Professional Documents
Culture Documents
CMV Review 2021
CMV Review 2021
Uploaded by
Iralda ValenciaCopyright:
Available Formats
You might also like
- Abdoul Karim Itinerary Qatar Airways Flight TicketDocument1 pageAbdoul Karim Itinerary Qatar Airways Flight TicketPeter GrayNo ratings yet
- CH371 Novel Separation ProcessDocument3 pagesCH371 Novel Separation ProcessIrfan K MoiduNo ratings yet
- BMJ n1212 FullDocument10 pagesBMJ n1212 FullRosela ObandoNo ratings yet
- 1-s2.0-S0196439923000259-CMVDocument8 pages1-s2.0-S0196439923000259-CMVaurimeryNo ratings yet
- Congenital Cytomegalovirus-HistoryDocument6 pagesCongenital Cytomegalovirus-Historydossantoselaine212No ratings yet
- NohlpsbfurnDocument17 pagesNohlpsbfurnTri Setya NNo ratings yet
- Acta Paediatrica - 2020 - Lüsebrink - Retrospectively Diagnosing Congenital Cytomegalovirus Infections in SymptomaticDocument6 pagesActa Paediatrica - 2020 - Lüsebrink - Retrospectively Diagnosing Congenital Cytomegalovirus Infections in Symptomaticdossantoselaine212No ratings yet
- Congenital Cytomegalovirus Infection: Current Strategies and Future PerspectivesDocument17 pagesCongenital Cytomegalovirus Infection: Current Strategies and Future PerspectivesAfif AriyanwarNo ratings yet
- CMV Pregnancy 20Document20 pagesCMV Pregnancy 20Татьяна ТутченкоNo ratings yet
- Prevention of Congenital Cytomegalovirus Infection With Vaccines State of The ArtDocument11 pagesPrevention of Congenital Cytomegalovirus Infection With Vaccines State of The Artmadimadi11No ratings yet
- Jurnal CMVDocument4 pagesJurnal CMVmuarifNo ratings yet
- TORCH InfectionsDocument37 pagesTORCH InfectionsEylin Halim Rahardjo100% (1)
- Maedica 15 253Document5 pagesMaedica 15 253Fer AguilarNo ratings yet
- CMV 3Document11 pagesCMV 3Birgitta IvanaNo ratings yet
- Microorganisms 09 01749Document23 pagesMicroorganisms 09 01749Ga HernandezNo ratings yet
- Infectious and Tropical Pediatric Division Department of Child Health Medical Faculty, University of Sumatera UtaraDocument33 pagesInfectious and Tropical Pediatric Division Department of Child Health Medical Faculty, University of Sumatera UtaramaruliasnaNo ratings yet
- Evidence 3) Congenital Infection Causes Neurologic and Hematologic Damage andDocument5 pagesEvidence 3) Congenital Infection Causes Neurologic and Hematologic Damage andandamar0290No ratings yet
- Cytomegalovirus Infection: Dr. Hendra Purnasidha Bagaswoto, M.SC, Sp.A SMF Anak RSUP Dr. Soeradji Tirtonegoro KlatenDocument40 pagesCytomegalovirus Infection: Dr. Hendra Purnasidha Bagaswoto, M.SC, Sp.A SMF Anak RSUP Dr. Soeradji Tirtonegoro KlatenDonniehh Assassintilldeath NothinglastforeverNo ratings yet
- Bacterial Meningitis in Infants Over 3 Months of AgeDocument8 pagesBacterial Meningitis in Infants Over 3 Months of AgedrirrazabalNo ratings yet
- Prevalence of Anti-Cytomegalovirus Anticorps in Children at The Chantal Biya Foundation Mother Child Centre, CameroonDocument6 pagesPrevalence of Anti-Cytomegalovirus Anticorps in Children at The Chantal Biya Foundation Mother Child Centre, CameroonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Congenital Cytomegalovirus Infection Clinical Features and DiagnosisDocument21 pagesCongenital Cytomegalovirus Infection Clinical Features and Diagnosisgomitas21No ratings yet
- Meningitis Pada AnakDocument14 pagesMeningitis Pada AnakRayhanun MardhatillahNo ratings yet
- Herpes Simplex Congenital Infections, Part I: Cytomegalovirus, Toxoplasma, Rubella, andDocument13 pagesHerpes Simplex Congenital Infections, Part I: Cytomegalovirus, Toxoplasma, Rubella, andSyahrialNo ratings yet
- Cytomegalovirus Infection in Pregnancy: Review of The LiteratureDocument8 pagesCytomegalovirus Infection in Pregnancy: Review of The LiteratureDewina Dyani Rosari IINo ratings yet
- Bahan Jurding Kaken 2Document7 pagesBahan Jurding Kaken 2Monica Dea RosanaNo ratings yet
- Congenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasDocument3 pagesCongenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasMinerva StanciuNo ratings yet
- Child Infection CytomegalovirusDocument19 pagesChild Infection CytomegalovirusBishnoi MaheshNo ratings yet
- Knowledge of Cytomegalovirus and Available Prevention Strategies in Pregnancy A Cross-Sectional Study in PortugalDocument8 pagesKnowledge of Cytomegalovirus and Available Prevention Strategies in Pregnancy A Cross-Sectional Study in PortugalLissaberti AmaliahNo ratings yet
- Diagnostic Challenges in Congenital Cytomegalovirus Infection in Pregnancy A Case ReportDocument6 pagesDiagnostic Challenges in Congenital Cytomegalovirus Infection in Pregnancy A Case ReportBen HonorseekerNo ratings yet
- Review CMV 2011Document8 pagesReview CMV 2011francoNo ratings yet
- Infecciones Neonatale IDocument13 pagesInfecciones Neonatale IFidel RamonNo ratings yet
- Navti 2016Document7 pagesNavti 2016XXXI-JKhusnan Mustofa GufronNo ratings yet
- Cytomegalovirus Infection in Pregnancy: A Still Complicated Diagnostic ProblemDocument9 pagesCytomegalovirus Infection in Pregnancy: A Still Complicated Diagnostic ProblemRoy GoldenNo ratings yet
- Congenital Cytomegalovirus Infection in The Absence of Maternal Cmv-Igm Antibodies: A Case ReportDocument3 pagesCongenital Cytomegalovirus Infection in The Absence of Maternal Cmv-Igm Antibodies: A Case ReportVictoria CyntiaNo ratings yet
- CMV, Tosoplasma, Rubeóla, Herpes SimpleDocument13 pagesCMV, Tosoplasma, Rubeóla, Herpes SimplePau PuenteNo ratings yet
- CMV Postnatal JurnalDocument1 pageCMV Postnatal JurnalHanifa RahmaNo ratings yet
- Congenital Cytomegalovirus Infection: Description of VirusDocument6 pagesCongenital Cytomegalovirus Infection: Description of VirusMinerva StanciuNo ratings yet
- Journal Pone 0252309Document12 pagesJournal Pone 0252309XXXI-JKhusnan Mustofa GufronNo ratings yet
- Halaman DepanDocument6 pagesHalaman DepanzakiNo ratings yet
- Cytomegalovirus Infection in Pregnancy: Infecção Pelo Citomegalovírus Na GestaçãoDocument5 pagesCytomegalovirus Infection in Pregnancy: Infecção Pelo Citomegalovírus Na GestaçãoDewina Dyani Rosari IINo ratings yet
- TORCHDocument34 pagesTORCHItzel Sarahil Rubio SotoNo ratings yet
- Torch Infections LectureDocument77 pagesTorch Infections LectureL MollyNo ratings yet
- Primer On MicrocephalyDocument10 pagesPrimer On MicrocephalylilyNo ratings yet
- 2017 Congenital Cytomegalovirus Infection in Pregnancy and The Neonate - Consensus Recommendations For Prevention, Diagnosis, and TherapyDocument9 pages2017 Congenital Cytomegalovirus Infection in Pregnancy and The Neonate - Consensus Recommendations For Prevention, Diagnosis, and TherapyValentinaNo ratings yet
