Professional Documents
Culture Documents
21-Nature Reviews Cancer-Antitumour Immunity Regulated by Aberrant ERBB Family Signalling
21-Nature Reviews Cancer-Antitumour Immunity Regulated by Aberrant ERBB Family Signalling
Uploaded by
zhe zhCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
21-Nature Reviews Cancer-Antitumour Immunity Regulated by Aberrant ERBB Family Signalling
21-Nature Reviews Cancer-Antitumour Immunity Regulated by Aberrant ERBB Family Signalling
Uploaded by
zhe zhCopyright:
Available Formats
Reviews
Antitumour immunity regulated
by aberrant ERBB family signalling
Shogo Kumagai1,2,3, Shohei Koyama2,3 and Hiroyoshi Nishikawa 1,2,3 ✉
Abstract | Aberrant signalling of ERBB family members plays an important role in tumorigenesis
and in the escape from antitumour immunity in multiple malignancies. Molecular-targeted
agents against these signalling pathways exhibit robust clinical efficacy, but patients inevitably
experience acquired resistance to these molecular-targeted therapies. Although cancer
immunotherapies, including immune checkpoint inhibitors (ICIs), have shown durable antitumour
response in a subset of the treated patients in multiple cancer types, clinical efficacy is limited in
cancers harbouring activating gene alterations of ERBB family members. In particular, ICI
treatment of patients with non-small cell lung cancers with epidermal growth factor receptor
(EGFR) alterations and breast cancers with HER2 alterations failed to show clinical benefits,
suggesting that EGFR and HER2 signalling may have an essential role in inhibiting antitumour
immune responses. Here, we discuss the mechanisms by which the signalling of ERBB family
members affects not only autonomous cancer hallmarks, such as uncontrolled cell proliferation,
but also antitumour immune responses in the tumour microenvironment and the potential
application of immune-genome precision medicine into immunotherapy and molecular-targeted
therapy focusing on the signalling of ERBB family members.
Neoantigens
Members of the ERBB tyrosine kinase family present with sparse infiltration of T cells exhibit a waning of
Antigens derived from gene some of the most commonly altered proteins in cancer, neoantigen expression or copy-number loss of clonal
alterations in tumour cells. and aberrant tyrosine kinase activation through gene neoantigens during tumour development, suggesting
As they are recognized as alterations can drive tumorigenesis, tumour growth previous immuno-editing7. In addition, cancer cells
foreign bodies by the immune
and progression. Oncogenic alterations of genes encod- develop certain assets, such as inactivating alterations in
system, strong immune
responses are generally ing members of the ERBB family, leading to aberrant genes encoding interferon-γ (IFNγ) receptor and major
induced. ERBB signalling and driving tumour growth, have histocompatibility complex (MHC) molecules, which
been reported in various types of cancer including can hamper and gradually decay antitumour immune
breast, lung, head and neck, brain and gastrointestinal responses (equilibrium). Cancer cells acquire various
cancers1,2. Thus, molecular-targeted therapies, including immune escape mechanisms, including the recruitment
tyrosine kinase inhibitors (TKIs), monoclonal antibodies of immunosuppressive cells and elevated expression of
(mAbs) and antibody–drug conjugates (ADCs), target- various immunosuppressive molecules, such as immune
ing oncogenic epidermal growth factor receptor (EGFR) checkpoint molecules (escape). Consequently, these cells
1
Department of Immunology, or human epidermal growth factor receptor 2 (HER2) form clinically apparent cancers8. Thus, the expression of
Nagoya University Graduate
signalling have been developed and successfully used in immune checkpoint molecules by cancer cells is one
School of Medicine,
Nagoya, Japan.
the clinic, resulting in improved survival of patients with of the essential requirements for cancer development9,
2
Division of Cancer
cancers harbouring these gene alterations3–5. Yet, it is dif- indicating the possibility that full engagement of anti
Immunology, Research ficult to gain a long-lasting clinical benefit with these tumour immune responses may regain control of tumour
Institute, National Cancer molecular-targeted therapies, indicating the importance growth and progression. Indeed, immune checkpoint
Center, Tokyo, Japan. of developing more effective cancer therapies6. inhibitors (ICIs) have been proven to be clinically effi-
3
Division of Cancer Based on the cancer immuno-editing hypothesis, cient and have become a new standard treatment in
Immunology, Exploratory the immune system eradicates developing cancer cells various types of cancer. Although patients with cancer
Oncology Research & Clinical
Trial Center (EPOC), National
(elimination). In the initial phase of tumour develop- with a high tumour mutation burden (TMB) are thought
Cancer Center, Chiba, Japan. ment, some cancer cells reduce their immunogenicity by to respond to ICIs10–13, not only the absolute number of
✉e-mail: hnishika@ncc.go.jp decreasing the expression of abnormal proteins that can non-synonymous mutations but also mutational signa-
https://doi.org/10.1038/ otherwise be readily recognized by the immune system tures, such as smoking-related or APOBEC signatures,
s41568-020-00322-0 as neoantigens. A previous study showed that tumours have been demonstrated to correlate with the sensitivity
Nature Reviews | CAncER volume 21 | March 2021 | 181
Reviews
Antibody-dependent
to ICIs in several cancer types10,11,14,15. In addition, the and autocrine ligand-receptor stimulation35,51–54 (Table 1).
cellular cytotoxicity gene expression profile related to T cell accumulation These gene alterations abnormally activate EGFR and
(ADCC). When antibodies bind and activation and specific somatic mutations in cancers HER2 signalling, independent of ligand-receptor stim-
to the target cells, especially could have a positive or negative impact on the ther- ulation, resulting in tumorigenesis, tumour growth
cancer cells, immune cells such
as macrophages and natural
apeutic outcome of ICIs independent of the TMB16–18. and progression. The oncogenic functions of HER3
killer cells are attracted. These Moreover, cancer cells with oncogenic driver mutations are largely mediated via its overexpression and interac-
attracted immune cells possess often harbour low numbers of non-synonymous muta- tion with EGFR or HER2 because of its limited kinase
activating Fc receptors that tions, and some oncogenic alterations (for example, activity55–58. The role of HER4 is inconsistent in tumour
recognize the Fc region of the
alterations in STK11, PTEN, RHOA and so on) are asso- development as it has several isoforms, oncogenic iso-
antibody, and kill the targeted
cells to which the antibody
ciated with the resistance of ICIs19–25. By contrast, certain forms and tumour-suppressive isoforms, harbouring
binds through releasing inactivating genomic alterations (for example, ARID1A different activities59–61.
cytotoxic molecules. and so on) correlate with a favourable response to ICIs26.
Therefore, clarifying how specific oncogene alterations Targeting aberrant ERBB signalling
and the resulting intercellular and intracellular signalling Based on significant roles of ERBB signalling in tumor-
immunologically modulate the tumour microenviron- igenesis, tumour growth and progression, specific types
ment (TME) becomes more important with the expan- of agents targeting aberrantly activated ERBB signalling,
sion of cancer immunotherapies to a broad spectrum of such as TKIs, mAbs and ADCs, have been developed
cancer. Recent studies have revealed important roles and established as standard treatment strategies3–5,27.
of the ERBB family in evading antitumour immunity Several TKIs targeting EGFR inhibit kinase domain
in many cancer types, including breast, lung, head and binding to endogenous ATP1, suppress the tyrosine-
neck, brain and colon cancers3,27. phosphorylating activities of EGFR and prevent its
Despite the striking antitumour effects of ICIs28,29, downstream signalling. Subgroups of patients with
their clinical efficacy against cancers harbouring gene non-small cell lung cancer (NSCLC) harbour hyperac-
alterations of ERBB family members is limited, indicat- tivated EGFR based on the L858R mutation in exon 21
ing that ERBB family members may play an important or small deletions in exon 19 (ref.62) — these subgroups
role in evading the antitumour immune response20,30,31. of patients experience tumour regression in response
Here, we summarize how the aberrant signalling of to first-generation EGFR-TKIs6,49. However, acquired
ERBB family members impairs antitumour immune resistance to EGFR-TKIs develops after 9–14 months
responses by modulating the immunological landscape and about half of the cases with acquired resistance
of the TME and how therapeutic targeting helps to over- harbour the T790M mutation in EGFR63. Lapatinib,
come the resistance of tumours with alterations in ERBB one of the first-generation EGFR–HER2-TKIs, revers-
family genes to ICIs. ibly binds to the ATP-binding pocket and suppresses
the PI3K–AKT and MAPK pathways in HER2+ solid
ERBB family signalling cancers64–66. HER2 reactivation through acquisition
ERBB family members of the HER2 L755S mutation has been reported as a
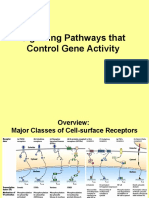
ERBB family members (ERBB1–ERBB4; also known mechanism of acquired resistance to lapatinib in HER2+
as EGFR, HER2, HER3 and HER4) are receptor tyro breast cancer67.
sine kinases (RTKs), each comprising an extracellular Compared with TKIs, mAbs inhibit ERBB family
ligand-binding domain, a single hydrophobic transmem- members (EGFR, HER2 and HER4) in different ways.
brane region and an intracellular segment with a tyrosine EGFR-targeted mAbs prevent ligands from binding
kinase domain32. The ligands for EGFR, HER3 and HER4 to EGFR and exhibit clinical efficacy through attenu-
are well studied33 and downstream signalling pathways ating downstream ERK signalling in cancers harbour-
activated by ERBB family members are interconnected ing wild type (WT) EGFR activated by ligand-receptor
and overlapping1,2,34,35 (Fig. 1). Two major representa- stimulation68–72. In inflammatory breast cancer, in vitro
tive signalling pathways are the phosphatidylinositol-3 experiments with human cancer cell lines showed that
kinase (PI3K)–AKT–mammalian target of rapamycin EGFR signalling promotes inflammation and cancer
(mTOR) and mitogen-activated protein kinase (MAPK) stem cell-like activity73. The phase II study evaluating the
pathways1,2,36,37, in addition to the phospholipase Cγ safety and efficacy of panitumumab plus neoadjuvant
(PLCγ)–protein kinase C (PKC)38,39 and Janus kinase 2 chemotherapy in patients with HER2– inflammatory
(JAK2)–signal transducer and activator of transcription breast cancer showed fairly good efficacy (pathological
3 (STAT3) pathways40,41. From an immunological view- complete response rate: 28%)72. The result of an ongoing
point, EGFR or HER2 signalling inhibits IFNγ responses randomized study should be awaited.
and suppresses expression of interferon regulatory fac- mAbs targeting HER2 are often used in the treatment
tors (IRFs) and inflammatory chemokine production via of HER2+ solid cancers4,74–80 and inhibit dimerization of
PI3K–AKT pathways20,42–45 (Fig. 2). HER2 and/or other ERBB family members, which is
independent of ligand-receptor stimulation, leading to
ERBB gene alterations in tumours inhibition of downstream signalling and induction of
Gene alterations of the ERBB family cause tumorigen antibody-dependent cellular cytotoxicity (ADCC)81–86.
esis, tumour growth and progression in multiple solid Antitumour activities of several mAbs against HER3
cancers1,3,6,27,46–50. Aberrant activation of EGFR and HER2 have also been investigated. mAbs against HER3 pre-
in cancer cells can be induced by various mechanisms, vent phosphorylation induced by ligand-receptor bind-
including gene amplification, point mutations, deletions ing, resulting in reduced HER3 expression on the cell
182 | March 2021 | volume 21 www.nature.com/nrc
Reviews
Multiple ligands: EGF, Impaired Multiple ligands: surface87,88. However, sufficient clinical efficacy of these
HB-EGF, BTC, TGFα, ligand-binding NRG1–NRG4 , BTC, mAbs has not been shown89.
AREG, EPGN or EREG domain NRG1–NRG4 HB-EGF or EREG
In addition to these reagents, one promising strategy
is an ADC that can specifically deliver its payload, a cyto-
EGFR HER2 HER3 HER4 toxic agent, to the targeted cancer cells by binding to tar-
get molecules, resulting in the internalization and release
Impaired of the cytotoxic agent in the cancer cells90. In terms of
Tyrosine
tyrosine ERBB family members, ADCs are being investigated
kinase with mAbs against EGFR, HER2 and HER3. Of these,
kinase domain
domain several ADCs derived from anti-HER2 mAbs have been
investigated91 and have exhibited encouraging clinical
efficacy and been approved for patients with solid cancers
with HER2 amplification5,92–96. Clinical efficacy of a novel
RAS NCK1 PLCγ PI3K JAK
HER3-targeting ADC, U3-1402, is under investigation97.
Mechanisms of resistance to ERBB-targeted therapies
RAF PAK PKC AKT STAT3 have been investigated over the last decades. The com-
mon resistance mechanisms of TKIs, mAbs and ADCs
MEK JNK TSC2 include upregulation of downstream signalling pathways,
signalling through alternate RTK pathways, upregulation
of anti-apoptotic pathways and histological transforma-
ERK JUN AP1 FOS RHEB tions. One of the TKI resistance mechanisms is based
on acquisition of additional mutations in the tyrosine
mTOR kinase domain. Secondary gene alterations in EGFR or
HER2 include second-site mutations that weaken the
efficacy of TKIs and, less often, amplifications or loss of
S6K 4E-BP1 the targeted genes. There are several forms of second-site
mutations with structural and functional character-
S6 istics: gatekeeper mutations (such as EGFR T790M),
covalent binding site mutations (such as EGFR C797S,
HER2 C805S), solvent-front mutations (such as EGFR
Nucleus Gene transcription Translation G796S/R) and so on98–101. Defects in binding to the tar-
get cause resistance to anti-EGFR mAb or anti-HER2
mAb. The EGFR S492R mutation contributes to acquired
DNA resistance to cetuximab but keeps tumours sensitive
Cell proliferation and survival Tumour cell
to panitumumab102. HER2 truncations (p95) are not
recognized by trastuzumab, pertuzumab or T-DM1
(ref.103). The mechanisms of resistance to ERBB-targeted
Fig. 1 | Signalling pathways caused by ERBB family members. ERBB family therapies are summarized in Table 2.
members (ERBB1–ERBB4; also known as epidermal growth factor receptor (EGFR),
human epidermal growth factor receptor 2 (HER2), HER3 and HER4) are receptor Immunology of EGFR-mutant tumours
tyrosine kinases (RTKs) harbouring an analogous structure, which comprise an Tumour-infiltrating immune cells
extracellular ligand binding domain, a single hydrophobic transmembrane region Tumour mutation burden and CD8+ T cell infiltration.
and an intracellular tyrosine kinase domain (except for HER3). Among the EGFR Cancer cells harbour somatic mutations that generate
ligands, EGF, transforming growth factor-α (TGFα), amphiregulin (AREG) and epigen non-self proteins, peptides of which can be presented
(EPGN) interact solely with EGFR, whereas epiregulin (EREG), heparin-binding to the immune system as tumour-specific antigens
EGF-like growth factor (HB-EGF) and betacellulin (BTC) also bind to and activate such as neoantigens, and/or epigenetic alterations that
HER4. A family of EGF-related ligands, neuregulins (NRGs; composed of NRG1–NRG4)
lead to high or aberrant expression of normal proteins,
bind to HER3 and HER4. HER2 directly binds to none of these EGF-related ligands.
HER3 is considered to have an impaired tyrosine kinase domain and to provide little which are referred to as tumour-associated antigens in
kinase activity. Therefore, in order to activate and provide signalling of HER2 and the process of tumour development13,104. It is thought
HER3, their heterodimerization with other ERBB family members is needed32,320–323. that tumours harbouring a high level of neoantigens
Downstream signalling pathways activated by ERBB family members overlap and exhibit robust inflammation, with high levels of effec-
influence each other. In phosphatidylinositol-3 kinase (PI3K)–AKT–mammalian tor T cells that are specific for these antigens. The TMB
target of rapamycin (mTOR) pathways, AKT phosphorylates and inhibits the tumour is the total amount of gene alterations (substitutions,
suppressor TSC2, thereby activating RHEB, which positively regulates mTOR. insertions and deletions) and is thought to correlate
mTOR upregulates the canonical mRNA translation through activation of ribosomal with higher levels of neoantigens. The TMB is there-
protein S6 kinase (S6K) and suppression of eukaryotic translation initiation factor fore considered to be a biomarker of the clinical efficacy
4E-BP1, and is strongly associated with cell proliferation. RAS–RAF–MEK–ERK
of ICIs105. There is intertumoural diversity of the lev-
contributes to cell survival, proliferation and growth. NCK adaptor protein 1
(NCK1)–p21-activated kinase (PAK)–JNK and phospholipase Cγ (PLCγ)–protein els of TMB and the potential neoantigenicity of each
kinase C (PKC) lead to activation of the dimeric activator protein 1 (AP1) mutation is variable depending on the diversity of the
transcription factor that promotes tumorigenesis. The Janus kinase 2 (JAK2)–signal patients, such as MHC12. Consequently, the TME exhib-
transducer and activator of transcription 3 (STAT3) pathway contributes to cell its different immune landscapes, referred to as inflamed
proliferation. or non-inflamed (indicative of the high or low levels of
Nature Reviews | CAncER volume 21 | March 2021 | 183
Reviews
effector T cell infiltration observed in these tumours, non-smoking patients with EGFR-WT NSCLCs,
respectively). Tumours with alterations in ERBB family which potentially leads to the relatively low TMB of
genes, particularly EGFR alterations, frequently develop EGFR-mutated NSCLCs110.
non-inflamed TMEs 20,30,31,106,107. The non-inflamed
TMEs of tumours with EGFR alterations are thought to Regulatory T cell infiltration. Regulatory T cells
be reflective of and caused by their low TMB20,30,31,106,108. (Treg cells) are immunosuppressive CD4+ T cells express-
A previous clinical study suggests that the TMB of ing the master transcription factor, forkhead box pro-
EGFR-mutated NSCLCs is significantly lower than that tein P3 (FOXP3), and play essential roles in maintaining
of EGFR-WT NSCLCs, resulting in impaired clinical self-tolerance111. Tumour-infiltrating Treg cells also sup-
responses to ICIs108. The relatively low TMB in patients press antitumour immunity112, and predict unfavourable
with EGFR-mutated NSCLCs could be explained by outcomes of PD1 blockade therapy, particularly when
the high prevalence of non-smokers among patients harbouring high PD1 expression113,114. As Treg cell migra-
with EGFR-mutated NSCLCs and sufficient strength tion is mostly induced by chemokine networks in the
of oncogenic EGFR signalling for carcinogenesis109. TME, Treg cells are often accompanied by effector T cells
Additionally, patients with EGFR-mutated NSCLCs in the inflamed TME112,115,116. However, EGFR-mutated
reportedly show lower APOBEC signatures than NSCLCs with a non-inflamed TME contain abundant
EGFR
Tumour Tyrosine kinase domain Activating gene alteration IFNγ
cell
IFNγ
NCK1 PLCγ RAS JAK2 PI3K RAS JAK2 PI3K
receptor
NF-κB IRF1
IL-6 NF-κB
CCL22 • IL-6 CXCL10
• IL-8
• IL-10 Myeloid cell
• VEGF Pro-tumoral
↑ NKG2D inflammation
ligand • Immuno-
suppressive
cytokines
• Pro-tumoral
cytokines
NKG2D EGFR ligand • EGFR ligands
NK PI3K
cell
↑ Treg M1 ↑ M2 ↓ CD8+ GSK3β
↓ DC
cell TAM TAM T cell
FOXP3 degradation
EGFR EGFR EGFR EGFR
signalling signalling signalling signalling Treg cell
inhibition inhibition inhibition inhibition
↓ Treg ↑ M1 ↓ M2 ↑ CD8+ ↑ Adenosine AMP ATP
cell ↑ DC T cell
TAM TAM
CD73 CD39
Tumour cell
Fig. 2 | The effects of EGFR signalling on immune cells in the TME. EGFR ligands. In addition, EGFR signalling in myeloid cells induces
Cancers with activating alterations in the epidermal growth factor pro-tumoural inflammation and leads to increased expression of EGFR
receptor (EGFR) gene commonly establish the non-inflamed tumour ligands, such as HB-EGF. EGFR signalling in Treg cells prevents glycogen
microenvironment (TME). EGFR signalling downregulates CXC-chemokine synthase kinase 3β (GSK3β) from degrading forkhead box protein P3
ligand 10 (CXCL10), concurrent with interferon regulatory factor 1 (IRF1), a (FOXP3), enhancing the immunosuppressive function of Treg cells.
positive regulator of CXCL10, via phosphatidylinositol-3 kinase (PI3K)–AKT Consequently, EGFR-tyrosine kinase inhibitor or anti-EGFR treatment
pathways, resulting in the reduction of effector CD8+ T cells. Regulatory (summarized as EGFR signalling inhibition in the figure) increases
T cells (Treg cells) are recruited in the non-inflamed TME of EGFR-mutated the numbers of CD8 + T cells, dendritic cells (DCs) and M1-like
cancers by upregulating CC-chemokine ligand 22 (CCL22) expression tumour-associated macrophages (TAMs) and decreases Treg cell infiltration,
through JNK–JUN activation. RAS–RAF–MEK–ERK, Janus kinase 2 (JAK2)– resulting in the inhibition of conversion of M1-like TAMs to M2-like TAMs.
signal transducer and activator of transcription 3 (STAT3) and PI3K–AKT– IFNγ, interferon-γ; NCK1, NCK adaptor protein 1; NK cell, natural killer cell;
nuclear factor-κB (NF-κB) pathways produce pro-tumoural cytokines and PLCγ, phospholipase Cγ.
