Professional Documents
Culture Documents
Hipertensi Glaukoma
Hipertensi Glaukoma
Uploaded by
Cherry LilacCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hipertensi Glaukoma
Hipertensi Glaukoma
Uploaded by
Cherry LilacCopyright:
Available Formats
Increased Risks of Open-Angle Glaucoma in
Untreated Hypertension
JIHEI SARA LEE1, YONG JOON KIM1, SUNYEUP KIM, HYOUNG WON BAE, SUNG SOO KIM,
SEUNG WON LEE2, AND CHAN YUN KIM2
G
• PURPOSE: Hypertension (HTN) has been associated laucoma is one of the leading causes of
with open-angle glaucoma (OAG), but whether elevated blindness worldwide.1 In addition to intraocu-
blood pressure (BP) alone is associated with OAG is un- lar pressure (IOP),2 other additional pathogenic
known. Whether stage 1 hypertension, as per the 2017 mechanisms have been suggested as risk factors for the
American College of Cardiology/American Heart Asso- development and progression of open-angle glaucoma
ciation (ACC/AHA) BP guidelines, increases the risk of (OAG). For instance, alterations in blood flow to the op-
the disease is uncertain. tic nerve head are believed to contribute to the patho-
• DESIGN: Retrospective, observational, cohort study. genesis of the disease.3 In support of this view, numerous
• METHODS: A total of 360,330 subjects who were ≥40 large population-based studies have identified cardiovas-
years of age and not taking antihypertensive or antiglau- cular disease as 1 of the risk factors for the development
coma drugs at the time of health examinations between and progression of OAG,4-6 including systemic hyperten-
January 1, 2002, and December 31, 2003, were included. sion (HTN). Affecting at least 25% of the adult population
Subjects were categorized based on their untreated BP, worldwide,7 , 8 systemic HTN has been identified to increase
into normal BP (systolic BP [SBP] <120 and diastolic risk for OAG.4
BP [DBP] <80 mm Hg; n = 104,304), elevated BP The impact of HTN on OAG, however, is disputed be-
(SBP 120-129 and DBP <80 mm Hg; n = 33,139), cause antihypertensive medications are believed also to play
stage 1 HTN (SBP 130-139 or DBP 80-89 mm Hg; a role, whether it be through the mechanism of the medica-
n = 122,534), or stage 2 HTN (SBP ≥140 or DBP tion itself or treatment-related hypotension.9 Amid the un-
≥90mm Hg; n = 100,353). Cox regression analysis was certainty, the American College of Cardiology/American
performed to calculate hazard ratios (HR) of OAG risk. Heart Association (ACC/AHA) published, in 2017, new
• RESULTS: The mean age of the subjects was 51.17 high blood pressure (BP) guidelines, which lowered the def-
± 8.97 years, and 56.2% were male. During a mean inition of HTN.10 According to these guidelines, stage 1
follow-up period of 11.76 ± 1.37 years, 12,841 sub- HTN is either systolic BP (SBP) between 130 and 139 mm
jects (3.56%) were diagnosed with OAG. Multivariable- Hg, or diastolic BP (DBP) between 80 and 89 mm Hg. This
adjusted HRs (95% CIs) were 1.056 (0.985-1.132) for new definition has resulted in nearly half of the adult pop-
elevated BP, 1.101(1.050-1.155) for stage 1 HTN, and ulation in the United States having high BP, and stage 1
1.114(1.060-1.170) for stage 2 HTN with normal BP as HTN has been associated with significantly increased risks
the reference. for cardiovascular disease in young adults aged 20 to 39
• CONCLUSIONS: The risk for OAG becomes greater years11 ; however, its effect on the prevalence of OAG has
with increases in untreated BP. Stage 1 HTN per the not yet been thoroughly investigated. Using nationwide
2017 ACC/AHA BP guidelines is a significant risk factor health screening data from the Korean National Health In-
for OAG. (Am J Ophthalmol 2023;252: 111–120. © surance database, we sought to investigate OAG risks asso-
2023 Elsevier Inc. All rights reserved.) ciated BP unaffected by antihypertensive medication, and
to compare risks among elevated BP, stage 1 HTN, and stage
2 HTN as defined in the 2017 ACC/AHA BP guidelines.
Supplemental Material available at AJO.com.
Accepted for publication March 21, 2023.
Department of Ophthalmology, Severance Hospital, Institute of Vi-
sion Research, Yonsei University, South Korea; Department of Data Sci- METHODS
ence, Sejong University, College of Software convergence, Seoul, Korea;
Department of Precision MEdicine, Sungkyunkwan University College of
Medicine, Seoul, Korea
• DATA SOURCE: The data source has been described in
Inquiries to Chan Yun Kim, Yonsei University College of Medicine, detail in a previous study.12 Briefly, the National Health
Seoul, Korea; e-mail: kcyeye@yuhs.ac Insurance Service (NHIS) is the sole provider of health
1 Jihei Sara Lee and Yong Joon Kim equally contributed as co−first au-
care in South Korea, and more than 97% of South Koreans
thors.
a Seung Won Lee and Chan Yun Kim equally contributed to this work are currently enrolled.13 The NHIS provides general health
as co−last authors. screening to all individuals 40 years and older once every 2
0002-9394/$36.00 © 2023 ELSEVIER INC. ALL RIGHTS RESERVED. 111
https://doi.org/10.1016/j.ajo.2023.03.032
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
years, and the results are collected and available to qualified and DBP <90 mm Hg); and (8) stage 2 SDH (SBP ≥140
researchers upon request. The health screening dataset for mm Hg and DBP ≥90 mm Hg). Individuals’ status on to-
the current study comprised a 10% simple random sample bacco smoking (never, past, or current), alcohol consump-
of all South Korean adult health screening participants in tion (none, 1-2 times/wk, or ≥3 times/wk), and physical ex-
2002 and 2003 in South Korea. The cohort contained ap- ercise (none, 1-2 times/wk, or ≥3times/wk) were collected
proximately 510,000 adult NHIS beneficiaries between the from self-reports. Body mass index (BMI), serum fasting
ages of 40 and 79 years as of 2002 (http://nhiss.nhis.or.kr/bd/ glucose, and serum total cholesterol levels were obtained
ab/bdaba022Heng.do). Their health screening results and during the examinations. Prescription histories of glucose-
national insurance claims were followed up through 2015. lowering16 and lipid-lowering medications within 1 year
The cohort selection process and its profile are described before the baseline examination were obtained from the
in detail elsewhere.13 The study adhered to the Declaration claims data.
of Helsinki and all federal laws in the country. The study
protocol was approved by the Institutional Review Board • OUTCOME: The primary outcome was diagnosis of OAG,
of Yonsei University Severance Hospital (approval number which was considered to be present if both of the following
4-2022-0632). The NHIS approved the use of their data criteria were satisfied: (1) at least 2 outpatient/ambulatory
for the present study (approval number NHIS-2022-2-335). visits between 2004 and 2015 containing ICD-10 codes of
Informed consent was waived because of the retrospective OAG (H40.10x, H40.13x, and H40.19x); and (2) prescrip-
study design and de-identified and routinely collected na- tions of topical glaucoma medication at least once during
ture of the data. the same period.17 The first date on which both criteria
were satisfied was counted as the outcome. Outcomes were
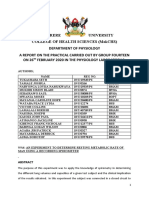
• STUDY POPULATION: The study population was selected available through December 31, 2015.