- Viral Infections in Pregnant Women: Departemen Mikrobiologi Fak - Kedokteran USU MedanDocument46 pagesViral Infections in Pregnant Women: Departemen Mikrobiologi Fak - Kedokteran USU MedanSyarifah FauziahNo ratings yet
- Neonatal Sepsis 2019.Document6 pagesNeonatal Sepsis 2019.Jean Paúl LópezNo ratings yet
- Congenital and Perinatal Cytomegalovirus Infection: Chun Soo Kim, M.D., PH.DDocument7 pagesCongenital and Perinatal Cytomegalovirus Infection: Chun Soo Kim, M.D., PH.Dasri khazaliNo ratings yet
- Infections of The Fetus and NewbornDocument55 pagesInfections of The Fetus and Newbornlordoftheweb100% (4)
- Mother-To-Child Transmission of Chikungunya Virus: A Systematic Review and Meta-AnalysisDocument20 pagesMother-To-Child Transmission of Chikungunya Virus: A Systematic Review and Meta-AnalysisMarcelo QuipildorNo ratings yet
- Omphalitis: Cme R ADocument2 pagesOmphalitis: Cme R AthonjustineNo ratings yet
- Cytomegalovirus in PregnancyDocument6 pagesCytomegalovirus in PregnancyshwetaijmrNo ratings yet
- CongenitalDocument25 pagesCongenitalSUTHANNo ratings yet
- Jurnal Fixxxx 1Document14 pagesJurnal Fixxxx 1heryanggunNo ratings yet
- Neonatal SepsisDocument39 pagesNeonatal SepsisBryan KernsNo ratings yet
- Cortical Visual Impairment inDocument11 pagesCortical Visual Impairment inDwi juliana DewiNo ratings yet
- K28 A Congenital CMV KBKDocument37 pagesK28 A Congenital CMV KBKJoice RumondangNo ratings yet
- Citomegalovirus PDFDocument18 pagesCitomegalovirus PDFNADIANo ratings yet
- 2012 Number 1 947445146213461Document5 pages2012 Number 1 947445146213461MedstudNo ratings yet
- Livret MF GB21Document20 pagesLivret MF GB21mary15eugNo ratings yet
- Citomegalovirus en EmbarazoDocument8 pagesCitomegalovirus en EmbarazoJuan FranciscoNo ratings yet
- Endometrial Gene Expression: An Emerging Paradigm for Reproductive DisordersFrom EverandEndometrial Gene Expression: An Emerging Paradigm for Reproductive DisordersJoanne Kwak-KimNo ratings yet
- 1 - Pattent IDocument8 pages1 - Pattent IAmirNo ratings yet
- Icse Class X Physics Practise Sheet 1 ForceDocument3 pagesIcse Class X Physics Practise Sheet 1 ForceMehnaaz Brar100% (2)
- Week 4 - Stadelman-Cohen & Hillman (2014)Document22 pagesWeek 4 - Stadelman-Cohen & Hillman (2014)kehanNo ratings yet
- Chapter 2Document22 pagesChapter 2Abdullahi BaballoNo ratings yet
- Test BenchDocument16 pagesTest BenchAdriana VeronicaNo ratings yet
- Dell Service ManualDocument220 pagesDell Service ManualYeik ThaNo ratings yet
- Integrity Management of Safety Critical Equipment and SystemsDocument10 pagesIntegrity Management of Safety Critical Equipment and SystemsLi QiNo ratings yet
- Silage Pile Sizing Documentation 5 12 2016 3Document9 pagesSilage Pile Sizing Documentation 5 12 2016 3Zaqueu Ferreira RodriguesNo ratings yet
- The Evolution of Water Reverse Osmosis TechnologyDocument35 pagesThe Evolution of Water Reverse Osmosis TechnologyQassim LaouiraNo ratings yet
- SM DH Series ManualDocument154 pagesSM DH Series Manualkikyangello90No ratings yet
- Business Finance Test PracticeDocument49 pagesBusiness Finance Test PracticeLovan So0% (1)
- Foundations Expansive Soils: Chen CDocument6 pagesFoundations Expansive Soils: Chen CBolton Alonso Yanqui SotoNo ratings yet
- EE Syllabus PDFDocument100 pagesEE Syllabus PDFShahid LoneNo ratings yet
- Despite', in Spite Of', Although', Though' and Even Though'Document4 pagesDespite', in Spite Of', Although', Though' and Even Though'pikorl4327No ratings yet
- Full ReportDocument78 pagesFull ReportHiwot Wubetu100% (5)
- Ship SizeDocument4 pagesShip SizeBaki PınarlıNo ratings yet
- MicroPara Lecture 6Document24 pagesMicroPara Lecture 6Pearl NoconNo ratings yet
- Released FOR Manufacturing: 2509 ANTAMINA PERU SMC 100/14400 Truck Bridge Assembly Truck Bridge Steel Structure - RightDocument1 pageReleased FOR Manufacturing: 2509 ANTAMINA PERU SMC 100/14400 Truck Bridge Assembly Truck Bridge Steel Structure - RightCarlos ParedesNo ratings yet
- THE Lymphatic System & Body DefensesDocument39 pagesTHE Lymphatic System & Body DefensesSaiful AmriNo ratings yet
- Idioms For IELTS SpeakingDocument21 pagesIdioms For IELTS SpeakingРоза АсановаNo ratings yet
- Lifted 28 Days To Focus Your Mind Strengthen Your Body and Elevate Your Spiri PDFDocument276 pagesLifted 28 Days To Focus Your Mind Strengthen Your Body and Elevate Your Spiri PDFDiego100% (3)
- High Voltage Switching Operations: The Next StepDocument2 pagesHigh Voltage Switching Operations: The Next Steplenon chidzivaNo ratings yet
- Sop BM RHF Oprn ProcedureDocument2 pagesSop BM RHF Oprn ProcedurewrbmrhfispNo ratings yet
- AdulterantsDocument7 pagesAdulterantsNeeraj SharmaNo ratings yet
- Fa 5541Document46 pagesFa 5541Ricardo Nicolau WerlangNo ratings yet
- Eqpt - No. 50CH0203LC10 Fly Ash Fly Ash Material 200 T Capacity 1 No QtyDocument62 pagesEqpt - No. 50CH0203LC10 Fly Ash Fly Ash Material 200 T Capacity 1 No Qtykumar gauravNo ratings yet
- Figure 1 Concept of Structure and Function: Philippine-EagleDocument8 pagesFigure 1 Concept of Structure and Function: Philippine-EagleShekaina Faith Cuizon Lozada100% (2)
- Betag 2014Document7 pagesBetag 2014MelmakPolytronNo ratings yet
CMV Review 2021
CMV Review 2021
Uploaded by
Iralda ValenciaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CMV Review 2021
CMV Review 2021
Uploaded by
Iralda ValenciaCopyright:
Available Formats
REVIEW Journal of Bangladesh Perinatal Society
Vol. 1, No. 2, July 2020; Page 75-83
ARTICLE
Updates in Cytomegalovirus Infection in Pregnancy,
Neonates and Infancy: Diagnosis and Treatment 75
Kanij Fatema1, Md Mizanur Rahman2, Shaheen Akhter3
Vol. 1, No. 2, July 2020 BPS journal
................................................................................................................................................
1. Associate Professor, Abstract:
Department of Pediatric
Neurology Congenital cytomegalovirus infection (cCMV) is the most common congenital infection. It is an
Institute of Pediatric important cause of hearing, neurodevelopmental and visual impairment of children particularly
Neurodisorder and in developing countries. There are controversies concerning the diagnosis, treatment modalities
Autism (IPNA), of cCMV infection in infants. There is also debate in treatment of maternal CMV infection. This
Bangabandhu Sheikh
review will highlight the clinical features, investigation protocol and treatment modalities of CMV
Mujib Medical
University (BSMMU). infected neonates, infants and pregnant mothers.
