Professional Documents
Culture Documents
Premature Physeal Closure Following Distal Tibia Physeal Fractures
Premature Physeal Closure Following Distal Tibia Physeal Fractures
Uploaded by
Deborah SalinasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Premature Physeal Closure Following Distal Tibia Physeal Fractures
Premature Physeal Closure Following Distal Tibia Physeal Fractures
Uploaded by
Deborah SalinasCopyright:
Available Formats
ORIGINAL ARTICLE
Premature Physeal Closure
Following Distal Tibia Physeal Fractures
A New Radiographic Predictor
Adam Barmada, MD, Tracey Gaynor, MA, and Scott J. Mubarak, MD
mature physeal closure (PPC) in distal tibia physeal fractures
Abstract: The incidence and predictors of premature physeal clo- has been reported as low as 2% to 5%.2,15 Factors proposed as
sure (PPC) after pediatric distal tibial fractures were investigated.
influencing rates of growth disturbances include fracture type
PPC was defined as evidence of growth plate disturbance on the in-
jured side compared with the uninjured side. Ninety-two fractures and location, displacement, energy of injury, quality of reduc-
were reviewed with at least 1 year of follow-up, or until physiologic tion, number of reduction attempts, and method of treat-
closure of the growth plates. Twenty-five fractures (27.2%) were ment.1,2,7–9,20,21 Salter-Harris (SH) type I and II fractures have
complicated by PPC, as confirmed by CT scan in most cases. Salter- been considered low-risk injuries.20,23 The importance of ana-
Harris III and IV (medial malleolar type) fractures resulted in the tomic reduction to decrease the potential of future growth dis-
highest percentage of PPC by fracture type (38%). Salter-Harris I and turbances has been debated.7,16,21 Several authors have sug-
II fractures resulted in PPC in 36% of cases, followed by triplane gested that growth disturbances in distal tibia SH II fractures
fractures (21%) and Tillaux fractures (0%). Initial displacement,
may be more common than previously realized.9,21 Interposi-
number of reduction attempts, or treatment method did not signifi-
tion of periosteum and other soft tissues is occasionally re-
cantly affect the incidence of PPC. More anatomic reductions resulted
in a statistically significant decrease in PPC rates. Residual physeal sponsible for creating a block to reduction in these injuries.8,23
gap (>3 mm) following reduction was determined from radiographs Researchers have found that periosteum folded into a physeal
in Salter-Harris I and II fractures. If a residual gap was seen on the defect in sheep results in physeal growth arrest.24 Others dis-
radiograph, the incidence of PPC increased to 60%; if no gap was covered that periosteum after fractures could form bone, car-
present, the incidence decreased to 17%. Open reduction was per- tilage, or fibrous tissue, cause resorption of bone, and lead to
formed in five Salter-Harris II fractures that had a residual gap. Peri- increased rates of growth plate disturbances in rat models.5,18
osteum was entrapped in the physis in all of these cases. Residual gaps This theory has not been demonstrated in humans.
in the physis following closed reduction may represent entrapped Medial malleolar (SH III and IV) fractures have resulted
periosteum in Salter-Harris I and II fractures. This can lead to a higher in higher complication rates. Consequently, anatomic reduc-
incidence of PPC, suggesting that open reduction and removal of the
tion is recommended for preservation of the physis and the
entrapped periosteum may be beneficial.
articular surface.1,8,9,20,21,23 Triplane (SH IV) and Tillaux (SH
Key Words: distal tibia fracture, physeal closure, growth plate, peri- III) fractures occur closer to skeletal maturity, and PPC has not
osteum, pediatric ankle been considered a problem. Anatomic reduction in these inju-
(J Pediatr Orthop 2003;23:733–739) ries is recommended for articular surface congruity.
P hyseal fractures of the distal tibia represent a significant
percentage of long bone physeal injuries, second only to
distal radius physeal fractures.11,12,16,23 The incidence of pre-
MATERIALS AND METHODS
The records of 92 patients treated for distal tibia physeal
fractures at San Diego Children’s Hospital between 1991 and
2000 were reviewed. All were treated by one of six pediatric
Study conducted at Children’s Hospital and Health Center, San Diego, Cali-
fornia. orthopaedic surgeons. We recorded gender, age, and mecha-
From Portland Bone & Joint Center, LLC, Portland, Oregon (Dr Barmada) and nism of injury. Initial injury radiographs were categorized ac-
Children’s Hospital and Health Center, San Diego, California (Ms Gaynor, cording to a modification of the SH classification (Fig. 1). Ini-
Dr Mubarak). tial fracture displacement was recorded in millimeters, mea-
Supported by the Children’s Hospital-San Diego Orthopedic Research and
suring the largest displacement between the epiphysis and
Education Fund.
Reprints: Scott J. Mubarak, MD, 3030 Children’s Way, Suite 410, San Diego, metaphysis on the AP or lateral radiograph. The categories of
CA 92123 (e-mail: pedsortho@chsd.org). treatment were closed reduction and casting, closed reduction
Copyright © 2003 by Lippincott Williams & Wilkins. and percutaneous pinning (CRPP), and open reduction internal
J Pediatr Orthop • Volume 23, Number 6, November/December 2003 733
Barmada et al J Pediatr Orthop • Volume 23, Number 6, November/December 2003
FIGURE 1. Modified SH fracture classification. A: SH II (AP/lateral views). B: Medial malleolar fractures: SH III (left) and SH IV (right).
