Professional Documents
Culture Documents
Lansing 05 SPECT
Lansing 05 SPECT
Uploaded by
Felipe Orejuela SotoCopyright:
Available Formats
You might also like
- Risk Assessment - Cable Pulling Laying, Glanding and Termination From RT Bay Outdoor Enclosure To RT Control BuildingDocument14 pagesRisk Assessment - Cable Pulling Laying, Glanding and Termination From RT Bay Outdoor Enclosure To RT Control Buildingnsadnan91% (82)
- VAC Swachh Bharat - 230612 - 155724Document14 pagesVAC Swachh Bharat - 230612 - 155724Tera Kal92% (13)
- User Manual ECG EDAN SE-3Document104 pagesUser Manual ECG EDAN SE-3Andreé Montúfar100% (1)
- Planning Fixed Partial Dentures For Severely Misaligned AbutmentsDocument7 pagesPlanning Fixed Partial Dentures For Severely Misaligned AbutmentsAntonny VasquezNo ratings yet
- Art Therapy Masks Reflect Emotional Changes in MilDocument13 pagesArt Therapy Masks Reflect Emotional Changes in MilRawan SalehNo ratings yet
- Michael Esterman2020Document13 pagesMichael Esterman2020Raul Morales VillegasNo ratings yet
- HHS Public Access: Longitudinal Changes in Brain Function Associated With Symptom Improvement in Youth With PTSDDocument21 pagesHHS Public Access: Longitudinal Changes in Brain Function Associated With Symptom Improvement in Youth With PTSDLeonardo PunshonNo ratings yet
- Psychotherapies For Complex Trauma A Combination Between Emdr and MindfulnessDocument1 pagePsychotherapies For Complex Trauma A Combination Between Emdr and MindfulnessRUBY SANTAMARIA FLOREZNo ratings yet
- Bradley Et Al. (2006)Document14 pagesBradley Et Al. (2006)jehonol883No ratings yet
- Change in Negative Cognitions Associated With PTSD Predicts Symptom Reduction in Prolonged ExposureDocument9 pagesChange in Negative Cognitions Associated With PTSD Predicts Symptom Reduction in Prolonged Exposureericaduran4824No ratings yet
- Emdr 2002Document14 pagesEmdr 2002jivinaNo ratings yet
- Higher Cortisol Levels Following Exposur PDFDocument34 pagesHigher Cortisol Levels Following Exposur PDFIván CornuNo ratings yet
- Neuroimage: Clinical: SciencedirectDocument9 pagesNeuroimage: Clinical: SciencedirectMoumi PanditNo ratings yet
- 1 s2.0 S0890856714004079 MainDocument10 pages1 s2.0 S0890856714004079 MainPar DoNo ratings yet
- Neuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderDocument2 pagesNeuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderClaudio PeñafielNo ratings yet
- Rehabilitas Cedera OtakDocument2 pagesRehabilitas Cedera Otakbotet_2306No ratings yet
- Jkms 33 E306Document6 pagesJkms 33 E306Mer P HNo ratings yet
- Traumatic AmnesiaDocument6 pagesTraumatic AmnesiakatiaNo ratings yet
- Which Clinical Factors Delay A Proper Treatment in Panic Di - 2022 - NeurosciencDocument2 pagesWhich Clinical Factors Delay A Proper Treatment in Panic Di - 2022 - NeurosciencloloasbNo ratings yet
- JTS 34 851Document13 pagesJTS 34 851MARIA FERNANDA OLIVEIRA SOARESNo ratings yet
- Prazosin TX PTSDMetaanalysis 2020Document8 pagesPrazosin TX PTSDMetaanalysis 2020Dr. José Juan PeralesNo ratings yet
- Pubs Shin 2010 Neural CorDocument8 pagesPubs Shin 2010 Neural CorTJSNo ratings yet
- 1 s2.0 S0028393217302403 MainDocument8 pages1 s2.0 S0028393217302403 MaincursosNo ratings yet
- 1 s2.0 S105381192100519X MainDocument13 pages1 s2.0 S105381192100519X MainSantai JakNo ratings yet
- A Paradigm Shift in Trauma Treatment - Converging Evidence For A Novel AdaptationDocument3 pagesA Paradigm Shift in Trauma Treatment - Converging Evidence For A Novel AdaptationTeresa GMNo ratings yet
- From Pro-Inflammatory Molecules To The Brain's Resting-State Connectivity The Future of Clinical Diagnosis of DepressionDocument36 pagesFrom Pro-Inflammatory Molecules To The Brain's Resting-State Connectivity The Future of Clinical Diagnosis of DepressiondgavrileNo ratings yet
- Calancie AnnNYAcadSci 2018Document19 pagesCalancie AnnNYAcadSci 2018Barbara Kowalska MarquesNo ratings yet
- Brain Circuit Dysfunction in Post - Traumatic Stress Disorder: From Mouse To Man - Robert J. FensterDocument17 pagesBrain Circuit Dysfunction in Post - Traumatic Stress Disorder: From Mouse To Man - Robert J. FensterAlvaro Arboledas LoriteNo ratings yet
- Artikel InternasionalDocument15 pagesArtikel InternasionalFitriatul MunawarohNo ratings yet
- Advancing Preclinical Chronic Stress Models To Promote Therapeutic Discovery For Human Stress DisordersDocument12 pagesAdvancing Preclinical Chronic Stress Models To Promote Therapeutic Discovery For Human Stress DisordersMoo Gee100% (1)
- tmp6BD2 TMPDocument1 pagetmp6BD2 TMPFrontiersNo ratings yet
- Brain-Based Biotypes of Psychiatric Vulnerability in The Acute Aftermath of TraumaDocument13 pagesBrain-Based Biotypes of Psychiatric Vulnerability in The Acute Aftermath of TraumaRicardo EscNo ratings yet
- Effect of Group V Individual Cognitive Processing Therapy in Active-Duty Military Seeking Treatment For Posttraumatic Stress DisorderDocument9 pagesEffect of Group V Individual Cognitive Processing Therapy in Active-Duty Military Seeking Treatment For Posttraumatic Stress DisorderBrandon Gray100% (1)
- 1 s2.0 S2213158219303511 MainDocument8 pages1 s2.0 S2213158219303511 MainGilbert SihombingNo ratings yet
- 1 s2.0 S0005791616301343 MainDocument7 pages1 s2.0 S0005791616301343 MainTulaNo ratings yet
- Cognitive-Behavior Therapy Vs Exposure Therapy in The Treatment of PTSD in RefugeesDocument15 pagesCognitive-Behavior Therapy Vs Exposure Therapy in The Treatment of PTSD in RefugeesAna CristeaNo ratings yet
- Euenc JdeeDocument65 pagesEuenc JdeeGustavoNo ratings yet
- 2022, The Efficacy of TMS and Negative Symptoms of SchizophreniaDocument12 pages2022, The Efficacy of TMS and Negative Symptoms of Schizophreniafelix08121992No ratings yet
- Neuromodulation in Response To Electroconvulsive Therapy Inschizophrenia and Major DepressionDocument8 pagesNeuromodulation in Response To Electroconvulsive Therapy Inschizophrenia and Major DepressionPablo RamirezNo ratings yet
- Neural Correlates of Recall of Life Events in Conversion DisorderDocument9 pagesNeural Correlates of Recall of Life Events in Conversion DisorderMarcus Vinicius AlvesNo ratings yet
- Sequential Fear Generalization and Network Connectivity in Trauma Exposed Humans With and Without PsychopathologyDocument9 pagesSequential Fear Generalization and Network Connectivity in Trauma Exposed Humans With and Without Psychopathologyheidarihamed4No ratings yet
- 10 1192@bjp 2020 158Document7 pages10 1192@bjp 2020 158Olga MichailidouNo ratings yet
- Cognitive Outcomes in Patients With Major Depression Treated With Electroconvulsive TherapyDocument8 pagesCognitive Outcomes in Patients With Major Depression Treated With Electroconvulsive TherapyPsiholog Monica StănescuNo ratings yet
