Professional Documents
Culture Documents
Oab Guidelines
Oab Guidelines
Uploaded by
amirzoevaCopyright:
Available Formats
You might also like
- Original PDF Microeconomics 13th Edition by Michael Parkin PDFDocument51 pagesOriginal PDF Microeconomics 13th Edition by Michael Parkin PDFmonica.bass495100% (42)
- Medical DoctorsDocument10 pagesMedical DoctorsDarius Mubita MwangalaNo ratings yet
- Creog Urogyn ReviewDocument97 pagesCreog Urogyn ReviewAlexandriah AlasNo ratings yet
- Constipation NCPDocument3 pagesConstipation NCPSeth Amiel MotaNo ratings yet
- Assignment GiDocument14 pagesAssignment GiVoid LessNo ratings yet
- Incontinence: M.Indumathi, M.sc-1 Year Med-Surg DepartDocument36 pagesIncontinence: M.Indumathi, M.sc-1 Year Med-Surg DepartAnn Merlin JobinNo ratings yet
- Assessment Diagnosis Rationale Expected Outcome Implementation Rationale EvaluationDocument5 pagesAssessment Diagnosis Rationale Expected Outcome Implementation Rationale EvaluationRazzel Daza100% (1)
- Evaluation and Treatment of IncontinenceDocument52 pagesEvaluation and Treatment of IncontinenceAlexandriah AlasNo ratings yet
- Obstetrics - GynaecologyDocument137 pagesObstetrics - GynaecologyCiel100% (1)
- Urinery IncontinsetenceDocument1 pageUrinery IncontinsetenceLanaAmerieNo ratings yet
- Irregular Bowel HabitDocument66 pagesIrregular Bowel Habitfahim ahamedNo ratings yet
- NCP ConstipationDocument3 pagesNCP ConstipationKingJayson Pacman06No ratings yet
- Sirosis Hepatis Dan KomplikasiDocument36 pagesSirosis Hepatis Dan KomplikasiMuhammad HafizdNo ratings yet
- Incontinence: DR - Swathi Singh MPT Orthopaedics, MiapDocument69 pagesIncontinence: DR - Swathi Singh MPT Orthopaedics, MiapSonu GuptaNo ratings yet
- ISUOG Basic Training: Examining The Uterus, Cervix, Ovaries & Adnexae: Normal FindingsDocument51 pagesISUOG Basic Training: Examining The Uterus, Cervix, Ovaries & Adnexae: Normal FindingsDian Putri NingsihNo ratings yet
- Biophysical ProfileDocument8 pagesBiophysical ProfileAmritaNo ratings yet
- BPH 180828154943Document42 pagesBPH 180828154943Amandeep SinghNo ratings yet
- Factsheet: Bladder Control After A Prostate OperationDocument7 pagesFactsheet: Bladder Control After A Prostate OperationYosalfa Adhista KurniawanNo ratings yet
- 4 ConstipationDocument58 pages4 ConstipationPonkiya Ankit100% (1)
- NCM 116Document19 pagesNCM 116Gail Leslie HernandezNo ratings yet
- Female Reproductive System AssessmentDocument8 pagesFemale Reproductive System Assessmentluna nguyenNo ratings yet
- Journal of Alternative Medical Research: Basti (Medicated Enemata)Document3 pagesJournal of Alternative Medical Research: Basti (Medicated Enemata)Madhav DalviNo ratings yet
- Surgery - Female Urology and Incontinence (Tutorial)Document6 pagesSurgery - Female Urology and Incontinence (Tutorial)halesNo ratings yet
- Comprehensive Overview of Constipation: William E. Whitehead, PHD Center Co-DirectorDocument3 pagesComprehensive Overview of Constipation: William E. Whitehead, PHD Center Co-DirectornehaNo ratings yet
- Solifen Refresher SlidesDocument21 pagesSolifen Refresher SlidesDr.Muhammad UmerNo ratings yet
- Bladder Incontinence in Spinal Cord InjuriesDocument50 pagesBladder Incontinence in Spinal Cord Injuriessuketu215100% (4)
- Laboratory Exams/Diagnostic TestsDocument7 pagesLaboratory Exams/Diagnostic Testsmark OrpillaNo ratings yet
- Benign Prostatic Hyperplasia. NCM 109Document16 pagesBenign Prostatic Hyperplasia. NCM 109Niña Jean Tormis AldabaNo ratings yet
- The AbdomenDocument38 pagesThe AbdomenJesusa AbanesNo ratings yet
