Professional Documents
Culture Documents
Hannan Et Al 2024 Laparoscopic Versus Open Appendicectomy Performed by Adult General Surgeons in Pre Teenage Years
Hannan Et Al 2024 Laparoscopic Versus Open Appendicectomy Performed by Adult General Surgeons in Pre Teenage Years
Uploaded by
syeda rabikaCopyright:
Available Formats
You might also like
- Chapter 1 Partnership Formation Test BanksDocument46 pagesChapter 1 Partnership Formation Test BanksRaisa Gelera92% (24)
- Life Cycle of SecurityDocument40 pagesLife Cycle of SecurityPuneet Sachdeva50% (2)
- RPM Sample Book2 PDFDocument52 pagesRPM Sample Book2 PDFዘቃልአብሞላ100% (8)
- Treatise Superior Law Higher Law My LawDocument54 pagesTreatise Superior Law Higher Law My Law1 watchman100% (2)
- Appendicitis NaddlerDocument6 pagesAppendicitis NaddlerMedardo ApoloNo ratings yet
- Alganabi2021 Article SurgicalSiteInfectionAfterOpenDocument9 pagesAlganabi2021 Article SurgicalSiteInfectionAfterOpenWahyudhy SajaNo ratings yet
- Apendicitis - LaparosDocument3 pagesApendicitis - LaparosLaura CampañaNo ratings yet
- Pediatric Inguinal Hernia PDFDocument5 pagesPediatric Inguinal Hernia PDFade-djufrieNo ratings yet
- Saluja 2017Document6 pagesSaluja 2017AndikaNo ratings yet
- Journal of Pediatric Surgery: Steven L. Lee, Lara Spence, Kyle Mock, James X. Wu, Huan Yan, Daniel A. DeugarteDocument6 pagesJournal of Pediatric Surgery: Steven L. Lee, Lara Spence, Kyle Mock, James X. Wu, Huan Yan, Daniel A. DeugarteMelian AnitaNo ratings yet
- Optimal Timing For Soave Primary Pull-Through in Short-SegmentDocument7 pagesOptimal Timing For Soave Primary Pull-Through in Short-SegmentNate MichalakNo ratings yet
- Andolfi 2020 Article Robot-assistedLaparoscopicPyelDocument7 pagesAndolfi 2020 Article Robot-assistedLaparoscopicPyelAntonio López MolláNo ratings yet
- 03-Ira MunawwarahDocument8 pages03-Ira MunawwarahMayaNo ratings yet
- Use of White Blood Cell Count and Negative Appendectomy RateDocument8 pagesUse of White Blood Cell Count and Negative Appendectomy RatePremaKurniaNo ratings yet
- Comparative Videolaryngoscope Performance in Children: Data From The Pediatric Difficult Intubation RegistryDocument3 pagesComparative Videolaryngoscope Performance in Children: Data From The Pediatric Difficult Intubation RegistryTan AndiNo ratings yet
- Research Journal ClubDocument12 pagesResearch Journal ClubUsama SalehNo ratings yet
- Laparoscopic Versus Open Surgery For Gastric Gastrointestinal Stromal Tumors: A Propensity Score Matching AnalysisDocument10 pagesLaparoscopic Versus Open Surgery For Gastric Gastrointestinal Stromal Tumors: A Propensity Score Matching AnalysisFerdian PriantoNo ratings yet
- @medicinejournal European Journal of Pediatric Surgery January 2020Document126 pages@medicinejournal European Journal of Pediatric Surgery January 2020Ricardo Uzcategui ArreguiNo ratings yet
- DMCN 13480Document9 pagesDMCN 13480contoisaNo ratings yet
- Enhanced Recovery After Surgery (ERAS) in The Paediatric PopulationDocument6 pagesEnhanced Recovery After Surgery (ERAS) in The Paediatric PopulationkhalidNo ratings yet
- Masson Et Al-2007-Colorectal DiseaseDocument4 pagesMasson Et Al-2007-Colorectal DiseaseCamy CarmenNo ratings yet
- Editorial: Ureteropelvic Junction Obstruction (Upjo) in InfantsDocument2 pagesEditorial: Ureteropelvic Junction Obstruction (Upjo) in InfantssandyNo ratings yet
- Am J Otolaryngol: Derek K. Kong, Amanda M. Kong, Isaac Wasserman, Dillan F. Villavisanis, Alyssa M. HackettDocument6 pagesAm J Otolaryngol: Derek K. Kong, Amanda M. Kong, Isaac Wasserman, Dillan F. Villavisanis, Alyssa M. HackettYusi nursiamNo ratings yet
- 10 1016@j Jpedsurg 2020 02 024Document6 pages10 1016@j Jpedsurg 2020 02 024Rizka Desti AyuniNo ratings yet
- Yeh 2019Document5 pagesYeh 2019sigitdwimulyoNo ratings yet
- Laparoscopic Versus Open Appendicectomy: A Comparative StudyDocument7 pagesLaparoscopic Versus Open Appendicectomy: A Comparative StudyChristianWicaksonoNo ratings yet
- Bakker 2012Document10 pagesBakker 2012ieoNo ratings yet
- 1 s2.0 S002234681930301X 2Document5 pages1 s2.0 S002234681930301X 2suyudi kimikoNo ratings yet
- Apendisitis MRM 3Document8 pagesApendisitis MRM 3siti solikhaNo ratings yet
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDocument6 pagesSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedNo ratings yet
- Radiography: G. Ogunmefun, M. Hardy, S. BoynesDocument8 pagesRadiography: G. Ogunmefun, M. Hardy, S. BoynesDian J PutraNo ratings yet
- AppendicitisDocument13 pagesAppendicitisASdaNo ratings yet
- 06-Systematic Review of Perforated Appendicitis and PhlegmonDocument7 pages06-Systematic Review of Perforated Appendicitis and PhlegmonTo MarNo ratings yet
- Unukovych 2016Document7 pagesUnukovych 2016jdavies231No ratings yet
- Braces e Escoliose2Document8 pagesBraces e Escoliose2Erika Galiza BritoNo ratings yet
- Clinical Diagnosis of Uncomplicated, Acute Appendicitis Remains An Imperfect ScienceDocument3 pagesClinical Diagnosis of Uncomplicated, Acute Appendicitis Remains An Imperfect ScienceHector ReinozoNo ratings yet
- Elbourne 87846Document5 pagesElbourne 87846Dian NovitasariNo ratings yet
- Clinical Diognosis ColorectalDocument2 pagesClinical Diognosis ColorectalRizal Sven VollfiedNo ratings yet
- Intravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofDocument1 pageIntravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofoomculunNo ratings yet
- Laparoscopic Appendectomy For Perforated Appendicitis in Children Has Complication Rates Comparable With Those of Open AppendectomyDocument7 pagesLaparoscopic Appendectomy For Perforated Appendicitis in Children Has Complication Rates Comparable With Those of Open AppendectomyGina Kristina NanginNo ratings yet
- Laparoscopic Compared With Open Surgery TOADocument7 pagesLaparoscopic Compared With Open Surgery TOARizka AdiNo ratings yet
- Pediatric Pulmonology - 2023 - Zarfati - Conservative and Operative Management of Spontaneous Pneumothorax in Children andDocument7 pagesPediatric Pulmonology - 2023 - Zarfati - Conservative and Operative Management of Spontaneous Pneumothorax in Children andRezidenti GrigoreNo ratings yet
