Professional Documents
Culture Documents
Articulo
Articulo
Uploaded by
katcaval.28Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articulo
Articulo
Uploaded by
katcaval.28Copyright:
Available Formats
ORIGINAL RESEARCH
published: 21 December 2020
doi: 10.3389/fmed.2020.595028
Anxiety, Practice Modification, and
Economic Impact Among Iraqi
Dentists During the COVID-19
Outbreak
Anas F. Mahdee 1 , Sarhang S. Gul 2*, Ali A. Abdulkareem 3 and Syed Saad B. Qasim 4
1
Department of Restorative and Aesthetic Dentistry, College of Dentistry, University of Baghdad, Baghdad, Iraq,
2
Department of Periodontics, College of Dentistry, University of Sulaimani, Sulaimani, Iraq, 3 Department of Periodontics,
College of Dentistry, University of Baghdad, Baghdad, Iraq, 4 Department of Bioclinical Sciences, Faculty of Dentistry, Kuwait
University, Safat, Kuwait
Objectives: As health care workers on the front line during the coronavirus (COVID-19)
pandemic, dental practitioners are amongst those at risk due to their close contact with
potentially infected individuals. The aim of the current study was to assess the anxiety,
Edited by: awareness practice modification, and economic impact amongst Iraqi dentists whilst
Fang Hua, working during the outbreak.
Wuhan University, China
Reviewed by: Methods: This study was performed using an online survey questionnaire with aid
Faris Hasan al Lami, of Google forms from 2nd to 23rd July 2020. A total of 484 clinicians responded.
University of Baghdad, Iraq
The questionnaire was composed of open end, closed end, and Likert five-point
Armelia Sari Widyarman,
Trisakti University, Indonesia scale questions to assess anxiety, awareness and financial impact of COVID-19 on
*Correspondence: dentists. Mann–Whitney test was used to compare two groups, whilst Kruskal–Wallis
Sarhang S. Gul was performed by post-hoc test for multigroup comparisons.
sarhang.hama@univsul.edu.iq
orcid.org/0000-0003-1413-4934 Results: The mean age of participants was 36.51 ± 9.164 years and the majority
(75.2%) of these were graduate dentists only. More than 80% of participants reported
Specialty section:
This article was submitted to
anxiety of catching COVID-19. The recorded anxiety level was higher amongst younger
Infectious Diseases - Surveillance, dentists and females. Awareness and practice levels among these dentists of precautions
Prevention and Treatment, and infection-control measures associated with COVID-19 (94%) was found to be high
a section of the journal
Frontiers in Medicine and to be statistically significantly affected by age, qualification and designation (except
Received: 14 August 2020 GP vs. Specialist). With respect to the economic impact, about 75% of practitioners,
Accepted: 02 December 2020 regardless of demographical variables, reported that their income had declined by
Published: 21 December 2020
about 50%.
Citation:
Mahdee AF, Gul SS, Abdulkareem AA Conclusions: The investigation provides clear insights into the anxiety, practice
and Qasim SSB (2020) Anxiety, modifications and economic impact on dentists working in Iraq. Although there is a high
Practice Modification, and Economic
Impact Among Iraqi Dentists During
level of knowledge and awareness of required practice regarding the COVID-19 outbreak
the COVID-19 Outbreak. among Iraqi dentists, they also reported a high level of anxiety.
Front. Med. 7:595028.
doi: 10.3389/fmed.2020.595028 Keywords: anxiety, coronavirus, Iraqi dentists, economic, practice management
Frontiers in Medicine | www.frontiersin.org 1 December 2020 | Volume 7 | Article 595028
Mahdee et al. Impact of COVID-19 Among Dentists
INTRODUCTION period (10). The expense of these precautionary measures and
limitations in the treatment of patients may have had serious
Since the emergence of the novel coronavirus disease (COVID- economic impact on the dentistry field. Hence, the future careers
19) in Wuhan, China, all aspects of life have been influenced of dentists could be affected if the outbreak continues for an
worldwide. The COVID-19 pandemic has spread in an indefinite period.
exponential manner (1, 2), affecting millions of people worldwide Meanwhile, no study has assessed the levels of anxiety among
and causing hundreds of thousands of deaths (3). Many countries Iraqi dentists in the wake of the COVID-19 outbreak, their
have shut down their teaching institutes, industries, sport awareness about this illness and the infection control guidelines
activities, social gatherings, public events, and airports. Drastic to prevent its spread, or the financial impact on their current
measures such as individual self-quarantine and social distancing practice. Therefore, the aim of this study was to use a specially
rules have been introduced in an attempt to control the spread of designed online-based questionnaire to assess the impact of
the infection (4). The condition in Iraq has been no better than in the COVID-19 outbreak on Iraqi dentists in terms of their
many other countries. Since the first registered case of COVID-19 anxiety, awareness and practice modification, and the financial
was recorded on the 24th of February 2020 in an Iranian student implications for their dental practice.
attending the city of Najaf in the south of Iraq, the spread of the
virus has been escalating and as of 1st of July there were 51,524
confirmed cases and 2,050 deaths. METHODS
COVID-19 belongs to the Coronaviridae virus family, which Survey Administration
is characterized by a single strand RNA structure (5). This A cross-sectional survey was conducted using an online
virus has potential to cause severe respiratory tract infection questionnaire that was electronically sent to Iraqi dentists by Iraqi
and pneumonia among infected individuals, and can be Dental Association (IDA). Administration of the questionnaire
easily transmitted via hand contact, saliva, nasal droplets and started on 02/07/2020 for a period of 2 weeks, which was
contaminated surfaces (2, 6). Health care workers and dentists in extended for another week after a reminder was sent, and ended
particular are categorized as at high risk of catching this infection on 23/07/2020. The study was approved by the ethics committee
(7). This could be because their close contact with patients of the College of Dentistry, University of Baghdad in compliance
during routine dental procedures increases the possibility of with the Helsinki declaration (Ref No. 579/06/2020).
infection transmission (8, 9). Droplets and aerosols that are
generated during dental procedures by such as high speed
handpieces, air-water syringes, and ultrasonic scaling could
Study Population and Sample Size
produce a contaminated pathogenic environment within the The survey was exclusively sent to registered Iraqi dentists
dental working field during treatment of an infected person and only completed forms were included in the final analysis.
(6, 9, 10). Therefore, the risk of infection transmission within the All incomplete forms and those returned outside the required
dental team cannot be controlled through the standard protective timeframe were excluded.
measures of daily dental practice (8). This categorization as The total number of registered Iraqi dentists, as officially
high-risk professionals could increase fear within the dental provided by the IDA, was 6,463. Sample size was determined
community (11, 12). according to the following formulas (17, 18):
Regarding the rapid spread of the infection, the World Health
Organization (WHO) and American Dental Association (ADA) Sample size = (distribution of 50%)/[(margin of error%/
published specific precaution guidelines to be implemented confidence level score)2 ]
by dentists during treatment of urgent and emergency cases Confidence level = 1.96 (for confidence level of 95%),
only. Otherwise, they stipulated that dental offices should be
kept closed during the outbreak (13, 14). These guidelines margin of error = 0.05.
emphasized the use of the appropriate precautions including True sample = (sample size × population)/
wearing personal protective equipment (PPE) during dental (sample size + population − 1)
procedures (13, 14). In addition, the use of antibacterial mouth
washes, rubber dam, and high-volume section during treatment The calculated sample size was equal to 363 which was further
procedures with frequent cleaning and disinfecting of surfaces of adjusted to take account of the dropout risk, previously estimated
chairs, door handles and floors was highly recommended (8, 15). from a pilot study, by using the following formula:
Providing a secure environment is of paramount importance for
dentists and dental staff to conduct dental work in a safe working
environment. The high infection rate of COVID-19 and lack of N = n/[1 − (z/100)]
PPE might affect the anxiety of the dentist. The levels anxiety
of dentists have shown a negative impact on decision making, Where N is the adjusted sample size, n is the calculated sample
quality of work, and burnout (16). size, z represents the hypothesized attrition rate (25%). The
On the other hand, in dental practice the demand arose final sample size was equal to 484 dentists. Accordingly, the
for more expensive aerosol controlling equipment such as the questionnaire link was distributed via emails to corresponding
high efficiency particulate arrestor (HEPA) during the outbreak number of randomly selected dentists.