2. Chairman and Most of the cCMV infected neonates are asymptomatic. Among the symptomatic patients the
Professor, important clinical features are microcephaly, hearing loss, chorioretinitis, hepatitis, petechiae etc.
Department of Pediatric Pregnant women usually present with nonspecific viral illness. Viral culture is the gold standard
Neurology
Bangabandhu Sheikh
for diagnosis but it is seldom used for diagnosis, the important investigations for detection is
Mujib Medical PCR for CMV DNA in saliva, serum, urine or CSF.
University (BSMMU). Treatment of infected pregnant mother is not widely recommended and should be individualized.
3. Professor Treatment of moderately or severely symptomatic neonate in 1st month of life with valgancyclovir
Department of Pediatric
for 6 month is widely recommended. There is evidence that public health approaches based on
Neurology
Institute of Pediatric hygiene can dramatically reduce the rate of primary maternal cytomegalovirus infections during
Neurodisorder and pregnancy.
Autism (IPNA)
Key words: congenital Cytomegalovirus (cCMV), neonates, pregnant mother
Bangabandhu Sheikh
Mujib Medical ................................................................................................................................................
University (BSMMU).
Background: congenital CMV (cCMV) infection,
shaheenk33@gmail.com
Address of Cytomegalovirus (CMV) is the most transmission through placenta can occur
Correspondence: common cause of congenital infection during any time of pregnancy. 5-8
Dr. Kanij Fatema worldwide. It is an important cause of Asymptomatic cCMV infection is
FCPS (Pediatric Neurology defined as the presence of CMV in any
and Development), FCPS hearing impairment in children. The
(Pediatrics). disease is asymptomatic in about 85 to secretion within first 3 weeks of life but
Associate Professor
90 percent cases of neonates.1 The the normal clinical, laboratory and
Department of Pediatric
imaging evaluations and symptomatic
Neurology, Institute of symptomatic cases often have signi-
Pediatric Neurodisorder cCMV infection is defined who have
ficant morbidity and mortality.2 The
and Autism (IPNA), clinically evident disease at birth.
Bangabandhu Sheikh children who survive have multiorgan
Mujib Medical University Symptomatic cCMV cases comprise
involvement most importantly neuro-
(BSMMU). only 7-10% of all infected cases.9
Mobile: 01713097751 developmental impairment, hearing
Email: and visual impairment. There are This review will highlight the clinical
mailmonami@gmail.com. features, investigation protocol and
controversies regarding the manage-
ment protocol of infected cases.3,4 treatment modalities of congenital
cytomegalovirus infected neonates,
CMV is a global infection; the infants and pregnant mothers.
prevalence of women of reproductive
age infected with CMV is about 45 to Clinical features:
90%. Transmission of CMV occurs In neonates
through body fluids namely breast CMV is now the leading nongenetic
feeding, sexual activity, blood transfusion, cause of congenital malformations.
organ transplantation and close contact. Most of the infants with cCMV are
Both the primary and secondary asymptomatic at birth. During pregnancy
infection of mother can lead to the features may be polyhydramnios,
Updates in Cytomegalovirus Infection in Pregnancy, Neonates and Infancy: Diagnosis Kanij Fatema et al.
oligohydramnios, fetal ascites, intrauterine growth • Central nervous system involvement such
restriction etc. Fetal demise may occur in utero in as microcephaly, radiographic abnormalities
the form of abortion, nonimmune hydrops, intra 76
consistent with cytomegalovirus central
uterine death or still birth. In symptomatic neonates nervous system disease (ventriculomegaly,
the presenting features are intrauterine growth
Vol. 1, No. 2, July 2020 BPS journal
intracerebral calcifications, periventricular
restriction, preterm low birth weight, hepatomegaly, echogenicity, cortical or cerebellar
splenomegaly, bleeding manifestations, jaundice, malformations), abnormal cerebrospinal
neonatal seizure, blueberry muffin spots, fluid indices for age, chorioretinitis,
microcephaly, intracranial calcification, sensorineural hearing loss, or the detection
ventriculomegaly, hearing loss, chorioretinitis, of cytomegalovirus DNA in cerebrospinal
etc.10,11 In infancy and childhood they may develop fluid
intellectual disability, hypotonia, cerebral palsy,
epilepsy, failure to thrive, behavioural disorder etc. 2. Mild symptomatic congenital cytomegalo virus
Additionally, approximately 15% of initially disease
asymptomatic CMV-infected newborns develop • Might occur with one or two isolated
long-term neurological sequelae before the age of 5 manifestations of congenital cytomegalo-
years. Central nervous system manifestations are virus infection that are mild and transient
present in about two third of infants of symptomatic (eg, mild hepatomegaly or a single
cCMV. Other less frequent features are pneumonia, measurement of low platelet count or raised
osteitis and intracranial hemorrhage.12,13 levels of alanine aminotransferase). These
Table -I: Clinical features of congenital cytomegalo virus might overlap with more severe mani-
infection.13-15 festations. However, the difference is that
they occur in isolation
• Adverse pregnancy outcomes including
stillbirth, neonatal death, intrauterine growth 3. Asymptomatic congenital cytomegalovirus
restriction and preterm birth infection with isolated sensorineural hearing loss
• Maternal pregnancy complications such as • No apparent abnormalities to suggest
preeclampsia congenital cytomegalovirus disease, but
• Fetal injury including sensorineural hearing loss (³21 decibels)
- Sensori-neural hearing loss 4. Asymptomatic congenital cytomegalovirus
- Vision loss, optic atrophy, strabismus and infection
chorioretinitis
• No apparent abnormalities to suggest
- Hepatomegaly and splenomegaly congenital cytomegalovirus disease, and
Thrombocytopenia
normal hearing
- Petechiae and jaundice
- Microcephaly, seizures and mental disability
In Pregnant women:
Table-II: Definitions of congenital cytomegalovirus
Symptoms of maternal CMV are nonspecific;
infection and disease16,17
typically there is fever, fatigue and headache. About
1. Moderate to sever symptomatic congenital 25-50% pregnant women are asymptomatic.18 Thus
cytomegalo virus disease diagnosis is challenging. Diagnosis is done by IgM
• Multiple manifestations attributable to antibody for CMV, seroconversion of previously
congenital cytomegalovirus infection: seronegative women (IgG or IgM of CMV) or low to
moderate CMV IgG avidity. When these antibodies
thrombocytopenia, petechiae, hepatomegaly,
are detected using validated assays particularly
splenomegaly, intrauterine growth
before 12–16 weeks of gestation, they indicate a
restriction, hepatitis (raised transaminases
higher risk for symptomatic congenital infection.
or bilirubin), or
Thus the consensus recommendation is that CMV
serology test should be offered to a pregnant woman
Table continued
76 Vol. 1 | No. 2 | July 2020
Updates in Cytomegalovirus Infection in Pregnancy, Neonates and Infancy: Diagnosis Kanij Fatema et al.
