Professional Documents
Culture Documents
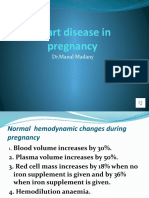
Cardiac Disease Pregnancy Guideline Short
Cardiac Disease Pregnancy Guideline Short
Uploaded by
collins gikunguCopyright:
Available Formats
You might also like
- Uw Step3 NotesDocument34 pagesUw Step3 NotesAakash ShahNo ratings yet
- What Constitutes A Nephrology ClearanceDocument95 pagesWhat Constitutes A Nephrology Clearancegillian102290100% (2)
- Rheumatic Heart Disease in Pregnancy: What Is RHD?Document5 pagesRheumatic Heart Disease in Pregnancy: What Is RHD?dedy chandraNo ratings yet
- Mecca - 606991860Document50 pagesMecca - 606991860Rendy Adhitya PratamaNo ratings yet
- Heart Disease in Pregnancy: Mohana PreeshaDocument50 pagesHeart Disease in Pregnancy: Mohana PreeshaChuks LeviNo ratings yet
- Cardiac Disease in PregnencyDocument35 pagesCardiac Disease in PregnencyMannat ZaidiNo ratings yet
- Pregnancy Cardiovascular ComplicationsDocument13 pagesPregnancy Cardiovascular Complicationsits charitaNo ratings yet
- Cbs Pulm0 h3m@ N0tesDocument26 pagesCbs Pulm0 h3m@ N0tesLINDSLEY GONo ratings yet
- Cardiac Diseases in PregnancyDocument13 pagesCardiac Diseases in PregnancyAbdullah MatarNo ratings yet
- Cardio Vascular Disease in PregnancyDocument57 pagesCardio Vascular Disease in PregnancySanthosh.S.U0% (1)
- Outcome Pada Penyakit Jantung Terhadap Ibu Dan Janin Selama KehamilanDocument28 pagesOutcome Pada Penyakit Jantung Terhadap Ibu Dan Janin Selama KehamilanRaras PraminingrumNo ratings yet
- Heart Failure in Pregnant Women: Is It Peripartum Cardiomyopathy?Document6 pagesHeart Failure in Pregnant Women: Is It Peripartum Cardiomyopathy?NengLukmanNo ratings yet
- Dr. Senthil Priya Heart Disease in Pregnancy FINALDocument68 pagesDr. Senthil Priya Heart Disease in Pregnancy FINALKai ParkerNo ratings yet
- Management of Cardiac Disease in LaborDocument6 pagesManagement of Cardiac Disease in LaborHassan osmanNo ratings yet
- CARDIAC2Document36 pagesCARDIAC2A.H.ANo ratings yet
- Article 10.1111/tog.12599Document8 pagesArticle 10.1111/tog.12599KeeranmayeeishraNo ratings yet
- Cardiac Diseases in PregnancyDocument27 pagesCardiac Diseases in PregnancyHoney May Rollan Vicente50% (2)
- Dr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiDocument35 pagesDr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiNailahRahmahNo ratings yet
- Heart Disease and Bronchial AsthmaDocument45 pagesHeart Disease and Bronchial AsthmaVissalini JayabalanNo ratings yet
- Cardiovascular Disease and Pregnancy Journal o NCM 102Document15 pagesCardiovascular Disease and Pregnancy Journal o NCM 102MichelleIragAlmarioNo ratings yet
- CARDIAC Diseases IN PREGDocument40 pagesCARDIAC Diseases IN PREGStella CooKeyNo ratings yet
- K - 16 Heart Disease in PregnancyDocument19 pagesK - 16 Heart Disease in PregnancyPathrecia Natalia SiagianNo ratings yet
- The Pregnant Woman With Heart Disease: Management of Pregnancy and DeliveryDocument5 pagesThe Pregnant Woman With Heart Disease: Management of Pregnancy and DeliveryMichael SusantoNo ratings yet
- Nursing Acn-IiDocument80 pagesNursing Acn-IiMunawar100% (6)
- Cardiac Disease and Pregnancy: Clinical GuidelinesDocument9 pagesCardiac Disease and Pregnancy: Clinical GuidelinesBagus Wanda Habibullah100% (1)
- 46-M21-Cardiac Diseases During PregnancyDocument35 pages46-M21-Cardiac Diseases During Pregnancyاحمد احمدNo ratings yet
