Professional Documents
Culture Documents
Obstetrics and Gynaecology Cases Reviews Ogcr 10 249
Obstetrics and Gynaecology Cases Reviews Ogcr 10 249
Uploaded by
fitaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obstetrics and Gynaecology Cases Reviews Ogcr 10 249
Obstetrics and Gynaecology Cases Reviews Ogcr 10 249
Uploaded by
fitaCopyright:
Available Formats
ISSN: 2377-9004
Citil. Obstet Gynecol Cases Rev 2023, 10:249
DOI: 10.23937/2377-9004/1410249
Obstetrics and
Volume 10 | Issue 3
Open Access
Gynaecology Cases - Reviews
Case Report
Huge Retroperitoneal and Pelvic Hematoma Following
VBAC (TOLAC): A Case Report
Ayse Citil, MD*
Check for
updates
Department of Obstetrics and Gynecology, Inova Hospital, Aksaray, Turkey
*Corresponding author: Ayse Citil, MD, Department of Obstetrics and Gynecology, Inova Hospital, Aksaray, 68100,
Turkey, Tel: +90(538)-385-5477
Introduction
Abstract
Retroperitoneal hematomas following vaginal delivery
Postpartum retroperitoneal hematomas are rare
are life threatening rare complication in obstetrics. There life-treatening obstetric complication following vaginal
is no report showed that identification of retroperitoneal or cesarian delivery Patient can admit to hospital with
hematoma following vaginal birth after cesarean (VBAC) in just simple pelvic pain to hypovolemic shock [1]. It has
the literature.
been mentioned mostly with case reports. Accurate
Case presentation: A 35-year-old G3P1A1, VBAC incidence and management of this complication are
patient, presented in the clinic with severe rectal pain a
few hours following uncomplicated vaginal delivery with
difficult [2]. Even though, etiology remains unclear, the
small mediolateral episiotomy. In initial findings, patient traction and damage to pelvic veins during the second
was hypotensive and tachycardic. The hemoglobin stage of labor or episiotomy repair are most common
(Hb) measurements were low (postpartum to 8.6 g/dL). causes for this complication and can’t be completely
Episiotomy was reopened 2 hour later after delivery. Huge
right pelvic hematoma, approximately 12 cm diameter, was ruled out [3].
drained and multiple tight sutures were carefully replaced In Turkey, there is no established national guidelines
every layer of perineum and bleeding was taken under
control. Hb level was risen to 10.4 g/dL after transfusion of for diagnosis and treatment of VBAC, physicians are
2 units of packed red blood cells (RBC). Patient was stable following the international guideliness [4]. During
with no pain and her vital signs were normal at postoperative prenatal visits, VBAC score is calculated depending on
intensive care. However, the Hb level was measured low in patient age, ethnicity, body mass index (BMI), previous
follow-ups to 6.4 g/dL at postpartum 12 hours. Evaluation
of MRI showed large extraperitoneal bleeding which was obstetric history and interdelivery interval and this
reaching from perinea to umbilicus and surrounding bladder score is used for the management strategies of VBAC
bilaterally. No fluid was detected in Douglas pouch. There [5]. Previously, data is getting acumulated about VBAC
was a huge hematoma, so immediately active management
[4], so we want to make a contrubition about our
of postpartum bleeding was performed. Blood supplies was
given, close monitoring of her vital sign and coagulation experience.
parameters was measured. The operation was performed
conservatively because vital signs were normal. Patient was
This case report summarizes a case of retroperitoneal
stable postoperative days and discharged from hospital on hematoma that developed at 3 hours following an
the 7th day. uncomplicated vaginal delivery. This is the first case
Postpartum hematomas should be managed carefully. with retroperitoneal hematoma during VBAC trial in the
Surgical removal and arterial embolization are the treatment literature.
options of postpartum hematoma.
