Professional Documents
Culture Documents
AUTHENTIC MORNING ADHKAR - Precious Gems From The Quran and Sunnah
AUTHENTIC MORNING ADHKAR - Precious Gems From The Quran and Sunnah
Uploaded by
Omar Is CrazyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AUTHENTIC MORNING ADHKAR - Precious Gems From The Quran and Sunnah
AUTHENTIC MORNING ADHKAR - Precious Gems From The Quran and Sunnah
Uploaded by
Omar Is CrazyCopyright:
Available Formats
Dental Management of Systemic Diseases Relevant to
Dentist
Gastrointestinal Diseases
It is well known that a considerable number of systemic diseases can affect the oral
cavity. Among these are the gastrointestinal disorders (GIDs), which have a high
worldwide prevalence and a growing incidence. Although gastrointestinal signs and
symptoms are predominant, oral manifestations may occur and even herald the onset of
the underlying GID.
The term inflammatory bowel disease (IBD) involves a group of chronic inflammatory
disorders of not well known etiology that affects different portions of the gastrointestinal
tract, mainly the bowels. The two main forms of IBD are Crohn’s disease (CD) and
Ulcerative Colitis (UC).
-Crohn’s disease:
Patients with Crohn´s disease develop chronic inflammation and non-caseating
granulomas in different parts of the gastrointestinal tract, especially in the distal ileum
and colon. The most common signs and symptoms include diarrhea and abdominal pain,
but some patients could experience extra-intestinal manifestations of the disease,
involving eyes, joints, skin and mouth.
• Oral manifestations:
Patients with active CD have been reported to have a higher degree of oral lesions.
- Labial swelling and fissuring: cracks or crusts along the vermilion.
- Mucosal tags: Tags present in the vestibule and retro-molar region.
- Cobblestoning: The mucosa exhibits normal color plaques separated by mild
depressions or fissures, giving the appearance of cobblestones.
- Mucogingivitis: The gingival tissues may become hyperplasic and granular, not
only the free gingiva but also the attached gingiva.
- Recurrent aphtous stomatitis (RAS) like ulceration present as recurrent bouts of
usually multiple, round or ovoid superficial ulcers that have circumscribed
margins surrounded by an erythematous halo, clinically indestenguible from
RAS.
- Angular cheilitis: The commissure and adjacent skin may have recurrent fissures
and indurated erythematous plaques not necessarily related with candida
infection.
Hadeel Gamal FD-ASU 1
Dental Management of Systemic Diseases Relevant to
Dentist
• The treatment of CD is focused in the control of the underlying intestinal
involvement and in some circumstances, this is usually performed by drug
administration such as steroids. Oral lesions are well managed with topical
steroids, but the use of systemic agents might be necessary for some cases.
-Ulcerative colitis:
Chronic inflammation of the gastrointestinal tract limited to the mucosa of the rectum
and colon, and only in some rare instances it can spread to upward portions of the
digestive tube (e.g. small intestine). Within the inflammation there is no granuloma
formation, which is a main feature of CD. The disease usually progresses with
repeatedly periods of remissions and exacerbations.
• Oral manifestations:
- Pyostomatitis vegetans (PV): a chronic mucocutaneous pathology that consists in
the formation of numerous pustules (intra and sub epithelial abscesses) of white-
yellowish content with an erythematous and edematous base. These lesions may
break or coalesce giving a snail track appearance.
- Others: RAS like ulcers, glossitis, cheilitis, stomatitis, mucosal ulcers and
gingival inflammation. These lesions (like in CD) usually arise as a result of the
nutritional deficiencies (e.g. iron, folate or B12) secondary to the intestinal
involvement and/or as an adverse side effect of drugs used to treat UC.
• The first line treatment consists in the use systemic corticosteroids, which
usually helps in the remission of the oral manifestations. Immunosuppressive
and biological agents are also commonly used.