Frontiers in Medicine | www.frontiersin.org 2 December 2020 | Volume 7 | Article 595028
Mahdee et al. Impact of COVID-19 Among Dentists
TABLE 1 | The study questionnaire.
Age
Country
Sex A-Male B-Female
Qualification A-Graduate B-Postgraduate
Designation A-General practitioner B-Specialist C-Consultant
Working place A-Clinic B-Hospital C-Both
Working type A-Private B-Government C-Both
1- Do you have a anxiety of being infected with COVID-19 by a patient or co-worker? Yes No
2- Are you afraid of providing treatment for any patient? Yes No
3- If a patient is coughing or suspected to be infected with COVID-19, are you afraid to provide treatment for him/her? Yes No
4- Do you anxious talking to the patients in close proximity? Yes No
5- Are you afraid that you could carry the infection from your practice back to your family? Yes No
6- Do you feel anxious when you hear that one of your co-workers or colleagues has been infected with COVID-19? Yes No
7- Do you know the illness problems associated with COVID-19 virus? Yes No
8- Do you know the mode of transmission of COVID-19 virus? Yes No
9- Are you updated with the current WHO guidelines for cross-infection control for COVID-19 virus? Yes No
10- Are you currently asking every patient if he/she has recently been in contact with an infected COVID-19 person? Yes No
11- Are you or your staff members taking every patient’s body temperature before performing dental treatment? Yes No
12- Are you deferring dental treatment for patients with suspicious symptoms? Yes No
13- Do you think the routine surgical mask is effective to prevent COVID-19 cross infection? Yes No
14- Do you think that N-95 masks should be used routinely in dental practice because of the current COVID-19 outbreak? Yes No
15- Do you routinely follow universal infection control protocol for every patient? Yes No
16- Do you currently use rubber dam isolation for every patient as a part of your infection control? Yes No
17- Do you routinely use high volume section for every patient as part of droplets and airborne isolation precautions? Yes No
18- Do you routinely prepare antimicrobial mouth rinse for every patient to be used before starting treatment? Yes No
19- Have you changed or increased the procedure of infection control during the COVID-19 pandemic? Yes No
20- Has the schedule of your practice been changed to make it safer for you and the patient? Yes No
21- Do you routinely wash your hands with soap and water/ use sanitizer before and after treatment of every patient? Yes No
22- Do you and your staff members get tested for COVID-19 as a precautionary measure? Yes No
23- Do you know which authority to contact if you come across a patient with suspected COVID-19 infection? Yes No
25- What is the average drop in the number of patients visiting your practice as compared to the period before the COVID-19 pandemic?
A- N/A B- <25% C- 25–50% D- 50–75% E- >75%
26- How many appointments for non-urgent cases have you canceled recently as a part of COVID-19 precaution protocol?
A- N/A B- <25% C- 25–50% D- 50–75% E- >75%
27- Because of the COVID-19 pandemic, how much have the prices for your dental services been reduced, if at all?
A- N/A B- <25% C- 25–50% D- 50–75% E- >75%
28- If any, how much financial compensation (governmental and non-governmental) are you receiving for your losses in your practice?
A- N/A B- <25% C- 25–50% D- 50–75% E- >75%
29- To what extent have you reduced the staff numbers in your clinic?
A- N/A B- <25% C- 25–50% D- 50–75% E- >75%
30- By how much has the practice’s income been reduced due to the COVID 19 pandemic?
A- N/A B- <25% C- 25–50% D- 50–75% E- >75%
31- What percentage of your stored dental materials have expired during the COVID-19 pandemic?
A- N/A B- <25% C- 25–50% D- 50–75% E- >75%
32- If applicable, what has been the average reduction of working days during the COVID-19 outbreak?
A- N/A B- <25% C- 25–50% D- 50–75% E- >75%
Questionnaire Design the country. Before distributing the questionnaire, a pilot study
Google forms was used to create the link for the questionnaire was conducted which included 36 dentists (about 10% of the
(illustrated in Table 1) that was distributed to the targeted sample size). Then data were entered on spreadsheet and
population electronically via IDA to ensure uniform and double-checked by two authors which was followed pre-launch
validated distribution across all groups of dentists, including analysis was performed to check the internal consistency of all
general practitioners, specialists, and consultants, throughout questionnaire’s components.
Frontiers in Medicine | www.frontiersin.org 3 December 2020 | Volume 7 | Article 595028
Mahdee et al. Impact of COVID-19 Among Dentists
The questionnaire was adapted and modified from previously TABLE 2 | Demographic characteristics of the study population.
published surveys (19, 20). The questionnaire used for this study
AGE (YEARS)
was composed of demographic/practice-related, closed end, and
(mean± SD) 36.51 ± 9.16
Likert five-point scale questions. These questions were divided
Age range 23–70
into four sections:
AGE GROUPS (YEARS)
Section 1 was designed to collect demographic/practice-related ≤35 222 (51)§
variables of the respondents. >35 213 (49)§
Section 2, questions #1 to #6, was intended to assess the anxiety Gender
among dentists deriving from the COVID-19 infection. Male 218 (50.1) §
Section 3, questions #7 to #23, was designed to evaluate Female 217 (49.9)§
the dentists’ awareness and practice modification about QUALIFICATION
the precautions and infection-control measures for Graduate 327 (75.2)§
COVID-19 infection. Postgraduate 108 (24.8)§
Section 4, questions #24 to #32, consisted of questions that DESIGNATION
explored the economic impact of COVID-19 on dental practice. General practitioner 208 (47.8)§
For closed end questions, each positive response “Yes” was Specialist 206 (47.4)§
marked as “1” while “No” was marked with “0.” The frequency Consultant 21 (4.8)§
of the positive/negative responses was used to assess the dentists’ WORKPLACE
anxiety (section 2) and awareness (section 3) regarding the Clinic 202 (46.4)§
COVID-19 infection. For section 4, the responses “N/A,” “<25%,” Hospital 70 (16.1)§
“25–50%,” “50–75%,” “>75%” received sequential scores of “1,” Both 163 (37.5)§
“2,” “3,” “4,” “5,” respectively. The scores for each section were EMPLOYMENT TYPE
summed together to calculate the mean of the answers to evaluate Private 135 (31.1)§
the response according to the different independent variables. Governmental 98 (22.5)§
Both 202 (46.4)§
Statistical Analysis Total 435 (100)§
Demographic data and total responses for each question were
§ Frequency, percentage.
