Professional Documents
Culture Documents
Serial Abdominal Closure With Gore Tex Mesh and
Serial Abdominal Closure With Gore Tex Mesh and
Uploaded by
Research ExpertsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Serial Abdominal Closure With Gore Tex Mesh and
Serial Abdominal Closure With Gore Tex Mesh and
Uploaded by
Research ExpertsCopyright:
Available Formats
Published online: 26.07.
2019
Case Report
Serial abdominal closure with Gore‑tex mesh and
Rives‑Stoppa for an open abdomen secondary to
intra‑abdominal hypertension in burns
R Raja Shanmugakrishnan, Charles Yuen Yung Loh, Abhijeet Wakure, Naguib El‑Muttardi
St Andrew’s Centre for Burns and Plastic Surgery, Broomfield Hospital, Chelmsford, Essex, CM1 7ET, UK
Address for correspondence: Dr. Charles Yuen Yung Loh, St Andrew’s Centre for Burns and Plastic Surgery, Broomfield Hospital, Court
Road, Chelmsford, Essex, CM1 7ET, UK. E‑mail: chloh_yy@hotmail.com
ABSTRACT
Intra‑abdominal hypertension (IAH) leading to abdominal compartment syndrome (ACS) commonly
occurs in major burns. To relieve the excess pressure, decompressive laparotomy is done which
can lead to an open abdomen. Closure of the abdomen after a decompressive laparotomy
is very difficult with bowel oedema. We describe our technique of closing the open abdomen in
such situations with a combination of serial abdominal wall closure with a layered mesh and the
Rives‑Stoppa component separation technique.
KEY WORDS
Abdominal compartment syndrome; abdominal hypertension; bogota; burn abdomen; component
separation; goretex mesh; Intra‑abdominal hypertension; mesh repair; open abdomen; postburn;
Rives‑Stoppa; PTFE mesh; polytetrafluoroethylene
INTRODUCTION fluid loss, temperature loss, desiccation of the bowels
leading to enterocutaneous fistula and loss of abdominal
I
ntra‑abdominal hypertension (IAH) domain, thus increasing the morbidity and mortality for
leading to abdominal compartment syndrome (ACS) the patient. We describe how we managed a major burn
commonly occurs in major burns due to extensive fluid with IAH and a combination of techniques for safe closure
resuscitation, thick eschars over the abdomen and sepsis.[1] of an open abdomen after the decompression of IAH.
To relieve the excess pressure, decompressive laparotomy
is done which can lead to an open abdomen. Closure of CASE REPORT
the abdomen after a decompressive laparotomy is very
difficult with bowel oedema and expedient closure A 20‑year‑old woman sustained 48% deep burns with
results in increased pressure again and multi‑organ inhalational injury while cooking. She was resuscitated,
failure. Keeping the abdomen open is fraught with
This is an open access journal, and articles are distributed under the terms of the
Creative Commons Attribution‑NonCommercial‑ShareAlike 4.0 License, which
allows others to remix, tweak, and build upon the work non‑commercially, as long as
Access this article online
appropriate credit is given and the new creations are licensed under the identical terms.
Quick Response Code:
Website:
For reprints contact: reprints@medknow.com
www.ijps.org
How to cite this article: Shanmugakrishnan RR, Yung Loh CY,
DOI: Wakure A, El-Muttardi N. Serial abdominal closure with Gore-tex
10.4103/ijps.IJPS_75_18 mesh and Rives-Stoppa for an open abdomen secondary to intra-
abdominal hypertension in burns. Indian J Plast Surg 2018;51:324-6.
