Professional Documents
Culture Documents
Braz J Oral Sci-2024v23e240338
Braz J Oral Sci-2024v23e240338
Uploaded by
Dadi SindhuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Braz J Oral Sci-2024v23e240338
Braz J Oral Sci-2024v23e240338
Uploaded by
Dadi SindhuCopyright:
Available Formats
Original Article
Volume 23
2024
e240338
Demineralized freeze-dried
bone allograft with/without
i-Platelet-rich fibrin in
3 wall intrabony defects
Rinnu Mathew1 , Anuradha Bhatsange2*
Demineralized freeze-dried bone allograft (DFDBA) contains
1
Former Post Graduate Student, bone morphogenetic proteins (BMPs), hence is osteoinductive.
Department of Periodontics, JMF’s Autologous platelet concentrates exhibit a higher quantity
ACPM Dental college, Sakri Road,
Dhule, Maharashtra, India. of growth factors. Both these biomaterials aid in bone
regeneration when placed in three-wall intrabony defects.
2
Professor, Department of
Periodontics, JMF’s ACPM However, their efficacy when used alone and in conjugation is
Dental college, Sakri Road, Dhule, not clear. Aim: To assess clinical and radiographic efficacy of
Maharashtra, India.
injectable platelet-rich fibrin (i-PRF) with microsurgical access
flap in the treatment of three-wall intrabony defects in chronic
periodontitis patients. Methods: Thirty sites with three-wall
intrabony defects were randomly assigned to control and test
group by computer generated method. The test group obtained
i-PRF mixed with DFDBA while the control group received only
DFDBA. Clinical parameters such as site-specific Plaque index
(PI), Radiographic intrabony defect depth (IBDD), modified-
Sulcular bleeding index (mSBI), Clinical attachment level (CAL),
Corresponding author: and Probing pocket depth (PPD) were measured at baseline,
Anuradha Bhatsange
Professor, Dept. of Periodontics,
three and six months. Results: Intragroup comparison within
JMF’s ACPM Dental college the control group and test group exhibited statistically highly
JMF’s ACPM dental college, significant variation of mean PI, mSBI, PPD, CAL, and IBDD
Sakri Road, Dhule, Maharashtra,
India, 424001. score from baseline to 3 months and from 3-6 months
Phone numbers: 9960881275; (p<0.001). However, intergroup comparison demonstrated no
E-mail: anujaps219@gmail.com
statistically significant variation of mean IBDD at all 3 intervals
Editor: Altair A. Del Bel Cury (p>0.05). Conclusion: i-PRF combined with DFDBA enhanced
the radiographic and clinical parameters as opposed to DFDBA
Received: July 15, 2022 alone. The role of i-PRF is promising in its capacity for easy
Accepted: June 02, 2023 obtainability and increased potential to aid in regeneration.
Keywords: Periodontitis. Allografts. Alveolar bone loss. Platelet-
Rich Fibrin. Regeneration.
http://dx.doi.org/10.20396/bjos.v23i00.8670338 Braz J Oral Sci. 2024;23:e240338 1
Mathew et al.
Introduction
Regeneration of periodontium is a process of restoring the complete architecture
and function of the periodontium1. It involves new functional periodontal attach-
ment between newly formed bone and cementum1,2. The process constitutes a
multi‑dependent sequence of biological events including cell adhesion, migration,
proliferation, and differentiation3.
Periodontitis is defined as an inflammatory disease of the supporting structural
apparatus resulting in progressive destruction of the “periodontal ligament”, alve-
olar bone with pocket formation, recession, or both. Bone loss that occurs as a
consequence of this inflammatory disease results in different patterns and in vari-
ous combinations. The vertical/ angular defects that occur in an oblique direction,
with a hollow trough in the bone alongside the root with base located apical to the
surrounding bone is termed as intrabony defect4. These defects when surrounded
by two or three walls become more amenable to regeneration as it provides the
best spatial relationship for defect bridging by providing vascular and cellular ele-
ments from the periodontal ligament and adjacent osseous wall5. Although various
attempts to accomplish goals of regeneration have been tried using bone grafts,
[autografts, allografts, xenografts, alloplasts] membranes, polypeptide growth fac-
tors, tissue engineering applications etc, reconstruction of fully functioning peri-
odontium still remains a big challenge despite the advances. “Demineralized freeze-
dried bone allograft” (DFDBA) a widely used allograft, exhibits osteoinductive and
osteoconductive properties owing to its content of bone morphogenetic proteins2.
These proteins orchestrate mesenchymal cell migration, new attachment, and
osteogenesis that help to regenerate cementum, bone, and periodontal ligament
with histological evidence6. However the amount of bone fill found with the use of
DFDBA has not been very clear. Hence, in the quest to enhance the efficacy of peri-
odontal regeneration with various bone grafts, polypeptide growth factors derived
from the autologous blood concentrates in the form of “platelet-rich plasma” (PRP)
and “platelet-rich fibrin” (PRF) have been used. These show the ability to induce cell
proliferation and differentiation and osteoinduction. The initial biochemical analysis
of PRF composition indicated it to be an intimate assembly of cytokines, glycanic
chains, and structural glycoproteins enmeshed within a slowly polymerized fibrin
network7. Later on the use of PRF membrane has been shown to exhibit a significant
but, slow sustained release of key “growth factors” for ≥ 1 week and ≤ 28 days, sug-
gesting its ability to stimulate its environment for wound healing8. However, another
form of PRF, i.e. an injectable form of PRF (i-PRF) demonstrated good results with
higher concentration of stem cells and better potential for regeneration due to its
capacity of inducing higher cell migration and mRNA expression of “Transforming
growth factor-beta” (TGF-β), “platelet derived growth factor” (PDGF), and collagen1.
The property of i-PRF forming a hydrogel even after 10 days hypothesized it to
release additional growth factors9.
Good and predictable outcomes of regenerative procedures are accomplished
by incorporation of microsurgery applications too. Microsurgery refers to refine-
ment in surgical technique with vision enhancement through magnification and
Braz J Oral Sci. 2024;23:e240338 2
Mathew et al.
was introduced to the speciality of Periodontics in 199210. Periodontal microsur-
gery helps to: 1) improve tissue preservation and better handling of specific flap
designs to access the defects; 2) optimize defect debridement and root instru-
mentation; 3) ensure optimal delivery of the regenerative technology; 4) optimize
flap mobility to achieve primary closure of the interdental space11. It’s application
promises to change clinical concepts of periodontal surgical care by improve-
ment in predictability, cosmetic result and patient comfort level over conventional
periodontal surgical procedures12. This implies placement of accurately mapped
incisions, elevation of flap with minimal damage, precise wound closure without
tension, resulting in reduction of postoperative morbidity. Rendering maximum
benefit to the patient with advancements in the treatment aspects, and the best
regenerative material available, the current study was carried out to explore the
clinical and radiographic effectiveness of i-PRF combined with DFDBA by micro-
surgical access flap in the treatment of three-wall intrabony defects in patients
with “chronic periodontitis”.