-Celiac disease:
An autoimmune disease in which genetically predisposed individuals exhibit damages
in the small intestine villi as a consequence of an abnormal immune response subsequent
to the ingestion of gluten (present in most cereals).
Hadeel Gamal FD-ASU 2
Dental Management of Systemic Diseases Relevant to
Dentist
It has been estimated that CD affects approximately 1% of the world’s population, but
over the last years, CD has experienced a large increase, affecting 1 in every 85 to 300
people.
• Oral Manifestations:
Oral lesions would be useful in early detection of atypical CD, which corresponds to
the most common form of this disease.
- Dental enamel defects, specifically enamel hypoplasia that is distributed
bilaterally and symmetrically in both dental arches.
- Atrophic glossitis and glossodynia: These signs and symptoms are likely to be
secondary to anemia rather than be caused by the disease itself.
- A decrease in salivary flow rates have been reported to be associated with the
active phase of the disease, resulting in a dry mouth and burning sensation of
the tongue and increased susceptibility to caries of the hypoplastic enamel.
- RAS like oral ulceration.
- Bleeding tendency: Celiac disease has been associated with alterations in
coagulation, caused by poor absorption of vitamin K.
• The treatment of CD consists in the elimination of gluten from diet.
-Peptic ulcer:
Peptic ulcer disease is a common benign ulceration of the epithelial lining of the
stomach (gastric ulcer) or duodenum (duodenal ulcer).
Risk factors:
• Helicobacter pylori
• NSAIDs, corticosteroids Smoking, alcohol, diet and Stress.
Signs and symptoms: Patients with gastric ulcers often present with epigastric pain
radiating to the back. The pain is aggravated by food while Duodenal ulcer pain usually
occurs when the stomach is empty or when not enough of a meal remains in the stomach
to adequately buffer the acid stimulated by the meal.
Hadeel Gamal FD-ASU 3
Dental Management of Systemic Diseases Relevant to
Dentist
• Oral manifestations: persistent regurgitation of gastric acid as a result of pyloric
stenosis leads to dental erosion, typically of the palatal aspect of the maxillary
teeth.
-Gastroesophageal reflux disease:
Gastroesophageal reflux (GER) is considered a normal physiological event of the
human body. This natural process involves the regurgitation of gastric contents into the
esophagus, which is then removed and neutralized by several protecting factors (e.g.
esophageal peristalsis and saliva). In some individuals this reflux of gastric and
duodenal contents towards the esophagus generates a clinical picture called
gastroesophageal reflux disease (GERD), characterized by the occurrence of different
clinical signs and symptoms that are usually located in the esophagus (esophageal
syndrome).
GERD classical symptoms are heartburn and sour taste.
GERD is a global health problem with a high incidence and prevalence.
• Oral manifestations:
- Dental erosion: It usually affects the lingual or palatal surface of the
anterior teeth . The severity can be variable, with most cases showing only
a mild loss of enamel, while others can have a severe exposure of dentin.
- Xerostomia: It is likely that xerostomia appears as an adverse side effect
of the medication taken for treating GERD, rather than being cause by
GERD itself.
- Halitosis
- Mucositis: It might appear due the contact of the acids or its vapors with
the oral mucosa.
Hadeel Gamal FD-ASU 4
Dental Management of Systemic Diseases Relevant to
Dentist
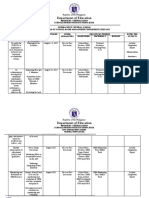
Oral manifestations of some gastrointestinal disorders:
Etiology Disease Oral manifestations Managment
Crohn´s - Mucosal tags Oral lesions
disease - Cobblestoning, are managed
Inflammatory I - Mucogingivitis, with topical
B - Labial and facial steroids, but
D swelling, the use of
- RAS like ulcerations systemic
- Angular cheilitis. agents might
Ulcerativ - Pyostomatitis vegetans. be necessary
e colitis - RAS like ulcerations for some
- Angular cheilitis, cases.