- Untreated Initial Psychosis: Relation To Cognitive Deficits and Brain Morphology in First-Episode SchizophreniaDocument7 pagesUntreated Initial Psychosis: Relation To Cognitive Deficits and Brain Morphology in First-Episode SchizophreniaelvinegunawanNo ratings yet
- Ect Skizo ResistenDocument28 pagesEct Skizo ResistenZulvikar UmasangadjiNo ratings yet
- (Intro - General ImRs) Arntz-2012-Imagery-Rescripting-As-A-Therapeutic-Technique-Review-Of-Clinical-Trials-Basic-Studies-And-Research-AgendaDocument19 pages(Intro - General ImRs) Arntz-2012-Imagery-Rescripting-As-A-Therapeutic-Technique-Review-Of-Clinical-Trials-Basic-Studies-And-Research-AgendaDolunay UludağNo ratings yet
- Linking Molecules To Mood: New Insight Into The Biology of DepressionDocument16 pagesLinking Molecules To Mood: New Insight Into The Biology of Depressiondudul pudlianNo ratings yet
- Biological Psychology: ArticleinfoDocument15 pagesBiological Psychology: ArticleinfoManuela SilvaNo ratings yet
- TMP ED34Document9 pagesTMP ED34FrontiersNo ratings yet
- Yang 2021Document10 pagesYang 2021Andrea Galindo EscobosaNo ratings yet
- Olive 2018 Superior Colliculus Resting State NDocument12 pagesOlive 2018 Superior Colliculus Resting State Nbenoit berthailNo ratings yet
- Fpsyg 08 01750Document10 pagesFpsyg 08 01750Nerea F GNo ratings yet
- Electroconvulsive TherapyDocument10 pagesElectroconvulsive TherapyYasinNo ratings yet
- Richardson 2018Document7 pagesRichardson 2018Maria Von ShaftNo ratings yet
- King 2016Document13 pagesKing 2016Realidades InfinitasNo ratings yet
- Amphetamine-Induced Striatal Dopamine Release in SchizotypalDocument11 pagesAmphetamine-Induced Striatal Dopamine Release in Schizotypaleva para eva love is loveNo ratings yet
- Raboni Sleep + Emdr Nyas 06Document6 pagesRaboni Sleep + Emdr Nyas 06Felipe Orejuela SotoNo ratings yet
- Irritability in Pre-Clinical Huntington's Disease: NeuropsychologiaDocument9 pagesIrritability in Pre-Clinical Huntington's Disease: NeuropsychologiaJose Bryan GonzalezNo ratings yet
- Auricular Causative Diagnosis-Finding The Roots of Diseases: A Study of Clinical CasesDocument11 pagesAuricular Causative Diagnosis-Finding The Roots of Diseases: A Study of Clinical Casesyan92120No ratings yet
- Psych Trans PDFDocument21 pagesPsych Trans PDFWinnie AriolaNo ratings yet
- Artifact 15Document16 pagesArtifact 15api-348971279No ratings yet
- Predictors of Poor Treatment Response ToDocument13 pagesPredictors of Poor Treatment Response ToMaite Novo del valleNo ratings yet
- 16546-Article Text-64861-1-10-20160825Document11 pages16546-Article Text-64861-1-10-20160825THIARE GALDAMES HERNANDEZNo ratings yet
- Fundamentals and Clinics of Deep Brain Stimulation: An Interdisciplinary ApproachFrom EverandFundamentals and Clinics of Deep Brain Stimulation: An Interdisciplinary ApproachYasin TemelNo ratings yet
- Jacobson y Christensen (1996) Acceptance and Change in Couple TherapyDocument308 pagesJacobson y Christensen (1996) Acceptance and Change in Couple TherapyFelipe Orejuela SotoNo ratings yet
- Sustainable Practice ChecklistDocument6 pagesSustainable Practice ChecklistFelipe Orejuela SotoNo ratings yet
- Hypothetical ThinkingDocument215 pagesHypothetical ThinkingFelipe Orejuela SotoNo ratings yet
- Diagnosis, Conceptualization and Treatment Planning For AdultsDocument350 pagesDiagnosis, Conceptualization and Treatment Planning For AdultsFelipe Orejuela SotoNo ratings yet
- Sectores Pag 29Document47 pagesSectores Pag 29cghortaNo ratings yet
- 11 cсынып емтихан сурактарыDocument6 pages11 cсынып емтихан сурактарыakzharNo ratings yet
- Linagliptin Drug MonographDocument7 pagesLinagliptin Drug MonographNearMelowNo ratings yet
- Stein Sept 29 LetterDocument2 pagesStein Sept 29 LetterMitchell BlackNo ratings yet
- GC 4Document1 pageGC 4ais82603No ratings yet
- EXT - 230914 - 0850 - MS32 - V001 - BMW15.10 - SYN - QA - MS - 0032 - 01-ESD CoatingDocument13 pagesEXT - 230914 - 0850 - MS32 - V001 - BMW15.10 - SYN - QA - MS - 0032 - 01-ESD CoatingТамер БакировNo ratings yet
- Manuscript 2 FinalDocument60 pagesManuscript 2 FinalKape Ka BaNo ratings yet
- Pulsed Electro Magnetic Energy (PEME)Document9 pagesPulsed Electro Magnetic Energy (PEME)NATARAJAN KAVITHANo ratings yet
- Media Bulletin 11.07.2020 27 Pages English 491 KBDocument27 pagesMedia Bulletin 11.07.2020 27 Pages English 491 KBKathirasan RamalingamNo ratings yet
- Standards For Competence For Registered MidwivesDocument14 pagesStandards For Competence For Registered MidwivescarNo ratings yet
- Sanet Me0803120575Document169 pagesSanet Me0803120575parallax1957No ratings yet
- Healthy Eating Patterns and Risk of Total and Cause-Specific Mortality - JAMA Intern MedDocument12 pagesHealthy Eating Patterns and Risk of Total and Cause-Specific Mortality - JAMA Intern MedSamitti ChotsriluechaNo ratings yet
- Weekly Current Affairs 8-Jan-2024 To 14-Jan-2024Document25 pagesWeekly Current Affairs 8-Jan-2024 To 14-Jan-2024Vandana VermaNo ratings yet
- Arc Flash Safety BulletinDocument4 pagesArc Flash Safety BulletinVictor Manuel Flores ZuñigaNo ratings yet
- Articles Rgarding Importantce of Minerals and Effects of Food DepletionDocument16 pagesArticles Rgarding Importantce of Minerals and Effects of Food Depletionapi-3827527No ratings yet
- Clinical-Trial AIIADocument6 pagesClinical-Trial AIIAkaushal ahirwarNo ratings yet
- QC How To Make A Good Method StatementDocument3 pagesQC How To Make A Good Method StatementRsjBugtongNo ratings yet
- Clinical Nursing Judgement PaperDocument5 pagesClinical Nursing Judgement Paperapi-663930784No ratings yet
- 7 Ways To Treat A Fever Naturally - Reader ModeDocument14 pages7 Ways To Treat A Fever Naturally - Reader Modeedward nodzoNo ratings yet
- Report No. 11 of 2023 - PA On PMJAY - English PDF A 064d22bab2b83b5.38721048Document168 pagesReport No. 11 of 2023 - PA On PMJAY - English PDF A 064d22bab2b83b5.38721048arish.khanNo ratings yet
- 3 23 2005 Aviation EnglishDocument14 pages3 23 2005 Aviation EnglishSky LukeNo ratings yet
- Halime Fetahu Osmani - The Structure of KinesiologyDocument6 pagesHalime Fetahu Osmani - The Structure of Kinesiologynuno costeNo ratings yet
- Dialogo de Ingles Paciente A OdontologoDocument4 pagesDialogo de Ingles Paciente A OdontologoKimberly Pinzon0% (1)
- EFfCI GMP Position Paper Certificates of AnalysisDocument5 pagesEFfCI GMP Position Paper Certificates of AnalysisAladdin MobarakNo ratings yet
- Mackey 2016 CVDocument8 pagesMackey 2016 CVapi-304462343No ratings yet
- F2 Mid-Year Exam Section BDocument3 pagesF2 Mid-Year Exam Section BAnne Marian Anak JOSEPHNo ratings yet
Lansing 05 SPECT
Lansing 05 SPECT
Uploaded by
Felipe Orejuela SotoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lansing 05 SPECT
Lansing 05 SPECT
Uploaded by
Felipe Orejuela SotoCopyright:
Available Formats
High–Resolution Brain
SPECT Imaging and
Eye Movement
Desensitization and
Reprocessing in Police
Officers With PTSD
Karen Lansing, M.F.T, B.C.E.T.S.
