Professional Documents
Culture Documents
Farxaan A
Farxaan A
Uploaded by
farhanabdiwahab272Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Farxaan A
Farxaan A
Uploaded by
farhanabdiwahab272Copyright:
Available Formats
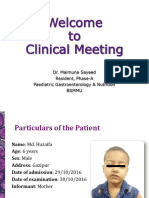
Farhan abdiwahab Ibrahim
karamara General hospital
Name: ahmed yasin halane
Age: 30 Sex: male
Occupation: house
Religion: muslim
Address: hodlay
Date of Admission was : 22/8/2024
Ethnicity: somali
The Department: surgery word:
surgery Bed No: 03
Marital Status: married
Date of Clerking: 23/8/2024
Source of History: The Patient himself
PREVIOUS ADMISSION =non
CHIEF
COMPLAINT
Yellowish discoloration of eyes of one month duration
HPI *
The patient was last relatively healthy 04 weeks back at which time he started to
experience dark
colored urine & clay colored stool associated with itching sensation which began from his
hands & later progressed to include all of his body. The itching worsens during night time.
2
weeks prior to admission his father began to notice persistent yellowish discoloration of his
eyes. In addition to this he started to experience steady epigastric pain without radiation
which was aggravated by eating heavy foods and relieving by using analgesics . He has also
low grade intermittent fever but no chills
or rigor. 03 days prior to admission he started to experience nausea & non blood tingled,
non
bilious vomiting of ingested matter about 6 times /day.
Has anorexia, easily fatigability & unquantified weight loss for the past 4 weeks to
the extent his trousers become loose
He Has history of tinnitus, blurring of vision & light headedness
No history of cigarette smoking or chronic alcohol consumption
His regular dietary habit is rice, spaghetti.
Otherwise.
No history of similar illness in the family
No history of previous abdominal surgery
No history of multiple sexual partner, contact with jaundiced patient or blood
transfusion
No history of medication
No history of chronic cough, contact with chronic cougher or previous TB
By: Dr Ahmed Abdulahi title HO
treated
No self/family history of HTN or asthma. No family history of DM
He has been screened for RVI 6months back & found to be NR
Finally, he was admitted to karamarda general hospital
.
PAST ILLNESS
No hx of childhood illnesses like chicken pox, mumps or small pox. Not vaccinated.
No hx of previous surgery, trauma, psychiatry problems or drug allergy.
Review of system (ROS)
H.E.E.N.T
Head: No hx of headache or head injury
Eyes: No hx of blurring of vision, pain in the eyes, eye itching, or sontaneous
lacrimation
Ears:
No hx of Earache, deafness, ear discharge, vertigo or tinnitus
Nose:
No hx of nasal bleeding or discharge
Mouth and throat:
No hx gum bleeding, tooth extraction
Lymphoglandular system (LGS):
Hx of swelling in the neck,
No hx of heat or cold intolerance.
Respiratory System (RS):
No hx of cough, chest pain or fast breathing
Cardiovascular system (cvs):
No hx dyspnea, orthonea or PND
Gastrointestinal system (GIS):
No hx of diarrhea or constipation
Genitourinary system (GUS):
No hx of flank pain, see HPI
Integumentary system (IGS):
No hx of skin rash or ulcers
Muskuloskeletal system (MSS):
No hx of loss of limb function or joint pain.
Central nervous system (CNS):
No forgetfulness,abnormal body mov’t or insomnia.
Personal History
He was born and raised in hodlay, where he lived all his life. He had a healthy
childhood and was an active boy who liked helping his father around the farm.
There was no school near his village and like his parents, he never went to
school. But he is able to read and write numbers.
He is a farmer and also raises cattle, sheep and goat.
He usually eats ‘injera’ made of ‘teff & ‘shiro’ made of ’atter’ basta,rice
By: Dr Ahmed Abdulahi title HO
He is currently married and has ten children. All are alive & healthy.
He doesn't use alcohol and chat abuse
Family History
Father and mother:
Both his father and mother are dead. His father died around 30 years ago at unknown age
by
unknown cause while his mother died two years ago
Siblings:
He has two sisters and four brothers. All are alive & well.
