Professional Documents
Culture Documents
Report bc90b 1710052260449
Report bc90b 1710052260449
Uploaded by
muralinaiduCopyright:
Available Formats
You might also like
- Rayner Trading Course PDFDocument39 pagesRayner Trading Course PDFmuralinaidu100% (2)
- Laboratory Test Report: Test Name Result Biological Reference Interval Uric AcidDocument5 pagesLaboratory Test Report: Test Name Result Biological Reference Interval Uric AcidBalraj EnjamuriNo ratings yet
- Report 190a3 1695110951228Document13 pagesReport 190a3 1695110951228Mohd Jaffer ShareefNo ratings yet
- ReportDocument16 pagesReport847x2rn6nwNo ratings yet
- Report Eaaf4 1695467677147Document16 pagesReport Eaaf4 1695467677147Mohd Jaffer ShareefNo ratings yet
- Report f642c 1704009629273Document16 pagesReport f642c 1704009629273Er Sumit SiwatchNo ratings yet
- Subhra Pattnaik ReportDocument4 pagesSubhra Pattnaik ReportSubhra pattnaikNo ratings yet
- 2024 06 08 Mr. Gajendra SolankiDocument2 pages2024 06 08 Mr. Gajendra SolankiGajendra SolankiNo ratings yet
- ReportDocument3 pagesReportPawan MadhesiyaNo ratings yet
- Nilesh Karani 13295 29-10-2023 20231029084151 StationerypdfmergedDocument22 pagesNilesh Karani 13295 29-10-2023 20231029084151 StationerypdfmergedsteelblackNo ratings yet
- 052305240050 Garg AXcrGl ZlPYxiDocument2 pages052305240050 Garg AXcrGl ZlPYximongasandy71No ratings yet
- Uetquwiuj 912083949Document4 pagesUetquwiuj 912083949TzvineZNo ratings yet
- Report GNDocument3 pagesReport GNPawan MadhesiyaNo ratings yet
- Report 9c0fcfa7Document3 pagesReport 9c0fcfa7Shivam SharmaNo ratings yet
- LFT (Liver Function Test) : Biological Reference Results Units Test NameDocument4 pagesLFT (Liver Function Test) : Biological Reference Results Units Test Namemetepraju0210No ratings yet
- N8 R 9 W3 Pupeyo RF RTWB 42 BRDocument2 pagesN8 R 9 W3 Pupeyo RF RTWB 42 BRPrashant KumarNo ratings yet
- 1-Liver Function Test - PO3921596584-773 - 230517 - 125136Document4 pages1-Liver Function Test - PO3921596584-773 - 230517 - 125136Moksh GujjarNo ratings yet
- Inborn Errors of Metabolism (Iem) Summary Report: Sr. No. Test Methodology Result Test TypeDocument2 pagesInborn Errors of Metabolism (Iem) Summary Report: Sr. No. Test Methodology Result Test TypeMallikharjunaRao medaNo ratings yet
- LabreportnewDocument5 pagesLabreportnewrudranshsahu5162No ratings yet
- Mrs Sonali Upadhiya: Interpretation: Interpretation For Hba1C% As Per American Diabetes Association (Ada)Document3 pagesMrs Sonali Upadhiya: Interpretation: Interpretation For Hba1C% As Per American Diabetes Association (Ada)CHINMAY UPADHYAYA X-DNo ratings yet
- Mr_Gyanendra_Singh_22_06_2024_04_17_39_PMDocument13 pagesMr_Gyanendra_Singh_22_06_2024_04_17_39_PMGyan AkshitaNo ratings yet
- Biochemistry: Investigation Observed Value Unit Biological Reference IntervalDocument15 pagesBiochemistry: Investigation Observed Value Unit Biological Reference IntervalAshutoshNo ratings yet
- Diabetic ProfileDocument3 pagesDiabetic ProfileAhmed EzzatNo ratings yet
- Babita DeviDocument4 pagesBabita Devitomofficialyt87No ratings yet
- Biochemistry CDCL CDCL-14403 17-18Document1 pageBiochemistry CDCL CDCL-14403 17-18Ashutosh SinghNo ratings yet
- Biochemistry CDCL CDCL-14403 17-18 PDFDocument1 pageBiochemistry CDCL CDCL-14403 17-18 PDFAshutosh SinghNo ratings yet
