Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
3 viewsP.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21
P.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21
Uploaded by
mendoza.mmxxiiCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Carla Hernandez Clinical WorksheetDocument2 pagesCarla Hernandez Clinical WorksheetJasmyn Rose100% (1)
- Amniotic Fluid EmbolismDocument10 pagesAmniotic Fluid EmbolismRebecca ApeladoNo ratings yet
- Asphyxia Case StudyDocument8 pagesAsphyxia Case StudySanny Ramos100% (2)
- Impaire Spontaneous VentilationDocument4 pagesImpaire Spontaneous VentilationSkyla FiestaNo ratings yet
- P.01D Foundations of Neonatal Resuscitation Part 1 & 2Document8 pagesP.01D Foundations of Neonatal Resuscitation Part 1 & 2Yndhira Xheyenn LayloNo ratings yet
- CVS Embryology Questions and Study Guide - Quizlet Flashcards by Hugo - OxfordDocument5 pagesCVS Embryology Questions and Study Guide - Quizlet Flashcards by Hugo - OxfordAzizNo ratings yet
- Physiologic Transition From Intrauterine To Extrauterine LifeDocument12 pagesPhysiologic Transition From Intrauterine To Extrauterine Lifeyhojar PisfilNo ratings yet
- P.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21Document9 pagesP.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21mendoza.mmxxiiNo ratings yet
- Neonatal ResuscitationDocument7 pagesNeonatal Resuscitation2012100% (3)
- Physiologic Adaptation of The Newborn and Nursing AssessmentDocument108 pagesPhysiologic Adaptation of The Newborn and Nursing AssessmentRevathi DadamNo ratings yet
- M.02L Neonatal Resuscitation (Dr. Balud) (03!13!2020)Document4 pagesM.02L Neonatal Resuscitation (Dr. Balud) (03!13!2020)mendoza.mmxxiiNo ratings yet
- Birth AsphyxiaDocument7 pagesBirth AsphyxiaAmy LalringhluaniNo ratings yet
- 21 - Normal NewbornDocument10 pages21 - Normal NewbornGen XNo ratings yet
- #10 - NCM109 (Pedia) - TransesDocument70 pages#10 - NCM109 (Pedia) - TransesJaimie BanaagNo ratings yet
- KP 3 2 2 Perubahan Anatomi Fisiologi Sirkulasi Fetus Bayi DewasaDocument30 pagesKP 3 2 2 Perubahan Anatomi Fisiologi Sirkulasi Fetus Bayi DewasaMutammamin UlaNo ratings yet
- Neonatal Resuscitation: Ryan D. Kearney Mark D. LoDocument12 pagesNeonatal Resuscitation: Ryan D. Kearney Mark D. LoAuliaNo ratings yet
- Featl Transition Togdwwdq HvawDocument55 pagesFeatl Transition Togdwwdq HvawmunshiNo ratings yet
- Anatomi Fisiologi Sirkulasi Fetus Bayi Dan Dewasa 2013Document23 pagesAnatomi Fisiologi Sirkulasi Fetus Bayi Dan Dewasa 2013omafdskNo ratings yet
- Foun Ations o Neonata R Esuscitation: What You Will LearnDocument12 pagesFoun Ations o Neonata R Esuscitation: What You Will LearnAndreaNo ratings yet
- Adjustment To Extrauterine LifeDocument4 pagesAdjustment To Extrauterine LifeFrancine LaxaNo ratings yet
- Resiratory Disorders in The NewbornDocument36 pagesResiratory Disorders in The NewbornRaquel CarvalhoNo ratings yet
- Postnatal Cardiovascular AdaptationDocument5 pagesPostnatal Cardiovascular AdaptationChristian MartínezNo ratings yet
- Neonatalresuscitationmanual2 PDFDocument75 pagesNeonatalresuscitationmanual2 PDFSatya Prakash TiwariNo ratings yet
- Resuscitation of The Depressed Newborn: Raleigh, North CarolinaDocument6 pagesResuscitation of The Depressed Newborn: Raleigh, North CarolinaJoulo YabutNo ratings yet
- 2006 Clearance of Fluid From LungsDocument7 pages2006 Clearance of Fluid From LungsyaritzaalviarezNo ratings yet
- 5 NCM207 Fetal CirculationDocument5 pages5 NCM207 Fetal CirculationVhiance Czaramae LahuranNo ratings yet
- Fet Al Circul Ation: 5. Ductus ArteriosusDocument5 pagesFet Al Circul Ation: 5. Ductus ArteriosusVhiance Czaramae LahuranNo ratings yet
- Adjustments of The Infant To Extrauterine LifeDocument11 pagesAdjustments of The Infant To Extrauterine LifeAntoine TimmermansNo ratings yet
- Fetus Circulation LectureDocument28 pagesFetus Circulation LecturecandrastefannNo ratings yet
- From Liquid To Air: Breathing After Birth: A B. P, MD, P G. D, MD, S B. H, P D, C J. M, MDDocument5 pagesFrom Liquid To Air: Breathing After Birth: A B. P, MD, P G. D, MD, S B. H, P D, C J. M, MDmaria jose amayaNo ratings yet
- Pulmonary Edema in Infants and Children: Hugh O'BrodovichDocument4 pagesPulmonary Edema in Infants and Children: Hugh O'Brodovichhectorpaula788No ratings yet
- Disease, Most Often Occurs In: Respiratory Distress SyndromeDocument6 pagesDisease, Most Often Occurs In: Respiratory Distress Syndromejoyrena ochondraNo ratings yet
- OB C. 17 Study GuideDocument12 pagesOB C. 17 Study GuidePaige Nicole GauthreauxNo ratings yet
- Applied Physiology of Newborn ResuscitationDocument8 pagesApplied Physiology of Newborn Resuscitationmichael andres bedoya vergaraNo ratings yet
- Complications in The Transition From Fetal To Neonatal LifeDocument10 pagesComplications in The Transition From Fetal To Neonatal LifeCIRUABCNo ratings yet
- GD - L08 - Disturbance in Neonatal AdaptationDocument14 pagesGD - L08 - Disturbance in Neonatal AdaptationGarry SoloanNo ratings yet
- Fetal CorrectionDocument9 pagesFetal Correctionprabhdeep kaurNo ratings yet
- FetalcirculationDocument32 pagesFetalcirculationannu panchalNo ratings yet
- ncm 107 midtermDocument24 pagesncm 107 midtermNURSING WORKSTUFFSNo ratings yet
- Foetal Adaptations To Extra Uterine LifeDocument14 pagesFoetal Adaptations To Extra Uterine Lifepsy9kfd4d7No ratings yet
- Physiologic Transition From Intrauterine To Extrauterine Life - UpToDateDocument7 pagesPhysiologic Transition From Intrauterine To Extrauterine Life - UpToDateGuilherme Kazuo OgawaNo ratings yet
- PPHNDocument25 pagesPPHNFunda TüzünNo ratings yet
- Resuscitation of The NewbornDocument9 pagesResuscitation of The NewbornKarina Jiménez AyónNo ratings yet
- 2 Newborn Assessment 93667Document122 pages2 Newborn Assessment 93667Izziddin YassineNo ratings yet