as shown in Figure 1. A total of 514,791 adults 40 years and
older underwent national health screening between January • STATISTICAL ANALYSES: Continuous data were pre-
2002 and December 2003. Subjects with missing BP data sented as mean ± SD, and categorical data were reported
were excluded (n = 334). Those with any previous hospi- as frequency and percentage. The incidence rates of OAG
tal claims of any form of glaucoma (n = 33,989) according were calculated for each BP group, and the cumulative in-
to International Classification of Diseases, 10th Revision (ICD- cidence of OAG for each BP group was estimated using the
10) coding (H40.x, H42.x, and Q15.0) before the baseline Kaplan−Meier method. The hazard ratios (HR) and 95%
examination were excluded. Those prescribed antihyper- confidence intervals (CI) for OAG events in each BP group
tensive medication in claims data prior to the baseline ex- were calculated using Cox proportional hazards models, in
amination (n = 117,343) were excluded as well. Antihy- which the normal BP group served as the reference. The
pertensive medications were identified in the claims data end of the observation was the date of the primary outcome,
according to the protocol developed by the Korean Society that is, the last follow-up or December 31, 2015, whichever
of Hypertension.14 Subjects with prior prescriptions of top- came first. The HRs were adjusted for age, sex, household
ical glaucoma medication (n = 383) and less than 1 year of income, residential area, total cholesterol, fasting glucose,
follow-up from the baseline (n = 2,412) were also excluded, lipid-lowering agents, and glucose-lowering agents, selected
leaving a final sample of 360,330 subjects for analysis. The a priori on the basis of their known associations with BP and
study protocol was adapted from the work by Lee et al.11 OAG.18 , 19
Follow-up BP measurements between 2007 and 2010
• BLOOD PRESSURE CLASSIFICATION: During the health were available in 301,408 of the subjects included in the
screening, at least 2 repeated BP measurements were taken study (Supplementary Figure 1). The 4-year follow-up pe-
by trained medical personnel in 5-minute intervals us- riod was chosen to maximize the number of individuals with
ing auscultatory or oscillometric methods.15 Subjects were follow-up BP measurements, as individuals undergo health
given a minimum of 5 minutes of rest in a seated position screenings every 2 years. The year 2010 allowed for 5 years
before the measurement. For the purpose of our analysis, the of additional follow-up within the study period after sec-
subjects were categorized into 8 mutually exclusive groups ond BP measurement. Use of antihypertensive medication
based on the BP measurements obtained from the baseline at the time of BP follow-up measurement was not an indica-
examination: (1) normal BP (SBP <120 mm Hg and DBP tion for exclusion. This subset of subjects was additionally
<80 mm Hg); (2) elevated BP (SBP 120-129 mm Hg and categorized based on changes in BP from the baseline exam-
DBP <80 mm Hg); (3) stage 1 isolated diastolic hyperten- ination (2002-2003) to the follow-up examination (2007-
sion (IDH; SBP <130 mm Hg and DBP 80-89 mm Hg); (4) 2010). For those with multiple BP measurements during the
stage 1 isolated systolic hypertension (ISH; SBP 130-139 follow-up period, the last recorded BP was used for classifi-
mm Hg and DBP <80 mm Hg); (5) stage 1 systolic and di- cation. The HR and 95% CI for OAG events for all com-
astolic hypertension (SDH; SBP 130-139 mm Hg and DBP binations of changes in BP groups were calculated. For the
80-89 mm Hg); (6) stage 2 IDH (SBP <140 mm Hg and purpose of the analysis, the stage 2 IDH, ISH, and SDH
DBP ≥90 mm Hg); (7) stage 2 ISH (SBP ≥140 mm Hg were merged into a single-stage 2 HTN group. A sensitivity
112 AMERICAN JOURNAL OF OPHTHALMOLOGY MONTH 2023
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
FIGURE 1. A flowchart of study population selection. From 514,791 subjects who underwent health examinations between January
1, 2002, and December 31, 2003, those with a previous glaucoma diagnosis (n = 33,989), previous antihypertensive medication
prescription (n = 117,343), previous glaucoma medication prescription (n = 383), and less than 1 year of follow-up (n = 2,412)
were excluded, to obtain a total of 360,330 subjects as the final study population.
analysis was conducted, in which BP measurements from having stage 1 HTN, 66,463 subjects had IDH, 13,738
2004 to 2005 were used to calculate HRs for OAG risk. had ISH, and 42,333 had SDH. As for those with stage
Statistical analyses were performed using SAS version 9.4 2 HTN, 27,388 had IDH, 23,163 had ISH, and 49,802
(SAS Institute Inc) and R version 3.5.3 (R Foundation for had SDH.
Statistical Computing).
• ASSOCIATION BETWEEN OAG RISK AND BASELINE BP:
During a mean follow-up period of 11.76 ± 1.37 years,
12,841 subjects (3.56%) were diagnosed with OAG
RESULTS (Figure 2). The OAG incidence rates per 100,000 person-
years were 251.0 for normal BP, 294.7 for elevated BP, 306.5
• BASELINE CHARACTERISTICS: A total of 360,330 sub- for stage 1 HTN, and 354.8 for stage 2 HTN (Figure 3).
jects were included in this study (51.17 ± 8.97 years, The cumulative incidence of OAG was highest in the
56.2% male) (Table 1). None of the participants were tak- stage 2 HTN group, followed by the stage 1 hyperten-
ing antihypertensive medication or IOP-lowering medica- sion group. When age, sex, household income, residential
tion at baseline. When subjects were divided by their BP area, fasting glucose, total cholesterol, and the use of lipid-
at baseline, 104,304 subjects had normal BP; 33,139 sub- lowering and glucose-lowering agents were adjusted, ele-
jects had elevated BP; 122,534 subjects had stage 1 HTN; vated BP was not associated with higher OAG risk in com-
and 100,353 subjects had stage 2 HTN. Among those parison to normal BP (Figure 3). However, stage 1 HTN
VOL. 252 GLAUCOMA AND UNTREATED BLOOD PRESSURE 113
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
114
TABLE 1. Baseline Characteristics of Study Population According to BP Groups.
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
Normal Elevated Stage 1 HTN (n=122,534) Stage 2 HTN (n=100,353)
BP BP
(n = 104,304) (n = 33,139) Stage1 IDH (n = 66,463) Stage1 ISH (n = 13,738) Stage1 SDH (n = 42,333) Stage2 IDH (n = 27,388) Stage2 ISH (n = 23,163) Stage2 SDH (n = 49,802)
Age, y, n (%)
40-49 62,298(17.29) 17,149 (4.76) 38,588(10.71) 5637 (1.56) 20,737 (5.76) 15,209 (4.22) 7087 (1.97) 19,995 (5.55)
50-59 26,663 (7.4) 8897 (2.47) 18,004 (5.00) 3807 (1.06) 12,431 (3.45) 7981 (2.21) 6563 (1.82) 15,864 (4.4)
60-69 12,292 (3.41) 5460 (1.52) 8062 (2.24) 3095 (0.86) 7266 (2.02) 3497 (0.97) 6648 (1.84) 10,573 (2.93)
70-79 2958 (0.82) 1582 (0.44) 1756 (0.49) 1156 (0.32) 1834 (0.51) 679 (0.19) 2743 (0.76) 3239 (0.90)
AMERICAN JOURNAL OF OPHTHALMOLOGY
≥80 93 (0.03) 51 (0.01) 53 (0.01) 43 (0.01) 65 (0.02) 22 (0.01) 122 (0.03) 131 (0.04)
Sex, n (%)
Male 45,528 (12.64) 17,038 ± 4.73 40,483 (11.23) 7270 (2.02) 26,429 (7.33) 19,061 (5.29) 13,068 (3.63) 33,746 (9.37)
Female 58,776(16.31) 16,101 ± 4.47 25,980 (7.21) 6468 (1.80) 15,904 (4.41) 8327 (2.31) 10,095 (2.80) 16,056 (4.46)
SBP (mm Hg) 106.40 ± 7.24 121.91 ± 2.77 118.56 ± 5.16 131.99 ± 2.76 131.38 ± 2.59 128.38 ± 5.53 145.07 ± 7.32 149.95 ± 11.71
DBP (mm Hg) 66.73 ± 5.97 70.83 ± 4.52 80.65 ± 1.77 71.72 ± 4.55 81.44 ± 2.61 90.88 ± 2.66 80.03 ± 5.45 95.05 ± 7.31
BMI (kg/m2 ) 23.01 ± 2.72 23.62 ± 2.8 23.71 ± 2.83 23.88 ± 2.85 24.10 ± 2.87 24.31 ± 2.89 24.20 ± 3.03 24.61 ± 3.04
Fasting glucose (mg/dL) 92.90 ± 28.58 96.01 ± 30.75 95.44 ± 30.77 98.68 ± 33.25 98.04 ± 32.91 97.74 ± 33.78 102.01 ± 38.43 101.70 ± 38.23
reserved.
