Professional Documents
Culture Documents
Epilepsy in Children 2
Epilepsy in Children 2
Uploaded by
Another 74Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Epilepsy in Children 2
Epilepsy in Children 2
Uploaded by
Another 74Copyright:
Available Formats
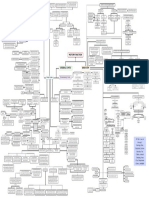
1.
Motor activity is the most important symptom, tonic or clonic tend to involve the
face, neck and extremities. Versive seizures consisting of head turning and conjugate
eye movements are particularly common
2. No automatisms
Uses of EEG in epilepsy:
1. Demonstration of paroxysmal discharge on EEG 3. Positive aura (chest discomfort, headache), may be the only manifestation of the
Focal aware
during a clinical seizure is diagnostic of epilepsy. seizure.
4. The average seizure persists for 10–20 sec. Patient is conscious and mey verbalize
2. A normal EEG dose not exclude the diagnosis of during the seizure. No post ictal phenomenon
epilepsy, because the interictal recording is normal in
about 40% of patient. 5. The EEG may show spikes or sharp waves unilaterally or bilaterally or a multifocal
spike pattern.
3. Activation procedure such as hyperventilation, eye 1. Brief blank stare or a sudden cessation or pause in activity.
closure, photic stimulation and sleep deprivation
may increase the positive yield. -In infants: Alimentary automatisms, including lip smacking,
chewing, swallowing, and excessive salivation.
2. Automatisms are a common feature of focal unaware seizure in infants and children, 50–75% of cases -In older children: semi-purposeful, incoordinated, and
(increase with age). Automatisms develop after the loss of consciousness and may persist into the unplanned gestural automatisms, including picking and pulling
postictal phase at clothing or bedsheets, rubbing or caressing objects and
1. Usually begin between the ages of 4 and 8 mo and are characterized by brief
walking or running in a nondirective, repetitive and often fearful
symmetric contractions of the neck, trunk, and extremities.
fashion.
1. Flexor spasms: occur in clusters or volleys and consist of sudden flexion of the neck,
arms, and legs onto the trunk. 3. With or without an aura. An aura: unpleasant feelings, epigastric discomfort, or fear, the presence of
Focal unaware an aura always indicates a focal onset of the seizure.
2. Extensor spasms: produce extension of the trunk and extremities and are
the least common form of infantile spasm. 2. Types Focal 40% of
4. The average duration of focal unaware seizure is 1–2 min. The aura is usually followed by impaired
3. Mixed infantile spasms: consisting of flexion in some volleys and extension in
childhood seizures consciousness or the onset may start with an impaired state of consciousness.
others, is the most common type of infantile spasm.
In those with normal routine interictal
1. Cryptogenic (idiopathic): account for 10–20% of cases. EEG we use the following:
5. EEG may be able to identify the abnormal event in 80% but approximately 20% of infants and children 1- A sleep-deprived EEG study.
Prognosis: Infants with cryptogenic infantile spasms have a good
prognosis. with focal have a normal routine interictal EEG. CT scanning and especially MRI are most likely to identify 2- Zygomatic leads during EEG
an abnormality in the temporal lobe. 3- Prolonged EEG recording.
2. Symptomatic infantile spasms are related directly to: 4- Video EEG study of the hospitalized
3. Etiology patient weaned from anticonvulsants.
A. Several prenatal, perinatal, factors. Like hypoxic-ischemic encephalopathy, congenital
infections, inborn errors of metabolism, tuberous sclerosis, lissencephaly and schizencephaly
and prematurity.
Infantile spasms 1. BPEC is a common type of focal epilepsy in childhood. Typically starts during childhood (ages 3-10 yr) in normal
children with an unremarkable history and normal neurologic examination. There is often a positive family history of
B. Postnatal conditions include CNS infections, head trauma and hypoxic-ischemic epilepsy.
encephalopathy.
Prognosis: The symptomatic type 80–90% risk of mental retardation. 2. The seizures are usually focal, the motor signs and somatosensory symptoms are often confined to the face.