184 | March 2021 | volume 21 www.nature.com/nrc
Reviews
Table 1 | Alterations of genes encoding ERBB family members and their ligands motility and localization of tumour-specific cytotoxic
T cells through nitric oxide synthase (iNOS)122 and
Gene Alteration Type of cancer induce M2 TAMs123, resulting in impaired antitumour
EGFR Mutation NSCLC and glioma immunity. By contrast, a study has revealed that EGFR
Amplification Head and neck cancer, oesophageal cancer, NSCLC, expression positively correlates with the expression of
colorectal cancer and glioma ligands for natural killer cell activating receptor NKG2D
HER2 Mutation Breast cancer, NSCLC and gastric, bladder and endometrial in cancer cells, which is reduced by EGFR-TKIs124. It is
cancer therefore important to test in clinical studies whether
Amplification Breast, gastric and oesophageal cancer patients with EGFR-overexpressing or EGFR-mutated
tumours express NKG2D ligand at higher levels than
HER3 Mutation Breast and gastric cancer patients with EGFR-WT tumours or whether natu-
HER4 Mutation NSCLC, melanoma and medulloblastoma ral killer cells accumulate and activate in the TME of
TGFA Overexpression Lung, pancreas, prostate, ovary, colon and head and EGFR-overexpressing or EGFR-mutated tumours.
neck cancer
NREG Overexpression Colorectal and head and neck cancer EGFR inhibition interacts with immune cell infiltration.
NSCLC, non-small cell lung cancer.
EGFR-mutated cancer cells also overproduce negative
immune modulators, such as TGFβ, IL-10, VEGF, IDO,
ARG1 and adenosine, which can directly suppress nat-
levels of Treg cells and macrophages, the latter of which ural killer cell killing, dendritic cell maturation and
can produce chemokines recruiting more Treg cells in the cytotoxic T cell function and proliferation, although
inflamed TME (Fig. 2). A preclinical lung cancer mouse the detailed mechanism(s) remains to be determined125.
model with activating EGFR mutations also demon- Therefore, EGFR-TKI treatment potentially breaks this
strated the upregulation of Treg cell-associated genes in negative spiral of immune suppression in the TME of
the lung early after induction of aberrantly upregulated EGFR-overexpressing or EGFR-mutated tumours. As
EGFR signalling117. We have recently shown that, in such, short-term EGFR-TKI treatment of EGFR-mutated
addition to the low TMB, EGFR signalling downreg- lung tumours in mouse models increased the numbers
ulates CXC-chemokine ligand 10 (CXCL10), which is of CD8+ T cells, dendritic cells and M1-like TAMs and
known to recruit effector CD8+ T cells44,45, concurrent decreased Treg cell infiltration, resulting in the inhibition
with IRF1, a positive regulator of CXCL10, via PI3K– of the conversion of M1-like TAMs to M2-like TAMs126.
AKT pathways20,42,43. Moreover, Treg cells are recruited to The percentage of mononuclear myeloid-derived sup-
the non-inflamed TMEs of tumours with EGFR muta- pressor cells (MDSCs), which are immunosuppressive,
tions by upregulating CCL22 expression via the JNK– in lung tumours was elevated throughout the treat-
cJun pathway, which has been shown using a murine ment period. After prolonged EGFR-TKI treatment,
model with cell lines transduced with EGFR 19del20,116. no significant change or even a decrease in antitumour
Consequently, EGFR-TKI treatment can promote the effector cells and increasing secretion of IL-10 and
recruitment of CD8+ T cells and inhibit Treg cell infiltra- CCL2 in serum are observed as compared with the
tion in the TME of EGFR-mutated tumours in vivo20. untreated group126.
Thus, the mechanism behind the non-inflamed pheno In clinical studies, CD8 + or FOXP3 + tumour-
type seems to be that EGFR signalling not only pre- infiltrating lymphocyte (TIL) densities were investi-
vents the recruitment of effector CD8+ T cells but also gated in paired clinical EGFR-mutated NSCLC tis-
promotes Treg cell infiltration. Furthermore, it has been sue samples obtained from patients before and after
shown that EGFR blockade by antibodies or kinase acquired resistance to EGFR-TKI treatment127. The
inhibitors promotes the secretion of chemokines (CCL2, densities of both CD8+ and FOXP3+ TILs were signifi-
CCL5 and CXCL10) in head and neck squamous cell cantly decreased after acquired resistance to EGFR-TKI
carcinoma (HNSCC) cells and keratinocytes upon treatment. In this study, however, 48% of patients
IFNγ and tumour necrosis factor (TNF) stimulation received cytotoxic chemotherapy between the termi-
in vitro118,119. Together, EGFR signalling negatively affects nation of EGFR-TKI treatment and re-biopsy of tis-
T cell accumulation in the TME through modulating the sue specimens, thus it is difficult to conclude that this
chemokine milieu. immunological phenotype derived only from acquired
resistance to EGFR-TKI. Single-cell RNA sequencing of
Innate immune cells and stromal cells. In addition to EGFR-mutated NSCLC biopsies from patients showed
modulating acquired immunity such as T cell balance that whereas EGFR-TKIs were effective, more CD8+
through chemokines, EGFR signalling influences the T cell infiltration and less macrophage infiltration were
characteristics of innate immune cells and stromal cells observed than before EGFR-TKI treatment. On the
in the TME. EGF secreted by colon cancer cells pro- other hand, when tumours were resistant to EGFR-TKI
motes M2 polarization of tumour-associated macro treatment, the infiltration of fewer CD8+ T cells and
phages (TAMs), which are associated with suppression of more macrophages in the TME were found than
of cytotoxic T cell function120. In some cases, podopla- when EGFR-TKIs were effective128. However, epithelial–
nin (PDPN)+ cancer-associated fibroblasts infiltrate into mesenchymal transition is one of the major mechanisms
the TME of EGFR-mutated lung adenocarcinomas and of acquired resistance to EGFR-TKI treatment129–131. TGFβ
induce primary resistance to EGFR-TKIs in patients121. is often upregulated in cancer cells with mesenchymal
PDPN + cancer-associated fibroblasts regulate the phenotypes132, resulting in inhibition of effector T cell
Nature Reviews | CAncER volume 21 | March 2021 | 185
Reviews
Table 2 | Mechanisms of resistance to ERBB-targeted therapies
Mechanism Therapy Molecular mechanism Refs
Mutation of the tyrosine kinase EGFR-TKI EGFR T790M, exon 20 insertions, C797S, 98–101
domain G796S/R
HER2-TKI HER2 T798I, C805S, exon 20 insertions 266,267
EGFR mAb EGFR S492R 102
HER2 mAb/HER2-targeted ADC p95HER2 (lacking extracellular domains) 103
Mucin 4 (masking the epitope) 268
CD44–hyaluronan polymer complex 269,270
(masking the epitope)
Upregulation of downstream EGFR-TKI, EGFR mAb RAS–RAF pathway upregulation 271–277
signalling pathways
HER2 and EGFR-TKI, HER2 mAb, PI3K–AKT pathway upregulation 129,278–286
EGFR-TKI, HER2-targeted ADC
EGFR-TKI JAK–STAT pathway upregulation 287–290
EGFR-TKI SRC activation 291,292
Signalling through alternate EGFR-TKI, HER2 and EGFR-TKI, Other ERBB members upregulation 293–296
RTK pathways HER2 mAb (including their ligands)
EGR-TKI IGF1R upregulation 297,298
EGFR-TKI, HER2 mAb MET upregulation 129,299–302
EGFR-TKI AXL upregulation 303,304
Upregulation of anti-apoptotic HER2 and EGFR-TKI, EGFR-TKI Low expression of BIM 305–307
pathways
EGFR-TKI High expression of YAP1 308
HER2 mAb Downregulation of CDK inhibitors 85,309
Histological transformation EGFR-TKI Small cell transformation 129,310
EGFR-TKI Epithelial–mesenchymal transformation 129–131
Defects in ADCC HER2 mAb FcγR III polymorphism 311
Drug efflux pump HER2-targeted ADC MRP1/MDR1/MDR4 induction 286,312
Trafficking protein modulation HER2-targeted ADC CAV1 upregulation (co-localizing in 313,314
caveolae and not lysosomes)
Lysosomal defects HER2-targeted ADC SLC46A3 (lysosomal transporter) 286,315
downregulation
ADC, antibody–drug conjugate; ADCC, antibody-dependent cellular cytotoxicity; EGFR, epidermal growth factor receptor;
HER2, human epidermal growth factor receptor 2; JAK, Janus kinase; mAb, monoclonal antibody; mTOR, mammalian target
of rapamycin; PI3K, phosphatidylinositol-3 kinase; RTK, receptor tyrosine kinase; STAT, signal transducer and activator of
transcription; TKI, tyrosine kinase inhibitor.
function, downregulation of MHC class I in cancer cells immune responses against infection and cancer140,141.
and accumulation of immunosuppressive cells such as Two different mechanisms regulating MHC expres-
Treg cells and macrophages133–137 and cancer-associated sion in human malignancies have been noted142. One
fibroblasts138. Therefore, larger clinical studies addressing mechanism is the transcriptional regulation of MHC
these issues are warranted. expression under physiologic conditions143. Constitutive
MHC expression is regulated by distinct regions within
MHC expression MHC promoters, to which transcription factors such as
MHC is important for the presentation of tumour anti- nuclear factor-κB (NF-κB), IRF1 and cAMP-responsive
gens to T cells. MHC class I molecules bind antigen element-binding protein (CREB) for MHC class I and
peptides of 8–10 amino acids and are expressed on the class II major histocompatibility complex transactiva-
surface of almost all nucleated cells, and MHC class I– tor (CIITA) for MHC class II can bind. Another mech-
peptide complexes present antigenic information to anism is the induced regulation of MHC expression in
CD8+ T cells. CD8+ T cells recognize cognate antigens response to certain cytokines: type I interferons, IFNγ
and are thus involved in immune surveillance against and TNF for MHC class I; and IFNγ for MHC class II.
non-self components such as malignancies and infec- MHC molecules are upregulated via changes in tran-
tions. MHC class II molecules bind antigen peptides scription factors and/or co-activators caused by these
of 10–20 amino acids and are constitutively expressed cytokines144. In cancer settings, MHC molecules play an
on the surface of antigen-presenting cells, including important role in presenting tumour antigens to T cells
B cells, macrophages and dendritic cells139, and MHC to induce antitumour immune responses145,146. However,
class II–peptide complexes present antigenic informa- tumours are equipped with several immunosuppressive
tion to CD4+ T cells. Activated CD4+ T cells help various mechanisms to escape antitumour immune responses147.
186 | March 2021 | volume 21 www.nature.com/nrc
Reviews
One typical example is the downregulation of the surface an anti-EGFR mAb, could upregulate MHC class I and
expression of MHC molecules. This downregulation is MHC class II expression induced by IFNγ in primary
caused by various mechanisms, including the genetic human keratinocytes and a malignant keratinocyte
loss of the MHC locus and epigenetic silencing145,148–151. cell line165. In head and neck cancer cell lines, erlotinib,
Some studies, which focus on the interaction between dacomitinib (a pan-ERBB inhibitor) and cetuximab
EGFR signalling and MHC molecules, have shown that promote the induction of MHC class II expression by
EGFR ligands, EGF and TGFα, reduce the expression IFNγ166,167. In studies using NSCLC cell lines with EGFR
of both MHC class I and MHC class II molecules152–155 mutations, gefitinib increased MHC class I expression
(Fig. 3). PI3K–AKT pathways, which are downstream of in cancer cells168. Additionally, the tumour-derived
EGFR signalling, also suppress MHC class I and MHC exosomes containing activated EGFR signalling play
class II expression156–158. Accordingly, EGFR inhibition a role in the suppression of interferon signalling by
in human cell lines in vitro increased the expression of triggering the activation of MEK kinase 2, leading to a
both MHC class I and MHC class II along with other decrease in MHC expression169.
important components of antigen presentation, includ-
ing transporters associated with antigen processing 1 Immunosuppressive molecule expression
(TAP1), TAP2 and β2-microglobulin (β2M)106. In EGFR- The expression of PDL1, which is one of the most
mutated human lung cancer cell lines, MHC class I important immune checkpoint molecules, is induced
expression is significantly downregulated compared by two different mechanisms: genetic alterations (that
with that in EGFR-WT cell lines in response to IFNγ is, amplification, fusion and 3ʹ untranslated region dis-
in vitro159. As discussed above20, the downregulation ruption, leading to intrinsic expression) and inflam-
of IRF1 via PI3K–AKT pathways in lung cancer cells mation (that is, IFNγ stimulation, leading to acquired
with EGFR alterations supports the notion that mutated expression) in cancer cells170–172. PDL1 expression is
EGFR signalling negatively regulates IFNγ signalling, reportedly affected by EGFR signalling via two oppo-
which is essential for MHC class I expression. In addi- site mechanisms in NSCLCs20,117,173 (Fig. 3). Intrinsically,
tion to the PI3K–AKT pathways, EGFR-downstream PDL1 expression is upregulated by activation of the
MAPK pathways, especially phospho-ERK, are negative PI3K–AKT, RAS–RAF–MEK–ERK or JAK–STAT3
regulators of MHC class I expression160. Indeed, MHC pathway by EGFR signalling117,173–176. Accordingly, a
class I and MHC class II expression is elevated when sublethal dose of in vitro EGFR-TKI treatment reduces
MAPK pathways in cancer cells are suppressed by several PDL1 expression in cell lines through inhibiting EGFR
inhibitors, such as BRAF or MEK inhibitors160–164. TKIs signalling117. On the other hand, PDL1 expression is also
(such as PD168393 and AG1478) as well as cetuximab, regulated by IFNγ via IRF1 signalling20. In our study,
EGFR ERBB HER2
Tyrosine kinase Activating Tumour
domain gene alteration cell IFNγ
IFNγ
receptor
RAS JAK2 PI3K RAS PI3K
↓ IRF1 ↓ IRF3
AKT Endosome
↓ Type I/II interferon ↓ Type I/II interferon TBK1
EGFR HER2
heterodimer dsDNA
signalling cGAS or
signalling STING
inhibition cGAMP
inhibition
↑ Type I/II interferon ↑ Type I/II interferon
↓ MHC PDL1
class I or II HER2
heterodimer
EGFR signalling signalling
inhibition inhibition
↑ MHC class I or II
Fig. 3 | Reduced antigenicity in EGFR-mutated or HER2-amplified transducer and activator of transcription 3 (STAT3) pathways. On the other
cancer. In epidermal growth factor receptor (EGFR)-mutated cancers, hand, PDL1 expression is also upregulated by interferon-γ (IFNγ) via IRF1
phosphatidylinositol-3 kinase (PI3K)–AKT pathways downregulate interferon signalling. In cancers with human epidermal growth factor receptor 2 (HER2)
signalling, via interferon regulatory factor 1 (IRF1; one of the transcriptional amplification, HER2 induces loss of phosphorylation of TANK-binding kinase 1
factors of major histocompatibility complex (MHC)), and RAS–RAF–MEK– (TBK1) and attenuates stimulator of interferon genes (STING) signalling,
ERK pathways also negatively regulate MHC expression. PDL1 expression by resulting in the impairment of interferon signalling, especially IRF3, one of
EGFR-mutated cancers is affected by EGFR signalling via two opposite the transcriptional factors of MHC. Molecular-targeted therapies that inhibit
mechanisms. In cancer cells, PDL1 expression is upregulated by the EGFR or HER2 heterodimer signalling increase the expression of MHC class I
activation of PIK3–AKT, RAS–RAF–MEK–ERK and Janus kinase 2 (JAK2)–signal and MHC class II in EGFR-mutated and HER2+ cancers.