- 01 Altaf HossainDocument5 pages01 Altaf Hossainsumanbs8913No ratings yet
- Ap Land Titling ActDocument7 pagesAp Land Titling ActmurtyaretyNo ratings yet
- Multi Lab Id ReportDocument12 pagesMulti Lab Id ReportMayuresh NaikNo ratings yet
- PR1546497Document2 pagesPR1546497basavajsalagar1No ratings yet
- Department of Chemical Pathology: Liver Function TestsDocument3 pagesDepartment of Chemical Pathology: Liver Function TestsbabarchuhanNo ratings yet
- Lab ReportDocument7 pagesLab Reportabdulsamad202000No ratings yet
- LabReportNew - 2023-09-08T160827.328Document3 pagesLabReportNew - 2023-09-08T160827.328viraj kshirsagarNo ratings yet
- Test Name Result Biological Ref. Interval Method: SerumDocument5 pagesTest Name Result Biological Ref. Interval Method: SerumPranav SujayNo ratings yet
- LFT LalpathDocument2 pagesLFT Lalpathmoyic39272No ratings yet
- PdfText - 2024-03-15T191650.936Document1 pagePdfText - 2024-03-15T191650.936jayanthmahesh0403No ratings yet
- Test Results Units Biological Reference Range Hematology:::::: Ms. Farha MemonDocument5 pagesTest Results Units Biological Reference Range Hematology:::::: Ms. Farha MemonKM GASTRO CENTERNo ratings yet
- Date 16/feb/2020 02:12PM Unit Bio - Ref.Range: Laboratory Investigation ReportDocument1 pageDate 16/feb/2020 02:12PM Unit Bio - Ref.Range: Laboratory Investigation ReportBhupender SinghNo ratings yet
- Wa0002Document6 pagesWa0002swati_iabmNo ratings yet
- 09 Gouri Bala BagDocument5 pages09 Gouri Bala Bagsumanbs8913No ratings yet
- Department of Biochemistry Test Name Result Unit Bio. Ref. RangeDocument5 pagesDepartment of Biochemistry Test Name Result Unit Bio. Ref. RangeSudhanshuNo ratings yet
- Https2Ftdiagnostics Telangana Gov In2FViewFiles aspxReportId y7jhWHgPKAseGQIDocument8 pagesHttps2Ftdiagnostics Telangana Gov In2FViewFiles aspxReportId y7jhWHgPKAseGQIbhushanNo ratings yet
- Hba1C %Document10 pagesHba1C %Jatinder Singh (Sugar sales/HO)No ratings yet
- Clinical Biochemistry: Test Report Reg - No Age Name::: Reg - Date Collection:: Received: 15-Jul-2019 / 09:25 AMDocument8 pagesClinical Biochemistry: Test Report Reg - No Age Name::: Reg - Date Collection:: Received: 15-Jul-2019 / 09:25 AMAnuradha KommojuNo ratings yet
- Lab Report - ShivanandhamDocument7 pagesLab Report - ShivanandhamPO, ITDA BhadrachalamNo ratings yet
- Report 8b3a3101Document11 pagesReport 8b3a3101Pooja AgarwalNo ratings yet
- Apollo247 249052700 LabreportDocument7 pagesApollo247 249052700 LabreportASHWAQ JAANNo ratings yet
- Report of Mr. Amresh Kshirsagar PDFDocument4 pagesReport of Mr. Amresh Kshirsagar PDFSanket KathareNo ratings yet
- CD080524127_Vimlesh_7bb8Document9 pagesCD080524127_Vimlesh_7bb8shuklanarender66No ratings yet
- Biochemistry Test Name Result Bio. Ref. Range Method: C-Reactive Protein 0-5 Immuno Turbidometric AssayDocument10 pagesBiochemistry Test Name Result Bio. Ref. Range Method: C-Reactive Protein 0-5 Immuno Turbidometric AssayAnkur DeyNo ratings yet
- Course Case Studies - Viral HepatitisDocument5 pagesCourse Case Studies - Viral HepatitiswqmxmNo ratings yet
- Date 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalDocument11 pagesDate 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalAmit SinghNo ratings yet
- LIVER PROFILE LFT Test Report Format Example Sample Template Drlogy Lab ReportDocument1 pageLIVER PROFILE LFT Test Report Format Example Sample Template Drlogy Lab ReportM ShafiqNo ratings yet