- AcalasiaDocument3 pagesAcalasiaSamantha Lara GarciaNo ratings yet
- Menopausal Symptoms and Surgical Complications After Opportunistic Bilateral Salpingectomy, A Register-Based Cohort StudyDocument10 pagesMenopausal Symptoms and Surgical Complications After Opportunistic Bilateral Salpingectomy, A Register-Based Cohort StudytriNo ratings yet
- Laparoscopic Versus Open Reduction of Idiopathic IDocument8 pagesLaparoscopic Versus Open Reduction of Idiopathic IDaGiTrVel'zNo ratings yet
- BAaadDocument5 pagesBAaadekalospratamaNo ratings yet
- The Utility of Ultrasonography in The Diagnosis of Polycystic Ovarian Syndrome PCOS in Adolescents 2014 Journal of Pediatric and Adolescent GynecologyDocument1 pageThe Utility of Ultrasonography in The Diagnosis of Polycystic Ovarian Syndrome PCOS in Adolescents 2014 Journal of Pediatric and Adolescent GynecologyfujimeisterNo ratings yet
- Comparison of Urokinase and Video-Assisted Thoracoscopic Surgery For Treatment of Childhood EmpyemaDocument7 pagesComparison of Urokinase and Video-Assisted Thoracoscopic Surgery For Treatment of Childhood EmpyemaDr Nilesh NagdeveNo ratings yet
- RCCM 200601-027ocDocument7 pagesRCCM 200601-027ocDiego AndradeNo ratings yet
- MOC IV 2014 Laparoscopy and Elective Colon Resection June 2012Document18 pagesMOC IV 2014 Laparoscopy and Elective Colon Resection June 2012pingusNo ratings yet
- Parade New AnakDocument10 pagesParade New AnakMukhizalNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Khemani2009Document7 pagesKhemani2009Dwi Putri SekariniNo ratings yet
- JournalDocument6 pagesJournalYosuaNo ratings yet
- 1 Bjs 10662Document8 pages1 Bjs 10662Vu Duy KienNo ratings yet
- Bun V34N3p223Document6 pagesBun V34N3p223pingusNo ratings yet
- Monn - 2013 - Trends in Robot-Assisted Laparoscopic Pyeloplasty in Pediatric PatientsDocument6 pagesMonn - 2013 - Trends in Robot-Assisted Laparoscopic Pyeloplasty in Pediatric PatientsAntonio López MolláNo ratings yet
- VOTE PSR AnakDocument9 pagesVOTE PSR AnakINGGRID 102015016No ratings yet
- El Beheiry2019Document4 pagesEl Beheiry2019achmadaNo ratings yet
- Advancesinsurgeryfor Abdominalwalldefects: Gastroschisis and OmphaloceleDocument12 pagesAdvancesinsurgeryfor Abdominalwalldefects: Gastroschisis and OmphaloceleSitti HazrinaNo ratings yet
- Shorts 10 107Document4 pagesShorts 10 107Imam AlifurqonNo ratings yet
- Management of The Acute Appendix Mass: A Survey of Surgical PracticeDocument3 pagesManagement of The Acute Appendix Mass: A Survey of Surgical PracticeSamuel H SihotangNo ratings yet
- Indocyanine Green Fluorescence Angiography and The.17Document7 pagesIndocyanine Green Fluorescence Angiography and The.17Icaro DanielNo ratings yet
- The SAGES Manual of Flexible EndoscopyFrom EverandThe SAGES Manual of Flexible EndoscopyPeter NauNo ratings yet
- Routine Use of Laparoscopic Techniques in Daily Practice Improves Outcomes After AppendectomyDocument7 pagesRoutine Use of Laparoscopic Techniques in Daily Practice Improves Outcomes After Appendectomysyeda rabikaNo ratings yet
- 27Document1 page27syeda rabikaNo ratings yet
- 13Document1 page13syeda rabikaNo ratings yet
- 35Document1 page35syeda rabikaNo ratings yet
- 16Document1 page16syeda rabikaNo ratings yet
- 15Document2 pages15syeda rabikaNo ratings yet
- 18Document1 page18syeda rabikaNo ratings yet
- The 16 Types of Camera Shots & Angles (2020 Video Guide) - BoordsDocument14 pagesThe 16 Types of Camera Shots & Angles (2020 Video Guide) - BoordsPatrick R. EtienneNo ratings yet
- SMPH BrochureDocument2 pagesSMPH BrochureChristine M.No ratings yet
- ESIC by CA Pranav ChandakDocument15 pagesESIC by CA Pranav ChandakMehak Kaushikk100% (1)
- Menu Plan Assignment - Emalea BriggsDocument2 pagesMenu Plan Assignment - Emalea Briggsapi-490916133No ratings yet
- Review Trip Details and BookDocument1 pageReview Trip Details and BookHamza HamdanNo ratings yet
- Odoacer: - Doh - S Odóakros)Document13 pagesOdoacer: - Doh - S Odóakros)SashimiTourloublancNo ratings yet
- CHAPTER 10 - Compensation IncomeDocument3 pagesCHAPTER 10 - Compensation IncomeDeviane CalabriaNo ratings yet
- Supreme CourtDocument5 pagesSupreme CourtDivyasri JeganNo ratings yet
- Unit 1 4 Delhi Through The AgesDocument80 pagesUnit 1 4 Delhi Through The AgesNitigya ThakurNo ratings yet
- Agreement Draft For Sub ContractDocument6 pagesAgreement Draft For Sub ContractBittudubey officialNo ratings yet
- Rpt-Sow Form 3 2024Document6 pagesRpt-Sow Form 3 2024g-16025707No ratings yet
- Japan Secuireties 2018Document381 pagesJapan Secuireties 2018TôThànhPhongNo ratings yet
- GP IRR ChecklistDocument4 pagesGP IRR ChecklistMUSA BLINKNo ratings yet
- Builder NocDocument3 pagesBuilder NocLonari Kunbi SamajNo ratings yet
- Simulation TestDocument18 pagesSimulation TestNhiNo ratings yet
- 4PS FinalDocument44 pages4PS Finalcorazon lopez100% (2)
- EmbodymercyDocument5 pagesEmbodymercyapi-465627486No ratings yet
- Plea Bargaining Framework in Drugs CasesDocument6 pagesPlea Bargaining Framework in Drugs CasesMack Hale BunaganNo ratings yet
- Balancing National Security and Civil LibertiesDocument2 pagesBalancing National Security and Civil LibertiesNico FrimponNo ratings yet
- Manifesto For Wendy TeoDocument2 pagesManifesto For Wendy Teoapi-3853288No ratings yet
- Final BasantDocument22 pagesFinal BasantMuqaddas IsrarNo ratings yet
- Offer Letter Shorey SinghDocument6 pagesOffer Letter Shorey Singhkz9g9mfn67No ratings yet
- Subodh KhareDocument10 pagesSubodh Kharepragmatic.desiNo ratings yet
- Maxim Australia - December 2017Document100 pagesMaxim Australia - December 2017wdmalik60% (5)
- KS NRO Progress Report 2015Document47 pagesKS NRO Progress Report 2015CALORIE CALORIENo ratings yet
- Asstt - Library Information OfficerDocument6 pagesAsstt - Library Information OfficerSanjit MandalNo ratings yet
Hannan Et Al 2024 Laparoscopic Versus Open Appendicectomy Performed by Adult General Surgeons in Pre Teenage Years
Hannan Et Al 2024 Laparoscopic Versus Open Appendicectomy Performed by Adult General Surgeons in Pre Teenage Years