- Heart Diseases in PregnancyDocument70 pagesHeart Diseases in PregnancySergiu HelciugNo ratings yet
- CPG Medical ComplicationsDocument134 pagesCPG Medical ComplicationsAiko EscobidoNo ratings yet
- Management of Rheumatic Heart Disease: Quick Reference Guide For Health ProfessionalsDocument4 pagesManagement of Rheumatic Heart Disease: Quick Reference Guide For Health ProfessionalsgireeshsachinNo ratings yet
- Maternal Risk StratificationDocument59 pagesMaternal Risk StratificationannisNo ratings yet
- Heart Disease in PregnancyDocument5 pagesHeart Disease in PregnancyAngeliqueNo ratings yet
- ACOG Practice Bulletin No. 212 Summary - Pregnancy and Heart DiseaseDocument6 pagesACOG Practice Bulletin No. 212 Summary - Pregnancy and Heart DiseaseYuly Andrea Marquez CastañedaNo ratings yet
- Ventricular TachycardiaDocument17 pagesVentricular TachycardiaAyu Rezki FadliyaNo ratings yet
- 3 2 PDFDocument8 pages3 2 PDFNengLukmanNo ratings yet
- 111 Cardiac Disease in PregnancyDocument7 pages111 Cardiac Disease in PregnancyAfiat WijayaNo ratings yet
- Heart Disease in PregnancyDocument3 pagesHeart Disease in PregnancyNasehah SakeenahNo ratings yet
- Modified World Health Organization (WHO) Classification of Maternal Cardiovascular Risk - ApplicationDocument1 pageModified World Health Organization (WHO) Classification of Maternal Cardiovascular Risk - ApplicationIwi DancelNo ratings yet
- Heart Disease in Pregnancy VoiceoverDocument30 pagesHeart Disease in Pregnancy VoiceoverMohammed AbdNo ratings yet
- 10.1258 Om.2008.080002Document5 pages10.1258 Om.2008.080002ade lydia br.siregarNo ratings yet
- Heart Disease in PregnancyDocument20 pagesHeart Disease in PregnancyAnironOrionNo ratings yet
- Cardio BBDocument73 pagesCardio BBايات عبدالرحمنNo ratings yet
- Medical Diseases Complicating Pregnancy: By: Maysam Hamarsheh DR - FirasDocument22 pagesMedical Diseases Complicating Pregnancy: By: Maysam Hamarsheh DR - Firas'محمد علي' محمد لافيNo ratings yet
- BMJ Insuficiencia Mitral y Estenosis Ao en EmbarazoDocument4 pagesBMJ Insuficiencia Mitral y Estenosis Ao en EmbarazoSol LakosNo ratings yet
- Cardiac Disease in PregnancyDocument19 pagesCardiac Disease in PregnancyCarolina Orjuela Camargo0% (1)
- Short Answer Questions AnaesthesiaDocument91 pagesShort Answer Questions AnaesthesiaMeena Ct100% (12)
- KEMH Guidelines On Cardiac Disease in PregnancyDocument7 pagesKEMH Guidelines On Cardiac Disease in PregnancyAyesha RazaNo ratings yet
- TX Vent Arrhyt in EldDocument11 pagesTX Vent Arrhyt in EldDavy JonesNo ratings yet
- Heart Disease and PregnancyDocument6 pagesHeart Disease and PregnancyBagus Wanda Habibullah100% (1)
- Management of Atrial Fibrilillation: Dr. Dilip Kumar Jain Dr. RajmaniDocument34 pagesManagement of Atrial Fibrilillation: Dr. Dilip Kumar Jain Dr. RajmaniAshish SoniNo ratings yet
- Heart Disease Complicating PregnancyDocument169 pagesHeart Disease Complicating PregnancyRajeev Sood100% (2)
- 2 Chapter20 Pregnant With Preexisting IllnessDocument80 pages2 Chapter20 Pregnant With Preexisting IllnessElgen B. AgravanteNo ratings yet
- Cardiac Disease in PregnancyDocument44 pagesCardiac Disease in PregnancyNariska Cooper100% (1)
- Cardiovascular Diseases in PregnancyDocument27 pagesCardiovascular Diseases in PregnancyAlphine DalgoNo ratings yet
- Heart Disorder in PregnancyDocument15 pagesHeart Disorder in Pregnancyshygirl72No ratings yet