Oropharyngeal symptoms include tonic contractions and parasthesia of the tongue, unilateral numbness of the
4. The spasms occur during sleep or arousal but have a tendency to develop while cheek (particularly along the gum), gutteral noises, dysphagia and excessive salivation. Focal seizure may proceed to
patients are drowsy or immediately on awakening. A cry may precede or follow an secondary generalization.
infantile spasm, accounting for the confusion with colic in a few cases. Unilateral tonic-clonic contractures of the lower face frequently accompany the oropharyngeal symptoms, as do
clonic movements or paresthesias of the ipsilateral extremities.
5. EEG: hypsarrhythmia Rolandic
3. BPEC occurs during sleep in 75% of patients. consciousness may be intact or impaired
6. Pathogenesis:
1. One hypothesis implicates corticotropin-releasing hormone (CRH) overproduction, resulting in
4. Has an excellent prognosis since it is outgrown by adolescence. 1\4th have repeated clusters of seizures and
neuronal hyperexcitability and seizures.
anticonvulsants are necessary for patients who have frequent seizures.
2. The number of CRH receptors reaches maximum in an infant's brain followed by spontaneous Epilepsy in children Carbamazepine is the preferred drug, which is continued for at least 2 yr or until 14–16 yr of age, when spontaneous
reduction with age, perhaps accounting for the eventual resolution of infantile spasms, even remission of BPEC usually occurs.
without therapy.
5. The EEG pattern is diagnostic, characterized by a repetitive spike focus localized in the centrotemporal or
3. Exogenous ACTH and glucocorticoids suppress CRH synthesis, which may account for their Rolandic area with normal background activity
effectiveness in treating infantile spasms.
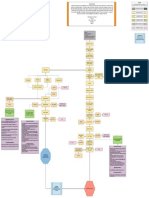
1st step:
1. Ensure that the patient has a seizure disorder and not a condition that mimics epilepsy.
1. This is uncommon before age 5 yrs., more prevalent in girls.
2. Typical absence seizures (petit mal) are characterized by a sudden cessation of motor activity or speech 2. 1st afebrile convulsion, negative family history, normal results of a physical
with a blank facial expression and flickering of the eyelids. Patients do not lose body tone, but their head may examination and EEG, and a cooperative and compliant family, antiepileptics should not
fall forward slightly. be used. Approximately 50% will not experience another convulsion.
3. Never associated with an aura. Typical abscence 3. A recurrent seizure, particularly if it occurs in close proximity to the 1st seizure, is an
4. Automatic behavior frequently found. indication to begin an anticonvulsant.
2nd step:
5. Rarely persist longer than 30 sec and may experience countless seizures daily, and are not associated
with a postictal state, Immediately after the seizure, patients resume activity.
1. Choosing an anticonvulsant depends on the classification of the seizure, determined
6. Hyperventilation for 3–4 min routinely produces an absence seizure. The EEG shows a typical 3 by the history and EEG findings.
spike /sec and generalized wave discharge
Abscence 2. The goal for every patient should be the use of only one drug with the fewest possible
1. Have associated motor components consisting of myoclonic movement of the face, fingers, or extremities side effects for the control of seizures. The drug is increased slowly until seizure control
and, on occasion, loss of body tone Treatment is accomplished or until undesirable side effects develop.
Atypical abscence
2. These seizures produce atypical EEG spike and wave, accompanied by 1- to 2-Hz spike-and–slow-wave
A minimum of two seizure-free years is an adequate and safe period of treatment for a
discharges. patient with no risk factors. When the decision is made to discontinue the drug, the
weaning process should occur over 3–6 mo because abrupt withdrawal may cause
1. Similar to typical absences but occur at a later age. These are usually associated with juvenile status epilepticus.
myoclonic epilepsy
Jeuvenile abscence
3. Recurrence is ≈20–25%, particularly in the 1st 6 mo after discontinuation of the
2. Accompanied by 4- to 6-Hz spike-and–slow-wave and polyspike and–slow-wave discharges.
anticonvulsant
1. These seizures are common ,may follow focal seizure or occur de novo Common antiepileptic medications:
2. Suddenly lose consciousness and, in some cases, emit a shrill, piercing cry. eyes roll back, entire body musculature 1- Carbamazepine (Tegretol): for Generalized tonic-clonic ,focal
undergoes tonic contractions, become cyanotic in association with apnea. seizures.