- DR. Neelanjana SHARMADocument5 pagesDR. Neelanjana SHARMADr. Neelanjana SharmaNo ratings yet
- Saras 20231105033954957Document3 pagesSaras 20231105033954957Miracle of HornbillsNo ratings yet
- Erythrocytes: Reference: DR - NAINI SETALVAD Abhishek Khemka VID: 106191000857Document11 pagesErythrocytes: Reference: DR - NAINI SETALVAD Abhishek Khemka VID: 106191000857Abhishek KhemkaNo ratings yet
- Null 1Document3 pagesNull 1akshatbhandari08No ratings yet
- Geeta-Seth. 2404364Document4 pagesGeeta-Seth. 2404364BadAss GamingNo ratings yet
- Sample Hematology ResultDocument3 pagesSample Hematology ResultRaul ArranguezNo ratings yet
- Smart Full Body Checkup: Test Description Value(s) Unit(s) Reference RangeDocument13 pagesSmart Full Body Checkup: Test Description Value(s) Unit(s) Reference RangeShamsher SiddiqueNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Chamatkaram 2Document51 pagesChamatkaram 2muralinaiduNo ratings yet
- Cart Information - Reference Number: CHY0WR99LDWDocument1 pageCart Information - Reference Number: CHY0WR99LDWmuralinaiduNo ratings yet
- JeerapornKummabutr PaperDocument12 pagesJeerapornKummabutr PapermuralinaiduNo ratings yet
- Documents RequiredDocument1 pageDocuments RequiredmuralinaiduNo ratings yet
- Max Life - Comprehensive Accident Benefit Rider: UIN: 104B025V01Document7 pagesMax Life - Comprehensive Accident Benefit Rider: UIN: 104B025V01muralinaiduNo ratings yet
- Eleaflet Lifecover PDFDocument2 pagesEleaflet Lifecover PDFmuralinaiduNo ratings yet
- What A Song PDFDocument40 pagesWhat A Song PDFmuralinaiduNo ratings yet
- CostsOfSetting Up anSKADocument4 pagesCostsOfSetting Up anSKAmuralinaiduNo ratings yet
- Evaluation of Memory in Abacus LearnersDocument9 pagesEvaluation of Memory in Abacus LearnersmuralinaiduNo ratings yet
- Aha! Activities ExcerptsDocument10 pagesAha! Activities ExcerptsmuralinaiduNo ratings yet
- Old Adangal Application Form PDFDocument1 pageOld Adangal Application Form PDFmuralinaiduNo ratings yet
- Section 100-Index-Finally CorrectedDocument2 pagesSection 100-Index-Finally CorrectedmuralinaiduNo ratings yet
- NTPC Limited: Engineering Office Complex A-8A, SEC-24, NOIDA, U.P.201301 PH.:0120-2410333, FAX:0120-2410136Document2 pagesNTPC Limited: Engineering Office Complex A-8A, SEC-24, NOIDA, U.P.201301 PH.:0120-2410333, FAX:0120-2410136muralinaiduNo ratings yet
- BOQ For EarthworkDocument1 pageBOQ For EarthworkmuralinaiduNo ratings yet
- Annexure-100-A.1 (IS - IRC-List) - FINALLY CORRECTEDDocument14 pagesAnnexure-100-A.1 (IS - IRC-List) - FINALLY CORRECTEDmuralinaiduNo ratings yet
- Pulling Option ChainDocument317 pagesPulling Option ChainmuralinaiduNo ratings yet
- Bitumen Impregnated BoardDocument2 pagesBitumen Impregnated Boardmuralinaidu100% (1)
- Section-1000 (Materials For Structures)Document12 pagesSection-1000 (Materials For Structures)muralinaiduNo ratings yet
- Class-14 - Plasma Lipoproteins - EnzymesDocument39 pagesClass-14 - Plasma Lipoproteins - EnzymesAyi FurqonNo ratings yet
- CA2005 User Manual 1.3-Custom-FDocument34 pagesCA2005 User Manual 1.3-Custom-FDinesh SreedharanNo ratings yet
- Sarah Ding 3 PDFDocument108 pagesSarah Ding 3 PDFEdd NoddNo ratings yet
- Reflotron Plus Training ManualDocument54 pagesReflotron Plus Training ManualtransilvanpopNo ratings yet