- Wide Qrs Tachy 2Document6 pagesWide Qrs Tachy 2Mohit TandonNo ratings yet
- Heart Disease in PregnancyDocument14 pagesHeart Disease in PregnancyManisha ThakurNo ratings yet
- Marfan ENDocument8 pagesMarfan ENDewinsNo ratings yet
- Mitral Stenosis For Non-Cardiac Surgery Case FileDocument4 pagesMitral Stenosis For Non-Cardiac Surgery Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Cvs-k7-Valvular Heart Disease Nora2010Document52 pagesCvs-k7-Valvular Heart Disease Nora2010shiloinNo ratings yet
- Pacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- MCQ CardioDocument12 pagesMCQ CardioAhmed MahanaNo ratings yet
- (2019) Passmedicine - Passmedicine MRCP Part IDocument6,249 pages(2019) Passmedicine - Passmedicine MRCP Part IAchyut KanungoNo ratings yet
- Acute Coronary Syndromes AlgorithmDocument5 pagesAcute Coronary Syndromes AlgorithmLiuk IrawatiNo ratings yet
- L 7 NephroDocument6 pagesL 7 NephroAhmed Gh Al-zechrawiNo ratings yet
- Ischemic Heart DiseaseDocument116 pagesIschemic Heart Diseasedrmsupriya09115983% (6)
- Mitral Valve SurgeryDocument2 pagesMitral Valve SurgeryLena MarieNo ratings yet
- ECG Basics: Acute Myocardial InfarctionDocument34 pagesECG Basics: Acute Myocardial InfarctionnengninisNo ratings yet
- Renal FailureDocument23 pagesRenal FailurerjfeeleyNo ratings yet
- Cardiovascular Assessment Pocket Reference Card PDFDocument8 pagesCardiovascular Assessment Pocket Reference Card PDFerikaNo ratings yet
- Ton Mitral Valve ReplacementDocument3 pagesTon Mitral Valve ReplacementSony TonNo ratings yet
- Hi-Yield Notes in Im & PediaDocument20 pagesHi-Yield Notes in Im & PediaJohn Christopher LucesNo ratings yet
- 28.03.23 Nephrology SeminarDocument5 pages28.03.23 Nephrology SeminarJerin XavierNo ratings yet
- EKG Primer2woEKGsDocument26 pagesEKG Primer2woEKGsDiana HyltonNo ratings yet
- Chronic Renal FailureDocument40 pagesChronic Renal FailureSarumathy PrabakaranNo ratings yet
- Research Paper On Congenital Heart DiseaseDocument4 pagesResearch Paper On Congenital Heart Diseasetgkeqsbnd100% (1)
- JurnalDocument12 pagesJurnalFKWNo ratings yet
- Shazia Kazi ResumeDocument2 pagesShazia Kazi Resumeshazia kaziNo ratings yet
- Mitral Valve ProlapseDocument3 pagesMitral Valve ProlapseKristine CastilloNo ratings yet
- Diagnosis Dan Tatalaksana Terkini Penyakit Jantung HipertensiDocument8 pagesDiagnosis Dan Tatalaksana Terkini Penyakit Jantung HipertensidhyassNo ratings yet
- 9.b dc2022-0229 Patient Registry For LTO Renewal (PRDR)Document2 pages9.b dc2022-0229 Patient Registry For LTO Renewal (PRDR)Michael Marc Andico DeleonNo ratings yet
- Rapportrein2017 PDFDocument382 pagesRapportrein2017 PDFShareDialysisNo ratings yet
- Glomerular Syndromes PKDocument33 pagesGlomerular Syndromes PKamalasywaq2771No ratings yet
- Department of Education: Individual Workweek Plan August 2021Document5 pagesDepartment of Education: Individual Workweek Plan August 2021Jeffren P. MiguelNo ratings yet
- Acute Coronary Syndrome (Myocardial Infarction and Unstable Angina) (Clinical) - LecturioDocument36 pagesAcute Coronary Syndrome (Myocardial Infarction and Unstable Angina) (Clinical) - Lecturiokujtimepira2No ratings yet
- Chest PainDocument50 pagesChest PainGrafu Andreea AlexandraNo ratings yet
- Introduction of EcgDocument52 pagesIntroduction of Ecgmiss_studyNo ratings yet
- Cardiac Sarcoidosis EHJ Review 2023Document16 pagesCardiac Sarcoidosis EHJ Review 2023AnaNo ratings yet