-Atrophic glossitis.
- Enamel hypoplasias,
- Delayed tooth eruption
Hypersensitivity Celiac - Bleeding tendency Elimination
disease caused by poor of gluten
absorption of vitamin K. from diet
- Signs and symptoms
secondary to the anemia
- Dark erythematous
tongue with yellowish
Infectious coating. Antacids
Peptic Ulcer - Dental erosion, typically
disease of the palatal aspect of
the maxillary teeth
- Dental erosions.
- Sour taste.
Others Gastroesoph - Halitosis. Antacids
ageal reflux - Mucositis.
disease - Burning mouth.
- RAS like ulcerations.
Hadeel Gamal FD-ASU 5
Dental Management of Systemic Diseases Relevant to
Dentist
Dental management:
1. Lengthy dental procedures should be avoided or spread out over shorter appointments
to minimize stress.
2. To avoid aspirations, patients should not be left in a supine position for lengthy
periods during dental appointments.
3. Dentists should avoid administering drugs that exacerbate ulceration and cause
gastrointestinal distress such as aspirin and other NSAIDs. Instead, acetaminophen
products should be recommended.
4. The prescription of systemic steroids should be avoided in patients with peptic ulcers
as this may lead to perforation leading to pain and blood loss.
5. Because many of the antacids contain calcium, magnesium, and aluminum salts that
bind antibiotics, such as erythromycin and tetracycline, dentists should remember that
administering one of these drugs within 1 hour of antacid therapy may decrease the
absorption of the antibiotic. Consequently, erythromycin and tetracycline should be
taken 1 hour before or 2 hours after ingestion of antacids.
6. Chronic use of glucocorticosteroids can also result in adrenal suppression. Patients
undergoing surgery may require supplemental glucocorticosteroids before and after the
procedure.
7. The following laboratory studies may be indicated before surgical procedures are
performed: complete blood count; hematocrit level; hemoglobin level; platelet count;
coagulation studies (prothrombin time/INR, and partial thromboplastin time); liver
function test; and blood glucose level.
Hadeel Gamal FD-ASU 6
Dental Management of Systemic Diseases Relevant to
Dentist
Kidney diseases
Patients with kidney disorders are increasingly encountered in dental practice due to
improvements in medical care leading to prolonged life expectancy. In order to
provide appropriate and safe dental care for these patients it is important to have a
working knowledge of renal disorders and related problems.
Functions of the kidneys:
I. Excretory II. Non-excretory
functions functions
1. Excretion of nitrogenous
end products of protein
metabolism (eg, creatinine, 1. Synthesis and activation of
uric acid, urea). hormones
- Erythropoietin (stimulates
erythrocyte production by bone
2. Maintenance of ECF
marrow)
volume and blood pressure - Renin (important in
by altering Na+ excretion. regulation of blood pressure)
- 1,25-Dihydroxyvitamin D3
(most potent form)
3. Maintenance of plasma
electrolyte concentration, - Prostaglandins (vasodilators)
osmolarity by altering water
excretion and pH by
eliminating excess H+ and
regenerating HCO3-.
2. Degradation of polypeptide
hormones (insulin, glucagon, growth
hormone, antidiuretic hormone,
4. Route
of excretion for gastrin, vasoactive intestinal
most drugs. polypeptides)
Hadeel Gamal FD-ASU 7
Dental Management of Systemic Diseases Relevant to
Dentist
Kidney diseases are as complicated as the organ itself. They can be divided into
developmental anomalies and inherited diseases or acquired diseases. With respect to
the further course of illness they can be divided into acute and chronic kidney diseases
Chronic renal disease (CRD), a progressive and irreversible decline in renal function
indicated by reduced glomerular filtration rate persisting more than three months.
In dental practice, the function of the kidneys can be assessed indirectly through
plasmatic creatinine (Cr). Normal values of serum Cr are 0.5- 1.4 mg/dl; in patients with
renal insufficiency, Cr will be of 1.5 mg/dl or more.