Daniel G. Amen, M.D.
Chris Hanks, Ph.D.
Lisa Rudy, B.A.
Eye movement desensitization and reprocessing
(EMDR) has been shown to be an effective treat- I ndividuals in law enforcement are at a much greater
risk of experiencing traumatic events than are average
citizens.1 Over the course of their careers, many police
ment for posttraumatic stress disorder (PTSD). In
officers experience traumatic events that result in post-
this study, the authors evaluated the effectiveness
traumatic stress disorder (PTSD), or they endure trau-
and physiological effects of EMDR in police offi-
matic experiences that accumulate and manifest in
cers involved with on-duty shootings and who delayed-onset PTSD upon reaching some threshold. Our
had PTSD. Six police officers involved with on- clinical experience finds that, without complete recov-
duty shootings and subsequent delayed-onset ery, these officers experience diminished ability to man-
PTSD were evaluated with standard measures, age the chronic stressors and dangers inherent in their
the Posttraumatic Stress Diagnostic Scale, and jobs.2
high-resolution brain single photon emission com- Imaging studies have identified several brain regions
puted tomography (SPECT) imaging before and implicated in PTSD. In case-controlled studies using sin-
after treatment. All police officers showed clinical gle photon emission computed tomography (SPECT),
improvement and marked reductions in the Post- Shin et al.3 and Sachinvala et al.4 found increased activ-
traumatic Stress Diagnostic Scale Score (PDS). In ity in the limbic regions, particularly in the posterior
addition, there were decreases in the left and right cingulate gyrus, amygdaloid complex, and right basal
ganglia. Also using SPECT, Zubieta et al.5 found signifi-
occipital lobe, left parietal lobe, and right precen-
cant increases in the blood flow to the medial prefrontal
tral frontal lobe as well as significant increased
cortex in PTSD patients but not in the comparison
perfusion in the left inferior frontal gyrus. In our groups, which correlated at trend levels with psycho-
study EMDR was an effective treatment for physical measures of stress response. Activation studies
PTSD in this police officer group, showing both conducted by Berthier et al.,6 using SPECT, Benkelfat et
clinical and brain imaging changes. al.,7 using positron emission tomography (PET), and
(The Journal of Neuropsychiatry and Clinical
Neurosciences 2005; 17:526–532) Received March 23, 2004; revised June 17, 2004; accepted June 24, 2004.
From the Amen Clinic, Department of Research and Information Sys-
tems, Newport Beach, California. Address correspondence to Dr.
Hanks, chanks@amenclinic.com (E-mail).
Copyright 䉷 2005 American Psychiatric Publishing, Inc.
526 http://neuro.psychiatryonline.org J Neuropsychiatry Clin Neurosci 17:4, Fall 2005
LANSING et al.
Liberzon et al.,8 using SPECT, each found PTSD to be that a third-party clinician had to confirm clinical di-
associated with increased paralimbic activity. Using agnoses of PTSD using DSM–IV criteria. Third, the score
functional magnetic resonance imaging (fMRI), Rauch on the Foa Posttraumatic Stress Diagnostic Scale (PDS),
et al.9 found PTSD patients to exhibit exaggerated amyg- a 49-item self-report instrument designed to aid in the
dala responses to masked-fearful versus masked-happy detection and diagnosis of PTSD,23 must be in the mod-
faces. erate to severe range (scores greater than 21 on a scale
A number of studies have shown eye movement de- of 0–51). Because the study included pharmacologically
sensitization and reprocessing (EMDR) therapy to be an sensitive functional brain imaging, subjects who began
effective treatment for PTSD.10–18 Additionally, brain the study on medications were required to remain on
SPECT imaging has been used to show before- and after- the same dosage throughout. Five of the six subjects
treatment effects. In a case study design, Levin et al. were on no medications, and one remained on an anti-
found activations in the anterior cingulate gyrus and left depressant only (Celexa 20 mg.). The mean age of sub-
frontal lobe in four of six patients after three sessions of jects was 38.6 years (SD⳱7.69 years; minimum⳱31,
EMDR.19 Using high-resolution brain SPECT imaging to maximum⳱50), and the mean level of education was 2
examine the effects of EMDR on both clinical outcomes years of college. Four of six subjects had PTSD symp-
and regional cerebral blood flow in six police officers toms that emerged between 42 and 63 months after they
with delayed-onset PTSD, the research presented in this were involved in the shooting. Two subjects experienced
study goes beyond the case study design. a shooting within 3 months of the onset of PTSD. A
The precise causes of EMDR’s effectiveness remain range of symptom severity was sought across our study
unknown. A number of studies have found it to be the population to increase the generalizability of our results.
therapeutic equivalent of exposure therapy,20,21 while
other studies equate its effects to cognitive behavior Treatment Protocol
therapy.22 However, Levin et al. argue that therapeutic Upon seeking treatment from a therapist contracted
components specific to EMDR activate a cognitive net- with a police department, patients gave a personal his-
work that helps patients differentiate real threats from tory and submitted to an unstructured clinical diagnos-
imagined ones.19 We hypothesized that subjects would tic interview to establish a diagnosis of PTSD; likewise,
experience significantly improved clinical outcomes and they completed the PDS scale at this time. Potential sub-
that these improvements would be reflected in some jects who met the preliminary criteria of a clinical PTSD
functional pattern of activity in their respective post- diagnosis and who had a PDS score greater than 21 were
EMDR brain SPECT scans. given the opportunity to participate in the study, where-
upon they were given specific details and signed in-
formed consent. All interviews were conducted by the
METHOD same therapist, who is level II certified by the EMDR
International Association.