Case Presentatıon
Keywords
A white, 35-year-old woman (gravida 3, para 1,
Retroperitoneal hematoma, VBAC, TOLAC, Dinoproston,
Conservative management
abortus 1) at 40 weeks 2-day pregnancy, who was
Citation: Citil A (2023) Huge Retroperitoneal and Pelvic Hematoma Following VBAC (TOLAC): A Case
Report. Obstet Gynecol Cases Rev 10:249. doi.org/10.23937/2377-9004/1410249
Accepted: September 28, 2023: Published: September 30, 2023
Copyright: © 2023 Citil A, et al. This is an open-access article distributed under the terms of the
Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction
in any medium, provided the original author and source are credited.
Citil. Obstet Gynecol Cases Rev 2023, 10:249 • Page 1 of 4 •
DOI: 10.23937/2377-9004/1410249 ISSN: 2377-9004
eligible for VBAC after 9 years of uncomplicated section of service. After 3 hours, she began reporting
cesarian section (CS), was admitted to our clinic and bulging and severe pain on her episiotomy area. On
hospitalized at Jan 2022 for labor induction with pelvic exam, we found that she had approximately
diagnosis of oligohydroamnios. On previous prenatal 6 cm hematoma under the incision. Her control Hb
visits, predicted chance of VBAC was calculated around level was 11.6 g/dL however postural hypotension
60-70%. Her BMI was around 25. She had no specific and tachycardia was detected in physical examination.
previous medical history, drug usage or surgery except Under anesthesia and antisepsis conditions, patient
CS at previous pregnancy. She had an emergency CS in underwent surgery. During the operation, pelvic
2013, 9 years ago with the diagnoses of small gestational hematoma was drained out vaginally but there was
age + rupture of membranes + anhydroamniosis. great crater in the right side of perineum; (left wall of
crater was rectal mucosa, posterior and right wall was
Cervix was central, soft, open (2 cm) but tight,
levator ani muscle). Compression sutures were carefully
her bishop score was 7, slightly unfavorable, so
applied every layer of perineum. Intraoperative control
dinoprostone was placed to posterior fornix for
Hb was 8.6 g/dL. After 2 units packed RBC infusion, her
induction of labor. The latent phase continued for 3-4
Hb rose up to10.4 g/dL. Her pain score was relief and
hour and active phase was 3-4 hours, respectively. Small
vital signs were within normal limits. Wound care and
right mediolateral episiotomy was performed to reduce
broad-spectrum antibiotics were started intravenously.
afterload of uterus. The newborn weighed 3050g and
was in good health on an initial assessment (APGAR She was cooperative and oriented but in postop 14
scores was 8 and 9, respectively). Her uterine tonus was hours period, her follow-up Hb level started dropping
toned, and episiotomy cut was clear. After episiotomy from 10.4 to 8.6, 6.9 and 6.7 respectively. Most serious
repair stiches, patient was transferred to postpartum complication of VBAC for patient including doctor is
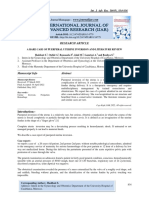
Figure 1 1A
1B 1C
Figure 1: MR showed that big dissemine retroperitoneal fluid was all around the pelvis reaching umbilicus and was
squeezing the bladder bilaterally. (a) T1 weighted fat-suppressed transvers MR imaging; (b) T1 weighted fat-suppressed
sagittal MR imaging; (c) T2 weighted transvers MR imaging.
Citil. Obstet Gynecol Cases Rev 2023, 10:249 • Page 2 of 4 •
DOI: 10.23937/2377-9004/1410249 ISSN: 2377-9004
uterine rupture. Transvaginal and suprapubic ultrasound well, first and second stage of labor progressed well
was performed to rule out this diagnosis immediately, with no delay. Small episiotomy was performed to
and USG showed that uterus was intact, and no fluid reduce afterload of uterus and help us for management
was found in Douglas pouch. Pelvic MR showed that big of TOLAC. Fetus was relatively small. Delivery went
(measurements) retroperitoneal fluid was all around uneventfully. Maternal age and BMI is favorable. There
the pelvis reaching umbilicus and was squeezing the was no presense reason for excessive bleeeding.
bladder bilaterally (Figure 1a, Figure 1b and Figure 1c).