Nature Reviews | CAncER volume 21 | March 2021 | 187
Reviews
EGFR signalling inhibited IRF1 expression, thereby meta-analyses about the efficacy of PD1 blockade, the
inhibiting acquired PDL1 expression by IFNγ in in vitro authors analysed the data of not only NSCLCs but also
experiments using human cell lines20. Therefore, how other types of cancer and demonstrated that signifi-
EGFR signalling affects PDL1 expression is still under cantly prolonged progression-free survival and over-
debate. Nevertheless, in clinical samples, many studies all survival were observed in patients with EGFR-WT
have shown that PDL1 expression assessed by immuno cancers receiving PD1 blockade but not in those with
histochemistry is significantly higher in EGFR-WT EGFR-mutated cancers205. Therefore, EGFR-mutated
NSCLCs than EGFR-mutated NSCLCs108,177–181 and that cancer is generally resistant to ICIs mainly due to its
PDL1 expression is elevated following EGFR-TKI treat- non-inflamed TME.
ment in EGFR-mutated NSCLCs30,127,182. Furthermore, in However, the level of ICI efficacy in EGFR-mutated
one of these studies, two of the five patients who showed NSCLCs varies depending on the types of EGFR
an increase in PDL1 expression in cancer cells tended alterations206,207. As such, EGFR exon 19-deleted cancers
to exhibit a durable clinical response to subsequent ICI exhibit worse response rates than EGFR L858R-mutated
treatment, suggesting that EGFR-TKI treatment may cancers206. This may be partially due to the substantially
favourably affect ICI efficacy127. In addition to PDL1, lower TMB of EGFR exon 19-deleted cancers compared
the expression of PDL2, another ligand for PD1, in with EGFR L858R-mutated cancers207. The TMB is
in vitro experiments with human cancer cell lines could known to increase significantly with age208. The lower
also be regulated by EGFR signalling in NSCLCs183. For TMB of EGFR exon 19-deleted cancers than EGFR
another B7 family molecule, the expression of HERV-H L858R-mutated cancers may be caused by older age at
LTR-associating 2 (HHLA2), which could inhibit T cell diagnosis for EGFR L858R-mutated cancers209,210. TP53
function as an immune checkpoint184, is upregulated in mutations are reported to be associated with higher
clinical specimens from patients with EGFR-mutated TMB among EGFR-mutated cancers, which may reflect
NSCLC as compared with patients with EGFR-WT genetically unstable states caused by co-occurring
NSCLC185. Further investigation of the mechanism(s) mutations207. Recently, several groups have addressed the
regulating HHLA2 expression in EGFR-mutated cancers relationship between EGFR T790M mutation, one of
is warranted. the major causes of acquired resistance to EGFR-TKI,
CD73 is one of the negative immunomodulatory and immunological phenotypes. Lower PDL1 expres-
molecules expressed by multiple cancer types and sion and higher levels of FOXP3+ T cell infiltration were
immune cells that promotes production of adenosine186. observed in EGFR T790M-positive tumours compared
Adenosine functions as an immunosuppressive media- with EGFR T790M-negative tumours, although the
tor in the TME. When adenosine stimulates adenosine underlying mechanism(s) remains to be elucidated211,212.
receptors, including A2AR, on each immune cell, both Moreover, EGFR T790M-mutated tumours show a
infiltration and immunosuppressive activity of Treg cells significantly worse response rate to ICIs than EGFR
and MDSCs are enhanced187–189 and activity of dendritic T790M-WT tumours211,213.
cells, effector T cells, natural killer cells and NKT cells is EGFR alterations other than L858R mutation and
inhibited190–197. Supporting the notion that CD73 pro- exon 19 deletion are known as uncommon mutations,
motes immunosuppression via adenosine and allows such as L861Q and G719X, and are observed in 10–20%
tumour growth, high expression of CD73 is associated of patients with NSCLC harbouring activating EGFR
with poor prognosis in patients with NSCLCs, although alterations214,215. Uncommon EGFR alterations in patients
these data are preliminary198. In addition, higher levels with NSCLCs are associated with heavier smoking
of baseline tumour adenosine signalling are associated history216 and preliminary data show that these types of
with resistance to ICIs in various types of cancer199. In patients harbour a higher TMB compared with patients
preliminary analysis of clinical samples, higher expres- with NSCLCs harbouring common EGFR alterations217.
sion of CD73 is related to EGFR-mutated NSCLCs than The higher TMB may lead to higher PDL1 expression
to EGFR-WT NSCLCs198,200. CD73 expression is induced by tumours and higher frequency of CD8+ T cell infil-
by EGF and is inhibited by EGFR-TKIs in in vitro tration in the TME of NSCLCs harbouring uncommon
experiments200. These findings suggest that aberrant EGFR alterations218. Patients with NSCLCs harbouring
EGFR signalling increases CD73 expression and that the uncommon EGFR alterations reportedly show signifi-
CD73–adenosine axis is another possible immunosup- cantly better response to ICIs than those with NSCLCs
pressive mechanism in EGFR-mutated tumours, which harbouring common EGFR alterations213. Therefore,
is potentially targeted by EGFR-TKI. ICI treatment may be more favourable for patients with
uncommon EGFR alterations than those with common
PD1–PDL1 blockade EGFR alterations. To understand the molecular mech-
All of the immunosuppressive mechanisms in EGFR- anism of improved sensitivity to ICIs in uncommon
mutated cancer discussed above establish a non-inflamed EGFR alteration, immunological analysis comparing
NKT cells TME, resulting in resistance to cancer immunotherapies, common and uncommon EGFR-mutated NSCLCs will
A type of T cells that also including PD1–PDL1 blockade. Several meta-analyses be necessary in addition to evaluating the TMB.
possess the characteristics of on the clinical efficacy of PD1 blockade versus docetaxel In EGFR-altered tumours, to variable degrees
natural killer cells. The T cell in patients with pretreated advanced NSCLCs have depending on the type of EGFR alterations, EGFR sig-
receptors of natural killer
T (NKT) cells recognize
recently reported that ICIs significantly prolonged nalling establishes an immunosuppressive environment,
glycolipids presented on overall survival in the EGFR-WT subgroup but not leading to resistance to ICI treatment. Therefore, in
CD1d molecules as antigens. in the EGFR-mutated subgroup201–204. In one study on order to improve the efficacy of ICIs in EGFR-altered
188 | March 2021 | volume 21 www.nature.com/nrc
Reviews
tumours, it is necessary to target the immunosuppressive ERBB family members has been investigated in immune
factors caused by aberrant EGFR signalling. cells, particularly macrophages and T cells, in the TME
(Fig. 2). EGFR is expressed by macrophages in the TME of
Immunity affected by other ERBB signals both human and mouse cancers, including hepato
Amplification is the most common alteration in HER2, cellular carcinomas and colorectal cancers (CRCs)235,236.
which is found in patients with breast, gastric and Mice lacking Egfr in myeloid cells showed decreased
oesophageal cancers in contrast to other gene altera- carcinogenesis due to the reduction in IL-6 production
tions, such as EGFR alterations. HER2 amplification via STAT3, suggesting a tumour-promoting function by
seems to result in a non-inflamed TME31. In breast myeloid cell-intrinsic EGFR signalling235,236. In addition,
cancers, triple-negative breast cancers harbour the macrophages produce HB-EGF, leading to cell growth
most abundant TILs, whereas relatively low infiltra- and invasion of myxoid liposarcoma through EGFR
tion of TILs is observed in breast cancers with HER2 signalling237. The expression of EGFR is also detected
amplification219–221. Additionally, a subset of breast can- in CD4+ T cells, especially FOXP3+ Treg cells, but not in
cers with HER2 amplification exhibits an inflammatory CD8+ T cells238. Compared with the other EGFR ligands,
phenotype through activation of the PI3K–AKT–mTOR the binding of AREG to EGFR on tumour-infiltrating
pathway, resulting in IL-8 secretion in the TME222,223. Treg cells induces the activation of MAPK pathways,
IL-8 not only promotes malignant phenotypes in can- enhancing the suppressive function of Treg cells 238.
cer cells, including invasion and metastasis222, but also Regarding EGFR ligands, Treg cells themselves pro-
recruits neutrophils into the TME, which contributes to duce AREG, which can promote tumour cell prolifer-
resistance to PD1–PDL1 blockade treatment in several ation via EGFR signalling, in addition to inhibiting the
types of cancer224. HER2 amplification also induces loss antitumour immune response239. However, our study
of phosphorylation of TANK-binding kinase 1 (TBK1) detected little expression of EGFR on tumour-infiltrating
and attenuates stimulator of interferon genes (STING) Treg cells20. Therefore, the function of EGFR in Treg cells
signalling, resulting in impairment of the interferon remains controversial and may be dependent on the
response and antitumour immune responses225 (Fig. 3). pathological condition, such as in the context of cancers
Associations between MHC expression and HER2 and inflammation.
have been investigated for a long time. In studies using
HER2-overexpressing cell lines, the expression of Targeted therapies and combinations
HER2 inversely correlates with MHC class I expres- ERBB family signalling, especially EGFR and HER2
sion and other components of the antigen processing signalling, plays a key role in not only promoting
machinery226. Consistent with these results, knockdown tumour cell proliferation but also inducing a more or
of HER2 or anti-HER2 mAbs leads to an increase in less immunosuppressive TME through multiple mecha
MHC class I expression165,227,228. nisms as described in the above sections. Because the
For PDL1 expression, post-translational modifica- inhibition of ERBB family signalling potentially switches
tions, which include phosphorylation, glycosylation non-inflamed and even immunosuppressive profiles
and ubiquitylation, have been reported to regulate the of tumours with ERBB alterations into inflamed pro-
protein stability of PDL1 and the interaction between files, several combinations of immunotherapy and
PD1 and PDL1 (refs229–232). EGF signalling in breast molecular-targeted therapy for ERBB family signal-
cancer cells stabilizes PDL1 expression through glyco- ling have been under investigation ( Fig. 4; Table 3;
sylation by glycogen synthase kinase 3β (GSK3β)230 and Supplementary Table 1). Combination immunother-
promotes direct interaction between PDL1 and PD1 apies including ICIs and CD73–adenosine axis inhib-
through β-1,3-N-acetylglucosaminyl transferase 232. itors with ERBB targeting agents provide synergistic
Recently, the clinical efficacy of PD1 blockade therapies antitumour immune responses compared with mono
in tumours with HER2 amplification has been evaluated. therapy of either agent alone. TKIs or mAbs against
PD1 blockade therapies have shown limited antitumour EGFR alterations prevent the infiltration of immuno-
efficacy in breast cancers and gastric cancers with HER2 suppressive cells and potentially strengthen antitumour
amplification233,234, although numerous clinical tri- responses, especially in NSCLCs and CRCs20, sug-
als are still ongoing (NCT03032107, NCT03747120, gesting that combination treatment of EGFR-targeted
NCT02605915, NCT03199885, NCT03125928, therapies with ICIs could be a reasonable option as a
NCT03726879 and NCT03417544). Further clinical tri- combination immunotherapy. Whereas the clinical
als testing the clinical efficacy of combinatory immuno trial of the combination therapy of the third-generation
therapies with HER2-targeted therapies, including EGFR-TKI osimertinib with or without durvalumab,
mAbs or ADCs, are ongoing with much expectation an anti-PDL1 antibody, was closed prematurely due
(see the section Targeted therapies and combinations). to the increased incidence of interstitial lung disease240,
As analyses of the TME of cancers with HER3 or HER4 the combination of nivolumab, an anti-PD1 antibody,
alterations are limited, further studies are warranted. with the second-generation EGFR-TKI erlotinib was
well tolerated and showed clinical efficacy in patients
The roles of EGFR in immune cells with erlotinib-resistant advanced EGFR-mutated
ERBB family members are potentially expressed in NSCLCs241. Interestingly, adenocarcinoma with EGFR
various haematopoietic cells and play important func- exon 21 mutations demonstrated favourable clin-
tions in the TME of cancers without alterations of ical outcomes from ICI treatment compared with
ERBB family members. The function of EGFR among EGFR exon 19 deletions due to relatively higher TMB
Nature Reviews | CAncER volume 21 | March 2021 | 189
Reviews
in EGFR exon 21 mutations206,207. Accordingly, fur- subset of EGFR-mutated cancers is the optimal target
ther investigations are necessary to evaluate whether for combination immunotherapies. Recently, Gong et al.
there is an increased risk of developing adverse events have shown that EGFR-TKIs upregulate interferons
when combining PD1–PDL1 blockade with osimerti- not only in EGFR-mutated human cancer cell lines
nib compared with the other EGFR-TKIs and which but also in EGFR-WT human cancer cell lines 242.
a EGFR EGFR inhibitor b EGFR inhibitor
Anti-PD1
↑ CD8+ ↑ CD8+
Tyrosine kinase Activating T cell T cell
domain gene alteration PD1
Tumour dsDNA Cytotoxic
↓ Type I/II chemotherapy
cell
interferon ↑ CXCL10
↓ Suppressive
↑ MHC cytokines
class I or II PDL1
↓ EGFR
ligands VEGF
Anti-PDL1 ↑ DC ↑ DC
↓ CCL22 Anti-VEGF
↓ Treg ↑ M1 ↓ M2 ↓ Treg ↑ M1 ↓ M2
cell TAM TAM cell TAM TAM
HER2 Anti-HER2
c d
EGFR, HER3 or HER4 CD16
↑ NK ADCC
cell
dsDNA
↑ Type I/II ↑ CD8+
↑ CD8+ interferon T cell
T cell
↑ MHC Cytotoxic
class I or II ↑ PDL1 chemotherapy
CD39 CD73 ↓ Adenosine
ATP AMP
Anti-CD73 ↑ DC
A2AR ↑ DC
A2AR
antagonist
↓ Treg ↑ M1 ↓ M2 ↓ Treg ↑ M1 ↓ M2 DC maturation
cell TAM TAM cell TAM TAM
Fig. 4 | Targeting molecular pathways of ERBB family signalling for reduction in immunosuppressive cells, especially regulatory T cells
combination immunotherapies. The concepts of combinations of (Treg cells). This combination treatment strategy may be beneficial to the
immunotherapy and molecular-targeted therapy for molecular pathways treatment of EGFR-TKI-resistant tumours with EGFR mutations. c | CD73
of ERBB family signalling are shown. a | Tyrosine kinase inhibitors (TKIs) mAbs or A2AR antagonists dampen Treg cells and myeloid-derived
(or monoclonal antibodies (mAbs)) inhibiting epidermal growth factor suppressor cells (MDSCs) and enhance the activity of dendritic cells (DCs)
receptor (EGFR) signalling prevent the infiltration of immunosuppressive and effector T cells. d | Anti-human epidermal growth factor receptor 2
cells and potentially strengthen antitumour responses. EGFR-TKIs (anti-HER2) mAbs induce antibody-dependent cellular cytotoxicity
promote the production of interferons and effector T cell-recruiting (ADCC), leading to upregulation of PD1 expression by T cells and of PDL1
chemokines such as CXC-chemokine ligand 10 (CXCL10) by cancer cells expression by tumour cells. Antibody–drug conjugates (ADCs) retain the
and decrease the production of immunosuppressive cytokines and function of anti-HER2 mAbs and induce immunogenic cell death and
chemokines, resulting in improvement of the efficacy of PD1/PDL1 major histocompatibility complex (MHC) class I expression in cancer cells,
blockade. b | VEGF inhibitors are one of the options for combination resulting in DC maturation, differentiation of tumour-associated
treatment with immune checkpoint inhibitors (ICIs). The improved efficacy macrophages (TAMs) into the pro-inflammatory M1 type and increased
of ICIs in combination with anti-VEGF mAb may be attributed to the T cell infiltration.
190 | March 2021 | volume 21 www.nature.com/nrc
Reviews
Table 3 | Combination treatments including immunotherapies in cancers with aberrant ERBB family signalling
Target Evaluation criteria Type of cancer Treatment Clinical trials Refs
EGFR Mutations NSCLC TKI + anti-PD(L)1 mAb NCT01454102, NCT02013219, NCT02040064, 20,240,241,
(or anti-CTLA4 mAb) NCT02088112, NCT02143466, NCT02364609, 316–318
NCT02039674, NCT02574078, NCT02454933,
NCT03083041
Anti-PD(L)1 mAb + anti-VEGF mAb NCT04147351, NCT04426825 –
Chemotherapy + anti-PD(L)1 mAb NCT04405674, NCT03515837 –
Chemotherapy + anti-PD(L)1 mAb + NCT03647956, NCT03786692, NCT02366143, 246,247
anti-VEGF mAb NCT03802240
CD73–adenosine axis blockade + NCT03454451, NCT02503774, NCT03835949, –
anti-PD(L)1 mAb NCT04262375, NCT04262388, NCT03549000,
NCT02754141, NCT03819465, NCT03833440,
NCT03822351, NCT02740985, NCT03207867,
NCT02403193, NCT04262856, NCT03629756,
NCT03846310, NCT03337698
CD73–adenosine axis blockade + NCT03381274
EGFR-TKI
Overexpression HNSCC Anti-EGFR mAb + anti-PD(L)1 mAb NCT01935921, NCT02764593, NCT04429542, 254
(or anti-CTLA4 mAb) NCT02947386, NCT03051906, NCT04305795,
NCT03082534, NCT04297995
HER2 Overexpression Solid tumours Anti-HER2 mAb + anti-PD(L)1 mAb NCT02605915, NCT02649686, NCT04040699, 257,258
including (and anti-CTLA4 mAb) NCT04162327, NCT02689284, NCT03409848,
BC and GC NCT03820141, NCT03988036, NCT04082364,
NCT03219268
Chemotherapy + anti-HER2 mAb + NCT02605915, NCT02901301, NCT03125928, –
anti-PD(L)1 mAb NCT03409848, NCT03414658, NCT04034823,
NCT04082364, NCT03615326
Chemotherapy + anti-HER2 mAb + NCT02605915, NCT03894007, NCT03726879 –
HER2-targeted ADC + anti-PDL1 mAb
HER2-targeted ADC + anti-PD(L)1 mAb NCT03032107, NCT02605915, NCT03523572, 261,262,
(or anti-CTLA4 mAb) NCT04042701, NCT04278144, NCT04280341, 319,320
NCT02924883
HER3 Overexpression BC and GC HER3-targeted ADC + anti-PD(L)1 mAb NA 263
See Supplementary Table 1 for details. ADC, antibody–drug conjugate; BC, breast cancer; EGFR, epidermal growth factor receptor; GC, gastric cancer;
HER, human epidermal growth factor receptor; HNSCC, head and neck squamous cell cancer; mAb, monoclonal antibody; NA, not applicable; NSCLC, non-small
cell lung cancer; TKI, tyrosine kinase inhibitor.
