Professional Documents
Culture Documents
Review Article Osteophytes
Review Article Osteophytes
Uploaded by
rroxanarrusu0 ratings0% found this document useful (0 votes)
5 views3 pagesOriginal Title
Review Article osteophytes
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
5 views3 pagesReview Article Osteophytes
Review Article Osteophytes
Uploaded by
rroxanarrusuCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 3
Review Article: Osteophytes Siu Him Janus Wong, Kwong Yuen Chiu, Chun Hoi Yan
Department of Orthopaedics & Traumatology, The University of Hong Kong, Hong
Kong ABSTRACT An osteophyte is a fibrocartilage-capped bony outgrowth that is one
of the features of osteoarthritis. This study reviewed the types, risk factors,
pathophysiology, clinical presentations, and medical and surgical treatment of
osteophytes. Extraspinal osteophytes are classified as marginal, central, periosteal, or
capsular, whereas vertebral osteophytes are classified as traction or claw. Risk factors
for development of osteophytes include age, body mass index, physical activity, and
other genetic and environmental factors. Transforming growth factor β plays a role in
the pathophysiology of osteophyte formation. Osteophytes can cause pain, limit range
of motion, affect quality of life, and cause multiple symptoms at the spine. Medical
treatment involves the use of bisphosphonates and other non-steroidal anti-
inflammatory agents. Surgical treatment in the form of cheilectomy for impingement
syndromes during joint replacement is recommended. Key words: osteophyte;
physiopathology; risk factors; treatment outcome introduction An osteophyte is one of
the features of osteoarthritis.1 This study reviewed the types, risk factors,
pathophysiology, clinical presentations, and medical and surgical treatment of
osteophytes. classification Osteophytes can be classified as extraspinal or vertebral.
According to their radiographic appearance and formation mechanism, there are 4 types
of extraspinal osteophytes.2 Marginal osteophytes arise from the periphery of joints and
appear as a ‘lip’. They are caused by endochondral ossification stimulated by
vascularisation of subchondral bone marrow.3 They are found in non-pressure segments
and thus not usually associated with significant adjacent sclerosis or subchondral cysts.
They usually predominate on one side of the joint (Fig. 1a). Central osteophytes are
projections to the interior joint space and have an irregular rough articular contour. They
are caused by hypervascularity stimulating endochondral ossification. The original
calcified cartilage demarcating the bases of button like excrescences is known as
‘reduplication’. They are most commonly found in the hips and knees (Fig. 1b).
Periosteal and synovial osteophytes appear as thickened intra-articular cortices. They
are caused by intramembranous ossification as a result of stimulation of the periosteal
and synovial membrane with appositional bone growth. Femoral neck buttressing is one
example.4 Capsular osteophytes develop as a result of capsular traction and form along
the direction of capsular tension. Bony outgrowth in the silhouette of seagull wings
(‘seagull sign’) at the interphalangeal joints is one example. Vertebral osteophytes are
classified as traction or claw.5 Traction osteophytes are horizontal bone Address
correspondence and reprint requests to: Chun Hoi Yan, Department of Orthopaedics &
Traumatology, The University of Hong Kong, Hong Kong. Email:
yanchunhoi@gmail.com 404 SHJ Wong et al. Journal of Orthopaedic Surgery
extrusions from the attachment of the outermost annulus fibrosus fibres >2 mm from the
distal edge of the vertebral body. They are a sign of instability and regress as stability
improves (Fig. 2a). Claw osteophytes are curved toward the adjacent disc (Fig. 2b) and
are more common. In 20 cadavers, no corresponding similar spur was noted at the
adjacent vertebral rim of a traction osteophyte, as would be expected if its formation
was due to instability of the intervening disc.6 Thus, both types of spinal osteophytes
are considered to be secondary to the same degenerative process rather than 2 distinct
pathologies.6 An alternative classification system categorises osteophytes into 3 types:
the real osteochondrophyte (arising in the synovium overlying bone at the junctional
zone), traction spur (at the enthesis), and inflammatory spur (e.g. syndesmophytes in
ankylosing spondylitis).7 risK factors Age is associated with higher osteophyte grade at
the lumbar spine8 and outward osteophyte size at the knee at the left medial tibia
(r=0.329, p=0.002).9 Spinal osteophytes have been reported in up to 60% of women and
80% of men aged 50 years.10 Osteophytes had been used as a forensic estimator of
age,11 but the association is insufficient to yield a predictive power beyond a general
estimate.12 Increased body mass index (BMI) and obesity are associated with larger
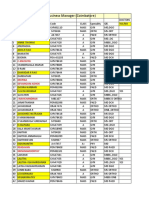
osteophytes at multiple joints. In 126 Japanese women (a) (b) Figure 1 (a) Marginal
osteophytes at the medial edge of the tibial plateau (arrow), and (b) central osteophytes
at the tibial spines (arrows). aged >60 years with back pain, the mean lumbar osteophyte
area correlated with weight (r=0.557) and BMI (r=0.486).13 In a UK study, increasing
BMI was associated with increasing frequency of osteophytes at the lumbar spine,
particularly at the dorsal aspect.8 BMI correlates with outward osteophyte size at the
lateral left femur and right tibia (r=0.329, p=0.002).9 In 51 subjects with a mean age of
60 years who exercised regularly, painless weight-bearing activity did not accelerate
osteophytosis in the knee.14 Nonetheless, in a UK study of 499 men, heavy physical
activity was associated with development of osteophytes.8 In a Japanese cross-sectional
study, occupational kneeling and squatting (defined as >1 hour per day) was associated
with increased area of femoral and tibial osteophytes.15 In a study that compared 135
young athletes with 550 controls, athletes were at higher risk of tibiofemoral
osteophytes (adjusted odds ratio [OR]=2.9, 95% confidence interval [CI]=1.6–5.4) and
notch osteophytes (adjusted OR=2.3, 95% CI=1.1 4.7).16 Prior anterior cruciate
ligament surgery increased the risk of tibiofemoral osteophytes (adjusted OR=4.8, 95%
CI=2.4–9.4).16 Dietary factors may play a role in osteophyte formation in Japanese
women (but not in men).17 The osteophyte area was associated with a low (a) (b)
Figure 2 (a) Traction osteophytes at L5 and L4 and the inferior aspect of L3 (arrows)
and claw osteophytes at the superior aspects of L3 and L2 and the inferior aspect of L1
(arrowheads), and (b) mixture of claw and traction osteophytes at the anterosuperior
aspect of L3 and anteroinferior aspect of L2 (arrows). Vol. 24 No. 3, December 2016
pathophysiology Osteophytes 405 level intake of vitamin E (regression coefficient=