- MKT 036Document4 pagesMKT 036عبدالرحمن ابراهيمNo ratings yet
- Questions: Foetal Circulation Anaesthesia Tutorial of The Week 91 18 MAY 2008Document8 pagesQuestions: Foetal Circulation Anaesthesia Tutorial of The Week 91 18 MAY 2008leizt_13No ratings yet
- Newborn Assessment: By: Ledelle M. de Chavez, Claudine M. Francisco & Don Jayric V. DepalobosDocument5 pagesNewborn Assessment: By: Ledelle M. de Chavez, Claudine M. Francisco & Don Jayric V. Depalobosdonskii04No ratings yet
- Update Fetal Circulation - MDM AmyDocument10 pagesUpdate Fetal Circulation - MDM AmyNana Yunus100% (1)
- 2 Paediatrics and Neonatal AnesthesiaDocument87 pages2 Paediatrics and Neonatal Anesthesiahailemichael chekolNo ratings yet
- Obs Gynae Presentation by Roll No 127Document23 pagesObs Gynae Presentation by Roll No 127Siddharth KatyalNo ratings yet
- NEONATAL AND PEDIATRICS PhysiologyDocument45 pagesNEONATAL AND PEDIATRICS PhysiologyAbdulkadir HasanNo ratings yet
- Ses 12 Principles of Newborn Adaption To The Extra-Uterine LifeDocument25 pagesSes 12 Principles of Newborn Adaption To The Extra-Uterine Lifelandegre KNo ratings yet
- Study - Blueprint P2Document26 pagesStudy - Blueprint P2Natasha Drummond100% (1)
- 1 Fetal CirculationDocument21 pages1 Fetal Circulationdr_mohanad100% (1)
- Anatomi Fisiologi SirkulasiDocument20 pagesAnatomi Fisiologi SirkulasiAulia RahmiNo ratings yet
- Chapter 23 ContinuationDocument7 pagesChapter 23 ContinuationArabelle GO100% (1)
- Tumbang KabehDocument57 pagesTumbang KabehArif WicaksanaNo ratings yet
- Adaption of Infants To Extra-Uterine LifeDocument10 pagesAdaption of Infants To Extra-Uterine LifeJulienne QuintaoNo ratings yet
- Paed Respiratory DistressDocument45 pagesPaed Respiratory Distressaboje ochekwuNo ratings yet
- Neonatal Circulation Changes / Unbalanced Circulation: Neonatal Cardiac Conditions: Medical and Surgical ManagementDocument4 pagesNeonatal Circulation Changes / Unbalanced Circulation: Neonatal Cardiac Conditions: Medical and Surgical ManagementAnita Maria UlfaNo ratings yet
- Pleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Covid-19 Contact Tracers Performance Monitoring of Weekly AccomplishmentsDocument1 pageCovid-19 Contact Tracers Performance Monitoring of Weekly AccomplishmentsDancyneall InternetNo ratings yet
- 2012 Global Down Syndrome Foundation Press ClippingsDocument28 pages2012 Global Down Syndrome Foundation Press ClippingsGlobalDownSyndromeNo ratings yet
- Board EamDocument55 pagesBoard Eamjoycevillamor100% (1)
- FluDocument19 pagesFluBenny Lee KennedyNo ratings yet
- 2003 ADA Preconception Care DiabetesDocument3 pages2003 ADA Preconception Care Diabetesannisafaujiah033No ratings yet
- ReimbursementFormA B2016Document7 pagesReimbursementFormA B2016DESIGN CGMPNo ratings yet
- Register Rawat Inap 2020Document327 pagesRegister Rawat Inap 2020carolinaNo ratings yet
- Implementing Improvement Strategies To Prevent Unplanned Extubation in Neonatal Intensive Care Units - SLIDE DECKDocument19 pagesImplementing Improvement Strategies To Prevent Unplanned Extubation in Neonatal Intensive Care Units - SLIDE DECKeman hamzaNo ratings yet
- CPS Info Dimenhydrinate (Gravol)Document5 pagesCPS Info Dimenhydrinate (Gravol)Ann A.No ratings yet
- Semmelweis and HandwashingDocument3 pagesSemmelweis and HandwashingVijay KumarNo ratings yet
- AIIMS June 2002 PG Entrance Question Paper With Answer KeyDocument23 pagesAIIMS June 2002 PG Entrance Question Paper With Answer KeywithraviNo ratings yet
- Hematology 2Document28 pagesHematology 2saad samyNo ratings yet
- Effects of Drugs AbuseDocument6 pagesEffects of Drugs AbuseRamel OñateNo ratings yet
- Pulse OximeterDocument16 pagesPulse OximeterChing Wai Yong100% (1)
- Arrows Consele PDFDocument221 pagesArrows Consele PDFIsai Lara OsoriaNo ratings yet
- Chapter 2 Drug AddictionDocument24 pagesChapter 2 Drug AddictionKaren Joy Francisco HabanaNo ratings yet
- Thrombolytic Therapy For Acute Myocardial Infarction 01-30-13Document1 pageThrombolytic Therapy For Acute Myocardial Infarction 01-30-13Ushnish ChatterjeeNo ratings yet
- Propofol Maintenance TIVA Infusions Kgs-Lbs 03-12-11 LockedDocument1 pagePropofol Maintenance TIVA Infusions Kgs-Lbs 03-12-11 LockedCasandra TudoracheNo ratings yet
- Centers For TherapyDocument2 pagesCenters For TherapyCeline JohnsonNo ratings yet
- Aplio Series Cardiovascular TransducersDocument2 pagesAplio Series Cardiovascular TransducersQaiserAnwarNo ratings yet
- Hypertonic Saline (3% and 5% Sodium Chloride Injection) Drug Information - Description, User Reviews, Drug Side Effects, Interactions - Prescribing Information at RxListDocument2 pagesHypertonic Saline (3% and 5% Sodium Chloride Injection) Drug Information - Description, User Reviews, Drug Side Effects, Interactions - Prescribing Information at RxListMuhammad AsadNo ratings yet
- 30073665: Colloids Versus Crystalloids For Fluid Resuscitation in Critically Ill People PDFDocument210 pages30073665: Colloids Versus Crystalloids For Fluid Resuscitation in Critically Ill People PDFAngel VelásquezNo ratings yet
- Trigeminal NeuralgiaDocument16 pagesTrigeminal NeuralgiaJerry AbleNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanTrisNo ratings yet
- Lasik GuidelinesDocument4 pagesLasik GuidelinesIlmiahdmobgyn MaretmeiNo ratings yet
- Nazi ExperimentsDocument3 pagesNazi ExperimentsAngel SarteNo ratings yet
- Pavlik Harness Initiation On Barlow Positive Hips - Can We Wait?Document15 pagesPavlik Harness Initiation On Barlow Positive Hips - Can We Wait?Irene AntoniNo ratings yet
- NCP (Afp)Document7 pagesNCP (Afp)Summer SuarezNo ratings yet
P.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21
P.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21
Uploaded by
mendoza.mmxxii0 ratings0% found this document useful (0 votes)
3 views9 pagesCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