Total cholesterol (mg/dL) 194.12 ± 36.98 197.65 ± 37.11 199.05 ± 37.4 200.04 ± 37.99 201.26 ± 38.03 202.95 ± 38.44 202.46 ± 39.32 204.97 ± 39.48
Smoking, n (%)
Never 70,748(19.63) 21,364 (5.93) 39,169(10.87) 8894 (2.47) 25,036 (6.95) 14,784 (4.10) 14,570 (4.04) 28,010 (7.77)
Former 7145 (1.98) 2592 (0.72) 6240 (1.73) 1114 (0.31) 3958 (1.10) 2957 (0.82) 1995 (0.55) 4792 (1.33)
Current 22,144 (6.15) 7890 (2.19) 18,059 (5.01) 3195 (0.89) 11,542 (3.20) 8364 (2.32) 5628 (1.56) 14,875 (4.13)
Alcohol consumption, n (%)
None 80,001 (22.2) 24,017 (6.67) 45,046 (12.5) 9690 (2.69) 27,847 (7.73) 16,674 (4.63) 15,611 (4.33) 29,305 (8.13)
1-2/wk 14,375 (3.99) 5235 (1.45) 12,515 (3.47) 2089 (0.58) 8123 (2.25) 6286 (1.74) 3741 (1.04) 10,735 (2.98)
≥3/wk 7880 (2.19) 3258 (0.90) 7684 (2.13) 1666 (0.46) 5661 (1.57) 4010 (1.11) 3315 (0.92) 9073 (2.52)
Household income, n (%)
Q1, lowest 21,329 (5.92) 7315 (2.03) 13,977 (3.88) 3297 (0.91) 9721 (2.70) 5732 (1.59) 6195 (1.72) 12,937 (3.59)
Q2-Q3 32,726 (9.08) 10,562 (2.93) 21,263 (5.9) 4646 (1.29) 14,228 (3.95) 8919 (2.48) 8269 (2.29) 17,499 (4.86)
Q4, highest 50,249(13.95) 15,262 (4.24) 31,223 (8.67) 5795 (1.61) 18,384 (5.10) 12,737 (3.53) 8699 (2.41) 19,366 (5.37)
Residence, n (%)
Metropolitan 49,492(13.74) 15,258 (4.23) 29,871 (8.29) 6062 (1.68) 19,111 (5.30) 12,519 (3.47) 9505 (2.64) 21,578 (5.99)
Rural 54,812(15.21) 17,881 (4.96) 36,592(10.16) 7676 (2.13) 23,222 (6.44) 14,869 (4.13) 13,658 (3.79) 28,224 (7.83)
Follow-up, y 11.82 ± 1.23 11.78 ± 1.36 11.79 ± 1.32 11.72 ± 1.52 11.76 ± 1.41 11.78 ± 1.36 11.69 ± 1.60 11.72 ± 1.50
BMI = body mass index; BP = blood pressure; DBP = diastolic blood pressure; HTN = hypertension; IDH = isolated diastolic hypertension; ISH = isolated systolic hypertension; SBP = systolic
MONTH 2023
blood pressure; SDH = systolic and diastolic hypertension.
Data are presented as mean ± SD or as number (percentage).
FIGURE 2. Cumulative open-angle glaucoma (OAG) incidence of BP groups by Kaplan−Meier methods. Cumulative incidence of
OAG was calculated over the follow-up period. BP = blood pressure.
FIGURE 3. Cox regression analysis of open-angle glaucoma (OAG) risks in association with baseline blood pressure (BP groups).
Cox regression model was adjusted for age, sex, household income, residential area, total cholesterol, fasting glucose, lipid-lowering
agents, and glucose-lowering agents. The incidence rates are per 100,000 person-years. HR = hazard ratio.
increased OAG risk by a factor of 1.101 (95% CI = 1.050- 1 IDH, HR = 1.088, 95% CI = 1.029-1.151; stage 1
1.155), and stage 2 HTN increased the risk by a factor ISH, HR = 1.116, 95% CI = 1.019-1.223; stage 1 SDH,
of 1.114 (95% CI = 1.060-1.170). When stages 1 and 2 HR = 1.114, 95% CI = 1.046-1.185), as well as stage 2
HTN were further divided into IDH, ISH, and SDH (Sup- SDH (HR = 1.135, 95% CI = 1.071-1.204) and stage 2
plementary Figure 1), incidence rates per 100,000 person- ISH (HR = 1.107, 95% CI = 1.030-1.190) (Supplemen-
years were 282.9 for stage 1 IDH, 367.7 for stage 1 ISH, tary Figure 2).
323.9 for stage 1 SDH, 287.3 for stage 2 IDH, 409.7 for
stage 2 ISH. and 366.7 for stage 2 SDH (Supplementary • ASSOCIATION BETWEEN OAG RISK AND STAGE 1 HTN
Figure 2). The multivariable adjustment revealed that all REVERSAL OVER TIME: Of the 360,330 subjects included
types of stage 1 HTN were significantly associated with in the study, 301,408 had undergone additional BP mea-
higher risks for OAG in comparison to normal BP (stage surements between 2007 and 2010. Of the subjects with
VOL. 252 GLAUCOMA AND UNTREATED BLOOD PRESSURE 115
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
TABLE 2. Numbers of Subjects According to BP Changes Over Time.
Baseline Follow-up Examination
Normal BP Elevated BP Stage 1 HTN Stage 2 HTN
Normal BP 46,403 (51.80) 11,276 (12.59) 25,961 (28.98) 5,938 (6.63)
Elevated BP 9,593 (34.38) 4,127 (14.79) 10,670 (38.24) 3,513 (12.59)
Stage 1 HTN 28,965 (28.13) 12,350 (11.99) 44,280 (43.00) 17,385 (16.88)
Stage 2 HTN 13,075 (16.15) 7,366 (9.10) 35,269 (43.57) 25,237 (31.18)
BP = blood pressure; HTN = hypertension.
Data are presented as number (percentage).