- Role of Lasuna Taila Vasti in Artava Vyapada - Menstrual IrregularitiesDocument3 pagesRole of Lasuna Taila Vasti in Artava Vyapada - Menstrual IrregularitiesMSKCNo ratings yet
- Chapter 92, Small Intestinal MotilityDocument53 pagesChapter 92, Small Intestinal MotilitySangita MNo ratings yet
- UBC - Bowel Management in Older AdultsDocument41 pagesUBC - Bowel Management in Older Adultsb BNo ratings yet
- ScienceDocument3 pagesScienceMusa KaleemNo ratings yet
- Norzagaray DutyprojectDocument25 pagesNorzagaray DutyprojectSven OrdanzaNo ratings yet
- His Mother Stated That He Experienced Diarrhea and Abdominal Pain For Last 3 DaysDocument3 pagesHis Mother Stated That He Experienced Diarrhea and Abdominal Pain For Last 3 DaysKingJayson Pacman06No ratings yet
- MATERI SESI 4.1 - MAR DR - HeryDocument9 pagesMATERI SESI 4.1 - MAR DR - HerydewiswahyuNo ratings yet
- 4 EsophagealSpasm BajaDocument6 pages4 EsophagealSpasm Bajakint manlangitNo ratings yet
- ConstipationDocument6 pagesConstipationاحمد محمدNo ratings yet
- Pelvic Organ ProlapseDocument9 pagesPelvic Organ ProlapseSonny Dizon PareñasNo ratings yet
- Overactivebladder 160426102342Document53 pagesOveractivebladder 160426102342Tô Hoàng DũngNo ratings yet
- Cleft Lip & Palate: Nursing Management in Children With Congenital DiseaseDocument84 pagesCleft Lip & Palate: Nursing Management in Children With Congenital DiseaseAnonymous KXYykpaZPNo ratings yet
- 4-ASKEP GI DefectDocument84 pages4-ASKEP GI DefectAnonymous KXYykpaZPNo ratings yet
- MotilityDocument77 pagesMotilityrobelNo ratings yet
- Fetal Surveillance: By: Kristine R. Niñonuevo-Dayao, M.DDocument43 pagesFetal Surveillance: By: Kristine R. Niñonuevo-Dayao, M.DSanjay Kumar SanjuNo ratings yet
- Exercise With Pre & Post Natal ClientsDocument20 pagesExercise With Pre & Post Natal ClientsDan CowenNo ratings yet
- Ocp HCTMDocument2 pagesOcp HCTMEvelyn LimNo ratings yet
- ProlapseDocument51 pagesProlapsejijaniNo ratings yet
- IncontinenceDocument9 pagesIncontinenceHanaNo ratings yet
- What Is Faecal Incontinence?Document6 pagesWhat Is Faecal Incontinence?drm1238475No ratings yet
- UV Prolapse: DR Liyana Alya & DR Afifah Supervised by DR KamaliahDocument24 pagesUV Prolapse: DR Liyana Alya & DR Afifah Supervised by DR KamaliahAfifah SelamatNo ratings yet
- 1.1 GynaecologyDocument59 pages1.1 Gynaecologyayeshafarooq60No ratings yet
- Cleft Lip & Palate: Nursing Management in Children With Congenital DiseaseDocument75 pagesCleft Lip & Palate: Nursing Management in Children With Congenital DiseaseSherly Mectildis BakerNo ratings yet
- PancreATITIS OCT. 21, 2021Document33 pagesPancreATITIS OCT. 21, 2021Alyssa NicoleNo ratings yet
- Abortion BSN 0PR-2: Case Study of BelleDocument27 pagesAbortion BSN 0PR-2: Case Study of BellekervinNo ratings yet
- NCPDocument2 pagesNCPJoanne Pascual TuasonNo ratings yet
- All About Constipation Booklet 2016 05 RevDocument4 pagesAll About Constipation Booklet 2016 05 RevHana Jao100% (1)
- Basic Concepts, Development & Classification of TheoryDocument40 pagesBasic Concepts, Development & Classification of TheoryReshmiNo ratings yet
- ConstipatiaDocument34 pagesConstipatiaMaria Traian100% (2)
- Franchie M. Hsu Case StudyDocument5 pagesFranchie M. Hsu Case StudyFranchieNo ratings yet
- Digestive System: Diagnostic Tests For Diseases of The Digestive SystemDocument14 pagesDigestive System: Diagnostic Tests For Diseases of The Digestive Systemmai-maiNo ratings yet
- No-Risk Abs: A Safe Workout Program for Core StrengthFrom EverandNo-Risk Abs: A Safe Workout Program for Core StrengthNo ratings yet