- DefibrillatorPacemakers, Implantable ResynchronizationDocument110 pagesDefibrillatorPacemakers, Implantable ResynchronizationAbu OdaiNo ratings yet
- Cadrads 2.0 - Rsna - V3Document4 pagesCadrads 2.0 - Rsna - V3Carlos F Muñoz NúñezNo ratings yet
Cardiac Disease Pregnancy Guideline Short
Cardiac Disease Pregnancy Guideline Short
Uploaded by
collins gikunguOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiac Disease Pregnancy Guideline Short
Cardiac Disease Pregnancy Guideline Short
Uploaded by
collins gikunguCopyright:
Available Formats
Cardiac Disease in Pregnancy Guideline - Quick Reference Guide
Women with cardiac disease in pregnancy are at high risk of complications and cardiac disease is
the leading cause of maternal death. This ‘Quick Reference Guide’ summarises the key points
from the Greater Manchester and Eastern Cheshire Maternal Medicine Network guideline which
has been developed to promote seamless, multidisciplinary care for women with cardiac disease in
pregnancy.
Joint obstetric and cardiology clinics
There is a Joint Obstetric Cardiology service at the following hospitals
Hospital Obstetrician Cardiologist Frequency
Wigan Amit Verma Nayyar Naqvi Monthly 3rd Tues am
St Mary’s Hospital Sarah Vause, Prof Clarke, Weekly Tues am
Tel: 0161 276 6426 Anna Roberts Prof Keavney
Risk stratification
Following multidisciplinary assessment and risk stratification, appropriate care can be arranged at
a district general hospital or tertiary unit according to the complexity of the cardiac disease:
Low risk – care and delivery in local hospital, with escalation if clinical deterioration
Moderate risk – refer to joint obstetric cardiac clinic for assessment, but care may be
shared with local hospital
High risk – refer to joint obstetric cardiac clinic for care and delivery in tertiary centre
Low risk Moderate risk High risk
Uncomplicated, small or mild Unoperated atrial or ventricular Mechanical valve
septal defect Systemic right ventricle
- pulmonary stenosis
Repaired tetralogy of Fallot Fontan circulation
- patent ductus arteriosus Most arrhythmias Cyanotic or other complex congenital
Mild left ventricular impairment heart disease
- mitral valve prolapse
Hypertrophic cardiomyopathy Aortic dilatation >=40 mm in Marfan
Successfully repaired simple Native or tissue valvular heart syndrome
disease not considered WHO I Aortic dilatation >=45 mm in non
lesions (atrial or ventricular
or IV Marfan aortopathy
septal defect, patent ductus
arteriosus, anomalous Marfan syndrome without aortic Pulmonary arterial hypertension of
dilatation any cause
pulmonary venous drainage).
Aorta <45 mm in aortic disease Severe systemic ventricular
associated with bicuspid aortic dysfunction (LVEF <30%, NYHA III-
Atrial or ventricular ectopic beats valve IV)
Repaired coarctation Previous peripartum cardiomyopathy
with any residual impairment of left
ventricular function
Severe mitral stenosis, severe
symptomatic aortic stenosis
Native severe coarctation
Pre conception
All women of reproductive age with cardiac disease should have access to specialised
multidisciplinary preconception counselling in a joint obstetric and cardiac clinic, to empower them
to make choices about pregnancy. They should be given advice about contraception and how to
access services rapidly when they become pregnant.
