Professional Documents
Culture Documents
Slutsky 2010
Slutsky 2010
Uploaded by
Al VlaovicOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Slutsky 2010
Slutsky 2010
Uploaded by
Al VlaovicCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
the Massachusetts, New Hampshire, and Vermont kemia in Children Produced by Folic Acid An-
Medical Societies, so the name was changed back tagonist, 4-Aminopteroyl-Glutamic Acid (Amin-
to the New England Journal of Medicine. opterin)” by Sidney Farber et al.11 The most widely
The early pages of the Journal contain anec- cited review article appears in 1967 in five parts:
dotes of cases, new treatments of diseases, and “Fat Transport in Lipoproteins — An Integrated
reprints of lectures and talks given by eminent Approach to Mechanisms and Disorders” by
physicians in New England and Europe, as well Fredrickson et al.12 In this era, there are the
as news of physicians in the area and even local philosophical insights of Lewis Thomas, pub-
meteorologic summaries and a long treatise in lished as Notes of a Biology-Watcher, and the in-
1837 on the climate of Santa Cruz (now St. ternational perspective consisted primarily of
Croix).2 This early archive includes the classic John Lister’s reports called By the London Post.
1846 description by H.J. Bigelow of the first use The final volume in the Journal’s archive in-
of ether, “Insensibility during Surgical Opera- cludes the news-making, research-changing re-
tions Produced by Inhalation.”3 One finds every- port from the Physicians’ Health Study on the
thing from “On a New Method of Determining use of aspirin to prevent myocardial infarction.13
the Quantity of Urea in the Urine”4 to “The Pro- We hope that readers will find the new digital
duction and Management of Bees”5 (both from archive useful and informative.
1854) and from “Salicylic Acid in Rheuma- Disclosure forms provided by the authors are available with
tism”6 to a grisly treatise on “Hanging as a Fine the full text of this article at NEJM.org.
Art”7 (both 1876). This unfiltered historical rec-
1. Warren J. Remarks on angina pectoris. N Engl J Med Surg
ord of American medicine also contains a sur- 1812;1:1-11.
prising number of entries in the early 19th cen- 2. Tuckerman J. Observations on the climate, &c. of Santa Cruz.
tury about “alleged malpractice.” In the issue of Boston Med Surg J 1837;16:357-64, 373-9, 395-402.
3. Bigelow HJ. Insensibility during surgical operations pro-
April 13, 1865, the day before Abraham Lincoln duced by inhalation. Boston Med Surg J 1846;35:309-17.
was shot, one finds a report about the sudden 4. Draper JW. On a new method of determining the quantity of
death of a healthy, robust 19-year-old man. The urea in the urine. Boston Med Surg J 1854;50:49-50.
5. The production and management of bees. Boston Med Surg J
physicians conscientiously review the difficult 1854;50:15-7.
details, trying to understand whether this death 6. Towle SK. Salicylic acid in acute rheumatism. Boston Med
was because of a congenital ventricular septal de- Surg J 1876;94:593-5.
7. Hanging as a fine art. Boston Med Surg J 1876;94:197-8.
fect or rupture of the interventricular septum.8 8. Jackson JBS. Congenital interventricular opening of the heart
From the first issue of the more recent archive in an adult of robust health; or rupture of the septum two months
on January 4, 1945, one sees examples of the before death? Boston Med Surg J 1865;72:209-11.
9. D’Agati VC, Marangoni BA. The Waterhouse–Friderichsen
evolution of modern medicine, such as in a schol- syndrome. N Engl J Med 1945;232:1-7.
arly article on the Waterhouse–Friderichsen syn 10. Welcker ML. The porphyrins. N Engl J Med 1945;232:11-9.
drome, with attempts to understand the causa- 11. Farber S, Diamond LK, Mercer RD, Sylvester RF Jr, Wolff JA.
Temporary remissions in acute leukemia in children produced by
tive agent in this decimating physiological folic acid antagonist, 4-aminopteroyl-glutamic acid (aminopterin).
cascade.9 In the same issue, there is a compre- N Engl J Med 1948;238:787-93.
hensive review article on porphyrin metabolism, 12. Fredrickson DS, Levy RI, Lees RS. Fat transport in lipo
proteins — an integrated approach to mechanisms and disor-
which begins by noting that the average physi- ders. N Engl J Med 1967;276:34-44, 94-103, 148-56, 215-25, 273-
cian sees the topic as “bewilderingly complex.”10 81.