FIGURE 4. Cox regression analysis of open-angle glaucoma (OAG) risks in association with stage 1 hypertension (HTN) reversal
over time. Cox regression model was adjusted for age, sex, household income, residential area, total cholesterol, fasting glucose, lipid-
lowering agents, and glucose-lowering agents. Incidence rates are per 100,000 person-years. BP = blood pressure; HR = hazard
ratio.
normal BP at baseline, 51.8% (n = 46,403) maintained particular, had significantly higher risks for OAG in com-
normal BP on follow-up, and 6.63% (n = 5938) developed parison with normal BP. Stage 2 HTN, especially SDH, was
stage 2 HTN (Table 2). Among subjects with stage 1 HTN associated with greater risks for OAG in comparison to nor-
at baseline, 43.0% (n = 44,280) maintained stage 1 HTN, mal BP.
and 28.13% (n = 28,965) showed return to normal BP. We Several studies in the past have pointed to HTN as
evaluated whether normalization or reversal of stage 1 HTN an important risk factor for development and progression
over time attenuated OAG risk (Figure 4). Decreases from of OAG.4 , 6 The Blue Mountains Eye Study reported that
stage 1 to elevated BP were not associated with reduced HTN increased the risk of OAG by more than 50%, and
OAG risk. However, subjects whose BP changed from stage that a 10mm Hg increase in SBP increased the OAG
1 HTN to normal BP showed increased risks (HR = 1.183, prevalence by 10%.4 The Baltimore Eye Survey also found
95% CI = 1.043-1.342). To identify types of BP change as- an association between OAG and HTN.20 Our group
sociated with increased risk, stage 1 HTN was further di- has demonstrated similar findings in the past. A meta-
vided into ISH, IDH, and SDH (Supplementary Table 1). A analysis of population-based studies on the effect of sys-
return to normal BP from either stage 1 IDH (HR = 1.166, temic HTN on OAG estimated a pooled odds ratio of 1.22
95% CI = 1.006-1.350) or stage 1 SDH (HR = 1.258, 95% (95% CI = 1.09-1.36).6 An analysis of health screening
CI = 1.044-1.517) was associated with increased risk. data found that persons with HTN were more likely to
have OAG than those without HTN (HR = 1.16, 95%
CI = 1.09-1.24) when HTN was defined either as expo-
sure to antihypertensive medication or as BP higher than
DISCUSSION 140/80 mm Hg.12 However, reports on the association be-
tween HTN and OAG are not consistent. The relationship
In this study using nationwide health screening data of Ko- between BP and OAG were found to be not significant in a
rean adults aged 40 years or older, we evaluated risks of number of prior studies, including the Barbados Eye Study
OAG associated with untreated HTN, stratified according and the Proyecto Ver Studies.21 , 22 A negative association
to the 2017 ACC/AHA BP classification. The results in- has also been reported, whereby glaucoma risks were lower
dicated that adults with stage 1 HTN, SDH and IDH in in individuals with elevated BP.23 In 1 longitudinal study,
116 AMERICAN JOURNAL OF OPHTHALMOLOGY MONTH 2023
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
HTN reduced the risk of OAG by nearly 50% during 4 years tihypertensive medications in response to chronic increases
of follow-up.23 Currently, the relationship between BP and in BP may also be relevant to the finding. The mechanism
OAG is believe to follow a U-shape, in which both high and through which HTN affects the development and progres-
low BP are risk factors for the disease.24-26 In addition, anti- sion of OAG is likely multifactorial and evolving with time;
hypertensive medication is also suspected to contribute to further studies are necessary to discover the complex nature
the progression and development of OAG9 by inducing ex- of the relationship between the 2 diseases.
aggerated nocturnal hypotensive episodes, which compro- Increased OAG risk in individuals whose BP changed
mise blood flow to the optic nerve head. Antihypertensive from stage 1 HTN to normal range over time was rather
therapy also complicates studies on the association between surprising. In an attempt to single out subjects with in-
OAG and HTN because it is used for several medical condi- creased risk, we further divided subjects with stage 1 HTN
tions other than HTN, such as Raynaud disease, tachycar- into those with stage 1 SDH, IDH, and ISH. We found that
dia, and renal stones, just to name a few.27 In this context, normalization of stage 1 IDH and SDH were associated with
we sought to reaffirm our previous findings by investigating increased risks, whereas that of stage 1 ISH was not (Supple-
the relationship between OAG and untreated BP. mentary Figure 3). From these results, we extrapolate that
Our analysis of the relationship between untreated BP changes in DBP may possibly be associated with increased
and OAG revealed that increasing BP increased OAG risk. risk of OAG. Numerous studies have identified DBP as an
According to our results, stage 1 HTN increased OAG important factor in OAG in the past.9 , 23 , 45 , 46 The Thes-
risk by a factor of 1.101 (95% CI = 1.050-1.155). Stage saloniki Eye Study reported that DBP lower than 90 mm
2 HTN was found to increase the risk further, by a factor Hg as a result of antihypertensive treatment was associated
of 1.114 (95% CI = 1.060-1.170). Systemic BP may con- with increased cupping.9 , 45 The Barbados Eye Study23 as
tribute to the pathogenesis of glaucoma in a number of ways. well as the Rotterdam Study46 also found increased risks of
One postulated mechanism is overproduction of aqueous developing glaucoma when diastolic ocular perfusion pres-
humor, which results from elevated ciliary flow and capil- sure was low. Because low DBP is increasingly found to be
lary pressure.28 , 29 Another possible mechanism is impaired critical in OAG,34 more flexible HTN management to pos-
outflow of aqueous humor subsequent to elevated episcleral sibly aim for moderate increases in DBP has been previ-
venous pressure.30 , 31 Systemic inflammation and metabolic ously suggested.47 In light of this view, our results suggest
stress are also possible mechanisms, resulting in disrupted that increases in DBP above normal range may not neces-
axonal transport and retinal ganglion cell death.24 , 32 For sarily be protective against OAG, as none of the subjects
instance, increases in systemic pro-inflammatory cytokines who showed isolated elevation in DBP (whether it be from
such as tumor necrosis factor−α (TNF-α) have been ob- normal BP to stage 1 IDH, from elevated BP to stage 1 IDH,
served in both HTN and OAG,33-35 in association with or maintenance of stage 1 IDH) demonstrated reduced risk
vascular endothelial apoptosis36 and retinal ganglion cell for OAG. The role of DBP in glaucoma development and
death,37 respectively. Based on the results of our study, progression needs to be investigated in greater depth in the
HTN may be a risk factor for OAG independent of medical future.
therapy. Finally, the results of the present study raise a number of
The results of our investigation further indicate that stage factors to consider in the management of glaucoma patients
1 HTN may increase OAG risk through chronic and perma- in a clinical setting. First, our analysis supports prior stud-
nent damage. This is because the reversal or normalization ies that HTN is a risk factor for OAG. Second, the newly
of BP from stage 1 hypertension in the subgroup of subjects defined stage 1 HTN according to the 2017 ACC/AHA BP
with additional BP measurements was not associated with guidelines, which, prior to the update, was considered to fall
reduced risk of OAG over time. Transient acute elevations within a normal range, was associated with increased risk for
in systemic BP are believed to have little effect on blood OAG. The resultant rise in the prevalence of HTN suggests
flow to the optic nerve head under normal circumstances, as that a greater number of individuals may be at risk for glau-
autoregulatory mechanisms maintain a constant flow.38 In coma than previously believed. Finally, further investiga-
fact, acute increases in BP have been shown to protect reti- tions may be needed to clearly identify whether antihyper-
nal function against IOP elevation in rats.39 Also, in young tensive medication plays a role in the pathogenesis of OAG,
adults, HTN showed a protective effect against OAG, likely as greater proportions of patients are now recommended for
by improving ocular perfusion pressure.40 In comparison, antihypertensive treatment following the changes in the
chronic increases in systemic BP are associated with im- guidelines.
paired autoregulation41 and vascular remodeling,34 causing The limitations of the study are as follows. First, the
reduced perfusion to end-organs such as the optic nerve study population consists of Korean adults under a universal
head. Chronic damages in vascular walls in HTN, such as health insurance and screening program. Normal-tension
arteriosclerosis, and increased wall-to-lumen ratio in pre- glaucoma is more prevalent among Korean adults,19 and
capillary arterioles,42 are also visible in ocular vessels, as systemic vascular dysregulation is believed to play a more
demonstrated in reduced retinal capillary density43 and reti- important role in the pathogenesis of normal-tension glau-
nal arterial and venous narrowing.44 Subsequent use of an- coma in comparison to primary open-angle glaucoma,48 so
VOL. 252 GLAUCOMA AND UNTREATED BLOOD PRESSURE 117
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
the results may not be generalizable to other ethnic groups may have been affected by numerous means of BP modifi-
or other populations under different health care systems. cation, including lifestyle changes, antihypertensive med-
Second, the number of OAG patients might have been un- ication and dietary changes. Finally, ocular factors such
derestimated, given its asymptomatic nature in the early as IOP were not available in this administrative claims
stages. Some diagnosed OAG may have also been moni- database.