Termination of pregnancy
Rapid access to termination of pregnancy services should be facilitated, if for whatever reason a
woman chooses this. The termination of pregnancy service should be able to provide the
appropriate level of medical care for the severity of the woman’s cardiac disease.
GMEC SCN Cardiac Disease in Pregnancy Guideline_shortversion v1 Final 260118
Antenatal care
All pregnant women with heart disease should be assessed clinically as soon as possible by the
multidisciplinary team.
All pregnant women with cardiac disease requiring treatment or care by other specialists should
have an integrated care plan developed and agreed between all specialities involved.
An escalation and transfer protocol must be available in all units should a woman with cardiac
disease deteriorate during pregnancy or post partum.
Intrapartum care
Senior input and multidisciplinary care are imperative
Aim for a vaginal delivery unless obstetric or cardiac indications for LSCS
Women with cardiac disease should see the obstetric anaesthetist antenatally to discuss
analgesia. When a woman with cardiac disease is admitted to the Delivery Suite the anaesthetic
staff should be involved early.
Fluid balance needs to be assessed accurately using an hourly input/output chart and an hourly
urometer in moderate and high risk cases.
Observations should be charted on a HDU chart in moderate and high risk cases
For some cardiac conditions hypotension is poorly tolerated. Prompt and accurate replacement of
lost volume is necessary. An arterial line may be indicated. This should be specified in the care
plan.
For other cardiac conditions, hypertensive surges may be poorly tolerated. Syntocinon is preferred
to syntometrine. For women with severe heart disease this may need to be given as a slow bolus
(Syntocinon 5u in 20 mls over 20 mins). This should be specified in the care plan.
.
For some women a short active second stage, or no active second stage may be necessary and
vaginal delivery should be assisted with forceps. If needed this should be specified in the care
plan.
Tocolytics, such as nifedipine, may severely compromise cardiac function. The use of tocolytics
should be discussed with the consultant. Atosiban is the tocolytic of choice for women with severe
cardiac disease as it has the least cardiovascular side effects.
Current NICE guidelines state that antibiotic prophylaxis against infective endocarditis should not
be offered for gynaecological and obstetric procedures or childbirth. However, there should be a
low threshold for antibiotic prophylaxis because of the serious nature of endocarditis and the low
risk of anaphylaxis.
For post partum haemorrhage, due to uterine hypotonia, mechanical methods such as bimanual
compression and a B Lynch suture can be used. Misoprostol should be used in preference to
hemabate as it has less vasoactive effects.
Postnatal Care
This is often a time of decompensation; hence close continued observation is appropriate. Staff
should not become complacent. Fluid balance should be monitored closely and there should be
daily medical review. An extended post natal stay may be indicated.
Women with cardiac disease should be supported with breastfeeding, given appropriate
contraception advice and offered lifestyle advice (diet, smoking, exercise).
Medication should be reviewed and appropriate cardiology follow-up arranged prior to discharge
from maternity care. A comprehensive discharge summary should be prepared by the woman’s
obstetrician.