Uploaded by
syeda rabikaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hannan Et Al 2024 Laparoscopic Versus Open Appendicectomy Performed by Adult General Surgeons in Pre Teenage Years
Hannan Et Al 2024 Laparoscopic Versus Open Appendicectomy Performed by Adult General Surgeons in Pre Teenage Years
Uploaded by
syeda rabikaCopyright:
Available Formats
LOWER GI SURGERY
Ann R Coll Surg Engl 2023; 000: 1–6
doi 10.1308/rcsann.2023.0044
Laparoscopic versus open appendicectomy
performed by adult general surgeons in pre-
teenage years children: a single-centre experience
E Hannan1, EMY Lim1, G Feeney1, L O’Brien2, JC Coffey1,3, C Peirce1,3
1
University Hospital Limerick, Dooradoyle, Ireland
2
Children’s Health Ireland at Crumlin, Dublin, Ireland
3
University of Limerick, Dooradoyle, Ireland
ABSTRACT
Introduction The utilisation of laparoscopic appendicectomy (LA) in children remains contentious despite the well-recognised advantages of laparoscopic
surgery. The purpose of this study was to compare intraoperative and postoperative outcomes in LA and open appendicectomy (OA) when performed by
adult general surgeons outside specialist paediatric practice in younger children.
Methods A retrospective review of all patients under the age of 13 who underwent LA for suspected appendicitis over a two-year period was conducted.
These were case-matched with an equivalent number of patients who underwent OA during the same period. Intraoperative and postoperative outcomes
were compared.
Results Fifty-one patients underwent LA during the study period. Patient demographics were statistically equivalent with the OA cohort. A statistically
significant longer median operating time (58 vs 49min) was noted in the LA group, but intraoperative outcomes were otherwise comparable. LA, when
compared with OA, was associated with a significant improvement in postoperative length of stay (2 vs 3 days, p < 0.001), postoperative
complication rate (0% vs 6%, p = 0.01), negative appendicectomy rate (3.9% vs 17.6%, p < 0.001) and 30-day readmission rate (0% vs 5.9%,
p = 0.03). No patients in the LA group required conversion to open surgery.
Conclusion LA can be safely delivered by adult general surgeons to younger paediatric populations outside the setting of paediatric specialist practice,
with statistically significant improvements in postoperative outcomes noted when compared with OA. These findings are of importance in the current
healthcare context where adult general surgeons continue to perform the majority of paediatric appendicectomies.
KEYWORDS
Acute appendicitis – Laparoscopic appendicectomy – Open appendicectomy – Paediatric
appendicectomy
Accepted 30 May 2023
CORRESPONDENCE TO
Enda Hannan, E: endahannan@rcsi.com
Introduction challenging and the proposed benefit of laparoscopic
incisions over a small Lanz incision questionable.8 Thus,
Acute appendicitis (AA) is the most common paediatric the uptake of LA has been slower for children compared
surgical emergency.1 Traditionally, appendicectomy has with adult populations.1–8
been performed by open surgery until the advent of It remains common in many healthcare services that
laparoscopic approaches in the 1980s.1,2 Laparoscopy is AA in children is managed by adult general surgeons
associated with a shorter length of stay (LOS), decreased because of the lack of availability of paediatric
analgesic requirements and reduced wound surgeons.8,9 Although there has been a demonstrable
complications.3–5 However, the benefit of laparoscopic increase in the utilisation of LA for children in the past
appendicectomy (LA) in the paediatric population decade, this has been largely observed in specialist
compared with open appendicectomy (OA) remains paediatric surgery practice.8,9 Recent multicentre studies
controversial.6,7 A recent meta-analysis revealed no show that most paediatric appendicectomies performed
significant difference in postoperative complications by adult general surgeons are by open surgery.9,10 This
between approaches in children, and criticisms of LA contrasts with the otherwise widespread utilisation of
include an increased operative cost, longer operating laparoscopy for index operations in adults.4,5,9
time and increased rate of intra-abdominal abscesses Although many studies have compared LA and OA in
(IAA).5–7 It has also been suggested that the small body children, few have examined outcomes in those
size of young children makes laparoscopic surgery performed by adult general surgeons outside paediatric
Ann R Coll Surg Engl 2023; 000: 1–6 1
HANNAN LIM FEENEY O’BRIEN COFFEY PEIRCE LAPAROSCOPIC VS OPEN PAEDIATRIC APPENDICECTOMY
specialist practice.6–9 Multiple studies have also examined at the base after placement of three Endoloops® (two
children defined as patients either under the age of 16 or proximal, one distal) and extracted via the subumbilical
18.6–10 In such groups, it is possible that many children in incision via specimen retrieval bag. OA was performed
their mid- to late-teens may be close to the size of an using either a Lanz or Gridiron muscle-splitting incision
adult, and the specific difficulties posed by LA in a with the appendix ligated at the base using a
smaller abdomen are not encountered.6–9 The purpose of non-absorbable suture, following which the appendix
this study was to compare intraoperative and stump was buried using a purse-string suture.
postoperative outcomes in LA and OA when performed
by adult general surgeons in children under the age of Ethics
13, thus largely focusing on children prior to or early in All patient data were anonymised for the purpose of this
puberty. This information could be used to inform safe study. No identifying information was retained by the
practice in healthcare services where paediatric authors or included in the article. Because this was a
emergency surgery is frequently delivered by adult retrospective service evaluation involving anonymised
general surgeons. data, ethics committee approval was not required.
