/kg H2O
Volume status Hypovolumic: sodium depletion in excess of water depletion
Euvolumic: excess of total body water with no change in total body sodium
Hypervolumic: increase in both total body water and sodium but with a relatively greater
increase in total body water than in sodium
Table 5 Comparison of US and European guidelines for treatment of acute or symptomatic hyponatremia6
Symptoms US guidelines European guidelines
Severe Bolus of 100 mL of 3% sodium chloride over Bolus of 150 mL of 3% sodium chloride over
10 minutes, 3 times as needed 20 minutes, 2 to 3 times as needed
Moderate Continuous infusion of 3% sodium chloride at 0.5-2 mL/kg/h Bolus of 150 mL of 3% sodium chloride over 20 minutes once
correction increases the risk of osmotic demyelination Methods
syndrome,6 which is characterized by extensive demye- Study Design and Search Strategy
lination in the brain and poor outcomes.10 We conducted this review by searching PubMed and
To regulate and improve hyponatremia management, Web of Science database entries from the inception of
professional organizations have developed 2 sets of guide- each database to April 7, 2019. We searched the terms
lines.3,7 Both guidelines support the administration of a hypertonic saline, 3% hypertonic saline, 3% sodium chloride,
bolus of 3% HTS for patients with acute or severely symp- hyperosmolar, peripheral administration, infusion, peripheral
tomatic hyponatremia. However, the US guideline recom- catheterization, critically ill, cerebral edema, hyponatremia,
mends a continuous infusion of 3% HTS for moderately neurocritical, and intensive care unit alone or in combina-
symptomatic patients with hyponatremia, whereas the tion. We screened titles and abstracts to determine whether
European guideline endorses a bolus dose only (Table 5). the publications met the eligibility criteria. To maximize
Hypertonic saline 3% has a high sodium level the search for relevant publications, we reviewed refer-
(513 mEq/L) and a high osmolarity (1026 mOsm/L) ence lists of the selected publications. English language
that exceeds the accepted limit for peripheral paren- was the only restriction.
teral nutrition recommended by the American Soci-
ety for Parenteral and Enteral Nutrition guideline (900 Eligibility Criteria
mOsm/L).9 A central intravenous catheter (CIVC) is Eligible studies met the inclusion criteria if the popu-
the preferred route of administration.9,11 However, insert- lation of interest was adults (age ≥ 18 years) with hypo-
ing a CIVC is not risk free. The risks include arterial natremia and/or a neurocritical situation. In included
puncture, pneumothorax, infection, thrombosis, and studies, the intervention was administration of 3% HTS
potential delay in medication administration in time- through a peripheral intravenous catheter (PIVC) com-
sensitive situations.9,11 Phlebitis and extravasation pared with standard supportive care (administration of
injuries are the main safety concerns with peripheral 3% HTS through a CIVC). Studies were excluded if they
administration of 3% HTS.9,11 This review article evalu- were conducted in a pediatric population, if the interven-
ates the safety and efficacy of continuous infusion of tion included HTS solutions other than 3% HTS, or if 3%
3% HTS via peripheral intravenous administration in HTS was administered through any route other than a
critically ill adult patients. central or peripheral catheter.
www.ccnonline.org CriticalCareNurse Vol 41, No. 1, FEBRUARY 2021 27
medical step-down setting who had hyponatremia (64%)
502 Articles were identified through database searches or cerebral edema (29%). Hypertonic saline 3% was adminis-
tered for 14 hours, with a median infusion rate of 32 mL/h.
483 Articles excluded because of topic: Infusion-related adverse events classified as grade 1 in
Pharmacokinetics: 19
Pharmacology/pathology: 282 severity were reported in 4 patients. According to the
Diagnosis: 10 Infusion Nurses Society infiltration scale, which was used
Other unrelated: 172
in the study, grade 1 is defined as blanched skin, edema
19 Articles less than 1 inch in any direction, skin cool to the touch,
and pain present or not present. In 2 patients (50%), the
10 articles excluded because of duplication IRAEs were managed by removing the PIVC and replac-
2 articles excluded because of pediatric
population ing the infusion at a different peripheral anatomical site.
Phlebitis accounted for 50% of the IRAEs; 2 patients had
7 Articles were included in the study erythema and edema less than 1 inch in diameter.14 In
2015, Ayus et al16 reported a case series of 64 patients.