(Some things do not change.) In 1948, there is 13. Steering Committee of the Physicians’ Health Study Research
Group. Final report on the aspirin component of the ongoing
the early report with some hope about a terrible Physicians’ Health Study. N Engl J Med 1989;321:129-35.
disease: “Temporary Remissions in Acute Leu- Copyright © 2010 Massachusetts Medical Society.
Neuromuscular Blocking Agents in ARDS
Arthur S. Slutsky, M.D.
In this issue of the Journal, Papazian and col- with severe, early acute respiratory distress syn-
leagues1 present intriguing results of their study drome (ARDS). The investigators randomly as-
examining neuromuscular blockade in patients signed 340 patients to receive the neuromuscular
1176 n engl j med 363;12 nejm.org september 16, 2010
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
editorials
blocking agent cisatracurium or placebo for a a direct antiinflammatory effect, though this
period of 48 hours. Both groups underwent me- seems unlikely to be the mechanism of death,
chanical ventilation according to a lung-protec- given the lack of effect on mortality of very potent
tive strategy previously shown to decrease mor- antiinflammatory agents in previous studies.5
tality.2 Both the adjusted 90-day survival rate Neuromuscular blocking agents could decrease
and time off the ventilator were greater in the the oxygen consumption of respiratory and other
cisatracurium group as compared with the pla- muscles, reducing cardiac output, increasing the
cebo group. mixed venous partial pressure of oxygen, and in-
ARDS is an inflammatory disease character- creasing the partial pressure of arterial oxygen.
ized by pulmonary edema, stiff lungs, and hypox In addition, ventilation–perfusion relationships
emia.3 It affects approximately 140,000 patients may be improved (or worsened), depending on
annually in the United States and is associated the distribution of lung injury and the effect that
with a mortality estimated at over 40%.4 Despite regional activation of respiratory muscles has on
intense research, there are no specific pharma- the distribution of ventilation and perfusion be-
cologic therapies proven to decrease this mor- fore paralysis. However, improved oxygenation
tality.5 The only confirmed therapy is a lung- is unlikely to be the major explanation for the
protective strategy involving the use of relatively positive results of Papazian and coworkers, since
small tidal volumes with limitation of the end- gas-exchange measurements were essentially the
inspiratory lung stretch.2 same in the two groups during the period of
The study by Papazian and coworkers can be administration of the neuromuscular blocking
viewed as a step back from a developing para- agent.
digm in critical care. Over the past decade, re- By paralyzing respiratory muscles, neuromus-
flecting increasing recognition of the iatrogenic cular blocking agents may indirectly minimize
consequences of many therapies, there has been various manifestations of ventilator-induced lung
a shift toward “less intervention.” Lung-protective injury,12 including “atelectrauma” (injury due to
ventilation is an example of this minimalist phi- repetitive opening and closing of lung units),
losophy, with a focus on less ventilation to pro- barotrauma (gross air leaks), volutrauma (in-
tect the lung from ventilator-induced lung injury, creased alveolar-capillary permeability due to
rather than more ventilation to maintain normal overdistention of the lung), and biotrauma (re-
blood gas levels. Other examples of the minimal- lease of mediators in the lung and translocation
ist approach include the administration of fewer of these mediators into the systemic circulation).
transfusions,6 less bed rest,7 fewer intubations,8 By preventing active expiration, neuromuscular
and less sedation.9 Until now, neuromuscular blocking agents may allow positive end-expira-
blocking agents have largely fallen under this tory pressures to be better controlled, resulting
“less-is-more” strategy. Although neuromuscular in decreased “atelectrauma.” Optimal implemen-
blocking agents are used in more than 25% of tation of mechanical ventilation can be complex,
patients with ARDS, most authorities recommend owing to difficulty in synchronizing the breaths
minimizing their use, largely because of concerns delivered by the ventilator and the patient’s in-
about long-term muscle weakness. herent respiratory drive. Pharmacologically par-
The study by Papazian and colleagues makes alyzing the patient and administering “con-
us reevaluate this philosophy. Of course, their trolled ventilation” prevents patient–ventilator
results need to be replicated, but assuming they dyssynchrony, including autotriggering, stops
are robust, it is interesting to speculate on the the patient from “fighting” the ventilator, and
possible mechanisms conferring the beneficial could minimize the risk of volutrauma and
effects. The two major causes of death in pa- barotrauma.