Inhibition of type I interferon signalling enhances mutations. Importantly, the clinical benefit of anti-PDL1
EGFR-TKI sensitivity in EGFR-mutated NSCLCs and mAb was only confirmed when it was administered
makes EGFR-WT/KRAS-mutated NSCLCs sensitive with the anti-VEGF mAb in EGFR-mutated NSCLCs247.
to inhibition of EGFR signalling in immunocompetent The improved efficacy of ICIs in combination with
animals. Perhaps, a combination of EGFR-TKIs and anti-VEGF mAb may be attributed to the reduction in
interferon-neutralizing antibodies could be efficient in immunosuppressive cells, especially Treg cells20,244, yet fur-
patients with NSCLCs, regardless of EGFR gene status. ther studies are needed to elucidate how VEGF blockade
VEGF inhibitors are another option for combi- sensitizes EGFR-mutated cancers to ICIs.
nation treatment with ICIs (Fig. 4b). VEGF-targeted Blockade of the CD73–adenosine axis, such as anti-
therapies have been demonstrated to improve the CD73 mAbs or A2AR antagonists, combined with ICIs
efficiency of EGFR-TKI in EGFR-mutated NSCLCs243 induces T cell activation including cytokine production
and reduce the suppressive immune cells, includ- (IFNγ and granzyme B) and exhibits antitumour effects
ing Treg cells and MDSCs, in clinical trials244,245. Thus, in murine tumours without ERBB alterations248,249 (Fig. 4c).
the inhibition of VEGF signalling can be a reason- Some clinical trials evaluating the efficacy of combination
able option to improve the efficacy of ICIs to treat therapies of A2AR inhibitors or anti-CD73 mAbs with
EGFR-mutated tumours. A clinical trial has revealed ICIs or of anti-CD73 mAbs and the EGFR-TKI osimer
that EGFR-mutated NSCLCs show a clinical benefit tinib, especially in EGFR-mutated NSCLCs, are under
from the combination of atezolizumab, an anti-PDL1 investigation (Table 3).
mAb, with standard first-line platinum-based chemo- The anti-EGFR mAb cetuximab is approved for locally
therapy and bevacizumab, an anti-VEGF mAb246. This advanced and recurrent and/or metastatic HNSCCs and
combination treatment strategy may be beneficial to the metastatic CRCs. Although similar clinical efficacy was
treatment of EGFR-TKI-resistant tumours with EGFR observed in clinical trials of CRCs between cetuximab
Nature Reviews | CAncER volume 21 | March 2021 | 191
Reviews
and the anti-EGFR mAb panitumumab, suggesting that could improve the efficacy of ICIs even in low TMB
preventing ligand binding and promoting the internal- EGFR-mutated tumours, which often exhibit resis
ization of EGFR250 would be the major mechanism of tance to PD1–PDL1 blockade monotherapy. Recently,
action in these drugs, several other studies have demon- promising outcomes were reported in clinical trials in
strated that cetuximab potentially induces ADCC251,252 which combinatory treatment of multikinase inhibi-
and triggers immunogenic cell death253, which is con- tors and ICIs was evaluated in gastric cancer and renal
sidered to be an important mechanism of action, when cell carcinoma264,265. These results may provide a clue
combined with ICIs. Cetuximab treatment upregulates to understanding underlying mechanisms in which
PD1 expression in natural killer cells, and PD1 blockade TKIs can improve the antitumour efficacy of ICIs
increases cetuximab-mediated ADCC against PDL1hi even in low TMB tumours, for example, by modulat-
HNSCC cells, where the majority of tumours express ing immunosuppressive cells. Although the results
EGFR without EGFR amplification254, indicating that the in preclinical models clearly show that EGFR-TKI
combination of anti-EGFR mAb and ICIs could augment treatment improves antitumour response in the TME
both innate and acquired antitumour immune responses and strengthens the efficacy of PD1 blockade treat-
to HNSCC expressing EGFR. In recurrent and/or meta- ment, long term follow-up studies of combinations of
static HNSCC, anti-PD(L)1 mAbs in combination with EGFR-TKI and ICIs or sequential ICI treatment after
cetuximab are being evaluated in phase II clinical trials EGFR-TKI will be necessary to determine significant
(NCT03082534 and NCT03082534). clinical benefits in addition to safety issues. Considering
Similar to anti-EGFR mAbs, anti-HER2 mAbs could the mechanisms of action, the combination of ERBB
be a rational therapeutic partner of ICIs against can- family-targeted mAbs or ADCs with ICIs could
cers with HER2 amplification (Fig. 4d). The anti-HER2 increase innate and acquired immune activation even
mAb trastuzumab prevents HER2 shedding, inhibits in non-inflamed tumours to potentially switch the TME
downstream PI3K–AKT signalling and induces ADCC, towards inflamed tumours. In addition, the combina-
leading to upregulation of PD1 expression by T cells and tion of ERBB family-targeted therapies and genetically
of PDL1 expression by tumour cells in breast cancers engineered immune cell therapies (for example, chi-
with HER2 amplification255,256. Indeed, recent phase Ib meric antigen receptor T cell therapies and TCR T cell
and II clinical trials have achieved promising outcomes therapies) may be examined as a novel treatment strat-
in combination therapies of anti-HER2 mAbs with egy. However, the evidence of clinical benefit for these
ICIs in breast cancer and gastric cancer with HER2 combination therapies is still limited. Further studies
amplification257,258, although the results of a randomized determining the cancer types that respond to combi-
phase III cohort study are still awaited. nation immunotherapies and elucidating the mecha-
ADCs are another attractive treatment modality for nisms of additional or synergistic effect are warranted.
cancers with HER2 amplification when combined with Altogether, combined comprehensive analyses of the
ICIs. ADCs retain the function of anti-HER2 mAbs259, TME to elucidate both immunological and genomic
and their conjugated cytotoxic reagents exert cytotox- landscapes are crucial for achieving immune-genome
icity against cancer cells with HER2 amplification as precision medicine.
well as neighbouring cells (called bystander effects)260.
Cancers with HER2 amplification frequently have Conclusions
intratumoural heterogeneity of HER2 expression. In Aberrant signalling of ERBB family members in cancer
these cancers, bystander effects are therefore required cells contributes to tumour development via the follow-
to increase antitumour efficacy by attacking HER2-low ing two aspects: augmented cell growth and/or survival;
or HER2-negative cancer cells surrounding cancer cells and the establishment of an immunosuppressive TME
with HER2 amplification in the TME, suggesting that via direct regulation of the immune system, enabling
ADCs access and kill target cancer cells independent tumours to escape from antitumour immune responses.
of either the TMB or TILs. The HER2-targeted ADCs Thus, targeting aberrant ERBB family signalling could
T-DM1 and DS-8201 or the HER3-targeting ADC be essential for improving the sensitivity to ICIs, possibly
U3-1402 reportedly augment the antitumour effects of through multiple mechanisms including upregulating
PD1 blockade in preclinical models by inducing immuno the tumour antigen presentation, disturbing and inac-
genic cell death and MHC class I expression in cancer tivating immunosuppressive cells, such as Treg cells and
cells, resulting in dendritic cell maturation, differentia- MDSCs, and downregulating immunosuppressive mol-
tion of TAMs into the pro-inflammatory M1 type and ecules. To optimize cancer immunotherapies in patients
increased T cell infiltration261–263. T-DM1 combined with with gene alterations leading to aberrantly increased
anti-PDL1 mAb atezolizumab versus T-DM1 alone in ERBB family signalling, it is necessary to develop novel
previously treated advanced breast cancer with HER2 therapeutic strategies targeting the immunosuppressive
amplification is being assessed in a randomized phase II pathways caused by aberrant signalling of ERBB family
clinical trial (NCT02924883). members. Targeting signalling with molecular-targeted
Numerous studies have addressed antitumour effi- therapies in combination with cancer immunotherapies
cacy of combinations of ICIs and ERBB-targeted ther- could increase antitumour efficacy, leading to the devel-
apies. Although anti-VEGF mAbs reportedly improve opment of optimal cancer therapy: immune-genome
the efficacy of ICIs in EGFR-mutated NSCLCs, the precision medicine.
detailed mechanisms remain to be determined espe-
cially in clinical settings. Importantly, anti-VEGF mAbs Published online 18 January 2021
192 | March 2021 | volume 21 www.nature.com/nrc
Reviews
1. Yarden, Y. & Pines, G. The ERBB network: 24. Kumagai, S. et al. An oncogenic alteration creates a 49. Pao, W. et al. EGF receptor gene mutations are
at last, cancer therapy meets systems biology. microenvironment that promotes tumor progression common in lung cancers from “never smokers”
Nat. Rev. Cancer 12, 553–563 (2012). by conferring a metabolic advantage to regulatory and are associated with sensitivity of tumors to
2. Roskoski, R. Jr. The ErbB/HER family of protein-tyrosine T cells. Immunity 53, 187–203.e8 (2020). gefitinib and erlotinib. Proc. Natl Acad. Sci. USA 101,
kinases and cancer. Pharmacol. Res. 79, 34–74 25. Koyama, S. et al. STK11/LKB1 deficiency promotes 13306–13311 (2004).
(2014). neutrophil recruitment and proinflammatory cytokine 50. Sugawa, N., Ekstrand, A. J., James, C. D. & Collins, V. P.
Together with Yarden and Pines (2012), this paper production to suppress T-cell activity in the lung Identical splicing of aberrant epidermal growth factor
presents comprehensive reviews of ERBB family tumor microenvironment. Cancer Res. 76, 999–1008 receptor transcripts from amplified rearranged genes
signalling in various types of cancer. (2016). in human glioblastomas. Proc. Natl Acad. Sci. USA 87,
3. Paez, J. G. et al. EGFR mutations in lung cancer: 26. Shen, J. et al. ARID1A deficiency promotes mutability 8602–8606 (1990).
correlation with clinical response to gefitinib therapy. and potentiates therapeutic antitumor immunity 51. Shigematsu, H. & Gazdar, A. F. Somatic mutations of
Science 304, 1497–1500 (2004). unleashed by immune checkpoint blockade. Nat. Med. epidermal growth factor receptor signaling pathway
4. Slamon, D. J. et al. Use of chemotherapy plus a 24, 556–562 (2018). in lung cancers. Int. J. Cancer 118, 257–262 (2006).
monoclonal antibody against HER2 for metastatic 27. Slamon, D. J. et al. Human breast cancer: correlation 52. Hynes, N. E. & Schlange, T. Targeting ADAMS and
breast cancer that overexpresses HER2. N. Engl. of relapse and survival with amplification of the ERBBs in lung cancer. Cancer Cell 10, 7–11 (2006).
J. Med. 344, 783–792 (2001). HER-2/neu oncogene. Science 235, 177–182 (1987). 53. Sharma, S. V. & Settleman, J. ErbBs in lung cancer.
5. Modi, S. et al. Trastuzumab deruxtecan in previously 28. Reck, M. et al. Pembrolizumab versus chemotherapy Exp. Cell Res. 315, 557–571 (2009).
treated HER2-positive breast cancer. N. Engl. J. Med. for PD-L1-positive non-small-cell lung cancer. N. Engl. 54. Jorissen, R. N. et al. Epidermal growth factor receptor:
382, 610–621 (2020). J. Med. 375, 1823–1833 (2016). mechanisms of activation and signalling. Exp. Cell Res.
6. Lynch, T. J. et al. Activating mutations in the epidermal 29. Borghaei, H. et al. Nivolumab versus docetaxel in 284, 31–53 (2003).
growth factor receptor underlying responsiveness of advanced nonsquamous non-small-cell lung cancer. 55. Motoyama, A. B., Hynes, N. E. & Lane, H. A. The efficacy
non-small-cell lung cancer to gefitinib. N. Engl. J. Med. N. Engl. J. Med. 373, 1627–1639 (2015). of ErbB receptor-targeted anticancer therapeutics
350, 2129–2139 (2004). 30. Gainor, J. F. et al. EGFR mutations and ALK is influenced by the availability of epidermal growth
7. Rosenthal, R. et al. Neoantigen-directed immune rearrangements are associated with low response factor-related peptides. Cancer Res. 62, 3151–3158
escape in lung cancer evolution. Nature 567, rates to PD-1 pathway blockade in non-small cell lung (2002).
479–485 (2019). cancer: a retrospective analysis. Clin. Cancer Res. 22, 56. Engelman, J. A. et al. ErbB-3 mediates
8. Schreiber, R. D., Old, L. J. & Smyth, M. J. Cancer 4585–4593 (2016). phosphoinositide 3-kinase activity in gefitinib-sensitive
immunoediting: integrating immunity’s roles in 31. Thorsson, V. et al. The immune landscape of cancer. non-small cell lung cancer cell lines. Proc. Natl Acad.
cancer suppression and promotion. Science 331, Immunity 48, 812–830.e14 (2018). Sci. USA 102, 3788–3793 (2005).
1565–1570 (2011). 32. Prenzel, N., Fischer, O. M., Streit, S., Hart, S. & 57. Holbro, T. et al. The ErbB2/ErbB3 heterodimer
This review summarizes an essential concept in the Ullrich, A. The epidermal growth factor receptor family functions as an oncogenic unit: ErbB2 requires ErbB3
cancer immunology field regarding the interaction as a central element for cellular signal transduction to drive breast tumor cell proliferation. Proc. Natl
between the immune system and cancer cells during and diversification. Endocr. Relat. Cancer 8, 11–31 Acad. Sci. USA 100, 8933–8938 (2003).
cancer development, ‘cancer immuno-editing’. (2001). 58. Fujimoto, N. et al. High expression of ErbB family
9. Pardoll, D. M. The blockade of immune checkpoints 33. Yarden, Y. & Sliwkowski, M. X. Untangling the members and their ligands in lung adenocarcinomas
in cancer immunotherapy. Nat. Rev. Cancer 12, ErbB signalling network. Nat. Rev. Mol. Cell Biol. 2, that are sensitive to inhibition of epidermal growth
252–264 (2012). 127–137 (2001). factor receptor. Cancer Res. 65, 11478–11485 (2005).
10. McGranahan, N. et al. Clonal neoantigens elicit T cell 34. Holbro, T., Civenni, G. & Hynes, N. E. The ErbB 59. Sundvall, M. et al. Role of ErbB4 in breast cancer.
immunoreactivity and sensitivity to immune checkpoint receptors and their role in cancer progression. J. Mammary Gland Biol. Neoplasia 13, 259–268
blockade. Science 351, 1463–1469 (2016). Exp. Cell Res. 284, 99–110 (2003). (2008).
11. Rizvi, N. A. et al. Cancer immunology. Mutational 35. Hynes, N. E. & MacDonald, G. ErbB receptors and 60. Gullick, W. J. c-erbB-4/HER4: friend or foe? J. Pathol.
landscape determines sensitivity to PD-1 blockade in signaling pathways in cancer. Curr. Opin. Cell Biol. 21, 200, 279–281 (2003).
non-small cell lung cancer. Science 348, 124–128 177–184 (2009). 61. Junttila, T. T., Sundvall, M., Maatta, J. A. & Elenius, K.
(2015). 36. Shih, A. J., Telesco, S. E. & Radhakrishnan, R. Erbb4 and its isoforms: selective regulation of growth
Together with McGranahan et al. (2016), this Analysis of somatic mutations in cancer: molecular factor responses by naturally occurring receptor
paper shows the importance of the TMB in the mechanisms of activation in the ErbB family of receptor variants. Trends Cardiovasc. Med. 10, 304–310
efficacy of ICIs. tyrosine kinases. Cancers 3, 1195–1231 (2011). (2000).
12. Schumacher, T. N. & Schreiber, R. D. Neoantigens in 37. Seshacharyulu, P. et al. Targeting the EGFR signaling 62. Pao, W. & Chmielecki, J. Rational, biologically based
cancer immunotherapy. Science 348, 69–74 (2015). pathway in cancer therapy. Expert Opin. Ther. Targets treatment of EGFR-mutant non-small-cell lung cancer.
13. van der Bruggen, P. et al. A gene encoding an antigen 16, 15–31 (2012). Nat. Rev. Cancer 10, 760–774 (2010).
recognized by cytolytic T lymphocytes on a human 38. Balz, L. M. et al. The interplay of HER2/HER3/PI3K 63. Suda, K., Rivard, C. J., Mitsudomi, T. & Hirsch, F. R.
melanoma. Science 254, 1643–1647 (1991). and EGFR/HER2/PLC-γ1 signalling in breast cancer Overcoming resistance to EGFR tyrosine kinase
14. Desrichard, A. et al. Tobacco smoking-associated cell migration and dissemination. J. Pathol. 227, inhibitors in lung cancer, focusing on non-T790M
alterations in the immune microenvironment of 234–244 (2012). mechanisms. Expert Rev. Anticancer Ther. 17,
squamous cell carcinomas. J. Natl Cancer Inst. 110, 39. Zhou, Q. et al. Activated human hydroxy-carboxylic 779–786 (2017).
1386–1392 (2018). acid receptor-3 signals to MAP kinase cascades via 64. Rusnak, D. W. et al. The effects of the novel, reversible
15. Wang, S., Jia, M., He, Z. & Liu, X. S. APOBEC3B and the PLC-dependent PKC and MMP-mediated EGFR epidermal growth factor receptor/ErbB-2 tyrosine
APOBEC mutational signature as potential predictive pathways. Br. J. Pharmacol. 166, 1756–1773 kinase inhibitor, GW2016, on the growth of human
markers for immunotherapy response in non-small cell (2012). normal and tumor-derived cell lines in vitro and
lung cancer. Oncogene 37, 3924–3936 (2018). 40. Fan, Q. W. et al. EGFR phosphorylates tumor- in vivo. Mol. Cancer Ther. 1, 85–94 (2001).
16. Cristescu, R. et al. Pan-tumor genomic biomarkers derived EGFRvIII driving STAT3/5 and progression in 65. O’Brien, N. A. et al. Activated phosphoinositide
for PD-1 checkpoint blockade-based immunotherapy. glioblastoma. Cancer Cell 24, 438–449 (2013). 3-kinase/AKT signaling confers resistance to
Science 362, eaar3593 (2018). 41. Colomiere, M. et al. Cross talk of signals between trastuzumab but not lapatinib. Mol. Cancer Ther. 9,
17. Ayers, M. et al. IFN-γ-related mRNA profile predicts EGFR and IL-6R through JAK2/STAT3 mediate 1489–1502 (2010).
clinical response to PD-1 blockade. J. Clin. Invest. epithelial–mesenchymal transition in ovarian 66. Konecny, G. E. et al. Activity of the dual kinase
127, 2930–2940 (2017). carcinomas. Br. J. Cancer 100, 134–144 (2009). inhibitor lapatinib (GW572016) against HER-2-
18. Hellmann, M. D. et al. Genomic features of response 42. Tseng, P. C., Chen, C. L., Shan, Y. S. & Lin, C. F. An overexpressing and trastuzumab-treated breast
to combination immunotherapy in patients with increase in galectin-3 causes cellular unresponsiveness cancer cells. Cancer Res. 66, 1630–1639 (2006).
advanced non-small-cell lung cancer. Cancer Cell 33, to IFN-γ-induced signal transduction and growth 67. Xu, X. et al. HER2 reactivation through acquisition
843–852.e4 (2018). inhibition in gastric cancer cells. Oncotarget 7, of the HER2 L755S mutation as a mechanism of
19. Rooney, M. S., Shukla, S. A., Wu, C. J., Getz, G. & 15150–15160 (2016). acquired resistance to HER2-targeted therapy
Hacohen, N. Molecular and genetic properties of 43. Matsuzaki, S. et al. Lysophosphatidic acid inhibits CC in HER2+ breast cancer. Clin. Cancer Res. 23,
tumors associated with local immune cytolytic activity. chemokine ligand 5/RANTES production by blocking 5123–5134 (2017).
Cell 160, 48–61 (2015). IRF-1-mediated gene transcription in human bronchial 68. Douillard, J. Y. et al. FOLFOX4 with cetuximab vs.
20. Sugiyama, E. et al. Blockade of EGFR improves epithelial cells. J. Immunol. 185, 4863–4872 UFOX with cetuximab as first-line therapy in metastatic
responsiveness to PD-1 blockade in EGFR-mutated (2010). colorectal cancer: the randomized phase II FUTURE
non-small cell lung cancer. Sci. Immunol. 5, eaav3937 44. Van Raemdonck, K., Van den Steen, P. E., Liekens, S., study. Clin. Colorectal Cancer 13, 14–26.e1 (2014).
(2020). Van Damme, J. & Struyf, S. CXCR3 ligands in disease 69. Jonker, D. J. et al. Cetuximab for the treatment of
This study shows an immunological role of EGFR and therapy. Cytokine Growth Factor Rev. 26, colorectal cancer. N. Engl. J. Med. 357, 2040–2048
signalling: aberrant EGFR signalling recruits Treg 311–327 (2015). (2007).
cells in the TME via chemokine production. 45. Peng, D. et al. Epigenetic silencing of TH1-type 70. Van Cutsem, E. et al. Open-label phase III trial of
21. Skoulidis, F. et al. STK11/LKB1 mutations and chemokines shapes tumour immunity and panitumumab plus best supportive care compared
PD-1 inhibitor resistance in KRAS-mutant lung immunotherapy. Nature 527, 249–253 (2015). with best supportive care alone in patients with
adenocarcinoma. Cancer Discov. 8, 822–835 46. Jaiswal, B. S. et al. Oncogenic ERBB3 mutations in chemotherapy-refractory metastatic colorectal cancer.
(2018). human cancers. Cancer Cell 23, 603–617 (2013). J. Clin. Oncol. 25, 1658–1664 (2007).