−0.15, 95% CI= −0.29 to −0.008, p=0.0383), vitamin K (regression coefficient= -0.10,
95% CI= −0.18 to −0.009, p=0.0302), vitamin B1 (regression coefficient= −0.35, 95%
CI= −0.56 to −0.13, p=0.0020), vitamin B2 (regression coefficient= −0.22, 95% CI=
−0.37 to −0.08, p=0.0025), Niacin (regression coefficient= −0.18, 95% CI= −0.33 to
−0.03, p=0.0195), and vitamin B6 (regression coefficient= −0.25, 95% CI= −0.42 to
−0.07, p=0.0053).17 In a cross-sectional study of elderly people, low serum β-carotene
level was a strong risk factor for lumbar osteophyte formation (OR=6.7, 95% CI=1.39–
32.6, p=0.02).18 In a US study of 791 older community-dwelling adults, a high serum
level of dephosphorylated-uncarboxylated matrix gla protein (indicative of low vitamin
K status) was associated with higher risk of osteophyte formation (OR=1.7, 95%
CI=1.1–2.5).19 The T29→C polymorphism of the TGFβ1 gene at chromosome 19q13.1
has been shown to exhibit inverse patterns of association with genetic susceptibility to
spinal osteophytosis.20 Low birth weight was associated with development of
osteophytes at the hip (OR=1.512, 95% CI=1.14–2.00, p=0.004).21 A hostile uterine
environment may play a role, with effects mediated through the vitamin D receptor
gene.21 Race may play a role in the prevalence and distribution of osteophytes as
evidenced by differences in African and Caucasian populations.22 Osteoarthritis of the
hip is uncommon among Asians (compared to Caucasians).23 Nonetheless,
osteoarthritis of the knee is slightly more prevalent in the Beijing Osteoarthritis Study
cohort than the Framingham Osteoarthritis Study cohort; the respective radiographic
and symptomatic osteoarthritis prevalence ratios were 1.45 (95% CI=1.31–1.60) and
1.43 (95% CI=1.16–1.75) respectively.24 In a Croatian study of 543 subjects, vertebral
deformities were associated with spinal osteophytes in those aged >45 years.25
Osteophytes have been noted in young patients with adolescent idiopathic scoliosis.26
In a UK study that compared 1135 subjects with controls, high bone mineral density (Z-
score) was associated with osteophytosis (OR=2.12, 95% CI=1.61–2.79, p
You might also like
- Balneo 305Document6 pagesBalneo 305Nicoleta TudorachiNo ratings yet
- عرض تقديمي 28Document33 pagesعرض تقديمي 28saifmajidhammadiNo ratings yet
- Arthrosis of KneeDocument30 pagesArthrosis of Kneebiomechy oktomalioputriNo ratings yet
- Arthrosis of KneeDocument30 pagesArthrosis of Kneebiomechy oktomalioputriNo ratings yet
- Nms 2 - 3 - OsteoarthritisDocument52 pagesNms 2 - 3 - OsteoarthritisAngga FirmansyahNo ratings yet
- Jact13i2p154 Arya Osteoarthritis of The Knee Joint An OverviewDocument9 pagesJact13i2p154 Arya Osteoarthritis of The Knee Joint An OverviewErwynk EriantoNo ratings yet
- Osteoarthritis of The KneeDocument8 pagesOsteoarthritis of The Kneeas3syamut649250% (2)
- Pathogenesis of Osteoporosis 2: Cli Ord J. RosenDocument13 pagesPathogenesis of Osteoporosis 2: Cli Ord J. RosenRonald TejoprayitnoNo ratings yet
- Researc OrofasdialDocument18 pagesResearc OrofasdialREANANDA MUBARAK SUGIARTONo ratings yet
- Lespasio Et Al 2017 Knee Osteoarthritis A PrimerDocument7 pagesLespasio Et Al 2017 Knee Osteoarthritis A PrimerMuhammad MuktiNo ratings yet
- Knee Oa NcbiDocument7 pagesKnee Oa NcbiFitria Dewi LestariNo ratings yet
- Childhood OsteoporosisDocument16 pagesChildhood OsteoporosisSimina SerbanNo ratings yet
- 485-Article Text-605-1-10-20161227 PDFDocument10 pages485-Article Text-605-1-10-20161227 PDFJeg1No ratings yet