- Incontinence a Time to Heal with Yoga and Acupressure: A Six Week Exercise Program for People with Simple Stress Urinary IncontinenceFrom EverandIncontinence a Time to Heal with Yoga and Acupressure: A Six Week Exercise Program for People with Simple Stress Urinary IncontinenceNo ratings yet
- Leica Rm2125rts Ifu 2v8l enDocument68 pagesLeica Rm2125rts Ifu 2v8l enNguyen Trung HuyNo ratings yet
- Cold Work PermitDocument1 pageCold Work PermitРудик НикитаNo ratings yet
- Laporan PDM 20 NovemberDocument21 pagesLaporan PDM 20 NovemberdeokNo ratings yet
- Injury PreventionDocument16 pagesInjury PreventionSim BuenNo ratings yet
- Nursing Care Plans: Assessment Nursing Diagnosis Planning Implementation Rationale EvaluationDocument2 pagesNursing Care Plans: Assessment Nursing Diagnosis Planning Implementation Rationale EvaluationRheeanne Mae Amilasan100% (1)
- 1st Periodical Test in Beauty Care 10 - Wellness MasssageDocument2 pages1st Periodical Test in Beauty Care 10 - Wellness MasssageBelinda Lapsit100% (5)
- Chili and Makabuhay Stem Extract As MolluscicideDocument27 pagesChili and Makabuhay Stem Extract As MolluscicideQueen Ann Navallo80% (10)
- Open Letter To Mayor-Elect Wu - Mass and CassDocument2 pagesOpen Letter To Mayor-Elect Wu - Mass and Cassdialynn dwyerNo ratings yet
- Instructions To The Candidate: Examination Centre: Centre Code: 2032 ID Number: Photo IDDocument1 pageInstructions To The Candidate: Examination Centre: Centre Code: 2032 ID Number: Photo IDuday xeroxNo ratings yet
- English As A Second Language: Paper 1: Reading and WritingDocument24 pagesEnglish As A Second Language: Paper 1: Reading and Writingﹺ ﹺ ﹺNo ratings yet
- Book Stress, the Psychology of Managing PressureDocument18 pagesBook Stress, the Psychology of Managing PressureNadia AdreNo ratings yet
- NCP Abruptio PlacentaDocument2 pagesNCP Abruptio PlacentaCarson Birth100% (1)
- ITR Prenatal v.3Document1 pageITR Prenatal v.3SHEBA RAE ESPERANZA100% (1)
- Cancer ScreeningDocument8 pagesCancer Screeninglakshminivas PingaliNo ratings yet
- The Influenza Pandemic of 1918 and The Current Covid 19 PandemicDocument4 pagesThe Influenza Pandemic of 1918 and The Current Covid 19 PandemicJescah JuneNo ratings yet
- Learning Activity 1 Hugo Andrez Bustos Restrepo Evidence: Regrets From The DyingDocument5 pagesLearning Activity 1 Hugo Andrez Bustos Restrepo Evidence: Regrets From The DyingAndres B RestrepoNo ratings yet
- Bi-Annual ExamDocument19 pagesBi-Annual ExamManuel Timothy Jude LoNo ratings yet
- 089 44 Final Biologi Fasa4 DLP T4-3-28Document26 pages089 44 Final Biologi Fasa4 DLP T4-3-28BF CLNo ratings yet
- Fire Drills Safety HandoutDocument2 pagesFire Drills Safety HandoutRahulPrakash100% (1)
- Questions and Answers A Guide To Fitness and Wellness 3Rd Edition Liguori Test Bank Full Chapter PDFDocument48 pagesQuestions and Answers A Guide To Fitness and Wellness 3Rd Edition Liguori Test Bank Full Chapter PDFmathewsandersa13j100% (9)
- RainforestHerbs BrochureDocument11 pagesRainforestHerbs BrochureErlena RahimNo ratings yet
- REV Skripsi LR Hubungan Pemberian ASIE DG Kejadian Stunting PD Bad YWKAe5GDocument89 pagesREV Skripsi LR Hubungan Pemberian ASIE DG Kejadian Stunting PD Bad YWKAe5GFauziyah AnnisaaNo ratings yet
- Manual de Instalación, Operación Mantenimiento de Balanza Fajas PDFDocument559 pagesManual de Instalación, Operación Mantenimiento de Balanza Fajas PDFCarlos Alberto Alvarado LoayzaNo ratings yet
- NCP Kenezo, Female 17Document2 pagesNCP Kenezo, Female 17labanesstephanyNo ratings yet