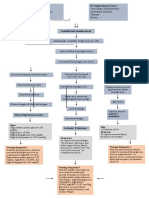
Figure Summary of article selection. The patients had 71 hyponatremic episodes due to inap-
propriate antidiuretic hormone syndrome (61%), thiazide
The primary outcome was identification of the diuretics (34%), or hypothyroidism (5%). The patients
infusion-related adverse events (IRAEs) and electrolyte received 500 mL of 3% HTS over 6 hours (83.3 mL/h)
disturbances most frequently reported with peripheral for the management of hyponatremia in the emergency
administration of 3% HTS. Secondary outcomes were department per the hospital protocol, and no infusion-
the rate and duration of the infusion, catheter gauge, related reactions were reported.16
anatomical site of catheter insertion, occurrence of The duration and rate of infusion of 3% HTS prescribed
cerebral demyelination, rate of hyponatremia correction, for PIVC administration may play a role in the develop-
and overall mortality rate. Infusion-related adverse events ment of IRAEs. In 2016, Jones et al12 conducted a large
included phlebitis, extravasation, and venous thrombus. retrospective cohort study of the safety of a continuous
According to published studies, frequently occurring peripheral infusion of 3% HTS. The study recruited 213
electrolyte abnormalities include hypokalemia, hyper- neurocritical care patients in the ICU or medical ward.
chloremia, hypernatremia, and hypobicarbonatemia. Of these, 157 patients (73.7%) received 3% HTS via a
PIVC with an infusion rate of 30 to 75 mL/h and a median
Results duration of 44 hours, 43 minutes. Fifteen IRAEs were
The initial search identified 502 publications. We reported, including 9 cases of phlebitis and 6 cases of
excluded 483 irrelevant publications after reviewing the extravasation with no venous thrombus in any of the
titles and abstracts, 10 publications because of duplica- patients.12 In a prospective study, Perez and Figueroa11
tion, and 2 publications because the population of inter- assessed the complication rate of 3% HTS infusion
est did not meet inclusion criteria. Seven publications through a PIVC. The sample was 28 patients with
were eligible. Of these, 3 were retrospective studies,11-13 2 neurocritical illness who received 3% HTS peripherally
were prospective studies,14,15 1 was a case series,16 and 1 for the management of cerebral hemorrhage, stroke,
was a case report.17 The population sizes ranged from 28 and tumors in different ICU settings. A 3% HTS solu-
to 213 patients in all studies except 1 case report that tion was infused at a rate of 30 to 50 mL/h for a mean
included 1 patient. Only 1 of the studies included was a duration of 36 hours. Local extravasation occurred in 2
multicenter study; all other studies were single-center patients, with no major complications except for throm-
studies (see Figure). bophlebitis in 1 of the patients.11 Similarly, a prospective
Four studies11-14 reported IRAEs and 2 studies12,15 study published by Meng et al13 in 2018 investigated the
reported electrolyte abnormalities due to 3% HTS admin- association of phlebitis with continuous PIVC infusion
istered through a PIVC. Dillon et al14 conducted a retro- of 3% HTS in 60 adult patients. Most patients (78%)
spective study to investigate the incidence of IRAEs received 3% HTS for the management of neurological
during peripheral administration of 3% HTS. The study injuries. Infusion rates ranged from 15 to 100 mL/h (mean
recruited 66 patients in an intensive care unit (ICU) or a infusion rate, 42 mL/h) and the mean infusion duration
28 CriticalCareNurse Vol 41, No. 1, FEBRUARY 2021 www.ccnonline.org
was 74.4 hours, or 3.1 days. Phlebitis was reported in 19 with hyponatremia (serum sodium level, 119 mEq/L)
patients whose infusion rates were 30 mL/h or less and who died 4 hours after admission to the hospital. The
in 13 patients whose infusion rates were greater than patient died because of a delay in the administration of
30 mL/h; this difference was not significant (P = .38).13 HTS; the hospital protocol limited the use of 3% HTS
Catheter gauge and anatomical site of administration to ICU settings and CIVC administration only.19 Wide-
may also affect the incidence of IRAEs. Four studies men- spread misconceptions without strong evidence about
tioned the needle or catheter gauge, which ranged from the peripheral administration of 3% HTS and IRAEs
16 to 24 gauge.11-14 Two studies associated the develop- exist. Concern about peripheral administration might
ment of phlebitis with the gauge. Jones et al12 reported 8 be valid when using a hypertonic peripheral parenteral
events in patients whose catheters had 20-gauge needles nutrition solution for more than 5 days.17
and 7 events in patients whose catheters had 18-gauge The IRAEs of thrombophlebitis, infusion extravasa-
needles. According to the study by Meng et al,13 phlebi- tion, and venous thrombus formation were minimally
tis was observed in 9 of 26 patients who received 16- to reported with administration of 3% HTS through a