- Comparative Hepatotoxicity of Fluconazole Ketocona PDFDocument10 pagesComparative Hepatotoxicity of Fluconazole Ketocona PDFPERMATASARI BKUNo ratings yet
- Clinical Chemistry 2 First GradingDocument25 pagesClinical Chemistry 2 First GradingMHEKAELLA SAMSONNo ratings yet
- Clinical EnzymologyDocument25 pagesClinical Enzymologyaminata6No ratings yet
- Aspartate Aminotransferase (Ast/Got)Document2 pagesAspartate Aminotransferase (Ast/Got)Ivana BajunovicNo ratings yet
- ENZYMOLOGYDocument2 pagesENZYMOLOGYCarla Lagar FloresNo ratings yet
- CC2 2Document13 pagesCC2 2Aedren TrillanaNo ratings yet
- Fahmida Nasrin: ID No: 1030883070 MS in Biotechnology Dept. of Biochemistry & Microbiology North South UniversityDocument28 pagesFahmida Nasrin: ID No: 1030883070 MS in Biotechnology Dept. of Biochemistry & Microbiology North South UniversitySadia Sharmin NilimaNo ratings yet
- Enzymes of Clinical SignificanceDocument65 pagesEnzymes of Clinical SignificancepaulaOrialNo ratings yet
- 1379 PDFDocument7 pages1379 PDFbalusaichanduNo ratings yet
- FRM Patient View All ReportDocument6 pagesFRM Patient View All ReportShailesh KumarNo ratings yet
- EN AST BAOSR6x09 USDocument2 pagesEN AST BAOSR6x09 UScarineNo ratings yet
- Chest InjuryDocument52 pagesChest InjuryJeyaganesh SellvarajuNo ratings yet
- CC 2 Lab - Amylase and LipaseDocument7 pagesCC 2 Lab - Amylase and LipaseAngelaAmmcoNo ratings yet
- KrushKrokMnemonics 1 1Document23 pagesKrushKrokMnemonics 1 1Fianyo DavidNo ratings yet
- Claudio Case Study of Pregnancy Induced HypertensionDocument78 pagesClaudio Case Study of Pregnancy Induced HypertensionTanya Victoria Lean ClaudioNo ratings yet
- Elitech Fully Automatic Chemistry AnalyzerDocument7 pagesElitech Fully Automatic Chemistry AnalyzerOmerNo ratings yet
- Topic: Protein Metabolism: Biochemistry & Biophysics: Paper-V, Unit-9Document14 pagesTopic: Protein Metabolism: Biochemistry & Biophysics: Paper-V, Unit-9aayushi tejwaniNo ratings yet
- Guillain Barre SyndromeDocument19 pagesGuillain Barre SyndromeCrisMartAgullanaNo ratings yet
- Hospi Clin ReviewDocument349 pagesHospi Clin ReviewCatherine AlduezaNo ratings yet
- CC1 Lab Fin V2Document22 pagesCC1 Lab Fin V2Melody PardilloNo ratings yet
- Laboratory Investigation Report: HaematologyDocument3 pagesLaboratory Investigation Report: HaematologyHarshitNo ratings yet
- Executive Health Check Up Package - RSPI - Pondok Indah - 2023Document20 pagesExecutive Health Check Up Package - RSPI - Pondok Indah - 2023stephanymelody123No ratings yet
- Liver Function TestsDocument3 pagesLiver Function TestsdanielazimzadehNo ratings yet
- Unit One Enzymes: General PropertiesDocument24 pagesUnit One Enzymes: General PropertiesHUAWEI HUAWEINo ratings yet
- Kaplan: Clinical Chemistry, 5 Edition: Clinical References - Methods of AnalysisDocument11 pagesKaplan: Clinical Chemistry, 5 Edition: Clinical References - Methods of AnalysispudjoNo ratings yet
- Clinical Enzymology-4th LevelDocument29 pagesClinical Enzymology-4th Leveltony maxxNo ratings yet
Report bc90b 1710052260449
Report bc90b 1710052260449
Uploaded by
muralinaiduOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Report bc90b 1710052260449
Report bc90b 1710052260449
Uploaded by
muralinaiduCopyright:
Available Formats
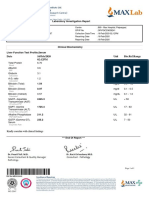
Name : Mr. N.
HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
BIOCHEMISTRY
Fasting Glucose 86 mg/dL Normal: 70-99
F- fluoride plasma,GOD-POD Impaired glucose: 100-125
Diabetes: >= 126
Creatinine 0.5 mg/dL 0.66-1.25
Serum,Enzymatic
Uric Acid 6.6 mg/dL 3.5-8.5
Serum,Uricase
Verified & Approved by: Reviewed by:
Page 1 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
LFT - LIVER FUNCTION TEST
Serum
Total Bilirubin 0.9 mg/dL Adult: 0.2-1.3
DSA Neonate: 1.0-10.5
Direct Bilirubin 0.1 mg/dL Neonate: 0.0-0.6
Calculated Adult: 0-0.3
Indirect Bilirubin 0.8 mg/dL Adult: 0.0-1.1
Dual wavelength Neonate: 0.6-10.5
Aspartate Transaminase(AST/ 20 U/L 17-49
SGOT)
MDH, UV Kinetic
Alanine Transaminase(ALT/ 14 U/L < 50
SGPT)
LDH, UV kinetic
Alkaline Phosphatase 211 U/L 74-390
PNPP, AMP Buffer
Gamma-Glutamyl Transferase 13 U/L 15-73
(GGT)
SZAZ Carboxylated Substrate
Total Protein 6.4 g/dL 6.0-8.3
Biuret
Albumin 4.2 g/dL 3.5-5.0
BCG
Globulin 2.2 g/dL 2.3-3.5
Calculated
A/G ratio 1.9 0.8-2.0
Calculated
Verified & Approved by: Reviewed by:
Page 2 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
SGOT/SGPT Ratio 1.4 0.7-1.4
Calculated
Total bilirubin is invariably increased in jaundice. Causes of jaundice are prehepatic, resulting from various hemolytic diseases; hepatic, resulting
from hepatocellular injury or obstruction; and posthepatic, resulting from obstruction of the hepatic or common bile ducts.
Aspartate aminotransferase is present in high activity in heart, skeletal muscle, and liver. Increased serum AST activity commonly follows
myocardial infarction, pulmonary emboli, skeletal muscle trauma, alcoholic cirrhosis, viral hepatitis, and drug-induced hepatitis.
Alanine aminotransferase is present in high activity in liver, skeletal muscle, heart, and kidney. Serum ALT increases rapidly in liver cell necrosis,
hepatitis, hepatic cirrhosis, liver tumours, obstructive jaundice, Reye’s syndrome, extensive trauma to skeletal muscle, myositis, myocarditis, and
myocardial infarction.
Alkaline phosphatase is elevated in fever and increased bone metabolism, for example, in adolescents and during the healing of a fracture;
primary and secondary hyperparathyroidism; Paget’s disease of bone; carcinoma metastatic to bone; osteogenic sarcoma; and Hodgkin’s disease if
bones are invaded. Hepatobiliary diseases involving cholestasis, inflammation, or cirrhosis increased ALP activity; also increased in renal infarction
and failure and in the complications of pregnancy. Low ALP activity may occasionally be seen in hypothyroidism.
Serum GGT is a sensitive indicator of hepatobiliary disease and is useful in the diagnosis of obstructive jaundice and chronic alcoholic liver
disease, in the follow-up of chronic alcoholics undergoing treatment, and in the detection of hepatotoxicity. GGT is more responsive to biliary
obstruction than AST, ALT, or ALP.