tored without medication because of low IOP. Third, sub- In conclusion, untreated stage 1 HTN as defined by the
jects’ BP in this study were the average value of multi- 2017 ACC/AHA BP guideline increased the risk of OAG
ple BP measurements during a single visit, whereas the in comparison to normal BP among adults 40 years and
2017 ACC/AHA guidelines recommend BP readings on older. OAG risk associated with untreated stage 2 HTN was
at least 2 separate visits for classification of hypertension even higher. Routine ophthalmic evaluation and screening
stage. Fourth, individuals’ BP might have been affected by may be necessary in individuals with HTN for early diagno-
“white coat syndrome.”49 Fifth, follow-up BP measurements sis of OAG.
Funding/Support: This paper was funded by the Basic Science Research Program through the National Research Foundation of Korea (No. NRF-2019
R1A2C1091089).
Financial Disclosures: The authors report no financial disclosures or conflicts of interest. All authors attest that they meet the current ICMJE criteria for
authorship.
Acknowledgments: Jihei Sara Lee and Yong Joon Kim equally contributed as co−first authors.
Seung Won Lee and Chan Yun Kim equally contributed to this work as co−last authors.
REFERENCES saloniki Eye Study. Am J Ophthalmol. 2013;155(5):843–851.
doi:10.1016/j.ajo.2012.12.007.
1. GBD 209 Blindness, Vision Impairment Collaborators. Vi- 10. Whelton PK, Carey RM, Aronow WS, et al. 2017
sion Loss Expert Group of the Global Burden of Disease ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/
Study. Causes of blindness and vision impairment in 2020 NMA/PCNA guideline for the prevention, detection,
and trends over 30 years, and prevalence of avoidable blind- evaluation, and management of high blood pressure in
ness in relation to VISION 2020: the Right to Sight: an adults: a report of the American College of Cardiol-
analysis for the Global Burden of Disease Study. Lancet Glob ogy/American Heart Association Task Force on Clinical
Health. 2021;9(2):e144–e160. doi:10.1016/S2214-109X(20) Practice Guidelines. Hypertension. 2018;71(6):e13–e115.
30489-7. doi:10.1161/HYP.0000000000000065.
2. Weinreb RN, Aung T, Medeiros FA. The pathophys- 11. Lee H, Yano Y, Cho SMJ, et al. Cardiovascular risk
iology and treatment of glaucoma: a review. JAMA. of isolated systolic or diastolic hypertension in young
2014;311(18):1901–1911. doi:10.1001/jama.2014.3192. adults. Circulation. 2020;141(22):1778–1786. doi:10.1161/
3. Flammer J, Orgul S, Costa VP, et al. The impact of ocular CIRCULATIONAHA.119.044838.
blood flow in glaucoma. Prog Retin Eye Res. 2002;21(4):359– 12. Rim TH, Lee SY, Kim SH, Kim SS, Kim CY. Increased inci-
393. doi:10.1016/s1350- 9462(02)00008- 3. dence of open-angle glaucoma among hypertensive patients:
4. Mitchell P, Lee AJ, Rochtchina E, Wang JJ. Open-angle an 11-year nationwide retrospective cohort study. J Hypertens.
glaucoma and systemic hypertension: the blue mountains 2017;35(4):729–736. doi:10.1097/HJH.0000000000001225.
eye study. J Glaucoma. 2004;13(4):319–326. doi:10.1097/ 13. Seong SC, Kim YY, Park SK, et al. Cohort profile:
00061198- 200408000- 00010. the National Health Insurance Service−National Health
5. Lee AJ, Wang JJ, Kifley A, Mitchell P. Open-angle glau- Screening Cohort (NHIS-HEALS) in Korea. BMJ Open.
coma and cardiovascular mortality: the Blue Mountains Eye 2017;7(9):e016640. doi:10.1136/bmjopen- 2017- 016640.
Study. Ophthalmology. 2006;113(7):1069–1076. doi:10.1016/ 14. Kim HC, Cho MCKorean Society of Hypertension, Hyper-
j.ophtha.2006.02.062. tension Epidemiology Research Working Group. Korea hyper-
6. Bae HW, Lee N, Lee HS, Hong S, Seong GJ, Kim CY. tension fact sheet 2018. Clin Hypertens. 2018;24:13. doi:10.
Systemic hypertension as a risk factor for open-angle glau- 1186/s40885- 018- 0098- 0.
coma: a meta-analysis of population-based studies. PLoS One. 15. Lee SW, Lee HY, Ihm SH, Park SH, Kim TH, Kim HC. Sta-
2014;9(9):e108226. doi:10.1371/journal.pone.0108226. tus of hypertension screening in the Korea National Gen-
7. Hedner T, Narkiewicz K, Kjeldsen SE. Hypertension eral Health Screening Program: a questionnaire survey on 210
control—a global challenge. Blood Press Suppl. 2005;1:4–5. screening centers in two metropolitan areas. Clin Hypertens.
doi:10.1080/08037050510034266. 2017;23:23. doi:10.1186/s40885- 017- 0075- z.
8. Kearney PM, Whelton M, Reynolds K, Muntner P, Whel- 16. Ko SH, Han K, Lee YH, et al. Past and current status of adult
ton PK, He J. Global burden of hypertension: analysis of type 2 diabetes mellitus management in Korea: a National
worldwide data. Lancet. 2005;365(9455):217–223. doi:10. Health Insurance Service database analysis. Diabetes Metab J.
1016/S0140- 6736(05)17741- 1. 2018;42(2):93–100. doi:10.4093/dmj.2018.42.2.93.
9. Topouzis F, Wilson MR, Harris A, et al. Association of open- 17. Kuang TM, Xirasagar S, Kao YW, Shia BC, Lin HC. Associa-
angle glaucoma with perfusion pressure status in the Thes- tion of Systemic hypertension with primary open-angle glau-
118 AMERICAN JOURNAL OF OPHTHALMOLOGY MONTH 2023
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
coma: a population-based case-control study. Am J Ophthal- Ophthalmol. 2007;144(3):461–462. doi:10.1016/j.ajo.2007.05.
mol. 2020;218:99–104. doi:10.1016/j.ajo.2020.04.020. 013.
18. D’Agostino Sr RB, Vasan RS, Pencina MJ, et al. General car- 32. Fechtner RD, Weinreb RN. Mechanisms of optic nerve
diovascular risk profile for use in primary care: the Framing- damage in primary open angle glaucoma. Surv Ophthalmol.
ham Heart Study. Circulation. 2008;117(6):743–753. doi:10. 1994;39(1):23–42. doi:10.1016/s0039- 6257(05)80042- 6.
1161/CIRCULATIONAHA.107.699579. 33. Bautista LE, Vera LM, Arenas IA, Gamarra G. Independent
19. Kim KE, Kim MJ, Park KH, et al. Prevalence, awareness, and association between inflammatory markers (C-reactive pro-
risk factors of primary open-angle glaucoma: Korea National tein, interleukin-6, and TNF-alpha) and essential hyperten-
Health and Nutrition Examination Survey 2008-2011. Oph- sion. J Hum Hypertens. 2005;19(2):149–154. doi:10.1038/sj.
thalmology. 2016;123(3):532–541. doi:10.1016/j.ophtha.2015. jhh.1001785.