18-gauge catheters and 23 of 80 patients who received peripheral vein. No permanent tissue injuries were
20- to 24-gauge catheters. In terms of the anatomical reported even with peripheral administration of 3%
site used to administer 3% HTS, Meng et al13 mentioned HTS with a prolonged duration and a high infusion
using a flexion site (including the antecubital fossa or rate.14 One study provided evidence that the develop-
wrist) in 32% of patients and a nonflexion site (such as ment of thrombophlebitis with peripheral adminis-
foot, hand, forearm, or arm) in 30% of patients. However, tration of 3% HTS was insignificant compared with
the association between catheter gauge or anatomical peripheral administration of all other solutions used in
site and the development of phlebitis was not significant routine care (47% vs 43%, P = .19).13 In addition, several
(P > .05).13 Other studies also mentioned the use of dif- studies did not report an increase in the rate of throm-
ferent sites of administration.11,12,14 botic events (deep venous thrombosis and pulmonary
Electrolyte abnormalities were discussed in studies embolism) with 3% HTS administration.11,20
by Jones et al12 and Mesghali et al.15 Hyperchloremia This review included 2 reports of venous thrombo-
(49.3% and 38.8%, respectively), hypokalemia (46.9% sis. In the study by Meng et al,13 1 patient developed a
and 24.7%, respectively), and hypernatremia (22.1% and superficial thrombus in the cephalic vein but did not
8.2%, respectively) were the electrolyte abnormalities require
most frequently reported with 3% HTS infusion. Hypobi- interven- Common infusion-related adverse
carbonatemia was also mentioned in a small proportion tion. In the events include extravasation; blanched
of patients (8.9%) in the study by Jones et al.12 Almost study by skin, erythema, and edema; phlebitis;
half of the patients with a hypokalemia-related abnor- Perez and venous thrombus; necrosis or ulceration;
mality (43.6%) required an intervention to correct the Figueroa,11 and life-threatening consequences.
potassium level, and a small proportion of patients with infiltration
hyperchloremia (16.9%) required an intervention. was noted in 1 patient after infusion of 3% HTS in the
left hand. The infusion was relocated to the right arm
Discussion and the patient developed infiltration. Doppler ultra-
Hyponatremia, traumatic brain injury, intracerebral sound of both arms showed thrombus in only the right
hemorrhage, and acute ischemic stroke are life-threatening brachial and basilic veins.
conditions that should be managed rapidly and effectively Many factors increase the risk for venous thrombosis
with consideration for the safety concerns related to hyper- with administration of 3% HTS. Examples are longer
tonic solutions. Central venous catheters, although con- duration of catheterization, the catheter material used,
sidered effective instruments in patient care, are associated the type of infusion, and vascular comorbidities. Vascu-
with complications that may increase the length of stay, lar comorbidities such as hypertension, diabetes, dyslip-
mortality rate, and cost of care.12,18 Any delay in HTS idemia, and coronary artery disease, reported in 57%
preparation, delivery, or catheter insertion may increase of the patients in the study by Meng et al,13 may play a
the patient’s likelihood of morbidity or mortality. Ayus major role in venous thrombosis related to HTS. The
and Moritz19 reported the case of a 21-year-old patient median catheter duration was also significantly longer
www.ccnonline.org CriticalCareNurse Vol 41, No. 1, FEBRUARY 2021 29
in patients receiving 3% HTS (2.6 days) than in those Acknowledgments
The authors listed in the byline are the only investigators responsible for this
receiving routine-care solutions (2.1 days, P = .01). With review article. This review was performed through electronic medical search
the available evidence, it is not possible to correlate engines at Al Imam Abdulrahman Bin Faisal Hospital. This review article has
been not presented at any conference or meeting.
venous thrombosis and the administration of 3% HTS
in the presence of vascular comorbidities. Financial Disclosures
None reported.
Neurological symptoms related to 3% HTS are usually
monitored closely in the ICU.19 Cerebral demyelination
See also
is a major neurological complication caused by overcor- To learn more about patient safety in the critical care setting, read “Safety
rection of the sodium level by more than 12 mEq/d in of Continuous Peripheral Infusion of 3% Sodium Chloride Solution in
Neurocritical Care Patients” by Jones et al in the American Journal of
patients with chronic hyponatremia.16 In a study of 71 Critical Care, 2017;26(1):37-42. Available at www.ajcconline.org.
patients with hyponatremia (mean [SEM] baseline sodium References
level, 114.1 [0.8] mEq/L) who received 3% HTS, mean 1. Liamis G, Rodenburg EM, Hofman A, Zietse R, Stricker BH, Hoorn EJ.
Electrolyte disorders in community subjects: prevalence and risk factors.