Total serum protein levels can be used for evaluation of nutritional status. Causes of high total serum protein concentration include dehydration,
Waldenström’s macroglobulinemia, multiple myeloma, hyperglobulinemia, granulomatous diseases, and some tropical diseases. Causes of low
total serum protein concentration include pregnancy, excessive intravenous fluid administration, cirrhosis or other liver diseases, chronic
alcoholism, heart failure, nephrotic syndrome, glomerulonephritis, neoplasia, protein-losing enteropathies, malabsorption, and severe malnutrition.
Verified & Approved by: Reviewed by:
Page 3 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
Glycosylated Haemoglobin - (HbA1c)
Whole Blood
Glycosylated Haemoglobin 5.3 % Normal: < 5.7
(HbA1c) Pre-Diabetes: 5.7-6.4
HPLC Diabetes: >= 6.5
Mean Blood Glucose 105 mg/dL
Calculated
HbA1C is used to monitor fluctuations in blood glucose concentration in the past 8 to 12 week’s period.
The reference interval defined as per American Diabetes Association guidelines 2016:
a) Less than 5.7% : Non Diabetic
b) 5.7 to 6.4% : at increased risk of developing diabetes in the future
c) More than 6.5% : Diabetic
d) Therapeutic glycemic target:
i. Adults: less than 7%
ii. Children with Type 1 diabetes : less than 7 %
e) Pregnant diabetic patients : less than 6.5%
Note:
• Targets may be individualized based on: Age/life expectancy, Comorbid conditions, Diabetes duration , Hypoglycemia status,
Individual patient considerations
Reference: American Diabetes Association. Standards of medical care in diabetes—2021.
Mean Blood Glucose is average Blood glucose which directly correlates with A1C, reported in the same units as blood sugar levels
(mg/dl). Thus it reflects the average glucose concentration in the past 8 to 12 weeks period. This should not be compared with
Fasting or Post prandial or random blood sugar which measures glucose concentration at that point of time of testing.
Blood Urea Nitrogen (BUN)
Serum
Blood Urea Nitrogen (BUN) 5.6 mg/dL 6-20
Calculated
Urea 12.0 mg/dL 19-42
Urease
Verified & Approved by: Reviewed by:
Page 4 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
HEMATOLOGY
Complete Blood Count
Whole Blood
RBC count 5.24 mill/cu.mm 4.5-5.5
DC Impedance method
Haemoglobin (Hb) 14.5 gm/dL 13.0-17.0
Cyanide-free SLS method
Haematocrit(PCV) 42.9 % 40-50
DC Impedance method
Mean Corpuscular Volume 81.8 fL 83-101
(MCV)
Calculated
Mean Corpuscular 27.6 pg 27-32
Haemoglobin(MCH)
Calculated
Mean Corpuscular 33.8 g/dL 31.5-34.5
Haemoglobin Concentration
(MCHC)
Calculated
Red cell distribution width 13.3 % 11.6-14.0
(RDW)
Calculated
Mentzer Index 16 Thal trait: <14, Iron deficiency
Calculated anaemia : >=14
Sehgal index 1277 Thal trait: <972, Iron deficiency
Calculated anaemia : >=972
Verified & Approved by: Reviewed by:
Page 5 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
Total WBC count - TC 4500 cells/cu.mm 4500-13500
Flow Cytometry
Differential Leucocyte Count - DC
Flow Cytometry
Neutrophils 45.0 % 40-80
Lymphocytes 42.4 % 20-40
Monocytes 9.8 % 2-10
Eosinophils 2.6 % 1-6
Basophils 0.2 % 0-2
Absolute Neutrophil Count 2025 / cu.mm 2000-7000
Calculated
Absolute Lymphocyte Count 1908 / cu.mm 1000-3000
Calculated
Absolute Monocyte Count 441 / cu.mm 200-1000
Calculated
Absolute Eosinophil Count 117 / cu.mm 20-500
Calculated
Absolute Basophil Count 9 / cu.mm 0-100
Calculated
NLR 1 % 1-3
Calculated
Verified & Approved by: Reviewed by:
Page 6 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
Platelet count 273 10^3/ul 150-450
DC Impedance method
Platelet Hematocrit 0.246 % 0.2-0.5
Mean Platelet Volume - MPV 9.0 µm3 7-13
1. Reference Ranges are in accordance with Dacie & Lewis Practical Hematology International Edition (12th).
2. As per International Council for Standardization in Hematology's recommendations Differential Leucocyte counts are additionally reported in
Absolute numbers in each cell per unit volume of blood.