C: Triplane (SH IV). D: Tillaux (SH III).
fixation (ORIF). Closed treatment was commonly performed (5.4%), baseball (4.3%), and indeterminate cause (17.3%).
under conscious sedation in the emergency department. Pa- Follow-up averaged 12 months (range 1–66 months). The
tients were instructed to be non-weight-bearing and were overall PPC rate across all fracture types was 27.2% (including
placed in a long-leg cast for 4 weeks, followed by short-leg Tillaux fractures). PPC was diagnosed at a mean of 7 months
casting and weight-bearing as tolerated for another 2 to 3 after injury (range 2–12 months). Sixteen of the 25 patients
weeks. If open reduction was performed, any interposed peri- (64%) with PPC underwent a subsequent operation for short-
osteum was noted. Fixation was obtained with percutaneous ening, angular deformity, or a high potential for either because
pins across the physis or screws parallel to the physis. Pins of remaining growth. Two of the four triplane injuries in which
were typically smooth 0.062 Kirschner wires that were re- PPC developed underwent tibia and fibula epiphysiodesis on
moved after 4 weeks. The number of reduction attempts was the injured side only.
recorded.
Postreduction radiographs were measured for residual
displacement in millimeters using the method described Fracture Types
above. Residual physeal gap was recorded for SH I and II frac- We identified eight (8.5%) medial malleolar (SH III and
tures. Gap was identified as positive if the physis was widened IV) injuries, with an average age of 12.6 years. Six of the in-
more than 3 mm on a standard AP or lateral radiograph (Fig. 2). juries underwent ORIF. PPC occurred in three (38%). This in-
Patients were followed for 1 year or until physiologic closure crease in PPC rate was significant (P = 0.04) compared with
of the physis. Ankle radiographs, including contralateral films, other fracture types. Nineteen triplane fractures (21%) were
were evaluated for physeal closure and CT scans were ob- identified, 15 of which were treated with ORIF. Average age
tained in most cases to further delineate size and location of was 14.0 years. PPC occurred in four (21%). Fourteen Tillaux
any physeal bar. Any evidence of shortening or angular defor- fractures were identified, 11 of which were treated with ORIF.
mity was recorded. Subsequent operations performed second- Average age was 14.8 years. PPC was not evident in any case.
ary to PPC, usually bar excision or epiphysiodesis, were docu- Associated fibula fractures were present in 44 (47.8%) cases.
mented. Fixation of the fibula, with Kirschner wires or screw, was per-
Statistical analysis was performed by dividing patients formed in 11% of these cases. One case of fibula PPC was
into PPC or non-physeal closure groups. 2 analysis and documented (2.3% PPC rate).
ANOVA were used for each variable as appropriate. The 45 SH II fractures accounted for the majority of in-
juries (48.9%). Six (6.5%) SH I injuries were identified, with
RESULTS four resulting in PPC. Since the fracture type, patient age, and
Ninety-two fractures were included (61 boys, 31 girls). mechanism of these injuries were similar, these two fracture
Forty-six of the fractures were left-sided and 46 were right- types were combined. Radiographs were available for 44 of the
sided. The most common cause of injury was nonspecific fall 51 SH I and II fractures. Treatment consisted of ORIF for 9,
(25%), followed by skateboard accidents (16.3%), motor ve- CRPP for 9, and closed treatment for 26. Average age in this
hicle accidents (12%), football (12%), soccer (7.6%), biking group was 12.1 years. PPC occurred in 36% (Fig. 3).
734 © 2003 Lippincott Williams & Wilkins
J Pediatr Orthop • Volume 23, Number 6, November/December 2003 Premature Physeal Closure After Tibial Fracture
FIGURE 2. Radiographs of SH II distal tibia fracture before (A) and after (B) closed reduction. Note the residual physeal gap after
reduction.
SH I/II Injuries were retrospectively found to have a residual gap prior to sur-
Fractures that were positive for PPC had an average ini- gery. All five had interposed periosteum removed from the
tial displacement of 7.5 mm versus 7.9 mm for the group with- physis at the time of surgery (Fig. 4). None of these five pa-
out PPC (P = 0.86). The incidence of PPC with initial displace- tients went on to develop PPC.
ment of at least 5 mm (31%) was not significantly different
from the incidence of PPC with initial displacement less than 5 DISCUSSION
mm (42%) (P = 0.51) The number of reduction attempts Previous reports have found low complication rates with
ranged from zero to four. There was no difference in incidence SH I and II fractures. Pacicca et al showed one “physeal dis-
of PPC based on the number of reduction attempts (P = 0.54). turbance” in 38 SH I and II fractures.15 Their overall incidence
Of the 16 cases complicated by PPC, 69% were treated by of physeal disturbance was 5%, much lower than ours. This
closed methods, 19% were treated by CRPP, and 12% were could be due to shorter follow-up, as fractures were “followed
treated by ORIF. This difference did not reach significance (P to union.” In our series fractures were followed for 1 year on
= 0.55). The average residual displacement after treatment of average, as many have recommended.1,8,21 Pacicca et al found
the positive PPC group was significantly greater (3.1 mm) than that the quality of reduction did not appear to correlate with
the group without PPC (1.4 mm) (P < 0.001). The incidence of physeal disturbance, contrary to our findings.