© 2019 Indian Journal of Plastic Surgery | Published by Wolters Kluwer ‑ Medknow 324
Shanmugakrishnan, et al.: Serial abdominal closure with mesh and Rives‑stoppa for open abdomen
and the all deep burns were excised and allografted on muscles and fascia to the midline on either side. After
the 3rd day. She later underwent sandwich grafting on days the fascia and the skin could be approximated, a definite
6, 18 and 27 post‑burns. Most of the grafts had obtained closure was done using the Rives‑Stoppa technique. Here,
except for a few areas which healed conservatively. both the posterior rectus sheaths were brought together
She developed pain and tenderness in the right upper and sutured in the midline. A prolene mesh was placed
quadrant of her abdomen 32 days after the burn. below the rectus muscles, and the anterior rectus sheath
Contrast‑enhanced computed tomography (CECT) scan and the skin were sutured in the midline. At 1 year after
showed free fluid in the abdomen. As the pain increased, the last operation, all her wounds healed and she had no
CECT scan was repeated on day 37 post‑burns which hernia [Figure 2].
showed bowel and mesentery oedema and increased
free fluid in the abdomen. Gastroscopy and colonoscopy DISCUSSION
were not contributory. Hence, diagnostic laparoscopy was
then planned. On inserting the trocar into the abdomen, Ivy et al.[2] have noted IAH in 70% of patients with major
insufflation of pneumoperitoneum could not be done, burns. Increase in IAP occurs when there is an increased
as the intra‑abdominal pressure (IAP) was 22 mm Hg intra‑abdominal content (free fluid and bowel oedema
indicating IAH. Decompressive laparotomy was done due to inappropriate resuscitation and sepsis) and due to
immediately to prevent the ACS. Laparotomy revealed a decrease in abdominal wall compliance[3] (abdominal
bowel and mesentery oedema and an old perforation in eschars and agitation). Increase in IAP usually occurs
the stomach which was sealed by the omentum. Colonic early due to over‑resuscitation, abdominal eschars
biopsies revealed cytomegalovirus infection of the colon. and agitation. In our case, it was late due to sepsis.
The abdomen was temporarily closed by negative‑pressure The normal IAP is between sub‑atmospheric levels to
wound therapy (NPWT). Peritoneal lavage was done twice
0 mm Hg and can rise to 5–7 mm Hg in the critically
later due to persistent necrotic tissues in the abdomen.
ill. IAH is defined when there is a sustained rise in
14 days after laparotomy, the oedema settled and she was
IAP >12 mm Hg. ACS is defined as a sustained increase
considered fit for closing the abdomen. Gore‑tex mesh was
in IAP >20 mm Hg with the organ failure.[4] ACS can
sutured on the fascia both sides, pulled together (PTFE -
lead to decreased venous return and cardiac output,
polytetrafluroethylene) and sutured in the midline. NPWT
reduced blood flow to the kidneys leading to oliguria
was applied over this to approximate the wound [Figure 1].
and anuria, reduced blood flow to the bowels resulting
in increased translocation of bacteria from the gut into
The patient was taken to the theatre every week, the mesh
the blood, reduced gut motility and liver dysfunction.
was progressively approximated, and NPWT applied over
It also increases intrathoracic pressure and intracranial
this for 4 weeks. Serial weekly excision of the Gore‑tex
pressure, hypoxia and hypercarbia leading to
mesh was performed with gradual advancement of the
a b a b
c c
Figure 1: (a) Photograph of the open abdomen after release for Figure 2: (a) Serial weekly excision of Gore‑tex mesh and advancement of
intra‑abdominal hypertension. (b) Coverage of the open abdomen with a edges of muscle in keeping with the patient constitution and stability. (b) Final
sheet of Gore‑tex mesh with suturing to the edges of the separated muscle. component separation using the Rives‑Stoppa technique in combination with
(c) Application of a vacuum‑assisted closure dressing over the Gore‑tex mesh ultrapro mesh for reinforcement in a subrectus fashion with approximation of
as a temporary closure method the tissues. (c) Photograph of the abdomen at 1‑year follow‑up
325 Indian Journal of Plastic Surgery Volume 51 Issue 3 September-December 2018
Shanmugakrishnan, et al.: Serial abdominal closure with mesh and Rives‑stoppa for open abdomen
death.[5] Thus, IAP needs to be measured at least every CONCLUSION
2 h in major burns. They can be done directly by an
intra‑abdominal catheter inserted for ascites drainage, This article highlights the need to watch out for IAH and
peritoneal dialysis or laparoscopy or they can be done highlights a possible method of closing an open abdomen
indirectly through the urinary bladder, rectum and after a decompressive laparotomy for ACS after a severe
uterus. Detecting IAH necessitates treating the cause, burn.