- Christopher W. DiGiovanni ArticleDocument10 pagesChristopher W. DiGiovanni ArticleRajiv NegandhiNo ratings yet
- Wagner2015 Article FragilityFracturesOfTheSacrumHDocument14 pagesWagner2015 Article FragilityFracturesOfTheSacrumHSandy DaengNo ratings yet
- Effects of Exercise and Physical Activity On Knee OsteoarthritisDocument9 pagesEffects of Exercise and Physical Activity On Knee OsteoarthritisJoseph LimNo ratings yet
- Osteoporosis The Evolution in DiagnosisDocument12 pagesOsteoporosis The Evolution in DiagnosisPakistan RevolutionNo ratings yet
- LID201112052004Document10 pagesLID201112052004Gia BảoNo ratings yet
- عرض تقديمي 28Document33 pagesعرض تقديمي 28saifmajidhammadiNo ratings yet
- Femoral Head Osteonecrosis Why Choose FreeDocument6 pagesFemoral Head Osteonecrosis Why Choose FreeFreestanding identificationNo ratings yet
- Sports Injuries in PediatricsDocument19 pagesSports Injuries in PediatricsmarinaNo ratings yet
- Apley OA 2Document11 pagesApley OA 2Koko AgungNo ratings yet
- West Indian Medical Journal: A Case of Pathological Rib Fractures: Focal Osteolysis or Osteoporosis?Document10 pagesWest Indian Medical Journal: A Case of Pathological Rib Fractures: Focal Osteolysis or Osteoporosis?IstianahNo ratings yet
- Bilateral OsteoarthritisDocument58 pagesBilateral OsteoarthritisMaya VilNo ratings yet
- MSK Study Schedule 2Document12 pagesMSK Study Schedule 2Aashish GiriNo ratings yet
- Lorentz On 2015Document23 pagesLorentz On 2015Sanita AurinNo ratings yet
- Example Research Paper On OsteoporosisDocument6 pagesExample Research Paper On Osteoporosisngqcodbkf100% (1)
- Osteoarthritis: in The ClinicDocument16 pagesOsteoarthritis: in The ClinicKurosaki IchigoNo ratings yet
- Exercise Interventions: Defusing The World's Osteoporosis Time BombDocument4 pagesExercise Interventions: Defusing The World's Osteoporosis Time BombTom HollandNo ratings yet
- Osteoporotic Vertebral Compression Fractures and VDocument13 pagesOsteoporotic Vertebral Compression Fractures and VChristopherLawrenceNo ratings yet
- Osteoporosis and Periodontal Disease: History and Physical ExaminationDocument15 pagesOsteoporosis and Periodontal Disease: History and Physical ExaminationYenniy IsmullahNo ratings yet
- Szulc Et Al-2006-Journal of Bone and Mineral ResearchDocument9 pagesSzulc Et Al-2006-Journal of Bone and Mineral ResearchDeyan SyambasNo ratings yet
- Chapter 13Document27 pagesChapter 13Zaky DavidiaNo ratings yet
- Avascular Necrosis: Necrosis Blood Supply JointDocument9 pagesAvascular Necrosis: Necrosis Blood Supply JointAyaba RoselynNo ratings yet
- Osteoporosis: Screening, Prevention, and ManagementDocument20 pagesOsteoporosis: Screening, Prevention, and ManagementBernardo RomeroNo ratings yet
- Relationship Between Knee and Ankle Degeneration in A Population of Organ DonorsDocument11 pagesRelationship Between Knee and Ankle Degeneration in A Population of Organ DonorsNguyễn HùngNo ratings yet
- Liu 2015Document9 pagesLiu 2015mmm.orthoNo ratings yet
- Management of Elbow Osteoarthritis: Current Concepts ReviewDocument11 pagesManagement of Elbow Osteoarthritis: Current Concepts ReviewChristopher BermeoNo ratings yet
- Tutorial 4 Bone and Joint - ANSWERSDocument9 pagesTutorial 4 Bone and Joint - ANSWERSjessjohnson1612No ratings yet
- Normal Bone Anatomy and PhysiologyDocument9 pagesNormal Bone Anatomy and PhysiologyElsa GonçalvesNo ratings yet
- 2.7.12 SpondylolisthesisDocument4 pages2.7.12 SpondylolisthesisArfadin YusufNo ratings yet