Verified & Approved by: Reviewed by:
Page 7 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
CLINICAL PATHOLOGY
Urine Complete Analysis
Urine
PHYSICAL EXAMINATION
Volume 25 ml
Colour Pale Yellow Pale yellow
Manual
Appearance Clear Clear
Manual
CHEMICAL EXAMINATION
pH 6.0 5.0-8.0
Double indicator method
Specific gravity 1.025 1.001-1.035
Refractive Index
Protein Nil Nil
Protein error of pH indicator
Glucose Nil Nil
Enzyme method GOD POD
Ketone bodies Nil Nil
Dipstick
Bilirubin Nil Nil
Azo coupling method
Verified & Approved by: Reviewed by:
Page 8 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
Blood Negative Negative
Peroxidase activity
Urobilinogen Normal Normal
Azo coupling method
Leucocyte Esterase Negative Negative
Granulocyte esterase method
Nitrites Negative Negative
Griess method
MICROSCOPY EXAMINATION
Pus cells 1-2 /hpf 0-5
Flow digital Imaging
Epithelial cells 0-1 /hpf Occasional
Fixed point immuno-rate
RBCs Nil /hpf 0-2
Flow digital Imaging
Granular Casts Nil /hpf. Nil
Flow digital Imaging
Hyaline Casts Nil /hpf. Occasional.
Flow digital Imaging
Uric acid Crystals Nil /hpf. Nil
Flow digital Imaging
Phosphate Crystals Nil /hpf. Nil
Flow digital Imaging
Calcium Oxalate Crystals Nil /hpf. Nil
Flow digital Imaging
Verified & Approved by: Reviewed by:
Page 9 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
Amorphous urates Nil /hpf. Nil
Flow digital Imaging
Amorphous phosphates Nil /hpf. Nil
Flow digital Imaging
Yeast Nil /hpf. Nil
Flow digital Imaging
Bacteria Nil /hpf. Nil
Flow digital Imaging
Parasites Nil /hpf. Nil
Flow digital Imaging
Mucus Present /hpf. Nil
Flow digital Imaging
Verified & Approved by: Reviewed by:
Page 10 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
Name : Mr. N.HEMANTH CHOWDARY Age / Sex : 13 Year(s) / Male Collected On : 10/03/2024 08:56 AM
Patient ID : OHP6HJAL710391 Ref. Doctor : Received On : 10/03/2024 09:49 AM
Visit No. : HY7913001 Client : Getvisit TPA Reported On : 10/03/2024 10:39 AM
Test Results Units Biological Reference Interval
Increased protein in urine is seen in dehydration, kidney disorders, heart failure and transplant rejection. 24 hour urine
protein and Protein/creatinine ratio in a random urine sample recommended if increased.
Glucosuria can be seen in kidney disorders, uncontrolled diabetes mellitus, hormonal disorders, and pregnancy. To be
correlated with plasma glucose levels.
Ketonuria is seen in physical exercise, starvation, severe vomiting, exposure to cold, uncontrolled diabetes (diabetic
ketoacidosis)
Increased bilirubin levels should be followed up with Liver function tests and indicates conjugated hyperbilirubinemia.
Increased urobilinogen can be seen due to haemolysis, megaloblastic anaemia and haemorrhage in tissues.
Urobilinogen is absent or reduced in obstructive liver disease and antibiotic therapy.
RBCs in urine (Haematuria) can be seen in anticoagulant therapy, bleeding diathesis and traumatic catheterization
history to be looked into. Dysmorphic RBCs suggestive of glomerular pathology. Non glomerular diseases line
calculus, infections, tumours, after strenuous exercise and diseases of the prostate.
Increase in pus cells are elevated in cases of UTI, to be correlated with urine culture, if clinically indicated. Infection
can be in either the upper or lower urinary tract or with acute glomerulonephritis, tubule interstitial nephritis. Leucocyte
esterase detects esterase enzyme released from the granules of leucocytes.