Statistical analysis
Methods Statistical analysis was performed using IBM SPSS version
24 (SPSS Inc, Chicago, IL, USA). Non-parametric data were
Study design and data collection expressed as median with interquartile range and
A retrospective review of patients under the age of 13 years parametric data as a mean with standard deviation.
who underwent appendicectomy for suspected appendicitis Univariate analysis was performed using Student’s t-test
over a two-year period (July 2019–July 2021) was or Mann–Whitney U test for continuous variables, and
conducted in a tertiary referral university teaching Fischer’s exact test for categorical variables. A p-value of
hospital where adult general surgeons provide emergency <0.05 was considered statistically significant.
surgical care to paediatric patients. Currently, it is more
common in our institution for patients with AA in this age
demographic to be managed by OA. All patients in this age
group who underwent LA were identified by reviewing
Results
the operating theatre logbooks. These patients were Patient demographics
matched with an equivalent number who underwent OA During the two-year study period, 51 patients under the
during the same period. Patients who underwent OA age of 13 years underwent LA for AA. These were
were selected by a simple randomisation process that compared with 51 patients in the same age range who
blinded investigators to selection to avoid bias. Following underwent OA for AA during the same period and who
this, an in-depth review of medical records, operation were randomly selected from the operating theatre
notes, discharge summaries, radiology reports and logbooks to avoid selection bias. In the LA cohort, the
histopathology reports was performed for those included majority of patients were male (59%, n = 30) with a
in the study. Data collected included baseline median age of 10 years (range 6–12) and a median weight
demographics, operating time, estimated blood loss, of 35.2kg (range 23.3–76.6); most had an American
intraoperative findings, the presence of complicated Society of Anaesthesiologists (ASA) grade of I (76.5%,
appendicitis (defined as an intraoperative finding of n = 39). In the OA cohort, the majority of patients were
perforated appendicitis), postoperative LOS, opioid use, also male (61%, n = 31) with a median age of 9 years
postoperative complications and histological confirmation (range 4–12) and a median weight of 28.7kg (19–42.1);
of appendicitis. Patients admitted for an elective or again most had an ASA grade of I (88.2%, n = 45). No
interval appendicectomy were excluded from the study. statistical significance was observed in baseline
characteristics between the two cohorts (Table 1).
Surgical technique
All operations were performed either by a consultant Preoperative imaging
general surgeon or a general surgical registrar. The In the OA group, 43.1% (n = 22) underwent a preoperative
choice of surgical approach was based on individual ultrasound scan, whereas 37.3% (n = 19) underwent an
surgeon preference. LA was performed using a 3-trocar ultrasound scan in the LA group (p = 0.27). Ultrasound
technique with standard adult laparoscopic scanning was diagnostic of appendicitis in 31.8% (n = 7) of
instrumentation. A 12mm balloon port was placed open cases who underwent preoperative imaging,
subumbilical by Hasson technique and two 5mm ports compared with 5.2% (n = 1) in those who underwent LA
were inserted under laparoscopic vision in the left iliac (p = 0.049).
fossa and suprapubic region. A diagnostic laparoscopy
was routinely performed to identify the cause for the Intraoperative outcomes
patient’s symptoms, which included a small bowel walk In the LA group, the median operating time was 58min
and inspecting the ovaries in female patients. Following (range 32–107) compared with 49min (range 20–98) in
division of the mesoappendix, the appendix was divided the OA group (p = 0.01). Blood loss was minimal overall,
2 Ann R Coll Surg Engl 2023; 000: 1–6
HANNAN LIM FEENEY O’BRIEN COFFEY PEIRCE LAPAROSCOPIC VS OPEN PAEDIATRIC APPENDICECTOMY
with a median of 10ml recorded in both cohorts. No terminal ileal congenital band adhesion that appeared to
laparoscopic cases required conversion to open surgery. be causing subacute small bowel obstruction and was
The majority (96%, n = 49) of open procedures were thus divided. In the other case, terminal ileitis was
performed via a Lanz incision, with the remainder encountered. There were no open cases for suspected AA
performed via a Gridiron incision. A diagnostic in which the surgeon decided to leave the appendix in
laparoscopy was documented in all laparoscopic situ. No alternate diagnoses for the patient’s symptoms
procedures. Nine patients (17.6%) had complicated were made in any open cases, and there were no cases
appendicitis in the LA group, compared with eight in the during this time in which a paediatric patient underwent
OA group (15.7%). Wound closure was performed by an open exploration where an intraoperative decision to
absorbable sutures in all laparoscopic cases, whereas not remove the appendix was made (Table 2).
15.7% (n = 8) of open cases were closed by nonabsorbable
sutures or skin clips. The majority of open cases were Postoperative outcomes
performed by consultants (60.8%, n = 31), whereas most The median postoperative LOS was 2 days (range 1–6) in
laparoscopic cases were performed by registrars (56.9%, the LA cohort and 3 days (range 1–7) in the OA cohort
n = 29). A drain was placed in four open cases (7.8%) and (p < 0.001). Pain scores on the first postoperative day,
three laparoscopic cases (5.9%; p = 0.69). No adverse recorded using a 10-point visual analogue score, were
events related to laparoscopic port placement, such as higher in OA (median 6/10) compared with LA (median
bladder injury, were recorded. During the study period, 5/10; p = 0.16). Postoperative opioid use was also higher
two patients underwent a diagnostic laparoscopy for in patients who underwent open surgery, with 72.5%
suspected AA in which the decision was made not to (n = 37) of the OA cohort requiring opioids on the first
remove the appendix based on intraoperative findings. In postoperative day compared with 52.9% (n = 27) in the
both cases the operating surgeon decided that the LA cohort (p = 0.04). No postoperative complications
appendix was not acutely inflamed and that there was were recorded in the laparoscopic group, whereas six
alternate pathology present to explain the patient’s (11.8%) were recorded in those who underwent open
symptoms. In one case, the patient was found to have a surgery (p = 0.01). Of these complications, two were
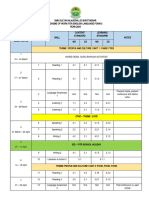
Table 1 Patient demographics
LA group (n = 51) OA group (n = 51) p-value
Median age (years) 10 (range 6–12) 9 (range 4–11) 0.25
Male (%) 59 (n = 30) 61 (n = 31) 0.42
Female (%) 41 (n = 21) 39 (n = 19) 0.34
ASA I (%) 76.5 (n = 39) 88.2 (n = 45) 0.06
ASA II (%) 21.6 (n = 11) 11.8 (n = 6) 0.09
ASA III (%) 2.0 (n = 1) 0 (n = 0) 0.16
Median weight (kg) 35.2 (range 23.3–76.6) 28.7 (range 9–42.1) 0.18
ASA = American Society of Anesthesiologists; LA = laparoscopic appendicectomy; OA = open appendicectomy
Table 2 Intraoperative outcomes
LA group (n = 51) OA group (n = 51) p-value
Median operating time (min) 58 (32–107) 49 (20–98) 0.01
Median blood loss (ml) 10 10 1
Complicated appendicitis (%) 17.6 (n = 9) 15.7 (n = 8) 0.39
Drain placement (%) 5.9 (n = 3) 7.8 (n = 4) 0.34
Conversion to open surgery (%) 0 (n = 0) N/A N/A
Nonabsorbable wound closure (%) 0 (n = 0) 15.7 (n = 8) 0.01
LA = laparoscopic appendicectomy; N/A = not applicable; OA = open appendicectomy
Ann R Coll Surg Engl 2023; 000: 1–6 3
HANNAN LIM FEENEY O’BRIEN COFFEY PEIRCE LAPAROSCOPIC VS OPEN PAEDIATRIC APPENDICECTOMY
postoperative IAAs managed by intravenous antibiotics, or clips. Despite an equivalent rate of perforation
two were postoperative ileus and two were superficial between the two cohorts, the incidence of postoperative
surgical site infections that were managed with oral IAA and ileus was lower in patients managed by LA and
antibiotics. The 30-day readmission rate was 5.9% (n = 3) no patients required conversion to open surgery.