22. Peng, W. et al. Loss of PTEN promotes resistance 47. Gilbertson, R. et al. Novel ERBB4 juxtamembrane 71. Van Cutsem, E. et al. Cetuximab and chemotherapy
to T cell-mediated immunotherapy. Cancer Discov. splice variants are frequently expressed in childhood as initial treatment for metastatic colorectal cancer.
6, 202–216 (2016). medulloblastoma. Genes Chromosomes Cancer 31, N. Engl. J. Med. 360, 1408–1417 (2009).
23. George, S. et al. Loss of PTEN is associated with 288–294 (2001). 72. Matsuda, N. et al. Safety and efficacy of panitumumab
resistance to anti-PD-1 checkpoint blockade therapy 48. Prickett, T. D. et al. Analysis of the tyrosine kinome plus neoadjuvant chemotherapy in patients with
in metastatic uterine leiomyosarcoma. Immunity 46, in melanoma reveals recurrent mutations in ERBB4. primary HER2-negative inflammatory breast cancer.
197–204 (2017). Nat. Genet. 41, 1127–1132 (2009). JAMA Oncol. 4, 1207–1213 (2018).
Nature Reviews | CAncER volume 21 | March 2021 | 193
Reviews
73. Wang, X. et al. EGFR signaling promotes inflammation 95. Ogitani, Y. et al. DS-8201a, a novel HER2-targeting 117. Akbay, E. A. et al. Activation of the PD-1 pathway
and cancer stem-like activity in inflammatory breast ADC with a novel DNA topoisomerase I inhibitor, contributes to immune escape in EGFR-driven lung
cancer. Oncotarget 8, 67904–67917 (2017). demonstrates a promising antitumor efficacy with tumors. Cancer Discov. 3, 1355–1363 (2013).
74. Piccart-Gebhart, M. J. et al. Trastuzumab after differentiation from T-DM1. Clin. Cancer Res. 22, This study shows that oncogenic EGFR signalling
adjuvant chemotherapy in HER2-positive breast 5097–5108 (2016). intrinsically elevates PDL1 expression and
cancer. N. Engl. J. Med. 353, 1659–1672 (2005). 96. Shitara, K. et al. Trastuzumab deruxtecan in previously contributes to escape from antitumour immune
75. Robert, N. et al. Randomized phase III study of treated HER2-positive gastric cancer. N. Engl. J. Med. responses in a preclinical model.
trastuzumab, paclitaxel, and carboplatin compared 382, 2419–2430 (2020). 118. Ma, W. et al. EGFR signaling suppresses type 1
with trastuzumab and paclitaxel in women with 97. Hashimoto, Y. et al. A novel HER3-targeting antibody– cytokine-induced T-cell attracting chemokine secretion
HER-2-overexpressing metastatic breast cancer. drug conjugate, U3-1402, exhibits potent therapeutic in head and neck cancer. PloS ONE 13, e0203402
J. Clin. Oncol. 24, 2786–2792 (2006). efficacy through the delivery of cytotoxic payload (2018).
76. Romond, E. H. et al. Trastuzumab plus adjuvant by efficient internalization. Clin. Cancer Res. 25, 119. Mascia, F., Mariani, V., Girolomoni, G. & Pastore, S.
chemotherapy for operable HER2-positive breast 7151–7161 (2019). Blockade of the EGF receptor induces a deranged
cancer. N. Engl. J. Med. 353, 1673–1684 (2005). 98. Wu, J. Y. et al. Lung cancer with epidermal growth chemokine expression in keratinocytes leading to
77. Bang, Y. J. et al. Trastuzumab in combination with factor receptor exon 20 mutations is associated with enhanced skin inflammation. Am. J. Pathol. 163,
chemotherapy versus chemotherapy alone for poor gefitinib treatment response. Clin. Cancer Res. 303–312 (2003).
treatment of HER2-positive advanced gastric or 14, 4877–4882 (2008). 120. Lian, G. et al. Colon cancer cell secretes EGF to
gastro-oesophageal junction cancer (ToGA): a phase 3, 99. Kobayashi, S. et al. EGFR mutation and resistance of promote M2 polarization of TAM through EGFR/PI3K/
open-label, randomised controlled trial. Lancet 376, non-small-cell lung cancer to gefitinib. N. Engl. J. Med. AKT/mTOR pathway. Technol. Cancer Res. Treat. 18,
687–697 (2010). 352, 786–792 (2005). 1533033819849068 (2019).
78. Baselga, J. et al. Pertuzumab plus trastuzumab 100. Thress, K. S. et al. Acquired EGFR C797S mutation 121. Yoshida, T. et al. Podoplanin-positive cancer-
plus docetaxel for metastatic breast cancer. N. Engl. mediates resistance to AZD9291 in non-small cell associated fibroblasts in the tumor microenvironment
J. Med. 366, 109–119 (2012). lung cancer harboring EGFR T790M. Nat. Med. 21, induce primary resistance to EGFR-TKIs in lung
79. Gianni, L. et al. Efficacy and safety of neoadjuvant 560–562 (2015). adenocarcinoma with EGFR mutation. Clin. Cancer Res.
pertuzumab and trastuzumab in women with locally 101. Ou, S. I. et al. Emergence of novel and dominant 21, 642–651 (2015).
advanced, inflammatory, or early HER2-positive acquired EGFR solvent-front mutations at Gly796 122. Cremasco, V. et al. FAP delineates heterogeneous and
breast cancer (NeoSphere): a randomised multicentre, (G796S/R) together with C797S/R and L792F/H functionally divergent stromal cells in immune-excluded
open-label, phase 2 trial. Lancet Oncol. 13, 25–32 mutations in one EGFR (L858R/T790M) NSCLC breast tumors. Cancer Immunol. Res. 6, 1472–1485
(2012). patient who progressed on osimertinib. Lung Cancer (2018).
80. Schneeweiss, A. et al. Pertuzumab plus trastuzumab in 108, 228–231 (2017). 123. Sakai, T. et al. Link between tumor-promoting
combination with standard neoadjuvant anthracycline- 102. Montagut, C. et al. Identification of a mutation in the fibrous microenvironment and an immunosuppressive
containing and anthracycline-free chemotherapy extracellular domain of the epidermal growth factor microenvironment in stage I lung adenocarcinoma.
regimens in patients with HER2-positive early breast receptor conferring cetuximab resistance in colorectal Lung Cancer 126, 64–71 (2018).
cancer: a randomized phase II cardiac safety study cancer. Nat. Med. 18, 221–223 (2012). 124. Vantourout, P. et al. Immunological visibility:
(TRYPHAENA). Ann. Oncol. 24, 2278–2284 (2013). 103. Scaltriti, M. et al. Expression of p95HER2, a posttranscriptional regulation of human NKG2D
81. Clynes, R. A., Towers, T. L., Presta, L. G. & Ravetch, J. V. truncated form of the HER2 receptor, and response ligands by the EGF receptor pathway. Sci. Transl. Med.
Inhibitory Fc receptors modulate in vivo cytotoxicity to anti-HER2 therapies in breast cancer. J. Natl 6, 231ra249 (2014).
against tumor targets. Nat. Med. 6, 443–446 Cancer Inst. 99, 628–638 (2007). 125. Passarelli, A., Aieta, M., Sgambato, A. & Gridelli, C.
(2000). 104. Fridman, W. H., Zitvogel, L., Sautes-Fridman, C. Targeting immunometabolism mediated by CD73
82. Ghosh, R. et al. Trastuzumab has preferential activity & Kroemer, G. The immune contexture in cancer pathway in EGFR-mutated non-small cell lung cancer:
against breast cancers driven by HER2 homodimers. prognosis and treatment. Nat. Rev. Clin. Oncol. 14, a new hope for overcoming immune resistance.
Cancer Res. 71, 1871–1882 (2011). 717–734 (2017). Front. Immunol. 11, 1479 (2020).
83. Junttila, T. T. et al. Ligand-independent HER2/HER3/ 105. Yarchoan, M., Hopkins, A. & Jaffee, E. M. Tumor 126. Jia, Y. et al. EGFR-targeted therapy alters the tumor
PI3K complex is disrupted by trastuzumab and is mutational burden and response rate to PD-1 microenvironment in EGFR-driven lung tumors:
effectively inhibited by the PI3K inhibitor GDC-0941. inhibition. N. Engl. J. Med. 377, 2500–2501 (2017). implications for combination therapies. Int. J. Cancer
Cancer Cell 15, 429–440 (2009). 106. Brea, E. J. et al. Kinase regulation of human 145, 1432–1444 (2019).
84. Molina, M. A. et al. Trastuzumab (herceptin), a MHC class I molecule expression on cancer cells. 127. Isomoto, K. et al. Impact of EGFR-TKI treatment
humanized anti-Her2 receptor monoclonal antibody, Cancer Immunol. Res. 4, 936–947 (2016). on the tumor immune microenvironment in EGFR
inhibits basal and activated Her2 ectodomain cleavage 107. MacDonald, F. & Zaiss, D. M. W. The immune system’s mutation-positive non-small cell lung cancer.
in breast cancer cells. Cancer Res. 61, 4744–4749 contribution to the clinical efficacy of EGFR antagonist Clin. Cancer Res. 26, 2037–2046 (2020).
(2001). treatment. Front. Pharmacol. 8, 575 (2017). In this study, CD8+ or FOXP3+ T cell densities in the
85. Yakes, F. M. et al. Herceptin-induced inhibition of 108. Dong, Z. Y. et al. EGFR mutation correlates with TME are investigated with paired EGFR-mutated
phosphatidylinositol-3 kinase and Akt is required uninflamed phenotype and weak immunogenicity, NSCLC tissue samples before and after acquired
for antibody-mediated effects on p27, cyclin D1, causing impaired response to PD-1 blockade in resistance to EGFR-TKI treatment.
and antitumor action. Cancer Res. 62, 4132–4141 non-small cell lung cancer. Oncoimmunology 6, 128. Maynard, A. et al. Therapy-induced evolution of
(2002). e1356145 (2017). human lung cancer revealed by single-cell RNA
86. Agus, D. B. et al. Targeting ligand-activated ErbB2 109. Shi, Y. et al. A prospective, molecular epidemiology sequencing. Cell 182, 1232–1251.e22 (2020).
signaling inhibits breast and prostate tumor growth. study of EGFR mutations in Asian patients with This study evaluates changes in immune
Cancer Cell 2, 127–137 (2002). advanced non-small-cell lung cancer of adenocarcinoma phenotypes during EGFR-TKI treatment by
87. Garrett, J. T. et al. Transcriptional and histology (PIONEER). J. Thorac. Oncol. 9, 154–162 single-cell RNA sequencing of TILs extracted
posttranslational up-regulation of HER3 (ErbB3) (2014). from EGFR-mutated NSCLC tumour samples.
compensates for inhibition of the HER2 tyrosine 110. Chen, Y. J. et al. Proteogenomics of non-smoking lung 129. Sequist, L. V. et al. Genotypic and histological
kinase. Proc. Natl Acad. Sci. USA 108, 5021–5026 cancer in East Asia delineates molecular signatures of evolution of lung cancers acquiring resistance to
(2011). pathogenesis and progression. Cell 182, 226–244.e17 EGFR inhibitors. Sci. Transl. Med 3, 75ra26 (2011).
88. Schoeberl, B. et al. An ErbB3 antibody, MM-121, is (2020). 130. Witta, S. E. et al. Restoring E-cadherin expression
active in cancers with ligand-dependent activation. This study shows that EGFR-mutated NSCLCs increases sensitivity to epidermal growth factor
Cancer Res. 70, 2485–2494 (2010). present lower APOBEC mutational signatures than receptor inhibitors in lung cancer cell lines.
89. Jacob, W., James, I., Hasmann, M. & Weisser, M. non-smoking EGFR-WT NSCLCs, which potentially Cancer Res. 66, 944–950 (2006).
Clinical development of HER3-targeting monoclonal lead to the relatively low TMB of EGFR-mutated 131. Yao, Z. et al. TGF-β IL-6 axis mediates selective and
antibodies: perils and progress. Cancer Treat. Rev. 68, NSCLCs. adaptive mechanisms of resistance to molecular
111–123 (2018). 111. Hori, S., Nomura, T. & Sakaguchi, S. Control of targeted therapy in lung cancer. Proc. Natl Acad.
90. Haag, R. & Kratz, F. Polymer therapeutics: concepts regulatory T cell development by the transcription Sci. USA 107, 15535–15540 (2010).
and applications. Angew. Chem. Int. Ed. Engl. 45, factor Foxp3. Science 299, 1057–1061 (2003). 132. Massagué, J. TGFβ in cancer. Cell 134, 215–230
1198–1215 (2006). 112. Togashi, Y., Shitara, K. & Nishikawa, H. Regulatory (2008).
91. Beck, A., Goetsch, L., Dumontet, C. & Corvaïa, N. T cells in cancer immunosuppression — implications 133. Tu, E., Chia, P. Z. & Chen, W. TGFβ in T cell biology
Strategies and challenges for the next generation of for anticancer therapy. Nat. Rev. Clin. Oncol. 16, and tumor immunity: angel or devil? Cytokine Growth
antibody–drug conjugates. Nat. Rev. Drug Discov. 16, 356–371 (2019). Factor Rev. 25, 423–435 (2014).
315–337 (2017). 113. Kumagai, S. et al. The PD-1 expression balance 134. Mariathasan, S. et al. TGFβ attenuates tumour
92. Verma, S. et al. Trastuzumab emtansine for HER2- between effector and regulatory T cells predicts response to PD-L1 blockade by contributing to
positive advanced breast cancer. N. Engl. J. Med. the clinical efficacy of PD-1 blockade therapies. exclusion of T cells. Nature 554, 544–548 (2018).
367, 1783–1791 (2012). Nat. Immunol. 21, 1346–1358 (2020). 135. Chen, X. H. et al. TGF-β and EGF induced HLA-I
93. Krop, I. E. et al. Trastuzumab emtansine versus 114. Kamada, T. et al. PD-1+ regulatory T cells amplified by downregulation is associated with epithelial–
treatment of physician’s choice for pretreated PD-1 blockade promote hyperprogression of cancer. mesenchymal transition (EMT) through upregulation
HER2-positive advanced breast cancer (TH3RESA): Proc. Natl Acad. Sci. USA 116, 9999–10008 (2019). of snail in prostate cancer cells. Mol. Immunol. 65,
a randomised, open-label, phase 3 trial. Lancet Oncol. 115. Nagarsheth, N., Wicha, M. S. & Zou, W. Chemokines 34–42 (2015).
15, 689–699 (2014). in the cancer microenvironment and their relevance in 136. Kudo-Saito, C., Shirako, H., Takeuchi, T. & Kawakami, Y.
94. Perez, E. A. et al. Trastuzumab emtansine with or cancer immunotherapy. Nat. Rev. Immunol. 17, Cancer metastasis is accelerated through
without pertuzumab versus trastuzumab plus taxane 559–572 (2017). immunosuppression during Snail-induced EMT of
for human epidermal growth factor receptor 2-positive, 116. Spranger, S. et al. Up-regulation of PD-L1, IDO, and cancer cells. Cancer Cell 15, 195–206 (2009).
advanced breast cancer: primary results from the Tregs in the melanoma tumor microenvironment is 137. Dongre, A. et al. Epithelial-to-mesenchymal transition
phase III MARIANNE study. J. Clin. Oncol. 35, driven by CD8+ T cells. Sci. Transl. Med. 5, 200ra116 contributes to immunosuppression in breast
141–148 (2017). (2013). carcinomas. Cancer Res. 77, 3982–3989 (2017).
194 | March 2021 | volume 21 www.nature.com/nrc
Reviews
138. Costa, A. et al. Fibroblast heterogeneity and 161. Hu-Lieskovan, S. et al. Improved antitumor activity 185. Cheng, H. et al. HHLA2, a new immune checkpoint
immunosuppressive environment in human breast of immunotherapy with BRAF and MEK inhibitors member of the B7 family, is widely expressed in
cancer. Cancer Cell 33, 463–479.e10 (2018). in BRAF(V600E) melanoma. Sci. Transl. Med. 7, human lung cancer and associated with EGFR
139. Roche, P. A. & Furuta, K. The ins and outs of MHC 279ra241 (2015). mutational status. Clin. Cancer Res. 23, 825–832
class II-mediated antigen processing and presentation. 162. Sabbatino, F. et al. Antitumor activity of BRAF (2017).
Nat. Rev. Immunol. 15, 203–216 (2015). inhibitor and IFNα combination in BRAF-mutant 186. Jin, D. et al. CD73 on tumor cells impairs antitumor
140. DeSandro, A., Nagarajan, U. M. & Boss, J. M. melanoma. J. Natl Cancer Inst. 108, djv435 (2016). T-cell responses: a novel mechanism of tumor-induced
The bare lymphocyte syndrome: molecular clues to the 163. Whipple, C. A. et al. The mitogen-activated protein immune suppression. Cancer Res. 70, 2245–2255
transcriptional regulation of major histocompatibility kinase pathway plays a critical role in regulating (2010).
complex class II genes. Am. J. Hum. Genet. 65, immunological properties of BRAF mutant cutaneous 187. Ring, S., Enk, A. H. & Mahnke, K. ATP activates
279–286 (1999). melanoma cells. Melanoma Res. 26, 223–235 regulatory T cells in vivo during contact hypersensitivity
141. Accolla, R. S. et al. Boosting the MHC class II-restricted (2016). reactions. J. Immunol. 184, 3408–3416 (2010).
tumor antigen presentation to CD4+ T helper cells: 164. Sapkota, B., Hill, C. E. & Pollack, B. P. Vemurafenib 188. Morello, S. & Miele, L. Targeting the adenosine A2b
a critical issue for triggering protective immunity and enhances MHC induction in BRAF(V600E) homozygous receptor in the tumor microenvironment overcomes
re-orienting the tumor microenvironment toward an melanoma cells. Oncoimmunology 2, e22890 (2013). local immunosuppression by myeloid-derived
anti-tumor state. Front. Oncol. 4, 32 (2014). 165. Pollack, B. P., Sapkota, B. & Cartee, T. V. suppressor cells. Oncoimmunology 3, e27989
142. Garrido, F., Cabrera, T. & Aptsiauri, N. “Hard” and Epidermal growth factor receptor inhibition (2014).
“soft” lesions underlying the HLA class I alterations augments the expression of MHC class I and II genes. 189. Zarek, P. E. et al. A2A receptor signaling promotes
in cancer cells: implications for immunotherapy. Clin. Cancer Res. 17, 4400–4413 (2011). peripheral tolerance by inducing T-cell anergy and the
Int. J. Cancer 127, 249–256 (2010). 166. Kumai, T. et al. EGFR inhibitors augment antitumour generation of adaptive regulatory T cells. Blood 111,
143. Kotekar, A. S., Weissman, J. D., Gegonne, A., helper T-cell responses of HER family-specific 251–259 (2008).
Cohen, H. & Singer, D. S. Histone modifications, immunotherapy. Br. J.Cancer 109, 2155–2166 190. Marteau, F. et al. Thrombospondin-1 and indoleamine
but not nucleosomal positioning, correlate with (2013). 2,3-dioxygenase are major targets of extracellular
major histocompatibility complex class I promoter 167. Kumai, T. et al. Targeting HER-3 to elicit antitumor ATP in human dendritic cells. Blood 106, 3860–3866
activity in different tissues in vivo. Mol. Cell. Biol. 28, helper T cells against head and neck squamous cell (2005).
7323–7336 (2008). carcinoma. Sci. Rep. 5, 16280 (2015). 191. Goto, T., Herberman, R. B., Maluish, A. & Strong, D. M.