Sequelae of renal failure:
1. Building up of nitrogenous end product Ureamia
2. Loss of sodium pump Polyuria
3. Accumulation of acids, loss of buffer Acidosis
Oral manifestations:
1. Pallor due to anemia (caused by the inability to produce erythropoeitin as well as
accelerated destruction of RBCs due to fluid and electrolyte imbalance and loss of
blood in hemodialysis patients.)
2. Gingival bleeding due to uremic toxins decrease platelets adhesion, deficiency of
platelet factor 3, increased prostacyclin activity and increased capillary fragility.
3. Ammonia-like taste and smell (due to breakdown of urea in saliva to ammonia).
4. Uremic stomatitis, due to rise in BUN , which may appear as red mucosa covered
with a pseudomembrane.
5. Xerostomia, probably caused by direct involvement of the salivary glands.
6. White plaques called “uremic frost” results from residual urea crystals left on the
epithelial surfaces.
7. Signs of renal osteodystrophy in the mandible and maxilla caused by abnormal
calcium and phosphorous metabolism, abnormal vitamin D metabolism and
increased parathyroid activity
• bone demineralization,
• loss of trabeculation,
• ground-glass appearance,
• total or partial loss of lamina dura,
• giant cell lesions or brown tumors, and metastatic calcifications..
• Tooth mobility, malocclusion, and metastatic soft tissue calcifications.
8. Abnormal bone repair after extraction, termed “socket sclerosis”
Hadeel Gamal FD-ASU 8
Dental Management of Systemic Diseases Relevant to
Dentist
9. Enamel hypoplasia (a white or brownish discoloration) is frequently seen in
patients whose renal disease started at a young age.
Dental management:
1. Consultation with the patient’s physician.
2. Avoid dental treatment if the disease is poorly controlled.
3. Screen for bleeding disorders.
4. Monitor blood pressure.
5. Manage acute infections aggressively.
6. For patients receiving hemodialysis.
a. Elective dental treatment as well as extractions and other surgeries should
be done on the net day of dialysis (the blood is free of uremic toxins, and
the patient is far enough removed from dialysis to allow sufficient time
after surgery for clotting).
b. Apart from serving as a potential site for infection, the AV site should
never be jeopardized. The arm with the vascular access should be identified
and noted on the patient’s chart with instructions to avoid both
intramuscular and IV injection of medication into this arm.
7. The challenge for dentists in prescribing medications is to maintain a therapeutic
regimen within a narrow range, avoiding sub therapeutic dosing and toxicity.
Type of drug Best avoided Dose reduction No dose change
needed
1) Antimicrobial Tetracycline Metronidazole Erythromycin
Ampicillin Minocycline
Acyclovir
2) Analgesic Aspirin Paracetamol Codeine
GA if Hg< 10
3) Local anesthetic gm/dl Lidocaine
Hadeel Gamal FD-ASU 9
You might also like
- Oral Pathology Mnemonics Online Course - PDF versionFrom EverandOral Pathology Mnemonics Online Course - PDF versionRating: 3.5 out of 5 stars3.5/5 (3)
- PTE Essay FormatDocument9 pagesPTE Essay Formatramji013No ratings yet
- (PDF) Dwonload Dr. John Chung S New SAT Math: New SAT Math Designed To Get A Perfect Score Full OnlineDocument1 page(PDF) Dwonload Dr. John Chung S New SAT Math: New SAT Math Designed To Get A Perfect Score Full OnlineDoraNo ratings yet