in the OA group, whereas no patients in the LA group Although a statistically significant difference in median
were readmitted (p = 0.03) (Table 3). operating time favouring OA was noted, it is difficult to
argue that a reduction of 9min is truly clinically
Histopathological findings significant, particularly in the context of a slower
The histopathological negative appendicectomy rate was recovery and higher complication rate.
higher in open surgery (n = 9, 17.6%) compared with It is interesting to note that the negative appendicectomy
laparoscopic surgery (n = 2, 3.9%; p < 0.001). In the open rate was significantly lower in patients who underwent LA
cohort, histopathological diagnoses included AA (51%, compared with OA. This is despite more patients in the
n = 26), acute suppurative appendicitis (9.8%, n = 5), open cohort undergoing preoperative ultrasound
acute gangrenous appendicitis (5.9%, n = 3) and scanning, of which a greater proportion were diagnostic of
perforated appendicitis (15.7%, n = 8). In the laparoscopic AA than in the laparoscopic cohort. This is perhaps
cohort, patients were diagnosed histopathologically with unsurprising, as performing a diagnostic laparoscopy is
AA (52.9%, n = 27), acute suppurative appendicitis (13.7%, recognised as a standard step in LA, especially when the
n = 7), acute gangrenous appendicitis (11.8%, n = 6) and diagnosis is made on history and clinical examination
perforated appendicitis (17.6%, n = 9). No patients were alone without the support of definitive radiology.10 In all
diagnosed with an appendiceal neoplasm or malignancy. laparoscopic cases, a diagnostic laparoscopy was routinely
performed, which allowed for the potential identification
of an alternate diagnosis that may explain the patient’s
Discussion symptoms, such as ovarian or small bowel pathology. This
In this retrospective comparative analysis, we observed allowed for two patients during the study period to both
that LA performed by adult general surgeons in younger avoid a negative appendicectomy and to have the cause of
paediatric patients is a safe and feasible means of their symptoms accurately diagnosed. This ability to
managing AA that compares favourably with OA, with a thoroughly evaluate the intraperitoneal cavity is a distinct
statistically significant reduction in the overall advantage of LA compared with access via an incision in
complication rate, postoperative LOS, opioid use, 30-day the right iliac fossa, during which the patient may have an
readmission rate and negative appendicectomy rate. alternate diagnosis missed and may also be exposed to the
Lower postoperative pain scores were also observed in risk of an unnecessary appendicectomy.3
the LA cohort, probably as a result of the reduced The results suggest that the management of paediatric
incision burden allowing for a quicker recovery and AA by the adult general surgeon outside paediatric
earlier discharge. Fewer wound-related complications specialist practice is best delivered by a laparoscopic
were observed in the LA cohort, whereas surgeons had a approach, with less postoperative morbidity compared
greater tendency to favour nonabsorbable wound closure with OA. This is important information because the
for open cases, thus subjecting children to a further majority of children undergoing appendicectomy in the
medical appointment to allow for the removal of sutures UK and Ireland do so in non-specialist paediatric centres
Table 3 Postoperative outcomes
LA group (n = 51) OA group (n = 51) p-value
Median postoperative LOS (days) 2 (range 1–6) 3 (range 1–7) <0.001
Median day one pain scores (scale 1–10) 5 6 0.16
Day one opioid use (%) 52.9 (n = 27) 72.5 (n = 37) 0.04
Overall complication rate (%) 0 (n = 0) 11.8 (n = 6) 0.01
IAA (%) 0 (n = 0) 3.9 (n = 2) 0.07
Ileus (%) 0 (n = 0) 3.9 (n = 2) 0.07
SSI (%) 0 (n = 0) 3.9 (n = 2) 0.07
30-day readmission (%) 0 (n = 0) 5.9 (n = 3) 0.03
Negative appendicectomy (%) 3.9 (n = 2) 17.6 (n = 9) <0.001
IAA = intra-abdominal abscess; LA = laparoscopic appendicectomy; LOS = length of stay; OA = open appendicectomy; SSI = surgical site infection
4 Ann R Coll Surg Engl 2023; 000: 1–6
HANNAN LIM FEENEY O’BRIEN COFFEY PEIRCE LAPAROSCOPIC VS OPEN PAEDIATRIC APPENDICECTOMY
(SPCs).8–11 In the current climate in which laparoscopic reduced morbidity and improved long-term
expertise continues to increase among adult general satisfaction.19 It is also true that OA has consistently
surgeons, it is logical that this expertise can be applied to been demonstrated to have a shorter operating time than
paediatric patients under their care, thus allowing LA, but our results would suggest that accepting an
children to benefit from the well-recognised advantages increase in median operating time of less than 10min can
of minimally invasive surgery for the most common lead to significantly improved postoperative outcomes.
paediatric surgical emergency.4,5,9 Finally, it has been debated as to whether multiple
Despite the well-recognised advantages of laparoscopic laparoscopic port sites truly offer a postoperative
surgery, the uptake of LA in paediatric patients recovery benefit compared with a small Lanz incision. In
internationally is behind that of adult patients.12,13 the current study, the LA cohort experienced reduced
Currently, there are no best practice guidelines postoperative pain scores, less postoperative opioid use
regarding the best surgical approach for management of and an earlier discharge from hospital, all suggesting
AA in the context of a non-SPC.12 However, relevant data that LA facilitates a quicker recovery compared with OA.
to guide practice do exist. Recent studies and
meta-analyses have reported no significant difference in Study limitations
IAA rates between OA and LA in children, with a The current study is not without limitations. It is
significant reduction in postoperative LOS, wound retrospective in nature, conducted in a single centre,
infection and ileus rates in LA.7,12,14 Long-term studies involves a relatively modest cohort of patients and lacks
have also demonstrated greater satisfaction regarding long-term follow-up. It is also important to note that the
cosmetic outcomes following LA.12,15 A recent laparoscopic cohort tended towards being slightly older
meta-analysis based on six randomised controlled trials and of greater weight than the open cohort, which may
and 33 case-control studies strongly advocated for LA suggest that the former group offered more favourable
over OA in children, reporting consistently superior conditions for minimally invasive surgery; however, these
postoperative outcomes.16 Despite these clear differences did not achieve statistical significance.
