Professional Documents
Culture Documents
Kertas Pemeriksaan Fisik - Final
Kertas Pemeriksaan Fisik - Final
Uploaded by
syafridasiregar700Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kertas Pemeriksaan Fisik - Final
Kertas Pemeriksaan Fisik - Final
Uploaded by
syafridasiregar700Copyright:
Available Formats
NAMA :
NO :
AGE /DOB :
DEPARTMENT/ PT :
PHYSICAL DIAGNOSTIC FORM
RIWAYAT PENYAKIT (HISTORY OF DISEASE)
Y/N Y/N
Rhinitis / Hay Fever Hearing Problems
Anemia Eye Problems
Asthma Epilepsy
T
Abnormal Blood Pressure Migraine
T
BronchitiS Head Injury
Heart Abnormalities T
Hepatitis
Chronic Skin Disorders Kidney Disorder
T
Chronic Chough Low Back Pain
Diarrhoea > 2 weeks Typhoid Fever
Diabetes T
History of surgeries
COMPLAINTS :
1. BASIC EXAMINATIONS
HEIGHT : cm BLOOD : mmHg
PRESSURE
x
WEIGHT : kg PULSE : /i
SpO2 : % EYESIGHT RIGHT (右): (Unaided)
LEFT (左): (Unaided)
TEMPRATURE : C COLOUR BLINDNESS :
BMI :
PATIENT BEHAVIOUR :
BEHAVIOUR YES NO
SMOKING
ALCOHOLIC
COFFEE DRINKER
EXCERSICE
ROKOK ( )BUNGKUS
PEMERIKSAAN FISIK/ KELUHAN TAMBAHAN :
3. GENERAL EXAMINATION
Type Yes No Description
Pale
Oedema
Cyanosis
Jaundice
Deformity
Skin Disorder
KELUHAN PENDENGARAN :
TELINGA SERUMEN ADA/TID
You might also like
- Dengue Assessment ChecklistDocument1 pageDengue Assessment ChecklistMitzi BelamideNo ratings yet
- PHA Individual Health Profile & Assessment Form As of Oct.09, 2017Document8 pagesPHA Individual Health Profile & Assessment Form As of Oct.09, 2017Eden VblagasyNo ratings yet
- ViewDocument2 pagesViewJohn Lorenz OrduñaNo ratings yet
- HypertenssionDocument17 pagesHypertenssionnadeemhumdardNo ratings yet
- Hypertension Follow Up EvaluationDocument1 pageHypertension Follow Up Evaluatione-MedTools100% (3)
- System Generated MerDocument2 pagesSystem Generated MerSyan ApuyanNo ratings yet
- 1st Patient Encounter RegistrationDocument2 pages1st Patient Encounter Registrationjefferson bustargaNo ratings yet
- Cap MR, T2DM R - o DkaDocument67 pagesCap MR, T2DM R - o DkaGROUP 1 2023No ratings yet
- SuhanaDocument3 pagesSuhanaM SonuNo ratings yet
- Cap 20 HipertensãoDocument26 pagesCap 20 Hipertensãoroquetv93No ratings yet
- Form 86Document8 pagesForm 86Hanna Jane BayarcalNo ratings yet
- Health Screening and Assessment v2Document4 pagesHealth Screening and Assessment v2Rudelyn Perlita C. ManzanoNo ratings yet
- Pharmacists Clinical Round Report: Faculty of Pharmacy & Alternative Medicine The Islamia University of BahawalpurDocument9 pagesPharmacists Clinical Round Report: Faculty of Pharmacy & Alternative Medicine The Islamia University of BahawalpurNoman ZakiNo ratings yet
- CPC 2023 No TransitionDocument41 pagesCPC 2023 No TransitionMonique BorresNo ratings yet
- Uhs Form 4 Pe Form With Philhealth Number and PWD For 2024Document4 pagesUhs Form 4 Pe Form With Philhealth Number and PWD For 2024plmbsbio1No ratings yet
- Clinical Case IiDocument3 pagesClinical Case IiEdalyn CapiliNo ratings yet
- Progress Note IcuDocument2 pagesProgress Note Icumena gergesNo ratings yet
- CompiledDocument9 pagesCompiledcogiezamoraNo ratings yet
- Diabetic FootDocument3 pagesDiabetic FootaminullahNo ratings yet
- Form 86 SHDDocument6 pagesForm 86 SHDEYEPATCH GHOUL22No ratings yet
- Care Plan 2 Medsurg - Selina DykesDocument10 pagesCare Plan 2 Medsurg - Selina Dykesapi-520664738No ratings yet
- Endocrine FinalDocument7 pagesEndocrine FinalBell GatesNo ratings yet
- Cap 23 HipertensãoDocument35 pagesCap 23 Hipertensãoroquetv93No ratings yet
- Medical Examination Report: A. Examinee DetailsDocument4 pagesMedical Examination Report: A. Examinee DetailsMohammed Bilal ShaikNo ratings yet
- Lung Cancer 1 1Document48 pagesLung Cancer 1 1sireenmahyobNo ratings yet
- Right Radial Head FractureDocument6 pagesRight Radial Head Fracturehemanarasimha gandikotaNo ratings yet