(SEM) sodium levels 3, 12, 24, and 48 hours after initia- Am J Med. 2013;126(3):256-263.
tion of 3% HTS infusion increased to 117.9 (1.3), 121.2 2. Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hypona-
tremia. Am J Med. 2006;119(7 suppl 1):S30-S35.
(1.2), 123.9 (1.0), and 128.3 (0.8) mEq/L, respectively.16 3. Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline
Development Group. Clinical practice guideline on diagnosis and treat-
Clinical and neurological symptoms markedly improved, ment of hyponatraemia. Nephrol Dial Transplant. 2014;29(suppl 2):i1-i39.
with patients making a full recovery after 48 hours of 3% 4. Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with
mild, moderate, and severe hyponatremia. Am J Med. 2009;122(9):857-865.
HTS infusion. Five patients with a significant overcorrec- 5. Ball SG, Iqbal Z. Diagnosis and treatment of hyponatraemia. Best Pract
Res Clin Endocrinol Metab. 2016;30(2):161-173.
tion of sodium (≥ 25 mEq/L over 48 hours) did not develop 6. Hoorn EJ, Zietse R. Diagnosis and treatment of hyponatremia: compila-
any neurological symptoms associated with cerebral demy- tion of the guidelines. J Am Soc Nephrol. 2017;28(5):1340-1349.
7. Verbalis JG, Goldsmith SR, Greenberg A, et al. Diagnosis, evaluation,
elination.16 No other studies discussed the relationship and treatment of hyponatremia: expert panel recommendations. Am J
Med. 2013;126(10 suppl 1):S1-S42.
between peripheral administration of 3% HTS and the 8. Klabunde RE. Diuretics. Cardiovascular Pharmacology Concepts. Updated
development of demyelination. More studies are required November 17, 2017. Accessed October 16, 2020. https://cvpharmacology.
com/diuretic/diuretics
to confirm the relationship between cerebral demyelin- 9. Boullata JI, Gilbert K, Sacks G, et al; American Society for Parenteral and
Enteral Nutrition. A.S.P.E.N. clinical guidelines: parenteral nutrition
ation and the peripheral administration of 3% HTS. ordering, order review, compounding, labeling, and dispensing. JPEN J
In 1 study, 5% HTS was infused peripherally over Parenter Enteral Nutr. 2014;38(3):334-377.
10. King JD, Rosner MH. Osmotic demyelination syndrome. Am J Med Sci.
15 minutes to 11 patients with an elevated intracranial 2010;339(6):561-567.
11. Perez CA, Figueroa SA. Complication rates of 3% hypertonic saline infusion
pressure, and no IRAEs were documented.21 Electrolyte through peripheral intravenous access. J Neurosci Nurs. 2017;49(3):191-195.
abnormalities were frequently reported, but the clinical 12. Jones GM, Bode L, Riha H, Erdman MJ. Safety of continuous peripheral
infusion of 3% sodium chloride solution in neurocritical care patients.
importance is still not clear. Am J Crit Care. 2016;26(1):37-42.
13. Meng L, Nguyen CM, Patel S, Mlynash M, Caulfield AF. Association
between continuous peripheral i.v. infusion of 3% sodium chloride injec-
Conclusions tion and phlebitis in adults. Am J Health Syst Pharm. 2018;75(5):284-291.
14. Dillon RC, Merchan C, Altshuler D, Papadopoulos J. Incidence of
This review article demonstrates that 3% HTS can be adverse events during peripheral administration of sodium chloride 3.
safely administered peripherally in acutely ill patients, J Intensive Care Med. 2018;33(1):48-53.
15. Mesghali E, Fitter S, Bahjri K, Moussavi K. Safety of peripheral line
causing a minimum of IRAEs even at a high rate of infu- administration of 3% hypertonic saline and mannitol in the emergency
department. J Emerg Med. 2019;56(4):431-436.
sion (83.3 mL/h) for a prolonged duration (≥6 hours). 16. Ayus JC, Caputo D, Bazerque F, Heguilen R, Gonzalez CD, Moritz ML.