The treatment format for all subjects proceeded in the
Subject Selection following three phases. Phase 1 was clinical, wherein
All subjects in this study sought treatment for duty- histories were taken for each subject. Subjects were
induced PTSD (N⳱6). Five subjects were right-handed, taught coping and “containment” techniques, how to
and one was left-handed. Three subjects had been in talk identify and develop support networks,24 and how to
therapy for duty-induced trauma prior to the study. log their trauma-related memories—a necessary precon-
Among these three, two presented with severe PTSD dition for EMDR. At the end of Phase 1 we acquired the
symptoms and one with moderate symptoms. The re- first (pre-EMDR) brain SPECT scans.
maining 3 subjects had never been in therapy for duty- In Phase 2, subjects began EMDR. For all EMDR ses-
induced trauma. Among them, two presented with sions in this study, we used a TheraTapper, which gave
moderate symptoms and one with severe symptoms. bilateral stimulation in the subjects’ palms and fingers,
There were three criteria for inclusion. First, because of thus allowing them to reexperience traumatic scenes
the high incidence of PTSD among officers involved in with their eyes closed. Eye movement has been shown
shootings,1 only subjects who had fired a weapon in the to be effective among law enforcement subjects.18 In our
line of duty were included. A second requirement was clinical experience, however, police officers have com-
J Neuropsychiatry Clin Neurosci 17:4, Fall 2005 http://neuro.psychiatryonline.org 527
POLICE OFFICERS WITH PTSD
plained about being distracted by the eye movement ele- butterfly. Subjects remained quiet for several minutes
ment in EMDR more than other patient populations. We with open eyes to allow acclimation to their environ-
thus chose to use an eyes-closed mode of EMDR to re- ment. Images were acquired while subjects performed a
duce the possibility of distraction. Although there are clinically standardized concentration task, the Connors
no published data on the efficacy of bilateral stimulation Continuous Performance Test (CPT), a 15-minute com-
in lieu of eye movements, this mode of EMDR has been puterized test of attention. We chose to scan the police
used clinically for over a decade and is approved by the officers during a concentration task (as opposed to other
EMDR International Association.24 In all cases it was ob- studies that scanned subjects while reexperiencing the
served that unsolicited REM-like activity occurred. traumatic event) to more accurately simulate their day-
EMDR sessions typically ran two to 3 hours in length to-day functioning. CPT scores were not recorded.
and were conducted three to 4 weeks apart, resulting in For both the pre- and post-EMDR brain images, sub-
a great deal of mental and emotional fatigue among sub- jects began the Connors CPT, and at 3 minutes they were
jects. Because of the nature of the subjects’ jobs in law injected with a 3 ml bolus containing 22 mCi of tech-
enforcement and their associated risks, the frequency netium technetium-99m exametazime (commercially
and duration of sessions in this study were dictated by available as Ceretec威). Tomographic brain imaging was
each subject’s individual recuperation time. The mean then performed approximately 45 minutes later using a
number of EMDR sessions was 3.83 (SD⳱2.41), and the high-resolution Picker Prism 3000 gamma camera with
mean number of EMDR hours was 10.25 (SD 4.84). fan beam collimators. Data were acquired in 128-by-128
Before the final (post-EMDR) PDS scores and SPECT matrices. One hundred twenty images with 3⬚ of sepa-
images were acquired, a minimum of 3 weeks was al- ration spanning 360⬚ rotation were obtained. The data
lowed to lapse after the final EMDR session for two were prefiltered using a low-pass filter with a high cut-
reasons. First, it was estimated that this would allow off. Attenuation correction was performed using linear
the brain to recover from any EMDR-induced mental methods. Coronal, sagittal, and transaxial tomographs
fatigue. Second, it would allow some period for sub- were parallel to the orbitomeatal line.
jects’ brain function to become regularized and also for
any short-term functional effects to dissipate. Phase 3 Statistical Analyses
constituted a “reconciliation phase” of treatment, fo- Statistical analyses of pre- and post- SPECT images were
cusing on the rescripting of relational patterns that performed using Statistical Parametric Mapping ’99
might not have been corrected once subjects became (SPM99).25 SPM99 performs voxel-by-voxel analyses us-
detraumatized. ing general linear methods, and it requires that all
SPECT scans be spatially preprocessed. Thus each pre-
Study Design, Data Collection, and Statistical Analysis EMDR scan was coregistered to its respective post-
Two sets of data were collected for analysis in this study: EMDR scan using the realign function, which created a
brain SPECT images and PDS scale measurements. Scan 12-parameter realignment matrix for each of 12 pairs of
data for each of 6 subjects were first collected immedi- pre- and post-EMDR scans. Each pair was then visually
ately prior to Phase 2 treatment, and again 3 weeks after inspected for coregistration errors. All 12 scans from
the completion of Phase 2, for a total of 12 scans (six pre- both conditions were then, using the Talairach map,26
and six post-EMDR). PDS scores were acquired prior to normalized to a single standardized anatomical space
Phase 1, and again 3 weeks after the completion of Phase using sinc interpolation and an 8-by-8-by-8 voxel kernel.
2, for a total of 12 PDS scores (six pre- and six post- Finally, all images were smoothed to 7 mm3 using a
EMDR). Phase 3 began after the final PDS and SPECT Gaussian kernel. Smoothing the data results in voxel
were performed. The study design was a simple single- clusters that better conform to the requirements of Gaus-
group pre-to-posttest comparison using t tests for both sian field theory, which allows us to make more reason-
sets of data, as described below. able statistical inferences about our data.27 Smoothing
also tends to minimize smaller, more statistically aber-
Brain SPECT Protocol and Image Acquisition rant results.
The brain SPECT studies were performed in the follow- We performed a global paired t test, which tests the
ing manner. Each subject was placed in a dimly lit, quiet hypotheses,
room. Intravenous access was obtained via small-gauge H1: l ⬆ 0; H0: l ⳱ 0,
528 http://neuro.psychiatryonline.org J Neuropsychiatry Clin Neurosci 17:4, Fall 2005
LANSING et al.
at each voxel, where l is the mean difference in the fre- comparisons unless otherwise noted. These results are
quency of photon emission from t1 to t2 . Global per- summarized in Table 1.
fusion values were proportionally rescaled to 50/ml/dl/ There were significant deactivations in the right thal-
min. Threshold masking was used to ensure that only amus, the precentral gyrus of the right frontal lobe, and
voxels that represent brain activity were included in the the postcentral gyrus of the left parietal lobe, and there
analyses, and the threshold for inclusion was set at 80% were bilateral deactivations in the occipital lobes (see
of the mean global voxel value. The initial significance Figure 1). Likewise, there were significant activations in
threshold was set at p⳱⬍.001. the left frontal lobe, notably in the middle frontal, infe-
Statistical comparisons were made of pre- and post- rior frontal, and superior frontal gyri. Most notable is
EMDR PDS scores using pairwise t tests in SAS v8.2. the 320-voxel cluster activation in the inferior frontal gy-
rus (p ⳱0.001, corrected for multiple comparisons).
(Figure 1.)
RESULTS
On the Foa PDS scale, our clinical outcome measure, DISCUSSION
there was a highly significant decrease from pre- to post-
EMDR treatment scores, falling from a pre-EMDR mean The significant decreases in PDS scores were consistent
of 43.2 ([SD⳱12.3] minimum⳱14, maximum⳱47— with the clinical improvement seen in the police officers
severe PTSD range) to a post- mean of 5.2 ([SD⳱1.9] and the reported effectiveness of EMDR in PTSD. Like-
minimum⳱1, maximum⳱6—mild to no PTSD symp- wise, our SPM analyses found significant functional dif-
toms). None of the six subjects had a post-EMDR PDS ferences in brain activity from pre- to post-EMDR im-
score above 6, indicating nearly complete alleviation of aging. EMDR and the procedures involved with this
clinical PTSD symptoms. A standard pooled t test re- treatment had both a positive clinical effect and a pos-
quires that the variance of the two groups being com- sible role in changing brain function.