- Unit #7 - Basic Quality Control For The Clinical LaboratoryDocument28 pagesUnit #7 - Basic Quality Control For The Clinical LaboratoryFaisal JamshedNo ratings yet
- The Three Levels of Moral DilemmasDocument9 pagesThe Three Levels of Moral DilemmasVictoria AntonetteNo ratings yet
- Project Selection-Numeric ModelsDocument39 pagesProject Selection-Numeric Modelsshrutimsawant835No ratings yet
- Stressors, Affectivity, and Self - Efficacy As Predictors of Librarians' Thriving at WorkDocument12 pagesStressors, Affectivity, and Self - Efficacy As Predictors of Librarians' Thriving at WorkIOER International Multidisciplinary Research Journal ( IIMRJ)No ratings yet
Oab Guidelines
Oab Guidelines
Uploaded by
amirzoevaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oab Guidelines
Oab Guidelines
Uploaded by
amirzoevaCopyright:
Available Formats
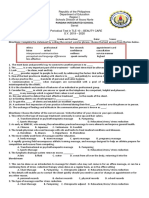
Overactive Bladder – clinical guidance
V2.1 Last reviewed: Jan 2023 Review date: Jan 2026
Overactive Bladder Clinical Guideline
Overactive Bladder (OAB) is urgency with or without urge incontinence, usually with frequency and nocturia.
Urge Urinary Incontinence is involuntary leakage of urine associated with urgency.
Mixed Urinary Incontinence is involuntary leakage of urine associated with urgency and also exertion, sneezing
or coughing.
Initial assessment: Refer to Urology / Urogynaecology if:
• Full history. • Visible haematuria.
• Frequency/Volume Chart (bladder diary). • Recurrent or persisting UTI associated with
• Urinalysis. haematuria in patients aged 40 years and older.
• Measurement of post-void residue. • Microscopic haematuria in patients aged >50
years.
Men • Suspected urinary tract malignancy or raised
• May include PR examination, PSA test, flow- PSA.
rate measurement. • Persisting bladder or urethral pain.
• Consider referral to Prostate Assessment Clinic. • Suspected neurological disease.
• Significant voiding difficulty.
Women • Suspected urogenital fistulae.
• Assessment of pelvic floor. • Previous continence/pelvic cancer surgery.
• Examine for vaginal atrophy and prolapse. • Previous pelvic radiation or chemotherapy
Conservative management
• All patients should have conservative treatment prior to commencement of medical therapy or referral to secondary care.
• Patients can be referred to the District Nurse Continence Clinic or the Continence Advisory Service for assessment and
conservative treatment.
• Should include patient education, lifestyle advice, bladder training and pelvic floor exercises.
• Manage patient’s environment (e.g., commode in place).
• Review medications (e.g., diuretics, anti-hypertensives, anti-depressants, antimuscarinics etc).
Post-menopausal
Post-menopausal womenwomen - Intravaginal oestrogens are recommended for women with vaginal atrophy and OAB
Intravaginal
symptoms (NICE 2006). are recommended for women with vaginal atrophy and OAB symptoms (NICE 2006).
oestrogens
E.g.,
E.g., estriol
estriol 0.1%
0.1% cream (Ovestin)(£4.45/15g)
cream (Ovestin) (£4.45/15g)or
orVagirux
Vagirux vaginal
vaginaltabs
tabs(£11.34/24).
(£11.34/24). Use
Usedaily
dailyfor
for22weeks,
weeks,then
thentwice
twice
weekly for 3 months.
weekly for 3 months.
Lifestyle
Lifestyleadvice
advice Bladder
Bladder Retraining
Retraining -- Minimum
Minimum of
of 6
6 weeks
weeks (NICE
(NICE 2006).
2006).
Modify
Modify highor
high orlow
lowfluid
fluidintake.
intake.
Healthy
Healthy eating, avoidcaffeine,
eating, avoid caffeine,reduce
reducealcohol
alcoholintake.
intake. Pelvicfloor
Pelvic floorexercises
exercises
Smoking cessation.
Smoking cessation.