when she develops influenza like symptoms not but within the 1st 3 weeks of life, with saliva as the
attributable to another specific infection.19 Moreover, preferred sample.16
if the USG or MRI of fetus finding are suggestive of 77
cCMV infection, serology tests should be done.20,21 Diagnosis of maternal cytomegalovirus
infection:
Vol. 1, No. 2, July 2020 BPS journal
Transmission and risk factors for maternal CMV Routine screening of CMV of all pregnant women is
infection not recommended by national public health bodies
The infection of fetus is mainly due to the maternal in any country. However, selective testing of
primary infection. Mother usually acquires the pregnant women is done. It is here to mention that
infection from children who attend day care. Urine women who are seropositive of CMV before
or saliva of these children is the main source of pregnancy can give birth to cCMV infected infants
infection. Moreover, a seronegative mother can (non-primary maternal CMV infection). Estimates
acquire the infection from her partner by sexual suggest that more than two-thirds (about 75%) of all
intercourse or saliva. 22-25 In addition to that, the congenital cytomegalovirus cases in the USA (and
women who are seropositive before conception can by implication in other developed countries) occur
be infected again with reactivation of latent virus in infants born to women with non-primary
infection or reinfection. 26-28 cytomegalovirus infection, presumably due to
reactivation of latent virus, reinfection with a new
Diagnosis of cCMV in neonates and infants: cytomegalovirus strain, or both. Moreover, there is
The diagnosis of cCMV infection in neonate is based increasing evidence that the risk of symptomatic
on clinical features along with demonstration of the infection, especially that resulting in hearing loss, is
virus by isolation from urine, blood, saliva or CSF. similar after maternal primary or non-primary
The identification is done by detection of CMV-DNA cytomegalovirus infection. Thus there is minimal use
by polymerase chain reaction (PCR). It has high of screening of pregnant women to diagnose primary
sensitivity (>97%) and specificity (99%). 16 For CMV infection and it is not recommended by most
confirmation of cCMV it is important that virus is of the authorities. Investigation to diagnose the
detected before 3 weeks of age. In can also be infection in mother are the following:
detected by CMV IgM in blood, however, only 70% 1. IgG seroconversion (appearance of virus-specific
of cCMV infected neonates have IgM antibody at IgG in the serum of a pregnant woman who was
birth. Sensitivity of IgM CMV ELISA in relation to previously seronegative)
viral culture is 63.2% and the specificity is 85%.29 2. Presence of anti-CMV IgM and IgG antibodies,
IgG antibodies are maternally transmitted mostly.30
3. Anti-CMV IgG avidity test. Seroconversion of
The CMV-IgG avidity test is an important test which
CMV IgG between two serum samples obtained
can detect the time of primary infection. It is a
in 2-3 weeks distance provides the most reliable
measure of the binding capacity of CMV-IgG
diagnosis of primary infection. When there is
antibodies. Low avidity IgG indicates antibody- presence of CMV-IgM in blood it suggests a
production induced by acute or recent primary CMV recent or ongoing infection, however it has a low
infection, whereas high avidity IgG indicates no specificity.16,36,37,38
current or recent primary infection. But this test is
unavailable in most of the laboratories.31-33 Role of other modalities of investigations in
diagnosis:
However, the gold standard for the diagnosis of
Neuroimaging is an important mode of diagnosis of
congenital CMV infection in newborns has
cCMV. In CT brain the changes are as follows:
traditionally been viral culture of urine or saliva
intracranial calcifications, white matter low density
specimens. But this method is expensive and
regions, ventriculomegaly, cerebral atrophy,
laborious, and, even with use of rapid culture assays, neuronal migration disorders. Calcification is the
results may be delayed several days. Thus it is not most frequent feature here, the calcification is
practiced widely.34 In this respect, the consensus particularly thick and chunky in germinal matrix and
recommendation is that the diagnosis of cCMV periventricular regions with faint and punctate basal
infection in neonates should include real-time PCR ganglia calcifications. In MRI the features are
of saliva, urine, or both, as soon as possible after birth ventriculomegaly, hydrocephalus, delayed
Vol. 1 | No. 2 | July 2020 77
Updates in Cytomegalovirus Infection in Pregnancy, Neonates and Infancy: Diagnosis Kanij Fatema et al.
Table-III: Diagnostic methods available for the diagnosis of maternal, fetal and neonatal CMV infection.35
Type of patient Diagnostic method Comments 78
Maternal infection 1. IgG seroconversion Two consecutive maternal blood
(appearance of virus- samples need to be collected 2-3 weeks
Vol. 1, No. 2, July 2020 BPS journal
specific IgG in the serum apart. IgM can be detected in:
of a pregnant woman who • reactivations or reinfections;
was previously • until more than one year after
seronegative) CMV primary infection;
• interference due to
2. Presence of anti-CMV rheumatoid factor of the IgM
IgM and IgG antibodies class or cellular antigen;
• false positive during other
3. Anti-CMV IgG avidity viral infections (B19 Virus,
test Epstein Barr Virus, etc.).
Low avidity means recent maternal
infection, but threshold differs
between virological methods.
Fetal infection Amniocentesis to assess • Perform the test after the 21st
the presence of CMV by week of gestation and after 5-6
PCR weeks from the estimated
onset of infection.
• Indications are: woman with
compatible clinical signs of
primary CMV infection;
compatible ultrasound
abnormalities; serologic
suspicion of a recent maternal
infection.
Neonatal infection Culture or CMV-DNA If infection is confirmed, classify as
testing by PCR in urine, symptomatic or asymptomatic and
blood, throat and CSF. follow-up at 1, 3, 6 and 12 months and
annually until school age in order to
detect sequelae with delayed onset.
myelination, periventricular and temporal pole cysts, loss at 6 years is 15.4%. SNHL is the most frequent
migrational abnormalities like lissencephaly, long-term consequence and is not manifested
pachygyria, cortical dysplasia, polymicrogyria, invariably at birth or in the neonatal period. Thus
schizencephaly etc.39 (Figure 1, B, C) formal audiological and visual assessment should be
done in all patients of cCMV. 40,41
Ophthalmological evaluation is important in cCMV
infected cases. The ophthalmological features are Treatment of cCMV infected neonates
cortical visual impairment, strabismus, optic atrophy, Most of the researchers suggest treatment with
chorioretinal patch, retinal detachment, nystagmus, antiviral to moderate and severe symptomatic cCMV
refractive error. Ophthalmological manifestations are infected neonates. Breastfeeding is encouraged.42
not progressive. (Figure 1, D) However, progressive However, some authors suggest treatment in the
hearing loss is common in symptomatic cCMV. The following cases:
prevalence of Sensory neural hearing loss (SNHL) 1. Evidence of central nervous system
caused by cCMV infection (symptomatic and involvement, including SNHL and develo-
asymptomatic) at birth is 5.2% and late-onset hearing pmental delay.
78 Vol. 1 | No. 2 | July 2020
Updates in Cytomegalovirus Infection in Pregnancy, Neonates and Infancy: Diagnosis Kanij Fatema et al.
79
Vol. 1, No. 2, July 2020 BPS journal
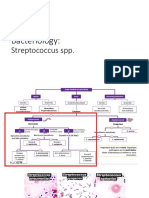
Fig.-1: A. Microcephaly in a cCMV infected infant; B. CT scan of brain showing calcification in the periventricular
areas; C. CT scan of brain showing lissencephaly and agyria (neuronal migration defect ) in cCMV infected case; D.
Chorioretinitis of cCMV infection.
2. Chorioretinitis (virus clearance 93% in VGCV and 80% in GCV
treated infants). Although the side effects of GCV
3. Critically ill preterm infant with life threatening
treated infants were more that the VGCV treated
CMV infection manifested by pneumonitis,
infants. Here treatment was given for a period of 6
hepatitis or encephalitis.43 Timing of treatment weeks in both groups.
is very important. Most of the authorities suggest
tostart the treatment within first month of life.16 Currently VGCV is the drug of choice by most of the
However, in some studies treatment was researchers. The dose of VGCV is 16mg/kg/dose 12
hourly. Based upon the fact that infants with cCMV
commenced beyond one month, up to 1 year of
demonstrates prolonged viral shedding and delayed
age.43
or progressive sequelae, recent recommendations are
Among currently available antivirals, intravenous in support of longer duration of treatment. The
ganciclovir (GCV) and oral valganciclovir (VGCV) collaborative antiviral study group (CASG)
have been studied for the treatment of infants with conducted a randomized, placebo-controlled trial
cCMV infection. Result from a study done by Kanij comparing 6 week oral VGCV therapy with 6 month
et al.44 showed that there was no statistical difference VGCV therapy in cCMV infants. There was
in virus clearance in VGCV and GCV treated infants improved outcome of hearing and neuro-
Vol. 1 | No. 2 | July 2020 79
Updates in Cytomegalovirus Infection in Pregnancy, Neonates and Infancy: Diagnosis Kanij Fatema et al.