Material and methods
Trial design and ethics approval
This was a randomized controlled clinico-radiographic study carried out in Dept. of
Periodontology. A sample size of thirty sites were chosen to employ statistical soft-
ware, projected by evaluating the prior literature performed in the field of research and
maintaining the confidence interval at 95% with a relative precision of 20%. The study
was approved by institutional review board.
Participants
Sixty-one patients were recruited from out-patient department and assessed for eligi-
bility. Out of these 31 patients were excluded as they did not meet the inclusion crite-
ria. Chronic periodontitis patients between 30-50 years of age with 30 sites exhibiting
3 wall intrabony defects>3mm deep (the distance among defect base and alveolar
crest on an “Intraoral Periapical Radiograph” (IOPA) combined with an interproximal
residual Probing Pocket Depth (PPD) >5mm were included. Patients diagnosed with
aggressive periodontitis, systemic illnesses, insufficient platelet count, pregnant/
lactating mothers, postmenopausal women, and smokers, on a therapeutic regimen
were excluded.
Intervention
After obtaining consent from the participants following clinical parameters were
recorded “Plaque Index” (PI)13, and “Modified Sulcus Bleeding Index” (mSBI)14. The
PPD and “Clinical Attachment Level” (CAL) were recorded with “University of North
Carolina-15” (UNC-15) periodontal probe along with an acrylic stent from marginal
gingiva to the depth of the pocket and from “cemento-enamel junction” (CEJ) to
the depth of pocket respectively. Radiographic assessment of IBDD was carried out
using a computer running Windows XP with ‘Kodak RVG 5000 digital radiography
program. Standardized paralleling techniques were used for radiographs. IBDD was
Braz J Oral Sci. 2024;23:e240338 3
Mathew et al.
evaluated using Digimizer software. where the resolution of the image was set at
a value where each pixel was equal to 0.026mm. The defect depth was computed
from the alveolar crest to its base. The readings obtained in pixels were converted
to mm by multiplying the pixel with 0.026.
The DFDBA’s particle size used was 500μm and obtained from Tata memorial cen-
tre, Kharghar, Navi Mumbai. Four weeks following phase I therapy, the selected
operative site was anaesthetized with 2% lignocaine hydrochloride using adrena-
line (1:80000) and a microsurgical flap for access was planned with microsurgical
instruments (Figure 1). Using 3.5×optical magnification dental loupes, buccal & lin-
gual sulcular incisions were made using microsurgical ophthalmic blades. Reflec-
tion of the mucoperiosteal flap was carried out using the microsurgical periosteal
elevator at the test site and control site maintaining as much interproximal soft
tissue as possible. (Figure 2, 3a,b,c,d.) Meticulous defect debridement as well as
root planning were performed with specific curettes. The preparation for i-PRF was
carried out with specifications as described15. Upon termination of centrifugation,
the upper orange colour fluid was collected using a 5ml syringe with a 26G needle
(Figure 4a,b,c,d). After 5 minutes DFDBA particles were added to i-PRF in a 1:1 ratio
and within 15 minutes the material was ready to use with a total working time of
20 minutes. The mixture was delivered to the test site with the help of a bone graft
carrier followed by sutures and placement of periodontal dressing. (Figure 5a,b,c,d).
The control group received DFDBA granules mixed with saline in the same propor-
tion. The mucoperiosteal flaps were stabilized using 5-0 sutures. A periodontal
dressing was used to protect the surgical area (Figure 6).
Figure 1. Microsurgical instruments with magnifing loupes.
Braz J Oral Sci. 2024;23:e240338 4
Mathew et al.
A B
C D
Figure 2. Preoperative view showing. a) probing depth assessment b) intrabony defect on Digimiser c)
placement of the incision d) Flap reflection.
A B
C D
Figure 3. The clinical picture at the control site showing a) probing depth assessment at baseline b)
Digimiser showing intrabony defect c) Placement of sulcular incision with microblade d) Flap reflection.
Braz J Oral Sci. 2024;23:e240338 5
Mathew et al.
A B
Figure 4. Clinical picture showing i-PRF preparation. a) Centrifuge machine b) Vacutainer c) Obtention of
i-PRF d) Loading of i-PRF in syringe.
A B
D E
Figure 5. Clinical picture showing a) i-PRF delivery into DFDBA b) Mixing of i-PRF and DFDBA c) Grafting
at the test site d) Placement of sutures e) Periodontal dressing.
Braz J Oral Sci. 2024;23:e240338 6
Mathew et al.
A B
C D
Figure 6. The clinical picture at the control site showing a) DFDBA b) Grafting c) Placement of sutures d)
Periodontal dressing.
The sutures were removed after 10 days. A complete re-evaluation of all the clinical
and radiographical parameters at the 3rd and 6th months post-surgically was under-
taken (Figure 7a,b,c,d).
A B C D
Figure 7. Postoperative view showing clinical and Digimiser picture at 3 months (a,b) and at 6 months
(c,d) at test site showing probing depth assessment and intrabony defect resolution.
Braz J Oral Sci. 2024;23:e240338 7
Mathew et al.
Assessed for eligibility
(n = 61)
Excluded (n = 31)
ENTROLLMENT Did not meet
inclusion criteria
Randomised (n = 30)
ALLOCATION
Teste group Control group
(n = 15) (n = 15)
Follow up after Follow up after
FOLLOW UP 6 months 6 months
Withdrawals (n = 0) Withdrawals (n = 0)
ANALYSIS
Analysed (n = 15) Analysed (n = 15)
Figure 8. CONSORT statement for study description.
Randomization
Randomization was carried out using computer generated numbers and were allo-
cated to test and control group.
Statistical method
Data measurements were determined at baseline, three, and six months. The para-
metric tests were applied to analyse the data statistically. Statistics were accepted
as significant at values of p<0.05. Data was provided as descriptive statistics by
minimum, maximum range, mean and standard deviation. Intragroup comparison
of mean difference of normally distributed variables was analysed using the ANOVA
test. Pairwise comparison was done using the Bonferroni Post Hoc test. Intergroup
comparison of non-normally distributed variables was done with “Mann Whitney
U-test” & an unpaired t-test. The “Statistical Package for the Social Sciences” (SPSS)
version 19 was applied to conduct the statistical analysis.