11.004. 34. Cui YK, Pan L, Lam T, Wen CY, Do CW. Mechanistic
20. Sommer A. Glaucoma risk factors observed in the Baltimore links between systemic hypertension and open angle glau-
Eye Survey. Curr Opin Ophthalmol. 1996;7(2):93–98. doi:10. coma. Clin Exp Optom. 2022;105(4):362–371. doi:10.1080/
1097/00055735- 199604000- 00016. 08164622.2021.1964332.
21. Leske MC, Connell AM, Wu SY, Hyman LG, Schachat AP. 35. Huang P, Qi Y, Xu YS, et al. Serum cytokine alteration is as-
Risk factors for open-angle glaucoma. The Barbados Eye sociated with optic neuropathy in human primary open angle
Study. Arch Ophthalmol. 1995;113(7):918–924. doi:10.1001/ glaucoma. J Glaucoma. 2010;19(5):324–330. doi:10.1097/IJG.
archopht.1995.01100070092031. 0b013e3181b4cac7.
22. Quigley HA, West SK, Rodriguez J, Munoz B, Klein R, Sny- 36. Barbaro NR, de Araujo TM, Tanus-Santos JE, Anhe GF,
der R. The prevalence of glaucoma in a population-based Fontana V, Moreno H. Vascular damage in resistant hy-
study of Hispanic subjects: Proyecto VER. Arch Ophthal- pertension: TNF-alpha inhibition effects on endothelial
mol. 2001;119(12):1819–1826. doi:10.1001/archopht.119.12. cells. Biomed Res Int. 2015;2015:631594. doi:10.1155/2015/
1819. 631594.
23. Leske MC, Wu SY, Nemesure B, Hennis A. Incident 37. Balaiya S, Edwards J, Tillis T, Khetpal V, Chalam KV. Tumor
open-angle glaucoma and blood pressure. Arch Ophthalmol. necrosis factor-alpha (TNF-alpha) levels in aqueous humor of
2002;120(7):954–959. doi:10.1001/archopht.120.7.954. primary open angle glaucoma. Clin Ophthalmol. 2011;5:553–
24. Funk RO, Hodge DO, Kohli D, Roddy GW. Multiple Sys- 556. doi:10.2147/OPTH.S19453.
temic Vascular Risk Factors Are Associated With Low- 38. Chung HJ, Hwang HB, Lee NY. The association between
Tension Glaucoma. J Glaucoma. Jan 1 2022;31(1):15–22. primary open-angle glaucoma and blood pressure: two as-
doi:10.1097/IJG.0000000000001964. pects of hypertension and hypotension. Biomed Res Int.
25. Memarzadeh F, Ying-Lai M, Chung J, Azen SP, Varma R. 2015;2015:827516. doi:10.1155/2015/827516.
Los Angeles Latino Eye Study G. Blood pressure, perfusion 39. van Koeverden AK, He Z, Nguyen CTO, Vingrys AJ, Bui BV.
pressure, and open-angle glaucoma: the Los Angeles Latino Systemic hypertension is not protective against chronic in-
Eye Study. Invest Ophthalmol Vis Sci. 2010;51(6):2872–2877. traocular pressure elevation in a rodent model. Sci Rep.
doi:10.1167/iovs.08-2956. 2018;8(1):7107. doi:10.1038/s41598- 018- 25264- 4.
26. Zhao D, Cho J, Kim MH, Guallar E. The association of blood 40. Tielsch JM, Sommer A, Katz J, Royall RM, Quigley HA,
pressure and primary open-angle glaucoma: a meta-analysis. Javitt J. Racial variations in the prevalence of primary
Am J Ophthalmol. 2014;158(3):615–627. doi:10.1016/j.ajo. open-angle glaucoma. The Baltimore Eye Survey. JAMA.
2014.05.029. 1991;266(3):369–374.
27. Mohamed-Noriega J, Scott A, Pinto LA, Rousseau A, 41. Wong TY, Mitchell P. The eye in hypertension. Lancet.
Garway-Heath D. Writing Committee for the Inter- 2007;369(9559):425–435. doi:10.1016/S0140-6736(07)
national Glaucoma Panel. Cautious interpretation of 60198-6.
the associations between systemic hypertension, an- 42. Hayreh SS. Role of nocturnal arterial hypotension in the de-
tihypertensive medications and the risk of develop- velopment of ocular manifestations of systemic arterial hyper-
ing glaucoma. J Hypertens. 2017;35(11):2328–2329. tension. Curr Opin Ophthalmol. 1999;10(6):474–482. doi:10.
doi:10.1097/HJH.0000000000001537. 1097/00055735- 199912000- 00017.
28. Charlson ME, de Moraes CG, Link A, et al. Nocturnal sys- 43. Chua J, Chin CWL, Hong J, et al. Impact of hypertension
temic hypotension increases the risk of glaucoma progres- on retinal capillary microvasculature using optical coherence
sion. Ophthalmology. 2014;121(10):2004–2012. doi:10.1016/j. tomographic angiography. J Hypertens. 2019;37(3):572–580.
ophtha.2014.04.016. doi:10.1097/HJH.0000000000001916.
29. Hennis A, Wu SY, Nemesure B, Leske MC. Barbados Eye 44. Ikram MK, Witteman JC, Vingerling JR, Breteler MM, Hof-
Studies G. Hypertension, diabetes, and longitudinal changes man A, de Jong PT. Retinal vessel diameters and risk of hyper-
in intraocular pressure. Ophthalmology. 2003;110(5):908–914. tension: the Rotterdam Study. Hypertension. 2006;47(2):189–
doi:10.1016/S0161- 6420(03)00075- 7. 194. doi:10.1161/01.HYP.0000199104.61945.33.
30. Krasinska B, Karolczak-Kulesza M, Krasinski Z, et al. Effects 45. Harris A, Topouzis F, Wilson MR, et al. Association of the op-
of the time of antihypertensive drugs administration on the tic disc structure with the use of antihypertensive medications:
stage of primary open-angle glaucoma in patients with arterial the Thessaloniki Eye Study. J Glaucoma. 2013;22(7):526–531.
hypertension. Blood Press. 2012;21(4):240–248. doi:10.3109/ doi:10.1097/IJG.0b013e31824d1e12.
08037051.2012.666423. 46. Ramdas WD, Wolfs RC, Hofman A, de Jong PT, Vinger-
31. Xu L, Wang H, Wang Y, Jonas JB. Intraocular pressure corre- ling JR, Jansonius NM. Ocular perfusion pressure and the
lated with arterial blood pressure: the beijing eye study. Am J incidence of glaucoma: real effect or artifact? The Rotter-
VOL. 252 GLAUCOMA AND UNTREATED BLOOD PRESSURE 119
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
dam Study. Invest Ophthalmol Vis Sci. 2011;52(9):6875–6881. 48. Kaiser HJ, Flammer J, Graf T, Stumpfig D. Systemic blood
doi:10.1167/iovs.11-7376. pressure in glaucoma patients. Graefes Arch Clin Exp Ophthal-
47. Jammal AA, Berchuck SI, Mariottoni EB, Tanna AP, mol. 1993;231(12):677–680. doi:10.1007/BF00919280.
Costa VP, Medeiros FA. Blood pressure and glaucomatous 49. Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Porcellati C.
progression in a large clinical population. Ophthalmology. Prognostic significance of the white coat effect. Hypertension.
2022;129(2):161–170. doi:10.1016/j.ophtha.2021.08.021. 1997;29(6):1218–1224. doi:10.1161/01.hyp.29.6.1218.