3 views9 pagesP.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21
P.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21
Uploaded by
mendoza.mmxxiiCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 9
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
P.01 FOUNDATIONS OF NEONATAL RESUSCITATION Alveoli is filled with lung fluid instead of air, and therefore no
(Part 1&2) gas exchange happens between the fetal lung and
Dr. Balud | 01/17/2021 pulmonary circulation. Instead, oxygen is transferred from
the maternal circulation to the fetal circulation via the
OUTLINE placenta
I. Neonatal Resuscitation Fetus are adapted to low po2 (20 mmHg)
II. Why do newborns require different approach to In utero, fetus dependent on placenta for gas exchange
resuscitation? Pulmonary arterioles are constricted:
III. Fetal Physiology o Since the alveoli are filled with fluid, the
IV. After Baby’s Birth surrounding pulmonary capillaries, arterioles and
V. Normal Transition venules are constricted
VI. What can go wrong during transition? Pulmonary blood flow is diminished:
VII. Signs of A Compromised Newborn o Because of this, there is marked decrease in blood
VIII. In Utero or Prenatal Compromise flow into the lungs
IX. Resuscitation Flow Diagram Blood flow is diverted across the patent ductus arteriosus:
X. Pre-resuscitation Preparation o Because of this hypertensive state, blood that is
XI. Neonatal Resuscitation supposed to flow to the lungs is then diverted into
the aorta via the patent ductus arteriosus, diluting
OBJECTIVES: further the oxygen concentration of the blood in
Importance of resuscitation skills the aorta
Physiologic changes during and after birth
Neonatal Resuscitation Flow diagram format FROM THE ATTACHED VIDEO CLIP:
Communication and teamwork skills used by effective Because of the constricted blood vessels in the lungs, most
resuscitation teams of the blood bypasses the lungs, and instead passes into the
aorta via the ductus arteriosus
I. NEONATAL RESUSCITATION
NEONATAL DEATHS
45% of under-five deaths in 2015
35%of under-five deaths in 2015
WHY LEARN NEONATAL RESUSCITATION?
Birth asphyxia 23% of approximately 4M neonatal
deaths/year worldwide
For many NB appropriate resuscitation not readily available
o Improved by more widespread use of resuscitation
techniques
WHICH BABIES REQUIRE RESUSCITATION?
ALL newborns (NB)require assessment
Figure 1: Fetal Circulation Anatomy
~10%of NB requires some assistance to begin breathing at
birth
<1%need extensive resuscitative measures to survive
IV. AFTER BABY’S BIRTH
A. LUNGS AND CIRCULATION AFTER DELIVERY
II. WHY DO NEWBORNS REQUIRE DIFFERENT APPROACH TO
Fetal lung fluid leaves alveoli:
RESUSCITATION?
o At birth, as the newborn takes the first few
A. ADULT CARDIAC ARREST
breaths, several changes occur, whereby the lungs
Most often a complication of trauma or existing heart
take over the lifelong function of respiration.
disease
o Following birth, the lungs expand as they filled
o A sudden arrhythmia → ineffective heart
with air. The fetal lung fluid gradually leaves the
contraction → decreased cardiac output and most
alveoli.
importantly, brain circulation → loss of
o Hematogenous
consciousness → stops breathing
o Lymphatics
o During the arrest, O 2 and CO2in the blood are
o Aspiration
usually normal
o Vaginal squeeze
o Chest compressions are needed to be started
o Expelled
immediately in order to maintain circulation until
electrical defibrillations or medications restore
Lung expands with air:
cardiac functions
o It is important that the bay takes the initial
respiration immediately for a more efficient
B. NEWBORNS NEEDING RESUSCITATION
clearing of the alveolar fluid from the baby’s lungs.
Most newborns requiring resuscitation have a healthy heart
o Otherwise, fluid will be retained and may cause
Newborns requiring resuscitation have a problem in
unwanted complications such as transient
respiration, in contrast to adults whose main problem is
tachypnea or worse, persistent pulmonary
cardiac→ inadequate gas exchange
hypertension of the newborn.
o Respiratory failure may occur before or during
birth
FROM THE ATTACHED VIDEO CLIP:
o Placenta responsible for in utero respiration
Fluid in the alveoli is absorbed into the lung tissue, and
replaced by air. The oxygen in the air diffuses into blood
vessels that surround the alveoli.
III. FETAL PHYSIOLOGY
A. IN THE FETUS
PEDIA II|1of 9 [MALINGAN, MENDOZA, ASPURIA]
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
Blood oxygen levels rise:
o And since the lungs now take over the function of
the placenta for gas exchange, the pulmonary
blood now will be increasingly oxygenated.
Ductus arteriosus now constricts:
o This increase in the oxygen concentration on the
blood will now cause a constriction of the ductus
arteriosus, which will usually be completed by the
10th day of life
Blood flow through the lungs to pick up oxygen:
o There will now be increased blood flow through
the lungs to pick up oxygen for peripheral
circulation.
Figure 2: Constricted Blood Vessels and Fluid-filled Alveoli
FROM THE ATTACHED VIDEO CLIP:
As blood levels of oxygen increase and pulmonary blood
vessels relax, the ductus arteriosus begins to constrict.
Blood previously diverted through the ductus arteriosus, now
flows through the lungs where it picks up more oxygen to
transport to tissues throughout the body.
Figure 3: Infant’s First Breath with Fetal Lung Fluid
Figure 7: Fetal Lung and Circulation Before Birth
Figure 4: Infant’s Second Breath with Air
Figure 8: Fetal Lung and Circulation After Birth
Pulmonary arterioles dilate
Pulmonary blood flow increases
o As a consequence of the clearance of the alveolar
fluid leaving the alveoli, the pulmonary vessels
now relax, and thus allows increase in pulmonary
blood flow.