144. van den Elsen, P. J. Expression regulation of major 168. Okita, R. et al. Contrasting effects of the cytotoxic Cyclic AMP as a mediator of prostaglandin E-induced
histocompatibility complex class I and class II anticancer drug gemcitabine and the EGFR tyrosine suppression of human natural killer cell activity.
encoding genes. Front. Immunol. 2, 48 (2011). kinase inhibitor gefitinib on NK cell-mediated J. Immunol. 130, 1350–1355 (1983).
145. Seliger, B. Molecular mechanisms of MHC class I cytotoxicity via regulation of NKG2D ligand in 192. Nowak, M. et al. The A2aR adenosine receptor
abnormalities and APM components in human non-small-cell lung cancer cells. PloS ONE 10, controls cytokine production in iNKT cells. Eur. J.
tumors. Cancer Immunol. Immunother. 57, e0139809 (2015). Immunol. 40, 682–687 (2010).
1719–1726 (2008). 169. Gao, L. et al. Tumor-derived exosomes antagonize 193. Panther, E. et al. Adenosine affects expression
146. Hastings, K. T. GILT: shaping the MHC class innate antiviral immunity. Nat. Immunol. 19, of membrane molecules, cytokine and chemokine
II-restricted peptidome and CD4+ T cell-mediated 233–245 (2018). release, and the T-cell stimulatory capacity of human
immunity. Front. Immunol. 4, 429 (2013). 170. Wintterle, S. et al. Expression of the B7-related dendritic cells. Blood 101, 3985–3990 (2003).
147. Kim, R., Emi, M., Tanabe, K. & Arihiro, K. molecule B7-H1 by glioma cells: a potential 194. Panther, E. et al. Expression and function of adenosine
Tumor-driven evolution of immunosuppressive mechanism of immune paralysis. Cancer Res. 63, receptors in human dendritic cells. FASEB J. 15,
networks during malignant progression. Cancer Res. 7462–7467 (2003). 1963–1970 (2001).
66, 5527–5536 (2006). 171. Budczies, J. et al. Pan-cancer analysis of copy number 195. Zhang, H. et al. Adenosine acts through A2 receptors
148. Marincola, F. M., Jaffee, E. M., Hicklin, D. J. & changes in programmed death-ligand 1 (PD-L1, to inhibit IL-2-induced tyrosine phosphorylation
Ferrone, S. Escape of human solid tumors from T-cell CD274) — associations with gene expression, of STAT5 in T lymphocytes: role of cyclic adenosine
recognition: molecular mechanisms and functional mutational load, and survival. Genes Chromosomes 3′,5′-monophosphate and phosphatases. J. Immunol.
significance. Adv. Immunol. 74, 181–273 (2000). Cancer 55, 626–639 (2016). 173, 932–944 (2004).
149. Seliger, B. Different regulation of MHC class I 172. Kataoka, K. et al. Aberrant PD-L1 expression through 196. Deaglio, S. et al. Adenosine generation catalyzed by
antigen processing components in human tumors. 3′-UTR disruption in multiple cancers. Nature 534, CD39 and CD73 expressed on regulatory T cells
J. Immunotoxicol. 5, 361–367 (2008). 402–406 (2016). mediates immune suppression. J. Exp. Med. 204,
150. Seliger, B. The link between MHC class I abnormalities 173. Lastwika, K. J. et al. Control of PD-L1 expression by 1257–1265 (2007).
of tumors, oncogenes, tumor suppressor genes, and oncogenic activation of the AKT–mTOR pathway in 197. Ohta, A. et al. A2A adenosine receptor may allow
transcription factors. J. Immunotoxicol. 11, 308–310 non-small cell lung cancer. Cancer Res. 76, 227–238 expansion of T cells lacking effector functions in
(2014). (2016). extracellular adenosine-rich microenvironments.
151. van der Burg, S. H., Arens, R., Ossendorp, F., 174. Chen, N. et al. Upregulation of PD-L1 by EGFR J. Immunol. 183, 5487–5493 (2009).
van Hall, T. & Melief, C. J. Vaccines for established activation mediates the immune escape in 198. Park, L. C. et al. Immunologic and clinical implications
cancer: overcoming the challenges posed by immune EGFR-driven NSCLC: implication for optional immune of CD73 expression in non-small cell lung cancer
evasion. Nat. Rev. Cancer 16, 219–233 (2016). targeted therapy for NSCLC patients with EGFR (NSCLC). J. Clin. Oncol. 36, 12050–12050
152. Schreiber, A. B., Schlessinger, J. & Edidin, M. mutation. J. Thorac. Oncol. 10, 910–923 (2015). (2018).
Interaction between major histocompatibility complex 175. Zhang, N. et al. The EGFR pathway is involved in the 199. Sidders, B. et al. Adenosine signaling is prognostic
antigens and epidermal growth factor receptors on regulation of PD-L1 expression via the IL-6/JAK/STAT3 for cancer outcome and has predictive utility for
human cells. J. Cell Biol. 98, 725–731 (1984). signaling pathway in EGFR-mutated non-small cell lung immunotherapeutic response. Clin.Cancer Res. 26,
153. Sporn, M. B. & Roberts, A. B. Autocrine growth cancer. Int. J. Oncol. 49, 1360–1368 (2016). 2176–2187 (2020).
factors and cancer. Nature 313, 745–747 (1985). 176. Gao, S. P. et al. Mutations in the EGFR kinase domain This study shows that high levels of baseline
154. Lahat, N., Sheinfeld, M., Sobel, E., Kinarty, A. & mediate STAT3 activation via IL-6 production in tumour adenosine signalling are associated with
Kraiem, Z. Divergent effects of cytokines on human human lung adenocarcinomas. J. Clin. Invest. 117, resistance to ICIs in various types of cancer.
leukocyte antigen-DR antigen expression of neoplastic 3846–3856 (2007). 200. Streicher, K. et al. Increased CD73 and reduced
and non-neoplastic human thyroid cells. Cancer 69, 177. Takada, K. et al. PD-L1 expression according to IFNG signature expression in relation to response
1799–1807 (1992). the EGFR status in primary lung adenocarcinoma. rates to anti-PD-1(L1) therapies in EGFR-mutant
155. Pollack, B. P. EGFR inhibitors, MHC expression and Lung Cancer 116, 1–6 (2018). NSCLC. J. Clin. Oncol. 35, 1150 (2017).
immune responses: can EGFR inhibitors be used as 178. Lee, J. et al. PD-L1 expression in ROS1-rearranged 201. Wang, C., Yu, X. & Wang, W. A meta-analysis of
immune response modifiers? Oncoimmunology 1, non-small cell lung cancer: a study using simultaneous efficacy and safety of antibodies targeting PD-1/PD-L1
71–74 (2012). genotypic screening of EGFR, ALK, and ROS1. in treatment of advanced nonsmall cell lung cancer.
156. Chandrasekaran, S. et al. Phosphoinositide 3-kinase Thorac. Cancer 10, 103–110 (2019). Medicine 95, e5539 (2016).
signaling can modulate MHC class I and II expression. 179. Heigener, D. F. & Reck, M. Impact of PD-L1 expression 202. Khan, M. et al. Comparative analysis of immune
Mol. Cancer Res. 17, 2395–2409 (2019). in EGFR-positive NSCLC? The answer remains the checkpoint inhibitors and chemotherapy in the
157. Marijt, K. A. et al. Metabolic stress in cancer cells same. J. Thorac. Oncol. 13, 1060–1061 (2018). treatment of advanced non-small cell lung cancer:
induces immune escape through a PI3K-dependent 180. Ji, M. et al. PD-1/PD-L1 expression in non-small-cell a meta-analysis of randomized controlled trials.
blockade of IFNγ receptor signaling. J. Immunother. lung cancer and its correlation with EGFR/KRAS Medicine 97, e11936 (2018).
Cancer 7, 152 (2019). mutations. Cancer Biol. Ther. 17, 407–413 (2016). 203. Lee, C. K. et al. Clinical and molecular characteristics
158. Sivaram, N. et al. Tumor-intrinsic PIK3CA represses 181. Li, J. et al. A systematic and genome-wide correlation associated with survival among patients treated with
tumor immunogenecity in a model of pancreatic meta-analysis of PD-L1 expression and targetable checkpoint inhibitors for advanced non-small cell lung
cancer. J. Clin. Invest. 129, 3264–3276 (2019). NSCLC driver genes. J. Thorac. Dis. 9, 2560–2571 carcinoma: a systematic review and meta-analysis.
159. Watanabe, S. et al. Mutational activation of the (2017). JAMA Oncol. 4, 210–216 (2018).
epidermal growth factor receptor down-regulates 182. Han, J. J. et al. Change in PD-L1 expression after This meta-analysis fails to show overall survival
major histocompatibility complex class I expression acquiring resistance to gefitinib in EGFR-mutant benefit of ICIs for patients with EGFR-mutated
via the extracellular signal-regulated kinase in non-small-cell lung cancer. Clin. Lung Cancer 17, NSCLCs in second-line therapy.
non-small cell lung cancer. Cancer Sci. 110, 52–60 263–270.e2 (2016). 204. Lee, C. K. et al. Checkpoint inhibitors in metastatic
(2019). 183. Shibahara, D. et al. Intrinsic and extrinsic regulation EGFR-mutated non-small cell lung cancer — a
This study shows that aberrant EGFR signalling of PD-L2 expression in oncogene-driven non-small meta-analysis. J. Thorac. Oncol. 12, 403–407
inhibits MHC class I expression. cell lung cancer. J. Thorac. Oncol. 13, 926–937 (2017).
160. Mimura, K. et al. The MAPK pathway is a predominant (2018). 205. Sun, L. et al. Clinical efficacy and safety of anti-PD-1/
regulator of HLA-A expression in esophageal and 184. Zhao, R. et al. HHLA2 is a member of the B7 family PD-L1 inhibitors for the treatment of advanced or
gastric cancer. J. Immunol. 191, 6261–6272 and inhibits human CD4 and CD8 T-cell function. metastatic cancer: a systematic review and
(2013). Proc. Natl Acad. Sci. USA 110, 9879–9884 (2013). meta-analysis. Sci. Rep. 10, 2083 (2020).
Nature Reviews | CAncER volume 21 | March 2021 | 195
Reviews
206. Hastings, K. et al. EGFR mutation subtypes and 228. Choudhury, A. et al. Small interfering RNA (siRNA) anti-PD-1 and anti-CTLA-4 mAbs. Clin. Cancer Res.
response to immune checkpoint blockade treatment inhibits the expression of the Her2/neu gene, 19, 5626–5635 (2013).
in non-small-cell lung cancer. Ann. Oncol. 30, upregulates HLA class I and induces apoptosis of 250. Ciardiello, F. & Tortora, G. EGFR antagonists in cancer
1311–1320 (2019). Her2/neu positive tumor cell lines. Int. J. Cancer 108, treatment. N. Engl. J Med. 358, 1160–1174 (2008).
This study shows that the clinical efficacy of ICIs in 71–77 (2004). 251. Trivedi, S. et al. Anti-EGFR targeted monoclonal
EGFR-mutated NSCLCs is variable depending on 229. Burr, M. L. et al. CMTM6 maintains the expression antibody isotype influences antitumor cellular
the types of EGFR mutations. of PD-L1 and regulates anti-tumour immunity. Nature immunity in head and neck cancer patients.
207. Offin, M. et al. Tumor mutation burden and efficacy 549, 101–105 (2017). Clin. Cancer Res. 22, 5229–5237 (2016).
of EGFR-tyrosine kinase inhibitors in patients with 230. Li, C. W. et al. Glycosylation and stabilization of 252. Trotta, A. M. et al. Prospective evaluation of
EGFR-mutant lung cancers. Clin. Cancer Res. 25, programmed death ligand-1 suppresses T-cell activity. cetuximab-mediated antibody-dependent cell
1063–1069 (2019). Nat. Commun. 7, 12632 (2016). cytotoxicity in metastatic colorectal cancer patients
208. Chalmers, Z. R. et al. Analysis of 100,000 human 231. Mezzadra, R. et al. Identification of CMTM6 and predicts treatment efficacy. Cancer Immunol. Res. 4,
cancer genomes reveals the landscape of tumor CMTM4 as PD-L1 protein regulators. Nature 549, 366–374 (2016).
mutational burden. Genome Med. 9, 34 (2017). 106–110 (2017). 253. Pozzi, C. et al. The EGFR-specific antibody cetuximab
209. Dogan, S. et al. Molecular epidemiology of EGFR 232. Li, C. W. et al. Eradication of triple-negative breast combined with chemotherapy triggers immunogenic
and KRAS mutations in 3,026 lung adenocarcinomas: cancer cells by targeting glycosylated PD-L1. cell death. Nat. Med. 22, 624–631 (2016).
higher susceptibility of women to smoking-related Cancer Cell 33, 187–201.e10 (2018). 254. Concha-Benavente, F. et al. PD-L1 mediates
KRAS-mutant cancers. Clin. Cancer Res. 18, 233. Kubota, Y., et al. The impact of molecular subtype on dysfunction in activated PD-1+ NK cells in head and
6169–6177 (2012). efficacy of chemotherapy and checkpoint inhibition neck cancer patients. Cancer Immunol. Res. 6,
210. Lee, B., Lee, T., Lee, S. H., Choi, Y. L. & Han, J. in advanced gastric cancer. Clin. Cancer Res. 26, 1548–1560 (2018).
Clinicopathologic characteristics of EGFR, KRAS, and 3784–3790 (2020). 255. Varadan, V. et al. Immune signatures following single
ALK alterations in 6,595 lung cancers. Oncotarget 7, This study shows that PD1 blockade therapies dose trastuzumab predict pathologic response to
23874–23884 (2016). show limited antitumour efficacy in gastric cancers preoperativetrastuzumab and chemotherapy in
211. Haratani, K. et al. Tumor immune microenvironment with HER2 amplification. HER2-positive early breast cancer. Clin. Cancer Res.
and nivolumab efficacy in EGFR mutation-positive 234. Dirix, L. Y. et al. Avelumab, an anti-PD-L1 antibody, in 22, 3249–3259 (2016).
non-small-cell lung cancer based on T790M status patients with locally advanced or metastatic breast 256. Chaganty, B. K. R. et al. Trastuzumab upregulates
after disease progression during EGFR-TKI treatment. cancer: a phase 1b JAVELIN Solid Tumor study. PD-L1 as a potential mechanism of trastuzumab
Ann. Oncol. 28, 1532–1539 (2017). Breast Cancer Res. Treat. 167, 671–686 (2018). resistance through engagement of immune effector
212. Hata, A. et al. Programmed death-ligand 1 expression 235. Lanaya, H. et al. EGFR has a tumour-promoting role cells and stimulation of IFNγ secretion. Cancer Lett.
and T790M status in EGFR-mutant non-small cell lung in liver macrophages during hepatocellular carcinoma 430, 47–56 (2018).
cancer. Lung Cancer 111, 182–189 (2017). formation. Nat. Cell Biol. 16, 972–977 (2014). 257. Loi, S. et al. Pembrolizumab plus trastuzumab in
213. Yamada, T. et al. Retrospective efficacy analysis 236. Srivatsa, S. et al. EGFR in tumor-associated myeloid trastuzumab-resistant, advanced, HER2-positive
of immune checkpoint inhibitors in patients cells promotes development of colorectal cancer in breast cancer (PANACEA): a single-arm, multicentre,
with EGFR-mutated non-small cell lung cancer. mice and associates with outcomes of patients. phase 1b-2 trial. Lancet Oncol. 20, 371–382
Cancer Med. 8, 1521–1529 (2019). Gastroenterology 153, 178–190.e10 (2017). (2019).
214. Mok, T. S. et al. Gefitinib or carboplatin–paclitaxel 237. Nabeshima, A. et al. Tumour-associated macrophages 258. Janjigian, Y. Y. et al. First-line pembrolizumab and
in pulmonary adenocarcinoma. N. Engl. J. Med. 361, correlate with poor prognosis in myxoid liposarcoma trastuzumab in HER2-positive oesophageal, gastric,
947–957 (2009). and promote cell motility and invasion via the or gastro-oesophageal junction cancer: an open-label,
215. Evans, M. et al. Large-scale EGFR mutation testing HB–EGF–EGFR–PI3K/Akt pathways. Br. J.Cancer single-arm, phase 2 trial. Lancet Oncol. 21, 821–831
in clinical practice: analysis of a series of 18,920 112, 547–555 (2015). (2020).
non-small cell lung cancer cases. Pathol. Oncol. Res. 238. Zaiss, D. M. et al. Amphiregulin enhances regulatory Together with Loi et al. (2019), this paper shows
25, 1401–1409 (2019). T cell-suppressive function via the epidermal growth promising outcomes in combination therapies of
216. Lohinai, Z. et al. Distinct epidemiology and clinical factor receptor. Immunity 38, 275–284 (2013). anti-HER2 mAbs with ICIs in breast cancer and
consequence of classic versus rare EGFR mutations in 239. Green, J. A., Arpaia, N., Schizas, M., Dobrin, A. & gastric cancer with HER2 amplification.
lung adenocarcinoma. J. Thorac. Oncol. 10, 738–746 Rudensky, A. Y. A nonimmune function of T cells in 259. Junttila, T. T., Li, G., Parsons, K., Phillips, G. L. &
(2015). promoting lung tumor progression. J. Exp. Med. 214, Sliwkowski, M. X. Trastuzumab-DM1 (T-DM1) retains
217. Sheng, Q. et al. An activated ErbB3/NRG1 autocrine 3565–3575 (2017). all the mechanisms of action of trastuzumab and
loop supports in vivo proliferation in ovarian cancer 240. Gourd, K. AstraZeneca halts two lung cancer drug efficiently inhibits growth of lapatinib insensitive
cells. Cancer Cell 17, 298–310 (2010). trials. Lancet Respir. Med. 3, 926 (2015). breast cancer. Breast Cancer Res. Treat. 128,
218. Chen, K. et al. PD-L1 expression and T cells infiltration 241. Gettinger, S. et al. Nivolumab plus erlotinib in patients 347–356 (2011).
in patients with uncommon EGFR-mutant non-small with EGFR-mutant advanced NSCLC. J. Thorac. Oncol. 260. Birrer, M. J., Moore, K. N., Betella, I. & Bates, R. C.
cell lung cancer and the response to immunotherapy. 13, 1363–1372 (2018). Antibody–drug conjugate-based therapeutics: state
Lung Cancer 142, 98–105 (2020). 242. Gong, K. et al. EGFR inhibition triggers an adaptive of the science. J. Natl Cancer Inst. 111, 538–549
219. Loi, S. et al. Prognostic and predictive value of response by co-opting antiviral signaling pathways in (2019).
tumor-infiltrating lymphocytes in a phase III lung cancer. Nat. Cancer 1, 394–409 (2020). 261. Müller, P. et al. Trastuzumab emtansine (T-DM1)
randomized adjuvant breast cancer trial in node- This study shows that EGFR-TKIs upregulate renders HER2+ breast cancer highly susceptible to
positive breast cancer comparing the addition of interferons not only in EGFR-mutated human CTLA-4/PD-1 blockade. Sci. Transl. Med. 7, 315ra188
docetaxel to doxorubicin with doxorubicin-based cancer cell lines but also in EGFR-WT human cancer (2015).
chemotherapy: BIG 02-98. J. Clin. Oncol. 31, cell lines. 262. Iwata, T. N. et al. A HER2-targeting antibody-drug
860–867 (2013). 243. Saito, H. et al. Erlotinib plus bevacizumab versus conjugate, trastuzumab deruxtecan (DS-8201a),
220. Yamaguchi, R. et al. Tumor-infiltrating lymphocytes erlotinib alone in patients with EGFR-positive enhances antitumor immunity in a mouse model.
are important pathologic predictors for neoadjuvant advanced non-squamous non-small-cell lung cancer Mol. Cancer Ther. 17, 1494–1503 (2018).
chemotherapy in patients with breast cancer. (NEJ026): interim analysis of an open-label, 263. Haratani, K. et al. U3-1402 sensitizes HER3-
Hum. Pathol. 43, 1688–1694 (2012). randomised, multicentre, phase 3 trial. Lancet Oncol. expressing tumors to PD-1 blockade by immune
221. Ali, H. R. et al. Association between CD8+ T-cell 20, 625–635 (2019). activation. J. Clin. Invest. 130, 374–388 (2020).
infiltration and breast cancer survival in 12,439 244. Tada, Y. et al. Targeting VEGFR2 with ramucirumab Together with Müller et al. (2015) and Iwata et al.
patients. Ann. Oncol. 25, 1536–1543 (2014). strongly impacts effector/activated regulatory T cells (2018), this paper shows that ERBB-targeted
222. Todorović-Raković, N. & Milovanović, J. Interleukin-8 and CD8+ T cells in the tumor microenvironment. ADCs augment antitumour effects of PD1 blockade
in breast cancer progression. J. Interferon Cytokine J. Immunother. Cancer 6, 106 (2018). in preclinical models.