analyzed by descriptive statistics expressed by mean, standard
deviation, and frequency/percentage. Inferential analysis for
sections 2, 3, and 4 was performed by using Mann–Whitney
test for comparing two groups while Kruskal–Wallis followed
by post-hoc test was used for multiple groups comparisons. The aggravated (397, 91%) if a patient was showing a sign of suspected
statistically significant value was set at p < 0.05. All analyses were infection such as coughing (Q3). Moreover, about 72% (316) of
performed by using GraphPad Prism (Version 8.4.3, GraphPad the respondents were not comfortable with being in close contact
Software, San Diego, CA, USA). with their patients (Q4). The highest scoring response among
the participants (413, 94%) was associated with the anxiety of
RESULTS carrying infection home to their family (Q5), whilst the second
highest response (395, 90%) related to hearing that a co-worker
A total of 435 dentists (218 male and 217 female) with mean had been infected with COVID-19 (Q6).
age of 36.51 ± 9.164 years (ranging from 23 to 70 years) Regarding responses to section 3 questions, the dentists’
participated in the study (Table 2). The number of respondents highest scores related to their knowledge about the COVID-19
represented 89.9% of the calculated sample size (484) after illness (Q7, 413, 94%) (Figure 1B) and its modes of transmission
excluding 49 dentists who did not response to the questionnaire (Q8, 424, 97%), modification in infection control procedure
within the specified time. The number of the respondents (435) (Q19, 410, 94%) re-scheduling patients’ appointments (Q20, 404,
was considered as a satisfactory response rate (89.8%). The 93%), and washing hands before and after treatment (Q21, 416,
majority of respondents (327, 75.2%) were graduate dentists, in 95%). Additionally, three questions achieved (>80%) positive
comparison to 108 (24.8%) who had postgraduate degrees. The responses including: the dentist had updated information
proportions of general practitioners, specialists and consultants about the current WHO guidelines for infection control (Q9),
were 47.8% (208), 47.4% (206), and 4.8% (20), respectively. deferring treatment of patients with suspicious symptoms
Furthermore, 202 (46%) of respondents working in clinics (12), and following universal infection control protocol (Q15).
worked in both the private and governmental sector (Table 2). Whereas, the lowest awareness score (138, 31.7%) related to the
Responses to section 2 questions relating to dentists’ feelings effectiveness of surgical masks to prevent cross infection (Q13),
about the COVID-19 pandemic indicated that the majority of in comparison to nearly 80% of respondents who thought that
respondents (386, > 80%) (Figure 1A) were anxious of catching N95 masks should be used routinely in dental practice (Q14). The
the COVID-19 infection (Q1). Over 60% (274) of the dentists response to (Q16) about the use of rubber dam as an infection
were afraid of treating any patients (Q2). This anxiety was further control measure was equally low at 31.7% (138), but a higher
Frontiers in Medicine | www.frontiersin.org 4 December 2020 | Volume 7 | Article 595028
Mahdee et al. Impact of COVID-19 Among Dentists
FIGURE 1 | Dentists’ responses to anxiety and awareness questions: (A) responses to individual questions on anxiety of COVID-19 and (B) awareness of precaution
and infection control-measures.
percentage of respondents (265, >60%) confirmed that they used Inferential analysis of the questionnaire sections showed
high volume section as a droplets precaution measure (Q17). that older (>35 years old) and male respondents exhibited a
The economic impact of COVID-19 was investigated in this statistically significant lower degree of anxiety of COVID-19
study via the section 4 questions (Figure 2). About 27% of compared to younger (≤35 years old, p = 0.018) and female
the respondents suggested that the price of personal protection (p = 0.003) respondents, respectively (Table 3). Furthermore,
equipment had increased by >75% of the original price (Q24). the respondents who worked only in a hospital or in a
Meanwhile, 32% of the dentists indicated that the number clinic and hospital showed a statistically significantly higher
of patients had declined by 25–50% (Q25). The influence of anxiety than those working only in a clinic. Similarly, those
COVID-19 on income was very apparent as >75% of the dentists working only in the government sector or in the government
reported that their income had dropped by 25–50% (Q30), with and private sector showed statistically significantly higher
a similar response regarding the reduction in their working anxiety from COVID-19 than those working only in private
days (Q32). The level of financial compensation received by the clinics. However, respondents’ qualifications and designation
dentists was unsatisfactory as more than half of the respondents did not show a statistically significant impact on anxiety
were not eligible for any support programmes (Q28). However, of COVID-19 (Table 3). Generally, the mean of responses
the majority of the respondent dentists had not decreased their showed a high level of anxiety of COVID-19 infection
staff numbers (Q29) (Figure 2). (5.01 ± 1.37; Table 3).
Frontiers in Medicine | www.frontiersin.org 5 December 2020 | Volume 7 | Article 595028
Mahdee et al. Impact of COVID-19 Among Dentists
TABLE 3 | Respondents’ anxiety of the COVID-19 infection.
Variables Mean ± SD Comparison p-value
AGE
≤35 5.14 ± 1.27 ≤ 35 vs. > 35 0.018*
>35 4.87 ± 1.45
GENDER
Male 4.78 ± 1.57 Male vs. female 0.003*
Female 5.24 ± 1.08
QUALIFICATION
Graduate 4.9 ± 1.39 Postgraduate vs. 0.363*
Graduate
Postgraduate 5.04 ± 1.36
DESIGNATION
General practitioner 4.89 ± 1.43 GP vs. Specialist 0.377†
FIGURE 2 | Dentists’ responses on the economic impact of COVID-19 (GP)
outbreak on their practice. Specialist 5.11 ± 1.34 GP vs. Consultant >0.999†
Consultant 5.23 ± 0.88 Consultant vs. Specialist >0.999†
WORKPLACE
Clinic 4.76 ± 1.45 Clinic vs. Both 0.003†
The mean awareness of respondents (section 3) was 12.65
Hospital 5.31 ± 1.08 Clinic vs. Hospital 0.015†
± 2.36 (Table 4). Age of the study participants have shown
Both 5.19 ± 1.33 Hospital vs. Both >0.999†
a statistically significant impact on respondents’ awareness,
EMPLOYMENT TYPE
whereas, this is not the case when male and female compared.
Private 4.71 ± 1.51 Private vs. Governmental 0.046†
Furthermore, qualification and designation (except for GP vs.
Governmental 5.12 ± 1.09 Private vs. Both 0.015†
Specialist) were found to have a statistically significant effect
Both 5.2 ± 1.36 Governmental vs. Both 0.064†
on respondents’ awareness (P < 0.05, Table 4). Meanwhile,
Total 5.01 ± 1.37
no statistically significant differences in respondents’ awareness
were identified according to workplace and employment type *Mann–Whitney test, †Kruskal–Wallis test.
(Table 4).
Regarding the economic impact, no demographic variables
emerged as having a statistically significant economic effect due to the quick spread of the virus, general feelings of stress
(Table 5). However, the mean economic effect was recorded as and fear among healthcare workers for their own safety and
equal to 2.72 ± 0.71 out of 5 (Table 5), i.e., the economic losses that of their families (23). Additionally, the nature of this
incurred by the dental community amounted to more than 50%. disease, with its prolonged incubation period (as long as 14
days), its spectrum that ranged from asymptomatic to death,
DISCUSSION and the absence of a vaccine or treatment, are all factors
potentially exacerbating stressful feelings among healthcare
The present cross-sectional study reported a high level of workers, especially dentists. This confirms findings from studies
anxiety among Iraqi dentists as a result of the COVID-19 about COVID-19 (11), or previous outbreaks of similar infectious
outbreak and high awareness about preventing its transmission respiratory diseases such as SARS, which demonstrated severe
and avoiding infection; in addition, they and their practices and sustained psychological trauma, especially among the front
have been economically affected due to this pandemic situation. line healthcare workers (24, 25).