The most frequently reported IRAE was thrombophlebi- Treatment of hyponatremic encephalopathy with a 3% sodium chloride
protocol: a case series. Am J Kidney Dis. 2015;65(3):435-442.
tis (< 10% of patients), with an insignificant difference 17. Timmer JG, Schipper HG. Peripheral venous nutrition: the equal rele-
vance of volume load and osmolarity in relation to phlebitis. Clin Nutr.
between patients who received 3% HTS and patients 1991;10(2):71-75.
who received routine-care solutions. The current recom- 18. Leistner R, Hirsemann E, Bloch A, Gastmeier P, Geffers C. Costs and
prolonged length of stay of central venous catheter-associated blood-
mendation to administer 3% HTS through CIVCs should stream infections (CVC BSI): a matched prospective cohort study. Infec-
tion. 2014;42(1):31-36.
therefore be reevaluated. Peripheral intravenous cathe- 19. Ayus JC, Moritz ML. Misconceptions and barriers to the use of hyper-
ters can be used safely and effectively for the administra- tonic saline to treat hyponatremic encephalopathy. Front Med (Laus-
anne). 2019;6:47.
tion of 3% HTS in patients in critical circumstances. 20. Froelich M, Ni Q, Wess C, Ougorets I, Härtl R. Continuous hypertonic
saline therapy and the occurrence of complications in neurocritically ill
Additional studies are required to evaluate the effects of patients. Crit Care Med. 2009;37(4):1433-1441.
peripheral administration of 3% HTS on length of stay, 21. Carter C, Human T. Efficacy, safety, and timing of 5% sodium chloride
compared with 23.4% sodium chloride for osmotic therapy. Ann Phar-
mortality rate, and health care costs. CCN macother. 2017;51(8):625-629.
30 CriticalCareNurse Vol 41, No. 1, FEBRUARY 2021 www.ccnonline.org
CCN Fast Facts CriticalCareNurse
The journal for high acuity, progressive, and critical care nursing
Safety of Peripheral Administration of
3% Hypertonic Saline in Critically Ill
Patients: A Literature Review
H yponatremia and neurocritical injury are life-
threatening conditions requiring immediate
management with consideration of the safety
concerns related to peripheral intravenous administration
of hypertonic solutions. Although a central intravenous
• Neurological symptoms related to 3% HTS are usually
monitored closely by health care providers in the
intensive care unit. Cerebral demyelination is a major
neurological complication caused by overcorrection
of the sodium level by more than 12 mEq/d in
catheter is the preferred route of administration, central patients with chronic hyponatremia.
intravenous catheters have many complications and can
potentially delay medication administration in urgent sit- • In 1 study, 5% HTS was infused peripherally over 15
uations. This review article evaluates the safety and effi- minutes to 11 patients with an elevated intracranial
cacy of continuous infusion of 3% hypertonic saline (HTS) pressure, and no IRAEs were documented. Electrolyte
via peripheral intravenous administration in critically ill abnormalities were frequently reported, but the clini-
adult patients. cal importance is still not clear.
• Central venous catheters, although considered effec- • This review article demonstrates that 3% HTS can be
tive instruments in patient care, are associated with safely administered peripherally in acutely ill patients,
complications that may increase the length of stay, causing a minimum of IRAEs even at a high rate of infu-
mortality rate, and cost of care. sion (83.3 mL/h) for a prolonged duration (≥ 6 hours).
• Widespread misconceptions without strong evidence • The most frequently reported IRAE was thrombophle-
about the peripheral administration of 3% HTS and bitis (< 10% of patients), with an insignificant difference
infusion-related adverse events (IRAEs) exist. between patients who received 3% HTS and patients
who received routine-care solutions. The current rec-
• The IRAEs of thrombophlebitis, infusion extravasa- ommendation to administer 3% HTS through central
tion, and venous thrombus formation were minimally intravenous catheters should therefore be reevaluated.
reported with administration of 3% HTS through a
peripheral vein. No permanent tissue injuries were • Peripheral intravenous catheters can be used safely
reported even with peripheral administration of 3% and effectively for the administration of 3% HTS in
HTS with a prolonged duration and a high infusion rate. patients in critical circumstances. CCN
• Many factors increase the risk for venous thrombosis
with administration of 3% HTS. Examples are longer
duration of catheterization, the catheter material used,
the type of infusion, and vascular comorbidities. Vas-
cular comorbidities such as hypertension, diabetes,
dyslipidemia, and coronary artery disease may play a
major role in venous thrombosis related to HTS.