Results
Sixty-one patients were assessed for eligibility out of which 31 were excluded as they did
not meet the inclusion criteria. Thirty sites evaluated in thirty patients out of which 15
sites each were randomly allocated to test and control group. Intragroup comparison
within the test and control group presented statistically highly substantial variation of
mean site-specific PI, modified SBI, PPD, CAL, and IBDD score during different durations
that is from baseline to 3 months & from 3 to 6 months (p<0.001) [Table 1 and 3]. Similar
results were obtained with pairwise comparisons within the two groups at (p<0.001)
[Table 2, 4]. The inter-group comparison revealed no statistically substantial variation
of mean site-specific PI at baseline, 3, and 6 months (p>0.05). The scores of mSBI at 3
Braz J Oral Sci. 2024;23:e240338 8
Mathew et al.
months showed statistically significant variation (p<0.05), but not at 6 months (p>0.05).
The assessment of PPD and CAL revealed statistically no significant (p>0.05) variation
at baseline and six months but in 3rd month, the test group presented a greater reduc-
tion in PPD and higher gain in attachment than the control group which was statistically
significant (p<0.05). Regarding IBDD, there was statistically no significant variation of
mean intra bony depth defect at all 3 intervals between the test & control group (p>0.05)
[Table 5]. A change and a comparison of the change in PI, mSBI, PPD, CAL, and IBD from
baseline to six months in between the 2 groups was compared with the “Mann-Whitney
U test” which revealed that there was statistically no significant (p>0.05) variation of
mean changes at six months as depicted. [Table 6 and 7]
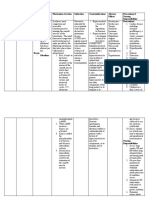
Table 1. Intragroup comparison of PI, mSBI, CAL, PPD, IBDD score at baseline, 3- and 6-months interval
in Test group.
SUM OF MEAN
PARAMETERS BASELINE 3 MONTHS 6 MONTHS F P VALUE
SQUARES SQUARE
PI 2.80±0.41 1.73±.458 0.87±.352 28.133 14.067 75.74 <0.001
mSBI 2.73±.458 1.13±.352 0.67±.488 32.044 16.022 60.807 <0.001
PPD 8.00±2.138 4.40±1.056 1.87±1.407 284.978 142.489 55.757 <0.001
CAL 6.27±1.831 2.80±1.320 0.47±.516 255.511 127.756 71.480 <0.001
IBDD 5.07±0.80 3.20±.86 1.67±.61 86.978 43.489 117.5889 <0.001
IBDD-Intrabony defect depth, “CAL-Clinical attachment level, PPD-Probing Pocket Depth”, mSBI-modified Sulcus
Bleeding Index, F-ANOVA Test, PI-Plaque Index, P-Probability value. (p<0.05)
Table 2. Pairwise difference of PI, mSBI, CAL, PPD, and IBDD at baseline, 3 to 6 months interval in the
Test group.
MEAN DIFFERENCE
PARAMETERS
BASELINE-3 MONTH BASELINE-6 MONTH 3-6 MONTHS
PI 1.07 1.93 .867
mSBI 1.600* 2.067* .467*
PPD 3.600* 6.133* 2.533*
CAL 3.467* 5.800* 2.333*
IBDD 1.87 3.40 1.53
PPD-Probing Pocket Depth, mSBI- “modified Sulcus Bleeding Index, CAL-Clinical attachment level,” PI-Plaque
Index, IBDD-Intrabony defect depth. (p<0.05)
Table 3. Intragroup comparison of PI, mSBI, CAL, PPD, IBDD score at baseline, 3 months 6 months in the
test group.
SUM OF MEAN
PARAMETERS BASELINE 3 MONTHS 6 MONTHS F P VALUE
SQUARES SQUARE
PI 2.60±0.51 1.60±.507 .60±.507 30.000 15.000 58.333 <0.001
mSBI 2.47±.516 1.47±.516 .40±.507 32.044 16.022 60.807 <0.001
PPD 7.00±1.648 3.67±.724 1.27±1.100 248.711 124.356 83.880 <0.001
CAL 5.07±1.438 1.80±.676 .27±.458 180.311 90.156 98.951 <0.001
IBDD 4.53±.640 2.93±.704 1.27±.704 80.044 40.022 85.762 <0.001
PPD-Probing Pocket Depth, mSBI- “modified Sulcus Bleeding Index, CAL-Clinical attachment level”, PI-Plaque
Index, IBDD-Intrabony defect depth. (p<0.05).
Braz J Oral Sci. 2024;23:e240338 9
Mathew et al.
Table 4. Pairwise difference of PI, mSBI, CAL, PPD, and IBDD in between baseline, 3 & 6months intervals
in the control group.
MEAN DIFFERENCE
PARAMETERS
“BASELINE-3 MONTH BASELINE-6 MONTH 3 MONTH-6 MONTHS”
PI 1.000* 2.000* 1.000*
mSBI 1.000* 2.067* 1.067*
PPD 3.333* 5.733* 2.400*
CAL 3.267* 4.800* 1.533*
IBDD 1.600* 3.267* 1.667*
PPD-Probing Pocket Depth, m SBI-modified Sulcus Bleeding Index, CAL-Clinical attachment level, PI-Plaque
Index, IBDD-Intrabony defect depth. (p<0.05).
Table 5. Intergroup comparison of PI, mSBI, CAL, PPD, and IBDD at baseline, 3 & 6 months.
BASELINE 3 MONTHS 6 MONTHS
PARAMETERS TEST CONTROL TEST CONTROL TEST CONTROL
GROUP GROUP GROUP GROUP GROUP GROUP”
PI 2.80±0.41 2.60±0.51 1.73±.458 1.60±.507 .87±.352 .60±.507
mSBI 2.73±.458 2.47±.516 1.13±.352 1.47±.516 .67±.488 .40±.507
PPD 8.00±2.138 7.00±1.648 4.40±1.056 3.67±.724 1.87±1.407 1.27±1.100
CAL 6.27±1.831 5.07±1.438 2.80±1.320 1.80±.676 .47±.516 .27±.458
IBDD 5.07±0.80 4.53±.640 3.20±.862 2.93±.704 1.67±.617 1.27±.704
PPD-Probing Pocket Depth, m SBI-modified Sulcus Bleeding Index, CAL-Clinical attachment level, PI-Plaque
Index, IBDD-Intrabony defect depth. (p<0.05).
Table 6. Change in Pi, SBI, PPD, and IBD from baseline to 6 months between the 2 groups.