Some of the reported iatrogenic causes of puerperal
Patient was stable. Under analgesia her pelvic pain
retroperitoneal hematomas include traumatic
was absent, and her abdominal examinations were
deliveries, manual removal of placenta, inadequate
normal. Even though patient was stable, 2nd surgery
hemostasis at CS, and anticoagulation therapy [11]. Our
was considered to manage postpartum hemorrhage.
patient did not have any of these situations.
There was a chance that another surgery to patient and
surgical evacuation might lead to loss of the advantages As in our patient, most common sings of hematoma
of the tamponing effect on the bleeding source which are postural hypotension, tachycardia and pain. So,
could result in undue dissection and end up with a fatal we needed to drain out pelvic hematoma via vaginal
outcome. So, we decided to follow up the hematoma route because of pain and hemodynamic status of
conservatively with close, careful monitoring. Tersier patient. After evacuation of right pelvic hematoma,
referral hospital was informed about possible arterial huge crater left in there so compression sutures were
embolization, or another further surgery as needed. carefully applied to every layer of perineum. After
surgery, pain was relieved, vitals signs were normal
The patient was transfused 3 more units of packed
however hemoglobin level started to drop again at
RBCs (totally 5 unit packed RBCs) and 2 unit fresh frozen
postop 12 hours. Most crucial complication of TOLAC
plasma (FFP). Her coagulation parameters, especially
is uterine rupture [12] but MR and ultrasound showed
fibrinogen level was within normal range (What were
that bleeding was in extraperitoneum and myometrium
the measures?). Transamine was given two times to
was intact. Retroperitoneal hematomas occur as a
lead coagulation better [6]. The patient was closely
consequence of injury to branches of the internal iliac
monitored for a week with supportive treatment. The
arteries. The majority of cases occur in the context of
patient became more stable and was finally discharged
uterine artery lacerations during hysterectomy, uterine
from hospital on the 7th day.
rupture, or as an extension of a paravaginal hematoma
She was fully recovered with no sequelae and [3].
showed no signs of hematoma at her 2-month follow-
Our hypothesis of about that complication is, pelvic
up. Second abdominal MRI was planned at 3 month
area was taken undercontrol with sutures but bleeding
follow up, May 2022 to check resolution of hematoma.
has still continued from pelvic venous plexus to all
Discussion around the lower abdomen until umbliculus. After MRI
report, we thought that there was a chance to damage
Postpartum retroperitoneal hematomas are rare, life-
the venous plexus during the surgery but there was a
threteaning obsterics complications. There is no actual
huge crater after evacuation so it could be happened
incidence and management algoritm [2]. The literature
before surgery. These veins could be damaged on the
shows in only case reports, and different managements
second stage of labor or could be damaged during
of this complication. Also, our patient is the first case of
episyotomy. There is a slight possibility that our patient
TOLAC with complication of retroperitoneal hematoma.
have undiagnosed mild bleeding disorder related
Recently, more TOLAC case were diagnosed [4]. with connective tissue or coagulation cascade and
Risk factors, contraindications and complications are paravaginal hematoma extened from pelvic floor to
getting more clear but still we do not have certain umbliculus.
criterias and/or national guidelines for Turkey. We are
Management of retroperitoneal hematomas are
guided by literature and our best knowledge on patient
conservatively, surgically, or through use of angiographic
experience is the key point for the management. Patient
embolization [13]. The patient’s hemodynamic stability
age, ethnicity, BMI, previous obstetric history and
plays a key role in the management plan. Conservative
interdelivery interval are the factors that effects TOLAC
management is usually preferred for hemodynamically
decision [5].