Weight Trial for at least 33months
Trial for at least monthssupervised
supervisedpelvic
pelvicfloor
floormuscle
muscle
Weightloss
lossand
andexercise,
exercise,healthy
healthyeating.
eating. training by continence advisor or physiotherapist.
Constipation advice. training by continence advisor or physiotherapist.
Constipation advice.
Improved
Review at 3 months Continue
Ongoing problems
Medication therapy (See flowchart below)
Page 1 Author: R Parkinson. Ratified by Nottinghamshire APC Jan 2023
Overactive Bladder – clinical guidance
V2.1 Last reviewed: Jan 2023 Review date: Jan 2026
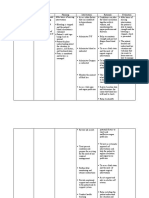
Overactive Bladder Clinical Guideline – Medication Therapy
Conservative management (as above)
All patients should have conservative treatment prior to commencement of medical therapy or referral to secondary care.
Post-menopausal women - Intravaginal oestrogens are recommended for women with vaginal atrophy and OAB symptoms.
E.g., estriol 0.1% cream (Ovestin) or Vagirux vaginal tablets. Use daily for 2 weeks, then twice weekly for 3 months.
YES Are anticholinergics contraindicated?
(e.g., myasthenia gravis, narrow angle glaucoma, Sjögren-syndrome, cognitive impairment).
No
First Line: Generic anticholinergics
NICE NG123: when offering antimuscarinics “take account of other existing medication affecting total anticholinergic load”.
Consider calculating the anticholinergic burden score using the ACB calculator.
These medicines can potentially cause an increase in falls risk. See Medicines and Falls Chart
Anticholinergic medications have similar efficacy and side-effect profiles, therefore select one with the lowest acquisition cost.
If the initial choice is not effective, or has troublesome side effects, consider lowering dose/strength, or a trial of an
alternative medicine from the first line options.
Medicine Strength Dose Cost/28days (Dec 22)
Oxybutynin IR* 2.5mg Twice a day £1.52
Oxybutynin IR* 5mg Twice a day (titrate to three times a day as tolerated) £1.41 - £2.12
Tolterodine* 2mg Twice a day £3.06
Solifenacin 5-10mg Once a day £3.04 - £3.56
Trospium 20mg Twice a day £4.93
*Do not offer oxybutynin or tolterodine to frail, elderly patients.
If swallowing difficulties or unable to tolerate solid formulations
1st: Oxybutynin patches 36mg (3.9mg/24hrs) Apply twice weekly £27.20
2nd: Solifenacin liquid 5-10mg Once a day £27.62 - £55.24
Improved
Review at 4-8 weeks Continue
Troublesome side effects/lack of efficacy
Second line medication β-3 agonist (non-anticholinergic):
Mirabegron 50mg MR tablet once a day (£27.07).
(contra-indicated in severe uncontrolled hypertension systolic ≥ 180 or diastolic ≥110mmHg)
Reduce to 25mg once a day if moderate hepatic impairment or eGFR <30ml/min.
Blood pressure should be taken before starting treatment and monitored regularly during treatment.
Troublesome side effects Improved
Review at 4-8 weeks Continue
Lack of efficacy
Third line medication combination:
Mirabegron MR tablet once a day + solifenacin once a day
(Unless troublesome side effects on either monotherapy)
Improved
Review at 4-8 weeks Continue
Troublesome side effects/lack of efficacy
Consider referral to Urology/Urogynaecology
Page 2 Author: R Parkinson. Ratified by Nottinghamshire APC Jan 2023
You might also like
- Original PDF Microeconomics 13th Edition by Michael Parkin PDFDocument51 pagesOriginal PDF Microeconomics 13th Edition by Michael Parkin PDFmonica.bass495100% (42)
- Medical DoctorsDocument10 pagesMedical DoctorsDarius Mubita MwangalaNo ratings yet
- Creog Urogyn ReviewDocument97 pagesCreog Urogyn ReviewAlexandriah AlasNo ratings yet