By 6 months
Group Minimum Maximum Mean Std. Deviation
Change in
Test 1 3 1.93 .060
PI
Control 1 3 2.00 .37
Test 1 3 2.07 .46
SBI
Control 1 3 2.07 .45
Test 2 10 6.13 2.4
PPD
Control 3 9 5.73 1.8
Test 3 9 5.80 1.82
CAL
Control 2 8 4.80 1.56
Test 2 6 3.40 0.91
IBD
Control 3 4 3.27 .45
m SBI-modified Sulcus Bleeding Index, PPD-Probing Pocket Depth, CAL-Clinical attachment level, PI-Plaque
Index, IBDD-Intrabony defect depth. (p<0.05).
Braz J Oral Sci. 2024;23:e240338 10
Mathew et al.
Table 7. Comparison of change in PI, mSBI, PPD, and IBD from baseline to six months between the 2 groups.
Six months PI Six months Six months of Six months CAL Six months
change mSBI change PPD change change IBDD change
Mann-Whitney
105.500 112.500 104.000 82.500 104.50
U
Z-score -.448 .000 -.360 -1.271 -0.379
P value .654 1.000 .719 .204 .704
PPD-Probing Pocket Depth, m SBI-modified Sulcus Bleeding Index, CAL-Clinical attachment level, PI-Plaque
Index, IBDD-Intrabony defect depth. Z-score. (p<0.05).
Discussion
The primary purpose of periodontal therapy is resolution of inflammation, elimination
of infection, disease progression cessation, and prevention of recurrence16. DFDBA
was chosen in this study due to its inductive properties of stimulating host stem cells
to differentiate into osteoblasts. Its regenerative properties have stimulated physi-
cians to broadly utilize it in infrabony defects17. In addition DFDBA has been shown to
withstand displacement due to its physical property2.
Platelet concentrates possess growth factors that act as vital modulators induc-
ing the differentiation, proliferation, attachment, and migration of periodontal pro-
genitor cells5. Advantages of using platelet concentrates is its simpler preparation,
inexpensive nature and antibacterial effect due to presence of leukocytes18. With
the speculation, that the addition of autologous plasma derivatives like PRP, PRF,
and i-PRF might show synergistic and predictable outcomes, this study combined
these two biomaterials that is i-PRF and DFDBA. i-PRF can be employed to mix graft
cohesively and sprayed over surgical sites due to its injectable form19. i-PRF remark-
ably influences osteoblast behaviour by impacting the migration, proliferation, and
differentiation of human osteoblasts according to a study and has been shown to
complement graft materials in aiding regeneration20,21. Taking into consideration the
above aspects, the efficiency of i-PRF with DFDBA and DFDBA alone was tested clin-
ically and radiographically. Assessment period of 6 months for evaluation of radio-
graphs was chosen as evidence of rising bone density is frequently not observed
until then1.
The clinical parameters studied were PI, mSBI, PPD, CAL and IBDD. PI showed statis-
tically high significant difference between the three intervals in both groups depict-
ing good plaque control which could be due to reinforcement of oral hygiene instruc-
tions. However intergroup comparison revealed no statistically substantial difference.
This was in line with research conducted by Sharma and Pradeep22, Elgendy and Abp
Shady20 and Agarwal et al.5.
Modified SBI was recorded to assess the presence or absence of gingival inflamma-
tion. Both the groups showed a remarkable reduction in inflammation at various inter-
vals. The outstanding potential of i-PRF being an anti-inflammatory has been high-
lighted due to its property of reducing proinflammatory M1 macrophage phenotype
and activation of dendritic cells23.
Braz J Oral Sci. 2024;23:e240338 11
Mathew et al.
PPD was used to evaluate the effectiveness of the therapy and a gain in the CAL
remains the gold standard for evaluating the success of periodontal treatment. A
reduction in PPD from baseline to six months was noted in the test and control group
which was statistically highly significant. At 3 months, the test group fared better
than the “control group” [p<0.05], but intergroup comparison however failed to reach
a statistically significant difference at 6 months suggesting that i-PRF combined with
DFDBA as well as DFDBA alone when used was effective in reducing the probing
pocket depth.
Progressive improvement in the mean CAL from baseline to three months and from
3-6 months was observed which was highly significant in both groups. However inter-
group comparison revealed no statistical significance. These outcomes were consis-
tent with the research performed by Khosropanah et al.24 and Agarwal et al.5. Gain in
CAL is attributed to raised resistance to probing caused by a drop in inflammation,
gingival fibers reformation, and a long junctional epithelium25.
In the current work, the mean IBDD in both groups from baseline to six months was
statistically highly significant (p-value <0.05). Both the groups demonstrated a drop in
defect depth with formation of new bone on the radiograph. Radiographically better
bone fill was observed in the test group. This might be attributed to the addition of
i-PRF with DFDBA. However, the test group failed to reach a statistically significant
value. The outcomes are in line with the research performed by Agrawal et al.5 and
Khosropanah et al24.
Refinements in surgical procedures have entailed use of the minimally invasive surgi-
cal method which create minimum flap reflection, minimal wounds, and gentle han-
dling of the hard & soft tissues26. The benefits include better visual acuity, ease of
soft tissue handling, and precise wound closure, enabling healing with primary inten-
tion27. In the present study, microsurgical flap access was employed that allowed a
more accurate, less traumatic access to periodontal defect however no parameters
were included to evaluate the impact of the microsurgical approach on the healing of
the flap. Histologic analysis or surgical re-entry was not opted due to ethical reasons
which were limitations of the study.
Conclusion
In the current research, it may be inferred that DFDBA alone or in combination with
i-PRF can be used to treat 3-walled intrabony defects. Thus, the future scope of
the study includes exploring i-PRF’s potential to be used for its anti-inflammatory
property in conjunction with other bone graft materials for which more longitudinal
studies are required.
Funding
None.
Conflicts of interest
None.
Braz J Oral Sci. 2024;23:e240338 12
Mathew et al.
Authors’ Contribution
All authors actively participated in the discussion of the manuscript’s findings and
have revised and approved the final version of the manuscript.
Data availability
Datasets related to this article will be available upon request to the corresponding
author.
References:
1. Brunsvold MA, Mellonig JT. Bone grafts and periodontal regeneration. Periodontol 2000.
1993 Feb;1:80-91.
2. Zhou S, Sun C, Huang S, Wu X, Zhao Y, Pan C, et al. Efficacy of adjunctive bioactive materials in the
treatment of periodontal intrabony defects: a systematic review and meta-analysis. Biomed Res Int.