- Vertebroplasty and Kyphoplasty For The Treatment.6Document12 pagesVertebroplasty and Kyphoplasty For The Treatment.6cooperorthopaedicsNo ratings yet
- 4.2.1 Congenital ScoliosisDocument15 pages4.2.1 Congenital ScoliosisPutri AnderkaNo ratings yet
- Journal Reading: OsteoarthritisDocument37 pagesJournal Reading: OsteoarthritisSyalara FatharaniNo ratings yet
- Osteoporosis of The Vertebra and Osteochondral Remodeling of The Endplate Causes Intervertebral Disc Degeneration in Ovariectomized MiceDocument15 pagesOsteoporosis of The Vertebra and Osteochondral Remodeling of The Endplate Causes Intervertebral Disc Degeneration in Ovariectomized MicePietroNo ratings yet
- Osteoarthrosis / Osteoarthritis: Entitlement Eligibility GuidelinesDocument26 pagesOsteoarthrosis / Osteoarthritis: Entitlement Eligibility GuidelinesNinaNo ratings yet
- Pa ThoDocument1 pagePa Tho022389No ratings yet
- Oa Ar GoutDocument18 pagesOa Ar GoutnerdwaldoNo ratings yet
- Death&Birth 00Document23 pagesDeath&Birth 00kyz79No ratings yet
- Rad. Patho - Skeletal SystemDocument77 pagesRad. Patho - Skeletal SystemNikko L. Pescueso100% (1)
- Osteoporosis PHD ThesisDocument5 pagesOsteoporosis PHD Thesislizsimswashington100% (2)
- REFERAT Lumbar Compression FractureDocument25 pagesREFERAT Lumbar Compression FractureTaufik Ghockil ZlaluwNo ratings yet
- AJO Do Not Copy: Disk Degeneration in Lumbar Spine Precedes Osteoarthritic Changes in HipDocument4 pagesAJO Do Not Copy: Disk Degeneration in Lumbar Spine Precedes Osteoarthritic Changes in HipabdulfatahalhemeryNo ratings yet
- Osteoid Osteoma and Osteoblastoma of The Spine PDFDocument8 pagesOsteoid Osteoma and Osteoblastoma of The Spine PDFSuwirna AfriniNo ratings yet
- Typical Clinical Symptoms Are Pain, Particularly After ProlongedDocument12 pagesTypical Clinical Symptoms Are Pain, Particularly After Prolongedifa afifahNo ratings yet
- mjm11 1p51Document7 pagesmjm11 1p51toaldoNo ratings yet
- RRL - Scoliosis - Etiologic StudiesDocument6 pagesRRL - Scoliosis - Etiologic StudiesShao Anunciacion0% (1)
- Review Article: Aging and Osteoarthritis: An Inevitable Encounter?Document7 pagesReview Article: Aging and Osteoarthritis: An Inevitable Encounter?Iicha Phine'ToxicNo ratings yet
- Cartilage Injury of the Knee: State-of-the-Art Treatment and ControversiesFrom EverandCartilage Injury of the Knee: State-of-the-Art Treatment and ControversiesAaron J. KrychNo ratings yet
- Enfoque Inicial en ReumatologíaDocument33 pagesEnfoque Inicial en ReumatologíaLuis Alberto Romero JaimesNo ratings yet
- MonoarthritisDocument7 pagesMonoarthritisSalsa NadillaNo ratings yet
- Effectiveness of Neuromuscular Taping Application and Combination of Ultrasound Therapy Plus Exercise Therapy Protocol To Reduce Pain and Functional Disability in Elderly With Knee OsteoarthritisDocument6 pagesEffectiveness of Neuromuscular Taping Application and Combination of Ultrasound Therapy Plus Exercise Therapy Protocol To Reduce Pain and Functional Disability in Elderly With Knee OsteoarthritisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Jurnal - PPT Total Hip ReplacementsDocument11 pagesJurnal - PPT Total Hip ReplacementsEric GibsonNo ratings yet
- Your Hip - A Guide For Patients (Corin LTD)Document28 pagesYour Hip - A Guide For Patients (Corin LTD)BlingBling1972No ratings yet
- Role of Janu Basti and Nadi Swedana in Janu Sandhigata Vata Osteoarthritis of Knee Joint A Single Case StudyDocument5 pagesRole of Janu Basti and Nadi Swedana in Janu Sandhigata Vata Osteoarthritis of Knee Joint A Single Case StudyAbhishek Kumar DubeyNo ratings yet