The clonic phase of the seizure is heralded by rhythmic clonic contractions alternating with relaxation of all muscle
2- Ethosuximide (Zarontin): for Absence seizure.
3- Phenobarbital: for generalized tonic- clonic seizure.
groups. Persists for a few minutes, children may bite their tongue but rarely vomit. Loss sphincter control, particularly
the bladder.
Tonic clonic Generalized 4- Phenytoin (Dilantin): for Generalized tonic-clonic, focal
seizure, status epileptics.
3. Postictally, children are initially semicomatose and typically remain in a deep sleep from 30 min to 2 hr. The 5- Valproic: for generalized tonic-clonic ,absence and myoclonic
postictal phase is often associated with vomiting and an intense bifrontal headache seizures.
6- ACTH: is the preferred drug of infantile spasm, prednisolone is
4. During the seizure: Tight clothing and jewelry around the neck should be loosened, the patient should be placed on
one side, and the neck and jaw should be gently hyperextended to enhance breathing. equally effective.
1. Benign myoclonus begins during infancy and consists of clusters of myoclonic movements
confined to the neck, trunk, and extremities. The myoclonic activity may be confused with infantile
spasms.
2. The EEG is normal in patients with benign myoclonus Benign myoclonus of infancy
3. The prognosis is good, with normal development and the cessation of myoclonus by 2 yr of age.
An anticonvulsant is not indicated. This disorder is characterized by repetitive seizures consisting of brief,
often symmetric muscular contractions with loss of body tone and falling
1. The mean age of onset is ≈2 yr, but the range spreads from 6 mo to 4 yr. Have unremarkable or slumping forward, which has a tendency to cause injuries to the face
Myoclonic
pregnancy, labor, and delivery and intact developmental milestones
and mouth
2. A few patients have febrile convulsions or generalized tonic-clonic afebrile seizures that
precede the onset of myoclonic epilepsy. Variable frequency\ days or weeks.
Typical myoclonus
3. The EEG is abnormal , 1\3rd + F\H of epilepsy.
4. Mental retardation develops in the minority, Learning and language problems and emotional and
behavioral disorders occur and >50% are seizure-free several years later.
You might also like
- Fibroblast Training ManualDocument49 pagesFibroblast Training Manual72034430100% (14)
- Task 1 - Model AnswerDocument4 pagesTask 1 - Model AnswerShauryaNo ratings yet
- Love Stories of Shimla Hills - Chaudhry, MinakshiDocument251 pagesLove Stories of Shimla Hills - Chaudhry, MinakshiAnkit BhattNo ratings yet
- HALOPERIDOL Drug StudyDocument2 pagesHALOPERIDOL Drug Studyanreilegarde89% (9)
- DMS Boolean Algebra TutorialDocument15 pagesDMS Boolean Algebra TutorialLalith KrishnanNo ratings yet
- Catalog KloskaDocument4 pagesCatalog KloskakatadotiNo ratings yet
- Friedman 2014 Epilepsy Imaging in Adults Getting It RightDocument11 pagesFriedman 2014 Epilepsy Imaging in Adults Getting It RightNestor EsquivelNo ratings yet
- Definisi-Klasifikasi EpilepsiDocument40 pagesDefinisi-Klasifikasi Epilepsianita tri hastuti100% (1)
- Assisting During EEGDocument49 pagesAssisting During EEGmikeraz11011No ratings yet