developmental parameters in 6 month group.17 Treatment of pregnant mother, intervention to treat
Prolonged VGCV treatment was associated with fetal CMV:
neutropenia, although the incidence was markedly Currently there is no approved treatment for fetal 80
lower than previously observed with intravenous CMV infection. Several studies have been done on
GCV. Thus, VGCV treatment for 6 months is CMV Human immunoglobulin (HIG) and antivirals
Vol. 1, No. 2, July 2020 BPS journal
recommended for congenitally infected neonates. (VGCV) to pregnant women with primary CMV
Currently, there is no definitive evidence about the infection. But no randomized, placebo-controlled
potential benefit of antiviral for treatment of mildly clinical trials have established the efficacy of
symptomatic or asymptomatic infants with isolated potential prenatal treatments for fetal CMV infection.
sensorineural hearing loss, so they should not Thus antenatal treatment is not widely
routinely be given antiviral therapy.16,17,44 recommended. If treatment is recommended to a
patient, it should be accompanied by forthright
VGCV and GCV provides similar systemic exposure.
explanation regarding the level of certainty (or
Dose of GCV is 5-6 mg/kg/dose 12 hourly. GCV is uncertainty) of benefit or adverse effects. Some
associated with a number of drug toxicities. The experts recommend that such interventions be
adverse effects are myelosuppression (such a confined to clinical trials and is individualized.
granulocytopenia, anemia, thrombocytopenia) , Further study in this field is needed.49,50
raised liver enzymes, hypokalemia and renal
impairment. For GCV-induced neutropenia, it has Prevention of infection of pregnant mother:
been demonstrated that Granulocyte Colony Preventing CMV infections in pregnant women is
Stimulating Factor could be used to increase the an important public health concern. Till date no CMV
absolute neutrophil count, while continuing long- vaccine is in practice. Two important form of
term GCV therapy. Another challenge is maintaining exposure is contact with young children and sexual
the intravenous access. All these side effects are contact. Avoiding both the modalities are difficult.
reversible after stopping the drug for 3-7 days or Thus only way of prevention is to maintain proper
decreasing the dose of the drug.35 Toxicity of VGCV hygiene by regular hand washing, particularly after
is similar to that of GCV. About 38% of the patients changing diapers. Hygiene education of mother
develop neutropenia in VGCV treated cases while plays important role. Studies of hygiene education
63% of that of GCV treated cases.45 to decrease maternal CMV infection rates during
pregnancy have had promising results. In one study
Table-IV: Hygiene precautions and behavioural there was a statistically significant decrease in CMV
interventions that could prevent cytomegalovirus infection rate from 42% to 6% when women who
infection in pregnant women. 46-48 were pregnant got hygiene education. The
information can be given by video, in writing,
1. Do not share food, drinks, or utensils used by pictorial teaching, demonstrations to group etc. 46-48
young children
Follow up cCMV infected neonates:
2. Do not put a child’s dummy/soother/pacifier It is important to identify all infants with cCMV
in your mouth infection so that appropriate developmental
3. Avoid contact with saliva when kissing a child interventions and long-term follow-up can be
established. Once diagnosed they should be tested
4. Thoroughly wash hands with soap and water for hearing impairment every 6 months for 3 years
for 15–20 seconds, especially after changing and then yearly for at least 1-2 years. The
nappies/ diapers, feeding a young child, or interventions suggested are physical therapy,
wiping a young child’s nose or saliva occupational therapy, hearing aids, cochlear implants
5. Other precautions that can be considered, but according to the problem status. 17
are likely to less frequently prevent infection,
Conclusion:
include clean toys, countertops, and other
Cytomegalovirus remains the major infectious cause
surfaces that come into contact with children’s
of fetus and infants. This review summarizes the
urine or saliva, and not sharing a toothbrush
clinical features, diagnosis, treatment protocol of
with a young child.
cCMV infected fetus and infants along with pregnant
80 Vol. 1 | No. 2 | July 2020
Updates in Cytomegalovirus Infection in Pregnancy, Neonates and Infancy: Diagnosis Kanij Fatema et al.
mothers with updated information. It may thus help infections during pregnancy: description and
to develop a protocol to manage pregnant women outcome. Prenat. Diagn. 2013 ;33(8):751-58.
with infection, manage fetus and infants with 3. Kylat RI, Kelly EN, Ford-Jones EL. Clinical findings and 81
congenitally acquired infection and thus prevent the adverse outcome in neonates with symptomatic congenital
cytomegalovirus (SCCMV) infection. Eur. J. Pediatr.
sequelae of this infection particularly hearing and
Vol. 1, No. 2, July 2020 BPS journal
2006 ;165(11):773-78.
neurodevelopmental deficit.
4. Boppana SB, Pass RF, Britt WJ, Stagno S, Alford CA.
Table-V: Recommended treatment regimen and Symptomatic congenital cytomegalovirus infection:
monitoring of the congenitally cytomegalovirus-infected neonatal morbidity and mortality. Pediatr.
neonate.16 Infect. Dis. J. 1992;11(2):93-99.
5. Manicklal S, Emery VC, Lazzarotto T, Boppana SB, Gupta
1. Who to treat RK. The ‘‘silent’’ global burden of congenital
cytomegalovirus. Clin Microbiol Rev 2013; 26: 86–102.
• Neonates with moderately to severely
symptomatic congenital cytomegalovirus 6. Cannon MJ, Schmid DS , Hyde TB. Review of
disease cytomegalovirus seroprevalence and demographic
characteristics associated with infection. Rev Med Virol
2. When to treat 2010; 20: 202–213.
• Within the first month of life 7. Basha J, Iwasenko JM, Robertson P, Craig ME, Raslinson
WD. Congenital cytomegalovirus infection is associated
3. What to treat with with high maternal socio-economic status and
corresponding low maternal cytomegalovirus seropositivity.
• Oral valganciclovir 16 mg/kg per dose
J Paediatr Child Health 2014; 50: 368–372.
orally, twice a day
8. Hyde TB, Schmid DS , Cannon MJ. Cytomegalovirus
4. How long to treat seroconversion rates and risk factors: implications for
congenital CMV. Rev Med Virol 2010; 20: 311–326.
• Treatment duration for the goal of
improving audiological or developmental 9. Conboy TJ, Pass RF, Stagno S, Alford CA, Myers GJ, Britt
WJ, et al. Early clinical manifestations and intellectual
outcomes should not exceed 6 months
outcome in children with symptomatic congenital
5. Monitoring during treatment cytomegalovirus infection. J Peds 1987; 111: 343-48.
• Absolute neutrophil counts should be 10. Boppana SB, Fowler KB, Britt WJ, Stagno S, Pass RF.
Symptomatic congenital cytomegalovirus infection in
followed weekly for 6 weeks, then at week
infants born to mothers with preexisting immunity to
8, then monthly for the duration of therapy cytomegalovirus. Pediatrics 1999; 104 :55–60.
• Levels of transaminases should be followed 11. Ross SA, Fowler KB, Ashrith G, Stagno S, Britt WJ, Pass
monthly throughout therapy RF, et al. Hearing loss in children with congenital
cytomegalovirus infection born to mothers with preexisting
6. Follow up -An ophthalmological examination immunity. J Pediatr 2006; 148:332–336.
should be done early in the course of treatment, 12. Dahl HH, Ching TY, Hutchison W, Hou S, Seeto M, Sjahalam-
with follow-up eye examinations as suggested King J. Etiology and audiological outcomes at 3 years for
by the ophthalmologist -Audiological testing 364 children in Australia. PLoS One 2013; 8: e59624 .
should be done at 6-month intervals for the first 13. Dollard SC, Grosse SD, Ross DS. New estimates of the
3 years of life, and annually thereafter through prevalence of neurological and sensory sequelae and
adolescence (ages 10–19). mortality associated with congenital cytomegalovirus
infection. Rev Med Virol 2007; 17: 355–63.