pared be distributed similarly. As the distribution of Prior research has found activations in PTSD subjects
scores was significantly different from pre- to post- in the posterior3,4 and anterior cingulate gyrus5,6 and the
EMDR (folded F⳱40.21, p⳱0.001), a Satterthwaite ad- amygdala;3–6,8 thus, we might have expected post-
justment was made for comparing groups with unequal EMDR deactivations in these areas. Instead we saw de-
variances (t⳱ ⳮ5.34, p⳱0.003). activations in three areas found by Gundel et al. to be
Our SPM analysis yielded five significant deactiva- associated with image-induced grief 28: the left cuneus,
tions and three activations at the voxel level. All results which has been suggested to process motor imagery;29,30
assume a height threshold uncorrected for multiple the right lingual gyrus, which has been implicated in
TABLE 1. Summary of SPM Results: Voxel-Level Gray Matter Activations and Deactivations from Pre- to Post-EMDR (Nⴔ6)
Brain Region Talairach Coordinates (x, y, z) Valence t-value
Occipital lobe
Right lingual gyrus (BA 18) 18, ⳮ80, ⳮ12 Deactivation 13.84*
Left cuneus/precuneus 0, ⳮ74, 30 Deactivation 6.68*
Sub-lobar thalamus
Right pulvinar 22, ⳮ28, 10 Deactivation 13.14*
Frontal lobe
Right precentral gyrus (BA 4) 52, ⳮ12, 42 Deactivation 10.23*
Left middle frontal gyrus (BA 11) ⳮ44, 36, ⳮ12 Activation 6.81*
Left inferior frontal gyrus (BA 44) ⳮ48, 48, 0 Activation 7.92*
Left superior frontal gyrus (BA 8) ⳮ24, 42, 42 Activation 9.55*
Left medial ventral frontal gyrus (BA 9) ⳮ18, 36, 20 Activation 5.77**
Parietal lobe
Left postcentral gyrus (BA 40) ⳮ52, ⳮ28, 50 Deactivation 7.68*
*Significant at p⳱⬍0.001, uncorrected for multiple comparisons
** Significant at p⳱⬍0.005, uncorrected for multiple comparisons
SPM⳱statistical parametric mapping
BA⳱Brodmann’s area
J Neuropsychiatry Clin Neurosci 17:4, Fall 2005 http://neuro.psychiatryonline.org 529
POLICE OFFICERS WITH PTSD
processing motor imagery30 and in judging emotionally we saw no significant activity at p⳱0.001, we did see
evocative stimuli;31 and Brodmann’s area (BA) 4 of the MVPFC activation at p⳱0.005 (BA 9, Talairach coordi-
right precentral gyrus. Deactivations in these areas may nates x⳱–18, y⳱36, z⳱20). This finding may indicate
be relieving trauma-induced grief. that EMDR brings both modes of cognition to bear on
We saw further deactivations in the left parietal lobe PTSD recovery.
at BA 40, known to be an association area, and in the There are two significant limitations to this study.
right pulvinar. Although the primary function of the First, our sample contained a left-handed subject, a con-
pulvinar is unclear, it is thought to be an associative sequence of the nature by which our sample was re-
thalamic nucleus that helps regulate cortical circuitry.32 cruited. Second, our design was a nonexperimental pre-
The combination of these two deactivations along with test/posttest comparison. Without a control group this
those implicated in grief may constitute the diminution study was subject to validity threats such as history and
of a network of traumatic memories. maturation effects, and thus we cannot make scientific
In addition to right hemisphere decreases, our SPM claims about the effects of EMDR on clinical outcomes.
analyses showed three left prefrontal cortical activa- Instead we must extrapolate based on the clinical suc-
tions, in Brodmann areas 8, 11, and 44. Recent research cess of prior experimental studies,13–19 and we must fur-
has found PTSD subjects to have low activity in BAs 8 ther extend this reasoning to the differences we found
and 44,33,34 and thus significant activations in these areas in post-EMDR brain function. Additional imaging stud-
appear to be directly correlated with subjects’ improved ies using more robust experimental designs are needed
PDS scores. Further studies have found that depression to confirm these results.
is linked to low activity in the dorsolateral prefrontal In summary, our findings of the specific increases and
cortex (DLPFC)39–40 and that increased activity in this decreases seen on SPECT are consistent with many eti-
area is associated with improvements in clinical out- ological improvements, including depression41–43 and
comes.38 Our finding of activation in BA 11 of the general affective disorders.44–48 These analyses find
DLPFC is consistent with this research and with the re- EMDR to be associated with significant changes in brain
ported effects of EMDR on symptoms of depression.19 function as measured by SPECT, and that the emergent
Many studies having to do with both mood and cog- post-EMDR pattern of brain activity is consistent with
nition find that the DLPFC activates reciprocally with changes that may be mitigating PTSD.
the medial ventral prefrontal cortex (MVPFC).36–40 Stud- Partial funding for SPECT scans was provided by the Eye
ies by Goel and Dolan have found that subjects engaged Movement Desensitization and Reprocessing International
in emotional reasoning show activation in the MVPFC Association and Amen Clinics, Inc.
and deactivation in the DLPFC and that this pattern re- The authors thank Jill Prunella, Research Associate, for her
verses when subjects are engaged in logic.37,40 Although contributions.
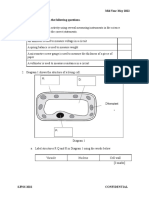
FIGURE 1. Glass Brain Representations of Activations in Post-EMDR Brains at pⴔ⬍0.005a
Posterior Anterior Right Left Right
An SPM glass brain representation of activations at p⳱⬍0.005 for each voxel. Degrees of freedom for individual voxels ⳱ 1, 5; number of
voxels was 217,449. p⳱⬍0.001.
530 http://neuro.psychiatryonline.org J Neuropsychiatry Clin Neurosci 17:4, Fall 2005
LANSING et al.
References
1. Rivard JM, Dietz P, Martell D, et al: Acute disassociative re- EMDR versus a traditional stress management program. Int J
sponses in law enforcement officers involved in critical shooting Stress Mgt 2001; 8:179–200
incidents: the clinical and forensic implications. J Forensic Sci 19. Levin P, Lazrove S, van der Kolk B: What psychological testing
2002; 47:1093–1100 and neuroimaging tell us about the treatment of posttraumatic
2. Abrams KM, Robinson GE: Occupational effects of stalking. Can stress disorder by eye movement desensitization and reprocess-
J Psychiatry 2002; 47:468–472 ing. J Anxiety Disord 1999; 13:159–172
3. Shin LM, Orr SP, Carson MA, et al: Regional cerebral blood flow 20. Davidson R, Parker KCH: Eye movement desensitization and
in the amygdala and medial prefrontal cortex during traumatic reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol
imagery in male and female Vietnam veterans with PTSD. Arch 2001; 69:305–316
Gen Psychiatry 2004; 61:168–176 21. Ironson G, Freund B, Strauss JL, et al: Comparison of two treat-
4. Sachinvala N, Kling A, Suffin S, et al: Increased regional cerebral ments for traumatic stress: a community-based study of EMDR
perfusion by 99mTc hexamethyl propylene amine oxime single and prolonged exposure. J Clin Psychol 2002; 58:113–128
photon emission computed tomography in post-traumatic stress 22. Hyer L, Brandsma JM: EMDR minus eye movements equals
disorder. Curr Psychiatry Rep 2002; 4:254–263 good psychotherapy. J Trauma Stress 1997; 10:515–522
5. Zubieta JK, Chinitz JA, Lombardi U, et al: Medial frontal cortex 23. Foa EB, Riggs DS, Dancu CV, et al: Reliability and validity of a
involvement in PTSD symptoms: a SPECT study. J Psychiatr Res brief instrument for assessing post-traumatic stress disorder. J
1999; 33:259–264 Trauma Stress 2002; 6:459–473
6. Berthier ML, Posada A, Puentes C: Dissociative flashbacks after 24. Shapiro F: Eye Movement Desensitization and Reprocessing: Ba-
right frontal injury in a Vietnam veteran with combat-related sic Principles, Protocols, and Procedures, 2nd ed. New York,
posttraumatic stress disorder. J Neuropsychiatry Clin Neurosci Guilford, 2001
2001; 13(1):101–105 25. University College London, Wellcome Department of Imaging
7. Benkelfat C, Bradwejn J, Meyer E, et al: Functional neuroanat- Neuroscience, http://www.fil.ion.ucl.ac.uk/spm
omy of CCK4-induced anxiety in normal healthy volunteers. 26. Talairach J, Tournoux P: Co-Planar Stereotactic Atlas of the Hu-
Am J Psychiatry 1995; 152:1180–1184 man Brain. Stuttgart, Beorg Thieme Verlag, 1988
8. Liberzon I, Taylor SF, Amdur R, et al: Brain activation in PTSD 27. Brett M: Smoothing tutorial at http://www.mrc-cbu.cam.ac.uk/
in response to trauma-related stimuli. Biol Psychiatry 1999; Imaging/smoothing.html.