2018 May;2018:8670832. doi: 10.1155/2018/8670832.
3. Panda S, Ramamoorthi S, Jayakumar ND, Sankari M, Varghese SS. Platelet rich fibrin and
alloplast in the treatment of intrabony defect. J Pharm Bioallied Sci. 2014 Apr;6(2):127-31.
doi: 10.4103/0975-7406.129178.
4. Prichard JF. The etiology, diagnosis and treatment of the intrabony defect. J Periodontol.
1967 Nov-Dec;38(6):455-65. doi: 10.1902/jop.1967.38.6_part1.455.
5. Agarwal P, Chatterjee A, Gokhale S, Singh HP, Kandwal A. Evaluation of platelet-rich plasma alone
or in combination with demineralized freeze dried bone allograft in treatment of periodontal
infrabony defects: A comparative clinical trial. J Indian Soc Periodontol. 2016 Jan-Feb;20(1):42-7.
doi: 10.4103/0972-124X.170811.
6. Jethwa J, Ireland RS, Chan D. Does a combination of platelet-rich plasma and decalcified freeze-dried
bone allograft offer advantages over decalcified freeze-dried bone allograft alone when using pocket
depth and clinical attachment level as markers for periodontal healing? A literature review. J Investig
Clin Dent. 2019 May;10(2):e12397. doi: 10.1111/jicd.12397.
7. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF):
a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod. 2006 Mar;101(3):e45-50. doi: 10.1016/j.tripleo.2005.07.009.
8. Pradeep AR, Bajaj P, Rao NS, Agarwal E, Naik SB. Platelet-rich fibrin combined with a
porous hydroxyapatite graft for the treatment of 3-wall intrabony defects in chronic
periodontitis: a randomized controlled clinical trial. J Periodontol. 2017 Dec;88(12):1288-96.
doi: 10.1902/jop.2012.110722.
9. Miron RJ, Fujioka-Kobayashi M, Hernandez M, Kandalam U, Zhang Y, Ghanaati S, et al.
Injectable platelet rich fibrin (i-PRF): opportunities in regenerative dentistry? Clin Oral Investig.
2017 Nov;21(8):2619-27. doi: 10.1007/s00784-017-2063-9.
10. Shanelec DA. Periodontal microsurgery. J Esthet Restor Dent. 2003;15(7):402-7; discussion 408.
doi: 10.1111/j.1708-8240.2003.tb00965.x.
11. Cortellini P, Tonetti MS. Microsurgical approach to periodontal regeneration. Initial evaluation in a
case cohort. J Periodontol. 2001 Apr;72(4):559-69. doi: 10.1902/jop.2001.72.4.559.
12. Jain R, Kudva P, Kumar R, Nagar S. Periodontal microsurgery-magnifying facts, maximizing results.
J Adv Med Dent Sci Res. 2014;2(3):24-34.
Braz J Oral Sci. 2024;23:e240338 13
Mathew et al.
13. Silness J, Loe H. Periodontol disease in pregnancy. Il. Correlation between oral hygiene and
periodontal condition. Acta Odontol Scand. 1964 Feb;22:121-35. doi: 10.3109/00016356408993968.
14. Mombelli A, van Oosten MA, Schurch E Jr, Land NP. The microbiota associated with successful
or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987 Dec;2(4):145-51.
doi: 10.1111/j.1399-302x.1987.tb00298.x.
15. Mourão CF, Valiense H, Melo ER, Mourão NB, Maia MD. Obtention of injectable platelets
rich-fibrin (i-PRF) and its polymerization with bone graft: technical note. Rev Col Bras Cir.
2015 Nov-Dec;42(6):421-3. doi: 10.1590/0100-69912015006013.
16. Sculean A, Nikolidakis D, Nikou G, Ivanovic A, Chapple IL, Stavropoulos A. Biomaterials for
promoting periodontal regeneration in human intrabony defects: a systematic review. Periodontol
2000. 2015 Jun;68(1):182-216. doi: 10.1111/prd.12086.
17. Bowers G, Felton F, Middleton C, Glynn D, Sharp S, Mellonig J, et al. Histologic comparison of
regeneration in human intrabony defects when osteogenin is combined with demineralized freeze-
dried bone allograft and with purified bovine collagen. J Periodontol. 1991 Nov;62(11):690-702.
doi: 10.1902/jop.1991.62.11.690.
18. Najeeb S, Khurshid Z, Agwan MAS, Ansari SA, Zafar MS, Matinlinna JP. Regenerative Potential of
Platelet Rich Fibrin (PRF) for curing intrabony periodontal defects: a systematic review of clinical
studies. Tissue Eng Regen Med. 2017 Sep;14(6):735-42. doi: 10.1007/s13770-017-0079-5.
19. Shah R, Gowda TM, Thomas R, Kumar T, Mehta DS. Biological activation of bone
grafts using injectable platelet-rich fibrin. J Prosthet Dent. 2019 Mar;121(3):391-3.
doi: 10.1016/j.prosdent.2018.03.027.
20. Elgendy EA, Abo Shady TE. Clinical and radiographic evaluation of nanocrystalline hydroxyapatite
with or without platelet-rich fibrin membrane in the treatment of periodontal intrabony defects.
J Indian Soc Periodontol. 2015 Jan-Feb;19(1):61-5. doi: 10.4103/0972-124X.148639.
21. Wang X, Zhang Y, Choukroun J, Ghanaati S, Miron RJ. Effects of an injectable platelet-rich fibrin
on osteoblast behavior and bone tissue formation in comparison to platelet-rich plasma. Platelets.
2018 Jan;29(1):48-55. doi: 10.1080/09537104.2017.1293807.
22. Sharma A, Pradeep AR. Treatment of 3-wall intrabony defects in patients with chronic periodontitis
with autologous platelet-rich fibrin: a randomized controlled clinical trial. J Periodontol.
2011 Dec;82(12):1705-12. doi: 10.1902/jop.2011.110075.
23. Zhang J, Yin C, Zhao Q, Zhao Z, Wang J, Miron RJ, et al. Anti-inflammation effects of injectable
platelet-rich fibrin via macrophages and dendritic cells. J Biomed Mater Res A. 2020 Jan;108(1):61-8.
doi: 10.1002/jbm.a.36792.
24. Khosropanah H, Shahidi S, Basri A, Houshyar M. Treatment of intrabony defects by DFDBA alone or
in combination with PRP: a split-mouth randomized clinical and three-dimensional radiographic trial.
J Dent (Tehran). 2015 Oct;12(10):764-73.