- Developmental assessments beginning at
14. Iwasenko JM, Howard J, Arbuckle S, Graf N, Hall B, Craig
the first year of life might be helpful in some ME, et al. Human cytomegalovirus infection is detected
children with symptomatic congenital frequently in stillbirths and is associated with fetal
cytomegalovirus disease, and should be thrombotic vasculopathy. J Infect Dis 2011; 203: 1526–33.
employed on a case-by-case basis 15. Pereira L, Petitt M, Fong A, Tsuge M, Tabata T, Fang-Hoover
J et al. Intrauterine growth restriction caused by underlying
Reference: congenital cytomegalovirus infection. J Infect Dis 2014; 10:
1. Lazzarotto T, Guerra B, Gabrielli L, Lanari M, Landini MP. 1573–84.
Update on the prevention, diagnosis and management of 16. Rawlinson WD, Boppana SB, Fowler KB, Kimberlin DW ,
cytomegalovirus infection during pregnancy. Clin. Lazzarotto T, Alain S et al. Congenital cytomegalovirus
Microbiol. Infect. 2011 ;17(9):1285-93. infection in pregnancy and the neonate: consensus
2. Picone O, Vauloup-Fellous C, Cordier AG, Guitton S, Senat recommendations for prevention, diagnosis, and therapy.
MV, Fuchs F et al. A series of 238 cytomegalovirus primary Lancet Infect Dis. 2017 ;17(6):e177-e188.
Vol. 1 | No. 2 | July 2020 81
Updates in Cytomegalovirus Infection in Pregnancy, Neonates and Infancy: Diagnosis Kanij Fatema et al.
17. Kimberlin DW, Jester PM, Sanchez PJ, Ahmed A, Arav- of recent primary human cytomegalovirus infection in
Boger R, Michaels MG et al. Valganciclovir for symptomatic single serum sample of second trimester pregnancy. J Med
congenital cytomegalovirus disease. N Engl J Med 2015; Virol 2000; 60: 324-30. 82
372: 933–43. 32. Grangeot-Keros L, Mayaux MJ, Lebon P, Freymuth F,
18. Nigro G, Anceschi MM, Cosmi EV. Clinical manifestations Eugene G, Stricker R et al. Value of cytomegalovirus (CMV)
Vol. 1, No. 2, July 2020 BPS journal
and abnormal laboratory findings in pregnant women with IgG avidity index for the diagnosis of primary CMV
primary cytomegalovirus infection. BJOG 2003; 110: infection in pregnant women. J Infect Dis 1997; 175: 944-46.
572–77. 33. Baccard-Longere M, Freymuth F, Cointe D, Seigneurin JM,
19. Revello MG, Gerna G. Diagnosis and management of Grangeot-Keros L. Multicenter evaluation of a rapid and
human cytomegalovirus infection in the mother, fetus, and convenient method for determination of cytomegalovirus
newborn infant. Clin Microbiol Rev 2002; 15: 680–715. immunoglobulin G avidity. Clin Diagn Lab Immunol 2001;
20. Munro SC, Hall B, Whybin LR, Leader L, Robertson 8: 429-31.
P, Maine GT et al. Diagnosis of and screening for 34. Ross SA, Ahmed A, Palmer AL, Michaels MG, Sánchez PJ,
cytomegalovirus infection in pregnant women. J Clin Bernstein DI et al. National Institute on Deafness and Other
Microbiol 2005; 43: 4713–4718. Communication Disorders CHIMES Study, Detection of
21. Mace M, Sissoeff L, Rudent A, Grangeot-Keros L. A Congenital Cytomegalovirus Infection by Real-Time
serological testing algorithm for the diagnosis of primary Polymerase Chain Reaction Analysis of Saliva or Urine
CMV infection in pregnant women. Prenat Diagn 2004; 24: Specimens, The Journal of Infectious Diseases 2014; 210( 9):
861–63. 1415–18.
22. Adler SP. Molecular epidemiology of cytomegalovirus: A 35. Buonsenso D, Serranti D, Gargiullo L, Ceccarelli M, Ranno
study of factors affecting transmission among children at O, Valentini P. Congenital cytomegalovirus infection:
three day-care centers. Pediatr Infect Dis J 1991; 10: 584–90. current strategies and future perspectives. Eur Rev Med
Pharmacol Sci. 2012 ;16(7):919-35.
23. Mocarski E, Shenk T , Pass R. Cytomegaloviruses. In: Knipe
D, Howley P, Griffin D, et al. (eds) Fields virology 5th ed. 36. Forsgren M. Prevention of congenital and perinatal
Philadelphia: Lippincott Williams & Wilkins, 2007, infections. Euro Surveill 2009; 14: 2–4.
pp.2701–2772. 37. Rahav G. Congenital cytomegalovirus infection—a question
24. Hyde TB, Schmid DS , Cannon MJ. Cytomegalovirus of screening. Isr Med Assoc J 2007; 9: 392–94.
seroconversion rates and risk factors: implications for 38. Doutre S. Reducing congenital cytomegalovirus infection
congenital CMV. Rev Med Virol 2010; 20: 311–26. through policy and legislation in the United States.
25. Adler SP. Cytomegalovirus and child day care: Risk factors Microbiology Australia 2015; November: 162–164.
for maternal infection. Pediatr Infect Dis J 1991; 10: 39. Lanari M, Capretti MG, Lazzarotto T, Gabrielli L, Rizzollo
590–594. S, Manzoni P. Neuroimaging in CMV congenital infected
26. Staras SA, Dollard SC, Radford KW, Flanders WD, Pass neonates: how and when. Early human development,
RF, Cannon MJ. Seroprevalence of cytomegalovirus 2012;88 (2): S3-5.
infection in the United States. Clin Infect Dis 2006; 43:1143– 40. Jin HD, Demmler-Harrison GJ, Coats DK, Paysse EA, Bhatt
51. A, Edmond JC et al. Long-term Visual and Ocular Sequelae
27. de Vries JJ, van Zwet EW, Dekker FW, Kroes AC, Verkerk in Patients With Congenital Cytomegalovirus
PH, Vossen AC. The apparent paradox of maternal Infection. Pediatr Infect Dis J. 2017; 36(9):877–82.
seropositivity as a risk factor for congenital cytomegalovirus doi:10.1097/INF.0000000000001599
infection: a population-based prediction model. Rev Med 41. Fowler KB, McCollister FP, Sabo DL, Shoup AG, Owen KE,
Virol 2013; 23:241–249. Woodruff JL, et al. A Targeted Approach for Congenital
28. Kenneson A, Cannon MJ. Review and meta-analysis of the Cytomegalovirus Screening Within Newborn Hearing
epidemiology of congenital cytomegalovirus (CMV) Screening. Pediatrics. 2017 Feb;139(2):2016-2128.
infection. Rev Med Virol 2007; 17:253–76. 42. Elizabeth KS, Pablo JS. Cytomegalovirus Infection in the
29. Albanna EA, El-Latif RS, Sharaf HA, Gohar MK, Ibrahim Fetus and Neonate. NeoReviews 2005; 6 (1): e38-
BM. Diagnosis of congenital cytomegalovirus infection in e45; DOI: 10.1542/neo.6-1-e38
high risk neonates. Mediterr J Hematol Infect Dis. 43. Amanda G, Nigel C, Suzanne MG, Tom GC, Andrew JD.
2013;5(1):e2013049. Which infants with congenital cytomegalovirus infection
30. Revello MG, Zavattoni M, Baldanti F, Sarasini A, Paolucci benefit from antiviral therapy?.Arch Dis Child June 2014
S, Gerna G. Diagnostic and prognostic value of human ;99 ( 6): 597-601.
cytomegalovirus load and IgM antibody in blood of 44. Fatema K, Rahman MM, Akhtar S, Shefa J. Efficacy of
congenitally infected newborns. J Clin Virol 1999; 14: Valganciclovir versus Ganciclovir in treatment of
57-66. symptomatic cytomegalovirus infection in infants: An open-
31. Eggers M, Bader U, Enders G. Combination of label randomized controlled trial. JICNA 2019;1(1) 1-8.
microneutralization and avidity assays: improved diagnosis https://doi.org/10.17724/jicna.2019.133.
82 Vol. 1 | No. 2 | July 2020
Updates in Cytomegalovirus Infection in Pregnancy, Neonates and Infancy: Diagnosis Kanij Fatema et al.