stable patients with no active bleeding [13]. Fortunately,
Risk factors for retroperitoneal hematoma includes our patient was hemodynamically stable so we could
multiparity, macrosomia, preeclampsia, prolonged treated her conservatively.
second stage of labour, multi-fetal pregnancy, vulvar
If it is available, selective arterial embolization (SAE)
varicosities, pregnancy itself and blood clotting disorders
is more appropriate treatment option because pelvic
[1,7-10].
blood supply is more complicated and source of bleeding
Our case was a TOLAC patient, her induction went during laparotomy can’t be identified. Also, surgery can
Citil. Obstet Gynecol Cases Rev 2023, 10:249 • Page 3 of 4 •
DOI: 10.23937/2377-9004/1410249 ISSN: 2377-9004
remove tampon effect of coagulum and cause to restart 5. Blackwell SC (2009) Predicting VBAC success: From
bleeding again. Surgery can be preferred at selective theory to clinical practice. Am J Perinatol 26: 691-692.
cases. For further surgery or SAE application we had 6. Bakanlıggı TC, Saglık, Genel Muudurlugu ACSAP (2009)
been in contact of referral center. Gebelikte Kanama Yonetimi in Mehmet Rifat KÖSE, Acil
Obstetrik Bakım Yonetim Rehberi (Damla Matbaacılık:
Conclusions Ankara).
7. Guerriero S, Ajossa S, Bargellini R, Amucano G, Marongiu
Postpartum retroperitoneal hematomas must be
D, et al. (2004) Puerperal vulvovaginal hematoma:
managed carefully. Timely diagnosis and management Sonographic findings with MRI correlation. J Clin Ultrasound
properly are essential. It is rare and dangerous 32: 415-418.
complication of obstetrics. Suspicion and awareness 8. Propst AM, Thorp JM (1998) Traumatic vulvar hematomas:
of this complication is the key attitude and it should be Conservative versus surgical management. South Med J
considered at TOLAC pregnancies. Management of that 91: 144-146.
complication should carefully apply according to patient 9. Ridgway LE (1995) Puerperal emergency. Vaginal and
status, hospital set up and clinical expertise. vulvar hematomas. Obstet Gynecol Clin North Am 22: 275-
282.
TOLAC experience of clinics are getting rise and
this case contribute to literature about that rare 10. Saleem Z, Rydhstrom H (2004) Vaginal hematoma during
parturition: A population-based study. Acta Obstet Gynecol
complication, retroperitoneal hematomas, on TOLAC Scand 83: 560-562.
patients.
11. Wingert AL, Hartling M, Sebastianski C, Johnson R,
References Featherstone B, et al. (2019) Clinical interventions that
influence vaginal birth after cesarean delivery rates:
1. Maroyi R, Ngeleza N, Kalunga K, Buhendwa C, Shahid Systematic Review & Meta-Analysis. BMC Pregnancy
U, et al. (2021) Large retroperitoneal hematoma following Childbirth 19: 529.
vaginal delivery: A case report. J Med Case Rep 15: 290.
12. Lazarou A, Oestergaard M, Netzl J, Siedentopf JP, Henrich
2. Rafi J, Muppala H (2010) Retroperitoneal haematomas W (2021) Vaginal birth after cesarean (VBAC): fear it or
in obstetrics: Literature review. Arch Gynecol Obstet 281: dare it? An evaluation of potential risk factors. J Perinat
435-441. Med 49: 773-782.
3. Alturki F, Ponette V, Boucher LM (2018) Spontaneous 13. Chan YC, Morales JP, Reidy JF, Taylor PR (2008)
retroperitoneal hematomas following uncomplicated Management of spontaneous and iatrogenic retroperitoneal
vaginal deliveries: A case report and literature review. J haemorrhage: conservative management, endovascular
Obstet Gynaecol Can 40: 712-715. intervention or open surgery?. Int J Clin Pract 62: 1604-
4. Wu Y, Kataria Y, Wang Z, Ming WK, Ellervik C (2019) 1613.
Factors associated with successful vaginal birth after a
cesarean section: A systematic review and meta-analysis.