PPC in patients with a residual displacement of at least 2 mm Spiegel et al grouped 184 fractures into low-risk, high-
was 73% (11/15 patients), whereas the incidence of PPC in risk, and unpredictable categories based on the rate of compli-
patients with a residual displacement of less than 2 mm was cations, which included PPC, shortening, joint incongruity,
18% (5/28 patients) (P = 0.001). and angular deformity.21 The overall complication rate was
Twenty of the fractures were positive for gap. All gaps 14.1%. It is difficult to know whether shortening or angular
were found anteriorly or medially. The presence of a gap was deformity was a result of PPC in most of their cases. Low-risk
associated with a 60% PPC rate; if no gap was found, the PPC injuries included all fibula fractures, SH I distal tibia fractures,
rate was 17% (P = 0.003). This represents a 3.5-fold increased and SH III and IV fractures with less than 2 mm of displace-
risk. Nine patients were treated with open reduction after failed ment. High-risk injuries included SH III and IV fractures with
closed reduction. The reason was inadequate reduction in six 2 mm or more of displacement and triplane and Tillaux frac-
patients and evidence of extensor retinaculum syndrome (as tures. The unpredictable group included only SH II fractures.
described by Mubarak14) in three patients. Five of the nine They concluded that prognosis was related to the quality of
© 2003 Lippincott Williams & Wilkins 735
Barmada et al J Pediatr Orthop • Volume 23, Number 6, November/December 2003
FIGURE 3. Flow chart for SH I and II fractures. Gap is defined as a physis widened ⱖ3 mm on postreduction AP or lateral
radiographs. *The operative report for this patient made no mention of entrapped periosteum or other tissue. †This patient was
treated for compartment syndrome and later developed osteomyelitis.
reduction, consistent with our findings. According to our data, Historically, triplane and Tillaux fractures have been
the presence of a residual physeal gap in these injuries may treated based on displacement at the articular surface. Due to
predict a higher rate of PPC (Fig. 5). We did not find SH I limited growth remaining, PPC has not been considered a sig-
fractures to be low-risk injuries, although our number of cases nificant problem. We found a PPC rate of 21% in triplane in-
in this category was small (n = 6). This low incidence could be
related to the difficulty in diagnosing minimally or nondis-
placed SH I injuries.
Kling et al reviewed 65 distal tibia physeal fractures.9
The incidence of PPC could not be determined because half of
these fractures were referred for growth plate closures. They
concluded that medial malleolar (SH III and IV) fractures, and
“perhaps type II” fractures, commonly result in growth distur-
bances. They suggested that anatomic reduction of the physis
by open or closed methods decreases the incidence of these
growth disturbances. We agree, and also found SH III and IV
medial malleolar fractures to result in the highest incidence of
growth problems.
Cass et al found that 9 of 18 medial malleolar (SH IV)
fractures resulted in partial growth arrest.1 They stressed the
importance of distinguishing SH IV injuries from SH III inju-
ries by obtaining oblique radiographs. They noted the diffi-
culty of identifying the small metaphyseal fragment in many
SH IV medial malleolar injuries. SH III and IV medial malleo-
lar fractures were categorized in the same group because of FIGURE 4. Periosteum interposed in the physis with subse-
their similarity and are treated similarly at our institution. quent residual gap.
736 © 2003 Lippincott Williams & Wilkins
J Pediatr Orthop • Volume 23, Number 6, November/December 2003 Premature Physeal Closure After Tibial Fracture
FIGURE 5. Ankle fracture in a 12-year-old boy. A: Initial injury PA radiograph showing SH II fracture of the distal tibia. B: Initial
injury lateral radiograph. C: After closed reduction and casting; note the residual gap seen medially on the AP radiograph. D: The
residual gap is also seen anteriorly on the lateral radiograph. E: Nine months after injury, the AP radiograph shows partial PPC
centrally. F: The closure is also noted centrally on the lateral radiograph. Due to older bone age and limited remaining growth
potential, subsequent surgery was not necessary.
juries, half of which received a subsequent operation. At in- for growth plate disturbances. Tillaux fractures never resulted
jury, the average age of boys was 14.6 years; that of girls was in PPC and can be followed to union. At injury, the average age
12.7 years. We recommend careful follow-up of these injuries of boys was 15.5 years; that of girls was 13.1 years. Our op-
© 2003 Lippincott Williams & Wilkins 737
Barmada et al J Pediatr Orthop • Volume 23, Number 6, November/December 2003
erative indication is consistent with most authors: more than 2 tion and significant growth disturbances compared with frac-
mm of displacement at the articular surface.3,8,19,22 tures with intact physes.4,18 We believe that the residual phy-
Some have suggested that PPC results from the trauma to seal gap seen after reduction attempts in SH I and II fractures
the physis at the time of injury.2 The presence of larger initial represents interposed periosteum in most cases. Phan et al sug-
displacement or physeal crush (SH V) injury may lead one to gested that physeal widening may indicate the presence of ro-
infer a higher-energy injury, more significant injury to sur- tational deformity.17 However, they noted a poor correlation
rounding tissues and blood supply, and therefore a higher PPC between physeal widening and rotational deformity at follow-
rate. We did not identify any SH V injuries and were not able to up. Kling et al stated, “any residual gap between the fractured
support this hypothesis. physeal edges may result in a partial growth arrest.”9 Our re-
Repeated reduction attempts are contraindicated secondary sults showed a 3.5-fold increase in the PPC rate if a gap was
to additional physeal damage. We did not find a relationship be- present on the postreduction film in SH I and II fractures. Open
tween the number of reduction attempts and PPC rates. However, reduction and removal of interposed periosteum may decrease
we recognize the difficulty of defining and documenting each “re- the incidence of PPC (Fig. 6).