25. Caton JG, Greenstein G. Factors related to periodontal regeneration. Periodontol 2000.
1993 Feb;1(1):9-15.
26. Kao RT, Nares S, Reynolds MA. Periodontal regeneration - intrabony defects: a systematic
review from the AAP Regeneration Workshop. J Periodontol. 2015 Feb;86(2 Suppl):S77-104.
doi: 10.1902/jop.2015.130685.
27. Wachtel H, Schenk G, Böhm S, Weng D, Zuhr O, Hürzeler MB. Microsurgical access flap and enamel
matrix derivative for the treatment of periodontal intrabony defects: a controlled clinical study. J Clin
Periodontol. 2003 Jun;30(6):496-504. doi: 10.1034/j.1600-051x.2003.00013.x.
Braz J Oral Sci. 2024;23:e240338 14
You might also like
- Homeopathic Care For Cats and Dogs Don Hamilton.03381 1contentsDocument8 pagesHomeopathic Care For Cats and Dogs Don Hamilton.03381 1contentsSantosh Kumar0% (3)
- Cairo: Pilbeam's Mechanical Ventilation, 6th EditionDocument6 pagesCairo: Pilbeam's Mechanical Ventilation, 6th Editionفاتن المطيريNo ratings yet
- 17A. Immune ToleranceDocument8 pages17A. Immune ToleranceEssington BeloNo ratings yet
- B-Medium Opening ActivatorDocument31 pagesB-Medium Opening ActivatorAbiha Ali100% (1)
- Journal Homepage: - : IntroductionDocument9 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Assessment of Alveolar Bone Augmentation in Intrabony Defects Employing Platelet-Rich Fibrin (PRF) Membrane and Sticky Bone (Injectable-PRF & Demineralized Freeze-Dried Bone Graft) - A Case ReportDocument4 pagesAssessment of Alveolar Bone Augmentation in Intrabony Defects Employing Platelet-Rich Fibrin (PRF) Membrane and Sticky Bone (Injectable-PRF & Demineralized Freeze-Dried Bone Graft) - A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 2022 - Management of Periodontal Intrabony Defect Using Sticky Bone and GTR Membrane: A Case ReportDocument4 pages2022 - Management of Periodontal Intrabony Defect Using Sticky Bone and GTR Membrane: A Case ReportJontavius GilbertNo ratings yet
- JCDR 11 ZC73Document5 pagesJCDR 11 ZC73dimiz77No ratings yet
- Surgical Management of A Large Periapical Lesion With PRF and Xenograft - A Case ReportDocument3 pagesSurgical Management of A Large Periapical Lesion With PRF and Xenograft - A Case ReportJohn SmithNo ratings yet
- In Vitro Biocompatibility of Biohybrid Polymers Membrane Evaluated in Human Gingival FibroblastsDocument9 pagesIn Vitro Biocompatibility of Biohybrid Polymers Membrane Evaluated in Human Gingival Fibroblasts赵忠琪No ratings yet
- Implantoplasty Enhancing Peri-Implant Bone Stability Over A 3-Year Follow-Up: A Case SeriesDocument8 pagesImplantoplasty Enhancing Peri-Implant Bone Stability Over A 3-Year Follow-Up: A Case SeriesBagis Emre GulNo ratings yet
- Rde 39 51Document5 pagesRde 39 51Sashwat SathishNo ratings yet
- Caso Clínico de Sausage TechniqueDocument12 pagesCaso Clínico de Sausage Techniquealessandra camposNo ratings yet
- Surgical Management of Periapical Lesion Inmaxillary Incisorswith Combined Bone Graft and Platelet - Rich Fibrin: A Case ReportDocument5 pagesSurgical Management of Periapical Lesion Inmaxillary Incisorswith Combined Bone Graft and Platelet - Rich Fibrin: A Case ReportTMDCH JournalNo ratings yet
- 06.Long-Term Follow-Up On Soft and Hard TissueDocument8 pages06.Long-Term Follow-Up On Soft and Hard Tissue친절No ratings yet
- 2022 - Platelet-Rich Fibrin - A Wonder Material For Periodontal Regeneration - A Clinical Case SeriesDocument4 pages2022 - Platelet-Rich Fibrin - A Wonder Material For Periodontal Regeneration - A Clinical Case SeriesJontavius GilbertNo ratings yet
- 3929269 (2) (3)Document8 pages3929269 (2) (3)RosaNo ratings yet
- Clin Oral Invest BTCP Type 1 Col ConesDocument10 pagesClin Oral Invest BTCP Type 1 Col ConesPathivada LumbiniNo ratings yet
- Journal of Periodontology - 2022 - Monje - Significance of Barrier Membrane On The Reconstructive Therapy ofDocument13 pagesJournal of Periodontology - 2022 - Monje - Significance of Barrier Membrane On The Reconstructive Therapy of安西 泰規No ratings yet
- Parative Outcomes of Platelet Concentrates and Blood ClotDocument11 pagesParative Outcomes of Platelet Concentrates and Blood ClotmarisabelNo ratings yet
- Pradeep 2012Document14 pagesPradeep 2012Anonymous Y9FLG5kQdNo ratings yet
- 27 de Oct - Histologic Evaluation of Human Intrabony Periodontal Defects Treated With Deproteinized Bovine Bone Mineral in Combination With OrthodonticDocument10 pages27 de Oct - Histologic Evaluation of Human Intrabony Periodontal Defects Treated With Deproteinized Bovine Bone Mineral in Combination With OrthodonticLaura Andrea Agudelo WilchesNo ratings yet
- 10 1111@cid 12748Document8 pages10 1111@cid 12748Behnam TaghaviNo ratings yet
- Guided Bone Regeneration Simultaneous With Implant Placement Using Bovine-DerivedDocument13 pagesGuided Bone Regeneration Simultaneous With Implant Placement Using Bovine-DerivedCamilo Andrés Sabogal ArguelloNo ratings yet
- Bone Replacement Grafts With Guided Tissue RegenerationDocument16 pagesBone Replacement Grafts With Guided Tissue RegenerationIrvin EduardoNo ratings yet
- Art4 PDFDocument9 pagesArt4 PDFDiana RuizNo ratings yet
- RetrieveDocument10 pagesRetrieveDANTE DELEGUERYNo ratings yet
- Cone Beam Computed Tomography As A Tool For The Analysis of Bone Fill in Intrabony Defects With Use of Nanogentm Bone GraftDocument10 pagesCone Beam Computed Tomography As A Tool For The Analysis of Bone Fill in Intrabony Defects With Use of Nanogentm Bone GraftIJAR JOURNALNo ratings yet