advantages, overall rates of utilisation of paediatric LA Nonetheless, the findings are of importance. Although
lag behind adult usage and experience both in and out of many studies have examined outcomes between LA and
SPCs.12 OA in paediatric patients, few have specifically looked at
Perceived disadvantages of LA in the paediatric this when performed by adult general surgeons outside
population have generated some resistance to utilising paediatric specialist practice. This is an important
minimally invasive approaches in the management of AA consideration, because it has been demonstrated that the
in children. Many surgeons have avoided LA for fear of a majority of appendicectomies are performed by adult
higher incidence of postoperative IAA compared with OA. general surgeons outside SPCs, and thus these results
This belief has been supported by previous meta-analyses reflect the reality of current practice. This study also
that included data from early experiences with LA in specifically examined patients under the age of 13,
children.17,18 However, subsequent studies based on more whereas other recent studies have included patients
recent data have shown that IAA rates are largely either under the age of 16 or 18.6–10,12,16 This distinction
equivalent between both modalities.16 It is likely that was made to focus on children who were smaller in size
early experiences regarding higher rates of IAA post-LA and thus the challenges posed by laparoscopy in a
reflect the initial learning curve with this technique, with smaller intra-abdominal cavity would be most apparent.
outcomes improving with developing expertise in Our results suggest that, even with the challenge posed
laparoscopic surgery. The findings of our study concur by a reduced working space for laparoscopic surgery, LA
that LA currently does not pose a greater risk of IAA is nonetheless safe and feasible.
when compared with OA. Another frequently proposed
disadvantage of LA in children is that the smaller size of
the patient may make the procedure more technically
challenging owing to reduced working space in the
Conclusions
intra-abdominal cavity.8 This was not the case in the LA can be safely delivered by adult general surgeons
current study, where all procedures were successfully outside SPCs to a younger paediatric population, with
completed laparoscopically without intraoperative or numerous advantages when compared with OA. A
postoperative complications. It has also been proposed statistically significant difference in postoperative LOS,
that LA in children is not cost-effective, creating a postoperative complication rate, 30-day readmission rate
requirement for expensive specialised paediatric and negative appendicectomy rate was observed in the
laparoscopic equipment.8 However, in the current study, laparoscopic cohort. No patients in the LA group
no additional cost was generated owing to the required conversion to open surgery, suggesting the
requirement for such equipment, because all feasibility of this approach. The clear benefits of LA
laparoscopic cases were completed using standard adult compared with OA in this cohort demonstrated by the
equipment. One retrospective study reported the cost of current study are of importance in a context in which the
surgery in paediatric LA being €150 higher than OA, but majority of paediatric appendicectomies are performed
it is important to consider this against a shorter LOS, by adult general surgeons.
Ann R Coll Surg Engl 2023; 000: 1–6 5
HANNAN LIM FEENEY O’BRIEN COFFEY PEIRCE LAPAROSCOPIC VS OPEN PAEDIATRIC APPENDICECTOMY
Data availability and code availability 7 Aziz O, Athanasiou T, Tekkis PP et al. Laparoscopic versus open appendectomy in
children: a meta-analysis. Ann Surg 2006; 243: 17–27.
The data that support the findings of this study are 8 Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for
available from the corresponding author upon reasonable suspected appendicitis. Cochrane Database Syst Rev 2010: CD001546.
9 Adwan H, Weerasuriya CK, Endleman P et al. Laparoscopic versus open
request. Data analysis was performed using the software appendicectomy in children: a UK district general hospital experience. J Pediatr
package SPSS (SPSS Inc, Chicago, IL). Surg 2014; 49: 277–279.
10 Ahmed O, Mealy K, Sorensen J. Exploring geographic variation in acute appendectomy
in Ireland: results from a national registry study. BMJ Open 2019; 9: e025231.
Open Access This is an open-access article 11 Tiboni S, Bhangu A, Hall NJ; Paediatric Surgery Trainees Research Network and the
National Surgical Research Collaborative. Outcome of appendicectomy in children
distributed under the terms of the performed in paediatric surgery units compared with general surgery units. Br J
Creative Commons Attribution 4.0 International License, Surg 2014; 101: 707–714.
which permits unrestricted use, distribution, 12 O’Connell RM, Elwahab SA, Mealy K. Should all paediatric appendicectomies
reproduction, and adaptation in any medium, provided be performed in a specialist or high-volume setting? Ir J Med Sci 2020; 189:
1015–1021.
the original work is properly attributed.
13 Bhatt NR, Dunne E, Faraz M et al. Trends in the use of laparoscopic versus open
paediatric appendicectomy: a regional 12-year study and a national survey. World J
Surg 2018; 42: 3792–3802.
References 14 Naqvi M, Adams H, Jaunoo S. Senior general surgical trainees’ perspectives on the
1 Fujishiro J, Watanabe E, Hirahara N et al. Laparoscopic versus open appendectomy need for paediatric surgical experience. The Bulletin 2018; 100: 177–178.
for acute appendicitis in children: a nationwide retrospective study on 15 Lee SL, Yaghoubian A, Kaji A. Laparoscopic vs open appendectomy in children:
postoperative outcomes. J Gastrointest Surg 2021; 25: 1036–1044. outcomes comparison based on age, sex, and perforation status. Arch Surg 2011;
2 Schneuer FJ, Adams SE, Bentley JP et al. A population-based comparison of the 146: 1118–1121.
post-operative outcomes of open and laparoscopic appendicectomy in children. 16 Kapischke M, Pries A, Caliebe A. Short term and long term results after open vs.
Med J Aust 2018; 209: 80–85. laparoscopic appendectomy in childhood and adolescence: a subgroup analysis.
3 Tate JJT, Dawson JW, Chung SCS et al. Laparoscopic versus open appendicectomy: BMC Pediatr 2013; 13: 154.
prospective randomised trial. The Lancet 1993; 342: 633–637. 17 Low ZX, Bonney GK, So JBY et al. Laparoscopic versus open appendectomy in
4 Southgate E, Vousden N, Karthikesalingam A et al. Laparoscopic vs open pediatric patients with complicated appendicitis: a meta-analysis. Surg Endosc
appendectomy in older patients. Arch Surg 2012; 147: 557–562. 2018; 33: 4066–4077.
5 Thomson J-E, Kruger D, Jann-Kruger C et al. Laparoscopic versus open surgery for 18 Markar SR, Blackburn S, Cobb R et al. Laparoscopic versus open appendectomy for
complicated appendicitis: a randomized controlled trial to prove safety. Surg complicated and uncomplicated appendicitis in children. J Gastrointest Surg 2012;
Endosc 2015; 29: 2027–2032. 16: 1993–2004.
6 Dai L, Shuai J. Laparoscopic versus open appendectomy in adults and children: a 19 Zhang S, Du T, Jiang X, Song C. Laparoscopic appendectomy in children with
meta-analysis of randomized controlled trials. United European Gastroenterol J perforated appendicitis: a meta-analysis. Surg Laparosc Endosc Percutaneous
2017; 5: 542–553. Tech 2017; 27: 262–266.