GMEC SCN Cardiac Disease in Pregnancy Guideline_shortversion v1 Final 260118
You might also like
- Uw Step3 NotesDocument34 pagesUw Step3 NotesAakash ShahNo ratings yet
- What Constitutes A Nephrology ClearanceDocument95 pagesWhat Constitutes A Nephrology Clearancegillian102290100% (2)
- Rheumatic Heart Disease in Pregnancy: What Is RHD?Document5 pagesRheumatic Heart Disease in Pregnancy: What Is RHD?dedy chandraNo ratings yet
- Mecca - 606991860Document50 pagesMecca - 606991860Rendy Adhitya PratamaNo ratings yet
- Heart Disease in Pregnancy: Mohana PreeshaDocument50 pagesHeart Disease in Pregnancy: Mohana PreeshaChuks LeviNo ratings yet
- Cardiac Disease in PregnencyDocument35 pagesCardiac Disease in PregnencyMannat ZaidiNo ratings yet
- Pregnancy Cardiovascular ComplicationsDocument13 pagesPregnancy Cardiovascular Complicationsits charitaNo ratings yet
- Cbs Pulm0 h3m@ N0tesDocument26 pagesCbs Pulm0 h3m@ N0tesLINDSLEY GONo ratings yet
- Cardiac Diseases in PregnancyDocument13 pagesCardiac Diseases in PregnancyAbdullah MatarNo ratings yet
- Cardio Vascular Disease in PregnancyDocument57 pagesCardio Vascular Disease in PregnancySanthosh.S.U0% (1)
- Outcome Pada Penyakit Jantung Terhadap Ibu Dan Janin Selama KehamilanDocument28 pagesOutcome Pada Penyakit Jantung Terhadap Ibu Dan Janin Selama KehamilanRaras PraminingrumNo ratings yet
- Heart Failure in Pregnant Women: Is It Peripartum Cardiomyopathy?Document6 pagesHeart Failure in Pregnant Women: Is It Peripartum Cardiomyopathy?NengLukmanNo ratings yet
- Dr. Senthil Priya Heart Disease in Pregnancy FINALDocument68 pagesDr. Senthil Priya Heart Disease in Pregnancy FINALKai ParkerNo ratings yet
- Management of Cardiac Disease in LaborDocument6 pagesManagement of Cardiac Disease in LaborHassan osmanNo ratings yet
- CARDIAC2Document36 pagesCARDIAC2A.H.ANo ratings yet
- Article 10.1111/tog.12599Document8 pagesArticle 10.1111/tog.12599KeeranmayeeishraNo ratings yet
- Cardiac Diseases in PregnancyDocument27 pagesCardiac Diseases in PregnancyHoney May Rollan Vicente50% (2)
- Dr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiDocument35 pagesDr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiNailahRahmahNo ratings yet
- Heart Disease and Bronchial AsthmaDocument45 pagesHeart Disease and Bronchial AsthmaVissalini JayabalanNo ratings yet
- Cardiovascular Disease and Pregnancy Journal o NCM 102Document15 pagesCardiovascular Disease and Pregnancy Journal o NCM 102MichelleIragAlmarioNo ratings yet
- CARDIAC Diseases IN PREGDocument40 pagesCARDIAC Diseases IN PREGStella CooKeyNo ratings yet
- K - 16 Heart Disease in PregnancyDocument19 pagesK - 16 Heart Disease in PregnancyPathrecia Natalia SiagianNo ratings yet
- The Pregnant Woman With Heart Disease: Management of Pregnancy and DeliveryDocument5 pagesThe Pregnant Woman With Heart Disease: Management of Pregnancy and DeliveryMichael SusantoNo ratings yet
- Nursing Acn-IiDocument80 pagesNursing Acn-IiMunawar100% (6)
- Cardiac Disease and Pregnancy: Clinical GuidelinesDocument9 pagesCardiac Disease and Pregnancy: Clinical GuidelinesBagus Wanda Habibullah100% (1)
- 46-M21-Cardiac Diseases During PregnancyDocument35 pages46-M21-Cardiac Diseases During Pregnancyاحمد احمدNo ratings yet
- Heart Diseases in PregnancyDocument70 pagesHeart Diseases in PregnancySergiu HelciugNo ratings yet
- CPG Medical ComplicationsDocument134 pagesCPG Medical ComplicationsAiko EscobidoNo ratings yet