BMC Pregnancy Childbirth 19: 360.
Citil. Obstet Gynecol Cases Rev 2023, 10:249 • Page 4 of 4 •
You might also like
- Business and Society Stakeholders Ethics Public Policy 17Th Edition Anne Lawrence Full ChapterDocument67 pagesBusiness and Society Stakeholders Ethics Public Policy 17Th Edition Anne Lawrence Full Chaptermichael.lynch15578% (9)
- Sakurai Solutions 5-1 5-2Document8 pagesSakurai Solutions 5-1 5-2Raza Ali RazaNo ratings yet
- PlasentaDocument4 pagesPlasentaLois YunikeNo ratings yet
- Laparoscopic Management of Cervical-Isthmic Pregnancy: A Proposal MethodDocument4 pagesLaparoscopic Management of Cervical-Isthmic Pregnancy: A Proposal MethodDinorah MarcelaNo ratings yet
- Normal Vaginal Delivery at Term After Expectant Management of Heterotopic Caesarean Scar Pregnancy: A Case ReportDocument3 pagesNormal Vaginal Delivery at Term After Expectant Management of Heterotopic Caesarean Scar Pregnancy: A Case Reportdiaaabdallah209No ratings yet
- Caesarean Scar Ectopic Pregnancy: Case ReportDocument3 pagesCaesarean Scar Ectopic Pregnancy: Case ReportDewi SaftariNo ratings yet
- Caso ClinicoDocument3 pagesCaso Clinicojohav91670No ratings yet
- Case Reports in Women's HealthDocument4 pagesCase Reports in Women's Healthowadokunquick3154No ratings yet
- Successful Conservative Treatment of Microinvasive Cervical Cancer During PregnancyDocument3 pagesSuccessful Conservative Treatment of Microinvasive Cervical Cancer During PregnancyEres TriasaNo ratings yet
- Research ArticlesDocument3 pagesResearch ArticlesKeeranmayeeishraNo ratings yet
- Ectopic Abdominal Pregnancies: About 2 CasesDocument10 pagesEctopic Abdominal Pregnancies: About 2 CasesIJAR JOURNALNo ratings yet
- Uterine VaricesDocument3 pagesUterine VaricesCindy AuliaNo ratings yet
- Barel 2019Document3 pagesBarel 2019Mariana González DíazNo ratings yet
- Interesting Case FinalDocument33 pagesInteresting Case Finalazenith dumlaoNo ratings yet
- Unavoidable Myomectomy During Cesarean Section: A Case ReportDocument3 pagesUnavoidable Myomectomy During Cesarean Section: A Case ReportGuia Nina DuranNo ratings yet
- Cesarean Scar Pregnancies and Their ManagementDocument7 pagesCesarean Scar Pregnancies and Their ManagementClinton SitanggangNo ratings yet
- Ectopic Pregnancy in Uncommon Implantation Sites: The Egyptian Journal of Radiology and Nuclear MedicineDocument10 pagesEctopic Pregnancy in Uncommon Implantation Sites: The Egyptian Journal of Radiology and Nuclear MedicinerezachandraNo ratings yet
- Case Report: Recurrent Cesarean Scar Ectopic Pregnancy Treated With Systemic MethotrexateDocument5 pagesCase Report: Recurrent Cesarean Scar Ectopic Pregnancy Treated With Systemic MethotrexatesaryindrianyNo ratings yet
- Placenta Increta Causing Um in The 26th Week of Pregnancy 2Document3 pagesPlacenta Increta Causing Um in The 26th Week of Pregnancy 2Kester ApostolNo ratings yet
- Anterior Cervical Wall Rupture As A Result of Induced AbortionDocument4 pagesAnterior Cervical Wall Rupture As A Result of Induced AbortionnawriirwanNo ratings yet
- 655 NKJDocument5 pages655 NKJEka AriasyahNo ratings yet