- Live ProjectDocument53 pagesLive Projectritesh chauhanNo ratings yet
- Oral Manifestation of GIT DiseasesDocument33 pagesOral Manifestation of GIT DiseasesSura Abdel JabbarNo ratings yet
- Gitoralmanifestation 180812171655Document74 pagesGitoralmanifestation 180812171655hassonamonaNo ratings yet
- 08 Oral ManifestationDocument7 pages08 Oral ManifestationFachri MubarokNo ratings yet
- Oral Manifestations of Systemic DiseaseDocument10 pagesOral Manifestations of Systemic DiseasedrnainagargNo ratings yet
- Oral CutaneousDocument73 pagesOral CutaneouskurreanushaNo ratings yet
- Dental Management of Patients With Inflammatory Bowel DiseaseDocument17 pagesDental Management of Patients With Inflammatory Bowel DiseaseLeonid GroysmanNo ratings yet
- Mouth Ulcers and Diseases of The Oral Cavity: Key PointsDocument7 pagesMouth Ulcers and Diseases of The Oral Cavity: Key PointsAimen ZahidNo ratings yet
- 2008 2 D Aiuto Massi Benedetti enDocument4 pages2008 2 D Aiuto Massi Benedetti enMaría Jesús EspínolaNo ratings yet
- 17) Oral Manifestations of Systemic DiseasesDocument39 pages17) Oral Manifestations of Systemic Diseasesxj74fr4ddxNo ratings yet
- Diseases of Oral CavityDocument60 pagesDiseases of Oral Cavityfredrick damian80% (5)
- COPYDocument21 pagesCOPYrodrigo guiboneNo ratings yet
- Oral MedicineDocument174 pagesOral Medicineindah100% (1)
- Periodontitis As Manifestation On Systemic DiseasesDocument67 pagesPeriodontitis As Manifestation On Systemic DiseasesTristan Ingrid Del ValleNo ratings yet
- Oral Manifestations Gastrointestinal DisordersDocument42 pagesOral Manifestations Gastrointestinal DisordersakkamilaNo ratings yet
- Oral Manifestaions of Systemic DiseasesDocument116 pagesOral Manifestaions of Systemic DiseaseslikhithaNo ratings yet
- GingivitisDocument4 pagesGingivitisrichardananNo ratings yet
- Diseases of ParadontDocument71 pagesDiseases of ParadontIsak ShatikaNo ratings yet
- Periodont Al Disease-2: Harshit Bansal Bds 2 YearDocument43 pagesPeriodont Al Disease-2: Harshit Bansal Bds 2 YearharshitNo ratings yet
- Gingival Diseases in ChildrenDocument57 pagesGingival Diseases in ChildrenFourthMolar.com100% (3)
- Oral Medicine - Update For The Dental Practitioner: Red and Pigmented LesionsDocument7 pagesOral Medicine - Update For The Dental Practitioner: Red and Pigmented LesionsKaty LunaNo ratings yet
- The Gastrointestinal SystemDocument6 pagesThe Gastrointestinal SystemRex HuangNo ratings yet
- Oral Manifestations and Complications of Diabetes Mellitus: A ReviewDocument3 pagesOral Manifestations and Complications of Diabetes Mellitus: A ReviewKiftiyah RahmadhantiNo ratings yet
- Oral Medicine: (I. Penyakit Mulut)Document178 pagesOral Medicine: (I. Penyakit Mulut)claudiaciwiNo ratings yet
- Oral Ulcerative LesionsDocument34 pagesOral Ulcerative LesionsAhmed NajmNo ratings yet
- Ms Report NikolDocument31 pagesMs Report NikolMinbinNo ratings yet
- Periodontal Problems in ChildrenDocument21 pagesPeriodontal Problems in ChildrenEslam HafezNo ratings yet
- Diseases of The Oral Cavity and Stomatitis Ali Sadiek AssiutDocument17 pagesDiseases of The Oral Cavity and Stomatitis Ali Sadiek AssiutAli H. Sadiek أ.د. علي حسن صديق100% (4)