namely, paralysing the patient with agitation, diuresis
with increased fluids, escharotomies with abdominal Declaration of patient consent
eschars and treating sepsis. When the patient is The authors certify that they have obtained all appropriate
refractory to the above treatment, decompressive patient consent forms. In the form, the patient has given her
laparotomy is done. consent for her images and other clinical information to be
reported in the journal. The patient understand that name
To prevent fluid loss, temperature loss, enterocutaneous and initial will not be published and due efforts will be made
fistula leading on to desiccation of bowels and loss of to conceal identity, but anonymity cannot be guaranteed.
abdominal domain, the abdomen needs to be closed
Financial support and sponsorship
soon. The methods to close the open abdomen can be
Nil.
broadly divided into those that do not close the fascia
and those that aim for a delayed fascial closure.[6] Conflicts of interest
The former includes NPWT, skin approximation with There are no conflicts of interest.
towel clips, allowing for granulation and grafting.
These techniques are used when the patient is in poor REFERENCES
health and aim to treat a planned ventral hernia later.
However, repair of a ventral hernia later can be difficult 1. Vertrees A, Kellicut D, Ottman S, Peoples G, Shriver C. Early
due to the retraction of the fascia and loss of tone definitive abdominal closure using serial closure technique on
injured soldiers returning from Afghanistan and Iraq. J Am Coll
of the rectus muscle. The latter techniques include Surg 2006;202:762‑72.
dynamic retention sutures, Wittmann Patch, Bogota 2. Ivy ME, Atweh NA, Palmer J, Possenti PP, Pineau M, D’Aiuto M,
bag technique and using a Gore‑tex mesh. The former et al. Intra‑abdominal hypertension and abdominal compartment
syndrome in burn patients. J Trauma 2000;49:387‑91.
techniques involve suturing material to the fascia 3. Papavramidis TS, Marinis AD, Pliakos I, Kesisoglou I,
both sides and closing progressively in the midline. Papavramidou N. Abdominal compartment syndrome – Intra‑
NPWT is usually applied over it. Dynamic retention abdominal hypertension: Defining, diagnosing, and managing.
J Emerg Trauma Shock 2011;4:279‑91.
sutures can lead to fascial necrosis.[7] Wittman patch
4. Coccolini F, Roberts D, Ansaloni L, Ivatury R, Gamberini E,
is a Velcro‑like device that can be easily closed in Kluger Y, et al. The open abdomen in trauma and non‑trauma
the middle.[8] This is quite costly and not available patients: WSES guidelines. World J Emerg Surg 2018;13:7.
5. Maerz L, Kaplan LJ. Abdominal compartment syndrome. Crit
everywhere.
Care Med 2008;36:S212‑5.
6. Boele van Hensbroek P, Wind J, Dijkgraaf MG, Busch OR,
The Bogota technique involves suturing a plastic sheet Goslings JC. Temporary closure of the open abdomen:
A systematic review on delayed primary fascial closure in patients
to the fascia and progressively closing in the midline and
with an open abdomen. World J Surg 2009;33:199‑207.
is commonly used as it is very cheap.[9] We used Gore‑tex 7. Koniaris LG, Hendrickson RJ, Drugas G, Abt P, Schoeniger LO.
mesh because it can be safely applied over the bowels Dynamic retention: A technique for closure of the complex
abdomen in critically ill patients. Arch Surg 2001;136:1359‑62.
and is stronger than the plastic sheet used in Bogota
8. Tieu BH, Cho SD, Luem N, Riha G, Mayberry J, Schreiber MA,
technique.[1] NPWT above it helps to get the skin together et al. The use of the Wittmann patch facilitates a high rate of
and eases nursing care. After the fascia comes together, fascial closure in severely injured trauma patients and critically ill
a definitive abdominal closure is done as the Gore‑tex emergency surgery patients. J Trauma 2008;65:865‑70.