- Postpartum Hemorrhage With Associated Placenta PR 2024 International JournalDocument3 pagesPostpartum Hemorrhage With Associated Placenta PR 2024 International JournalRonald QuezadaNo ratings yet
- International Journal of Anesthetics and Anesthesiology Ijaa 6 095Document5 pagesInternational Journal of Anesthetics and Anesthesiology Ijaa 6 095daily of sinta fuNo ratings yet
- 10 1016@j Ijscr 2020 01 020Document4 pages10 1016@j Ijscr 2020 01 020ari naNo ratings yet
- 08 Re-LaparotomyaftercesareanDocument8 pages08 Re-LaparotomyaftercesareanFarhanNo ratings yet
- Delayed Interval Delivery in Twin Pregnancy Without Cerclage: CaseDocument2 pagesDelayed Interval Delivery in Twin Pregnancy Without Cerclage: Caselailatul husnaNo ratings yet
- BJSTR MS Id 003341Document4 pagesBJSTR MS Id 003341herryNo ratings yet
- Girija BS, Sudha TR: AbstractDocument4 pagesGirija BS, Sudha TR: AbstractALfuNo ratings yet
- Gynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernDocument3 pagesGynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernIrvin MarcelNo ratings yet
- Conservative Management of Placenta Accreta in A Multiparous WomanDocument10 pagesConservative Management of Placenta Accreta in A Multiparous WomanRobel Mae Lagos MontañoNo ratings yet
- Adenomyosis and Uterine Rupture During Labour in A Primigravida: An Unusual Obstetric Emergency in NigeriaDocument2 pagesAdenomyosis and Uterine Rupture During Labour in A Primigravida: An Unusual Obstetric Emergency in NigeriaMariam Carolina Viloria VargasNo ratings yet
- AkretaDocument7 pagesAkretaInna SeraLaratNo ratings yet
- A Rare Case of Puerperal Uterine Inversion and Literature ReviewDocument3 pagesA Rare Case of Puerperal Uterine Inversion and Literature ReviewIJAR JOURNALNo ratings yet
- Case Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyDocument4 pagesCase Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyChidimma VictoryNo ratings yet
- Poster T1BDocument1 pagePoster T1BHaris SetiaNo ratings yet
- Lactating Adenoma A Case ReportDocument3 pagesLactating Adenoma A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Kista Terpluntir NcbiDocument2 pagesKista Terpluntir NcbiFatimahNo ratings yet
- Rupture of The Cervix During Pregnancy After Cervical Pessary Insertion For Preventing Preterm BirthDocument4 pagesRupture of The Cervix During Pregnancy After Cervical Pessary Insertion For Preventing Preterm BirthNuril AzizahNo ratings yet
- 1 s2.0 S0090825804003610 Main PDFDocument3 pages1 s2.0 S0090825804003610 Main PDFRirin WahyuniNo ratings yet
- Katakam2009 PDFDocument1 pageKatakam2009 PDFandri anaNo ratings yet
- Case Report: Management of Cervical Fibroid During The Reproductive PeriodDocument4 pagesCase Report: Management of Cervical Fibroid During The Reproductive PeriodMetharisaNo ratings yet
- Adenomyosis Excision Followed by Successful Live Birth After Three Consecutive IVFDocument5 pagesAdenomyosis Excision Followed by Successful Live Birth After Three Consecutive IVFPyuzz RemakeNo ratings yet
- Case Report Rare Cesarean Section Scar Ectopic Pregnancy Successfully Treated by Methotrexate: A CaseDocument5 pagesCase Report Rare Cesarean Section Scar Ectopic Pregnancy Successfully Treated by Methotrexate: A Casemustafaali9711No ratings yet