- PhysicalFitness CertificateDocument2 pagesPhysicalFitness Certificatesoyamsidh dasNo ratings yet
- Group 4Document45 pagesGroup 4Nicole Juliette CCNo ratings yet
- OB GROUP 3 VIRTUAL PA TOOL Pre EclampsiaDocument23 pagesOB GROUP 3 VIRTUAL PA TOOL Pre EclampsiaAubrey Dynise C. TorralbaNo ratings yet
- Patient Health Assessment PDFDocument8 pagesPatient Health Assessment PDFVictor BarbosaNo ratings yet
- Endorsement: OCTOBER 19, 2021 Pgi Joseph I. AgujaDocument27 pagesEndorsement: OCTOBER 19, 2021 Pgi Joseph I. AgujaIrish AlonzoNo ratings yet
- Scribe America Final, Emergency DepartmentDocument41 pagesScribe America Final, Emergency DepartmentJulio CastilloNo ratings yet
- Physical Fitness - Certificate 2022Document2 pagesPhysical Fitness - Certificate 2022Warrior SoulNo ratings yet
- IM Worksheet CHOLECYSTITISDocument4 pagesIM Worksheet CHOLECYSTITISgorgNo ratings yet
- Amputated LegDocument21 pagesAmputated Legbhartibundi1234No ratings yet
- Surgery Department: Emergency Case ReportsDocument46 pagesSurgery Department: Emergency Case ReportsMohamad ZulfikarNo ratings yet
- Patient Report Sheet Fall 2023Document1 pagePatient Report Sheet Fall 2023Michelle DuBose AdamsNo ratings yet
- Review of Systems Was Unremarkable Physical Examination Was As FollowsDocument9 pagesReview of Systems Was Unremarkable Physical Examination Was As Followsjabby2685No ratings yet
- Rheumatic Heart Disease WithoutDocument26 pagesRheumatic Heart Disease Withoutapi-716714980No ratings yet
- Certificate of Physical FitnessDocument2 pagesCertificate of Physical FitnessHarsh SahuNo ratings yet
- Case Presentation STEMIDocument35 pagesCase Presentation STEMIFitriya Syaifuddin100% (1)
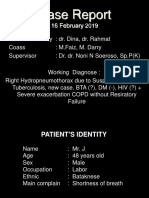
- Case ReportDocument12 pagesCase ReportSetiawan DanuNo ratings yet
- Lapkas Paru USU-16 Januari 2019Document21 pagesLapkas Paru USU-16 Januari 2019Sylvan LaminaNo ratings yet
- Surgery Department: Emergency Case ReportsDocument43 pagesSurgery Department: Emergency Case ReportsMukhizalNo ratings yet
- Complications & SignsDocument1 pageComplications & SignsDavid J BrentNo ratings yet
- Certificate of Physical Fitness: Personal DetailsDocument2 pagesCertificate of Physical Fitness: Personal DetailsVijay KumarNo ratings yet
- OSCE Internal MedicineDocument4 pagesOSCE Internal Medicinemohamed mowafeyNo ratings yet
- Patient History TemplateDocument2 pagesPatient History TemplateDr Shazana NazrinNo ratings yet
- Eluh Anf Atig Ue Nea Saa T Akt Ivita S, Da N Pad Am Alam Har IDocument37 pagesEluh Anf Atig Ue Nea Saa T Akt Ivita S, Da N Pad Am Alam Har IRicky SuritnoNo ratings yet
- Matrix MCUDocument5 pagesMatrix MCUleli apriyaniNo ratings yet
- IM Worksheet CHOLECYSTITISDocument4 pagesIM Worksheet CHOLECYSTITISgorgNo ratings yet
- Case PresentationDocument8 pagesCase PresentationTrang VuNo ratings yet
- Bab Ii Status PasienDocument12 pagesBab Ii Status PasienNita KurniasihNo ratings yet
- C105a-Pre-Sea-And-Periodic-Medical-Fitness-Examinations-For-Seafarers - by AstroDocument5 pagesC105a-Pre-Sea-And-Periodic-Medical-Fitness-Examinations-For-Seafarers - by Astroklinik utama Bali Puri MedikaNo ratings yet
- Case Write-Up 1Document22 pagesCase Write-Up 1Syed TalhaNo ratings yet
- Medical Certificate For Service at Sea: ConfidentialDocument4 pagesMedical Certificate For Service at Sea: ConfidentialADMIN MCU RSU SAHID SAHIRMAN100% (1)
- Fever Assessment Checklist: Criteria Yes No Details Patient DetailsDocument2 pagesFever Assessment Checklist: Criteria Yes No Details Patient DetailsKok Hui Diong100% (1)
- Luka TikamDocument8 pagesLuka TikamMohamad ZulfikarNo ratings yet
- Endocrinology Notes for Medical StudentsFrom EverandEndocrinology Notes for Medical StudentsRating: 4 out of 5 stars4/5 (1)
- Cardiac Care and COVID-19: Perspectives in Medical PracticeFrom EverandCardiac Care and COVID-19: Perspectives in Medical PracticeNo ratings yet