9. Kirshtein B, Roy‑Shapira A, Lantsberg L, Mizrahi S. Use of the
mesh left alone will cause infection. Rives‑Stoppa “Bogota bag” for temporary abdominal closure in patients with
technique[10] is a gold standard technique for the closure secondary peritonitis. Am Surg 2007;73:249‑52.
of ventral abdominal defects. As the posterior rectus 10. Forte A, Zullino A, Manfredelli S, Montalto G, Covotta F,
Pastore P, et al. Rives technique is the gold stardard for
sheath is closed, a prolene mesh can be used instead of incisional hernioplasty. An institutional experience. Ann Ital Chir
this technique. 2011;82:313‑7.
Indian Journal of Plastic Surgery Volume 51 Issue 3 September-December 2018 326
You might also like
- MACK Truck Electrical Wiring and Connections Manual CHU, CXU, GU, TD, MRU, LR SeriesDocument94 pagesMACK Truck Electrical Wiring and Connections Manual CHU, CXU, GU, TD, MRU, LR SeriesAlex Renne Chambi100% (9)
- Rexroth Analog Positioning ModeDocument12 pagesRexroth Analog Positioning ModehfvlNo ratings yet
- ArchIntSurg8278-4967316 134753Document3 pagesArchIntSurg8278-4967316 134753puravrt40No ratings yet
- Abdoinoscrotal HydrokelDocument3 pagesAbdoinoscrotal HydrokelTiara Intan RahmawatiNo ratings yet
- Caso Hernia EstranguladaDocument4 pagesCaso Hernia EstranguladaVanesa AngelicaNo ratings yet
- Case Report On Obstructed Obturator Richter Hernia Managed by Open Preperitoneal Mesh RepairDocument7 pagesCase Report On Obstructed Obturator Richter Hernia Managed by Open Preperitoneal Mesh RepairIJAR JOURNALNo ratings yet
- Rare Sigmoid Abdominal Wall Fistula After Appendectomy: A Case ReportDocument6 pagesRare Sigmoid Abdominal Wall Fistula After Appendectomy: A Case Reportjlcano1210No ratings yet
- Management of The Open Abdomen 2018Document6 pagesManagement of The Open Abdomen 2018xcarlosfxNo ratings yet
- JournalDocument5 pagesJournalKhumaira SantaNo ratings yet
- Case Report - Nissen FundoplicationDocument4 pagesCase Report - Nissen FundoplicationArianne Kamille AndesNo ratings yet
- International Journal of Surgery Case ReportsDocument5 pagesInternational Journal of Surgery Case ReportschrisantyNo ratings yet
- Damage Control Laparotomy and Management of The Open AbdomenDocument12 pagesDamage Control Laparotomy and Management of The Open AbdomenpipeudeaNo ratings yet
- Souza 2017Document4 pagesSouza 2017CRISTHIAN CASTILLO JIBAJANo ratings yet
- Ascr 02 0170Document5 pagesAscr 02 0170Fernando HuilcaNo ratings yet
- Intra Abdominal Hypertension AND Abdominal Compartment SyndromeDocument56 pagesIntra Abdominal Hypertension AND Abdominal Compartment SyndromeAmit JaiswalNo ratings yet
- Iwj 10 138Document7 pagesIwj 10 138Carlos HernándezNo ratings yet
- Zorrilla-Nunez ProofDocument3 pagesZorrilla-Nunez ProofDr. Luis Fernando Zorrilla NúñezNo ratings yet
- 1 s2.0 S2210261221012268 MainDocument4 pages1 s2.0 S2210261221012268 Mainzenatihanen123No ratings yet
- J Ijscr 2020 10 081Document4 pagesJ Ijscr 2020 10 081Fatma BalciNo ratings yet
- Jurnal Bedah 2Document5 pagesJurnal Bedah 2nafamaulidinaNo ratings yet