- Jced 13 E935Document6 pagesJced 13 E935Marwa Wagih ElboraeyNo ratings yet
- Kadkhodazadeh 2024Document7 pagesKadkhodazadeh 2024hugorhadelNo ratings yet
- Use of Fisiograft in Intrabony Defects-A Clinical and Radiological StudyDocument4 pagesUse of Fisiograft in Intrabony Defects-A Clinical and Radiological StudymaxNo ratings yet
- 1 - Aishwarya Das Sep 21Document4 pages1 - Aishwarya Das Sep 21Zeyneb KadirNo ratings yet
- Efeito Das Membranas de Colágeno Reticuladas Versus Não Reticuladas No Osso: Uma Revisão SistemáticaDocument10 pagesEfeito Das Membranas de Colágeno Reticuladas Versus Não Reticuladas No Osso: Uma Revisão SistemáticaJuliana Gomes BarretoNo ratings yet
- Jurnal Periapikal 2Document6 pagesJurnal Periapikal 2Rahmania AlikhlasNo ratings yet
- Dental Research JournalDocument9 pagesDental Research JournalLucianoNo ratings yet
- Arunjaroensuk 2017Document11 pagesArunjaroensuk 2017everaldocruzNo ratings yet
- Keywords: Collagenated Heterologous Bone Graft, Demineralized Bone Matrix, Maxillary Sinus AugmentationDocument8 pagesKeywords: Collagenated Heterologous Bone Graft, Demineralized Bone Matrix, Maxillary Sinus AugmentationJesse Coelho SchardosimNo ratings yet
- In Vitro Investigation of Gelatin/Polycaprolactone Nano Bers in Modulating Human Gingival Mesenchymal Stromal CellsDocument15 pagesIn Vitro Investigation of Gelatin/Polycaprolactone Nano Bers in Modulating Human Gingival Mesenchymal Stromal CellsZhongqi ZhaoNo ratings yet
- Bender 2005Document10 pagesBender 2005Posgrado Periodoncia2017No ratings yet
- Pi Is 1010518211000424Document6 pagesPi Is 1010518211000424Muthia FadhilaNo ratings yet
- JFB 14 00174Document14 pagesJFB 14 00174mNo ratings yet
- Retrieve 4Document8 pagesRetrieve 4dreneanastriNo ratings yet
- Natto. Efficacy of Collagen Matrix Seal and Collagen Sponge On Ridge Preservation in Combination With Bone AllograftDocument32 pagesNatto. Efficacy of Collagen Matrix Seal and Collagen Sponge On Ridge Preservation in Combination With Bone Allograftandrea.lopez.pNo ratings yet
- Reference For Longit. Section 2021Document11 pagesReference For Longit. Section 2021Marwa Wagih ElboraeyNo ratings yet
- Regenerative Potential of Cultured Gingival Fibroblasts - RCTDocument12 pagesRegenerative Potential of Cultured Gingival Fibroblasts - RCTDr.Niveditha SNo ratings yet
- Management of Two-Wall Infra - Bony DefecDocument6 pagesManagement of Two-Wall Infra - Bony DefecbubuvulpeaNo ratings yet
- Ab 2019Document7 pagesAb 2019Dome CárdenasNo ratings yet
- Jcpe 13086Document10 pagesJcpe 13086jcNo ratings yet
- Titanium Mesh Associated With Rhbmp-2 in Alveolar Ridge ReconstructionDocument8 pagesTitanium Mesh Associated With Rhbmp-2 in Alveolar Ridge ReconstructionSaptiadi OktoraNo ratings yet
- Titanium Mesh Ridges RecontructionDocument11 pagesTitanium Mesh Ridges RecontructionМилутинМићићNo ratings yet
- Management of Apico Marginal Defects With EndodontDocument9 pagesManagement of Apico Marginal Defects With EndodontROSIEL MARIA ELVIR HERRERANo ratings yet
- (2003 Kan) Dimensions of Peri-Implant Mucosa An Evaluation of Maxillary Anterior Single Implants in HumansDocument7 pages(2003 Kan) Dimensions of Peri-Implant Mucosa An Evaluation of Maxillary Anterior Single Implants in Humansyena1010100% (1)
- Healing of Intrabony Defects Following Regenerative SurgeryDocument13 pagesHealing of Intrabony Defects Following Regenerative SurgeryYou're Just As Sane As DivaNo ratings yet
- Intraoral Versus Extraoral Cementation of Implant Supported Single Crowns Clinical, Biomarker, and Microbiological ComparisonsDocument10 pagesIntraoral Versus Extraoral Cementation of Implant Supported Single Crowns Clinical, Biomarker, and Microbiological ComparisonsBagis Emre GulNo ratings yet
- Lasers: Effect of Low-Level Laser Therapy and Platelet-Rich Fibrin On The Treatment of Intra-Bony DefectsDocument8 pagesLasers: Effect of Low-Level Laser Therapy and Platelet-Rich Fibrin On The Treatment of Intra-Bony DefectsMegha PoojaryNo ratings yet
- Autogenous - Mineralized - Dentin - Versus - Xenograft - Granules - in - Ridge - Preservation - For Delayed - Implantation - in - Post-Extraction - SitesDocument11 pagesAutogenous - Mineralized - Dentin - Versus - Xenograft - Granules - in - Ridge - Preservation - For Delayed - Implantation - in - Post-Extraction - SitesSamantha TavaresNo ratings yet
- DR Bhaumik Nanavati Proof ApprovedDocument6 pagesDR Bhaumik Nanavati Proof ApprovedFahmi FirmansyahNo ratings yet
- Clinical and Radiographic Assessment of Bond Apatite in Horizontal Bone Augmentation Around Dental Implants: A Randomized Controlled TrialDocument10 pagesClinical and Radiographic Assessment of Bond Apatite in Horizontal Bone Augmentation Around Dental Implants: A Randomized Controlled TrialIJAR JOURNALNo ratings yet
- The Applications of Regenerative Medicine in Sinus Lift Procedures A Systematic ReviewDocument14 pagesThe Applications of Regenerative Medicine in Sinus Lift Procedures A Systematic ReviewBagis Emre GulNo ratings yet
- Ams 5 198Document5 pagesAms 5 198dayanaNo ratings yet
- Injectable Platelet Rich Fibrin With DemineralizedDocument22 pagesInjectable Platelet Rich Fibrin With DemineralizedDadi SindhuNo ratings yet
- 33 RD JC - SoniaDocument9 pages33 RD JC - SoniaDadi SindhuNo ratings yet