- Constipation NCPDocument3 pagesConstipation NCPSeth Amiel MotaNo ratings yet
- Assignment GiDocument14 pagesAssignment GiVoid LessNo ratings yet
- Incontinence: M.Indumathi, M.sc-1 Year Med-Surg DepartDocument36 pagesIncontinence: M.Indumathi, M.sc-1 Year Med-Surg DepartAnn Merlin JobinNo ratings yet
- Assessment Diagnosis Rationale Expected Outcome Implementation Rationale EvaluationDocument5 pagesAssessment Diagnosis Rationale Expected Outcome Implementation Rationale EvaluationRazzel Daza100% (1)
- Evaluation and Treatment of IncontinenceDocument52 pagesEvaluation and Treatment of IncontinenceAlexandriah AlasNo ratings yet
- Obstetrics - GynaecologyDocument137 pagesObstetrics - GynaecologyCiel100% (1)
- Urinery IncontinsetenceDocument1 pageUrinery IncontinsetenceLanaAmerieNo ratings yet
- Irregular Bowel HabitDocument66 pagesIrregular Bowel Habitfahim ahamedNo ratings yet
- NCP ConstipationDocument3 pagesNCP ConstipationKingJayson Pacman06No ratings yet
- Sirosis Hepatis Dan KomplikasiDocument36 pagesSirosis Hepatis Dan KomplikasiMuhammad HafizdNo ratings yet
- Incontinence: DR - Swathi Singh MPT Orthopaedics, MiapDocument69 pagesIncontinence: DR - Swathi Singh MPT Orthopaedics, MiapSonu GuptaNo ratings yet
- ISUOG Basic Training: Examining The Uterus, Cervix, Ovaries & Adnexae: Normal FindingsDocument51 pagesISUOG Basic Training: Examining The Uterus, Cervix, Ovaries & Adnexae: Normal FindingsDian Putri NingsihNo ratings yet
- Biophysical ProfileDocument8 pagesBiophysical ProfileAmritaNo ratings yet
- BPH 180828154943Document42 pagesBPH 180828154943Amandeep SinghNo ratings yet
- Factsheet: Bladder Control After A Prostate OperationDocument7 pagesFactsheet: Bladder Control After A Prostate OperationYosalfa Adhista KurniawanNo ratings yet
- 4 ConstipationDocument58 pages4 ConstipationPonkiya Ankit100% (1)
- NCM 116Document19 pagesNCM 116Gail Leslie HernandezNo ratings yet
- Female Reproductive System AssessmentDocument8 pagesFemale Reproductive System Assessmentluna nguyenNo ratings yet
- Journal of Alternative Medical Research: Basti (Medicated Enemata)Document3 pagesJournal of Alternative Medical Research: Basti (Medicated Enemata)Madhav DalviNo ratings yet
- Surgery - Female Urology and Incontinence (Tutorial)Document6 pagesSurgery - Female Urology and Incontinence (Tutorial)halesNo ratings yet
- Comprehensive Overview of Constipation: William E. Whitehead, PHD Center Co-DirectorDocument3 pagesComprehensive Overview of Constipation: William E. Whitehead, PHD Center Co-DirectornehaNo ratings yet
- Solifen Refresher SlidesDocument21 pagesSolifen Refresher SlidesDr.Muhammad UmerNo ratings yet
- Bladder Incontinence in Spinal Cord InjuriesDocument50 pagesBladder Incontinence in Spinal Cord Injuriessuketu215100% (4)
- Laboratory Exams/Diagnostic TestsDocument7 pagesLaboratory Exams/Diagnostic Testsmark OrpillaNo ratings yet
- Benign Prostatic Hyperplasia. NCM 109Document16 pagesBenign Prostatic Hyperplasia. NCM 109Niña Jean Tormis AldabaNo ratings yet
- The AbdomenDocument38 pagesThe AbdomenJesusa AbanesNo ratings yet
- Role of Lasuna Taila Vasti in Artava Vyapada - Menstrual IrregularitiesDocument3 pagesRole of Lasuna Taila Vasti in Artava Vyapada - Menstrual IrregularitiesMSKCNo ratings yet
- Chapter 92, Small Intestinal MotilityDocument53 pagesChapter 92, Small Intestinal MotilitySangita MNo ratings yet
- UBC - Bowel Management in Older AdultsDocument41 pagesUBC - Bowel Management in Older Adultsb BNo ratings yet
- ScienceDocument3 pagesScienceMusa KaleemNo ratings yet
- Norzagaray DutyprojectDocument25 pagesNorzagaray DutyprojectSven OrdanzaNo ratings yet