- Awareness of Oral Manifestations Related To Systemic DiseasesDocument5 pagesAwareness of Oral Manifestations Related To Systemic DiseasesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument63 pagesOral Medicine - Update For The Dental PractitionerPhuong MaiphuongNo ratings yet
- Oral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of SalivationDocument5 pagesOral Medicine - Update For The Dental Practitioner.: Dry Mouth and Disorders of SalivationGowriNo ratings yet
- Gingival Enlargement: Drg. Ade Ismail A. K.,MDSCDocument31 pagesGingival Enlargement: Drg. Ade Ismail A. K.,MDSCFina AkmaliaNo ratings yet
- Vpatho Module 1Document54 pagesVpatho Module 1Lib PalmaresNo ratings yet
- Ilovepdf MergedDocument157 pagesIlovepdf MergedSajjad AliNo ratings yet
- Mucogingival Deformities: Ni Made Ista PrestiyantiDocument55 pagesMucogingival Deformities: Ni Made Ista Prestiyantiista prestiyantiNo ratings yet
- Oral Medicine - Update For The Dental PractitionerDocument8 pagesOral Medicine - Update For The Dental PractitionernavyaNo ratings yet
- 4 Specific Non Dental Biofilm Induced Gingival and Periodontal Diseases PDFDocument49 pages4 Specific Non Dental Biofilm Induced Gingival and Periodontal Diseases PDFmarianaffernandes10No ratings yet
- StomatitisDocument17 pagesStomatitis4A - Hazel Ann G. EspinolNo ratings yet
- Acute Gingival InfectionsDocument31 pagesAcute Gingival InfectionsPathivada LumbiniNo ratings yet
- Pediatric Oral Manifestation of Sustemic DiseaseDocument43 pagesPediatric Oral Manifestation of Sustemic DiseaseMike SihombingNo ratings yet
- Lesi Dan Ulkus Dalam MulutDocument73 pagesLesi Dan Ulkus Dalam Mulutmega anggunNo ratings yet
- DermatologyDocument17 pagesDermatologysakrs4880No ratings yet
- Oral DisordersDocument24 pagesOral DisordersHayat AL AKOUMNo ratings yet
- Dental Management of Diabetic PatientDocument15 pagesDental Management of Diabetic Patientdr_jamal1983No ratings yet
- Oral Medicine: (I. Penyakit Mulut)Document165 pagesOral Medicine: (I. Penyakit Mulut)Susanna Arie KNo ratings yet
- Periodontal DiseaseDocument104 pagesPeriodontal DiseaseGaddafi HamzaNo ratings yet
- Gingivitis 160730200344Document27 pagesGingivitis 160730200344sri andewi inka pratiwiNo ratings yet
- 2 Diseases of Tongue Lips PDFDocument17 pages2 Diseases of Tongue Lips PDFmarianaffernandes10No ratings yet
- Jurnal Tentang GinjalDocument5 pagesJurnal Tentang GinjalnaveenNo ratings yet
- Salivary Gland ComplaintsDocument9 pagesSalivary Gland ComplaintsGowriNo ratings yet
- Public Health and Dentistry - AnithaDocument111 pagesPublic Health and Dentistry - AnithaK HMNo ratings yet
- Department of Periodontics and Oral Implantology: Kiliyamannil Campus, College Road Chattiparamb, MalappuramDocument21 pagesDepartment of Periodontics and Oral Implantology: Kiliyamannil Campus, College Road Chattiparamb, MalappuramFathima ShibiliNo ratings yet
- Prevention of Periodontal Disease HandoutDocument13 pagesPrevention of Periodontal Disease HandoutShady AnwarNo ratings yet
- Periodontal DiseasesDocument47 pagesPeriodontal DiseasesPratikNo ratings yet
- Article2 CitatDocument7 pagesArticle2 CitatMunteanu DragosNo ratings yet
- Oral DiseasesDocument4 pagesOral DiseasesAlphonse ElricNo ratings yet