Figure 5: Infant’s Subsequent Breaths with Air
Figure 6: Dilated Blood Vessels After Birth with Oxygen in
Alveoli Figure 9: Alveoli Before and After Birth
PEDIA II|2of 9 [MALINGAN, MENDOZA, ASPURIA]
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
When babies are deprived of oxygen (in utero or after
delivery), they undergo a well-defined sequence of events
V. NORMAL TRANSITION that starts with cessation of respiration.
The following 3 major changes take place within seconds During primary apnea, the newborn responds to stimulation.
after birth: Instruction Tip: Initiate resuscitation immediately.
o Alveolar fluid is absorbed into lung tissue and Resuscitation may be inappropriately delayed if the health
replaced by air care provider does not recognize the need for neonatal
o Umbilical arteries and vein constrict thus resuscitation. Any delay in transferring a compromised
increasing blood pressure: Umbilical arteries and newborn to the resuscitation team is unacceptable practice.
veins are clamped, removing the low resistance
placental circuit and increasing systemic blood B. SECONDARY APNEA
pressure. Continued O2 deprivation → secondary apnea + continued
o Blood vessels in the lungs relax, increasing fall in heart rate and blood pressure
pulmonary blood flow. Secondary apneaCANNOT be reversed by tactile
stimulation; assisted ventilation must be provided
VI. WHAT CAN GO WRONG DURING TRANSITION If oxygen deprivation continues, deep gasping respirations
Lack of ventilation of the newborn’s lungs → sustained develop, the heart rate continues to decrease, and the blood
constriction of the pulmonary arterioles → prevents systemic pressure decreases
arterial blood from being oxygenated An important point is that, during secondary apnea,
Prolonged lack of adequate perfusion and oxygenation → stimulation will not restart the baby’s breathing. Assisted
damage to brain, damage to other organs, or death ventilation must be provided to reverse the process
A baby may encounter difficulty before labor, during labor, triggered by oxygen deprivation. If a baby doesn’t begin to
or after birth. Some of the problems that may disrupt normal breathe immediately after being stimulated, he or she is
transition are: likely in secondary apnea and will require positive-pressure
o The baby may not breathe sufficiently to force ventilation.
fluid from the alveoli, or foreign material such as Instructor Tip: Quickly achieve and maintain oxygenation in
meconium that may prevent air from entering the full-term and post-term newborns after perinatal hypoxia-
alveoli. ischemia because they are especially prone to persistent
o Excessive blood loss may occur, or there may be pulmonary hypertension.
inadequate cardiac contractility, or bradycardia Initiation of effective POSITIVE PRESSURE
from hypoxia and ischemia. VENTILATION during secondary apnea usually results in:
RAPID IMPROVEMENT IN HEART RATE
VII. SIGNS OF A COMPROMISED NEWBORN Most babies in secondary apnea will respond to effective
The compromised baby may exhibit one or more of the ventilation with a rapid improvement in heart rate.
following clinical findings: The longer a baby has been in secondary apnea, the longer
o Poor muscle tone it will take for spontaneous breathing to resume.
o Depressed respiratory drive due to insufficient If heart rate does not improve rapidly with effective
oxygen reaching the brain ventilation, myocardial function may be compromised and
o Bradycardia chest compressions and/or medications may be required.
o Low blood pressure
o Tachypnea (rapid respirations) IX. RESUSCITATION FLOW DIAGRAM
o Cyanosis (blue color) Initial Assessment:
Words of caution: Other conditions, such as infection, o Determine if the baby can remain with the mother
hypoglycemia, or depressant drugs given to the mother or should be moved to a radiant warmer for
before birth, may also cause these symptoms. further evaluation
Airway:
o Perform the initial steps to establish an open
airway and support spontaneous respiration
Breathing:
o Positive pressure ventilation is provided to assist
breathing for babies with apnea or bradycardia
o Other interventions (CPAP: Continuous Positive
Airway Pressure or oxygen) maybe appropriate if
baby is breathing spontaneously but has labored
breathing (CPAP) or low oxygen saturation
(oxygen)
Circulation:
o If severe bradycardia persists despite assisted
ventilation, circulation is supported by performing
chest compressions, coordinated with PPV
(Positive Pressure Ventilation)
Drugs:
o If severe bradycardia persists despite assisted
Figure 10: Good Tone with Cyanosis VS Bad Tone with ventilation and coordinated chest compressions,
Cyanosis the drug EPINEPHRINE is administered as PPV and
chest compressions continue
VIII. IN UTERO OR PRENATAL COMPROMISE
A. PRIMARY APNEA
When a fetus/newborn first becomes deprived of oxygen, an
initial period of attempted rapid breathing occurs, followed
by primary apnea with dropping of heart rate. This improves
with TACTILE STIMULATION.
PEDIA II|3of 9 [MALINGAN, MENDOZA, ASPURIA]
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
X. PRE-RESUCITATION PREPARATION resuscitated will not make it, and other sensitive
FOCUS ON TEAMWORK information.
Poor teamwork and communication were the most
common root causes for potentially preventable infant EFFECTIVE COMMUNICATION
deaths in the delivery room Every team member shares responsibility for ongoing
Therefore, one of the emphasis also of the neonatal assessment
resuscitation program, whether it be the AAP or NRPh+ Share information: communicate with each other
version is the planning on how the team will be contacted, Direct request to a specific individual
who will be responding. And that before entering any Call team member by name
resuscitation calls or codes, each team members need to Make eye contact
understand his role and tasks he or she will be assigned. Speak clearly
Ask receiver to report back as soon as the task is completed.
PERSONNEL AND EQUIPMENT
ALL deliveries should be attended by at least 1 person whose only In order to have effective communication, again, every team
responsibility is the baby and who is capable of initiating member shares responsibility for ongoing assessment. If you were
resuscitation. Either that person or someone else, who is available the one who took the history it is your responsibility to share what
immediately, should have the skills required to perform a pertinent information should be shared with each team member.
complete resuscitation For example, the mother is Hepatitis B positive, then this should be
Prepare necessary equipment: shared to each member of the team especially those that will handle
o Turn on radiant warmer anything with blood, so that they will have to take necessary
o Set delivery room temperature to 26°C precautions like wearing of gloves and goggles. Or if the mother is
o Check the equipment COVID suspect, of has positive COVID swab, then every member of
the team should be alerted to be able to wear the proper protective
PRE-RESUCITATION BRIEFING equipment.
Planning how the team will be contacted and who will It would be better if we put our name on our chest area so that
respond we can call each other by name, and direct our request to a specific
Each team member needs to understand his role and the individual. Make an eye contact when talking to your members,
tasks he or she will be assigned. You try to identify the role speak clearly, and ask the receiver to report back as soon as the
of each member of the resuscitation team. Who will be there task is completed. For example, the leader orders: Gilbert, please
during the catch, and where will the help be contacted and administer epinephrine 1:10,000 dilution, 0.5 mL via the umbilical
how. catheter bolus now. Then after Gilbert does his task, he echoes by
Assess perinatal risk factors so that you will know what to saying epinephrine, 1:10,000 0.5mL given via umbilical catheter.
anticipate.