- His Mother Stated That He Experienced Diarrhea and Abdominal Pain For Last 3 DaysDocument3 pagesHis Mother Stated That He Experienced Diarrhea and Abdominal Pain For Last 3 DaysKingJayson Pacman06No ratings yet
- MATERI SESI 4.1 - MAR DR - HeryDocument9 pagesMATERI SESI 4.1 - MAR DR - HerydewiswahyuNo ratings yet
- 4 EsophagealSpasm BajaDocument6 pages4 EsophagealSpasm Bajakint manlangitNo ratings yet
- ConstipationDocument6 pagesConstipationاحمد محمدNo ratings yet
- Pelvic Organ ProlapseDocument9 pagesPelvic Organ ProlapseSonny Dizon PareñasNo ratings yet
- Overactivebladder 160426102342Document53 pagesOveractivebladder 160426102342Tô Hoàng DũngNo ratings yet
- Cleft Lip & Palate: Nursing Management in Children With Congenital DiseaseDocument84 pagesCleft Lip & Palate: Nursing Management in Children With Congenital DiseaseAnonymous KXYykpaZPNo ratings yet
- 4-ASKEP GI DefectDocument84 pages4-ASKEP GI DefectAnonymous KXYykpaZPNo ratings yet
- MotilityDocument77 pagesMotilityrobelNo ratings yet
- Fetal Surveillance: By: Kristine R. Niñonuevo-Dayao, M.DDocument43 pagesFetal Surveillance: By: Kristine R. Niñonuevo-Dayao, M.DSanjay Kumar SanjuNo ratings yet
- Exercise With Pre & Post Natal ClientsDocument20 pagesExercise With Pre & Post Natal ClientsDan CowenNo ratings yet
- Ocp HCTMDocument2 pagesOcp HCTMEvelyn LimNo ratings yet
- ProlapseDocument51 pagesProlapsejijaniNo ratings yet
- IncontinenceDocument9 pagesIncontinenceHanaNo ratings yet
- What Is Faecal Incontinence?Document6 pagesWhat Is Faecal Incontinence?drm1238475No ratings yet
- UV Prolapse: DR Liyana Alya & DR Afifah Supervised by DR KamaliahDocument24 pagesUV Prolapse: DR Liyana Alya & DR Afifah Supervised by DR KamaliahAfifah SelamatNo ratings yet
- 1.1 GynaecologyDocument59 pages1.1 Gynaecologyayeshafarooq60No ratings yet
- Cleft Lip & Palate: Nursing Management in Children With Congenital DiseaseDocument75 pagesCleft Lip & Palate: Nursing Management in Children With Congenital DiseaseSherly Mectildis BakerNo ratings yet
- PancreATITIS OCT. 21, 2021Document33 pagesPancreATITIS OCT. 21, 2021Alyssa NicoleNo ratings yet
- Abortion BSN 0PR-2: Case Study of BelleDocument27 pagesAbortion BSN 0PR-2: Case Study of BellekervinNo ratings yet
- NCPDocument2 pagesNCPJoanne Pascual TuasonNo ratings yet
- All About Constipation Booklet 2016 05 RevDocument4 pagesAll About Constipation Booklet 2016 05 RevHana Jao100% (1)
- Basic Concepts, Development & Classification of TheoryDocument40 pagesBasic Concepts, Development & Classification of TheoryReshmiNo ratings yet
- ConstipatiaDocument34 pagesConstipatiaMaria Traian100% (2)
- Franchie M. Hsu Case StudyDocument5 pagesFranchie M. Hsu Case StudyFranchieNo ratings yet
- Digestive System: Diagnostic Tests For Diseases of The Digestive SystemDocument14 pagesDigestive System: Diagnostic Tests For Diseases of The Digestive Systemmai-maiNo ratings yet
- No-Risk Abs: A Safe Workout Program for Core StrengthFrom EverandNo-Risk Abs: A Safe Workout Program for Core StrengthNo ratings yet
- Incontinence a Time to Heal with Yoga and Acupressure: A Six Week Exercise Program for People with Simple Stress Urinary IncontinenceFrom EverandIncontinence a Time to Heal with Yoga and Acupressure: A Six Week Exercise Program for People with Simple Stress Urinary IncontinenceNo ratings yet
- Leica Rm2125rts Ifu 2v8l enDocument68 pagesLeica Rm2125rts Ifu 2v8l enNguyen Trung HuyNo ratings yet
- Cold Work PermitDocument1 pageCold Work PermitРудик НикитаNo ratings yet
- Laporan PDM 20 NovemberDocument21 pagesLaporan PDM 20 NovemberdeokNo ratings yet