tients with ARDS are multiorgan failure10 sec- The potentially decreased oxygen consump-
ondary to infection, sepsis, hemodynamic com- tion after administration of neuromuscular block-
promise, or ventilator-induced lung injury11; and ing agents could decrease the ventilatory demand
severe hypoxemia.10 (and thus the risk of ventilator-induced lung in-
Neuromuscular blocking agents such as cis- jury due to a higher minute ventilation).13 The
atracurium may affect these risk factors through use of blocking agents would also minimize the
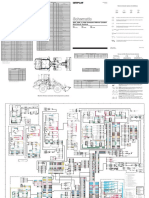
interrelated mechanisms (Fig. 1). They may have increase in minute ventilation due to the height-
n engl j med 363;12 nejm.org september 16, 2010 1177
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Before paralysis Ventilator-induced lung injury ↑ Mediators
Respiratory cycle (e.g., interleukin-8)
O2 molecules
Patient Alveolus
Biotrauma Surfactant
Translocation of
Dyssynchrony mediators from alveolar
Pressure
generated space to circulation
Dyssynchrony
Ventilator Barotrauma
↓ Venous
↑ Injury due ↑ Alveolar- PO2 ↓ Arterial
to ↑ pulmonary capillary PO2
blood flow permeability
Lung
volume
↑ Lung volume
Active ↑ Lung volume
expiration Dysfunction O2 used
↓ Lung volume or organ failure for muscle
due to: contraction
Increased tidal volume secondary to Volutrauma
↓ Arterial PO2
increased respiratory drive due to: Vital organs Muscles
↓ Blood flow
↓ Arterial PO2 ↑ Mediators
Lung reflexes
Anxiety
Permissive hypercapnia
Severely
reduced
venous PO2
“Atelectrauma” To lungs
After paralysis Less ventilator-induced lung injury ↓ Mediators
Respiratory cycle (e.g., interleukin-8)
Patient No pressure signal O2 molecules
Less
No dyssynchrony biotrauma
Less translocation of
Pressure mediators from alveolar
generated space to circulation
Ventilator Less barotrauma
Possible
• •
↓ Injury due ↑ Venous PO2 ↑V/Q
to ↓ pulmonary
blood flow
↑ Arterial
Lower tidal PO2
Direct anti-
volume
inflammatory
Lung effect of NMBA
volume
Less O2
used by
Less volutrauma Less muscles
No active expiration
organ
Vital organs Muscles
dysfunction
and
failure
Higher
venous
PO2
To lungs
Less “atelectrauma”
COLOR FIGURE
Draft 7 8/31/10
Author Slutsky
Fig # 1
1178 n engl j med 363;12 nejm.org september 16, 2010 Title
The New England Journal of Medicine ME
Downloaded from nejm.org on November 28, 2013. For personal use only. No other uses without
DE permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved. Artist Knoper and minions
AUTHOR PLEASE NOTE:
editorials
neuromuscular blocking agents. In the study by
Figure 1 (facing page). Possible Mechanisms by Which
Neuromuscular Blocking Agents (NMBAs) Might Lead Papazian and colleagues, the Kaplan–Meier curves
to Improved Survival in Patients with the Acute for the cisatracurium group and the placebo group
Respiratory Distress Syndrome (ARDS). started to separate only after approximately 12
Respiratory physiological features of a patient with days regarding the probability of breathing with-
ARDS are illustrated before (top) and after (bottom) out assistance and only after approximately 18
paralysis induced with the use of NMBAs. Before paraly-
days regarding mortality, even though the study
sis, increased respiratory drive from multiple causes can
lead to increased tidal volumes, active exhalation, and intervention was limited to the first 48 hours.
patient–ventilator asynchrony, all of which can poten- Biotrauma has also been suggested to explain
tially worsen various forms of ventilator-induced lung the decrease in mortality of the Acute Respira-
injury. In addition, muscle activation may divert blood tory Distress Syndrome Network (ARDSNet) study
flow away from vital organs and lead to a lower mixed
involving the lung-protective strategy.2
venous partial pressure of oxygen (PO2). These mecha-
nisms may lead to increased organ dysfunction and ulti- It is unclear from the present study which of
mately death. After paralysis, the administered NMBAs these (or other) mechanisms might explain the
prevent patient-initiated generation of high and low benefit from neuromuscular blockade. Variables
lung volumes and also prevent active expiration, allow- commonly used to assess the propensity for
ing for better lung-protective ventilation and less venti-
ventilator-induced lung injury (e.g., plateau pres-
lator-induced lung injury. Ventilator-induced lung injury
may also be lessened by less pulmonary blood flow sures and tidal volumes) did not differ signifi-
due to decreased oxygen consumption. NMBAs may cantly between the cisatracurium group and the
also indirectly improve arterial oxygenation by decreas- placebo group, a result that argues against an
ing blood flow to active muscle groups (because of de- effect on ventilator-induced lung injury as the
creased oxygen requirements) and by improving the
̇ major mechanism. Nonetheless, significantly
distribution of ventilation relative to perfusion (/Q).