These findings are understandable because dentists fall within Another interesting finding within the present study was
the highest risk category, since their practice is associated with that the recorded anxiety level was higher among younger than
generation of droplets and aerosols which is considered as a older dentists and females than males. This goes against the
main route of virus transmission (6). The high levels of anxiety reports that among infected individuals there are higher risk
recorded among these Iraqi dentists can be considered as natural groups, including older and male adults, who are more likely
human feelings during the pandemic situation, especially in to develop severe respiratory symptoms and die than younger
light of the increasing infection and mortality rates. In Iraq individuals and females (26). It may be that older dentists are
the mortality rate is considered to be higher (about 3.9%) in more experienced than younger dentists in dealing with similar
comparison to other regional countries, such as the UAE with pandemic situations. This may make them more confident and
only a (0.5%) mortality rate (3). This could possibly be due less prone to anxiety. This was also reflected in the finding by this
to differences in available health resources between these two study of a statistically significant higher level of awareness about
countries (21). The general weakness in the medical foundations the virus and its mode of transmission among dentists aged above
and care system in Iraq after four decades of military conflicts 35 years in comparison to those aged below 35 years. Moreover,
(22), and the exaggerated pressure on the health care system since females, as mothers, tend to have closer contact with their
Frontiers in Medicine | www.frontiersin.org 6 December 2020 | Volume 7 | Article 595028
Mahdee et al. Impact of COVID-19 Among Dentists
TABLE 4 | Respondents’ awareness of COVID-19 infection-control measures. TABLE 5 | Economic impact of the COVID-19 outbreak.
Variables Mean ± SD Comparison p-value Variables Mean ± SD Comparison p-value
AGE AGE
≤35 11.14 ± 2.41 ≤35 vs. >35 <0.001* ≤35 2.71 ± 0.69 ≤ 35 vs. > 35 0.955*
>35 12.99 ± 2.24 >35 2.72 ± 0.72
GENDER GENDER
Male 12.32 ± 2.58 Male vs. female 0.121* Male 2.67 ± 0.72 Male vs. female 0.109*
Female 12.8 ± 2.09 Female 2.77 ± 0.69
QUALIFICATION QUALIFICATION
Graduate 11.98 ± 2.49 Postgraduate vs. 0.003* Graduate 2.66 ± 0.8 Postgraduate vs. 0.468*
Graduate Graduate
Postgraduate 12.75 ± 2.28
Postgraduate 2.73 ± 0.67
DESIGNATION
DESIGNATION
General practitioner 12.48 ± 2.24 GP vs. Specialist >0.999†
General practitioner 2.71 ± 0.73 GP vs. Specialist 0.463†
(GP)
(GP)
Specialist 12.53 ± 2.48 GP vs. Consultant 0.016†
Specialist 2.74 ± 0.65 GP vs. Consultant 0.463†
Consultant 13.91 ± 1.92 Consultant vs. Specialist 0.027†
Consultant 2.54 ± 0.94 Consultant vs. Specialist 0.353†
WORKPLACE
WORKPLACE
Clinic 12.76 ± 2.07 Clinic vs. Both 0.569†
Clinic 2.73 ± 0.73 Clinic vs. Both >0.999†
Hospital 12.44 ± 2.58 Clinic vs. Hospital 0.963†
Hospital 2.68 ± 0.67 Clinic vs. Hospital >0.999†
Both 12.36 ± 2.58 Hospital vs. Both >0.999†
EMPLOYMENT TYPE Both 2.71 ± 0.69 Hospital vs. Both >0.999†
Private 12.82 ± 2.09 Private vs. Governmental 0.196† EMPLOYMENT TYPE
Governmental 12.26 ± 2.38 Private vs. Both >0.999† Private 2.63 ± 0.74 Private vs. Governmental >0.999†
Both 12.53 ± 2.52 Governmental vs. Both 0.674† Governmental 2.69 ± 0.67 Private vs. Both 0.077†
Total 12.65 ± 2.36 Both 2.79 ± 0.69 Governmental vs. Both 0.877†
Total 2.72 ± 0.71
*Mann–Whitney test, † Kruskal–Wallis test.
*Mann–Whitney test, † Kruskal–Wallis test.
children than other family members, the anxiety of transferring
infection to family members, especially their children, could during the routine examination to identify potentially infectious
increase feelings of stress among female in comparison to male conditions among patients and the necessary precautionary
dentists. In the same way, dentists who were working in the management. Indeed, under such pandemic circumstances, the
public sector, in clinics or hospitals, reported higher anxiety levels conventional precautions already recommended by WHO and
than others. This could be attributed to the large number of any other infectious control authority worldwide should be
dental patients visiting the public centers per day in comparison rigorously applied to prevent cross-infection within dental
to private clinics (27). Consequently, this may increase dentists’ practice. But unfortunately, more than 60% of the respondents
concerns and anxiety of being infected compared to those were not using rubber dam for every patient as a cross-infection
working only in private clinics, who have more control over their control. Rubber dam effectively limits the spread of aerosols
appointments, case selection and cancellation of non-emergency during use of rotary instruments, decreases the hazard of fine
cases. Finally, consultant dentists and those with postgraduate instrument swallowing, gives excellent isolation of the working
degree have higher levels awareness than their counterparts field and increases patients’ acceptance of dental procedures
and this can be explained by the fact the majority of these (28). Therefore, training courses and workshops are suggested
dentists work in academic field, thus more update about the new for Iraqi dentists, especially new graduates, to increase their
developments in their field including the COVID-19 outbreak. awareness about the effectiveness of rubber dam in controlling
Almost all of the responding dentists were aware of the nature the spread of infection. This could improve their hand skills and
of the COVID-19 illness and its mode of transmission. This increase their willingness to consider rubber dam as part of their
information is considered to be crucial in terms of applying routine practice. The usage of high volume suction should also be
infection control measures while carrying out dental treatment. considered as an essential method during routine dental practice
In the same way, over 80% of the dentists responded that to control aerosols and droplets evacuation (10).
they were up to date about the current WHO guidelines for The use of antimicrobial mouth washes before starting dental
cross-infection control measures within dental practice (14). procedure is also recommended in the WHO guidelines for the
This was reflected through over 70% of the respondents asking current pandemic. Interestingly, over 40% of the respondents
their patients if they had been in contact with an infected were complying with this recommendation. Mouthwashes such
COVID-19 individual, and above 60% recording patients’ as chlorhexidine (29), 1% hydrogen peroxide (6), or povidone
body temperature. Logically, this is basic information required iodine (30) can be employed to decrease microbial loading inside
Frontiers in Medicine | www.frontiersin.org 7 December 2020 | Volume 7 | Article 595028
Mahdee et al. Impact of COVID-19 Among Dentists
the oral cavity. The latter has virucidal activity against SARS-CoV patients (35). These financial impacts on dentistry as a profession
and MERS-CoV coronaviruses and is recommended to be used at may have serious implications for the future of this career.