6 Ann R Coll Surg Engl 2023; 000: 1–6
You might also like
- Chapter 1 Partnership Formation Test BanksDocument46 pagesChapter 1 Partnership Formation Test BanksRaisa Gelera92% (24)
- Life Cycle of SecurityDocument40 pagesLife Cycle of SecurityPuneet Sachdeva50% (2)
- RPM Sample Book2 PDFDocument52 pagesRPM Sample Book2 PDFዘቃልአብሞላ100% (8)
- Treatise Superior Law Higher Law My LawDocument54 pagesTreatise Superior Law Higher Law My Law1 watchman100% (2)
- Appendicitis NaddlerDocument6 pagesAppendicitis NaddlerMedardo ApoloNo ratings yet
- Alganabi2021 Article SurgicalSiteInfectionAfterOpenDocument9 pagesAlganabi2021 Article SurgicalSiteInfectionAfterOpenWahyudhy SajaNo ratings yet
- Apendicitis - LaparosDocument3 pagesApendicitis - LaparosLaura CampañaNo ratings yet
- Pediatric Inguinal Hernia PDFDocument5 pagesPediatric Inguinal Hernia PDFade-djufrieNo ratings yet
- Saluja 2017Document6 pagesSaluja 2017AndikaNo ratings yet
- Journal of Pediatric Surgery: Steven L. Lee, Lara Spence, Kyle Mock, James X. Wu, Huan Yan, Daniel A. DeugarteDocument6 pagesJournal of Pediatric Surgery: Steven L. Lee, Lara Spence, Kyle Mock, James X. Wu, Huan Yan, Daniel A. DeugarteMelian AnitaNo ratings yet
- Optimal Timing For Soave Primary Pull-Through in Short-SegmentDocument7 pagesOptimal Timing For Soave Primary Pull-Through in Short-SegmentNate MichalakNo ratings yet
- Andolfi 2020 Article Robot-assistedLaparoscopicPyelDocument7 pagesAndolfi 2020 Article Robot-assistedLaparoscopicPyelAntonio López MolláNo ratings yet
- 03-Ira MunawwarahDocument8 pages03-Ira MunawwarahMayaNo ratings yet
- Use of White Blood Cell Count and Negative Appendectomy RateDocument8 pagesUse of White Blood Cell Count and Negative Appendectomy RatePremaKurniaNo ratings yet
- Comparative Videolaryngoscope Performance in Children: Data From The Pediatric Difficult Intubation RegistryDocument3 pagesComparative Videolaryngoscope Performance in Children: Data From The Pediatric Difficult Intubation RegistryTan AndiNo ratings yet
- Research Journal ClubDocument12 pagesResearch Journal ClubUsama SalehNo ratings yet
- Laparoscopic Versus Open Surgery For Gastric Gastrointestinal Stromal Tumors: A Propensity Score Matching AnalysisDocument10 pagesLaparoscopic Versus Open Surgery For Gastric Gastrointestinal Stromal Tumors: A Propensity Score Matching AnalysisFerdian PriantoNo ratings yet
- @medicinejournal European Journal of Pediatric Surgery January 2020Document126 pages@medicinejournal European Journal of Pediatric Surgery January 2020Ricardo Uzcategui ArreguiNo ratings yet
- DMCN 13480Document9 pagesDMCN 13480contoisaNo ratings yet
- Enhanced Recovery After Surgery (ERAS) in The Paediatric PopulationDocument6 pagesEnhanced Recovery After Surgery (ERAS) in The Paediatric PopulationkhalidNo ratings yet
- Masson Et Al-2007-Colorectal DiseaseDocument4 pagesMasson Et Al-2007-Colorectal DiseaseCamy CarmenNo ratings yet
- Editorial: Ureteropelvic Junction Obstruction (Upjo) in InfantsDocument2 pagesEditorial: Ureteropelvic Junction Obstruction (Upjo) in InfantssandyNo ratings yet
- Am J Otolaryngol: Derek K. Kong, Amanda M. Kong, Isaac Wasserman, Dillan F. Villavisanis, Alyssa M. HackettDocument6 pagesAm J Otolaryngol: Derek K. Kong, Amanda M. Kong, Isaac Wasserman, Dillan F. Villavisanis, Alyssa M. HackettYusi nursiamNo ratings yet
- 10 1016@j Jpedsurg 2020 02 024Document6 pages10 1016@j Jpedsurg 2020 02 024Rizka Desti AyuniNo ratings yet
- Yeh 2019Document5 pagesYeh 2019sigitdwimulyoNo ratings yet
- Laparoscopic Versus Open Appendicectomy: A Comparative StudyDocument7 pagesLaparoscopic Versus Open Appendicectomy: A Comparative StudyChristianWicaksonoNo ratings yet
- Bakker 2012Document10 pagesBakker 2012ieoNo ratings yet
- 1 s2.0 S002234681930301X 2Document5 pages1 s2.0 S002234681930301X 2suyudi kimikoNo ratings yet
- Apendisitis MRM 3Document8 pagesApendisitis MRM 3siti solikhaNo ratings yet
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDocument6 pagesSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedNo ratings yet
- Radiography: G. Ogunmefun, M. Hardy, S. BoynesDocument8 pagesRadiography: G. Ogunmefun, M. Hardy, S. BoynesDian J PutraNo ratings yet
- AppendicitisDocument13 pagesAppendicitisASdaNo ratings yet
- 06-Systematic Review of Perforated Appendicitis and PhlegmonDocument7 pages06-Systematic Review of Perforated Appendicitis and PhlegmonTo MarNo ratings yet
- Unukovych 2016Document7 pagesUnukovych 2016jdavies231No ratings yet
- Braces e Escoliose2Document8 pagesBraces e Escoliose2Erika Galiza BritoNo ratings yet
- Clinical Diagnosis of Uncomplicated, Acute Appendicitis Remains An Imperfect ScienceDocument3 pagesClinical Diagnosis of Uncomplicated, Acute Appendicitis Remains An Imperfect ScienceHector ReinozoNo ratings yet
- Elbourne 87846Document5 pagesElbourne 87846Dian NovitasariNo ratings yet
- Clinical Diognosis ColorectalDocument2 pagesClinical Diognosis ColorectalRizal Sven VollfiedNo ratings yet
- Intravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofDocument1 pageIntravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofoomculunNo ratings yet
- Laparoscopic Appendectomy For Perforated Appendicitis in Children Has Complication Rates Comparable With Those of Open AppendectomyDocument7 pagesLaparoscopic Appendectomy For Perforated Appendicitis in Children Has Complication Rates Comparable With Those of Open AppendectomyGina Kristina NanginNo ratings yet
- Laparoscopic Compared With Open Surgery TOADocument7 pagesLaparoscopic Compared With Open Surgery TOARizka AdiNo ratings yet
- Pediatric Pulmonology - 2023 - Zarfati - Conservative and Operative Management of Spontaneous Pneumothorax in Children andDocument7 pagesPediatric Pulmonology - 2023 - Zarfati - Conservative and Operative Management of Spontaneous Pneumothorax in Children andRezidenti GrigoreNo ratings yet