- A Multilevel Analysis of Platform-Switching Flapless Implants Placed at Tissue Level: 4-Year Prospective Cohort StudyDocument13 pagesA Multilevel Analysis of Platform-Switching Flapless Implants Placed at Tissue Level: 4-Year Prospective Cohort Studyhkwgt7vskwNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Maresin 1 Promotes Wound Healing and Socket Bone Regeneration For Alveolar Ridge PreservationDocument8 pagesMaresin 1 Promotes Wound Healing and Socket Bone Regeneration For Alveolar Ridge PreservationDadi SindhuNo ratings yet
- Journal of Periodontology - 2023 - Saleh - Influence of Residual Pockets On Periodontal Tooth Loss A RetrospectiveDocument12 pagesJournal of Periodontology - 2023 - Saleh - Influence of Residual Pockets On Periodontal Tooth Loss A RetrospectiveDadi SindhuNo ratings yet
- 32 ND JC - SindhuDocument42 pages32 ND JC - SindhuDadi SindhuNo ratings yet
- 36 TH JC - SindhuDocument13 pages36 TH JC - SindhuDadi SindhuNo ratings yet
- 7 TH JC PDF - SindhuDocument5 pages7 TH JC PDF - SindhuDadi SindhuNo ratings yet
- 11th JC - SINDHU 2Document25 pages11th JC - SINDHU 2Dadi SindhuNo ratings yet
- 10 TH JC PDF - SINDHUDocument6 pages10 TH JC PDF - SINDHUDadi SindhuNo ratings yet
- 5 TH JC PDF - SindhuDocument5 pages5 TH JC PDF - SindhuDadi SindhuNo ratings yet
- 1 ST JC PDF - SindhuDocument32 pages1 ST JC PDF - SindhuDadi SindhuNo ratings yet
- Mediators: The Scientific World JournalDocument24 pagesMediators: The Scientific World JournalDadi SindhuNo ratings yet
- Turmeric: Nutrition ScienceDocument12 pagesTurmeric: Nutrition ScienceDadi SindhuNo ratings yet
- Amritsar PosterDocument1 pageAmritsar PosterDadi SindhuNo ratings yet
- Processing Technologies and Health Benefits of Quinoa: June 2019Document7 pagesProcessing Technologies and Health Benefits of Quinoa: June 2019Dadi SindhuNo ratings yet
- 5 TH JC - SindhuDocument34 pages5 TH JC - SindhuDadi SindhuNo ratings yet
- Are Periodontal Tissues and Periodontal Health Impacted by Food Supplements (Protein and Aminoacids, Natural Herbal Products, Minerals) ? - ReviewDocument13 pagesAre Periodontal Tissues and Periodontal Health Impacted by Food Supplements (Protein and Aminoacids, Natural Herbal Products, Minerals) ? - ReviewDadi SindhuNo ratings yet
- Università Degli Studi Di Trieste: Biomarkers To Define Optimal Protein RequirementDocument119 pagesUniversità Degli Studi Di Trieste: Biomarkers To Define Optimal Protein RequirementDadi SindhuNo ratings yet
- 15 THDocument8 pages15 THDadi SindhuNo ratings yet
- 12 TH JC PDF - SindhuDocument9 pages12 TH JC PDF - SindhuDadi SindhuNo ratings yet
- Clin Transl Allergy (2019)Document7 pagesClin Transl Allergy (2019)Nimesh ModiNo ratings yet
- Melphalan (AHFS DI)Document10 pagesMelphalan (AHFS DI)maryNo ratings yet
- Hypertensive DietDocument6 pagesHypertensive DietCarlos NiñoNo ratings yet
- Contributors: Consulting EditorDocument249 pagesContributors: Consulting EditorJasNo ratings yet
- ADA EASD Consensus 2012Document16 pagesADA EASD Consensus 2012Beta Cells in DiabetesNo ratings yet
- 31 01 2024 Current Affairs Descriptive TelegramDocument22 pages31 01 2024 Current Affairs Descriptive TelegramDd DdNo ratings yet
- Reten Modern Dressing 2023 PKDMTDocument51 pagesReten Modern Dressing 2023 PKDMTMasros TukiranNo ratings yet
- Synopsis in The Management of Urinary Incontinence - 2017Document102 pagesSynopsis in The Management of Urinary Incontinence - 2017Dennise IlieNo ratings yet
- Chapter 13 - Diseases of White Blood Cells, Lymph Nodes, Spleen, and ThymusDocument10 pagesChapter 13 - Diseases of White Blood Cells, Lymph Nodes, Spleen, and ThymusAgnieszka WisniewskaNo ratings yet
- Postoperative Care in MedicalDocument5 pagesPostoperative Care in MedicalMark Russel Sean LealNo ratings yet
- TriageDocument37 pagesTriagekyuleen05No ratings yet
- 4 Hour Heat Stress Training Student Manual 508Document42 pages4 Hour Heat Stress Training Student Manual 508ZakirhasNo ratings yet
- Immediate Care of The NewbornDocument19 pagesImmediate Care of The Newbornelijah aquinoNo ratings yet
- Infection Control NY NewDocument6 pagesInfection Control NY NewRC PmedNo ratings yet
- Espectro Neuromielitis Óptica 2022 NejmDocument9 pagesEspectro Neuromielitis Óptica 2022 NejmOscar BushNo ratings yet
- Maternal Experience With Neonatal JaundiceDocument9 pagesMaternal Experience With Neonatal JaundiceLorraine BuelvaNo ratings yet
- 1.19 Exam PracticeDocument5 pages1.19 Exam Practicesunnr008.211No ratings yet
- CH 2Document88 pagesCH 2Saurabh JorwalNo ratings yet
- Flinstones Sex-Linked Traits Worksheet - F12Document4 pagesFlinstones Sex-Linked Traits Worksheet - F12Sophia RichardsonNo ratings yet
- Malaria DrugsDocument2 pagesMalaria DrugsZinnirah AzizulNo ratings yet
- Body Temperature PDFDocument56 pagesBody Temperature PDFBanupriya-No ratings yet
- Welcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinDocument16 pagesWelcome To Course Title: Clinical Pharmacy Topic: TDM of DigoxinUmair MazharNo ratings yet
- FCPS II CardiologyDocument32 pagesFCPS II CardiologyAamir HamaadNo ratings yet
- DS ICS DuaventDecilone ForteDocument6 pagesDS ICS DuaventDecilone ForteThrinNo ratings yet
- Crispin Teufel, CEO of Lincare, Named Chairman of The Council For Quality Respiratory CareDocument2 pagesCrispin Teufel, CEO of Lincare, Named Chairman of The Council For Quality Respiratory CarePR.comNo ratings yet
- Cardiorespiratory Assessment: Medical Chart ReadingDocument7 pagesCardiorespiratory Assessment: Medical Chart ReadingPrasath SelvarajNo ratings yet