- Management of Rheumatic Heart Disease: Quick Reference Guide For Health ProfessionalsDocument4 pagesManagement of Rheumatic Heart Disease: Quick Reference Guide For Health ProfessionalsgireeshsachinNo ratings yet
- Maternal Risk StratificationDocument59 pagesMaternal Risk StratificationannisNo ratings yet
- Heart Disease in PregnancyDocument5 pagesHeart Disease in PregnancyAngeliqueNo ratings yet
- ACOG Practice Bulletin No. 212 Summary - Pregnancy and Heart DiseaseDocument6 pagesACOG Practice Bulletin No. 212 Summary - Pregnancy and Heart DiseaseYuly Andrea Marquez CastañedaNo ratings yet
- Ventricular TachycardiaDocument17 pagesVentricular TachycardiaAyu Rezki FadliyaNo ratings yet
- 3 2 PDFDocument8 pages3 2 PDFNengLukmanNo ratings yet
- 111 Cardiac Disease in PregnancyDocument7 pages111 Cardiac Disease in PregnancyAfiat WijayaNo ratings yet
- Heart Disease in PregnancyDocument3 pagesHeart Disease in PregnancyNasehah SakeenahNo ratings yet
- Modified World Health Organization (WHO) Classification of Maternal Cardiovascular Risk - ApplicationDocument1 pageModified World Health Organization (WHO) Classification of Maternal Cardiovascular Risk - ApplicationIwi DancelNo ratings yet
- Heart Disease in Pregnancy VoiceoverDocument30 pagesHeart Disease in Pregnancy VoiceoverMohammed AbdNo ratings yet
- 10.1258 Om.2008.080002Document5 pages10.1258 Om.2008.080002ade lydia br.siregarNo ratings yet
- Heart Disease in PregnancyDocument20 pagesHeart Disease in PregnancyAnironOrionNo ratings yet
- Cardio BBDocument73 pagesCardio BBايات عبدالرحمنNo ratings yet
- Medical Diseases Complicating Pregnancy: By: Maysam Hamarsheh DR - FirasDocument22 pagesMedical Diseases Complicating Pregnancy: By: Maysam Hamarsheh DR - Firas'محمد علي' محمد لافيNo ratings yet
- BMJ Insuficiencia Mitral y Estenosis Ao en EmbarazoDocument4 pagesBMJ Insuficiencia Mitral y Estenosis Ao en EmbarazoSol LakosNo ratings yet
- Cardiac Disease in PregnancyDocument19 pagesCardiac Disease in PregnancyCarolina Orjuela Camargo0% (1)
- Short Answer Questions AnaesthesiaDocument91 pagesShort Answer Questions AnaesthesiaMeena Ct100% (12)
- KEMH Guidelines On Cardiac Disease in PregnancyDocument7 pagesKEMH Guidelines On Cardiac Disease in PregnancyAyesha RazaNo ratings yet
- TX Vent Arrhyt in EldDocument11 pagesTX Vent Arrhyt in EldDavy JonesNo ratings yet
- Heart Disease and PregnancyDocument6 pagesHeart Disease and PregnancyBagus Wanda Habibullah100% (1)
- Management of Atrial Fibrilillation: Dr. Dilip Kumar Jain Dr. RajmaniDocument34 pagesManagement of Atrial Fibrilillation: Dr. Dilip Kumar Jain Dr. RajmaniAshish SoniNo ratings yet
- Heart Disease Complicating PregnancyDocument169 pagesHeart Disease Complicating PregnancyRajeev Sood100% (2)
- 2 Chapter20 Pregnant With Preexisting IllnessDocument80 pages2 Chapter20 Pregnant With Preexisting IllnessElgen B. AgravanteNo ratings yet
- Cardiac Disease in PregnancyDocument44 pagesCardiac Disease in PregnancyNariska Cooper100% (1)
- Cardiovascular Diseases in PregnancyDocument27 pagesCardiovascular Diseases in PregnancyAlphine DalgoNo ratings yet
- Heart Disorder in PregnancyDocument15 pagesHeart Disorder in Pregnancyshygirl72No ratings yet
- Wide Qrs Tachy 2Document6 pagesWide Qrs Tachy 2Mohit TandonNo ratings yet
- Heart Disease in PregnancyDocument14 pagesHeart Disease in PregnancyManisha ThakurNo ratings yet
- Marfan ENDocument8 pagesMarfan ENDewinsNo ratings yet