duction attempt” with a retrospective review. We limit the num- The overall incidence of PPC following distal tibia phy-
ber of closed reduction attempts to two prior to open reduction. seal fractures in this series was 32%. This excludes Tillaux
Studies in animal models have shown that periosteum fractures, which never resulted in PPC and should be treated
interposed into fractured physes results in physeal bar forma- based on articular incongruity. Over half (64%) of patients
FIGURE 6. Another ankle fracture in a 12-year-old boy. A: Initial injury PA radiograph showing a SH II distal tibia fracture with
associated fibula fracture. B: Initial injury lateral radiograph. C: After closed reduction and casting; note the residual gap seen
medially on the AP radiograph. D: The gap is also noted anteriorly on the lateral radiograph. E: AP radiograph after open
reduction, removal of interposed periosteum, and pin fixation. F: Lateral radiograph after open reduction and fixation; no gap is
seen. G: Twelve months after injury, the physis remains open on the AP radiograph. H: The lateral radiograph also shows a normal
physis.
738 © 2003 Lippincott Williams & Wilkins
J Pediatr Orthop • Volume 23, Number 6, November/December 2003 Premature Physeal Closure After Tibial Fracture
with PPC received a subsequent operation for shortening, an- due to growth disturbances after ankle fractures in children. J Bone Joint
Surg [Am]. 1984;66:1198–1210.
gular deformity, or a high potential for either. The presence of 7. Karrholm J, Hansson LI, Svensson K. Prediction of growth pattern after
PPC does not always lead to measurable growth disturbance. ankle fractures in children. J Pediatr Orthop. 1983;3:319–325.
Approximately 3 to 4 mm a year is gained from the distal tibia 8. Kay RM, Matthys GA. Pediatric ankle fractures: evaluation and treat-
ment. J Am Acad Orthop Surg. 2001;9:268–278.
physis.7 The importance of maintaining the distal tibia and 9. Kling TF Jr, Bright RW, Hensinger RN. Distal tibial physeal fractures in
fibula relationship for ankle alignment has been acknowl- children that may require open reduction. J Bone Joint Surg [Am]. 1984;
edged.6,10,13,20 The decision to intervene surgically includes 66:647–657.
10. Langenskiold A. Traumatic premature closure of the distal tibial epiphy-
these factors and the patient’s remaining growth. seal plate. Acta Orthop Scand. 1967;38:520–531.
We conclude that PPC after distal tibia physeal fractures 11. Mann DC, Rajmaira S. Distribution of physeal and nonphyseal fractures
is more common than previously reported. Patients should be in 2,650 long-bone fractures in children aged 0-16 years. J Pediatr Or-
thop. 1990;10:713–716.
followed for at least 1 year or until physiologic physeal clo- 12. Mizuta T, Benson WM, Foster BK, et al. Statistical analysis of the inci-
sure. Anatomic reduction of the physis appears to decrease the dence of physeal injuries. J Pediatr Orthop. 1987;7:518–523.
incidence of PPC. The radiographic presence of postreduction 13. Moon MS, Kim I, Rhee SK, et al. Varus and internal rotational deformity
of the ankle secondary to distal tibial physeal injury. Bull Hosp Jt Dis.
residual displacement and/or a physeal gap in SH I and II frac- 1997;56:145–148.
ture types is associated with a greater than three-fold increase 14. Mubarak SJ. Extensor retinaculum syndrome of the ankle after injury to
in the incidence of PPC. Open reduction and removal of any the distal tibial physis. J Bone Joint Surg [Br]. 2002;94:11–14.
15. Pacicca DM PA. Cramer K, Tornetta III P. Is anatomic reduction neces-
interposed soft tissue in these cases allows for a more anatomic sary for displaced physeal fractures of the tibia? Presented at American
reduction and may decrease the incidence of PPC. Academy of Orthopedic Surgeons Annual Meeting, San Francisco, 2001.
16. Peterson CA, Peterson HA. Analysis of the incidence of injuries to the
epiphyseal growth plate. J Trauma. 1972;12:275–281.
ACKNOWLEDGMENT 17. Phan VC, Wroten E, Yngve DA. Foot progression angle after distal tibial
The authors thank J. D. Bomar for his assistance with the physeal fractures. J Pediatr Orthop. 2002;22:31–35.
18. Phieffer LS, Meyer RA Jr, Gruber HE, et al. Effect of interposed perios-
preparation of this manuscript. teum in an animal physeal fracture model. Clin Orthop. 2000;(376):
15–25.
REFERENCES 19. Rapariz JM, Ocete G, Gonzalez-Herranz P, et al. Distal tibial triplane
fractures: long-term follow-up. J Pediatr Orthop. 1996;16:113–118.