(Arterial PO2 may also be decreased through this mech- more patients in the placebo group than in the
anism if /Q̇ is worsened.) Finally, NMBAs may have a cisatracurium group received open-label cisatra-
direct antiinflammatory effect. The relative effect of curium, presumably because they had a plateau
NMBAs on many of these mechanisms depends on the pressure of more than 32 cm of water and were
state of muscle activation before paralysis, which is de-
thus at greater risk for ventilator-induced lung
pendent on a number of factors, including the patient’s
level of sedation. injury. Most importantly, the placebo group had
a significantly higher incidence of barotrauma,
suggesting that abrogation of ventilator-induced
ened respiratory drive associated with permissive lung injury may have been central to the benefi-
hypercapnia, an approach often used as part of cial effects.
lung-protective strategies. Finally, the potential This study raises many unanswered questions
decrease in cardiac output (and decreased pul- in addition to those concerning putative mecha-
monary blood flow) associated with reduced oxy- nisms of action. What is the optimal duration of
gen consumption could also mitigate ventilator- use of neuromuscular blocking agents? Is the
induced lung injury.14 observed benefit specific to cisatracurium or
These respiratory mechanisms could lead to a shared within the drug class? Would very heavy
decrease in the release of pulmonary and system- sedation produce results similar to those report-
ic mediators (i.e., decreased biotrauma) and hence ed? Why does the beneficial effect appear to be
could minimize the development of organ dys- present only in patients with more severe hypox-
function.11 This hypothesis is in keeping with a emia? The answers to these and other questions
previous study showing that administration of will ultimately determine whether, how, and
cisatracurium over a 48-hour period was associat- when neuromuscular blocking agents are used to
ed with decreasing levels of interleukin-8 in bron- improve the outcomes of patients with ARDS.
choalveolar-lavage fluid and decreasing levels of Disclosure forms provided by the author are available with the
full text of this article at NEJM.org.
interleukin-6 and interleukin-8 in serum.15 On-
going cytokine release, related to the biotrauma From the Keenan Research Center at the Li Ka Shing Knowledge
Institute of St. Michael’s Hospital, the Interdepartmental Divi-
mechanism, can occur for many days and might sion of Critical Care Medicine, and the Department of Medi-
explain the time lag in the beneficial effects of cine, University of Toronto — all in Toronto.
n engl j med 363;12 nejm.org september 16, 2010 1179
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
1. Papazian L, Forel J-M, Gacouin A, et al. Neuromuscular v entilation in acute respiratory failure. Crit Care Med 2007;35:
blockers in early acute respiratory distress syndrome. N Engl J 2402-7.
Med 2010;363:1107-16. 9. Wunsch H, Kress JP. A new era for sedation in ICU patients.
2. The Acute Respiratory Distress Syndrome Network. Ventila- JAMA 2009;301:542-4.
tion with lower tidal volumes as compared with traditional tidal 10. Stapleton RD, Wang BM, Hudson LD, Rubenfeld GD,
volumes for acute lung injury and the acute respiratory distress Caldwell ES, Steinberg KP. Causes and timing of death in pa-
syndrome. N Engl J Med 2000;342:1301-8. tients with ARDS. Chest 2005;128:525-32.
3. Ware LB, Matthay MA. The acute respiratory distress syn- 11. Slutsky AS, Tremblay LN. Multiple system organ failure: is
drome. N Engl J Med 2000;342:1334-49. mechanical ventilation a contributing factor? Am J Respir Crit
4. Rubenfeld GD, Caldwell E, Peabody E, et al. Incidence and Care Med 1998;157:1721-5.
outcomes of acute lung injury. N Engl J Med 2005;353:1685- 12. Tremblay LN, Slutsky AS. Ventilator-induced lung injury:
93. from the bench to the bedside. Intensive Care Med 2006;32:
5. Raghavendran K, Pryhuber GS, Chess PR, Davidson BA, 24-33.
Knight PR, Notter RH. Pharmacotherapy of acute lung injury 13. Marini JJ. Early phase of lung-protective ventilation: a place
and acute respiratory distress syndrome. Curr Med Chem 2008; for paralytics? Crit Care Med 2006;34:2851-3.