- Mitral Stenosis For Non-Cardiac Surgery Case FileDocument4 pagesMitral Stenosis For Non-Cardiac Surgery Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Cvs-k7-Valvular Heart Disease Nora2010Document52 pagesCvs-k7-Valvular Heart Disease Nora2010shiloinNo ratings yet
- Pacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPacemaker Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- MCQ CardioDocument12 pagesMCQ CardioAhmed MahanaNo ratings yet
- (2019) Passmedicine - Passmedicine MRCP Part IDocument6,249 pages(2019) Passmedicine - Passmedicine MRCP Part IAchyut KanungoNo ratings yet
- Acute Coronary Syndromes AlgorithmDocument5 pagesAcute Coronary Syndromes AlgorithmLiuk IrawatiNo ratings yet
- L 7 NephroDocument6 pagesL 7 NephroAhmed Gh Al-zechrawiNo ratings yet
- Ischemic Heart DiseaseDocument116 pagesIschemic Heart Diseasedrmsupriya09115983% (6)
- Mitral Valve SurgeryDocument2 pagesMitral Valve SurgeryLena MarieNo ratings yet
- ECG Basics: Acute Myocardial InfarctionDocument34 pagesECG Basics: Acute Myocardial InfarctionnengninisNo ratings yet
- Renal FailureDocument23 pagesRenal FailurerjfeeleyNo ratings yet
- Cardiovascular Assessment Pocket Reference Card PDFDocument8 pagesCardiovascular Assessment Pocket Reference Card PDFerikaNo ratings yet
- Ton Mitral Valve ReplacementDocument3 pagesTon Mitral Valve ReplacementSony TonNo ratings yet
- Hi-Yield Notes in Im & PediaDocument20 pagesHi-Yield Notes in Im & PediaJohn Christopher LucesNo ratings yet
- 28.03.23 Nephrology SeminarDocument5 pages28.03.23 Nephrology SeminarJerin XavierNo ratings yet
- EKG Primer2woEKGsDocument26 pagesEKG Primer2woEKGsDiana HyltonNo ratings yet
- Chronic Renal FailureDocument40 pagesChronic Renal FailureSarumathy PrabakaranNo ratings yet
- Research Paper On Congenital Heart DiseaseDocument4 pagesResearch Paper On Congenital Heart Diseasetgkeqsbnd100% (1)
- JurnalDocument12 pagesJurnalFKWNo ratings yet
- Shazia Kazi ResumeDocument2 pagesShazia Kazi Resumeshazia kaziNo ratings yet
- Mitral Valve ProlapseDocument3 pagesMitral Valve ProlapseKristine CastilloNo ratings yet
- Diagnosis Dan Tatalaksana Terkini Penyakit Jantung HipertensiDocument8 pagesDiagnosis Dan Tatalaksana Terkini Penyakit Jantung HipertensidhyassNo ratings yet
- 9.b dc2022-0229 Patient Registry For LTO Renewal (PRDR)Document2 pages9.b dc2022-0229 Patient Registry For LTO Renewal (PRDR)Michael Marc Andico DeleonNo ratings yet
- Rapportrein2017 PDFDocument382 pagesRapportrein2017 PDFShareDialysisNo ratings yet
- Glomerular Syndromes PKDocument33 pagesGlomerular Syndromes PKamalasywaq2771No ratings yet
- Department of Education: Individual Workweek Plan August 2021Document5 pagesDepartment of Education: Individual Workweek Plan August 2021Jeffren P. MiguelNo ratings yet
- Acute Coronary Syndrome (Myocardial Infarction and Unstable Angina) (Clinical) - LecturioDocument36 pagesAcute Coronary Syndrome (Myocardial Infarction and Unstable Angina) (Clinical) - Lecturiokujtimepira2No ratings yet
- Chest PainDocument50 pagesChest PainGrafu Andreea AlexandraNo ratings yet
- Introduction of EcgDocument52 pagesIntroduction of Ecgmiss_studyNo ratings yet
- Cardiac Sarcoidosis EHJ Review 2023Document16 pagesCardiac Sarcoidosis EHJ Review 2023AnaNo ratings yet
- DefibrillatorPacemakers, Implantable ResynchronizationDocument110 pagesDefibrillatorPacemakers, Implantable ResynchronizationAbu OdaiNo ratings yet
- Cadrads 2.0 - Rsna - V3Document4 pagesCadrads 2.0 - Rsna - V3Carlos F Muñoz NúñezNo ratings yet