1. Cass JR, Peterson HA. Salter-Harris type IV injuries of the distal tibial 20. Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone
epiphyseal growth plate, with emphasis on those involving the medial Joint Surg [Am]. 1963;45:587–622.
malleolus. J Bone Joint Surg [Am]. 1983;65:1059–1070. 21. Spiegel PG, Cooperman DR, Laros GS. Epiphyseal fractures of the distal
2. Dugan G, Herndon WA, McGuire R. Distal tibial physeal injuries in chil- ends of the tibia and fibula. A retrospective study of two hundred and
dren: a different treatment concept. J Orthop Trauma. 1987;1:63–67. thirty-seven cases in children. J Bone Joint Surg [Am]. 1978;60:1046–
3. Ertl JP, Barrack RL, Alexander AH, et al. Triplane fracture of the distal 1050.
tibial epiphysis. Long-term follow-up. J Bone Joint Surg [Am]. 1988;70: 22. Spiegel PG, Mast JW, Cooperman DR, et al. Triplane fractures of the
967–976. distal tibial epiphysis. Clin Orthop. 1984;(188):74–89.
4. Gruber HE, Phieffer LS, Wattenbarger JM. Physeal fractures, Part II: Fate 23. Weber BG, Sussenbach F. Malleolar fractures. In Weber BG, Brunner C,
of interposed periosteum in a physeal fracture. J Pediatr Orthop. 2002; Freuler F, eds. Treatment of fractures in children and adolescents. New
22:710–716. York: Springer-Verlag, 1980:350–372.
5. Jarry L, Uhthoff HK. Pluripotency of periosteum and endosteum in frac- 24. Wirth T, Byers S, Byard RW, et al. The implantation of cartilaginous
ture healing. J Bone Joint Surg [Br]. 1969;51:387. and periosteal tissue into growth plate defects. Int Orthop. 1994;18:220–
6. Karrholm J, Hansson LI, Selvik G. Changes in tibiofibular relationships 228.
© 2003 Lippincott Williams & Wilkins 739
You might also like
- Salter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDocument6 pagesSalter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDeborah SalinasNo ratings yet
- ODONTOIDESDocument11 pagesODONTOIDESElianaNo ratings yet
- Outcome of Distal Tibial Physeal InjuriesDocument7 pagesOutcome of Distal Tibial Physeal InjuriesDeborah SalinasNo ratings yet
- Intramedullary Nailing of Distal Metaphyseal.5Document9 pagesIntramedullary Nailing of Distal Metaphyseal.5Joël Clarck EkowongNo ratings yet
- Weinraub2017 PDFDocument5 pagesWeinraub2017 PDFAkmal PutraNo ratings yet
- A Study On Management of Bothbones Forearm Fractures With Dynamic Compression PlateDocument5 pagesA Study On Management of Bothbones Forearm Fractures With Dynamic Compression PlateIOSRjournalNo ratings yet
- DL TPSFDocument5 pagesDL TPSFPramod N KNo ratings yet
- Pennock Et Al - 2014Document7 pagesPennock Et Al - 2014Tuğçe KabakcıNo ratings yet
- Ankle Fracture Fixation - Medial or Lateral First?Document5 pagesAnkle Fracture Fixation - Medial or Lateral First?Diana Marcela Benítez HernándezNo ratings yet
- Salter - Harris 2 Displaced Fractuers Best TreatmentDocument5 pagesSalter - Harris 2 Displaced Fractuers Best TreatmentDeborah SalinasNo ratings yet
- Clavicle Fracture Following Neck Dissection: Imaging Features and Natural CourseDocument6 pagesClavicle Fracture Following Neck Dissection: Imaging Features and Natural CourseAngel IschiaNo ratings yet
- FishtailDocument6 pagesFishtailsmbodeanuNo ratings yet
- Fijcmr 650 May 31 2Document3 pagesFijcmr 650 May 31 2khusnulNo ratings yet
- Tibial Tubercle Fractures in Pediatric PatientsDocument7 pagesTibial Tubercle Fractures in Pediatric PatientsNEUROLIVROS NEUROLIVROSNo ratings yet
- Effects On Inadvertent Endplate Fracture Following Lateral Cage Placement On Range of Motion and Indirect Spine Decompression in Lumbar Spine Fusion Constructs: A Cadaveric StudyDocument8 pagesEffects On Inadvertent Endplate Fracture Following Lateral Cage Placement On Range of Motion and Indirect Spine Decompression in Lumbar Spine Fusion Constructs: A Cadaveric Studysiti hanifahNo ratings yet
- Prabhakar 2020Document9 pagesPrabhakar 2020Lucas LozaNo ratings yet
- Marecek2016 PDFDocument4 pagesMarecek2016 PDFCande BenitoNo ratings yet
- Periprosthetic Femoral Fractures Above Total Knee ReplacementsDocument10 pagesPeriprosthetic Femoral Fractures Above Total Knee ReplacementsSpelliardNo ratings yet
- Acta 88 118Document11 pagesActa 88 118darshan tatiaNo ratings yet
- Odontoid Fractures: Update On Management: Review ArticleDocument12 pagesOdontoid Fractures: Update On Management: Review ArticleItha KiloonaNo ratings yet
- Augmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudyDocument7 pagesAugmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudytomimacagnoNo ratings yet