15:1911-24. 14. Broccard AF, Hotchkiss JR, Kuwayama N, et al. Conse-
6. Hébert PC, Wells G, Blajchman MA, et al. A multicenter, quences of vascular flow on lung injury induced by mechanical
randomized, controlled clinical trial of transfusion require- ventilation. Am J Respir Crit Care Med 1998;157:1935-42.
ments in critical care. N Engl J Med 1999;340:409-17. [Erratum, 15. Forel JM, Roch A, Marin V, et al. Neuromuscular blocking
N Engl J Med 1999;340:1056.] agents decrease inflammatory response in patients presenting
7. Kress JP. Clinical trials of early mobilization of critically ill with acute respiratory distress syndrome. Crit Care Med 2006;34:
patients. Crit Care Med 2009;37:Suppl:S442-S447. 2749-57.
8. Hill NS, Brennan J, Garpestad E, Nava S. Noninvasive Copyright © 2010 Massachusetts Medical Society.
From Palliation to Targeted Therapy in Myelofibrosis
Alessandro M. Vannucchi, M.D.
Myelofibrosis is a very debilitating chronic myelo benefits in myelofibrosis. It is hoped that the
proliferative neoplasm.1 It may be primary or Controlled Myelofibrosis Study with Oral JAK
develop late in the course of essential thrombo- Inhibitor Treatment (COMFORT) trials, two on-
cythemia or polycythemia vera, the two most going phase 3 studies involving either patients
common and benign myeloproliferative neo- receiving placebo (COMFORT-I; ClinicalTrials.
plasms. Patients with myelofibrosis have short gov number, NCT00952289) or a control group
ened survival and a reduced quality of life. The of patients receiving “best-available therapy”
current treatment is palliative and aimed at allevi- (COMFORT-II; NCT00934544), will strengthen
ating symptoms due to splenomegaly, controlling our enthusiasm. Furthermore, according to a
myeloproliferation, and improving anemia and preliminary report of a phase 2 trial (Study to
other cytopenias. Determine the Safety and Efficacy of INCB018424
In this issue of the Journal, Verstovsek et al. in Patients with Polycythemia Vera or Essential
report on the results of a phase 1−2 trial of an Thrombocythemia; NCT00726232), the drug also
oral Janus kinase 1 (JAK1) and Janus kinase 2 could have considerable efficacy in advanced
(JAK2) inhibitor, INCB018424, in advanced my- polycythemia vera or essential thrombocythemia
elofibrosis.2 The majority of the patients who that is refractory to hydroxyurea.3
received INCB018424 had prompt and durable Clinical development of JAK inhibitors for
improvement in constitutional symptoms and myeloproliferative neoplasms closely followed the
overall performance status. In more than half discovery of a V617F point mutation in the JAK2
the patients, the size of the enlarged spleen was gene in more than 90% of patients with poly-
reduced by at least 50%, with a reduction of ab- cythemia vera and 60% of patients with primary
dominal discomfort and gain in body weight. myelofibrosis or essential thrombocythemia.4 The
However, only 14% of the patients with anemia mutation results in constitutive kinase activity
became transfusion-independent, and new-onset of JAK2, a member of a family of receptor-asso-
anemia developed in a similar proportion of pa- ciated tyrosine kinases that transduce signals
tients. Thus, the results of this trial point to originating from numerous cytokine receptors
JAK1 and JAK2 inhibition as a new therapeutic (Fig. 1).5 The same spectrum of signaling abnor-
intervention associated with meaningful clinical malities and clinical phenotypes may be attributed
1180 n engl j med 363;12 nejm.org september 16, 2010
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2013. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
You might also like