Identify a team leader ACCURATE DOCUMENTATION
Delegate tasks: who is responsible to do the initial steps of Complete records are important for clinical decision making
resuscitation and positive pressure ventilation, who will be and source for quality improvement data for the future
doing the chest compressions, where will these people be Events during resuscitation documented as they occur;
positioned with respect to the baby, who will document all supplemented with retrospective narrative summary
the things going on during the resuscitation, who will be the Use single time reference to avoid confusion, especially
timer, who will be the nurse who is responsible for the when data is to be used for court cases
supplies and equipment, are all the equipment already Recorder should not be responsible for other roles (assigned
within reach? If not, then identify which are not available to experienced team member) as she needs to focus and not
and make sure to replenish them even before the delivery is be distracted as she documents the resuscitation
called, on when and how to and the proper way of Use well designed forms that follow NRP / NRPH+ flow
substituting the chest compressor. It would also be best if diagram for more rapid data entry
you already perform a mock code to orient you on how to go
about during the actual resuscitation. POST-RESUSCITATION DEBRIEFING
Identify who will document events as they occur Reinforces good teamwork habits and helps team identify
Determine what supplies and equipment will be needed areas of improvement for future resuscitations
Identify how to call for additional help Quick debriefing immediately after the event and a more
comprehensive debriefing may be scheduled afterward
TEAM LEADER Debriefings do not have to find major problems to be
Mastery of the Neonatal Resuscitation Program (NRP) Flow effective
Diagram o May identify series of small changes that result in
Effective leadership skills – good communication skill significant improvements in your team’s performance
o Clear directions: clear, direct and audible enough
o Share information with other members of the team,
for example, he should mention to the members of the
team that they should be wearing gloves because the
mother is a diagnosed case of HIV for their protection;
he should not be withholding such information from the
members of the team or else he will lose their trust.
o Delegate responsibilities ensuring coordinated
care
o Maintaining professional environment
Remain aware of entire clinical situation, not only about how
long the duration of the resuscitation is going on.
Maintain view of big picture (not distracted by single activity)
The leader should also be aware of other circumstances like
knowing that the baby is a precious child, wherein the
mother is already in her mid 40s and may not be able to
conceive a child anymore should this baby being
PEDIA II|4of 9 [MALINGAN, MENDOZA, ASPURIA]
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
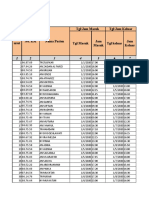
Category II or III fetal heart Shoulder dystocia
pattern
Maternal general anesthesia Meconium-stained amniotic fluid
Maternal magnesium therapy Prolapsed umbilical cord
Placental abruption
WHAT QUESTIONS TO ASK BEFORE EVERY BIRTH
What is the expected gestational age?
o Preterm: then you will need equipment particularly for
thermoregulation, assisting the breathing of the baby,
surfactant, umbilical venous catheter insertion and the
like.
o Postmature: then you will expect the baby to be
possibly meconium-stained if not aspirated meconium
already and that the baby might be born limp and will
require assistance in the initiation of breathing.
Is the amniotic fluid clear?
o A clear amniotic fluid would make the resuscitating
team at ease. But a meconium-stained fluid will
keep them on their toes as they will now need to
assess if the baby, upon birth, is active or limp.
How many babies are expected?
o Knowing the answer to this will make the team prepare
or additional team if we are expecting multiple
pregnancy, as compared to when this is a singleton
pregnancy.
Are there any additional risk factors?
o Does the mother have SLE? Was the baby antenatally
diagnosed to have congenital anomalies that will hinder
the normal transition process, does the baby need an
immediate surgical intervention upon birth, so that we
need the surgery team on stand by at the time the
baby is delivered?
Figure 11: Debriefing form.
Where questions are asked about what was the best part of the
RESUSCITATION TEAM
resuscitation event, what was the most challenging part, what areas
Every birth should be attended by at least 1 qualified
still need to be worked upon for improvement. (There are different
individual, skilled in the initial steps of newborn care and
available templates of debriefing form online, and your institution may
PPV, whose only responsibility is the management of the
have its own debriefing form being used)
newborn baby.
o This individual should be skilled in performing the initial
steps of newborn care and positive pressure ventilation.
XI. NEONATAL RESUSCITATION
If risk factors are present, at least 2 qualified people
PERINATAL FACTORS INCREASING THE LIKELIHOOD OF
should be at the delivery room, plus another members of the
NEONATAL RESUSCITATION
team on standby nearby. Again, these two qualified people
should be only managing the newly born baby.
It is ideal to know if there are any risk factors surrounding the
Qualified team should have at least one with full
birth of the baby so that the pediatric team would be ready, be able to
resuscitation skills, including endotracheal intubation,
organize a resuscitation team way before the birth of the baby,
chest compressions, emergency vascular access and
delegate task to each members of the team, check for the supplies and
medication administration, should be identified and
equipment and their functionality. But often times, in the real world,
immediately available for every resuscitation and should not
there are instances when the mother arrives at the emergency room
be on an on-call basis.
about to give birth, giving the pediatric team insufficient time to fully
organize a resuscitation team, much less delegate a task or have a
briefing. PRE-RESUSCITATION TEAM BRIEFING
Review the risk factors and management plans developed
ANTENATAL RISK FACTORS during antenatal counselling (during the briefing before
Gestational age <36 0/7 weeks Oligohydramnios entering the delivery room)
Gestational age >41 0/7 weeks Fetal hydrops o For example, you have a baby who had an
Preeclampsia or eclampsia Fetal macrosomia antenatal diagnosis of gastroschisis, and who is
Maternal hypertension Intrauterine growth restriction about to be delivered via NSD, aside from
Multiple gestation Significant fetal malformation or organizing the pediatric resuscitation team, you
anomalies ought also to have consulted a pediatric surgeon
Fetal anemia
prior to the delivery. The parents should have
Polyhydramnios No prenatal care
consulted this surgeon, who in turn will explain to
INTRAPARTUM RISK FACTORS
the parents what will be anticipated, whether they
Emergency cesarean delivery Intrapartum bleeding
will do direct closure of the defect immediately at
Forceps or vacuum-assisted Chorioamnionitis birth, or will they do a staged reduction of the
delivery intestines and perform the primary closure later.
Breech or other abnormal Narcotics administered to Identify team leader (based on the characteristics discussed
presentation mother within 4 hours of before), discuss the possible scenarios that your team may
delivery encounter, assign roles and responsibilities
PEDIA II|5of 9 [MALINGAN, MENDOZA, ASPURIA]
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
o Who will perform initial assessment beyond positive pressure ventilation, the nurse in charge
o Who will stimulate the baby should already lay out the equipment for better access
o Who will start PPV if needed during cannulation of the umbilical vessels.
o Who will document events: it would be best to For extremely preterm infants, aside from preferably
have a prepared documentation form or template using a blade double 0, be ready as well with a food-grade
for easier input of the data during the actual plastic bag, (or the resealable bag) which will be used to
resuscitation event. wrap the preterm upon birth for thermoregulation.