120 AMERICAN JOURNAL OF OPHTHALMOLOGY MONTH 2023
Downloaded for dr. Cisca Kuswidyati Sp.M., M.Sc (cisca.kuswidyati@gmail.com) at Atma Jaya Catholic University of Indonesia from
ClinicalKey.com by Elsevier on July 06, 2023. For personal use only. No other uses without permission. Copyright ©2023. Elsevier Inc. All rights
reserved.
You might also like
- 2dennis - M - Marchiori Clinical ImagingDocument1,481 pages2dennis - M - Marchiori Clinical Imagingsimona mariana dutuNo ratings yet
- Guidelines For The Transport of Critically Ill PatientsDocument13 pagesGuidelines For The Transport of Critically Ill PatientsnatioclinicNo ratings yet
- Astrazeneca Strategy Is Targeted On Innovation With 3 Strategic PrioritiesDocument3 pagesAstrazeneca Strategy Is Targeted On Innovation With 3 Strategic PrioritiesAhmedAdnanNo ratings yet
- Standard Operating Procedure 180 - Missing Persons - 180-MissingpersonsDocument15 pagesStandard Operating Procedure 180 - Missing Persons - 180-MissingpersonsDisability Rights AllianceNo ratings yet
- Postgradmedj 96 525Document5 pagesPostgradmedj 96 525Huda TrisenaNo ratings yet
- CKD HT 3Document8 pagesCKD HT 3Peer TutorNo ratings yet
- J American Geriatrics Society - 2022 - Ho - Time To Benefit For Stroke Reduction After Blood Pressure Treatment in OlderDocument11 pagesJ American Geriatrics Society - 2022 - Ho - Time To Benefit For Stroke Reduction After Blood Pressure Treatment in OlderARINTA DWI KOMALANo ratings yet
- Litrev Bu2Document8 pagesLitrev Bu2Deudeu Durotun NafisahNo ratings yet
- Optimal Target Blood Pressure and Risk of Cardiovascular Disease in Low-Risk Younger Hypertensive PatientsDocument9 pagesOptimal Target Blood Pressure and Risk of Cardiovascular Disease in Low-Risk Younger Hypertensive PatientsMohit Prakash MishraNo ratings yet
- Arterial HypertensionDocument13 pagesArterial HypertensionZedodurex100% (1)
- Prevalence and Prognosis of Atrial Fibrillation in A HypertensiveDocument8 pagesPrevalence and Prognosis of Atrial Fibrillation in A HypertensiveSyadzwina Putri salsabilaNo ratings yet
- Acute HypertentionDocument9 pagesAcute HypertentionAkmal HyugaNo ratings yet
- Initiation of Antihypertensive Therapy Based On.480Document2 pagesInitiation of Antihypertensive Therapy Based On.480jackie funtanillaNo ratings yet
- 67 Ej20-0159Document9 pages67 Ej20-0159desconocido 123 ambticonNo ratings yet
- The Prevalence of ArterialDocument8 pagesThe Prevalence of ArterialInternational Medical PublisherNo ratings yet
- Controlled Level and Variability of Systolic Blood Pressure On TheDocument7 pagesControlled Level and Variability of Systolic Blood Pressure On TheJeanette LuevanosNo ratings yet
- Ibpc 13 95 PDFDocument8 pagesIbpc 13 95 PDFKevin Palma AnguloNo ratings yet
- Hansford 2021Document12 pagesHansford 2021Acilino PortelaNo ratings yet
- Seminar: EpidemiologyDocument13 pagesSeminar: EpidemiologySol LakosNo ratings yet
- Prevalence and Associated Risk Factors of HypertensionDocument10 pagesPrevalence and Associated Risk Factors of HypertensionyuliNo ratings yet
- 1 s2.0 S0165032723005931 MainDocument8 pages1 s2.0 S0165032723005931 MainjuanNo ratings yet
- Sahle 2018Document7 pagesSahle 2018Ester DuwitNo ratings yet
- The Prevalence of Resistant Hypertension Among TypDocument7 pagesThe Prevalence of Resistant Hypertension Among TypProfessor Kamel AjlouniNo ratings yet
- BPJ Vol 11 No 2 P 821-825Document5 pagesBPJ Vol 11 No 2 P 821-825hendriNo ratings yet
- Abstracts: Nephrology Dialysis TransplantationDocument1 pageAbstracts: Nephrology Dialysis TransplantationrezkyfikriNo ratings yet
- Tgs Jurnal 1Document7 pagesTgs Jurnal 1suciNo ratings yet
- Hypertensive Emergencies and Urgencies In.800Document1 pageHypertensive Emergencies and Urgencies In.800Laura J LlanoNo ratings yet
- Effect of BmiDocument5 pagesEffect of BmiSyaiful Putra RanaNo ratings yet
- The Association of Hypertension With Periodontitis Is Highlighted in Female Adults: Results From The Fourth Korea National Health and Nutrition Examination SurveyDocument8 pagesThe Association of Hypertension With Periodontitis Is Highlighted in Female Adults: Results From The Fourth Korea National Health and Nutrition Examination SurveyPentiya Vita AyuniNo ratings yet
- Assessment of Medication Adherence To JNC-7 Guidelines and Risk Factors For Hypertension in A South Indian Tertiary Care HospitalDocument12 pagesAssessment of Medication Adherence To JNC-7 Guidelines and Risk Factors For Hypertension in A South Indian Tertiary Care HospitalSophian HaryantoNo ratings yet
- Estudo CompletoDocument16 pagesEstudo CompletoRitaIvoNo ratings yet
- 533 PDFDocument11 pages533 PDFErick AlvarezNo ratings yet
- Fibrilação Atrial e AVC IsquêmicoDocument9 pagesFibrilação Atrial e AVC IsquêmicoCalouro Carlos André SoaresNo ratings yet
- ImplicationsDocument6 pagesImplicationschandra9000No ratings yet
- Kanegae 2017Document9 pagesKanegae 2017Kennard Aristo ArifinNo ratings yet
- Materials and MethodsDocument5 pagesMaterials and Methodsike ikeNo ratings yet
- Cost Effectiveness and Resource AllocationDocument7 pagesCost Effectiveness and Resource AllocationSarah AmeliaNo ratings yet
- Oup Accepted Manuscript 2020Document11 pagesOup Accepted Manuscript 2020Luis Bonino SanchezNo ratings yet
- Clinical Treatment Outcomes of Hypetensive Emergency Patients Results From The Hypertension Registry Program in Northeastern ThailandDocument7 pagesClinical Treatment Outcomes of Hypetensive Emergency Patients Results From The Hypertension Registry Program in Northeastern ThailandClaudia FreyonaNo ratings yet
- Prehypertensive State, Mild Hypertension, Metabolic Syndrome and Cardiovascular Risk Factors Among Young Adults in Rural MalaysiaDocument8 pagesPrehypertensive State, Mild Hypertension, Metabolic Syndrome and Cardiovascular Risk Factors Among Young Adults in Rural MalaysiaIndah SundariNo ratings yet
- Shaya2005 PDFDocument6 pagesShaya2005 PDFHanaNo ratings yet
- 302 Cardiovascular Risk: AssessmentDocument1 page302 Cardiovascular Risk: AssessmentLêHữuHoàiNo ratings yet
- Theassessmentandimportance Ofhypertensioninthedental SettingDocument15 pagesTheassessmentandimportance Ofhypertensioninthedental SettingAngélica Valenzuela AndrighiNo ratings yet
- Prevalence and Awareness of Hypertension Amongst Staff and Students of A Tertiary Institution in NigeriaDocument6 pagesPrevalence and Awareness of Hypertension Amongst Staff and Students of A Tertiary Institution in NigeriaAmeliaNo ratings yet