- Apixaban For Stroke Prevention in Subclinical AFDocument11 pagesApixaban For Stroke Prevention in Subclinical AFalaahossam591No ratings yet
- Misinterpretation of TasawwufDocument260 pagesMisinterpretation of TasawwufSpirituality Should Be LivedNo ratings yet
- Medicinus Maret 2018 PDFDocument25 pagesMedicinus Maret 2018 PDFIsdiana IsmailNo ratings yet
- Pulmonary Hypertension: A Patient's Survival Guide: Fifth Edition, 2013 RevisionFrom EverandPulmonary Hypertension: A Patient's Survival Guide: Fifth Edition, 2013 RevisionRating: 5 out of 5 stars5/5 (1)
- 902, 906, & 908 Compact Wheel Loader Electrical System: Machine Harness Connector and Component LocationsDocument2 pages902, 906, & 908 Compact Wheel Loader Electrical System: Machine Harness Connector and Component Locationsait mimouneNo ratings yet
- Stat NotesDocument40 pagesStat Notesssckp86No ratings yet
- Biochemistry of Oxidative Stress - Physiopathology and Clinical Aspects (PDFDrive)Document448 pagesBiochemistry of Oxidative Stress - Physiopathology and Clinical Aspects (PDFDrive)Vitoria LimaNo ratings yet
- ASpirin Target KerjaDocument15 pagesASpirin Target KerjaANISA RACHMITA ARIANTI 2020No ratings yet
- Medical Management of Missed Abortion and Anembryonic PregnancyDocument2 pagesMedical Management of Missed Abortion and Anembryonic PregnancyIriamana Liasyarah MarudinNo ratings yet
- Section: of The History of MedicineDocument10 pagesSection: of The History of MedicineaceNo ratings yet
- PIIS0012369216529419Document3 pagesPIIS0012369216529419puskesmassedadap.2023No ratings yet
- Nejmcpc 1909628Document11 pagesNejmcpc 1909628MS R.No ratings yet
- Jurnal OnlineDocument5 pagesJurnal OnlineWireifnitedNo ratings yet
- Drug Information HandbookDocument2 pagesDrug Information HandbookdiahNo ratings yet
- A History of Pulmonary Embolism and Deep Venous ThrombosisDocument17 pagesA History of Pulmonary Embolism and Deep Venous ThrombosisAleksVaReNo ratings yet
- Brmedj03772 0032aDocument1 pageBrmedj03772 0032afpm5948No ratings yet
- ClassicsDocument2 pagesClassicsIndra Budi PermanaNo ratings yet
- Improving Outcomes in Heart Failure: A Personal PerspectiveDocument4 pagesImproving Outcomes in Heart Failure: A Personal PerspectiveyeinisehNo ratings yet
- Receptive SubstancesDocument22 pagesReceptive SubstancesDaniel ChaguenNo ratings yet
- Brjgenprac00016 0058bDocument2 pagesBrjgenprac00016 0058bM EhabNo ratings yet
- Drug Information HandbookDocument2 pagesDrug Information HandbookSarah NurhalizaNo ratings yet
- DR Eric Brestel's Sep 5 2000 Letter To EditorDocument2 pagesDR Eric Brestel's Sep 5 2000 Letter To EditorRobert Davidson, M.D., Ph.D.No ratings yet
- Glutathione Peroxidase 1 Activity and Cardiovascular Events in Patients With Coronary Artery DiseaseDocument9 pagesGlutathione Peroxidase 1 Activity and Cardiovascular Events in Patients With Coronary Artery Diseaseapi-26034055No ratings yet
- Fuller Albright-Primul Articol de HPPDocument2 pagesFuller Albright-Primul Articol de HPPadelinaNo ratings yet
- Coronary Heart Disease and Physical ActivityDocument12 pagesCoronary Heart Disease and Physical ActivityÁngelNo ratings yet
- Ketamine and Intracranial Pressure: No Contraindication Except HydrocephalusDocument3 pagesKetamine and Intracranial Pressure: No Contraindication Except Hydrocephaluslidwina143No ratings yet
- Ashtma Timeline T2Document21 pagesAshtma Timeline T2ISABEL SOFIA CABARCAS COGOLLONo ratings yet
- Trauma Brain Injury 2Document2 pagesTrauma Brain Injury 2lala putriNo ratings yet
- Pleural Disease During Treatment With Bromocriptine in Patients Previously Exposed To AsbestosDocument6 pagesPleural Disease During Treatment With Bromocriptine in Patients Previously Exposed To Asbestosgarberer1No ratings yet