- G3 IAH and ACSDocument29 pagesG3 IAH and ACSRoshin Mae E. TejeroNo ratings yet
- Post-Caesarean Rectus Sheath HaematomaDocument4 pagesPost-Caesarean Rectus Sheath HaematomatapayanaNo ratings yet
- Adhesive Intestinal Obstruction. What A Resident Should KnowDocument6 pagesAdhesive Intestinal Obstruction. What A Resident Should Knowrahul ranjanNo ratings yet
- Incisional and Laparoscopy Gastropexy For PreventiDocument7 pagesIncisional and Laparoscopy Gastropexy For PreventiAyu DinaNo ratings yet
- ESOPHAGOGASTROSTOMYDocument9 pagesESOPHAGOGASTROSTOMYdocdicNo ratings yet
- Open Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective StudyDocument3 pagesOpen Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective Study'Adil MuhammadNo ratings yet
- Laparoscopic Repair of Perforated Duodenal UlcerDocument3 pagesLaparoscopic Repair of Perforated Duodenal UlcerRoy D RogerNo ratings yet
- J Thorsurg 2018 07 001Document7 pagesJ Thorsurg 2018 07 001Gabriel RangelNo ratings yet
- SJM 812 646-649 FTDocument5 pagesSJM 812 646-649 FTreadresearchpublicationsNo ratings yet
- PRS 0000000000001135Document5 pagesPRS 0000000000001135VanessaGGSNo ratings yet
- 1 s2.0 S2210261223004741 MainDocument5 pages1 s2.0 S2210261223004741 MainDevita SanangkaNo ratings yet
- A Case Report of A Rare Presentation of Meckel's Diverticulum and Complex Abdominal Wall RepairDocument3 pagesA Case Report of A Rare Presentation of Meckel's Diverticulum and Complex Abdominal Wall RepairInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Diagnosing Gastric Volvulus in Chest X-Ray: Report of Three CasesDocument4 pagesDiagnosing Gastric Volvulus in Chest X-Ray: Report of Three CasesSuraj KurmiNo ratings yet
- Case 2Document4 pagesCase 2Malavika RaoNo ratings yet
- HerniaDocument6 pagesHerniavidro alifNo ratings yet
- Inguinal HerniaDocument9 pagesInguinal HerniaAmanda RapaNo ratings yet
- Appendiktomi Translate BookDocument19 pagesAppendiktomi Translate Bookalyntya melatiNo ratings yet
- Case Report: The Combination of Gastroschisis, Jejunal Atresia, and Colonic Atresia in A NewbornDocument5 pagesCase Report: The Combination of Gastroschisis, Jejunal Atresia, and Colonic Atresia in A NewbornAnonymous PmfX227No ratings yet
- Abdominal Cellulitis Following A Laparoscopic Procedure A Rare and Severe ComplicationDocument3 pagesAbdominal Cellulitis Following A Laparoscopic Procedure A Rare and Severe ComplicationWaqasskhanNo ratings yet
- JCDR 9 PD26Document2 pagesJCDR 9 PD26ceciliaNo ratings yet
- Ventral Hernia ThesisDocument6 pagesVentral Hernia Thesisjencloudcleveland100% (2)
- Skipidip Skipidap Colonic Hernia WoohooDocument3 pagesSkipidip Skipidap Colonic Hernia WoohooSu-sake KonichiwaNo ratings yet
- Surgical ExamDocument302 pagesSurgical ExamHossam SabriNo ratings yet
- 2021 Article 1069Document4 pages2021 Article 1069Natalindah Jokiem Woecandra T. D.No ratings yet
- Ameboma of Colon Simulating Colonic Adenocarcinoma: Case ReportDocument3 pagesAmeboma of Colon Simulating Colonic Adenocarcinoma: Case ReportJulio BarajasNo ratings yet