Remember that extremely preterm infants have weaker
muscle tone which causes now extension of all extremities,
RESUSCITATION SUPPLIES AND EQUIPMENT
increasing the body surface area, hence bigger area loss. We
Supplies and equipment should be prepared and checked
counter that disadvantage by trying to prevent all heat loss.
if functional. And when in the delivery room, it is already
An alternative will be to wrap the baby with plastic wrap.
laid out in such a way that when it is needed, it is already
If thermal mattress is also available, then it would be useful
within reach and without the necessity to look for it first
to use it while resuscitating a small preterm for heat
when asked by the team leader.
In areas where transport incubator may not be
Most important thing to check will be the bag-mask
available in transporting the baby to the nursery for more
apparatus, be sure that it really works, and you are using
intensive care, a close relative, preferably the father may
the appropriate volume. The 200-mL bag is for the
be asked to carry the baby, kangaroo-mother-care or
newborn, whereas the 700 mL is for older infants and
skin-to-skin-contact style in order to minimize
pediatric patients. Please don’t interchange.
evaporative heat loss during transport.
For the laryngoscope, make sure that the bulb has a
strong light, batteries should be changed regularly.
The blade appropriate to use for newborns would be UMBILIVAL VESSEL MISCELLANEOUS
straight compared to older children and adults where the CATHETERIZATION
curved blade is preferred. This is due to the peculiarity of Sterile gloves Gloves and appropriate personal
the anatomy of their larynx, especially of the epiglottis. An protection
extremely premature infant , or those who are less than Anti-septic prep solution Radiant warmer or other heat
28 weeks gestational age, would require a blade double sources
0. Bigger preterm infants will require blade 0, whereas Umbilical tape Temperature sensor with sensor
term infants would require blade 1. cover for radiant warmer (for
use during prolonged
SUCTION EQUIPMENT POSITIVE PRESSURE resuscitation)
VENTILATION EQUIPMENT Small clamp (hemostat) Firm, padded resuscitation
Bulb syringe Device for delivering PPV surface
Mechanical suction and tubing Face masks, newborn & preterm Forceps (optional) Timer or clock with second hand
sizes warmed linens
Suction, catheters, 5F or 6F, Oxygen source Scalpel Beanie
10F, 12F or 14F Umbilical catheters 3.5F, 5F Stethoscope
8F feeding tube or large syringe Compressed air source Three-way stop cock Tape ¾ or ½ inch
Meconium aspirator Oxygen blender to mix O2 & CA Syringes 3-ml, 5ml ECG monitor and ECG leads
with flowmeter & tubing Needle or puncture device for Intraosseous needle (optional)
Pulse oximeter with sensor & needleless system
cover NSS for flushes
Target O2 saturation table Clear adhesive dressing to
INTUMATION EQUIPMENT MEDICATIONS temporarily secure umbilical
Laryngoscope with straight Epinephrine 1:10,000 (Since the venous catheter to abdomen
blades, No 0 & No 1 commercially available (optional)
epinephrine is 1:1000 FOR VERY PREMATURE INFANTS
concentration, it would be best Size 00-laryngoscope blades (optional)
to have a pre-mixed 1:10,000) Food grade plastic blade (1-gallon size) or plastic wrap
Extra bulbs & batteries for NSS for volume expansion Thermal mattress
laryngoscope Transport incubator to maintain baby’s temperature during move to
Stylet (optional) D10W (optional) the nursery
Measuring tape NSS for flushes
Endotracheal tube insertion Syringes 1-ml, 3-ml, 5-ml to 60-
depth table ml FOCUS ON TEAMWORK
Scissors
Waterproof tape or tube- BEHAVIOR EXAMPLE
securing device • Anticipate and plan • Identify the risk factors so
Scissors that this will preempt you
Waterproof tape or tube- how to plan the resuscitation
securing device • Know which providers will be
Alcohol pads called to attend the birth
CO2 detector or capnograph based on the perinatal risk
Laryngeal mask and 5-ml factors
syringe • Perform a standardized
5F or 6F OGT if insertion port equipment check before
present on LM every birth
• Assign roles and
Be on the ready as well with the equipment for umbilical responsibilities (You can post
vessel catheterization. As the resuscitation progresses at the inner side of the
PEDIA II|6of 9 [MALINGAN, MENDOZA, ASPURIA]
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
nursery door the composition • Clearly identify the leader • If risk factors are present,
of the resuscitation team and identify a leader before the
their designated roles and birth and perform a pre-
responsibilities) resuscitation team briefing (&
mock resuscitation during
your free time so as to
master the correct sequence
of things) to ensure that
• Use all available information • A good history investigation everyone is prepared, and
• Use available resources prior to birth will be very responsibilities are defined.
useful in anticipating every
move inside the delivery NRP KEY BEHAVIORAL SKILLS
room Know your environment
• Ask the obstetric provider the Use available information
4 pre-birth questions to Anticipate and plan
identify risk factors and align Clearly identify a team leader
your preparation based on Communicate effectively
the risk factors provided. Delegate workload optimally
• Prepare additional supplies Allocate attention wisely
and equipment as necessary, Use available resources
based on these risk factors Call for additional help when needed
• If the baby has gastroschisis, Maintain professional behavior
then you might need already
the presence of pediatric
surgeon at the delivery room
as well
• Know your environment • Orienting yourself with the
nursery and its set-up prior to
starting to work in it
• Know how the resuscitation
team is called and how
additional personnel and
resources can be summoned.
• Know how to access
additional equipment and
supplies for a complex
resuscitation
PEDIA II|7of 9 [MALINGAN, MENDOZA, ASPURIA]
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
APPENDIX
PEDIA II|8of 9 [MALINGAN, MENDOZA, ASPURIA]
PEDIATRICS II
Saint Louis University School of Medicine MMXXII
This is the local version of the resuscitation flow diagram
that was created for the Philippines. This simplifies the
complicated flow diagram of the AAP and AHA.
Both algorithms emphasizes that the baby should already
have established breathing during the first 60 seconds of
life. If not yet, then we go down the resuscitation pathway
as outlined.