- R02Y2002N04A0248Document4 pagesR02Y2002N04A0248Víctor Hugo Chino ZúñigaNo ratings yet
- Binaural Beats White Paper SomadomeDocument5 pagesBinaural Beats White Paper Somadomernj1230No ratings yet
- AJR Teaching File: Intraventricular Mass: Clinical HistoryDocument4 pagesAJR Teaching File: Intraventricular Mass: Clinical HistoryDokdem AjaNo ratings yet
- R3 Basic Mental ProcessesDocument3 pagesR3 Basic Mental ProcessesScribdTranslationsNo ratings yet
- Mayo Clinic Neurology Board Review - (Section VIII Seizure and Epilepsy)Document1 pageMayo Clinic Neurology Board Review - (Section VIII Seizure and Epilepsy)Lawrence LauNo ratings yet
- 11ppt EegDocument15 pages11ppt EegramNo ratings yet
- Introduction To EEG WavesDocument18 pagesIntroduction To EEG WavesMahi AgrawalNo ratings yet
- Binaural Beats User GuideDocument31 pagesBinaural Beats User GuideMahesh PandyaNo ratings yet
- 13 Accomodative DysfunctionDocument2 pages13 Accomodative Dysfunctiondivya lakshmiNo ratings yet
- Eeg EogDocument19 pagesEeg EogpranoyrajNo ratings yet
- GP Exer 9 Caseous NecrosisDocument1 pageGP Exer 9 Caseous NecrosisClyde HinloNo ratings yet
- Dizziness and Vertigo Trans!Document4 pagesDizziness and Vertigo Trans!Alice TimbNo ratings yet
- Epidural Spinal Cord Stimulation Facilitates Immediate Restoration of Dormant Motor and Autonomic Supraspinal Pathways After Chronic Neurologically Complete Spinal Cord InjuryDocument41 pagesEpidural Spinal Cord Stimulation Facilitates Immediate Restoration of Dormant Motor and Autonomic Supraspinal Pathways After Chronic Neurologically Complete Spinal Cord InjurynorazmiNo ratings yet
- Best Position and Depth of Anaesthesia For.6Document7 pagesBest Position and Depth of Anaesthesia For.6dmandatari7327No ratings yet
- Lesson 4: Seizure: The Underlying Cause Is AnDocument6 pagesLesson 4: Seizure: The Underlying Cause Is AnRocelyn CristobalNo ratings yet
- Patient Factors: General AnaesthesiaDocument2 pagesPatient Factors: General AnaesthesiaKrishnendra MulgundNo ratings yet
- Jurding Neuro Fisher2017Document3 pagesJurding Neuro Fisher2017kenmitaNo ratings yet
- Pcol Seizure DrugsDocument13 pagesPcol Seizure DrugsJANICE MAXIMONo ratings yet
- Subdural HematomaDocument4 pagesSubdural Hematomarodamel gundanNo ratings yet
- CEREBELLUMDocument1 pageCEREBELLUMOscar Orengo AlbertorioNo ratings yet
- OSCE - Cranial Nerve ExaminationDocument2 pagesOSCE - Cranial Nerve ExaminationA.C.No ratings yet
- The Mind RederDocument3 pagesThe Mind RederIoana Augusta PopNo ratings yet
- Memory DisordersDocument10 pagesMemory DisordersCindy Van WykNo ratings yet
- Chandler 2008Document8 pagesChandler 2008TomiOngkoWijayaSigalinggingNo ratings yet
- Recognition of Interictal and Ictal Discharges On EEG. Focal Vs Generalized EpilepsyDocument7 pagesRecognition of Interictal and Ictal Discharges On EEG. Focal Vs Generalized EpilepsyLuís PachecoNo ratings yet
- Lec 03 - Assessing of Neurological System and Special SensesDocument7 pagesLec 03 - Assessing of Neurological System and Special SensesIRISH MANIAGONo ratings yet
- Seizure Updated ILAE ClassificationDocument12 pagesSeizure Updated ILAE ClassificationNasheei RadjaNo ratings yet
- Electroencephalography (EEG)Document61 pagesElectroencephalography (EEG)Arun50% (2)