45. Kim CS. Congenital and perinatal cytomegalovirus 48. Adler SP, Finney JW, Manganello AM, Best AM. Prevention
infection. Korean J Pediatr. 2010; 53(1):14-20. of child-to-mother transmission of cytomegalovirus among
46. Revello MG, Tibaldi C, Masuelli G, Frisina V, Sacchi pregnant women. J Pediatr 2004; 145: 485–91. 83
A, Furione M et al. Prevention of primary cytomegalovirus 49. Pass RF, Arav-Boger R. Maternal and fetal cytomegalovirus
infection in pregnancy. EBioMedicine 2015; 2: 1205–10. infection: diagnosis, management, and prevention.
Vol. 1, No. 2, July 2020 BPS journal
47. Vauloup-Fellous C, Picone O, Cordier AG, Parent-du- F1000Res. 2018;7:1-14. (doi: 10.12688/
Châtelet I, Senat MV, Frydman R et al. Does hygiene f1000research.12517.1)
counseling have an impact on the rate of CMV primary 50. Johnson J, Anderson B. Screening, prevention, and treatment
infection during pregnancy? Results of a 3-year prospective of congenital cytomegalovirus. Obstet Gynecol Clin North
study in a French hospital. J Clin Virol 2009; 46 (4): S49–53. Am. 2014; 41(4): 593–99.
Vol. 1 | No. 2 | July 2020 83
You might also like
- Abdoul Karim Itinerary Qatar Airways Flight TicketDocument1 pageAbdoul Karim Itinerary Qatar Airways Flight TicketPeter GrayNo ratings yet
- CH371 Novel Separation ProcessDocument3 pagesCH371 Novel Separation ProcessIrfan K MoiduNo ratings yet
- BMJ n1212 FullDocument10 pagesBMJ n1212 FullRosela ObandoNo ratings yet
- 1-s2.0-S0196439923000259-CMVDocument8 pages1-s2.0-S0196439923000259-CMVaurimeryNo ratings yet
- Congenital Cytomegalovirus-HistoryDocument6 pagesCongenital Cytomegalovirus-Historydossantoselaine212No ratings yet
- NohlpsbfurnDocument17 pagesNohlpsbfurnTri Setya NNo ratings yet
- Acta Paediatrica - 2020 - Lüsebrink - Retrospectively Diagnosing Congenital Cytomegalovirus Infections in SymptomaticDocument6 pagesActa Paediatrica - 2020 - Lüsebrink - Retrospectively Diagnosing Congenital Cytomegalovirus Infections in Symptomaticdossantoselaine212No ratings yet
- Congenital Cytomegalovirus Infection: Current Strategies and Future PerspectivesDocument17 pagesCongenital Cytomegalovirus Infection: Current Strategies and Future PerspectivesAfif AriyanwarNo ratings yet
- CMV Pregnancy 20Document20 pagesCMV Pregnancy 20Татьяна ТутченкоNo ratings yet
- Prevention of Congenital Cytomegalovirus Infection With Vaccines State of The ArtDocument11 pagesPrevention of Congenital Cytomegalovirus Infection With Vaccines State of The Artmadimadi11No ratings yet
- Jurnal CMVDocument4 pagesJurnal CMVmuarifNo ratings yet
- TORCH InfectionsDocument37 pagesTORCH InfectionsEylin Halim Rahardjo100% (1)
- Maedica 15 253Document5 pagesMaedica 15 253Fer AguilarNo ratings yet
- CMV 3Document11 pagesCMV 3Birgitta IvanaNo ratings yet
- Microorganisms 09 01749Document23 pagesMicroorganisms 09 01749Ga HernandezNo ratings yet
- Infectious and Tropical Pediatric Division Department of Child Health Medical Faculty, University of Sumatera UtaraDocument33 pagesInfectious and Tropical Pediatric Division Department of Child Health Medical Faculty, University of Sumatera UtaramaruliasnaNo ratings yet
- Evidence 3) Congenital Infection Causes Neurologic and Hematologic Damage andDocument5 pagesEvidence 3) Congenital Infection Causes Neurologic and Hematologic Damage andandamar0290No ratings yet
- Cytomegalovirus Infection: Dr. Hendra Purnasidha Bagaswoto, M.SC, Sp.A SMF Anak RSUP Dr. Soeradji Tirtonegoro KlatenDocument40 pagesCytomegalovirus Infection: Dr. Hendra Purnasidha Bagaswoto, M.SC, Sp.A SMF Anak RSUP Dr. Soeradji Tirtonegoro KlatenDonniehh Assassintilldeath NothinglastforeverNo ratings yet
- Bacterial Meningitis in Infants Over 3 Months of AgeDocument8 pagesBacterial Meningitis in Infants Over 3 Months of AgedrirrazabalNo ratings yet
- Prevalence of Anti-Cytomegalovirus Anticorps in Children at The Chantal Biya Foundation Mother Child Centre, CameroonDocument6 pagesPrevalence of Anti-Cytomegalovirus Anticorps in Children at The Chantal Biya Foundation Mother Child Centre, CameroonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Congenital Cytomegalovirus Infection Clinical Features and DiagnosisDocument21 pagesCongenital Cytomegalovirus Infection Clinical Features and Diagnosisgomitas21No ratings yet
- Meningitis Pada AnakDocument14 pagesMeningitis Pada AnakRayhanun MardhatillahNo ratings yet
- Herpes Simplex Congenital Infections, Part I: Cytomegalovirus, Toxoplasma, Rubella, andDocument13 pagesHerpes Simplex Congenital Infections, Part I: Cytomegalovirus, Toxoplasma, Rubella, andSyahrialNo ratings yet
- Cytomegalovirus Infection in Pregnancy: Review of The LiteratureDocument8 pagesCytomegalovirus Infection in Pregnancy: Review of The LiteratureDewina Dyani Rosari IINo ratings yet
- Bahan Jurding Kaken 2Document7 pagesBahan Jurding Kaken 2Monica Dea RosanaNo ratings yet
- Congenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasDocument3 pagesCongenital CMV Infection in Symptomatic Infants in Delhi and Surrounding AreasMinerva StanciuNo ratings yet
- Child Infection CytomegalovirusDocument19 pagesChild Infection CytomegalovirusBishnoi MaheshNo ratings yet
- Knowledge of Cytomegalovirus and Available Prevention Strategies in Pregnancy A Cross-Sectional Study in PortugalDocument8 pagesKnowledge of Cytomegalovirus and Available Prevention Strategies in Pregnancy A Cross-Sectional Study in PortugalLissaberti AmaliahNo ratings yet
- Diagnostic Challenges in Congenital Cytomegalovirus Infection in Pregnancy A Case ReportDocument6 pagesDiagnostic Challenges in Congenital Cytomegalovirus Infection in Pregnancy A Case ReportBen HonorseekerNo ratings yet
- Review CMV 2011Document8 pagesReview CMV 2011francoNo ratings yet
- Infecciones Neonatale IDocument13 pagesInfecciones Neonatale IFidel RamonNo ratings yet
- Navti 2016Document7 pagesNavti 2016XXXI-JKhusnan Mustofa GufronNo ratings yet
- Cytomegalovirus Infection in Pregnancy: A Still Complicated Diagnostic ProblemDocument9 pagesCytomegalovirus Infection in Pregnancy: A Still Complicated Diagnostic ProblemRoy GoldenNo ratings yet
- Congenital Cytomegalovirus Infection in The Absence of Maternal Cmv-Igm Antibodies: A Case ReportDocument3 pagesCongenital Cytomegalovirus Infection in The Absence of Maternal Cmv-Igm Antibodies: A Case ReportVictoria CyntiaNo ratings yet
- CMV, Tosoplasma, Rubeóla, Herpes SimpleDocument13 pagesCMV, Tosoplasma, Rubeóla, Herpes SimplePau PuenteNo ratings yet