- Injury PreventionDocument16 pagesInjury PreventionSim BuenNo ratings yet
- Nursing Care Plans: Assessment Nursing Diagnosis Planning Implementation Rationale EvaluationDocument2 pagesNursing Care Plans: Assessment Nursing Diagnosis Planning Implementation Rationale EvaluationRheeanne Mae Amilasan100% (1)
- 1st Periodical Test in Beauty Care 10 - Wellness MasssageDocument2 pages1st Periodical Test in Beauty Care 10 - Wellness MasssageBelinda Lapsit100% (5)
- Chili and Makabuhay Stem Extract As MolluscicideDocument27 pagesChili and Makabuhay Stem Extract As MolluscicideQueen Ann Navallo80% (10)
- Open Letter To Mayor-Elect Wu - Mass and CassDocument2 pagesOpen Letter To Mayor-Elect Wu - Mass and Cassdialynn dwyerNo ratings yet
- Instructions To The Candidate: Examination Centre: Centre Code: 2032 ID Number: Photo IDDocument1 pageInstructions To The Candidate: Examination Centre: Centre Code: 2032 ID Number: Photo IDuday xeroxNo ratings yet
- English As A Second Language: Paper 1: Reading and WritingDocument24 pagesEnglish As A Second Language: Paper 1: Reading and Writingﹺ ﹺ ﹺNo ratings yet
- Book Stress, the Psychology of Managing PressureDocument18 pagesBook Stress, the Psychology of Managing PressureNadia AdreNo ratings yet
- NCP Abruptio PlacentaDocument2 pagesNCP Abruptio PlacentaCarson Birth100% (1)
- ITR Prenatal v.3Document1 pageITR Prenatal v.3SHEBA RAE ESPERANZA100% (1)
- Cancer ScreeningDocument8 pagesCancer Screeninglakshminivas PingaliNo ratings yet
- The Influenza Pandemic of 1918 and The Current Covid 19 PandemicDocument4 pagesThe Influenza Pandemic of 1918 and The Current Covid 19 PandemicJescah JuneNo ratings yet
- Learning Activity 1 Hugo Andrez Bustos Restrepo Evidence: Regrets From The DyingDocument5 pagesLearning Activity 1 Hugo Andrez Bustos Restrepo Evidence: Regrets From The DyingAndres B RestrepoNo ratings yet
- Bi-Annual ExamDocument19 pagesBi-Annual ExamManuel Timothy Jude LoNo ratings yet
- 089 44 Final Biologi Fasa4 DLP T4-3-28Document26 pages089 44 Final Biologi Fasa4 DLP T4-3-28BF CLNo ratings yet
- Fire Drills Safety HandoutDocument2 pagesFire Drills Safety HandoutRahulPrakash100% (1)
- Questions and Answers A Guide To Fitness and Wellness 3Rd Edition Liguori Test Bank Full Chapter PDFDocument48 pagesQuestions and Answers A Guide To Fitness and Wellness 3Rd Edition Liguori Test Bank Full Chapter PDFmathewsandersa13j100% (9)
- RainforestHerbs BrochureDocument11 pagesRainforestHerbs BrochureErlena RahimNo ratings yet
- REV Skripsi LR Hubungan Pemberian ASIE DG Kejadian Stunting PD Bad YWKAe5GDocument89 pagesREV Skripsi LR Hubungan Pemberian ASIE DG Kejadian Stunting PD Bad YWKAe5GFauziyah AnnisaaNo ratings yet
- Manual de Instalación, Operación Mantenimiento de Balanza Fajas PDFDocument559 pagesManual de Instalación, Operación Mantenimiento de Balanza Fajas PDFCarlos Alberto Alvarado LoayzaNo ratings yet
- NCP Kenezo, Female 17Document2 pagesNCP Kenezo, Female 17labanesstephanyNo ratings yet
- Unit #7 - Basic Quality Control For The Clinical LaboratoryDocument28 pagesUnit #7 - Basic Quality Control For The Clinical LaboratoryFaisal JamshedNo ratings yet
- The Three Levels of Moral DilemmasDocument9 pagesThe Three Levels of Moral DilemmasVictoria AntonetteNo ratings yet
- Project Selection-Numeric ModelsDocument39 pagesProject Selection-Numeric Modelsshrutimsawant835No ratings yet
- Stressors, Affectivity, and Self - Efficacy As Predictors of Librarians' Thriving at WorkDocument12 pagesStressors, Affectivity, and Self - Efficacy As Predictors of Librarians' Thriving at WorkIOER International Multidisciplinary Research Journal ( IIMRJ)No ratings yet