Family Diseases:
No family history of DM, hypertension, Asthma, tuberculosis, allergy or sudden
deaths.
Physical Examination
General Appearance
Chronic sick looking,
Vital signs
BP: 110/70mmHg, right arm, sitting position
PR: 95bpm, Rt radial artery, regular & full volume
RR: 18 breath/min, shallow & regular
T0: 35.20c, axillary, @10 AM
Weight: 65kg
Height: 160cms
H.E.E.N.T
Head: Normal size, shape and hair distribution.No scar or tenderness
Ears: Normal contour of pinna.Clear external ear canal.
Eyes: No periorbital edema, ptosis, exophthalmoses or strabismus.
Pile conjunctivae, icteric sclera
Nose: The nasal septum is central. There is no polyp or active discharge
Mouse and throat: The lips show no fissure or ulceration
The gums are intact with no ulceration. There are no carious teeth,
extraction, dentures or filling.
Tongue – no atrophied papillae, The buccal mucosa is pink & wet.
Lymphoglandular system
There is no significantly enlarged..
Supraclavicular, periumbilical,axillary, inguinal lymph nodes, testis
Respiratory System
Inspection:
By: Dr Ahmed Abdulahi title HO
No peripheral or central cyanosis or clubbing or the finger nails
Breathing is shallow and regular
No SC or IC retraction
No chest wall deformity or surgical scar
No chest lag
Palpation:
Trachea is central
No subcutaneous emphysema
No chest wall tenderness
Tactile fremitus is comparable on both sides
Chest expansion is symmetrical
Percussion:
Resonant all over lung fields
Auscultation:
Vesicular breat
Cardiovascular system
Arterial:
All peripherally accessible arteries are palpable
No thickening of vessels wall
No radio-femoral delay
Venous:
JVP is not raised
No distended neck vein
Negative Hepato-jugular reflex
Precordial examination
Inspection:
No precordial bulging
Quite precordium
The apical impulse is not visible
Palpation:
No palpable heart sound
The PMI is at the 5th ICS lateral to MCL, localized & tapping.
By: Dr Ahmed Abdulahi title HO
There is no parasternal or apical heave. There is no thrill.
Auscultation:
S1 & S2 are well heard
No murmur or gallop
Abdominal examination
Inspection:
The abdomen is flat & symmetrical
It moves with respiration.
The flanks are not full
No distended abdominal vein
No surgical scar
Auscultation:
Normo-active bowel sound (8/min)
No bruit over renal artery, abdominal aorta or liver area
Palpation:
Superficial palpation:
o There is tenderness
o No superficially palpable mass
Deep palpation:
o No organomegally
Percussion:
No sign of fluid collection(shifting dullness/fluid thrill)
Total vertical liver span (TVLS) along the right mid-clavicular line =6cms
DRE
Inspection
o No ulceration or visible mass
Palpation
o Normal anal sphincter tone
o There is a mass which has smooth surface, regular border, firm consistency, not fixed
to rectal mucosa & palpable medial sulcus but the upper border isn’t reachable
o No blood on the examining finger
INVESTIGATION
Laboratory
Liver function test/LFT
o Serum bilirubin (Total & Direct), ALP, SGOT, SGPT, GGT
Predominant rise in ALP in relation to SGOT & SGPT reflects
cholestasis(intra/exra-hepatic) .