PEDIA II|9of 9 [MALINGAN, MENDOZA, ASPURIA]
You might also like
- Carla Hernandez Clinical WorksheetDocument2 pagesCarla Hernandez Clinical WorksheetJasmyn Rose100% (1)
- Amniotic Fluid EmbolismDocument10 pagesAmniotic Fluid EmbolismRebecca ApeladoNo ratings yet
- Asphyxia Case StudyDocument8 pagesAsphyxia Case StudySanny Ramos100% (2)
- Impaire Spontaneous VentilationDocument4 pagesImpaire Spontaneous VentilationSkyla FiestaNo ratings yet
- P.01D Foundations of Neonatal Resuscitation Part 1 & 2Document8 pagesP.01D Foundations of Neonatal Resuscitation Part 1 & 2Yndhira Xheyenn LayloNo ratings yet
- CVS Embryology Questions and Study Guide - Quizlet Flashcards by Hugo - OxfordDocument5 pagesCVS Embryology Questions and Study Guide - Quizlet Flashcards by Hugo - OxfordAzizNo ratings yet
- Physiologic Transition From Intrauterine To Extrauterine LifeDocument12 pagesPhysiologic Transition From Intrauterine To Extrauterine Lifeyhojar PisfilNo ratings yet
- P.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21Document9 pagesP.01 Foundations of Neonatal Resuscitation Dr. Balud 01-17-21mendoza.mmxxiiNo ratings yet
- Neonatal ResuscitationDocument7 pagesNeonatal Resuscitation2012100% (3)
- Physiologic Adaptation of The Newborn and Nursing AssessmentDocument108 pagesPhysiologic Adaptation of The Newborn and Nursing AssessmentRevathi DadamNo ratings yet
- M.02L Neonatal Resuscitation (Dr. Balud) (03!13!2020)Document4 pagesM.02L Neonatal Resuscitation (Dr. Balud) (03!13!2020)mendoza.mmxxiiNo ratings yet
- Birth AsphyxiaDocument7 pagesBirth AsphyxiaAmy LalringhluaniNo ratings yet
- 21 - Normal NewbornDocument10 pages21 - Normal NewbornGen XNo ratings yet
- #10 - NCM109 (Pedia) - TransesDocument70 pages#10 - NCM109 (Pedia) - TransesJaimie BanaagNo ratings yet
- KP 3 2 2 Perubahan Anatomi Fisiologi Sirkulasi Fetus Bayi DewasaDocument30 pagesKP 3 2 2 Perubahan Anatomi Fisiologi Sirkulasi Fetus Bayi DewasaMutammamin UlaNo ratings yet
- Neonatal Resuscitation: Ryan D. Kearney Mark D. LoDocument12 pagesNeonatal Resuscitation: Ryan D. Kearney Mark D. LoAuliaNo ratings yet
- Featl Transition Togdwwdq HvawDocument55 pagesFeatl Transition Togdwwdq HvawmunshiNo ratings yet
- Anatomi Fisiologi Sirkulasi Fetus Bayi Dan Dewasa 2013Document23 pagesAnatomi Fisiologi Sirkulasi Fetus Bayi Dan Dewasa 2013omafdskNo ratings yet
- Foun Ations o Neonata R Esuscitation: What You Will LearnDocument12 pagesFoun Ations o Neonata R Esuscitation: What You Will LearnAndreaNo ratings yet
- Adjustment To Extrauterine LifeDocument4 pagesAdjustment To Extrauterine LifeFrancine LaxaNo ratings yet
- Resiratory Disorders in The NewbornDocument36 pagesResiratory Disorders in The NewbornRaquel CarvalhoNo ratings yet
- Postnatal Cardiovascular AdaptationDocument5 pagesPostnatal Cardiovascular AdaptationChristian MartínezNo ratings yet
- Neonatalresuscitationmanual2 PDFDocument75 pagesNeonatalresuscitationmanual2 PDFSatya Prakash TiwariNo ratings yet
- Resuscitation of The Depressed Newborn: Raleigh, North CarolinaDocument6 pagesResuscitation of The Depressed Newborn: Raleigh, North CarolinaJoulo YabutNo ratings yet
- 2006 Clearance of Fluid From LungsDocument7 pages2006 Clearance of Fluid From LungsyaritzaalviarezNo ratings yet
- 5 NCM207 Fetal CirculationDocument5 pages5 NCM207 Fetal CirculationVhiance Czaramae LahuranNo ratings yet
- Fet Al Circul Ation: 5. Ductus ArteriosusDocument5 pagesFet Al Circul Ation: 5. Ductus ArteriosusVhiance Czaramae LahuranNo ratings yet
- Adjustments of The Infant To Extrauterine LifeDocument11 pagesAdjustments of The Infant To Extrauterine LifeAntoine TimmermansNo ratings yet
- Fetus Circulation LectureDocument28 pagesFetus Circulation LecturecandrastefannNo ratings yet
- From Liquid To Air: Breathing After Birth: A B. P, MD, P G. D, MD, S B. H, P D, C J. M, MDDocument5 pagesFrom Liquid To Air: Breathing After Birth: A B. P, MD, P G. D, MD, S B. H, P D, C J. M, MDmaria jose amayaNo ratings yet
- Pulmonary Edema in Infants and Children: Hugh O'BrodovichDocument4 pagesPulmonary Edema in Infants and Children: Hugh O'Brodovichhectorpaula788No ratings yet
- Disease, Most Often Occurs In: Respiratory Distress SyndromeDocument6 pagesDisease, Most Often Occurs In: Respiratory Distress Syndromejoyrena ochondraNo ratings yet
- OB C. 17 Study GuideDocument12 pagesOB C. 17 Study GuidePaige Nicole GauthreauxNo ratings yet
- Applied Physiology of Newborn ResuscitationDocument8 pagesApplied Physiology of Newborn Resuscitationmichael andres bedoya vergaraNo ratings yet
- Complications in The Transition From Fetal To Neonatal LifeDocument10 pagesComplications in The Transition From Fetal To Neonatal LifeCIRUABCNo ratings yet
- GD - L08 - Disturbance in Neonatal AdaptationDocument14 pagesGD - L08 - Disturbance in Neonatal AdaptationGarry SoloanNo ratings yet
- Fetal CorrectionDocument9 pagesFetal Correctionprabhdeep kaurNo ratings yet
- FetalcirculationDocument32 pagesFetalcirculationannu panchalNo ratings yet
- ncm 107 midtermDocument24 pagesncm 107 midtermNURSING WORKSTUFFSNo ratings yet
- Foetal Adaptations To Extra Uterine LifeDocument14 pagesFoetal Adaptations To Extra Uterine Lifepsy9kfd4d7No ratings yet
- Physiologic Transition From Intrauterine To Extrauterine Life - UpToDateDocument7 pagesPhysiologic Transition From Intrauterine To Extrauterine Life - UpToDateGuilherme Kazuo OgawaNo ratings yet
- PPHNDocument25 pagesPPHNFunda TüzünNo ratings yet
- Resuscitation of The NewbornDocument9 pagesResuscitation of The NewbornKarina Jiménez AyónNo ratings yet
- 2 Newborn Assessment 93667Document122 pages2 Newborn Assessment 93667Izziddin YassineNo ratings yet