Res. 33, 563–570 (2013). 245. Koinis, F. et al. Effect of first-line treatment on 264. Kawazoe, A. et al. Lenvatinib plus pembrolizumab in
223. Paplomata, E. & O’Regan, R. The PI3K/AKT/mTOR myeloid-derived suppressor cells’ subpopulations in patients with advanced gastric cancer in the first-line
pathway in breast cancer: targets, trials and biomarkers. the peripheral blood of patients with non-small cell or second-line setting (EPOC1706): an open-label,
Ther. Adv. Med. Oncol. 6, 154–166 (2014). lung cancer. J. Thorac. Oncol. 11, 1263–1272 single-arm, phase 2 trial. Lancet Oncol. 21,
224. Yuen, K. C. et al. High systemic and tumor-associated (2016). 1057–1065 (2020).
IL-8 correlates with reduced clinical benefit of PD-L1 246. Socinski, M. A. et al. Atezolizumab for first-line 265. Rini, B. I. et al. Pembrolizumab plus axitinib versus
blockade. Nat. Med. 26, 693–698 (2020). treatment of metastatic nonsquamous NSCLC. sunitinib for advanced renal-cell carcinoma. N. Engl.
225. Wu, S. et al. HER2 recruits AKT1 to disrupt STING N. Engl. J. Med. 378, 2288–2301 (2018). J. Med. 380, 1116–1127 (2019).
signalling and suppress antiviral defence and 247. Reck, M. et al. Atezolizumab plus bevacizumab 266. Hanker, A. B. et al. An acquired HER2(T798I)
antitumour immunity. Nat. Cell Biol. 21, 1027–1040 and chemotherapy in non-small-cell lung cancer gatekeeper mutation induces resistance to neratinib
(2019). (IMpower150): key subgroup analyses of patients in a patient with HER2 mutant-driven breast cancer.
This study shows that HER2 amplification induces with EGFR mutations or baseline liver metastases in Cancer Discov. 7, 575–585 (2017).
loss of phosphorylation of TBK1 and attenuates a randomised, open-label phase 3 trial. Lancet Respir. 267. Kosaka, T. et al. Response heterogeneity of EGFR and
STING signalling, resulting in the impairment Med. 7, 387–401 (2019). HER2 exon 20 insertions to covalent EGFR and HER2
of the interferon response and antitumour immune This clinical trial shows the additional clinical inhibitors. Cancer Res. 77, 2712–2721 (2017).
responses. benefit of anti-PDL1 mAb with chemotherapy plus 268. Nagy, P. et al. Decreased accessibility and lack of
226. Herrmann, F. et al. HER-2/neu-mediated regulation anti-VEGF mAb even in EGFR-mutated NSCLCs. activation of ErbB2 in JIMT-1, a herceptin-resistant,
of components of the MHC class I antigen-processing 248. Beavis, P. A. et al. Adenosine receptor 2A blockade MUC4-expressing breast cancer cell line. Cancer Res.
pathway. Cancer Res. 64, 215–220 (2004). increases the efficacy of anti-PD-1 through enhanced 65, 473–482 (2005).
227. Mortenson, E. D., Park, S., Jiang, Z., Wang, S. & antitumor t-cell responses. Cancer Immunol. Res. 3, 269. Pályi-Krekk, Z. et al. Hyaluronan-induced masking
Fu, Y. X. Effective anti-neu-initiated antitumor 506–517 (2015). of ErbB2 and CD44-enhanced trastuzumab
responses require the complex role of CD4+ T cells. 249. Allard, B., Pommey, S., Smyth, M. J. & Stagg, J. internalisation in trastuzumab resistant breast
Clin. Cancer Res. 19, 1476–1486 (2013). Targeting CD73 enhances the antitumor activity of cancer. Eur. J. Cancer 43, 2423–2433 (2007).
196 | March 2021 | volume 21 www.nature.com/nrc
Reviews
270. Ghatak, S., Misra, S. & Toole, B. P. Hyaluronan lung cancer cells with acquired MET amplification. antibody–drug conjugate targeting melanoma cells
oligosaccharides inhibit anchorage-independent Cancer Sci. 101, 167–172 (2010). expressing melanotransferrin/p97. Mol. Cancer Ther. 5,
growth of tumor cells by suppressing the 293. Takezawa, K. et al. HER2 amplification: a potential 1474–1482 (2006).
phosphoinositide 3-kinase/Akt cell survival pathway. mechanism of acquired resistance to EGFR inhibition 315. Kinneer, K. et al. SLC46A3 as a potential
J. Biol. Chem. 277, 38013–38020 (2002). in EGFR-mutant lung cancers that lack the second-site predictive biomarker for antibody-drug conjugates
271. Ohashi, K. et al. Lung cancers with acquired resistance EGFRT790M mutation. Cancer Discov. 2, 922–933 bearing noncleavable linked maytansinoid and
to EGFR inhibitors occasionally harbor BRAF gene (2012). pyrrolobenzodiazepine warheads. Clin. Cancer Res.
mutations but lack mutations in KRAS, NRAS, or 294. Lee-Hoeflich, S. T. et al. A central role for HER3 24, 6570–6582 (2018).
MEK1. Proc. Natl Acad. Sci. USA 109, E2127–E2133 in HER2-amplified breast cancer: implications for 316. Oxnard, G. R. et al. TATTON: a multi-arm, phase Ib
(2012). targeted therapy. Cancer Res. 68, 5878–5887 (2008). trial of osimertinib combined with selumetinib,
272. Ercan, D. et al. Reactivation of ERK signaling causes 295. Wilson, T. R. et al. Widespread potential for savolitinib, or durvalumab in EGFR-mutant lung
resistance to EGFR kinase inhibitors. Cancer Discov. 2, growth-factor-driven resistance to anticancer kinase cancer. Ann. Oncol. 31, 507–516 (2020).
934–947 (2012). inhibitors. Nature 487, 505–509 (2012). 317. Yang, J. C. et al. Pembrolizumab in combination
273. Diaz, L. A. Jr et al. The molecular evolution of acquired 296. Xia, W. et al. An heregulin–EGFR–HER3 autocrine with erlotinib or gefitinib as first-line therapy for
resistance to targeted EGFR blockade in colorectal signaling axis can mediate acquired lapatinib advanced NSCLC with sensitizing EGFR mutation.
cancers. Nature 486, 537–540 (2012). resistance in HER2+ breast cancer models. Breast J. Thorac. Oncol. 14, 553–559 (2019).
274. Misale, S. et al. Emergence of KRAS mutations and Cancer Res. 15, R85 (2013). 318. Yang, J. C. et al. Osimertinib plus durvalumab versus
acquired resistance to anti-EGFR therapy in colorectal 297. Cortot, A. B. et al. Resistance to irreversible EGF osimertinib monotherapy in EGFR T790M-positive
cancer. Nature 486, 532–536 (2012). receptor tyrosine kinase inhibitors through a multistep NSCLC following previous EGFR TKI therapy:
275. de Bruin, E. C. et al. Reduced NF1 expression mechanism involving the IGF1R pathway. Cancer Res. CAURAL brief report. J. Thorac. Oncol. 14, 933–939
confers resistance to EGFR inhibition in lung cancer. 73, 834–843 (2013). (2019).
Cancer Discov. 4, 606–619 (2014). 298. Guix, M. et al. Acquired resistance to EGFR tyrosine 319. Emens, L. et al. Results from KATE2, a randomized
276. Tricker, E. M. et al. Combined EGFR/MEK inhibition kinase inhibitors in cancer cells is mediated by loss of phase 2 study of atezolizumab (atezo)+trastuzumab
prevents the emergence of resistance in EGFR-mutant IGF-binding proteins. J. Clin. Invest. 118, 2609–2619 emtansine (T-DM1) vs placebo (pbo)+T-DM1 in
lung cancer. Cancer Discov. 5, 960–971 (2015). (2008). previously treated HER2+ advanced breast cancer
277. Ho, C. C. et al. Acquired BRAF V600E mutation as 299. Engelman, J. A. et al. MET amplification leads to (BC) [abstract PD3-01]. Cancer Res. 79 (Suppl. 4),
resistant mechanism after treatment with osimertinib. gefitinib resistance in lung cancer by activating ERBB3 PD3-01 (2019).
J. Thorac. Oncol. 12, 567–572 (2017). signaling. Science 316, 1039–1043 (2007). 320. Casalini, P., Iorio, M. V., Galmozzi, E. & Menard, S.
278. Chakrabarty, A. et al. H1047R phosphatidylinositol 300. Bean, J. et al. MET amplification occurs with or Role of HER receptors family in development and
3-kinase mutant enhances HER2-mediated without T790M mutations in EGFR mutant lung differentiation. J. Cell. Physiol. 200, 343–350
transformation by heregulin production and activation tumors with acquired resistance to gefitinib or (2004).
of HER3. Oncogene 29, 5193–5203 (2010). erlotinib. Proc. Natl Acad. Sci. USA 104, 321. Roskoski, R. Jr. The ErbB/HER receptor protein-tyrosine
279. Eichhorn, P. J. et al. Phosphatidylinositol 3-kinase 20932–20937 (2007). kinases and cancer. Biochem. Biophys. Res. Commun.
hyperactivation results in lapatinib resistance that is 301. Minuti, G. et al. Increased MET and HGF gene copy 319, 1–11 (2004).
reversed by the mTOR/phosphatidylinositol 3-kinase numbers are associated with trastuzumab failure in 322. Hynes, N. E., Horsch, K., Olayioye, M. A. &
inhibitor NVP-BEZ235. Cancer Res. 68, 9221–9230 HER2-positive metastatic breast cancer. Br. J. Cancer Badache, A. The ErbB receptor tyrosine family as
(2008). 107, 793–799 (2012). signal integrators. Endocr. Relat. Cancer 8, 151–159
280. Serra, V. et al. NVP-BEZ235, a dual PI3K/mTOR 302. Yano, S. et al. Hepatocyte growth factor induces (2001).
inhibitor, prevents PI3K signaling and inhibits the gefitinib resistance of lung adenocarcinoma with 323. Shi, F., Telesco, S. E., Liu, Y., Radhakrishnan, R.
growth of cancer cells with activating PI3K mutations. epidermal growth factor receptor-activating mutations. & Lemmon, M. A. ErbB3/HER3 intracellular
Cancer Res. 68, 8022–8030 (2008). Cancer Res. 68, 9479–9487 (2008). domain is competent to bind ATP and catalyze
281. Berns, K. et al. A functional genetic approach 303. Zhang, Z. et al. Activation of the AXL kinase causes autophosphorylation. Proc. Natl Acad. Sci. USA
identifies the PI3K pathway as a major determinant of resistance to EGFR-targeted therapy in lung cancer. 107, 7692–7697 (2010).
trastuzumab resistance in breast cancer. Cancer Cell Nat. Genet. 44, 852–860 (2012).
12, 395–402 (2007). 304. Byers, L. A. et al. An epithelial–mesenchymal Acknowledgements
282. Dave, B. et al. Loss of phosphatase and tensin transition gene signature predicts resistance to This study was supported by Grants-in-Aid for Scientific
homolog or phosphoinositol-3 kinase activation and EGFR and PI3K inhibitors and identifies Axl as a Research grant no. 17H06162 (to H.N.) from the Ministry of
response to trastuzumab or lapatinib in human therapeutic target for overcoming EGFR inhibitor Education, Culture, Sports, Science and Technology of Japan,
epidermal growth factor receptor 2-overexpressing resistance. Clin. Cancer Res. 19, 279–290 (2013). the Projects for Cancer Research by Therapeutic Evolution
locally advanced breast cancers. J. Clin. Oncol. 29, 305. Faber, A. C. et al. BIM expression in treatment-naive (P-CREATE; no. 16cm0106301h0001 to H.N. and no.
166–173 (2011). cancers predicts responsiveness to kinase inhibitors. 19cm0106335h0002 and 19cm0106310h0004 to S.Ko.),
283. Nagata, Y. et al. PTEN activation contributes to tumor Cancer Discov. 1, 352–365 (2011). the Development of Technology for Patient Stratification
inhibition by trastuzumab, and loss of PTEN predicts 306. Ng, K. P. et al. A common BIM deletion polymorphism Biomarker Discovery grant (no. 19ae0101074s0401 to H.N.)
trastuzumab resistance in patients. Cancer Cell 6, mediates intrinsic resistance and inferior responses from the Japan Agency for Medical Research and
117–127 (2004). to tyrosine kinase inhibitors in cancer. Nat. Med. 18, Development (AMED), and the National Cancer Center
284. Engelman, J. A. et al. Allelic dilution obscures 521–528 (2012). Research and Development Fund (no. 28-A-7 and 31-A-7
detection of a biologically significant resistance 307. Costa, C. et al. The impact of EGFR T790M mutations to H.N.).
mutation in EGFR-amplified lung cancer. J. Clin. Invest. and BIM mRNA expression on outcome in patients
116, 2695–2706 (2006). with EGFR-mutant NSCLC treated with erlotinib or Author contributions
285. Sos, M. L. et al. PTEN loss contributes to erlotinib chemotherapy in the randomized phase III EURTAC All authors contributed to each stage of the preparation of
resistance in EGFR-mutant lung cancer by activation trial. Clin. Cancer Res. 20, 2001–2010 (2014). this manuscript.
of Akt and EGFR. Cancer Res. 69, 3256–3261 308. Lee, J. E. et al. Hippo pathway effector YAP inhibition
(2009). restores the sensitivity of EGFR-TKI in lung Competing interests
286. Li, G. et al. Mechanisms of acquired resistance adenocarcinoma having primary or acquired EGFR-TKI S.Ko. received research funding from Ono Pharmaceutical
to trastuzumab emtansine in breast cancer cells. resistance. Biochem. Biophys. Res. Commun. 474, and Bristol-Myers Squibb outside this study. H.N. received
Mol. Cancer Ther. 17, 1441–1453 (2018). 154–160 (2016). honoraria and research funding from Ono Pharmaceutical,
287. Blakely, C. M. et al. NF-κB-activating complex 309. Nahta, R., Takahashi, T., Ueno, N. T., Hung, M. C. & Chugai Pharmaceutical, MSD and Bristol-Myers Squibb, and
engaged in response to EGFR oncogene inhibition Esteva, F. J. p27kip1 down-regulation is associated research funding from Taiho Pharmaceutical, Daiichi-Sankyo,
drives tumor cell survival and residual disease in lung with trastuzumab resistance in breast cancer cells. Kyowa Kirin, Zenyaku Kogyo, Oncolys BioPharma,
cancer. Cell Rep. 11, 98–110 (2015). Cancer Res. 64, 3981–3986 (2004). Debiopharma, Asahi-Kasei, Sysmex, Fujifilm, SRL, Astellas
288. Gao, S. P. et al. JAK2 inhibition sensitizes resistant 310. Niederst, M. J. et al. RB loss in resistant EGFR mutant Pharmaceutical, Sumitomo Dainippon Pharma and BD Japan
EGFR-mutant lung adenocarcinoma to tyrosine kinase lung adenocarcinomas that transform to small-cell lung outside this study. All other authors declare no competing
inhibitors. Sci. Signal. 9, ra33 (2016). cancer. Nat. Commun. 6, 6377 (2015). interests.
289. Chaib, I. et al. Co-activation of STAT3 and 311. Musolino, A. et al. Immunoglobulin G fragment C
YES-associated protein 1 (YAP1) pathway in receptor polymorphisms and clinical efficacy of Peer review information
EGFR-mutant NSCLC. J. Natl Cancer Inst. 109, trastuzumab-based therapy in patients with HER-2/ Nature Reviews Cancer thanks B. Pollack, F. Skoulidis and
djx014 (2017). neu-positive metastatic breast cancer. J. Clin. Oncol. N. Ueno for their contribution to the peer review of this work.
290. Shou, J. et al. Cyclosporine A sensitizes human 26, 1789–1796 (2008).
non-small cell lung cancer cells to gefitinib through 312. Kovtun, Y. V. et al. Antibody–maytansinoid conjugates Publisher’s note
inhibition of STAT3. Cancer Lett. 379, 124–133 designed to bypass multidrug resistance. Cancer Res. Springer Nature remains neutral with regard to jurisdictional
(2016). 70, 2528–2537 (2010). claims in published maps and institutional affiliations.