- InTech-Perforated AppendicitisDocument18 pagesInTech-Perforated Appendicitismelinda tannousNo ratings yet
- A Rare Mimic of Colon Cancer Ameboma 627.627Document2 pagesA Rare Mimic of Colon Cancer Ameboma 627.627Julio BarajasNo ratings yet
- Case Study (Appendicitis)Document8 pagesCase Study (Appendicitis)Jobelle AcenaNo ratings yet
- Imcrj 11 113Document4 pagesImcrj 11 113fauziyatun nNo ratings yet
- PERITONITISDocument27 pagesPERITONITISTiffany Adrias100% (1)
- Recurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Document2 pagesRecurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Motivational SpeechNo ratings yet
- 1 PBDocument6 pages1 PBrizalakbarsyaNo ratings yet
- IleostomyDocument3 pagesIleostomysgod34No ratings yet
- Umbilicalherniarepair TechniqueDocument9 pagesUmbilicalherniarepair Techniqueanz_4191No ratings yet
- 91 Clinical ScenariosDocument198 pages91 Clinical Scenarioszph7100% (1)
- Medical Surgical NursingDocument11 pagesMedical Surgical NursingJa DimasNo ratings yet
- Management of The Patient With The Open AbdomenDocument7 pagesManagement of The Patient With The Open Abdomenfabidol13No ratings yet
- Jurnal Windi 2Document6 pagesJurnal Windi 2Fiella Ardhilia NuchnumNo ratings yet
- Sabitson - Appendiks EngDocument17 pagesSabitson - Appendiks Engzeek powerNo ratings yet
- Case Report of Ectopic Hepatic Tissue, A Rare Finding DuringDocument4 pagesCase Report of Ectopic Hepatic Tissue, A Rare Finding DuringAnila CakeNo ratings yet
- Laparoscopic Cholecystectomy After Conservative Su - 2024 - International JournaDocument4 pagesLaparoscopic Cholecystectomy After Conservative Su - 2024 - International JournaRonald QuezadaNo ratings yet
- Post-cholecystectomy Bile Duct InjuryFrom EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorNo ratings yet
- Hypertonic Vs Hypotonic Vs Isotonic - Science TrendsDocument3 pagesHypertonic Vs Hypotonic Vs Isotonic - Science TrendsResearch ExpertsNo ratings yet
- Improving Isotonic Maintenance Intravenous Fluid Use in The Emergency Department - Pediatrics - American Academy of PediatricsDocument20 pagesImproving Isotonic Maintenance Intravenous Fluid Use in The Emergency Department - Pediatrics - American Academy of PediatricsResearch ExpertsNo ratings yet
- Burn Classification ArticleDocument3 pagesBurn Classification ArticleResearch ExpertsNo ratings yet
- Evaluation of The Metabolic Profile of Ringer.21Document5 pagesEvaluation of The Metabolic Profile of Ringer.21Research ExpertsNo ratings yet
- Writing Task 1 & 2Document4 pagesWriting Task 1 & 2Research ExpertsNo ratings yet
- Geh 6760Document98 pagesGeh 6760Hung NgoNo ratings yet
- Syngas TrainDocument4 pagesSyngas TrainShamshuddin TanekhanNo ratings yet
- Zxy 110 DatasheetDocument2 pagesZxy 110 DatasheetitembolehNo ratings yet
- Macquarie University:: 1.) Musec SchoolDocument6 pagesMacquarie University:: 1.) Musec SchoolUtsav ShroffNo ratings yet
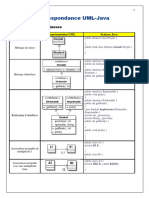
- 8 - Correspondance UML-JAVADocument3 pages8 - Correspondance UML-JAVAoussama sfiriNo ratings yet