- Medical Treatment of Tubar Ectopic Pregnancy With Living EmbrioDocument4 pagesMedical Treatment of Tubar Ectopic Pregnancy With Living EmbrioMuhammad Aji SantosoNo ratings yet
- Yan 2007Document3 pagesYan 2007Agustin LindaNo ratings yet
- Third Trimester Fetoscopic Laser Ablation of Type II Vasa PreviaDocument5 pagesThird Trimester Fetoscopic Laser Ablation of Type II Vasa PreviaSol MancipeNo ratings yet
- Clinical Medicine Insights: Case ReportsDocument4 pagesClinical Medicine Insights: Case ReportsJer KelNo ratings yet
- Gynecologic Oncology Reports: Natsuki Tsuji, Yusuke Butsuhara, Hiroko Yoshikawa, Koichi Terakawa, Tadayoshi NaganoDocument3 pagesGynecologic Oncology Reports: Natsuki Tsuji, Yusuke Butsuhara, Hiroko Yoshikawa, Koichi Terakawa, Tadayoshi NaganofujimeisterNo ratings yet
- Labor Epidural Analgesia With Severe ThrombocytopeniaDocument2 pagesLabor Epidural Analgesia With Severe Thrombocytopeniasand52525No ratings yet
- Hioerplasia Mamaria GestacionalDocument9 pagesHioerplasia Mamaria GestacionalOctavio LeyvaNo ratings yet
- Wright 2013Document3 pagesWright 2013cristian vivasNo ratings yet
- 1 s2.0 S1028455922002935 MainDocument4 pages1 s2.0 S1028455922002935 Mainmodacasper056No ratings yet
- Liao 2016Document4 pagesLiao 2016cristian vivasNo ratings yet
- Hysteroscopic Management of Omentum Incarceration (Ingles)Document6 pagesHysteroscopic Management of Omentum Incarceration (Ingles)silviadmcastellanNo ratings yet
- A Rare Case of Morbidly Adherent Placenta in A Young - 2024 - International JouDocument4 pagesA Rare Case of Morbidly Adherent Placenta in A Young - 2024 - International JouRonald QuezadaNo ratings yet
- Emergency Peripartum Hysterectomy As Life Saving Surgery For Postpartum Haemorrhage in Women With Single Kidney - A CaseReportDocument5 pagesEmergency Peripartum Hysterectomy As Life Saving Surgery For Postpartum Haemorrhage in Women With Single Kidney - A CaseReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Case Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaeDocument4 pagesCase Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaemelisaberlianNo ratings yet
- Torsion OvarianDocument6 pagesTorsion Ovarianrg2fpgqnc8No ratings yet
- A New Facilitating Technique For Postpartum Hysterectomy at Full Dilatation: Cervical ClampDocument4 pagesA New Facilitating Technique For Postpartum Hysterectomy at Full Dilatation: Cervical ClampJani SheNo ratings yet
- Uncomplicated Term Vaginal Delivery Following Magnetic Resonance-Guided Focused Ultrasound Surgery For Uterine FibroidsDocument4 pagesUncomplicated Term Vaginal Delivery Following Magnetic Resonance-Guided Focused Ultrasound Surgery For Uterine FibroidsMangku Liong GuanNo ratings yet
- Gynecology and Minimally Invasive Therapy: Case ReportDocument5 pagesGynecology and Minimally Invasive Therapy: Case Reportsexit47234No ratings yet
- PSC Unit 3Document18 pagesPSC Unit 3Santosh ReddyNo ratings yet
- Peavey Xr8000 SCHDocument12 pagesPeavey Xr8000 SCHLisandro Orrego SalvadorNo ratings yet
- Bending Stresses in BeamsDocument25 pagesBending Stresses in Beamsrajatapc12007No ratings yet