45:817–826 28. Gündel H, O’Connor MF, Littrell L, et al: Functional neuroanat-
9. Rauch SL, Whalen PJ, Shin LM, et al: Exaggerated amygdala omy of grief: an fMRI study. Am J Psychiatry 2003; 160:1946–1953
response to masked facial stimuli in posttraumatic stress disor- 29. Servos P, Osu R, Santi A, et al: The neural substrates of biological
der: a functional MRI study. Biol Psychiatry 2000; 47:769–776 motion perception: an fMRI study. Cereb Cortex 2002; 12:772–782
10. Shapiro F: EMDR 12 years after its introduction: past and future 30. Malouin F, Richards CL, Jackson PL, et al: Brain activations dur-
research. J Clin Psychol 2002; 58:1–22 ing motor imagery of locomotor-related tasks: a PET study. Hum
11. Carlson J, Chemtob CM, Rusnak K, et al: Eye movement desen- Brain Mapp 2003; 19:47–62
sitization and reprocessing (EMDR): treatment for combat-re- 31. Moll J, de Oliveira-Souza R, Bramati IE, et al: Functional net-
lated post-traumatic stress disorder. J Trauma Stress 1998; 11:3– works in emotional moral and nonmoral social judgments. Neu-
24 roimage 2002; 16:696–703
12. Edmond T, Rubin A, Wambach K: The effectiveness of EMDR 32. Shipp S: The functional logic of cortico-pulvinar connections.
with adult female survivors of childhood sexual abuse. Soc Work Philos Trans R Soc Lond B Biol Sci 2003; 358:1605–1624
Res 1999; 23:103–116 33. Bremner JD, Innis RB, Southwick SM, et al: Decreased benzodi-
13. Ironson GI, Freund B, Strauss JL, et al: Comparison of two treat- azepine receptor binding in prefrontal cortex in combat-related
ments for traumatic stress: A community-based study of emdr posttraumatic stress disorder. Am J Psychiatry 2000; 157:1120–
and prolonged exposure. J Clin Psychol 2002; 58:113–128 1126
14. Lee C, Gavriel H, Drummond P, et al: Treatment of post-trau- 34. Bremner JD: Neuroimaging studies in post-traumatic stress dis-
matic stress disorder: a comparison of stress inoculation training order. Curr Psychiatry Rep 2002; 4:254–263
with prolonged exposure and eye movement desensitization 35. Xing GQ, Russell S, Webster MJ, et al: Decreased expression of
and reprocessing. J Clin Psychol 2002; 58:1071–1089 mineralocorticoid receptor mRNA in the prefrontal cortex in
15. Marcus S, Marquis P, Sakai C: Controlled study of treatment of schizophrenia and bipolar disorder. Int J Neuropsychopharma-
PTSD using EMDR in an HMO setting. Psychotherapy 1997; col 2004:1–11
34:307–315 36. Brody AL, Barsom MW, Bota RG, et al: Prefrontal-subcortical
16. Power KG, McGoldrick T, Brown K, et al: A controlled compar- and limbic circuit mediation of major depressive disorder. Semin
ison of eye movement desensitization and reprocessing versus Clin Neuropsychiatry 2001; 6:102–112
exposure plus cognitive restructuring, versus waiting list in the 37. Bremner JD, Vythilingam M, Ng CK, et al: Regional brain met-
treatment of post-traumatic stress disorder. J Clin Psychol and abolic correlates of alpha-methylparatyrosine-induced depres-
Psychotherapy 2002; 9:299–318 sive symptoms: implications for the neural circuitry of depres-
17. Soberman GB, Greenwald R, Rule DL: A controlled study of sion. JAMA 2003; 289:3125–3134
eye movement desensitization and reprocessing (EMDR) for 38. Brody AL, Saxena S, Mandelkern MA, et al: Brain metabolic
boys with conduct problems. J Aggression, Maltreatment, and changes associated with symptom factor improvement in major
Trauma 2002; 6:217–236 depressive disorder. Biol Psychiatry 2001; 50:171–178
18. Wilson SA, Tinker RH, Becker LA, et al: Stress management with 39. Goel V, Dolan RJ: Explaining modulation of reasoning by belief.
law enforcement personnel: a controlled outcome study of Cognition 2003; 87:B11–22
J Neuropsychiatry Clin Neurosci 17:4, Fall 2005 http://neuro.psychiatryonline.org 531
POLICE OFFICERS WITH PTSD
40. Goel V, Dolan RJ: Reciprocal neural response within lateral and 44. Davidson RJ: Anterior cerebral asymmetry and the nature of
ventral medial prefrontal cortex during hot and cold reasoning. emotion. Brain Cogn 1992; 20:125–151
Neuroimage 2003; 20:2314–2321 45. Davidson RJ: Parsing affective space: perspectives from neuro-
41. Debener S, Beauducel A, Nessler D, et al: Is resting anterior EEG psychology and psychophysiology. Neuropsychology 1993;
alpha asymmetry a trait marker for depression? Neuropsycho- 7:464–475
biology 2000; 41:31–37 46. Flor-Henry P: Cerebral Basis of Psychopathology. Boston, John
42. Bench CJ, Friston KJ, Brown RG, et al: The anatomy of melan- Wright, 1983
cholia: focal abnormalities of cerebral blood flow in major de- 47. Heller W: Gender differences in depression: perspectives from
pression. Psychol Med 1992; 22:607–615 neuropsychology. J Affect Disord 1993; 29:129–143
43. Bruder GE, Quitkin FM, Stewart JW, et al: Cerebral laterality and 48. Schwartz GE, Davidson RJ, Maer F: Right hemisphere laterali-
depression: differences in perceptual asymmetry among diag- zation for emotion in the human brain: interactions with cog-
nostic subtypes. J Abnorm Psychol 1989; 98:177–186 nition. Science 1975; 19:286–288
532 http://neuro.psychiatryonline.org J Neuropsychiatry Clin Neurosci 17:4, Fall 2005
You might also like
- Risk Assessment - Cable Pulling Laying, Glanding and Termination From RT Bay Outdoor Enclosure To RT Control BuildingDocument14 pagesRisk Assessment - Cable Pulling Laying, Glanding and Termination From RT Bay Outdoor Enclosure To RT Control Buildingnsadnan91% (82)
- VAC Swachh Bharat - 230612 - 155724Document14 pagesVAC Swachh Bharat - 230612 - 155724Tera Kal92% (13)
- User Manual ECG EDAN SE-3Document104 pagesUser Manual ECG EDAN SE-3Andreé Montúfar100% (1)
- Planning Fixed Partial Dentures For Severely Misaligned AbutmentsDocument7 pagesPlanning Fixed Partial Dentures For Severely Misaligned AbutmentsAntonny VasquezNo ratings yet
- Art Therapy Masks Reflect Emotional Changes in MilDocument13 pagesArt Therapy Masks Reflect Emotional Changes in MilRawan SalehNo ratings yet
- Michael Esterman2020Document13 pagesMichael Esterman2020Raul Morales VillegasNo ratings yet