291. Kanda, R. et al. Erlotinib resistance in lung cancer 313. Sung, M. et al. Caveolae-mediated endocytosis
cells mediated by integrin β1/Src/Akt-driven bypass as a novel mechanism of resistance to trastuzumab Supplementary information
signaling. Cancer Res. 73, 6243–6253 (2013). emtansine (T-DM1). Mol. Cancer Ther. 17, 243–253 Supplementary information is available for this paper at
292. Yoshida, T. et al. Effects of Src inhibitors on cell (2018). https://doi.org/10.1038/s41568-020-00322-0.
growth and epidermal growth factor receptor and 314. Smith, L. M., Nesterova, A., Alley, S. C., Torgov, M. Y. &
MET signaling in gefitinib-resistant non-small cell Carter, P. J. Potent cytotoxicity of an auristatin-containing © Springer Nature Limited 2021
Nature Reviews | CAncER volume 21 | March 2021 | 197
You might also like
- Chapter 3 - Cell Signaling and Endocrine RegulationDocument75 pagesChapter 3 - Cell Signaling and Endocrine RegulationDee Buendia100% (1)
- Comparing Antibody and Small Molecule Therapies For CancerDocument14 pagesComparing Antibody and Small Molecule Therapies For CancerPatNo ratings yet
- Targeted Therapy in CancerDocument51 pagesTargeted Therapy in CancerSatya WangsaNo ratings yet
- Monoclonal Antibodies For The Therapy of Cancer: Oralpresentation Open AccessDocument3 pagesMonoclonal Antibodies For The Therapy of Cancer: Oralpresentation Open AccessSabiruddin Mirza DipuNo ratings yet
- Oncogene AddictionDocument5 pagesOncogene AddictionRoseli QueirozNo ratings yet
- Umor ImmunityDocument28 pagesUmor ImmunityGunjan sahuNo ratings yet
- Immune Therapy Opportunities in OvaDocument13 pagesImmune Therapy Opportunities in OvaShima YousefiNo ratings yet
- Ecancermedicalscience 2014 Article 441Document15 pagesEcancermedicalscience 2014 Article 441YulianaNo ratings yet
- Hype or Hope - Can Combination Therapies With Third Gener - 2021 - Critical ReviDocument22 pagesHype or Hope - Can Combination Therapies With Third Gener - 2021 - Critical ReviAndreea CohnNo ratings yet
- 10.1007@s40265 018 0916 4Document19 pages10.1007@s40265 018 0916 4Andreea CohnNo ratings yet
- Emss 53112Document20 pagesEmss 53112Baul luaBNo ratings yet
- 3 Tumor ImmunologyDocument12 pages3 Tumor ImmunologyWard KhalidNo ratings yet
- Targeted Therapy in Cancer - 2010Document48 pagesTargeted Therapy in Cancer - 2010Winson ChitraNo ratings yet
- Reviews: Systemic Immunity in CancerDocument15 pagesReviews: Systemic Immunity in Cancerliliana-contrerasNo ratings yet
- 7 Tumor ImmunityDocument51 pages7 Tumor ImmunityNanda SalmasNo ratings yet
- Targeting TAM Marco To Reprogram Macrophage in Cancer Cell 2016Document13 pagesTargeting TAM Marco To Reprogram Macrophage in Cancer Cell 2016Kudelko MatNo ratings yet
- Biotherapy: Historical PerspectiveDocument4 pagesBiotherapy: Historical PerspectiveArvin Jon BisligNo ratings yet
- Ne 2019 143972Document35 pagesNe 2019 143972Sara SabinaNo ratings yet
- Immune Checkpoint Inhibitors For Triple-Negative Breast Cancer - From Immunological Mechanisms To Clinical EvidenceDocument13 pagesImmune Checkpoint Inhibitors For Triple-Negative Breast Cancer - From Immunological Mechanisms To Clinical EvidenceasdffdsaNo ratings yet
- Chan 2019 ReviewDocument13 pagesChan 2019 ReviewYachao LiuNo ratings yet
- Melero 2007Document12 pagesMelero 2007Django BoyeeNo ratings yet
- 2015 Article 13Document8 pages2015 Article 13diahNo ratings yet
- ICI in OncologyDocument19 pagesICI in Oncologyraxi bacumabNo ratings yet
- Tumor Microenvironment Remodeling by Intratumoral Oncolytic Vaccinia Virus Enhances The Ef Ficacy of Immune-Checkpoint BlockadeDocument12 pagesTumor Microenvironment Remodeling by Intratumoral Oncolytic Vaccinia Virus Enhances The Ef Ficacy of Immune-Checkpoint BlockadeTaha AzadNo ratings yet
- Immunity To TumorDocument52 pagesImmunity To TumorSurya indra FirdausNo ratings yet
- 2020 - Tun - HL ImmunotherapyDocument10 pages2020 - Tun - HL ImmunotherapyMiguel ÁngelNo ratings yet
- Immune Checkpointtargeted Therapy Cancer and Autoimmune Diseases Represent Two Sides of The Same CoinDocument4 pagesImmune Checkpointtargeted Therapy Cancer and Autoimmune Diseases Represent Two Sides of The Same Coinpratiwi eka rahmawatiNo ratings yet
- 2021-Review-Tumour Neoantigen Mimicry by Microbial Species in Cancer ImmunotherapyDocument11 pages2021-Review-Tumour Neoantigen Mimicry by Microbial Species in Cancer ImmunotherapyCristian Felipe Sandoval QuiñonezNo ratings yet
- Chemoresistance Mechanisms of Breast Cancer and Their CountermeasuresDocument9 pagesChemoresistance Mechanisms of Breast Cancer and Their CountermeasuresPedro Olimpio CastilhoNo ratings yet
- Nri 1936 ArtigoDocument13 pagesNri 1936 ArtigoGlauce L TrevisanNo ratings yet
- Roovers2006 PDFDocument15 pagesRoovers2006 PDFAndre HaroNo ratings yet
- Host Defence Mechanisms Against TumorsDocument7 pagesHost Defence Mechanisms Against TumorsHamam AmastrdamNo ratings yet
- 2006 NRC Ab TherapyDocument14 pages2006 NRC Ab TherapyCandy TsaiNo ratings yet
- Molecular Biomarkers For The Treatment of Lung Cancer Personalized Therapy Beyond The EGFR MutationDocument12 pagesMolecular Biomarkers For The Treatment of Lung Cancer Personalized Therapy Beyond The EGFR MutationDiego Rodríguez VerdugoNo ratings yet
- Fonc 08 00086Document14 pagesFonc 08 00086Siska HarapanNo ratings yet
- Targeting TGF β signal transduction for cancer therapyDocument20 pagesTargeting TGF β signal transduction for cancer therapyIgnacio martinNo ratings yet
- Anti EGF Antibodies (Kashuf)Document12 pagesAnti EGF Antibodies (Kashuf)oshkashuflahoreNo ratings yet
- Vaccines 08 00321Document17 pagesVaccines 08 00321Kshitiz Raj ShresthaNo ratings yet
- Immunity To TumorDocument38 pagesImmunity To TumorAaryan PatelNo ratings yet
- Pharmaceuticals: Ye-Mi Kwon, Sou Hyun Kim, Young-Suk Jung and Jae-Hwan KwakDocument22 pagesPharmaceuticals: Ye-Mi Kwon, Sou Hyun Kim, Young-Suk Jung and Jae-Hwan KwakWalid Ebid ElgammalNo ratings yet
- Wedekind2018 Article PediatricCancerImmunotherapyOpDocument14 pagesWedekind2018 Article PediatricCancerImmunotherapyOpKAREN JAZMIN RUIZ MONROYNo ratings yet
- Immunopotent Part 1Document31 pagesImmunopotent Part 1samyNo ratings yet
- PT 1Document13 pagesPT 1wasan71No ratings yet
- Tumor Antigen: 1 Mechanism of Tumor AntigenesisDocument3 pagesTumor Antigen: 1 Mechanism of Tumor AntigenesisZiedTrikiNo ratings yet
- Harnessing The Power of The Immune SystemDocument3 pagesHarnessing The Power of The Immune SystemRAFEY AHMEDNo ratings yet
- Jones PA Et Al. 2019 Epigetnic Therapy in Immune-OncologyDocument11 pagesJones PA Et Al. 2019 Epigetnic Therapy in Immune-OncologyJasmyn KimNo ratings yet
- Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors For The Treatment of Non Small Cell Lung CancerDocument14 pagesEpidermal Growth Factor Receptor Tyrosine Kinase Inhibitors For The Treatment of Non Small Cell Lung CancerJimmy PrayogiNo ratings yet
- 17-Cancer and The Immune SystemDocument25 pages17-Cancer and The Immune SystemRami AlhilliNo ratings yet
- 18 JL 7Document15 pages18 JL 7Irma SihotangNo ratings yet
- Edbk 237967Document15 pagesEdbk 237967SYED MAAZ TARIQNo ratings yet
- 3 Tumor ImunotherapyDocument60 pages3 Tumor ImunotherapyXu FanNo ratings yet
- Boll Et Al-2023-Scientific ReportsDocument14 pagesBoll Et Al-2023-Scientific ReportsJoy IsmailNo ratings yet
- Cancer Ii - 230522 - 095514Document30 pagesCancer Ii - 230522 - 095514Tharuka ChandrasiriNo ratings yet
- 2021-Review-Gut Microbiota in Cancer Immune Response and ImmunotherapyDocument14 pages2021-Review-Gut Microbiota in Cancer Immune Response and ImmunotherapyCristian Felipe Sandoval QuiñonezNo ratings yet
- GMR 000665Document14 pagesGMR 000665Javier MartinNo ratings yet
- Triple-Negative Breast Cancer: Is It Possible To Reverse Receptor Negativity and Regain Sensitivity To Receptor-Targeting TherapiesDocument4 pagesTriple-Negative Breast Cancer: Is It Possible To Reverse Receptor Negativity and Regain Sensitivity To Receptor-Targeting TherapiesEditor SaraNo ratings yet
- Hallmarks PresentationDocument10 pagesHallmarks PresentationmanasNo ratings yet
- The Therapeutic Potential of Nanobodies: Ivana Jovčevska Serge MuyldermansDocument16 pagesThe Therapeutic Potential of Nanobodies: Ivana Jovčevska Serge MuyldermansJessica Asitimbay ZuritaNo ratings yet
- Imt.14.120 CART ImmunotherapyDocument13 pagesImt.14.120 CART ImmunotherapyMAGNo ratings yet
- Drake 2006Document3 pagesDrake 2006Ruben NatarîșNo ratings yet
- Targeted Therapies for Lung CancerFrom EverandTargeted Therapies for Lung CancerRavi SalgiaNo ratings yet
- Jamaoncology Wang 2020 VP 200013Document2 pagesJamaoncology Wang 2020 VP 200013zhe zhNo ratings yet
- 4.the Commensal Microbiome Is Associated With anti-PD-1 Efficacy in Metastatic Melanoma PatientsDocument6 pages4.the Commensal Microbiome Is Associated With anti-PD-1 Efficacy in Metastatic Melanoma Patientszhe zhNo ratings yet
- 2023-JTO-Genetic Intratumor Heterogeneity Remodels The Immune Microenvironment and Induces Immune Evasion in Brain Metastasis of Lung CancerDocument21 pages2023-JTO-Genetic Intratumor Heterogeneity Remodels The Immune Microenvironment and Induces Immune Evasion in Brain Metastasis of Lung Cancerzhe zhNo ratings yet
- 48.akkermansia Muciniphila Phospholipid Induces Homeostatic Immune ResponsesDocument21 pages48.akkermansia Muciniphila Phospholipid Induces Homeostatic Immune Responseszhe zhNo ratings yet
- 2019-Lancet Oncology-Changes in Clinical Trials of Cancer Drugs in Mainland China Over The Decade 2009-18 - A Systematic ReviewDocument8 pages2019-Lancet Oncology-Changes in Clinical Trials of Cancer Drugs in Mainland China Over The Decade 2009-18 - A Systematic Reviewzhe zhNo ratings yet
- 学数据库方法CDD-FSP1 confers ferroptosis resistance in KEAP1 mutant non-small cell lung carcinoma in NRF2-dependent and -independent mannerDocument11 pages学数据库方法CDD-FSP1 confers ferroptosis resistance in KEAP1 mutant non-small cell lung carcinoma in NRF2-dependent and -independent mannerzhe zhNo ratings yet
- METTL3 and STAT3 Form A Positive Feedback Loop To Promote Cell Metastasis in Hepatocellular CarcinomaDocument19 pagesMETTL3 and STAT3 Form A Positive Feedback Loop To Promote Cell Metastasis in Hepatocellular Carcinomazhe zhNo ratings yet
- One Off Low Dose CT For Lung Cancer Screening in China A Multicentre Population Based Prospective Cohort StudyDocument14 pagesOne Off Low Dose CT For Lung Cancer Screening in China A Multicentre Population Based Prospective Cohort Studyzhe zhNo ratings yet
- Risk Adapted Starting Age For Personalized Colorectal Cancer Screening Validated Evidence From National Population Based StudiesDocument21 pagesRisk Adapted Starting Age For Personalized Colorectal Cancer Screening Validated Evidence From National Population Based Studieszhe zhNo ratings yet
- 2022-Autophage-The COPS3-FOXO3 Positive Feedback Loop Regulates Autophagy To Promote Cisplatin Resistance in OsteosarcomaDocument19 pages2022-Autophage-The COPS3-FOXO3 Positive Feedback Loop Regulates Autophagy To Promote Cisplatin Resistance in Osteosarcomazhe zhNo ratings yet
- 2022-oncogene-UPF1:circRPPH1:ATF3 Feedback Loop Promotes The Malignant Phenotype and Stemness of GSCsDocument15 pages2022-oncogene-UPF1:circRPPH1:ATF3 Feedback Loop Promotes The Malignant Phenotype and Stemness of GSCszhe zhNo ratings yet
- E3 ubiquitin ligase UBR5 promotes pancreatic cancer growth and aerobic glycolysis by downregulating FBP1 via destabilization of C:EBPαDocument15 pagesE3 ubiquitin ligase UBR5 promotes pancreatic cancer growth and aerobic glycolysis by downregulating FBP1 via destabilization of C:EBPαzhe zhNo ratings yet
- Sci Adv. 2020.揭示阿尔兹海默症患者糖基化修饰分子网络改变机制Integrative glycoproteomics reveals protein N-glycosylation aberrations and glycoproteomic network alterations in Alzheimer's diseaseDocument19 pagesSci Adv. 2020.揭示阿尔兹海默症患者糖基化修饰分子网络改变机制Integrative glycoproteomics reveals protein N-glycosylation aberrations and glycoproteomic network alterations in Alzheimer's diseasezhe zhNo ratings yet
- Cancers Make Their Own Luck - Theories of Cancer OriginsDocument15 pagesCancers Make Their Own Luck - Theories of Cancer Originszhe zhNo ratings yet
- Epigenetic Clocks Aging and CancerDocument3 pagesEpigenetic Clocks Aging and Cancerzhe zhNo ratings yet
- 15.tertiary Lymphoid Structures in CancerDocument12 pages15.tertiary Lymphoid Structures in Cancerzhe zhNo ratings yet
- Learning The Metabolic Language of CancerDocument2 pagesLearning The Metabolic Language of Cancerzhe zhNo ratings yet
- Engineering Bacteria As Interactive Cancer TherapiesDocument7 pagesEngineering Bacteria As Interactive Cancer Therapieszhe zhNo ratings yet
- Jto Muc1 2023Document39 pagesJto Muc1 2023zhe zhNo ratings yet
- 30.defined Tumor Antigen-Specific T Cells Potentiate Personalized TCR-T Cell Therapy and Prediction of Immunotherapy ResponseDocument13 pages30.defined Tumor Antigen-Specific T Cells Potentiate Personalized TCR-T Cell Therapy and Prediction of Immunotherapy Responsezhe zhNo ratings yet
- Umeno2018 Article ClinicalFeaturesOfChronicEnterDocument9 pagesUmeno2018 Article ClinicalFeaturesOfChronicEnterzhe zhNo ratings yet
- NC-AhR Diminishes The Efficacy of Chemotherapy Via Suppressing STING Dependent Type-I Interferon in Bladder CancerDocument17 pagesNC-AhR Diminishes The Efficacy of Chemotherapy Via Suppressing STING Dependent Type-I Interferon in Bladder Cancerzhe zhNo ratings yet
- 28.engineering The Next Generation of Cell-Based TherapeuticsDocument21 pages28.engineering The Next Generation of Cell-Based Therapeuticszhe zhNo ratings yet
- 17.targeted Therapies For Lung Cancer Patients With Oncogenic Driver Molecular AlterationsDocument16 pages17.targeted Therapies For Lung Cancer Patients With Oncogenic Driver Molecular Alterationszhe zhNo ratings yet
- 16) Signaling Pathways That Control Gene ActivityDocument27 pages16) Signaling Pathways That Control Gene ActivityRNo ratings yet
- Factors Controlling Growth 05-01-2020Document20 pagesFactors Controlling Growth 05-01-2020kashif manzoorNo ratings yet
- Cell Physiology Revision QuestionsDocument6 pagesCell Physiology Revision QuestionsjoojoNo ratings yet
- Apoptosis and NecrosisDocument8 pagesApoptosis and NecrosisDaniela Mădălina GhețuNo ratings yet
- Chapter 12 Biosignaling: Multiple Choice QuestionsDocument3 pagesChapter 12 Biosignaling: Multiple Choice Questionssurankokila50% (4)
- PDF Desarrollo de Ejercicios CompressDocument19 pagesPDF Desarrollo de Ejercicios Compresslorenzo fabian cruz sigueñasNo ratings yet
- Figure For Question 2Document3 pagesFigure For Question 2Santhiya KunasegaranNo ratings yet
- IL1 AntagonistaDocument13 pagesIL1 AntagonistaZitlal-lin VictoriaNo ratings yet
- Understanding Apoptosis and Apoptotic Pathways Targeted CancerDocument14 pagesUnderstanding Apoptosis and Apoptotic Pathways Targeted Canceranupama_rani_2No ratings yet
- Cell Junctions, Gap Adhesions, and ExtracellularDocument58 pagesCell Junctions, Gap Adhesions, and ExtracellularFabian Christine MaeNo ratings yet
- Unit 4 Guided Notes For AP Daily VideosDocument4 pagesUnit 4 Guided Notes For AP Daily VideosjyfjytdjuNo ratings yet
- Biomedicine & Pharmacotherapy: ReviewDocument11 pagesBiomedicine & Pharmacotherapy: ReviewRasyidu MashuriNo ratings yet
- Steroid Hormones! Mechanisms of Action!Document14 pagesSteroid Hormones! Mechanisms of Action!leh.mo9315No ratings yet
- Comprehensive Biology of Antipyretic PathwaysDocument8 pagesComprehensive Biology of Antipyretic Pathwaysq9tt4ftcxnNo ratings yet
- Macrofagos Asociados A TumoresDocument9 pagesMacrofagos Asociados A Tumoresjuan ramon zepeda tejedaNo ratings yet
- Biochemistry of OlfactionDocument18 pagesBiochemistry of Olfactionroxy8marie8chanNo ratings yet
- TRANSFAC and JASPAR PWMs TableDocument9 pagesTRANSFAC and JASPAR PWMs Tablealya ghinaNo ratings yet
- Apoptosis Poster March 20106547Document1 pageApoptosis Poster March 20106547Achmad JunaidiNo ratings yet
- Pattern Recognition Receptors (PRRS) : Rossana Zaru, University of Dundee, UkDocument4 pagesPattern Recognition Receptors (PRRS) : Rossana Zaru, University of Dundee, UkFree Escort ServiceNo ratings yet
- Tinjauan Pustaka: Respon Imunologi Pada Dermatitis Kontak IritanDocument7 pagesTinjauan Pustaka: Respon Imunologi Pada Dermatitis Kontak IritanSatriadwykiyprasetya ThiodwkiyNo ratings yet
- Drug Receptor TheoryDocument9 pagesDrug Receptor TheoryFish YanNo ratings yet
- Ashrae DatabaseDocument81 pagesAshrae Databasesam100% (1)
- Mechanism of Hormone ActionDocument27 pagesMechanism of Hormone Actiondaffa fatihNo ratings yet
- Part 8 Cell CommunicationDocument28 pagesPart 8 Cell CommunicationLê Thanh HằngNo ratings yet
- Cell SignallingDocument14 pagesCell SignallingWei JernNo ratings yet
- Billesblle 2023 Structural Basis of Odorant RecogniDocument30 pagesBillesblle 2023 Structural Basis of Odorant RecogniAgnes_Agnes_AgnesNo ratings yet
- Rollno - 02 PDD GPCRDocument20 pagesRollno - 02 PDD GPCRJayesh KadamNo ratings yet
- Redaccao ForenseDocument9 pagesRedaccao ForenseBrado AfricanoNo ratings yet
- Nuclear Receptors 2006Document31 pagesNuclear Receptors 2006lsintaningtyasNo ratings yet