- CMV Postnatal JurnalDocument1 pageCMV Postnatal JurnalHanifa RahmaNo ratings yet
- Congenital Cytomegalovirus Infection: Description of VirusDocument6 pagesCongenital Cytomegalovirus Infection: Description of VirusMinerva StanciuNo ratings yet
- Journal Pone 0252309Document12 pagesJournal Pone 0252309XXXI-JKhusnan Mustofa GufronNo ratings yet
- Halaman DepanDocument6 pagesHalaman DepanzakiNo ratings yet
- Cytomegalovirus Infection in Pregnancy: Infecção Pelo Citomegalovírus Na GestaçãoDocument5 pagesCytomegalovirus Infection in Pregnancy: Infecção Pelo Citomegalovírus Na GestaçãoDewina Dyani Rosari IINo ratings yet
- TORCHDocument34 pagesTORCHItzel Sarahil Rubio SotoNo ratings yet
- Torch Infections LectureDocument77 pagesTorch Infections LectureL MollyNo ratings yet
- Primer On MicrocephalyDocument10 pagesPrimer On MicrocephalylilyNo ratings yet
- 2017 Congenital Cytomegalovirus Infection in Pregnancy and The Neonate - Consensus Recommendations For Prevention, Diagnosis, and TherapyDocument9 pages2017 Congenital Cytomegalovirus Infection in Pregnancy and The Neonate - Consensus Recommendations For Prevention, Diagnosis, and TherapyValentinaNo ratings yet
- Viral Infections in Pregnant Women: Departemen Mikrobiologi Fak - Kedokteran USU MedanDocument46 pagesViral Infections in Pregnant Women: Departemen Mikrobiologi Fak - Kedokteran USU MedanSyarifah FauziahNo ratings yet
- Neonatal Sepsis 2019.Document6 pagesNeonatal Sepsis 2019.Jean Paúl LópezNo ratings yet
- Congenital and Perinatal Cytomegalovirus Infection: Chun Soo Kim, M.D., PH.DDocument7 pagesCongenital and Perinatal Cytomegalovirus Infection: Chun Soo Kim, M.D., PH.Dasri khazaliNo ratings yet
- Infections of The Fetus and NewbornDocument55 pagesInfections of The Fetus and Newbornlordoftheweb100% (4)
- Mother-To-Child Transmission of Chikungunya Virus: A Systematic Review and Meta-AnalysisDocument20 pagesMother-To-Child Transmission of Chikungunya Virus: A Systematic Review and Meta-AnalysisMarcelo QuipildorNo ratings yet
- Omphalitis: Cme R ADocument2 pagesOmphalitis: Cme R AthonjustineNo ratings yet
- Cytomegalovirus in PregnancyDocument6 pagesCytomegalovirus in PregnancyshwetaijmrNo ratings yet
- CongenitalDocument25 pagesCongenitalSUTHANNo ratings yet
- Jurnal Fixxxx 1Document14 pagesJurnal Fixxxx 1heryanggunNo ratings yet
- Neonatal SepsisDocument39 pagesNeonatal SepsisBryan KernsNo ratings yet
- Cortical Visual Impairment inDocument11 pagesCortical Visual Impairment inDwi juliana DewiNo ratings yet
- K28 A Congenital CMV KBKDocument37 pagesK28 A Congenital CMV KBKJoice RumondangNo ratings yet
- Citomegalovirus PDFDocument18 pagesCitomegalovirus PDFNADIANo ratings yet
- 2012 Number 1 947445146213461Document5 pages2012 Number 1 947445146213461MedstudNo ratings yet
- Livret MF GB21Document20 pagesLivret MF GB21mary15eugNo ratings yet
- Citomegalovirus en EmbarazoDocument8 pagesCitomegalovirus en EmbarazoJuan FranciscoNo ratings yet
- Endometrial Gene Expression: An Emerging Paradigm for Reproductive DisordersFrom EverandEndometrial Gene Expression: An Emerging Paradigm for Reproductive DisordersJoanne Kwak-KimNo ratings yet
- 1 - Pattent IDocument8 pages1 - Pattent IAmirNo ratings yet
- Icse Class X Physics Practise Sheet 1 ForceDocument3 pagesIcse Class X Physics Practise Sheet 1 ForceMehnaaz Brar100% (2)
- Week 4 - Stadelman-Cohen & Hillman (2014)Document22 pagesWeek 4 - Stadelman-Cohen & Hillman (2014)kehanNo ratings yet
- Chapter 2Document22 pagesChapter 2Abdullahi BaballoNo ratings yet
- Test BenchDocument16 pagesTest BenchAdriana VeronicaNo ratings yet
- Dell Service ManualDocument220 pagesDell Service ManualYeik ThaNo ratings yet
- Integrity Management of Safety Critical Equipment and SystemsDocument10 pagesIntegrity Management of Safety Critical Equipment and SystemsLi QiNo ratings yet
- Silage Pile Sizing Documentation 5 12 2016 3Document9 pagesSilage Pile Sizing Documentation 5 12 2016 3Zaqueu Ferreira RodriguesNo ratings yet
- The Evolution of Water Reverse Osmosis TechnologyDocument35 pagesThe Evolution of Water Reverse Osmosis TechnologyQassim LaouiraNo ratings yet
- SM DH Series ManualDocument154 pagesSM DH Series Manualkikyangello90No ratings yet
- Business Finance Test PracticeDocument49 pagesBusiness Finance Test PracticeLovan So0% (1)
- Foundations Expansive Soils: Chen CDocument6 pagesFoundations Expansive Soils: Chen CBolton Alonso Yanqui SotoNo ratings yet
- EE Syllabus PDFDocument100 pagesEE Syllabus PDFShahid LoneNo ratings yet
- Despite', in Spite Of', Although', Though' and Even Though'Document4 pagesDespite', in Spite Of', Although', Though' and Even Though'pikorl4327No ratings yet
- Full ReportDocument78 pagesFull ReportHiwot Wubetu100% (5)
- Ship SizeDocument4 pagesShip SizeBaki PınarlıNo ratings yet
- MicroPara Lecture 6Document24 pagesMicroPara Lecture 6Pearl NoconNo ratings yet
- Released FOR Manufacturing: 2509 ANTAMINA PERU SMC 100/14400 Truck Bridge Assembly Truck Bridge Steel Structure - RightDocument1 pageReleased FOR Manufacturing: 2509 ANTAMINA PERU SMC 100/14400 Truck Bridge Assembly Truck Bridge Steel Structure - RightCarlos ParedesNo ratings yet
- THE Lymphatic System & Body DefensesDocument39 pagesTHE Lymphatic System & Body DefensesSaiful AmriNo ratings yet
- Idioms For IELTS SpeakingDocument21 pagesIdioms For IELTS SpeakingРоза АсановаNo ratings yet
- Lifted 28 Days To Focus Your Mind Strengthen Your Body and Elevate Your Spiri PDFDocument276 pagesLifted 28 Days To Focus Your Mind Strengthen Your Body and Elevate Your Spiri PDFDiego100% (3)
- High Voltage Switching Operations: The Next StepDocument2 pagesHigh Voltage Switching Operations: The Next Steplenon chidzivaNo ratings yet
- Sop BM RHF Oprn ProcedureDocument2 pagesSop BM RHF Oprn ProcedurewrbmrhfispNo ratings yet
- AdulterantsDocument7 pagesAdulterantsNeeraj SharmaNo ratings yet
- Fa 5541Document46 pagesFa 5541Ricardo Nicolau WerlangNo ratings yet
- Eqpt - No. 50CH0203LC10 Fly Ash Fly Ash Material 200 T Capacity 1 No QtyDocument62 pagesEqpt - No. 50CH0203LC10 Fly Ash Fly Ash Material 200 T Capacity 1 No Qtykumar gauravNo ratings yet
- Figure 1 Concept of Structure and Function: Philippine-EagleDocument8 pagesFigure 1 Concept of Structure and Function: Philippine-EagleShekaina Faith Cuizon Lozada100% (2)
- Betag 2014Document7 pagesBetag 2014MelmakPolytronNo ratings yet