- Plantillo Anteromedial + LCP + ApeDocument7 pagesPlantillo Anteromedial + LCP + ApeThiagoNo ratings yet
- Dynamic HIP Screw Vs Proximal Trochanteric Contoured Plate in Proximal End Fractures of FemurDocument8 pagesDynamic HIP Screw Vs Proximal Trochanteric Contoured Plate in Proximal End Fractures of FemurKrishna CaitanyaNo ratings yet
- Chang 2017. Skeletal RadiologyDocument7 pagesChang 2017. Skeletal RadiologyteresaNo ratings yet
- Seguridad Del PacienteDocument14 pagesSeguridad Del PacienteTamara PricilaNo ratings yet
- Medip, IJORO-2331 ODocument7 pagesMedip, IJORO-2331 Oprashant makadiaNo ratings yet
- Nuevas Indicaciones en ManguitoDocument10 pagesNuevas Indicaciones en ManguitoJose Antonio Pareja-EstebanNo ratings yet
- Reisoğlu 2017Document5 pagesReisoğlu 2017Tuğçe KabakcıNo ratings yet
- PRP An Mandibular FractureDocument6 pagesPRP An Mandibular Fracture6hd6mnrzw2No ratings yet
- PDR Rsik Factors For RedisplacementDocument6 pagesPDR Rsik Factors For RedisplacementCleff FlowersNo ratings yet
- Banaszek2018 PDFDocument10 pagesBanaszek2018 PDFGanesh VadiveluNo ratings yet
- FxClavícula PDFDocument7 pagesFxClavícula PDFPenélope CrespoNo ratings yet
- Distal Radius Fractures 2009Document10 pagesDistal Radius Fractures 2009Un SerNo ratings yet
- Chloros2008 231022 130529Document12 pagesChloros2008 231022 130529Cristian SanchezNo ratings yet
- Clinical Outcomes of Locked Plating of Distal Femoral Fractures in A Retrospective CohortDocument9 pagesClinical Outcomes of Locked Plating of Distal Femoral Fractures in A Retrospective Cohortisnida shela arloviNo ratings yet
- PHF MortalityDocument5 pagesPHF Mortalitydanirotman4384No ratings yet
- Andrade Et Al-2009-Clinical Anatomy PDFDocument7 pagesAndrade Et Al-2009-Clinical Anatomy PDFJakeCrNo ratings yet
- Treatment and Outcome of Diatl Tibia Saletr Harris II FracturesDocument6 pagesTreatment and Outcome of Diatl Tibia Saletr Harris II FracturesDeborah SalinasNo ratings yet
- malham2015Cage沉降分级 非通用Document9 pagesmalham2015Cage沉降分级 非通用kai liuNo ratings yet
- The Journal of Foot & Ankle SurgeryDocument5 pagesThe Journal of Foot & Ankle SurgeryGilbert Tormis DaguploNo ratings yet
- Protrusio Acetabuli PDFDocument10 pagesProtrusio Acetabuli PDFSoemantri DoankNo ratings yet
- Definingnoptimal Calcar Screw Positioning in Proximal Humerus Fracture FixationDocument7 pagesDefiningnoptimal Calcar Screw Positioning in Proximal Humerus Fracture FixationAJ CésarNo ratings yet
- OTA Highlight Paper Predicting Future Displacement of Nonoperatively Managed Lateral Compression Sacral Fractures - Can It Be DoneDocument6 pagesOTA Highlight Paper Predicting Future Displacement of Nonoperatively Managed Lateral Compression Sacral Fractures - Can It Be Doneakb601No ratings yet
- Tompkins, JPOSNA ARTICLE 172 - FINAL UPDATEDDocument13 pagesTompkins, JPOSNA ARTICLE 172 - FINAL UPDATEDTania RahamanNo ratings yet
- Clinical Implications of Impingement of The Anterior Femoral Cortex After Cephalomedullary NailingDocument7 pagesClinical Implications of Impingement of The Anterior Femoral Cortex After Cephalomedullary NailingKristianesgaNo ratings yet
- HIP ORTHOPEDICS October 2008Document4 pagesHIP ORTHOPEDICS October 2008kennice_nereaNo ratings yet
- Pennockaheyworthbe FACTSsettling Jses21Document9 pagesPennockaheyworthbe FACTSsettling Jses21euandianaeuanNo ratings yet
- Outcomes of Surgical Management of Floating Knee Injuries: Original ResearchDocument4 pagesOutcomes of Surgical Management of Floating Knee Injuries: Original ResearchManiDeep ReddyNo ratings yet
- Intramedullary Nailing of Subtrochanteric Fractures: Does Malreduction Matter?Document5 pagesIntramedullary Nailing of Subtrochanteric Fractures: Does Malreduction Matter?Reza ParkerNo ratings yet
- Acute Dislocation of The PatellaDocument17 pagesAcute Dislocation of The PatellaChEko SpaguettyNo ratings yet
- Phillips 2013Document6 pagesPhillips 2013thanawatsimaNo ratings yet
- Outcome of Distal Tibia Physeal FracturesDocument5 pagesOutcome of Distal Tibia Physeal FracturesDeborah SalinasNo ratings yet
- Core Decompression With Bone Grafting For Osteonecrosis of The Femoral HeadDocument8 pagesCore Decompression With Bone Grafting For Osteonecrosis of The Femoral Headmuhammad0umar-4No ratings yet
- Fai 2011 0818Document4 pagesFai 2011 0818Mohamed GoudaNo ratings yet