- Peacock 1990Document7 pagesPeacock 1990Alvaro Perez HenriquezNo ratings yet
- Evaluation of First Seizure and Newly Diagnosed.4Document31 pagesEvaluation of First Seizure and Newly Diagnosed.4CARMEN NATALIA CORTÉS ROMERONo ratings yet
- Fix MeredithDocument2 pagesFix MeredithNisrina ZhafirahNo ratings yet
- NCM104 1st Neuro IDocument14 pagesNCM104 1st Neuro IGabriel MatibagNo ratings yet
- Chapter 1Document2 pagesChapter 1pranavtsababayagaNo ratings yet
- UW Notes - 3 - MicrobiologyDocument45 pagesUW Notes - 3 - MicrobiologyKimberly KanemitsuNo ratings yet
- Nervi KranialisDocument4 pagesNervi KranialisNarendra Ardea PradanaNo ratings yet
- Seizures and Epilepsy in ChildhoodDocument28 pagesSeizures and Epilepsy in Childhoodhgp9ms5gjcNo ratings yet
- 1.05 (Surgery) General Anesthesia - Airway ManagementDocument3 pages1.05 (Surgery) General Anesthesia - Airway ManagementLeo Mari Go LimNo ratings yet
- Acute Onset AmnesiaDocument10 pagesAcute Onset AmnesiajavieroxbmxNo ratings yet
- Electrical Activity of The BrainDocument7 pagesElectrical Activity of The Brain381a53c99bNo ratings yet
- 1b, Amurao, Richmond A., HighercentersDocument2 pages1b, Amurao, Richmond A., HighercentersDr. RemedyNo ratings yet
- Case 5 Concept MapDocument1 pageCase 5 Concept MapdreamedyyyNo ratings yet
- Unit 2Document33 pagesUnit 2SasikumarNo ratings yet
- Child With SeizureDocument11 pagesChild With SeizuresitiNo ratings yet
- Memoria IDocument5 pagesMemoria Ibrxd69cmx7No ratings yet
- Limbic System - Memory - Study GuideDocument4 pagesLimbic System - Memory - Study Guideshivani patelNo ratings yet
- Intra-Extracranial ComaDocument6 pagesIntra-Extracranial ComaAnnisa Rizki SavitriNo ratings yet
- Coma - Bare EssentialsDocument10 pagesComa - Bare EssentialsMariana Hoyos GallegoNo ratings yet
- Pictorial Essay: Sonographic Evaluation of Cervical Lymph NodesDocument9 pagesPictorial Essay: Sonographic Evaluation of Cervical Lymph NodesAhmad SastiantoNo ratings yet
- Pediatric Neurology - Pediatric Epilepsy SyndromeDocument6 pagesPediatric Neurology - Pediatric Epilepsy Syndromemkct111100% (1)
- Journal of Sleep Research - 2012 - TERZAGHI - Dissociated Local Arousal States Underlying Essential Clinical Features ofDocument5 pagesJournal of Sleep Research - 2012 - TERZAGHI - Dissociated Local Arousal States Underlying Essential Clinical Features ofBruna PinheirosNo ratings yet
- Folleto de Servicio Marketing y Creatividad Ilustrado Doodle Azul y AmarilloDocument2 pagesFolleto de Servicio Marketing y Creatividad Ilustrado Doodle Azul y Amarillomateopadillita0529No ratings yet
- 2023 BME 3001 Intro BME Section 8 EEG Wearable DeviceDocument22 pages2023 BME 3001 Intro BME Section 8 EEG Wearable Deviceyibo wangNo ratings yet
- Chronic Bronchitis: Case ScenarioDocument1 pageChronic Bronchitis: Case ScenarioCourtney KateNo ratings yet
- Epileptic Auras Phenomenology and NeurophysiologyDocument14 pagesEpileptic Auras Phenomenology and NeurophysiologyEcaterina OjogNo ratings yet
- EEG2Document4 pagesEEG2Biway RegalaNo ratings yet
- Department of Education: Republic of The PhilippinesDocument8 pagesDepartment of Education: Republic of The PhilippinesAldrin Dela CruzNo ratings yet