- AcalasiaDocument3 pagesAcalasiaSamantha Lara GarciaNo ratings yet
- Menopausal Symptoms and Surgical Complications After Opportunistic Bilateral Salpingectomy, A Register-Based Cohort StudyDocument10 pagesMenopausal Symptoms and Surgical Complications After Opportunistic Bilateral Salpingectomy, A Register-Based Cohort StudytriNo ratings yet
- Laparoscopic Versus Open Reduction of Idiopathic IDocument8 pagesLaparoscopic Versus Open Reduction of Idiopathic IDaGiTrVel'zNo ratings yet
- BAaadDocument5 pagesBAaadekalospratamaNo ratings yet
- The Utility of Ultrasonography in The Diagnosis of Polycystic Ovarian Syndrome PCOS in Adolescents 2014 Journal of Pediatric and Adolescent GynecologyDocument1 pageThe Utility of Ultrasonography in The Diagnosis of Polycystic Ovarian Syndrome PCOS in Adolescents 2014 Journal of Pediatric and Adolescent GynecologyfujimeisterNo ratings yet
- Comparison of Urokinase and Video-Assisted Thoracoscopic Surgery For Treatment of Childhood EmpyemaDocument7 pagesComparison of Urokinase and Video-Assisted Thoracoscopic Surgery For Treatment of Childhood EmpyemaDr Nilesh NagdeveNo ratings yet
- RCCM 200601-027ocDocument7 pagesRCCM 200601-027ocDiego AndradeNo ratings yet
- MOC IV 2014 Laparoscopy and Elective Colon Resection June 2012Document18 pagesMOC IV 2014 Laparoscopy and Elective Colon Resection June 2012pingusNo ratings yet
- Parade New AnakDocument10 pagesParade New AnakMukhizalNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Khemani2009Document7 pagesKhemani2009Dwi Putri SekariniNo ratings yet
- JournalDocument6 pagesJournalYosuaNo ratings yet
- 1 Bjs 10662Document8 pages1 Bjs 10662Vu Duy KienNo ratings yet
- Bun V34N3p223Document6 pagesBun V34N3p223pingusNo ratings yet
- Monn - 2013 - Trends in Robot-Assisted Laparoscopic Pyeloplasty in Pediatric PatientsDocument6 pagesMonn - 2013 - Trends in Robot-Assisted Laparoscopic Pyeloplasty in Pediatric PatientsAntonio López MolláNo ratings yet
- VOTE PSR AnakDocument9 pagesVOTE PSR AnakINGGRID 102015016No ratings yet
- El Beheiry2019Document4 pagesEl Beheiry2019achmadaNo ratings yet
- Advancesinsurgeryfor Abdominalwalldefects: Gastroschisis and OmphaloceleDocument12 pagesAdvancesinsurgeryfor Abdominalwalldefects: Gastroschisis and OmphaloceleSitti HazrinaNo ratings yet
- Shorts 10 107Document4 pagesShorts 10 107Imam AlifurqonNo ratings yet
- Management of The Acute Appendix Mass: A Survey of Surgical PracticeDocument3 pagesManagement of The Acute Appendix Mass: A Survey of Surgical PracticeSamuel H SihotangNo ratings yet
- Indocyanine Green Fluorescence Angiography and The.17Document7 pagesIndocyanine Green Fluorescence Angiography and The.17Icaro DanielNo ratings yet
- The SAGES Manual of Flexible EndoscopyFrom EverandThe SAGES Manual of Flexible EndoscopyPeter NauNo ratings yet
- Routine Use of Laparoscopic Techniques in Daily Practice Improves Outcomes After AppendectomyDocument7 pagesRoutine Use of Laparoscopic Techniques in Daily Practice Improves Outcomes After Appendectomysyeda rabikaNo ratings yet
- 27Document1 page27syeda rabikaNo ratings yet
- 13Document1 page13syeda rabikaNo ratings yet
- 35Document1 page35syeda rabikaNo ratings yet
- 16Document1 page16syeda rabikaNo ratings yet
- 15Document2 pages15syeda rabikaNo ratings yet
- 18Document1 page18syeda rabikaNo ratings yet
- The 16 Types of Camera Shots & Angles (2020 Video Guide) - BoordsDocument14 pagesThe 16 Types of Camera Shots & Angles (2020 Video Guide) - BoordsPatrick R. EtienneNo ratings yet
- SMPH BrochureDocument2 pagesSMPH BrochureChristine M.No ratings yet
- ESIC by CA Pranav ChandakDocument15 pagesESIC by CA Pranav ChandakMehak Kaushikk100% (1)
- Menu Plan Assignment - Emalea BriggsDocument2 pagesMenu Plan Assignment - Emalea Briggsapi-490916133No ratings yet
- Review Trip Details and BookDocument1 pageReview Trip Details and BookHamza HamdanNo ratings yet
- Odoacer: - Doh - S Odóakros)Document13 pagesOdoacer: - Doh - S Odóakros)SashimiTourloublancNo ratings yet
- CHAPTER 10 - Compensation IncomeDocument3 pagesCHAPTER 10 - Compensation IncomeDeviane CalabriaNo ratings yet
- Supreme CourtDocument5 pagesSupreme CourtDivyasri JeganNo ratings yet
- Unit 1 4 Delhi Through The AgesDocument80 pagesUnit 1 4 Delhi Through The AgesNitigya ThakurNo ratings yet
- Agreement Draft For Sub ContractDocument6 pagesAgreement Draft For Sub ContractBittudubey officialNo ratings yet
- Rpt-Sow Form 3 2024Document6 pagesRpt-Sow Form 3 2024g-16025707No ratings yet
- Japan Secuireties 2018Document381 pagesJapan Secuireties 2018TôThànhPhongNo ratings yet
- GP IRR ChecklistDocument4 pagesGP IRR ChecklistMUSA BLINKNo ratings yet
- Builder NocDocument3 pagesBuilder NocLonari Kunbi SamajNo ratings yet
- Simulation TestDocument18 pagesSimulation TestNhiNo ratings yet
- 4PS FinalDocument44 pages4PS Finalcorazon lopez100% (2)
- EmbodymercyDocument5 pagesEmbodymercyapi-465627486No ratings yet
- Plea Bargaining Framework in Drugs CasesDocument6 pagesPlea Bargaining Framework in Drugs CasesMack Hale BunaganNo ratings yet
- Balancing National Security and Civil LibertiesDocument2 pagesBalancing National Security and Civil LibertiesNico FrimponNo ratings yet
- Manifesto For Wendy TeoDocument2 pagesManifesto For Wendy Teoapi-3853288No ratings yet
- Final BasantDocument22 pagesFinal BasantMuqaddas IsrarNo ratings yet
- Offer Letter Shorey SinghDocument6 pagesOffer Letter Shorey Singhkz9g9mfn67No ratings yet
- Subodh KhareDocument10 pagesSubodh Kharepragmatic.desiNo ratings yet
- Maxim Australia - December 2017Document100 pagesMaxim Australia - December 2017wdmalik60% (5)
- KS NRO Progress Report 2015Document47 pagesKS NRO Progress Report 2015CALORIE CALORIENo ratings yet
- Asstt - Library Information OfficerDocument6 pagesAsstt - Library Information OfficerSanjit MandalNo ratings yet