- JBJS 18 01178Document6 pagesJBJS 18 01178ภควัต วังทะพันธ์No ratings yet
- Percutaneous Screw Fixation of Crescent Fracture Dislocation of The Sacroiliac JointDocument7 pagesPercutaneous Screw Fixation of Crescent Fracture Dislocation of The Sacroiliac Jointgevowo3277No ratings yet
- MainDocument9 pagesMainMuhammad Tabish SaleemNo ratings yet
- FxbifosfonatoDocument23 pagesFxbifosfonatoAbi HinojosaNo ratings yet
- Tips and Tricks for Problem Fractures, Volume I: The Upper ExtremityFrom EverandTips and Tricks for Problem Fractures, Volume I: The Upper ExtremityDaniel S. HorwitzNo ratings yet
- Outcome of Distal Tibia Physeal FracturesDocument5 pagesOutcome of Distal Tibia Physeal FracturesDeborah SalinasNo ratings yet
- Salter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDocument6 pagesSalter Harris II Fractures of The Distal Tibia Does Surgical Management Reduce The Risk of Premature Physeal ClosureDeborah SalinasNo ratings yet
- Outcome of Distal Tibial Physeal InjuriesDocument7 pagesOutcome of Distal Tibial Physeal InjuriesDeborah SalinasNo ratings yet
- Open Reduction and Internal Fixation For Displaced Salter Harris 2Document7 pagesOpen Reduction and Internal Fixation For Displaced Salter Harris 2Deborah SalinasNo ratings yet
- Smith 2011Document6 pagesSmith 2011Deborah SalinasNo ratings yet
- Pone 0257038Document9 pagesPone 0257038Deborah SalinasNo ratings yet
- 10 1016@j Jhsa 2019 03 014Document6 pages10 1016@j Jhsa 2019 03 014Deborah SalinasNo ratings yet
- Wound Healing Complications in Diabetic Patients UDocument7 pagesWound Healing Complications in Diabetic Patients UDeborah SalinasNo ratings yet
- Pi Is 0363502317301211Document8 pagesPi Is 0363502317301211Deborah SalinasNo ratings yet
- S0749806321003303Document20 pagesS0749806321003303Deborah SalinasNo ratings yet
- Fsurg 08 662720Document6 pagesFsurg 08 662720Deborah SalinasNo ratings yet
- Helical 6-Strand Cruciate Tenorrhaphy: Description of A New Technique and Biomechanical Comparative Analysis With 2 Standard TechniquesDocument8 pagesHelical 6-Strand Cruciate Tenorrhaphy: Description of A New Technique and Biomechanical Comparative Analysis With 2 Standard TechniquesDeborah SalinasNo ratings yet
- 10 1016@j Jhsa 2020 08 001Document8 pages10 1016@j Jhsa 2020 08 001Deborah SalinasNo ratings yet
- The Biomechanical Effects of Simulated RadioscaphoDocument8 pagesThe Biomechanical Effects of Simulated RadioscaphoDeborah SalinasNo ratings yet
- 10.1007@s40520 015 0497 yDocument8 pages10.1007@s40520 015 0497 yDeborah SalinasNo ratings yet
- 10 1016@j Jhsa 2018 11 012Document5 pages10 1016@j Jhsa 2018 11 012Deborah SalinasNo ratings yet
- HandbookNeurorehabilitation UnknownDocument195 pagesHandbookNeurorehabilitation UnknownDeborah SalinasNo ratings yet
- 10 1016@j Cps 2019 03 008Document10 pages10 1016@j Cps 2019 03 008Deborah SalinasNo ratings yet
- 10 1016@j Cps 2019 02 006Document9 pages10 1016@j Cps 2019 02 006Deborah SalinasNo ratings yet
- Chappell 2020Document9 pagesChappell 2020Deborah SalinasNo ratings yet
- Adaptacion Emocional de La Perdida de Una ExtremidadDocument22 pagesAdaptacion Emocional de La Perdida de Una ExtremidadDeborah SalinasNo ratings yet
- Rehabilitation AmbulationDocument14 pagesRehabilitation AmbulationDeborah SalinasNo ratings yet
- Ambulation Spin Cord InjuryDocument16 pagesAmbulation Spin Cord InjuryDeborah SalinasNo ratings yet
- Imporving Orientation in Head Injued Adults by Repeat Parctice Multisensory Input and Peer ParticipátionDocument10 pagesImporving Orientation in Head Injued Adults by Repeat Parctice Multisensory Input and Peer ParticipátionDeborah SalinasNo ratings yet
- Assistive Devices For AmbulationDocument13 pagesAssistive Devices For AmbulationDeborah Salinas100% (1)
- Gaitan 1 PDFDocument12 pagesGaitan 1 PDFDeborah SalinasNo ratings yet
- Ambulation and Parkinson DiseaseDocument22 pagesAmbulation and Parkinson DiseaseDeborah SalinasNo ratings yet
- AMBULATIONDocument12 pagesAMBULATIONDeborah SalinasNo ratings yet
- Agingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDocument22 pagesAgingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDeborah SalinasNo ratings yet
- Falls, Aging and DisabilityDocument17 pagesFalls, Aging and DisabilityDeborah SalinasNo ratings yet
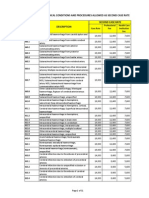
- PhilHealth Circular No. 0035, s.2013 Annex 3 List of Medical Conditions and Procedures Allowed As Second Case RateDocument31 pagesPhilHealth Circular No. 0035, s.2013 Annex 3 List of Medical Conditions and Procedures Allowed As Second Case RateChrysanthus Herrera0% (1)