- HHS Public Access: Longitudinal Changes in Brain Function Associated With Symptom Improvement in Youth With PTSDDocument21 pagesHHS Public Access: Longitudinal Changes in Brain Function Associated With Symptom Improvement in Youth With PTSDLeonardo PunshonNo ratings yet
- Psychotherapies For Complex Trauma A Combination Between Emdr and MindfulnessDocument1 pagePsychotherapies For Complex Trauma A Combination Between Emdr and MindfulnessRUBY SANTAMARIA FLOREZNo ratings yet
- Bradley Et Al. (2006)Document14 pagesBradley Et Al. (2006)jehonol883No ratings yet
- Change in Negative Cognitions Associated With PTSD Predicts Symptom Reduction in Prolonged ExposureDocument9 pagesChange in Negative Cognitions Associated With PTSD Predicts Symptom Reduction in Prolonged Exposureericaduran4824No ratings yet
- Emdr 2002Document14 pagesEmdr 2002jivinaNo ratings yet
- Higher Cortisol Levels Following Exposur PDFDocument34 pagesHigher Cortisol Levels Following Exposur PDFIván CornuNo ratings yet
- Neuroimage: Clinical: SciencedirectDocument9 pagesNeuroimage: Clinical: SciencedirectMoumi PanditNo ratings yet
- 1 s2.0 S0890856714004079 MainDocument10 pages1 s2.0 S0890856714004079 MainPar DoNo ratings yet
- Neuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderDocument2 pagesNeuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderClaudio PeñafielNo ratings yet
- Rehabilitas Cedera OtakDocument2 pagesRehabilitas Cedera Otakbotet_2306No ratings yet
- Jkms 33 E306Document6 pagesJkms 33 E306Mer P HNo ratings yet
- Traumatic AmnesiaDocument6 pagesTraumatic AmnesiakatiaNo ratings yet
- Which Clinical Factors Delay A Proper Treatment in Panic Di - 2022 - NeurosciencDocument2 pagesWhich Clinical Factors Delay A Proper Treatment in Panic Di - 2022 - NeurosciencloloasbNo ratings yet
- JTS 34 851Document13 pagesJTS 34 851MARIA FERNANDA OLIVEIRA SOARESNo ratings yet
- Prazosin TX PTSDMetaanalysis 2020Document8 pagesPrazosin TX PTSDMetaanalysis 2020Dr. José Juan PeralesNo ratings yet
- Pubs Shin 2010 Neural CorDocument8 pagesPubs Shin 2010 Neural CorTJSNo ratings yet
- 1 s2.0 S0028393217302403 MainDocument8 pages1 s2.0 S0028393217302403 MaincursosNo ratings yet
- 1 s2.0 S105381192100519X MainDocument13 pages1 s2.0 S105381192100519X MainSantai JakNo ratings yet
- A Paradigm Shift in Trauma Treatment - Converging Evidence For A Novel AdaptationDocument3 pagesA Paradigm Shift in Trauma Treatment - Converging Evidence For A Novel AdaptationTeresa GMNo ratings yet
- From Pro-Inflammatory Molecules To The Brain's Resting-State Connectivity The Future of Clinical Diagnosis of DepressionDocument36 pagesFrom Pro-Inflammatory Molecules To The Brain's Resting-State Connectivity The Future of Clinical Diagnosis of DepressiondgavrileNo ratings yet
- Calancie AnnNYAcadSci 2018Document19 pagesCalancie AnnNYAcadSci 2018Barbara Kowalska MarquesNo ratings yet
- Brain Circuit Dysfunction in Post - Traumatic Stress Disorder: From Mouse To Man - Robert J. FensterDocument17 pagesBrain Circuit Dysfunction in Post - Traumatic Stress Disorder: From Mouse To Man - Robert J. FensterAlvaro Arboledas LoriteNo ratings yet
- Artikel InternasionalDocument15 pagesArtikel InternasionalFitriatul MunawarohNo ratings yet
- Advancing Preclinical Chronic Stress Models To Promote Therapeutic Discovery For Human Stress DisordersDocument12 pagesAdvancing Preclinical Chronic Stress Models To Promote Therapeutic Discovery For Human Stress DisordersMoo Gee100% (1)
- tmp6BD2 TMPDocument1 pagetmp6BD2 TMPFrontiersNo ratings yet
- Brain-Based Biotypes of Psychiatric Vulnerability in The Acute Aftermath of TraumaDocument13 pagesBrain-Based Biotypes of Psychiatric Vulnerability in The Acute Aftermath of TraumaRicardo EscNo ratings yet
- Effect of Group V Individual Cognitive Processing Therapy in Active-Duty Military Seeking Treatment For Posttraumatic Stress DisorderDocument9 pagesEffect of Group V Individual Cognitive Processing Therapy in Active-Duty Military Seeking Treatment For Posttraumatic Stress DisorderBrandon Gray100% (1)
- 1 s2.0 S2213158219303511 MainDocument8 pages1 s2.0 S2213158219303511 MainGilbert SihombingNo ratings yet
- 1 s2.0 S0005791616301343 MainDocument7 pages1 s2.0 S0005791616301343 MainTulaNo ratings yet
- Cognitive-Behavior Therapy Vs Exposure Therapy in The Treatment of PTSD in RefugeesDocument15 pagesCognitive-Behavior Therapy Vs Exposure Therapy in The Treatment of PTSD in RefugeesAna CristeaNo ratings yet
- Euenc JdeeDocument65 pagesEuenc JdeeGustavoNo ratings yet
- 2022, The Efficacy of TMS and Negative Symptoms of SchizophreniaDocument12 pages2022, The Efficacy of TMS and Negative Symptoms of Schizophreniafelix08121992No ratings yet
- Neuromodulation in Response To Electroconvulsive Therapy Inschizophrenia and Major DepressionDocument8 pagesNeuromodulation in Response To Electroconvulsive Therapy Inschizophrenia and Major DepressionPablo RamirezNo ratings yet
- Neural Correlates of Recall of Life Events in Conversion DisorderDocument9 pagesNeural Correlates of Recall of Life Events in Conversion DisorderMarcus Vinicius AlvesNo ratings yet
- Sequential Fear Generalization and Network Connectivity in Trauma Exposed Humans With and Without PsychopathologyDocument9 pagesSequential Fear Generalization and Network Connectivity in Trauma Exposed Humans With and Without Psychopathologyheidarihamed4No ratings yet
- 10 1192@bjp 2020 158Document7 pages10 1192@bjp 2020 158Olga MichailidouNo ratings yet
- Cognitive Outcomes in Patients With Major Depression Treated With Electroconvulsive TherapyDocument8 pagesCognitive Outcomes in Patients With Major Depression Treated With Electroconvulsive TherapyPsiholog Monica StănescuNo ratings yet
- Untreated Initial Psychosis: Relation To Cognitive Deficits and Brain Morphology in First-Episode SchizophreniaDocument7 pagesUntreated Initial Psychosis: Relation To Cognitive Deficits and Brain Morphology in First-Episode SchizophreniaelvinegunawanNo ratings yet
- Ect Skizo ResistenDocument28 pagesEct Skizo ResistenZulvikar UmasangadjiNo ratings yet