o PT PT prolongation with Vitamin K administration is compatible with
obstructive jaundice
Viral markers
By: Dr Ahmed Abdulahi title HO
Hepatitis B surface antigen/HBsAg & Hepatitis C virus antibody/HCVAb
CBC—acute cholangitis
Urine bilirubin
Imaging
Abdominal Ultrasound
Important for documenting stones in the gallbladder (if still present) & determines size of
CBD (Common bile duct is said to be dilated when the diameter is >8mm)
Contrast CT-scan (abdominal)
MRI
DIFERENTIAL DIAGNOSIS
1. Congenital: Biliary atresia, choledochal cyst
2. Inflammatory: Ascending cholangitis, sclerosing cholangitis
3. Obstructive: Common bile duct (CBD) stones, biliary stricture, parasitic infestation
4. Neoplastic: Carcinoma of head of pancreas, periampulary carcinoma,
cholangiocarcinoma, Klatskin tumor
5. Extrinsic compression: Compression by lymph node
Assignment
obstructive jaundice
By: Dr Ahmed Abdulahi title HO
You might also like
- Scrib AssignmentDocument9 pagesScrib AssignmentShayne Jessemae AlmarioNo ratings yet
- Final Assessment Soap NoteDocument13 pagesFinal Assessment Soap Noteapi-494643478100% (3)
- CosmesisDocument5 pagesCosmesisizat husseinNo ratings yet
- Pedia 1Document8 pagesPedia 1Jani MisterioNo ratings yet
- FarhanDocument6 pagesFarhanfarhanabdiwahab272No ratings yet
- Case Report VI Internal MedicineDocument13 pagesCase Report VI Internal MedicineGidu SaidNo ratings yet
- Chief ComplaintDocument7 pagesChief ComplaintyohannesNo ratings yet
- Addis Ababa University School of Medicine Department of Gynecology & ObstetricsDocument13 pagesAddis Ababa University School of Medicine Department of Gynecology & Obstetricspilual tongyikNo ratings yet
- Constitutional: General Appearance: Healthy-Appearing, Well-Nourished, and Well-Developed. Level ofDocument10 pagesConstitutional: General Appearance: Healthy-Appearing, Well-Nourished, and Well-Developed. Level ofRichard ObinwankwoNo ratings yet
- HIVCase Report II Internal MedicineDocument12 pagesHIVCase Report II Internal Medicineaxmedfare138No ratings yet
- Case ReportDocument9 pagesCase ReportBerhanu DigamoNo ratings yet
- Case ReportDocument17 pagesCase ReportdenekeNo ratings yet
- Name: Wong Wai Kheong Matrix No: BMS12081154Document13 pagesName: Wong Wai Kheong Matrix No: BMS12081154myolie wuNo ratings yet
- History 1Document11 pagesHistory 1KaleabNo ratings yet
- APH Secondary To Placenta Previa 2Document10 pagesAPH Secondary To Placenta Previa 2sirgute tamratNo ratings yet
- Case Report IV Internal MedicineDocument11 pagesCase Report IV Internal MedicineGidu Said100% (1)
- IM Gastro FinalDocument10 pagesIM Gastro FinalIzzyMaxinoNo ratings yet
- Case Report II Internal MedicineDocument11 pagesCase Report II Internal MedicineGidu SaidNo ratings yet
- Case Report III Internal MedicineDocument12 pagesCase Report III Internal MedicineGidu Said0% (1)
- Case Report 1Document12 pagesCase Report 1mike sharewNo ratings yet
- Template Gyn Lo Abd PainDocument18 pagesTemplate Gyn Lo Abd PainHassan HarirNo ratings yet
- CRVHD Percipitated by IEDocument14 pagesCRVHD Percipitated by IEKemotherapy LifesucksNo ratings yet
- CASE 3 MEDICINE JULY 10 2019 AcutePyeloDocument15 pagesCASE 3 MEDICINE JULY 10 2019 AcutePyeloTrisNo ratings yet
- Health Assessment Project: Name: Ena Lewis Tutor: Sis Francis Group: 15Document27 pagesHealth Assessment Project: Name: Ena Lewis Tutor: Sis Francis Group: 15Blake KamminNo ratings yet
- Jiefang Rvenue, Hankou, Hubei. Tel: 857307523 and WifeDocument4 pagesJiefang Rvenue, Hankou, Hubei. Tel: 857307523 and WifeAmit GoswamiNo ratings yet