0.5% concentration as a mouthwash for patients before initiating The limitations of this study that should be considered is
a clinical procedure. Additionally, the operator is also advised the rapid changes in respondents’ psychology and practice in
to use povidone iodine as a nasal spray (0.4%) and mouthwash accordance with the progression of the current outbreak, the
(0.5%) before and after suspected patient contact (31). attitudes and awareness of dentists will certainly be altered by
A positive finding by the current study was that the majority future alteration in the scientific knowledge about COVID-19.
of Iraqi dentists were routinely focusing on hand hygiene before Additionally, although the distribution of the questionnaire for
and after treating each patient, which is considered as an essential the present study was done through the IDA, fewer responses
infection control measure for dental practitioners. Frequent were obtained from consultants in comparison to the other
hand washing with water and soap or using alcohol containing designations. This possibly because of the general panic situation
sanitizer is included in the WHO infection control guidelines during the COVID-19 outbreak altered the priorities for potential
for the current pandemic (14). The spread of respiratory viruses respondents. Thus, the findings of the current study should be
can be effectively avoided by proper hand washing and cleaning carefully interpreted to avoid generalization of the data.
with alcohol-based sanitizers (8, 32). Furthermore, the majority
of the study respondents agreed with the routine use of N- CONCLUSIONS
95 respirators rather than surgical masks in dental practice
during the COVID-19 outbreak. The use of such personal The emergence of the novel coronavirus has increased concern
protection equipment (PPE) is also recommended by the WHO among healthcare workers, especially dentists, regarding aerosols
and ADA guidelines when performing aerosols generating borne microbes rather than the conventional blood borne
procedures (33). microbes. This has dramatically increased the anxiety among
Carefulness in selecting cases, controlling appointments, and dentists about getting the infection and has altered their
receiving only emergency cases were also recommended by awareness toward a new era. Although, Iraqi dentists have gained
the ADA and WHO guidelines (13, 14). Almost all of the a high level of knowledge and practice to address the COVID-19
respondents in the current study stated that they had altered outbreak, their anxiety was high. It is important in the current
their appointment schedules to control the spread of the virus. scenario to modify the conventional dental practice to deal with
This process could be started by initially calling patients or emergencies only or close down practices until the outbreak
having video conferences to identify their need and decide if their recedes. However, this situation may last for an indefinite period,
condition requires clinical intervention (34). This could help in which would have a dramatic impact not only on the economy
limiting face-to-face contact, making diagnoses through remote which have shown to affect the majority of responders by
dental screening, deterring any COVID-19 susceptible patients, reducing their income by 50% but also on the future of the dental
delaying nonemergency work, and planning effectively for the profession such as increasing levels of anxiety amongst dentist
emergency cases (8, 34). and adapting to practice modification.
According to the findings of the present study, the
economic losses caused by the COVID-19 outbreak to the DATA AVAILABILITY STATEMENT
dental community in Iraq amounted to about 50%. This is
understandable during such a pandemic situation. The whole The raw data supporting the conclusions of this article will be
country has been affected by quarantines and lockdowns in an made available by the authors upon reasonable request.
attempt to control the spread of the infection. The lockdowns
consisted of intermittent periods of complete closure for all ETHICS STATEMENT
sectors followed by partial lockdown for specific sectors including
The study was approved by the ethics committee of the College
schools, universities, tourism, and others. This has had severe
of Dentistry, University of Baghdad in compliance with the
economic impact on almost all activities, including dentistry
Helsinki declaration.
(4). Additionally, the majority of respondents in the current
study reported reduction of their working days, rescheduling
AUTHOR CONTRIBUTIONS
of their appointments to see emergency cases only, absence
of governmental support, and reduction in their total income. AM: study conception. AA and SG: study design. AM, AA,
On the other hand, as some of the study participants received SG, and SQ: data collection. AA and SG: data analysis and
financial compensation, the degree of economic impact has manuscript drafting. AA and SG: data interpretation. SG and SQ:
shown to be varied from one to another dentist. However, none of critical revision of the manuscript. All authors: approval of the
demographical variables have shown an impact on income. This final version. All authors contributed to the article and approved
can be explained by the fact that during the national lockdown, the submitted version.
working in private dental clinics was stopped by government
and the only source of income were their monthly salary by ACKNOWLEDGMENTS
the government. According to a recent investigation conducted
in the U.S., this economic impact on dental services could be The authors would like to thank all the dentists who responded
extended to 2022 because of financial hardship among dental to this survey.
Frontiers in Medicine | www.frontiersin.org 8 December 2020 | Volume 7 | Article 595028
Mahdee et al. Impact of COVID-19 Among Dentists
REFERENCES regarding the COVID-19 pandemic: a multinational study. Dent Med Probl.
(2020) 57:11–7. doi: 10.17219/dmp/119743
1. Neher RA, Dyrdak R, Druelle V, Hodcroft EB, Albert J. Potential impact 21. Ji Y, Ma Z, Peppelenbosch MP, Pan Q. Potential association between COVID-
of seasonal forcing on a SARS-CoV-2 pandemic. Swiss Med Wkly. (2020) 19 mortality and health-care resource availability. Lancet Glob Health. (2020)
150:w20224. doi: 10.4414/smw.2020.20224 8:e480. doi: 10.1016/S2214-109X(20)30068-1
2. Khurshid Z, Asiri FYI, Al Wadaani H. Human saliva: Non-invasive fluid for 22. Al Hilfi TK, Lafta R, Burnham G. Health services in Iraq. Lancet. (2013)
detecting novel coronavirus (2019-nCoV). Int J Environ Res Public Health. 381:939–48. doi: 10.1016/S0140-6736(13)60320-7
(2020) 17:2225. doi: 10.3390/ijerph17072225 23. Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some
3. WHO. World Health Organization Coronavirus Disease (COVID-19) recommendations during the COVID-19 epidemic in China. Intens Care Med.
Dashboard. (2020). Available online at: https://covid19.who.int/?gclid= (2020) 46:837–40. doi: 10.1007/s00134-020-05979-7
EAIaIQobChMItvnC1ej16gIVxYjVCh0YUwNkEAAYASAAEgJRDfD_BwE. 24. Tam CW, Pang EP, Lam LC, Chiu HF. Severe acute respiratory
4. Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. syndrome (SARS) in Hong Kong in 2003: stress and psychological
The socio-economic implications of the coronavirus pandemic (COVID-19): impact among frontline healthcare workers. Psychol Med. (2004)
areview. Int J Surg. (2020) 78:185–93. doi: 10.1016/j.ijsu.2020.04.018 34:1197. doi: 10.1017/S0033291704002247
5. Chen Y, Liu Q, Guo D. Emerging coronaviruses: genome 25. McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, Sham PC, et al.
structure, replication, and pathogenesis. J Med Virol. (2020) Immediate and sustained psychological impact of an emerging infectious
92:418–23. doi: 10.1002/jmv.25681 disease outbreak on health care workers. Can J Psychiatry. (2007) 52:241–
6. Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 7. doi: 10.1177/070674370705200406
2019-nCoV and controls in dental practice. Int J Oral Sci. (2020) 12:1– 26. Jordan RE, Adab P, Cheng K. Covid-19: risk factors for severe disease and
6. doi: 10.1038/s41368-020-0075-9 death. BMJ. (2020) 368:m1198. doi: 10.1136/bmj.m1198
7. Administration OSaH. COVID-19 Control and Prevention/ Dentisrty Worker 27. Fernández-Feijoo J, Garea-Gorís R, Fernández-Varela M, Tomás-Carmona
and Employers. United States Deparment of Labor (2020). I, Diniz-Freitas M, Limeres-Posse J. Prevalence of systemic diseases among
8. Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus patients requesting dental consultation in the public and private systems. Med
disease 19 (COVID-19): implications for clinical dental care. J Endod. (2020) Oral Patol Oral Cir Bucal. (2012) 17:e89. doi: 10.4317/medoral.17313
46:584–95. doi: 10.1016/j.joen.2020.08.005 28. Madarati A, Abid S, Tamimi F, Ezzi A, Sammani A, Shaar MBAA, et al.
9. Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and Dental-dam for infection control and patient safety during clinical endodontic
future challenges for dental and oral medicine. J Dent Res. (2020) 99:481– treatment: preferences of dental patients. Int J Environ Res Public Health.
7. doi: 10.1177/0022034520914246 (2018) 15:2012. doi: 10.3390/ijerph15092012
10. Ge Z-y, Yang L-m, Xia J-j, Fu X-h, Zhang Y-z. Possible aerosol transmission of 29. Nayak SU, Kumari A, Rajendran V, Singh VP, Hegde A, Pai KK.
COVID-19 and special precautions in dentistry. J Zhejiang Univ Sci B. (2020) Comparative evaluation of efficacy of chlorhexidine and herbal mouthwash
21:361–8. doi: 10.1631/jzus.B2010010 as a preprocedural rinse in reducing dental aerosols: a microbiological study.
11. Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS, et al. Fear Int J Dent. (2020) 2020:2021082. doi: 10.1155/2020/2021082
and practice modifications among dentists to combat Novel Coronavirus 30. Eggers M, Koburger-Janssen T, Eickmann M, Zorn J. In vitro
Disease (COVID-19) outbreak. Int J Environ Res Public Health. (2020) bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash
17:2821. doi: 10.3390/ijerph17082821 against respiratory and oral tract pathogens. Infect Dis Ther. (2018)
12. Ng K, Poon BH, Kiat Puar TH, Shan Quah JL, Loh WJ, Wong YJ, et al. 7:249–59. doi: 10.1007/s40121-018-0200-7
COVID-19 and the risk to health care workers: a case report. Ann Intern Med. 31. Mady LJ, Kubik MW, Baddour K, Snyderman CH, Rowan NR.
(2020) 172:766–7. doi: 10.7326/L20-0175 Consideration of povidone-iodine as a public health intervention for
13. ADA. Summary of ADA Guidance During the COVID-19 Crisis. American COVID-19: Utilization as “Personal Protective Equipment” for frontline
Dental Association (2020). Available online at: https://www.ada.org/en/ providers exposed in high-risk head and neck and skull base oncology
press-room/news-releases/2020-archives/april/summary-of-ada-guidance- care. Oral Oncol. (2020) 105:104724. doi: 10.1016/j.oraloncology.2020.1
during-the-covid-19-crisis (cited September 16, 2020). 04724
14. WHO. Considerations for the Provision of Essential Oral Health Services in the 32. Fung ICH, Cairncross S. Effectiveness of handwashing in
Context of COVID-19. Interim Guidance: World Health Organization (2020). preventing SARS: a review. Trop Med Int Health. (2006)
Available online at: https://apps.who.int/iris/bitstream/handle/10665/333625/ 11:1749–58. doi: 10.1111/j.1365-3156.2006.01734.x
WHO-2019-nCoV-Oral_health-2020.1-eng.pdf (cited September 16, 2020). 33. Coulthard P. Dentistry and coronavirus (COVID-19)-moral decision-making.
15. CDC. Interim Infection Prevention and Control Recommendations for Br Dent J. (2020) 228:503–5. doi: 10.1038/s41415-020-1482-1
Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) 34. Ghai S. Teledentistry during COVID-19 pandemic. Diabetes Metab Syndr.
Pandemic. Centers for Disease Control and Prevention (2020). Available (2020) 14:933–5. doi: 10.1016/j.dsx.2020.06.029
online at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection- 35. Nasseh K, Vujicic M. Modeling the Impact of COVID-19 on U.S. Dental
control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fcdc. Spending: Health Policy Institute Research Brief. American Dental Association
gov%2Fcoronavirus%2F2019-ncov%2Finfection-control%2Fcontrol- (2020). Available online at: https://www.ada.org/$\sim$/media/ADA/Science
recommendations.html (cited September 16, 2020). %20and%20Research/HPI/Files/HPIBrief_0420_1.pdf?la=en.~
16. Chipchase SY, Chapman HR, Bretherton R. A study to explore if dentists’
anxiety affects their clinical decision-making. Br Dent J. (2017) 222:277– Conflict of Interest: The authors declare that the research was conducted in the
90. doi: 10.1038/sj.bdj.2017.173 absence of any commercial or financial relationships that could be construed as a
17. Taherdoost H. Determining sample size; how to calculate survey sample size. potential conflict of interest.
Int J Econ Manag. (2017) 2:237–9. Avialable online at: https://papers.ssrn.com/
sol3/papers.cfm?abstract_id=3224205 The reviewer FL declared a shared affiliation with several of the authors AA
18. Charan J, Biswas T. How to calculate sample size for different study and AM to the handling editor at time of review.
designs in medical research? Indian J Psychol Med. (2013) 35:121–
6. doi: 10.4103/0253-7176.116232 Copyright © 2020 Mahdee, Gul, Abdulkareem and Qasim. This is an open-access
19. Tysiac-Miśta M, Dziedzic A. The attitudes and professional approaches article distributed under the terms of the Creative Commons Attribution License (CC
of dental practitioners during the COVID-19 outbreak in Poland: BY). The use, distribution or reproduction in other forums is permitted, provided
a cross-sectional survey. Int J Environ Res Public Health. (2020) the original author(s) and the copyright owner(s) are credited and that the original
17:4703. doi: 10.3390/ijerph17134703 publication in this journal is cited, in accordance with accepted academic practice.
20. Kamate SK, Sharma S, Thakar S, Srivastava D, Sengupta K, Hadi AJ, No use, distribution or reproduction is permitted which does not comply with these
et al. Assessing Knowledge, Attitudes and Practices of dental practitioners terms.