- Lesson 10b: Aggregate Planning Finding An Optimal Production Plan Using Excel SolverDocument7 pagesLesson 10b: Aggregate Planning Finding An Optimal Production Plan Using Excel SolvervaraduNo ratings yet
- Unit of Competence:: Plan and Monitor System PilotDocument14 pagesUnit of Competence:: Plan and Monitor System PilotDo Dothings100% (2)
- Q PapersDocument53 pagesQ PapersTanu RdNo ratings yet
- UHN - Careers at UHN - Job Application PDFDocument4 pagesUHN - Careers at UHN - Job Application PDFKARTHIKEYAN ARTISTNo ratings yet
- BOMDocument1 pageBOMHytech Pvt. Ltd.No ratings yet
- Mazlan's Lecture MNE - Fire Fighting SystemDocument34 pagesMazlan's Lecture MNE - Fire Fighting SystemTuan JalaiNo ratings yet
- Samsung RF27T5501Document164 pagesSamsung RF27T5501Brian MasseyNo ratings yet
- Product Classification: SL110 Series Modular Jack, RJ45, Category 6, T568A/T568B, Unshielded, Without Dust Cover, BlackDocument2 pagesProduct Classification: SL110 Series Modular Jack, RJ45, Category 6, T568A/T568B, Unshielded, Without Dust Cover, BlackDWVIZCARRANo ratings yet
- Digital Signal Processing by Ramesh Babu PDFDocument303 pagesDigital Signal Processing by Ramesh Babu PDFJAYA CHANDRA AKULANo ratings yet
- Hypogear 85W-140 - BP Aust Pty LTDDocument4 pagesHypogear 85W-140 - BP Aust Pty LTDBiju_PottayilNo ratings yet
- Environmental Liabilities in Colombia: A Critical Review of Current Status and Challenges For A Megadiverse CountryDocument16 pagesEnvironmental Liabilities in Colombia: A Critical Review of Current Status and Challenges For A Megadiverse CountryDgo PalaciosNo ratings yet
- (CHIP IC) w25x20cl - A02Document51 pages(CHIP IC) w25x20cl - A02Felipe de san anicetoNo ratings yet
- Student Mentor RolesDocument5 pagesStudent Mentor RolesAravind MohanNo ratings yet
- BP 2009 Metro Availability PDFDocument66 pagesBP 2009 Metro Availability PDFEduardo LoureiroNo ratings yet
- 3 If D⋅∇=∈∇.Eand∇.J = σ∇.Ein a given material, the material is said to beDocument3 pages3 If D⋅∇=∈∇.Eand∇.J = σ∇.Ein a given material, the material is said to besai kumar vemparalaNo ratings yet
- Intro To Molecular BioengineeringDocument12 pagesIntro To Molecular BioengineeringjoyeesufNo ratings yet
- Portfolio AnswersDocument4 pagesPortfolio Answersa73609No ratings yet
- Trad Ic Mock ExamDocument15 pagesTrad Ic Mock ExamArvin AltamiaNo ratings yet
- A Framework For Improving Advertising Creative Using Digital MeasurementDocument15 pagesA Framework For Improving Advertising Creative Using Digital MeasurementMs Mariia MykhailenkoNo ratings yet
- Franchise Application Form: (I) APPLICANT INFORMATION (For Individuals, Please Fill in Applicable Fields)Document2 pagesFranchise Application Form: (I) APPLICANT INFORMATION (For Individuals, Please Fill in Applicable Fields)Nha Nguyen HoangNo ratings yet
- 3admin - 7Document13 pages3admin - 7JMXNo ratings yet
- 3 Odometer DisclosureDocument1 page3 Odometer DisclosureJuan Carlos MartinezNo ratings yet
- 11 SSFC PDFDocument50 pages11 SSFC PDFChaib MaamarNo ratings yet