- SOAP Note 1 - Breast CADocument4 pagesSOAP Note 1 - Breast CAacvalvarioNo ratings yet
- Form Health History Documentation: Biographical DataDocument7 pagesForm Health History Documentation: Biographical DataSandra SanonNo ratings yet
- Acute PancreatitisDocument7 pagesAcute PancreatitisPatrick DycocoNo ratings yet
- Soap FamedDocument79 pagesSoap FamedJane GarciaNo ratings yet
- Cagayan State University College of Medicine Carig CampusDocument11 pagesCagayan State University College of Medicine Carig CampusIsabel CastilloNo ratings yet
- Cwu Surgery Y5 AsyikinDocument21 pagesCwu Surgery Y5 AsyikinNurulasyikin MAANo ratings yet
- Type The Document Title: Department of Surgery Case Report-IiDocument10 pagesType The Document Title: Department of Surgery Case Report-IiEyosiyas AbiyNo ratings yet
- Cwu SurgeryDocument16 pagesCwu SurgeryAslah NabilahNo ratings yet
- Clinical Case: Section A - Group 8Document68 pagesClinical Case: Section A - Group 8madison Deli100% (1)
- 312 ENT Patient InterviewDocument5 pages312 ENT Patient InterviewDorish Faith CarilloNo ratings yet
- Clinicalmeetingoriginal 161117192705Document50 pagesClinicalmeetingoriginal 1611171927057dbnf4stjyNo ratings yet
- SOAP NoteDocument8 pagesSOAP NoteAnonymous p0y5mmLQNo ratings yet
- Case Clerking ApendicDocument15 pagesCase Clerking ApendicChen Cheng0% (1)
- Case Clerking ApendicDocument15 pagesCase Clerking ApendicMelvin Khung100% (1)
- Medical Report - PneumoniaeDocument8 pagesMedical Report - Pneumoniaenguyenhoavanchi2002No ratings yet
- AbortionDocument16 pagesAbortionKim Lompot100% (1)
- History: O Identifying DataDocument10 pagesHistory: O Identifying DataJofen Ann Hisoler TangpuzNo ratings yet
- BPH Sample To Case ReportDocument12 pagesBPH Sample To Case ReportBirhanu ShiferawNo ratings yet
- Addis Ababa University Faculty of MedicineDocument12 pagesAddis Ababa University Faculty of MedicinedenekeNo ratings yet
- Week 3 Case - DOBDocument3 pagesWeek 3 Case - DOBKirk Matthew ZhuNo ratings yet
- Burtee AdooDocument4 pagesBurtee AdooAndualemNo ratings yet
- Patient Profile Patient Address Age Sex MaritalDocument3 pagesPatient Profile Patient Address Age Sex Maritalunno hiquianaNo ratings yet
- Gynecology and Obstetrics Ward Case Report - 1: Balesew Enawgaw (C-1) Id: Medr 24/05Document10 pagesGynecology and Obstetrics Ward Case Report - 1: Balesew Enawgaw (C-1) Id: Medr 24/05denekeNo ratings yet
- Jocelyn PrietoDocument11 pagesJocelyn PrietoAndrew Joever PrietoNo ratings yet
- Case-1 On Open CholeDocument4 pagesCase-1 On Open CholeKhus RahoNo ratings yet
- Write Up Surgery 1 TambahDocument22 pagesWrite Up Surgery 1 Tambahazizi abd rahmanNo ratings yet
- Internal Medicine Cases PresentationsDocument68 pagesInternal Medicine Cases PresentationsEliudi Kituma100% (2)
- Pleural EffusionDocument106 pagesPleural EffusionFarica Armane Aquino0% (1)
- Mahmoud Alhaseen 46 Years Old French Male Was Admitted To The ER On 7 March Complaining of Abdominal Pain For 5 DaysDocument3 pagesMahmoud Alhaseen 46 Years Old French Male Was Admitted To The ER On 7 March Complaining of Abdominal Pain For 5 DaysMnsor svNo ratings yet
- Case Report: Tikur Anbesa Specialized HospitalDocument11 pagesCase Report: Tikur Anbesa Specialized HospitalTefera LeteboNo ratings yet
- Previous Admission: by Riyad and SharafDocument5 pagesPrevious Admission: by Riyad and SharafRiyad AbrahimNo ratings yet
- EVRMC 1st EndorsementDocument4 pagesEVRMC 1st EndorsementPatrick DycocoNo ratings yet
- H&P FormatDocument7 pagesH&P FormatRaffy Gutman100% (1)