Frontiers in Medicine | www.frontiersin.org 9 December 2020 | Volume 7 | Article 595028
You might also like
- Non Deliverable ForwardDocument17 pagesNon Deliverable ForwardManish GuptaNo ratings yet
- Original A Nation Wide SurveyDocument7 pagesOriginal A Nation Wide SurveyThe Heavenly ShadesNo ratings yet
- 1 s2.0 S0002817721006589 MainDocument11 pages1 s2.0 S0002817721006589 MainkhamilatusyNo ratings yet
- P.covid B.ingDocument9 pagesP.covid B.ingbudiNo ratings yet
- Corona Dentist Awareness PerceptionDocument7 pagesCorona Dentist Awareness PerceptionFirda IzzatiNo ratings yet
- 11 PDFDocument7 pages11 PDFfirdaizzatiNo ratings yet
- Covid-19. Are We Prepared For Future Outbreaks? An Online Survey To Assess Knowledge, Attitude and Awareness of Dental ProfessionalsDocument13 pagesCovid-19. Are We Prepared For Future Outbreaks? An Online Survey To Assess Knowledge, Attitude and Awareness of Dental ProfessionalsIJAR JOURNALNo ratings yet
- Impact of COVID-19 On Oral Emergency Services: Scientific Research ReportDocument55 pagesImpact of COVID-19 On Oral Emergency Services: Scientific Research ReportgeometrydashyioNo ratings yet
- JIndianAcadOralMedRadiol323203-5276647 143926Document2 pagesJIndianAcadOralMedRadiol323203-5276647 143926Nabila RizkikaNo ratings yet
- Change in Ophthalmology Practice During COVID-19 Pandemic: Egyptian PerspectiveDocument7 pagesChange in Ophthalmology Practice During COVID-19 Pandemic: Egyptian Perspectiveشهر رمزحنNo ratings yet
- Endodontic Treatment During COVID-19 Pandemic - Economic Perception of Dental ProfessionalsDocument8 pagesEndodontic Treatment During COVID-19 Pandemic - Economic Perception of Dental Professionalsbobs_fisioNo ratings yet
- Covid-19 Outbreak - Immediate and Long-Term Impacts On The Dental ProfessionDocument4 pagesCovid-19 Outbreak - Immediate and Long-Term Impacts On The Dental ProfessionYasir IsrarNo ratings yet
- Covid Dental AuxillariesDocument9 pagesCovid Dental AuxillariesfirdaizzatiNo ratings yet
- The Impact of Covid 19 Pandemic On Training and Mental Health of Residents A Cross Sectional StudyDocument11 pagesThe Impact of Covid 19 Pandemic On Training and Mental Health of Residents A Cross Sectional StudyramaNo ratings yet
- Fear and Practice Modifications Among Dentists To Combat Novel Coronavirus Disease (COVID-19) OutbreakDocument11 pagesFear and Practice Modifications Among Dentists To Combat Novel Coronavirus Disease (COVID-19) Outbreakharshita parasharNo ratings yet
- .Clinical Experience, Knowledge, Attitudes and Practice of Turkish Pediatric Dentists During The COVID-19 PandemicDocument23 pages.Clinical Experience, Knowledge, Attitudes and Practice of Turkish Pediatric Dentists During The COVID-19 PandemicMichael PomaNo ratings yet
- Assessment of Pediatric Dental Guidelines in The post-COVID 19 PeriodDocument14 pagesAssessment of Pediatric Dental Guidelines in The post-COVID 19 PeriodCha AlegriaNo ratings yet
- Impact of The COVID-19 Pandemic On The TimingDocument8 pagesImpact of The COVID-19 Pandemic On The TimingMichael PomaNo ratings yet
- Editing of ProposalDocument9 pagesEditing of ProposalMustafaNo ratings yet
- Assessment of Paediatric Dental Guidelines and CarDocument15 pagesAssessment of Paediatric Dental Guidelines and CarRisana RahoofNo ratings yet
- Alharbi Guideline Covid-19Document6 pagesAlharbi Guideline Covid-19desy purnama sariNo ratings yet
- IntJOralHealthDent 6 2 122 125Document5 pagesIntJOralHealthDent 6 2 122 125Laura Putri TraviraNo ratings yet
- Knowledge, Attitude and Practice Regarding COVID-19 and Its Impact On Dentistry: A Cross-Sectional Survey Among Nepalese DentistsDocument7 pagesKnowledge, Attitude and Practice Regarding COVID-19 and Its Impact On Dentistry: A Cross-Sectional Survey Among Nepalese DentistsSalon LamichhaneNo ratings yet
- Dental Patients' Perspective On COVID-19: A Systematic ReviewDocument18 pagesDental Patients' Perspective On COVID-19: A Systematic ReviewJohnny CHNo ratings yet
- COVID-19's Impact On Private Practice and Academic Dentistry in North AmericaDocument4 pagesCOVID-19's Impact On Private Practice and Academic Dentistry in North AmericaJoDaNo ratings yet
- Guidelines For Dental Care Provision During The COVID-19 PandemicDocument7 pagesGuidelines For Dental Care Provision During The COVID-19 PandemicFirda IzzatiNo ratings yet
- Impact of Pandemic Period of Covid - 19 in Dental MedicineDocument11 pagesImpact of Pandemic Period of Covid - 19 in Dental MedicineAndreea Andrei AndreeaNo ratings yet
- Dental Care and Personal Protective Measures For Dentists and Non-Dental Health Care WorkersDocument5 pagesDental Care and Personal Protective Measures For Dentists and Non-Dental Health Care WorkersKalpanaNo ratings yet
- COVID-19 PublicationDocument8 pagesCOVID-19 PublicationMariam TariqNo ratings yet
- Coronavirus Disease 2019 (COVID-19) : Emerging and Future Challenges For Dental and Oral MedicineDocument7 pagesCoronavirus Disease 2019 (COVID-19) : Emerging and Future Challenges For Dental and Oral MedicineDaniela Valencia FigueroaNo ratings yet
- Dentistry in Post COVIDDocument3 pagesDentistry in Post COVIDsagrika groverNo ratings yet
- Knowledge of Legal Aspects in Teledentistry AmongDocument6 pagesKnowledge of Legal Aspects in Teledentistry AmongGian ErnestoNo ratings yet
- The Impact of The COVID-19 Epidemic On The Utilization of Emergency Dental ServicesDocument4 pagesThe Impact of The COVID-19 Epidemic On The Utilization of Emergency Dental ServicesMishellKarelisMorochoSegarraNo ratings yet
- Pandemic Preparedness of Dentists Against Coronavirus Disease: A Saudi Arabian ExperienceDocument13 pagesPandemic Preparedness of Dentists Against Coronavirus Disease: A Saudi Arabian ExperiencenoviNo ratings yet
- A Scoping Review of Respirator Literature and A Survey Among Dental ProfessionalsDocument12 pagesA Scoping Review of Respirator Literature and A Survey Among Dental ProfessionalsHNiondiv EdvmpoeirmNo ratings yet
- Compliance With Health ProtocolsDocument7 pagesCompliance With Health Protocolskadoxe1682No ratings yet
- Maternal Practices Towards Dental Treatment of Primary School Children After The Emergence of Covid 19Document6 pagesMaternal Practices Towards Dental Treatment of Primary School Children After The Emergence of Covid 19International Journal of Innovative Science and Research TechnologyNo ratings yet
- JFMPC 2020 TDDocument2 pagesJFMPC 2020 TDTulika WakhlooNo ratings yet
- Pancasila Gigi JurnalDocument12 pagesPancasila Gigi Jurnalandini fitriNo ratings yet
- Challenges and Impact of COVID-19 Lockdown On Indian Optometry Practice: A Survey-Based StudyDocument9 pagesChallenges and Impact of COVID-19 Lockdown On Indian Optometry Practice: A Survey-Based StudyLaura Alvarado BrophyNo ratings yet
- Outpatient Otolaryngology in The Era of COVID-19: A Data-Driven Analysis of Practice PatternsDocument7 pagesOutpatient Otolaryngology in The Era of COVID-19: A Data-Driven Analysis of Practice PatternsMada Dwi HariNo ratings yet