- The Limitations of Medium in A Communication AmongDocument4 pagesThe Limitations of Medium in A Communication AmongChristine MarieNo ratings yet
- LEFORT, Claude. Thinking With and Against Hannah ArendtDocument14 pagesLEFORT, Claude. Thinking With and Against Hannah ArendtGabriel VecchiettiNo ratings yet
- Dealroom Embedded Finance v2Document32 pagesDealroom Embedded Finance v2Sushma KazaNo ratings yet
- Role of Open Surgical Drainage or Aspiration in Management of Amoebic Liver AbscessDocument9 pagesRole of Open Surgical Drainage or Aspiration in Management of Amoebic Liver AbscessIJAR JOURNALNo ratings yet
- Phosphoric Acid Industry - Problems & SolutionsDocument18 pagesPhosphoric Acid Industry - Problems & SolutionsRiyasNo ratings yet
- Allgaier Apt Tro Fluidizedbedtechnology en 2Document8 pagesAllgaier Apt Tro Fluidizedbedtechnology en 2Fer Lartiga VentocillaNo ratings yet
- Record Keeping MisconceptionsDocument9 pagesRecord Keeping MisconceptionsPeaceNo ratings yet
- (Welding) ANSI-AWS Standard A5.5-96 Specification For Low-Alloy Steel Electrodes For Shielded Metal Arc Welding (Ebook, 55 Pages)Document55 pages(Welding) ANSI-AWS Standard A5.5-96 Specification For Low-Alloy Steel Electrodes For Shielded Metal Arc Welding (Ebook, 55 Pages)hammadNo ratings yet
- Foreign Currency TranactionDocument11 pagesForeign Currency TranactionAngelieNo ratings yet
- Development On Plot No. Donyo Sabuk/Komarock BLOCK 1/25878 Client: Lilian Lutta MalobaDocument12 pagesDevelopment On Plot No. Donyo Sabuk/Komarock BLOCK 1/25878 Client: Lilian Lutta MalobaAustin AnindoNo ratings yet
- Osek Os: Session Speaker Deepak VDocument60 pagesOsek Os: Session Speaker Deepak VDaour DiopNo ratings yet
- Physical FeaturesDocument4 pagesPhysical FeaturesReshma SharmaNo ratings yet
- Pathogenesis TBDocument39 pagesPathogenesis TBGede Eka Putra NugrahaNo ratings yet
- Example 3 Relating Downhole Rate With The Rate at Standard ConditionsDocument8 pagesExample 3 Relating Downhole Rate With The Rate at Standard ConditionsMaisam AbbasNo ratings yet
- Wordsearch Fruits Fun Activities Games Games Icebreakers Oneonone Ac - 109759Document2 pagesWordsearch Fruits Fun Activities Games Games Icebreakers Oneonone Ac - 109759raquel lujanNo ratings yet
- Bluthner PRO 88 Owners enDocument20 pagesBluthner PRO 88 Owners enAnonymous pMgjvHvC41No ratings yet
- Radiation Heat Transfer ExperimentDocument6 pagesRadiation Heat Transfer ExperimentDaniel IsmailNo ratings yet
- Introduction SlidesDocument23 pagesIntroduction SlidesMathiselvan GopalNo ratings yet
- Review Exercises DAY 3Document4 pagesReview Exercises DAY 3Heba Abd-AllahNo ratings yet
- Company LawDocument15 pagesCompany Lawpreetibajaj100% (2)
- A Brief History of Jazz DrummingDocument8 pagesA Brief History of Jazz DrummingManoloPantalonNo ratings yet
- Assam High School TET Pedagogy Old PaperDocument19 pagesAssam High School TET Pedagogy Old PaperSharba BoruahNo ratings yet
- The Sinister Genius of Qassem Soleimani - WSJ PDFDocument5 pagesThe Sinister Genius of Qassem Soleimani - WSJ PDFMuhammad Anique RawnNo ratings yet
- SACH Tooth Brush - Launch Docket PDFDocument13 pagesSACH Tooth Brush - Launch Docket PDFSami ShaikhNo ratings yet