- All About DentistryDocument50 pagesAll About DentistryMohammed TalibNo ratings yet
- Oral Medicine & Pathology from A-ZFrom EverandOral Medicine & Pathology from A-ZRating: 5 out of 5 stars5/5 (9)
- A Simple Guide to Bad Breath and Mouth DiseasesFrom EverandA Simple Guide to Bad Breath and Mouth DiseasesRating: 5 out of 5 stars5/5 (3)
- Rizals First Published Essay El Amor PatDocument23 pagesRizals First Published Essay El Amor PatNelly MesiasNo ratings yet
- CDP Virtual Appliance Getting Started GuideDocument18 pagesCDP Virtual Appliance Getting Started GuideJulio RodanesNo ratings yet
- Islam A Challenge To Religion by G. A. ParwezDocument359 pagesIslam A Challenge To Religion by G. A. ParwezJamshed IqbalNo ratings yet
- CAPtain Online ExplainedDocument13 pagesCAPtain Online ExplainedRebekaNo ratings yet
- Values and Ethics - Key Definitions NotesDocument20 pagesValues and Ethics - Key Definitions NotesDHANASEKAR K IV A 9023No ratings yet
- Dio125 and Hornet2 RepsolDocument2 pagesDio125 and Hornet2 RepsolSibi SundarNo ratings yet
- Chemistry Test 11 Chap 1-5Document2 pagesChemistry Test 11 Chap 1-5Sabitra RudraNo ratings yet
- Statement of PurposeDocument1 pageStatement of Purposeapi-397556034No ratings yet
- TQ UcspDocument11 pagesTQ UcspDeron C. De CastroNo ratings yet
- Reading 23 NovDocument5 pagesReading 23 NovAdhwa QurrotuainiNo ratings yet
- Sodium Sulfite: Product Safety SummaryDocument5 pagesSodium Sulfite: Product Safety SummaryMannar1No ratings yet
- Module 2Document40 pagesModule 2surya989030No ratings yet
- Jody Howard Director, Social Responsibility Caterpillar, IncDocument17 pagesJody Howard Director, Social Responsibility Caterpillar, IncJanak ValakiNo ratings yet
- Mastering Sketching S11 BLAD Print2Document8 pagesMastering Sketching S11 BLAD Print2Interweave0% (1)
- GuillermoAG - Reading The ImageDocument15 pagesGuillermoAG - Reading The ImageAdrienne Villanueva100% (1)
- CirclesDocument15 pagesCirclesJustine ReanNo ratings yet
- ECG-Based Biometric Schemes For Healthcare: A Systematic ReviewDocument23 pagesECG-Based Biometric Schemes For Healthcare: A Systematic ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Department of Education: Republic of The PhilippinesDocument3 pagesDepartment of Education: Republic of The PhilippinesRussel RapisoraNo ratings yet
- Bad For Democracy How The Presidency Undermines The Power of The PeopleDocument272 pagesBad For Democracy How The Presidency Undermines The Power of The PeoplePaulNo ratings yet
- New Microsoft Word DocumentDocument4 pagesNew Microsoft Word DocumentVinothan VasavanNo ratings yet
- "The Pedestrian" By: Rey BradburyDocument7 pages"The Pedestrian" By: Rey BradburyGabBragatNo ratings yet
- Cash Out With WhatsappDocument22 pagesCash Out With WhatsappIDRIS JAMIUNo ratings yet
- Plagiarism Check - Satya Dea PrawiraDocument3 pagesPlagiarism Check - Satya Dea PrawiraSatya Dea PrawiraNo ratings yet
- NIT 1 4 7040 Lecture 1 VLSI EC601Document26 pagesNIT 1 4 7040 Lecture 1 VLSI EC601SANDIP PODDARNo ratings yet
- Important People - Exercises 2 PDFDocument2 pagesImportant People - Exercises 2 PDFDiana BerariNo ratings yet
- BEE301Document4 pagesBEE301cshohil300No ratings yet
- Desjoyaux PoolsDocument25 pagesDesjoyaux Poolslina casadiegoNo ratings yet