- Switchwords For Aches and Pain Removal (Have A Painless Life) PDFDocument4 pagesSwitchwords For Aches and Pain Removal (Have A Painless Life) PDFMustafa AliNo ratings yet
- Osteoarthritis 191016103144Document49 pagesOsteoarthritis 191016103144dr.abouzaid098No ratings yet
- Comparison of Clinic-And Home-Based Rehabilitation Programs After Total Knee ArthroplastyDocument10 pagesComparison of Clinic-And Home-Based Rehabilitation Programs After Total Knee ArthroplastyKaribeños San JavierNo ratings yet
- Boswellia SerrataDocument5 pagesBoswellia Serrataluis fazendaNo ratings yet
- Writing Subtest For NursingDocument4 pagesWriting Subtest For NursingDC BranchNo ratings yet
- How Magnetic Therapy & Negative Ion Technology Can Aid Well-Being & Exercise RecoveryDocument9 pagesHow Magnetic Therapy & Negative Ion Technology Can Aid Well-Being & Exercise RecoveryDilpreet SinghNo ratings yet
- Physiotherapy For Musculoskeletal Conditions: More Difficult Than Rocket ScienceDocument8 pagesPhysiotherapy For Musculoskeletal Conditions: More Difficult Than Rocket ScienceBenny WirawanNo ratings yet
- Readers Digest Asia - June July 2024Document116 pagesReaders Digest Asia - June July 2024ketziabrendakpNo ratings yet
- Jur 1Document5 pagesJur 1Yusti sriwulandariNo ratings yet
- Lovesick Janice KiecoltDocument27 pagesLovesick Janice Kiecoltximena sanchezNo ratings yet
- Boron and Medical HealthDocument40 pagesBoron and Medical Healthvavacane100% (1)
- Update On The Clinical Pharmacology of Etoricoxib A Potent Cyclooxygenase2 InhibitorDocument21 pagesUpdate On The Clinical Pharmacology of Etoricoxib A Potent Cyclooxygenase2 InhibitorAnh Quoc LeNo ratings yet
- Patologi Tulang Dan SendiDocument79 pagesPatologi Tulang Dan SendiDio Reynaldi SusantoNo ratings yet
- 2006 Consensus Agreement On The Design and Conduct of Clinical Studies With Low-Level Laser Therapy and Light Therapy For Musculoskeletal Pain and DisordersDocument2 pages2006 Consensus Agreement On The Design and Conduct of Clinical Studies With Low-Level Laser Therapy and Light Therapy For Musculoskeletal Pain and DisordersDetian WangNo ratings yet
- Senior Citizen's Day - 21 August 2023Document5 pagesSenior Citizen's Day - 21 August 2023Times MediaNo ratings yet
- 2033 Rheumatoid Arthritis 14-1 PDFDocument48 pages2033 Rheumatoid Arthritis 14-1 PDFAfif Al FatihNo ratings yet
- Coimbatore Hussain New Candidates DatasDocument34 pagesCoimbatore Hussain New Candidates DatasNarasimman NarayananNo ratings yet
- Thesis PDFDocument113 pagesThesis PDFDivya ThomasNo ratings yet
- Homotoxicologia Ejercicios ClinicosDocument70 pagesHomotoxicologia Ejercicios ClinicosCelia SteimanNo ratings yet
- Musculoskeletal ICD-10-CM Coding Tip Sheet: Overview of Key Chapter 13 UpdatesDocument3 pagesMusculoskeletal ICD-10-CM Coding Tip Sheet: Overview of Key Chapter 13 UpdatesAneez Malik100% (1)
- Dr. Abdul Rashad Senior Lecturer DPT, Mphill (Opt) Mppta United College of Physical TherapyDocument32 pagesDr. Abdul Rashad Senior Lecturer DPT, Mphill (Opt) Mppta United College of Physical Therapypasha100% (1)
- Rehab September 2023Document8 pagesRehab September 2023Faeyz OrabiNo ratings yet
- Effect of Foot Strengthening Exercises in Osteoarthritis KneeDocument5 pagesEffect of Foot Strengthening Exercises in Osteoarthritis KneefiaNo ratings yet
- Nonsurgical ManagementDocument11 pagesNonsurgical ManagementAlinaNo ratings yet