- Quantitative Interpretation of The Response of Surface Plasmon Resonance Sensors To Adsorbed FilmsDocument13 pagesQuantitative Interpretation of The Response of Surface Plasmon Resonance Sensors To Adsorbed FilmsKaren Régules MedelNo ratings yet
- Abstracts: IAFRI Metaldehyde Conference - 13 September - Fera Science LTD, York YO41 1LZDocument6 pagesAbstracts: IAFRI Metaldehyde Conference - 13 September - Fera Science LTD, York YO41 1LZbendel_boyNo ratings yet
- Euca FBB - Jiangxi MillDocument1 pageEuca FBB - Jiangxi MillBill King0% (1)
- Full Download Strategies For Teaching Learners With Special Needs 11th Edition Polloway Test BankDocument36 pagesFull Download Strategies For Teaching Learners With Special Needs 11th Edition Polloway Test Banklevidelpnrr100% (30)
- Total Result 2594 Total Result 2583Document2,897 pagesTotal Result 2594 Total Result 2583anjali shilpa kajalNo ratings yet
- Valorisation of Spent Coffee Grounds Production of Biodiesel Via Enzimatic Catalisis With Ethanol and Co-SolventDocument14 pagesValorisation of Spent Coffee Grounds Production of Biodiesel Via Enzimatic Catalisis With Ethanol and Co-SolventAline GonçalvesNo ratings yet
- Up ListDocument200 pagesUp Listprashant guptaNo ratings yet
- BIOL207 Open GeneticsDocument182 pagesBIOL207 Open GeneticsBi Anh100% (1)
- Module 2 (People and The Earth's Ecosystem)Document11 pagesModule 2 (People and The Earth's Ecosystem)chris ian0% (2)
- 5th Fancy BreadDocument7 pages5th Fancy BreadMera Funportal0% (1)
- CBSE Class 10 Revision WorksheetDocument13 pagesCBSE Class 10 Revision WorksheetEdward DevisNo ratings yet
- Samsung Galaxy S22 Ultra 5G - Full Phone SpecificationsDocument13 pagesSamsung Galaxy S22 Ultra 5G - Full Phone SpecificationsAb BossNo ratings yet
- CPS - Data Intensive Distributed ComputingDocument11 pagesCPS - Data Intensive Distributed ComputingManoj KavediaNo ratings yet
- Basic Monte Carlo TechniquesDocument10 pagesBasic Monte Carlo TechniquesMobeen AhmadNo ratings yet
- STRUCTURE Magazine - Condition Assessment of Old Stone Retaining Walls PDFDocument8 pagesSTRUCTURE Magazine - Condition Assessment of Old Stone Retaining Walls PDFShabbir LokhandwalaNo ratings yet
- Digsi4 DisplayDocument81 pagesDigsi4 Displaymohammed youisfNo ratings yet
- General Twin Seal 06Document24 pagesGeneral Twin Seal 06Gk GaneshNo ratings yet
- Class 9 - ScienceDocument228 pagesClass 9 - ScienceYashwanth KasturiNo ratings yet
- Global Stability Analysis of Eccentric Taylor Couette FlowDocument28 pagesGlobal Stability Analysis of Eccentric Taylor Couette FlowSreekanth MenonNo ratings yet
- Soal Latihan US Bahasa InggrisDocument5 pagesSoal Latihan US Bahasa Inggrispikri18120No ratings yet
- PPM Schedule Anmol Feeds PVT LTD - PanchlaDocument1 pagePPM Schedule Anmol Feeds PVT LTD - PanchlaSatyajit DasNo ratings yet
- BusDocument24 pagesBusSyed Noman AhmedNo ratings yet
- Cryolite JM File 2011Document5 pagesCryolite JM File 2011mutemuNo ratings yet
- Cancer and Its Easy Treatment in Homeopathy - Bashir Mahmud ElliasDocument5 pagesCancer and Its Easy Treatment in Homeopathy - Bashir Mahmud ElliasBashir Mahmud ElliasNo ratings yet
- Raychem Molded PartsDocument28 pagesRaychem Molded PartsAMNo ratings yet