Alenazi AO, Alhalimi ZM, Almatar MH, Alhajji TA. Safety of peripheral administration of 3% hypertonic saline in critically ill patients: a literature review. Critical
Care Nurse. 2021;41(1):25-31.
www.ccnonline.org CriticalCareNurse Vol 41, No. 1, FEBRUARY 2021 31
View publication stats
You might also like
- Uterine ProlapseDocument21 pagesUterine ProlapseFau Fau DheoboNo ratings yet
- Art 40Document4 pagesArt 40Francesca BertaccaNo ratings yet
- Aching Er 2017Document10 pagesAching Er 2017Anonymous Us5v7C6QhNo ratings yet
- Hyponatremia - Management ErrorsDocument5 pagesHyponatremia - Management ErrorsharvardboyNo ratings yet
- Nephrotic Syndrome Treatment With Unani Formulation: Bushra Sabir, Iqra Hashmi and MN KhanDocument5 pagesNephrotic Syndrome Treatment With Unani Formulation: Bushra Sabir, Iqra Hashmi and MN KhanUsmleNo ratings yet
- FILE 20201125 231142 Hyponatremia A Practical ApproachDocument12 pagesFILE 20201125 231142 Hyponatremia A Practical ApproachTrọng ThuNo ratings yet
- HiponatremiaDocument14 pagesHiponatremiaEliana Lopez BaronNo ratings yet
- Drug-Induced Kidney Disease: ArticleDocument11 pagesDrug-Induced Kidney Disease: Articledwi harisNo ratings yet
- A Case Report On Thiazide Induced Hyponatremia Addressing An Underestimated ComplicationDocument4 pagesA Case Report On Thiazide Induced Hyponatremia Addressing An Underestimated ComplicationIJAR JOURNAL100% (1)
- Ijem 18 760Document12 pagesIjem 18 760HafizahLatifNo ratings yet
- Hypernatremia NEJM 2000Document8 pagesHypernatremia NEJM 2000BenjamÍn Alejandro Ruiz ManzanoNo ratings yet
- GinjalDocument11 pagesGinjalOneng IfayaniNo ratings yet
- Hyponatremia in Cirrhosis: An Update: Joseph J. Alukal, MD, Savio John, MD and Paul J. Thuluvath, MD, FRCPDocument11 pagesHyponatremia in Cirrhosis: An Update: Joseph J. Alukal, MD, Savio John, MD and Paul J. Thuluvath, MD, FRCPMuzaffar MehdiNo ratings yet
- Hyponatremia in The Neurologically Ill Patient: A ReviewDocument9 pagesHyponatremia in The Neurologically Ill Patient: A ReviewSerque777No ratings yet
- Disorders-Of-Sodium-Balance - CAMBRIDGEDocument10 pagesDisorders-Of-Sodium-Balance - CAMBRIDGEDenisa Carmen ColiofNo ratings yet
- Ebp 8 72 PDFDocument10 pagesEbp 8 72 PDFMelati HasnailNo ratings yet
- Hiponatremia JonessDocument11 pagesHiponatremia JonessEfi AdriánNo ratings yet
- Siadh!!!Document10 pagesSiadh!!!Febri Dwi HaryonoNo ratings yet
- Dysnatremia in The ICU: Milap Pokaharel and Clay A. BlockDocument13 pagesDysnatremia in The ICU: Milap Pokaharel and Clay A. BlockJonathan Gustavo MenaNo ratings yet
- Neuro4Nurses: Syndrome of Inappropriate Release of Antidiuretic HormoneDocument2 pagesNeuro4Nurses: Syndrome of Inappropriate Release of Antidiuretic HormoneM Zainun IrsyadNo ratings yet
- JPM 13 00140 v2Document17 pagesJPM 13 00140 v2YeseniaNo ratings yet
- 2016 - CM Difficulties in The Diagnosis and Management ofDocument6 pages2016 - CM Difficulties in The Diagnosis and Management ofmihaelamocanNo ratings yet
- Hyponatremia Pathophysiology Impact and ManagementDocument5 pagesHyponatremia Pathophysiology Impact and ManagementREMAN ALINGASANo ratings yet
- Hyponatremia: Annals of Internal MedicineDocument19 pagesHyponatremia: Annals of Internal MedicineAbdallahMousaNo ratings yet
- Salt and Water A Review of HypernatremiaDocument8 pagesSalt and Water A Review of HypernatremiaDaniel LozanoNo ratings yet
- Hyper Nat Remi ADocument7 pagesHyper Nat Remi ALorenzo MacoNo ratings yet
- The Intensivist's Perspective of Shock, Volume Management, and Hemodynamic MonitoringDocument16 pagesThe Intensivist's Perspective of Shock, Volume Management, and Hemodynamic MonitoringKarem YoHalyNo ratings yet
- The Clinical Management of HyponatraemiaDocument5 pagesThe Clinical Management of HyponatraemiaRenaldyRajab100% (1)