- NIH Public Access: Author ManuscriptDocument20 pagesNIH Public Access: Author ManuscriptchameleonNo ratings yet
- Jurnal HipertensiDocument5 pagesJurnal HipertensiRanhie Pen'ned CendhirhieNo ratings yet
- Ijcmr 2942Document4 pagesIjcmr 2942SintariNo ratings yet
- Common Variants at Somatostatin Are Significantly A - 2018 - Journal of The AmerDocument20 pagesCommon Variants at Somatostatin Are Significantly A - 2018 - Journal of The AmerSiti Ria RumaisaNo ratings yet
- Righi (2016)Document6 pagesRighi (2016)PelagyalNo ratings yet
- Efficacy and Safety of Chinese Herbal Medicine Xiao Yao San in 2019 PhytomeDocument13 pagesEfficacy and Safety of Chinese Herbal Medicine Xiao Yao San in 2019 PhytomeJamila IthaiaNo ratings yet
- Effectiveness of Population-Based Hypertension Screening: A Multidimensional Regression Discontinuity DesignDocument68 pagesEffectiveness of Population-Based Hypertension Screening: A Multidimensional Regression Discontinuity DesignJosé Ángel Vicente GómezNo ratings yet
- HHS Public AccessDocument18 pagesHHS Public AccesscarlosNo ratings yet
- Preventive Medicine 118 (2019) 73-80Document8 pagesPreventive Medicine 118 (2019) 73-80helioNo ratings yet
- Rule of HalfDocument4 pagesRule of HalfMuhammad Thariq IsnainiNo ratings yet
- J Jacc 2020 04 038Document10 pagesJ Jacc 2020 04 038manos iabanjiNo ratings yet
- Biomarkers in Heart FailureDocument6 pagesBiomarkers in Heart Failurekevin ortegaNo ratings yet
- Pediatric Hypertension Review of The Definition DiDocument6 pagesPediatric Hypertension Review of The Definition Dijamespalullungan120No ratings yet
- 2017-Taravatmanesh, Et Al-2017 - Determining The Factors Associated With Cardiovascular Disease Recurrence Tehran Lipid and Glucose StudyDocument7 pages2017-Taravatmanesh, Et Al-2017 - Determining The Factors Associated With Cardiovascular Disease Recurrence Tehran Lipid and Glucose Studycipto susiloNo ratings yet
- ADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged AdultsDocument11 pagesADHD Medications and Risk of Serious Cardiovascular Events in Young and Middle-Aged AdultsGary KatzNo ratings yet
- Familial Clustering of Hypertensive Target Organ Damage in The CommunityDocument8 pagesFamilial Clustering of Hypertensive Target Organ Damage in The CommunityAnisa Iswari Pombaile-NgurawanNo ratings yet
- Stage 1 Hypertension, But Not Elevated Blood Pressure, Predicts 10-Year Fatal and Non-Fatal CVD Events in Healthy Adults: The ATTICA StudyDocument11 pagesStage 1 Hypertension, But Not Elevated Blood Pressure, Predicts 10-Year Fatal and Non-Fatal CVD Events in Healthy Adults: The ATTICA StudyNaomiNo ratings yet
- The Impact of Malnutritional Status On Survival in Elderly Hemodialysis PatientsDocument5 pagesThe Impact of Malnutritional Status On Survival in Elderly Hemodialysis PatientsTika MahelsaNo ratings yet
- Cherfan 2018Document13 pagesCherfan 2018Maya ElrifaiNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 4: VascularFrom EverandComplementary and Alternative Medical Lab Testing Part 4: VascularNo ratings yet
- MEM Devices For Drug DeliveryDocument52 pagesMEM Devices For Drug DeliveryTechnautsNo ratings yet
- Seinfeld Syncope'': To The EditorDocument1 pageSeinfeld Syncope'': To The EditorJason ChambersNo ratings yet
- Annual Report of Major General John R BrookeDocument347 pagesAnnual Report of Major General John R Brookeborisernesto2002No ratings yet
- The Millerton News - January 9, 2020Document10 pagesThe Millerton News - January 9, 2020Lakeville JournalNo ratings yet
- SotDL - Monstrous Pages - Horrific ParasitesDocument6 pagesSotDL - Monstrous Pages - Horrific ParasitesjohnnyappleseedNo ratings yet
- Pathognomonic Signs of DiseasesDocument4 pagesPathognomonic Signs of DiseasesmydewyboyNo ratings yet
- Avoid Gallbladder RemovalDocument2 pagesAvoid Gallbladder RemovalRoberto DiyNo ratings yet
- HSE - Operation Controls ABE-HSE-OP-01Document6 pagesHSE - Operation Controls ABE-HSE-OP-01Faisal RazaNo ratings yet
- Brachycephalization in Japan Has CeasedDocument9 pagesBrachycephalization in Japan Has CeasedangellisimalNo ratings yet
- Semi - NCM 101 BasisDocument44 pagesSemi - NCM 101 BasischarmaineNo ratings yet
- Hubungan Berat Badan Lahir Rendah (BBLR) Dengan Kejadian Stunting Pada Anak Usia 1-3 TahunDocument6 pagesHubungan Berat Badan Lahir Rendah (BBLR) Dengan Kejadian Stunting Pada Anak Usia 1-3 TahunMusdalifa IfhaaNo ratings yet
- Introduction To Predatory LeadershipDocument14 pagesIntroduction To Predatory LeadershipMatt Kramer100% (1)
- The Contemporary Relational Supervisor 2Nd Edition Robert Ernest Lee Thorana Strever Nelson Online Ebook Texxtbook Full Chapter PDFDocument69 pagesThe Contemporary Relational Supervisor 2Nd Edition Robert Ernest Lee Thorana Strever Nelson Online Ebook Texxtbook Full Chapter PDFwilliam.roper672100% (7)
- Rebuilding The Food PyramidDocument6 pagesRebuilding The Food PyramidXenita Vera Lataza PitosNo ratings yet
- Mineral Metabolism: General FunctionsDocument12 pagesMineral Metabolism: General FunctionsibntauhidNo ratings yet
- Vaccine TextDocument2,739 pagesVaccine TextMark Mast0% (2)
- Psycho PharmaDocument8 pagesPsycho PharmaMark JosephNo ratings yet
- Depot-Ped: 3 Months: 11.25 MG or 30 MG Q12weeks. (SQ) Lupron: Children: Initially, 50Document3 pagesDepot-Ped: 3 Months: 11.25 MG or 30 MG Q12weeks. (SQ) Lupron: Children: Initially, 50thuey epeNo ratings yet
- Spirometry Report Group-14Document11 pagesSpirometry Report Group-14Mwanja MosesNo ratings yet
- The School of Salernum, Regimen Sanitatis SalernitanumDocument3 pagesThe School of Salernum, Regimen Sanitatis SalernitanumcazzoNo ratings yet
- Risk Evaluation (Refer To Evaluation Form)Document3 pagesRisk Evaluation (Refer To Evaluation Form)Parvez Taslim OfficialNo ratings yet
- April222004 On Brand SwitchingDocument44 pagesApril222004 On Brand SwitchingMona LoveNo ratings yet
- Co DiovanDocument8 pagesCo DiovanPeter Rey Tanio TeopeNo ratings yet
- Amantasan NG Ungsod NG Aynila: Intramuros, Manila College of NursingDocument3 pagesAmantasan NG Ungsod NG Aynila: Intramuros, Manila College of NursingFlorianne Khaye GonzalesNo ratings yet
- Funda Rle PrelimsDocument13 pagesFunda Rle PrelimsIvan MaximusNo ratings yet
- Tata Institute of Social Sciences, Tuljapur Campus: Final Reflexive Journal SubmissionDocument50 pagesTata Institute of Social Sciences, Tuljapur Campus: Final Reflexive Journal SubmissionDISHANT D. RATHODNo ratings yet