- Ijerph 18 05889Document18 pagesIjerph 18 05889Febri YolandaNo ratings yet
- Knowledge Dental Anxiety and Patient ExpectationsDocument9 pagesKnowledge Dental Anxiety and Patient ExpectationsbenjoscoliNo ratings yet
- 1 s2.0 S1473309920302267 MainDocument2 pages1 s2.0 S1473309920302267 MainMarlo Jules LagunaNo ratings yet
- The Impact of COVID-19 Pandemic On The Academic Performance of Veterinary Medical StudentsDocument8 pagesThe Impact of COVID-19 Pandemic On The Academic Performance of Veterinary Medical StudentsRitam chaturvediNo ratings yet
- A Review of COVID-19 and The Implications For Orthodontic Provision in EnglandDocument8 pagesA Review of COVID-19 and The Implications For Orthodontic Provision in Englanddruzair007No ratings yet
- Ophthalmic Complaints in Face Mask Wearing Prevalence Treatment and Prevention With A Potential Protective Effect Against SARS CoV 2Document14 pagesOphthalmic Complaints in Face Mask Wearing Prevalence Treatment and Prevention With A Potential Protective Effect Against SARS CoV 2Feli FelNo ratings yet
- .Management of The Oral Health of Children During The COVID-19Document6 pages.Management of The Oral Health of Children During The COVID-19Michael PomaNo ratings yet
- Cross Infection 4444Document12 pagesCross Infection 4444khamilatusyNo ratings yet
- Dental Considerations After The Outbreak of 2019 Novel Coronavirus Disease: A Review of LiteratureDocument7 pagesDental Considerations After The Outbreak of 2019 Novel Coronavirus Disease: A Review of Literatureharshita parasharNo ratings yet
- Clinical Endodontic Management During The COVID-19 Pandemic: A Literature Review and Clinical RecommendationsDocument11 pagesClinical Endodontic Management During The COVID-19 Pandemic: A Literature Review and Clinical Recommendationsangel gudiyaNo ratings yet
- Covid 19 Article Dental ImpactDocument10 pagesCovid 19 Article Dental Impactwedad jumaNo ratings yet
- 1 s2.0 S1350946220300720 MainDocument32 pages1 s2.0 S1350946220300720 MainSaba ChavchavadzeNo ratings yet
- How COVID-19 Has Affected DentistryDocument13 pagesHow COVID-19 Has Affected DentistryDeborah AnneNo ratings yet
- Covid 19 ItaliaDocument9 pagesCovid 19 ItaliaSergio Losada AmayaNo ratings yet
- COVID-19-Orthodontic Care During and After The Pandemic: A Narrative ReviewDocument15 pagesCOVID-19-Orthodontic Care During and After The Pandemic: A Narrative ReviewAndreea Andrei AndreeaNo ratings yet
- Incidence of COVID-19 Virus Transmission in Three Dental Offices: A 6-Month Retrospective StudyDocument7 pagesIncidence of COVID-19 Virus Transmission in Three Dental Offices: A 6-Month Retrospective StudyAlexNo ratings yet
- Abbas 2020Document7 pagesAbbas 2020desy purnama sariNo ratings yet
- GJESM Volume 8 Issue 3 Pages 327-338Document12 pagesGJESM Volume 8 Issue 3 Pages 327-338GJESMNo ratings yet
- Index - PHPP Revista&tipo Pdf-Simple&pii S1578219021000603 3Document2 pagesIndex - PHPP Revista&tipo Pdf-Simple&pii S1578219021000603 3Iago GonçalvesNo ratings yet
- HEALTHCARE SERVICE QUALITY AND PATIENT SATISFACTION IN OMANI PUBLIC HOSPITALS THROUGHOUT COVID-19 ERA: AN EMPIRICAL INVESTIGATIONFrom EverandHEALTHCARE SERVICE QUALITY AND PATIENT SATISFACTION IN OMANI PUBLIC HOSPITALS THROUGHOUT COVID-19 ERA: AN EMPIRICAL INVESTIGATIONNo ratings yet
- Where To Find Large Datasets Open To The PublicDocument41 pagesWhere To Find Large Datasets Open To The PublicgeronimlNo ratings yet
- CCNA1 Mod 6Document28 pagesCCNA1 Mod 6KlokanNo ratings yet
- Phantom Turbo 6000Document22 pagesPhantom Turbo 6000Manos LoukianosNo ratings yet
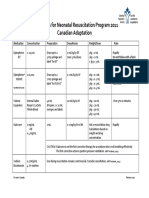
- Medications For Neonatal Resuscitation Program 2011 Canadian AdaptationDocument1 pageMedications For Neonatal Resuscitation Program 2011 Canadian AdaptationrubymayNo ratings yet
- General Definition of Sag and Tension in Electrical Transmission LinesDocument11 pagesGeneral Definition of Sag and Tension in Electrical Transmission Linesdskymaximus67% (3)
- People Vs OandasanDocument2 pagesPeople Vs OandasanAdoha Lei T Blanco100% (1)
- Nihongo Lesson FL 1Document21 pagesNihongo Lesson FL 1Lee MendozaNo ratings yet
- Managed Pressure Drilling Modeling & Simulation (A Case Study)Document8 pagesManaged Pressure Drilling Modeling & Simulation (A Case Study)Mejbahul SarkerNo ratings yet
- Class XII Applied Mathematics 2023-24 (K R Mangalam School)Document7 pagesClass XII Applied Mathematics 2023-24 (K R Mangalam School)GouriJayanNo ratings yet
- जनावरहरूमा फेनबेन्डाजोलको प्रयोग (Use of Fenbendazole in animals)Document17 pagesजनावरहरूमा फेनबेन्डाजोलको प्रयोग (Use of Fenbendazole in animals)Jibachha SahNo ratings yet
- Model QuestionsDocument27 pagesModel Questionskalyan555No ratings yet
- General Information: Location A Location BDocument2 pagesGeneral Information: Location A Location BNikNo ratings yet
- Lubricattng Oil For Marine EnginesDocument5 pagesLubricattng Oil For Marine Enginesemmsh71No ratings yet
- Laporan Kasus (Stroke NHS)Document4 pagesLaporan Kasus (Stroke NHS)keluargacendanaNo ratings yet
- Studying The Performance of Pongamia Biodiesel by Using Nano Partical Fuel AdditivesDocument6 pagesStudying The Performance of Pongamia Biodiesel by Using Nano Partical Fuel Additivessemi1919No ratings yet
- Dynamic Modeling of PMSMDocument10 pagesDynamic Modeling of PMSMHisham Magdi El DeebNo ratings yet
- Case Study CCTV BuildingDocument11 pagesCase Study CCTV BuildingChendra Ling LingNo ratings yet
- RIP Riverbed LabDocument13 pagesRIP Riverbed LabnekaNo ratings yet
- Section A - QuestionsDocument27 pagesSection A - Questionsnek_akhtar87250% (1)
- Multimedia Chapter 1 and 2Document22 pagesMultimedia Chapter 1 and 2tsegab bekeleNo ratings yet
- Game Master's Kit: An Accessory For The Dragon Age RPGDocument32 pagesGame Master's Kit: An Accessory For The Dragon Age RPGLuiz Fernando Rodrigues CarrijoNo ratings yet
- PMEC Flash CardsDocument17 pagesPMEC Flash CardsHariyantoNo ratings yet
- CSA Standard W178.2-01: Certification of Welding InspectorsDocument2 pagesCSA Standard W178.2-01: Certification of Welding InspectorsramalingamNo ratings yet
- DLL WK 10 LC 171819Document14 pagesDLL WK 10 LC 171819Regiel Guiang ArnibalNo ratings yet
- Japan TechnologyDocument4 pagesJapan TechnologyMa Leonora SorianoNo ratings yet
- Actuator DX PDFDocument6 pagesActuator DX PDFFelix Enrique MoratayaNo ratings yet
- CascadeTEK Vacuum Oven ManualDocument49 pagesCascadeTEK Vacuum Oven ManualCascade TEKNo ratings yet
- 72.61.00.045 26-MAR-2020 08-DEC-2021 Closed A319-100N, A320-200N, A321-200N, A321-200NX, A321-200NY 72-61 Iae LLC Pratt & Whitney TFU UpdateDocument9 pages72.61.00.045 26-MAR-2020 08-DEC-2021 Closed A319-100N, A320-200N, A321-200N, A321-200NX, A321-200NY 72-61 Iae LLC Pratt & Whitney TFU UpdatejivomirNo ratings yet
- BSN1-2 Lab Activity 2.2 Proteins DenaturationDocument3 pagesBSN1-2 Lab Activity 2.2 Proteins DenaturationCristine EchaveNo ratings yet