- (Intro - General ImRs) Arntz-2012-Imagery-Rescripting-As-A-Therapeutic-Technique-Review-Of-Clinical-Trials-Basic-Studies-And-Research-AgendaDocument19 pages(Intro - General ImRs) Arntz-2012-Imagery-Rescripting-As-A-Therapeutic-Technique-Review-Of-Clinical-Trials-Basic-Studies-And-Research-AgendaDolunay UludağNo ratings yet
- Linking Molecules To Mood: New Insight Into The Biology of DepressionDocument16 pagesLinking Molecules To Mood: New Insight Into The Biology of Depressiondudul pudlianNo ratings yet
- Biological Psychology: ArticleinfoDocument15 pagesBiological Psychology: ArticleinfoManuela SilvaNo ratings yet
- TMP ED34Document9 pagesTMP ED34FrontiersNo ratings yet
- Yang 2021Document10 pagesYang 2021Andrea Galindo EscobosaNo ratings yet
- Olive 2018 Superior Colliculus Resting State NDocument12 pagesOlive 2018 Superior Colliculus Resting State Nbenoit berthailNo ratings yet
- Fpsyg 08 01750Document10 pagesFpsyg 08 01750Nerea F GNo ratings yet
- Electroconvulsive TherapyDocument10 pagesElectroconvulsive TherapyYasinNo ratings yet
- Richardson 2018Document7 pagesRichardson 2018Maria Von ShaftNo ratings yet
- King 2016Document13 pagesKing 2016Realidades InfinitasNo ratings yet
- Amphetamine-Induced Striatal Dopamine Release in SchizotypalDocument11 pagesAmphetamine-Induced Striatal Dopamine Release in Schizotypaleva para eva love is loveNo ratings yet
- Raboni Sleep + Emdr Nyas 06Document6 pagesRaboni Sleep + Emdr Nyas 06Felipe Orejuela SotoNo ratings yet
- Irritability in Pre-Clinical Huntington's Disease: NeuropsychologiaDocument9 pagesIrritability in Pre-Clinical Huntington's Disease: NeuropsychologiaJose Bryan GonzalezNo ratings yet
- Auricular Causative Diagnosis-Finding The Roots of Diseases: A Study of Clinical CasesDocument11 pagesAuricular Causative Diagnosis-Finding The Roots of Diseases: A Study of Clinical Casesyan92120No ratings yet
- Psych Trans PDFDocument21 pagesPsych Trans PDFWinnie AriolaNo ratings yet
- Artifact 15Document16 pagesArtifact 15api-348971279No ratings yet
- Predictors of Poor Treatment Response ToDocument13 pagesPredictors of Poor Treatment Response ToMaite Novo del valleNo ratings yet
- 16546-Article Text-64861-1-10-20160825Document11 pages16546-Article Text-64861-1-10-20160825THIARE GALDAMES HERNANDEZNo ratings yet
- Fundamentals and Clinics of Deep Brain Stimulation: An Interdisciplinary ApproachFrom EverandFundamentals and Clinics of Deep Brain Stimulation: An Interdisciplinary ApproachYasin TemelNo ratings yet
- Jacobson y Christensen (1996) Acceptance and Change in Couple TherapyDocument308 pagesJacobson y Christensen (1996) Acceptance and Change in Couple TherapyFelipe Orejuela SotoNo ratings yet
- Sustainable Practice ChecklistDocument6 pagesSustainable Practice ChecklistFelipe Orejuela SotoNo ratings yet
- Hypothetical ThinkingDocument215 pagesHypothetical ThinkingFelipe Orejuela SotoNo ratings yet
- Diagnosis, Conceptualization and Treatment Planning For AdultsDocument350 pagesDiagnosis, Conceptualization and Treatment Planning For AdultsFelipe Orejuela SotoNo ratings yet
- Sectores Pag 29Document47 pagesSectores Pag 29cghortaNo ratings yet
- 11 cсынып емтихан сурактарыDocument6 pages11 cсынып емтихан сурактарыakzharNo ratings yet
- Linagliptin Drug MonographDocument7 pagesLinagliptin Drug MonographNearMelowNo ratings yet
- Stein Sept 29 LetterDocument2 pagesStein Sept 29 LetterMitchell BlackNo ratings yet
- GC 4Document1 pageGC 4ais82603No ratings yet
- EXT - 230914 - 0850 - MS32 - V001 - BMW15.10 - SYN - QA - MS - 0032 - 01-ESD CoatingDocument13 pagesEXT - 230914 - 0850 - MS32 - V001 - BMW15.10 - SYN - QA - MS - 0032 - 01-ESD CoatingТамер БакировNo ratings yet
- Manuscript 2 FinalDocument60 pagesManuscript 2 FinalKape Ka BaNo ratings yet
- Pulsed Electro Magnetic Energy (PEME)Document9 pagesPulsed Electro Magnetic Energy (PEME)NATARAJAN KAVITHANo ratings yet
- Media Bulletin 11.07.2020 27 Pages English 491 KBDocument27 pagesMedia Bulletin 11.07.2020 27 Pages English 491 KBKathirasan RamalingamNo ratings yet
- Standards For Competence For Registered MidwivesDocument14 pagesStandards For Competence For Registered MidwivescarNo ratings yet
- Sanet Me0803120575Document169 pagesSanet Me0803120575parallax1957No ratings yet
- Healthy Eating Patterns and Risk of Total and Cause-Specific Mortality - JAMA Intern MedDocument12 pagesHealthy Eating Patterns and Risk of Total and Cause-Specific Mortality - JAMA Intern MedSamitti ChotsriluechaNo ratings yet
- Weekly Current Affairs 8-Jan-2024 To 14-Jan-2024Document25 pagesWeekly Current Affairs 8-Jan-2024 To 14-Jan-2024Vandana VermaNo ratings yet
- Arc Flash Safety BulletinDocument4 pagesArc Flash Safety BulletinVictor Manuel Flores ZuñigaNo ratings yet
- Articles Rgarding Importantce of Minerals and Effects of Food DepletionDocument16 pagesArticles Rgarding Importantce of Minerals and Effects of Food Depletionapi-3827527No ratings yet
- Clinical-Trial AIIADocument6 pagesClinical-Trial AIIAkaushal ahirwarNo ratings yet
- QC How To Make A Good Method StatementDocument3 pagesQC How To Make A Good Method StatementRsjBugtongNo ratings yet
- Clinical Nursing Judgement PaperDocument5 pagesClinical Nursing Judgement Paperapi-663930784No ratings yet
- 7 Ways To Treat A Fever Naturally - Reader ModeDocument14 pages7 Ways To Treat A Fever Naturally - Reader Modeedward nodzoNo ratings yet
- Report No. 11 of 2023 - PA On PMJAY - English PDF A 064d22bab2b83b5.38721048Document168 pagesReport No. 11 of 2023 - PA On PMJAY - English PDF A 064d22bab2b83b5.38721048arish.khanNo ratings yet
- 3 23 2005 Aviation EnglishDocument14 pages3 23 2005 Aviation EnglishSky LukeNo ratings yet
- Halime Fetahu Osmani - The Structure of KinesiologyDocument6 pagesHalime Fetahu Osmani - The Structure of Kinesiologynuno costeNo ratings yet
- Dialogo de Ingles Paciente A OdontologoDocument4 pagesDialogo de Ingles Paciente A OdontologoKimberly Pinzon0% (1)
- EFfCI GMP Position Paper Certificates of AnalysisDocument5 pagesEFfCI GMP Position Paper Certificates of AnalysisAladdin MobarakNo ratings yet
- Mackey 2016 CVDocument8 pagesMackey 2016 CVapi-304462343No ratings yet
- F2 Mid-Year Exam Section BDocument3 pagesF2 Mid-Year Exam Section BAnne Marian Anak JOSEPHNo ratings yet