- PR 1993752Document4 pagesPR 1993752Verónica UriósteguiNo ratings yet
- Spontaneous Breathing During Mechanical Ventilation: A Two-Edged SwordDocument2 pagesSpontaneous Breathing During Mechanical Ventilation: A Two-Edged SwordKhanh Ha NguyenNo ratings yet
- PG 0063Document1 pagePG 0063Leah TigersNo ratings yet
- Unusual Cause of Neonatal Cyanosis: Journal of The Saudi Heart AssociationDocument3 pagesUnusual Cause of Neonatal Cyanosis: Journal of The Saudi Heart AssociationfikaNo ratings yet
- Treatment of Bronchospasm During Anesthesia .28Document4 pagesTreatment of Bronchospasm During Anesthesia .28Anish H DaveNo ratings yet
- Iron Overload and Hepatic Fibrosis in Response - JMDocument1 pageIron Overload and Hepatic Fibrosis in Response - JMBastomy EkaNo ratings yet
- MC Sparr On 2016Document10 pagesMC Sparr On 2016Matias FlammNo ratings yet
- Drug Information HandbookDocument1 pageDrug Information Handbookwulansari nurjanahNo ratings yet
- Aroxysmal Atrial Tachycardia With Atrioventricular BlockDocument7 pagesAroxysmal Atrial Tachycardia With Atrioventricular BlockDenisseRangelNo ratings yet
- New Classification of Stroke: Preliminary Communication: Mmol/lDocument3 pagesNew Classification of Stroke: Preliminary Communication: Mmol/lBella CoritaNo ratings yet
- Bronchial Asthma Research PaperDocument6 pagesBronchial Asthma Research Paperniisexgkf100% (1)
- Caso Clinico Fiebre GlandularDocument3 pagesCaso Clinico Fiebre GlandularJoana L. BauNo ratings yet
- Aair 2 165Document7 pagesAair 2 165HeheebNo ratings yet
- The Cold Water Cure As Practised by Vincent PriessnitzDocument144 pagesThe Cold Water Cure As Practised by Vincent PriessnitzDaz100% (1)
- Overview of Common Causes of Chronic Cough: ACCP Evidence-Based Clinical Practice GuidelinesDocument4 pagesOverview of Common Causes of Chronic Cough: ACCP Evidence-Based Clinical Practice GuidelineschuckyonfireNo ratings yet
- ACE Inhibitors and Abdominal Aortic AneurysmDocument2 pagesACE Inhibitors and Abdominal Aortic Aneurysmvfd08051996No ratings yet
- Penting PIIS0016508597004976Document5 pagesPenting PIIS0016508597004976afifahridhahumairahhNo ratings yet
- Prosiding Pertemuan IlmiahDocument5 pagesProsiding Pertemuan IlmiahVic CullundNo ratings yet
- Double Blind Evaluation of Verapamil, Propranolol and Isosorbide Dinitrate Against A Placebo in The Treatment of Angina PectorisDocument4 pagesDouble Blind Evaluation of Verapamil, Propranolol and Isosorbide Dinitrate Against A Placebo in The Treatment of Angina PectorisLoverz BeebzNo ratings yet
- Should We Question If Something Works Just Because We Don't Know How It Works?Document2 pagesShould We Question If Something Works Just Because We Don't Know How It Works?Liga Medicina InternaNo ratings yet
- E Resp MedDocument2,401 pagesE Resp MedbtaleraNo ratings yet
- Thorax00020 0093Document11 pagesThorax00020 0093Hario Tri HendrokoNo ratings yet
- Brmedj03163 0034Document4 pagesBrmedj03163 0034stevenburrow06No ratings yet
- Jclinpath00023 0077bDocument2 pagesJclinpath00023 0077bChyntia D. RahadiaNo ratings yet
- 527 FullDocument2 pages527 FullRadina RusevaNo ratings yet
- 1. !!!prac. СPRDocument55 pages1. !!!prac. СPRtop theNo ratings yet
- Bedell (1958)Document12 pagesBedell (1958)perceptive.wiseNo ratings yet
- Respiratory Effects of Amyotrophic Lateral Sclerosis, Problems and SolutionsDocument14 pagesRespiratory Effects of Amyotrophic Lateral Sclerosis, Problems and SolutionsMarcelaNo ratings yet
- Tablet 2 PDFDocument64 pagesTablet 2 PDFmaulida hasanahNo ratings yet