- Osteoarthritis of The Ankle The Role Of.3Document11 pagesOsteoarthritis of The Ankle The Role Of.3Alex BurhanNo ratings yet
- Regional Traumatology: The Ankle: by Niroshni and RajalakshmiDocument18 pagesRegional Traumatology: The Ankle: by Niroshni and RajalakshmiNiroshni SusanNo ratings yet
- Maisonneuve Fracture - Case PresentationDocument4 pagesMaisonneuve Fracture - Case Presentationtwinke1012No ratings yet
- DR N. Purushothama Rao,: Early Results of A New Single Approach "Document87 pagesDR N. Purushothama Rao,: Early Results of A New Single Approach "Purushothama Rao NalamatiNo ratings yet
- Iwj 15 971Document7 pagesIwj 15 971Francisco Castillo VázquezNo ratings yet
- Ankle Fractures Think 360Document8 pagesAnkle Fractures Think 360Ahmed TawfiqNo ratings yet
- Ankle FracturesDocument36 pagesAnkle FracturesReyhan FarandiNo ratings yet
- Study On Functional Outcome of Bimalleolar Ankle FDocument8 pagesStudy On Functional Outcome of Bimalleolar Ankle Fbhushan adhariNo ratings yet
- American Board of Orthopaedic Surgery: Acceptable CPT Codes For Orthopaedic Sports Medicine Subspecialty Case ListDocument15 pagesAmerican Board of Orthopaedic Surgery: Acceptable CPT Codes For Orthopaedic Sports Medicine Subspecialty Case ListAmerican Aesthetic MCNo ratings yet
- Abstract IOSSMA 2019 - Dr. Fajar Defian PutraDocument2 pagesAbstract IOSSMA 2019 - Dr. Fajar Defian PutrafadefianNo ratings yet
- Ankle FractureDocument11 pagesAnkle FracturecorsaruNo ratings yet
- Ankle: FracturesDocument87 pagesAnkle: FracturesrifkialbanaNo ratings yet
- Special Considerations in The Management of Diabetic Ankle FracturesDocument11 pagesSpecial Considerations in The Management of Diabetic Ankle FracturesArmando RodriguezNo ratings yet
- Common Lower Limb Fracture: DR Tarif Alakhras Orthopedic Surgeon KFMCDocument49 pagesCommon Lower Limb Fracture: DR Tarif Alakhras Orthopedic Surgeon KFMCahmad albab100% (1)
- Acumed Case Study EN AP3 Dual Plating For Posterior Pilon Fractures FNA70 08 ADocument4 pagesAcumed Case Study EN AP3 Dual Plating For Posterior Pilon Fractures FNA70 08 AmayankNo ratings yet
- Growth Plate InjuriesDocument41 pagesGrowth Plate Injurieskosmynin86No ratings yet
- A Prospective Randomized Multicenter Trial Comparing Clinical Outcomes of Patients Treated Surgically With A Static or Dynamic Implant For Acute Ankle Syndesmosis RuptureDocument8 pagesA Prospective Randomized Multicenter Trial Comparing Clinical Outcomes of Patients Treated Surgically With A Static or Dynamic Implant For Acute Ankle Syndesmosis RuptureJake sanchezNo ratings yet
- The Radiology Assistant - Ankle Fracture - Weber and Lauge-Hansen ClassificationDocument17 pagesThe Radiology Assistant - Ankle Fracture - Weber and Lauge-Hansen ClassificationlgtoalejandroNo ratings yet
- Deltoid Ligament Rupture in Ankle Fracture - Diagnosis and ManagementDocument11 pagesDeltoid Ligament Rupture in Ankle Fracture - Diagnosis and ManagementDiana Marcela Benítez HernándezNo ratings yet
- Ankle Fractures: What Is An Ankle Fracture?Document2 pagesAnkle Fractures: What Is An Ankle Fracture?introvert ikonNo ratings yet
- Russian Language ExerciseDocument11 pagesRussian Language ExerciseCopyright Free VideoNo ratings yet
- Ankle Fractures (Broken Ankle) : AnatomyDocument9 pagesAnkle Fractures (Broken Ankle) : AnatomyWisnu Syahputra SuryanullahNo ratings yet
- Ankle Fracture: Yunita Dewi IndrianiDocument23 pagesAnkle Fracture: Yunita Dewi IndrianiMultazam ZulfikarNo ratings yet
- 4443-Multiple Choice Questions in Orthopaedics and TraumaDocument32 pages4443-Multiple Choice Questions in Orthopaedics and TraumaAhmed ALi100% (1)
- The Radiology Assistant: Ankle Fracture - Weber and Lauge-Hansen ClassificationDocument16 pagesThe Radiology Assistant: Ankle Fracture - Weber and Lauge-Hansen ClassificationAnonymous V5xDcrNo ratings yet
- Alistair IEB (2021) - A Comparison of Fibula Pro-Tibia Fixation VersusDocument10 pagesAlistair IEB (2021) - A Comparison of Fibula Pro-Tibia Fixation VersusHariom ShuklaNo ratings yet
- Medial Malleolar FracturesDocument10 pagesMedial Malleolar FracturesSusan Ly VillalobosNo ratings yet
- Fractures of The Foot and Ankle 2018Document240 pagesFractures of The Foot and Ankle 2018okida192100% (2)
- Basic Fracture ManagementDocument107 pagesBasic Fracture ManagementPrabath ChinthakaNo ratings yet