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicFrom EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicRating: 5 out of 5 stars5/5 (1)
- Approach To Altered Mental StatusDocument19 pagesApproach To Altered Mental StatusMudassar SattarNo ratings yet
- Thoa 1994Document24 pagesThoa 199439 femina pcNo ratings yet
- Adult Langerhans Cell Histiocytosis A Rare Entity in Cervical Spine Compression Case ReportDocument4 pagesAdult Langerhans Cell Histiocytosis A Rare Entity in Cervical Spine Compression Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 61.functions of The Liver and BileDocument2 pages61.functions of The Liver and BileNek TeroNo ratings yet
- Hydrocephalus Teori FinalDocument19 pagesHydrocephalus Teori Finalaurelia_rlNo ratings yet
- Inflammation Robbins Basic Pathology XWORD 1Document2 pagesInflammation Robbins Basic Pathology XWORD 1Ac HonsaycoNo ratings yet
- Hypoxia: and Its Effects On HealthDocument36 pagesHypoxia: and Its Effects On HealthVeres András100% (2)
- Chapter 7: Pelvis and PerineumDocument22 pagesChapter 7: Pelvis and PerineumAlaz NellyNo ratings yet
- Abnormal Labor Concept MapDocument1 pageAbnormal Labor Concept MapRobert Timothy YapNo ratings yet
- Completed Project List 19072021Document18 pagesCompleted Project List 19072021ziyambicharles77No ratings yet
- Ataxia and Movement Disorders: Clinical Manifestations TreatmentDocument6 pagesAtaxia and Movement Disorders: Clinical Manifestations TreatmentMahfouzNo ratings yet
- 2017 Stroke in Childhood - Pathway PosterDocument1 page2017 Stroke in Childhood - Pathway PosterDeomicah SolanoNo ratings yet
- Presented By: Piyush Verma Mds 2 Yr Dept of Paedodontics & Preventive DentistryDocument51 pagesPresented By: Piyush Verma Mds 2 Yr Dept of Paedodontics & Preventive DentistryJodene Rose RojasNo ratings yet
- Health Assessment 51-100 QuestionnaireDocument27 pagesHealth Assessment 51-100 QuestionnairetflorenzNo ratings yet
- Media Kontras MriDocument13 pagesMedia Kontras MriKakhfi Gemah PNo ratings yet
- Isuog: GuidelinesDocument17 pagesIsuog: GuidelinesAndrés Gaviria CNo ratings yet
- Glioma: ClassificationDocument2 pagesGlioma: ClassificationAppas SahaNo ratings yet
- Core CH 7 Gas Exchange in HumansDocument6 pagesCore CH 7 Gas Exchange in HumansommpNo ratings yet
- The Postpartal Family Maybelle B. AnimasDocument43 pagesThe Postpartal Family Maybelle B. AnimasErika Anne Mercado CadawanNo ratings yet
- 2014 - MesenchymalDocument18 pages2014 - MesenchymalMiguel ÁngelNo ratings yet
- Coordination & Response 3 QP PDFDocument10 pagesCoordination & Response 3 QP PDFJeffrey PiggottNo ratings yet
- NCM116 - 3NC1 - Group 1 - CognitiveDisordersDocument15 pagesNCM116 - 3NC1 - Group 1 - CognitiveDisordersCARLOS JOSETON PAOLO SANTIAGO TORRENo ratings yet
- Barium Esophagogram As The First Step To Modern Tecniques: Poster No.: Congress: Type: AuthorsDocument55 pagesBarium Esophagogram As The First Step To Modern Tecniques: Poster No.: Congress: Type: AuthorsbenznakupNo ratings yet
- Solar RetinopathyDocument1 pageSolar RetinopathyJonas DiazNo ratings yet
- Patel 2013Document8 pagesPatel 2013joantyy 1No ratings yet
- SEGMENTAL MYOCLONUS IN A CHILD With Spinal TumorDocument8 pagesSEGMENTAL MYOCLONUS IN A CHILD With Spinal TumorVincentius Michael WilliantoNo ratings yet
- Classification of PainDocument3 pagesClassification of Painfeby alexesNo ratings yet
- Surgery by GiselleDocument15 pagesSurgery by GiselleTris100% (1)
- BPC-157 A Collection of StudiesDocument28 pagesBPC-157 A Collection of StudiesscribdNo ratings yet