- Cardiovascular Eponymic Signs: Diagnostic Skills Applied During the Physical ExaminationFrom EverandCardiovascular Eponymic Signs: Diagnostic Skills Applied During the Physical ExaminationNo ratings yet
- The Pituitary Gland, Volume 1: Anterior PituitaryFrom EverandThe Pituitary Gland, Volume 1: Anterior PituitaryG. W. HarrisNo ratings yet
- Physick to Physiology: Tales from an Oxford Life in MedicineFrom EverandPhysick to Physiology: Tales from an Oxford Life in MedicineNo ratings yet
- BS 03900 0 2010Document26 pagesBS 03900 0 2010selvaNo ratings yet
- 3b Domestic Water Meter Installation in Meter Room GuidelinesDocument10 pages3b Domestic Water Meter Installation in Meter Room GuidelinesVinish HARIDAS NAIRNo ratings yet
- Calibration Curve Between Pressure Drop and Mass Flow RateDocument2 pagesCalibration Curve Between Pressure Drop and Mass Flow RateMikail IsmailNo ratings yet
- Pia Calabarzon 7 Prs (April 12,15, 2013), Dispatch For April 15, 2013 (Monday)Document34 pagesPia Calabarzon 7 Prs (April 12,15, 2013), Dispatch For April 15, 2013 (Monday)Pia QuezonNo ratings yet
- Polynomial FunctionDocument36 pagesPolynomial FunctionfaithreignNo ratings yet
- To Study Well Design Aspects in HPHT EnvironmentDocument40 pagesTo Study Well Design Aspects in HPHT Environmentnikhil_barshettiwat100% (1)
- User S Manual Bedienungsanleitung: Version 1.0 October 1998Document32 pagesUser S Manual Bedienungsanleitung: Version 1.0 October 1998Ojit QuizonNo ratings yet
- Homework 2 SolutionDocument5 pagesHomework 2 SolutiongretabunciNo ratings yet
- Tutorial L298N Driver MotorDocument5 pagesTutorial L298N Driver MotorHairul Anam SNo ratings yet
- Australian Standard: Roof TilesDocument10 pagesAustralian Standard: Roof TilesVeetoau Joseph100% (1)
- Maun StreamDocument22 pagesMaun StreamPrasanth ReddyNo ratings yet
- Life On MarsDocument3 pagesLife On MarsSahar SmNo ratings yet
- Substation Construction and CommissioningDocument83 pagesSubstation Construction and CommissioningShung Tak ChanNo ratings yet
- Mathematics ECAT (Sir Nasim Zulfiqar) - 1Document134 pagesMathematics ECAT (Sir Nasim Zulfiqar) - 1AYESH qureshiNo ratings yet
- Lesson 6 Solving Rational Equations and InequalitiesDocument80 pagesLesson 6 Solving Rational Equations and InequalitiesCarbon Copy0% (1)
- Hydrodynamic Characteristics of The Kort-Nozzle Propeller by Different Turbulence ModelsDocument4 pagesHydrodynamic Characteristics of The Kort-Nozzle Propeller by Different Turbulence ModelstafocanNo ratings yet
- GO Price - escalation.GO - Ms.124.2007Document3 pagesGO Price - escalation.GO - Ms.124.2007hussainNo ratings yet
- Ielts Writing Tu NoiDocument7 pagesIelts Writing Tu NoiQuang Anh TốngNo ratings yet
- Drugs For Chemical EngineeringDocument34 pagesDrugs For Chemical Engineeringshivakumar hrNo ratings yet
- Techniques For Collection, Isolation and Preservation of MicroorganismsDocument42 pagesTechniques For Collection, Isolation and Preservation of Microorganismsaziskf100% (2)
- Lung Sounds Auscultation - 1Document3 pagesLung Sounds Auscultation - 1George BarajazNo ratings yet
- 2010 PriusDocument5 pages2010 PriusNext Day Design -Glassco Global LLCNo ratings yet
- FMEDA E3 ModulevelDocument21 pagesFMEDA E3 ModulevelRonny AjaNo ratings yet
- Indra Motion MLC - Trainning Manual PDFDocument36 pagesIndra Motion MLC - Trainning Manual PDFjorfleitasNo ratings yet
- Singer 291U1, U3Document46 pagesSinger 291U1, U3Datum VivelacriqueNo ratings yet
- Aquaculture Aeration ModulesDocument7 pagesAquaculture Aeration ModulesecosafeNo ratings yet
- 33 1rv18cv119 Umar BashirDocument10 pages33 1rv18cv119 Umar BashirUMARNo ratings yet
- Forensic Syllabus@Document6 pagesForensic Syllabus@YocobSamandrewsNo ratings yet