- MKT 036Document4 pagesMKT 036عبدالرحمن ابراهيمNo ratings yet
- Questions: Foetal Circulation Anaesthesia Tutorial of The Week 91 18 MAY 2008Document8 pagesQuestions: Foetal Circulation Anaesthesia Tutorial of The Week 91 18 MAY 2008leizt_13No ratings yet
- Newborn Assessment: By: Ledelle M. de Chavez, Claudine M. Francisco & Don Jayric V. DepalobosDocument5 pagesNewborn Assessment: By: Ledelle M. de Chavez, Claudine M. Francisco & Don Jayric V. Depalobosdonskii04No ratings yet
- Update Fetal Circulation - MDM AmyDocument10 pagesUpdate Fetal Circulation - MDM AmyNana Yunus100% (1)
- 2 Paediatrics and Neonatal AnesthesiaDocument87 pages2 Paediatrics and Neonatal Anesthesiahailemichael chekolNo ratings yet
- Obs Gynae Presentation by Roll No 127Document23 pagesObs Gynae Presentation by Roll No 127Siddharth KatyalNo ratings yet
- NEONATAL AND PEDIATRICS PhysiologyDocument45 pagesNEONATAL AND PEDIATRICS PhysiologyAbdulkadir HasanNo ratings yet
- Ses 12 Principles of Newborn Adaption To The Extra-Uterine LifeDocument25 pagesSes 12 Principles of Newborn Adaption To The Extra-Uterine Lifelandegre KNo ratings yet
- Study - Blueprint P2Document26 pagesStudy - Blueprint P2Natasha Drummond100% (1)
- 1 Fetal CirculationDocument21 pages1 Fetal Circulationdr_mohanad100% (1)
- Anatomi Fisiologi SirkulasiDocument20 pagesAnatomi Fisiologi SirkulasiAulia RahmiNo ratings yet
- Chapter 23 ContinuationDocument7 pagesChapter 23 ContinuationArabelle GO100% (1)
- Tumbang KabehDocument57 pagesTumbang KabehArif WicaksanaNo ratings yet
- Adaption of Infants To Extra-Uterine LifeDocument10 pagesAdaption of Infants To Extra-Uterine LifeJulienne QuintaoNo ratings yet
- Paed Respiratory DistressDocument45 pagesPaed Respiratory Distressaboje ochekwuNo ratings yet
- Neonatal Circulation Changes / Unbalanced Circulation: Neonatal Cardiac Conditions: Medical and Surgical ManagementDocument4 pagesNeonatal Circulation Changes / Unbalanced Circulation: Neonatal Cardiac Conditions: Medical and Surgical ManagementAnita Maria UlfaNo ratings yet
- Pleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleural Effusion, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Covid-19 Contact Tracers Performance Monitoring of Weekly AccomplishmentsDocument1 pageCovid-19 Contact Tracers Performance Monitoring of Weekly AccomplishmentsDancyneall InternetNo ratings yet
- 2012 Global Down Syndrome Foundation Press ClippingsDocument28 pages2012 Global Down Syndrome Foundation Press ClippingsGlobalDownSyndromeNo ratings yet
- Board EamDocument55 pagesBoard Eamjoycevillamor100% (1)
- FluDocument19 pagesFluBenny Lee KennedyNo ratings yet
- 2003 ADA Preconception Care DiabetesDocument3 pages2003 ADA Preconception Care Diabetesannisafaujiah033No ratings yet
- ReimbursementFormA B2016Document7 pagesReimbursementFormA B2016DESIGN CGMPNo ratings yet
- Register Rawat Inap 2020Document327 pagesRegister Rawat Inap 2020carolinaNo ratings yet
- Implementing Improvement Strategies To Prevent Unplanned Extubation in Neonatal Intensive Care Units - SLIDE DECKDocument19 pagesImplementing Improvement Strategies To Prevent Unplanned Extubation in Neonatal Intensive Care Units - SLIDE DECKeman hamzaNo ratings yet
- CPS Info Dimenhydrinate (Gravol)Document5 pagesCPS Info Dimenhydrinate (Gravol)Ann A.No ratings yet
- Semmelweis and HandwashingDocument3 pagesSemmelweis and HandwashingVijay KumarNo ratings yet
- AIIMS June 2002 PG Entrance Question Paper With Answer KeyDocument23 pagesAIIMS June 2002 PG Entrance Question Paper With Answer KeywithraviNo ratings yet
- Hematology 2Document28 pagesHematology 2saad samyNo ratings yet
- Effects of Drugs AbuseDocument6 pagesEffects of Drugs AbuseRamel OñateNo ratings yet
- Pulse OximeterDocument16 pagesPulse OximeterChing Wai Yong100% (1)
- Arrows Consele PDFDocument221 pagesArrows Consele PDFIsai Lara OsoriaNo ratings yet
- Chapter 2 Drug AddictionDocument24 pagesChapter 2 Drug AddictionKaren Joy Francisco HabanaNo ratings yet
- Thrombolytic Therapy For Acute Myocardial Infarction 01-30-13Document1 pageThrombolytic Therapy For Acute Myocardial Infarction 01-30-13Ushnish ChatterjeeNo ratings yet
- Propofol Maintenance TIVA Infusions Kgs-Lbs 03-12-11 LockedDocument1 pagePropofol Maintenance TIVA Infusions Kgs-Lbs 03-12-11 LockedCasandra TudoracheNo ratings yet
- Centers For TherapyDocument2 pagesCenters For TherapyCeline JohnsonNo ratings yet
- Aplio Series Cardiovascular TransducersDocument2 pagesAplio Series Cardiovascular TransducersQaiserAnwarNo ratings yet
- Hypertonic Saline (3% and 5% Sodium Chloride Injection) Drug Information - Description, User Reviews, Drug Side Effects, Interactions - Prescribing Information at RxListDocument2 pagesHypertonic Saline (3% and 5% Sodium Chloride Injection) Drug Information - Description, User Reviews, Drug Side Effects, Interactions - Prescribing Information at RxListMuhammad AsadNo ratings yet
- 30073665: Colloids Versus Crystalloids For Fluid Resuscitation in Critically Ill People PDFDocument210 pages30073665: Colloids Versus Crystalloids For Fluid Resuscitation in Critically Ill People PDFAngel VelásquezNo ratings yet
- Trigeminal NeuralgiaDocument16 pagesTrigeminal NeuralgiaJerry AbleNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanTrisNo ratings yet
- Lasik GuidelinesDocument4 pagesLasik GuidelinesIlmiahdmobgyn MaretmeiNo ratings yet
- Nazi ExperimentsDocument3 pagesNazi ExperimentsAngel SarteNo ratings yet
- Pavlik Harness Initiation On Barlow Positive Hips - Can We Wait?Document15 pagesPavlik Harness Initiation On Barlow Positive Hips - Can We Wait?Irene AntoniNo ratings yet
- NCP (Afp)Document7 pagesNCP (Afp)Summer SuarezNo ratings yet