- Difficulties in The Diagnosis and Management of HyponatremiaDocument6 pagesDifficulties in The Diagnosis and Management of HyponatremiaSilvia SilvaNo ratings yet
- Wernicke Encephalopathy: EtiologyDocument6 pagesWernicke Encephalopathy: EtiologyDrhikmatullah SheraniNo ratings yet
- Articolo 9Document6 pagesArticolo 9Francesca BertaccaNo ratings yet
- Hypon EmergencyDocument8 pagesHypon Emergencylakshminivas PingaliNo ratings yet
- Tajdid Gerakan MuhammadiyahDocument17 pagesTajdid Gerakan MuhammadiyahSih AtiiNo ratings yet
- Siadh Vs CSWDocument21 pagesSiadh Vs CSWBelinda Putri agustiaNo ratings yet
- Hyponatremia 2015Document19 pagesHyponatremia 2015gastonsaloNo ratings yet
- Evaluation and Treatment of HypernatremiaDocument9 pagesEvaluation and Treatment of HypernatremiaRESIDENTES MEDICINA INTERNANo ratings yet
- 2021 HiponatremiaDocument9 pages2021 HiponatremianaanrvNo ratings yet
- Complications and Management of Hyponatremia Sterns 2016Document6 pagesComplications and Management of Hyponatremia Sterns 2016Alejandro OlaveNo ratings yet
- Demystifying HyponatremiaDocument10 pagesDemystifying HyponatremiaJavier Vivanco100% (1)
- Page 1 of 6Document6 pagesPage 1 of 6Karissa MagaruNo ratings yet
- Top 5 - Considerations For Anesthesia of A Geriatric PatientDocument5 pagesTop 5 - Considerations For Anesthesia of A Geriatric PatientMabe AguirreNo ratings yet
- Hipertension Secundaria Drogas y ToxinasDocument8 pagesHipertension Secundaria Drogas y ToxinasResti SyafitriNo ratings yet
- Androgue MadiasDocument9 pagesAndrogue MadiasFariz Eka SetiawanNo ratings yet
- Evidence-Based Hyponatremia Management in Liver DiseaseDocument21 pagesEvidence-Based Hyponatremia Management in Liver DiseaseDea Fiesta JatikusumaNo ratings yet
- Maintenance Intravenous Fluids in Acutely Ill Patients: Review ArticleDocument11 pagesMaintenance Intravenous Fluids in Acutely Ill Patients: Review ArticleyoiiiNo ratings yet
- Review Article: Ijprbs Chirag Modi, IJPRBS, 2012: Volume1 (3) : 120-132Document13 pagesReview Article: Ijprbs Chirag Modi, IJPRBS, 2012: Volume1 (3) : 120-132Uci Ramadhanty D3 2018No ratings yet
- Jurnal Penatalaksanaan EdemaDocument7 pagesJurnal Penatalaksanaan EdemaMariska Nada Debora100% (1)
- Gunst Et Al-2024-Intensive Care MedicineDocument4 pagesGunst Et Al-2024-Intensive Care Medicinejaviercharcape2No ratings yet
- Hipo e Hipernatremia en PediatriaDocument10 pagesHipo e Hipernatremia en PediatriaPao GonzalezNo ratings yet
- Sodium Disorders AAFP PDFDocument12 pagesSodium Disorders AAFP PDFIvan Tintaya UrureNo ratings yet
- Diagnosis and Management of Hyponatremia A ReviewDocument12 pagesDiagnosis and Management of Hyponatremia A ReviewCynthia Huaman C.No ratings yet
- Hyponatremia in Cirrhosis: Pathophysiology and Management: Savio John, Paul J ThuluvathDocument10 pagesHyponatremia in Cirrhosis: Pathophysiology and Management: Savio John, Paul J ThuluvathNoven Afiyata NugrahaNo ratings yet
- Mechanism, Spectrum, Consequences and Management of Hyponatremia in Tuberculous Meningitis (Document19 pagesMechanism, Spectrum, Consequences and Management of Hyponatremia in Tuberculous Meningitis (hardi adiyatmaNo ratings yet
- Approach To ShockDocument40 pagesApproach To ShockDivesh NaiduNo ratings yet
- Lec 2Document10 pagesLec 2fbbqbcht6yNo ratings yet
- HyponatremiaDocument9 pagesHyponatremiaFebe ChristiantoNo ratings yet
- A Retrospective Chart Review The Prevalence of HypDocument7 pagesA Retrospective Chart Review The Prevalence of HypKaren Mae PadillaNo ratings yet
- Secondary Hypertension: Clinical Presentation, Diagnosis, and TreatmentFrom EverandSecondary Hypertension: Clinical Presentation, Diagnosis, and TreatmentGeorge A. MansoorNo ratings yet
- The Maudsley Prescribing Guidelines in PsychiatryFrom EverandThe Maudsley Prescribing Guidelines in PsychiatryRating: 5 out of 5 stars5/5 (1)
- Management of Periodontal Abscess (2nd Edition) 2017Document43 pagesManagement of Periodontal Abscess (2nd Edition) 2017Omeerul RafieNo ratings yet
- Vesicaria Communis John Henry Clarke: 21 Homeopathic Medicines Dr. Shah FaisalDocument3 pagesVesicaria Communis John Henry Clarke: 21 Homeopathic Medicines Dr. Shah FaisalShah FaisalNo ratings yet
- Therapeutic Fasting Book7.9Document224 pagesTherapeutic Fasting Book7.9Mu Sang Sa100% (6)
- Online Term Plan: Shriram LifeDocument10 pagesOnline Term Plan: Shriram LifeSivaramakrishna DavuluriNo ratings yet
- Transgender Health Survey 2014 - 02182014Document11 pagesTransgender Health Survey 2014 - 02182014Sana KhanNo ratings yet
- Atorvastatin Export Market AnalysisDocument19 pagesAtorvastatin Export Market AnalysisMr. Sunil KumarNo ratings yet
- Hiperhidrosis Generalizada y Sudoracion NocturnaDocument13 pagesHiperhidrosis Generalizada y Sudoracion NocturnaVar AndaNo ratings yet
- Laporan JARINGAN DAN JEJARING BULAN AGUSTUS 2019Document27 pagesLaporan JARINGAN DAN JEJARING BULAN AGUSTUS 2019Viera ThenuNo ratings yet
- Clinical Dermatology - 4th EdDocument170 pagesClinical Dermatology - 4th EdKaptan Tsubasa FanNo ratings yet
- SeminarskiDocument17 pagesSeminarskiKadric Nagla UtokaNo ratings yet
- Paskariatne Probo - Simple Approach To Peri Operative HypertensionDocument42 pagesPaskariatne Probo - Simple Approach To Peri Operative HypertensionCupit NubillisNo ratings yet
- Kode Kombinasi & Kode GandaDocument15 pagesKode Kombinasi & Kode GandaJuwitahasugianNo ratings yet
- Female Gestational Diabetes Mellitus 34 Years Old Diet (High Carbohydrate) Sedentary Lifestyle Obesity StressDocument4 pagesFemale Gestational Diabetes Mellitus 34 Years Old Diet (High Carbohydrate) Sedentary Lifestyle Obesity StressVictoria Castillo TamayoNo ratings yet
- CerebrolysinDocument1 pageCerebrolysineiad-mahmoudNo ratings yet
- Hydrocephalus: Common Names For DisorderDocument5 pagesHydrocephalus: Common Names For DisorderGita Herminda PutriNo ratings yet
- Mindanao State University - Iligan Institute of Technology Student: - SectionDocument2 pagesMindanao State University - Iligan Institute of Technology Student: - SectionJohn Pearl FernandezNo ratings yet
- Eaton Lambert SyndromeDocument8 pagesEaton Lambert Syndromeutami ridaNo ratings yet
- Neuro OphthalmologyDocument702 pagesNeuro OphthalmologyFauziah HafshohNo ratings yet
- Bartter SyndromeDocument3 pagesBartter SyndromeEnny Andriani100% (1)
- An Analysis of Notebook by Nicholas SparksDocument2 pagesAn Analysis of Notebook by Nicholas SparksMariane ManaliliNo ratings yet
- DermatologyDocument30 pagesDermatologyCarlos HernándezNo ratings yet
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument4 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses CentralNo ratings yet
- MCQsDocument13 pagesMCQsVinay BhatNo ratings yet
- How To Examine A Patient - A Pocket Guide To Students of Medicine (3rd Ed) (Gnv64)Document464 pagesHow To Examine A Patient - A Pocket Guide To Students of Medicine (3rd Ed) (Gnv64)Bogdan Lina100% (3)
- MastopatiDocument3 pagesMastopatiMerina RachmadinaNo ratings yet
- ImpetigoDocument13 pagesImpetigoTasya SyafhiraNo ratings yet
- Urinary Tract Infection in Children Diagnosis, Treatment, Imaging - Comparison of Current Guidelines 10.1016@j.jpurol.2017.07.018Document7 pagesUrinary Tract Infection in Children Diagnosis, Treatment, Imaging - Comparison of Current Guidelines 10.1016@j.jpurol.2017.07.018Gyanendra SharmaNo ratings yet
- List Summary of Sanjay Sharma MRCP Part 2Document22 pagesList Summary of Sanjay Sharma MRCP Part 2Ruku KhanNo ratings yet
- Renal Function Tests 1 PDFDocument56 pagesRenal Function Tests 1 PDFCharles Bryahn OkoboiNo ratings yet