Infected urine may contain considerable amounts of nitrite as a result of bacterial nitrate reductase activity, and
detection of nitrite in urine is routinely used in the diagnosis of bacterial cystitis. It is indicative of the requirement of
Urine culture and sensitivity testing for identification and treatment of UTI.
Hyaline casts are seen normally (not associated with disease states); seen after strenuous exercise and with non renal
diseases, such as dehydration.
Granular casts can be seen in acute glomerulonephritis and pyelonephritis.
-- End of Report --
Verified & Approved by: Reviewed by:
Page 11 / 11
Dr. Neha Jagdish Gajbi Dr. Abhijay Dharmadhikari
MD Pathologist
You might also like
- Rayner Trading Course PDFDocument39 pagesRayner Trading Course PDFmuralinaidu100% (2)
- Laboratory Test Report: Test Name Result Biological Reference Interval Uric AcidDocument5 pagesLaboratory Test Report: Test Name Result Biological Reference Interval Uric AcidBalraj EnjamuriNo ratings yet
- Report 190a3 1695110951228Document13 pagesReport 190a3 1695110951228Mohd Jaffer ShareefNo ratings yet
- ReportDocument16 pagesReport847x2rn6nwNo ratings yet
- Report Eaaf4 1695467677147Document16 pagesReport Eaaf4 1695467677147Mohd Jaffer ShareefNo ratings yet
- Report f642c 1704009629273Document16 pagesReport f642c 1704009629273Er Sumit SiwatchNo ratings yet
- Subhra Pattnaik ReportDocument4 pagesSubhra Pattnaik ReportSubhra pattnaikNo ratings yet
- 2024 06 08 Mr. Gajendra SolankiDocument2 pages2024 06 08 Mr. Gajendra SolankiGajendra SolankiNo ratings yet
- ReportDocument3 pagesReportPawan MadhesiyaNo ratings yet
- Nilesh Karani 13295 29-10-2023 20231029084151 StationerypdfmergedDocument22 pagesNilesh Karani 13295 29-10-2023 20231029084151 StationerypdfmergedsteelblackNo ratings yet
- 052305240050 Garg AXcrGl ZlPYxiDocument2 pages052305240050 Garg AXcrGl ZlPYximongasandy71No ratings yet
- Uetquwiuj 912083949Document4 pagesUetquwiuj 912083949TzvineZNo ratings yet
- Report GNDocument3 pagesReport GNPawan MadhesiyaNo ratings yet
- Report 9c0fcfa7Document3 pagesReport 9c0fcfa7Shivam SharmaNo ratings yet
- LFT (Liver Function Test) : Biological Reference Results Units Test NameDocument4 pagesLFT (Liver Function Test) : Biological Reference Results Units Test Namemetepraju0210No ratings yet
- N8 R 9 W3 Pupeyo RF RTWB 42 BRDocument2 pagesN8 R 9 W3 Pupeyo RF RTWB 42 BRPrashant KumarNo ratings yet
- 1-Liver Function Test - PO3921596584-773 - 230517 - 125136Document4 pages1-Liver Function Test - PO3921596584-773 - 230517 - 125136Moksh GujjarNo ratings yet
- Inborn Errors of Metabolism (Iem) Summary Report: Sr. No. Test Methodology Result Test TypeDocument2 pagesInborn Errors of Metabolism (Iem) Summary Report: Sr. No. Test Methodology Result Test TypeMallikharjunaRao medaNo ratings yet
- LabreportnewDocument5 pagesLabreportnewrudranshsahu5162No ratings yet
- Mrs Sonali Upadhiya: Interpretation: Interpretation For Hba1C% As Per American Diabetes Association (Ada)Document3 pagesMrs Sonali Upadhiya: Interpretation: Interpretation For Hba1C% As Per American Diabetes Association (Ada)CHINMAY UPADHYAYA X-DNo ratings yet
- Mr_Gyanendra_Singh_22_06_2024_04_17_39_PMDocument13 pagesMr_Gyanendra_Singh_22_06_2024_04_17_39_PMGyan AkshitaNo ratings yet
- Biochemistry: Investigation Observed Value Unit Biological Reference IntervalDocument15 pagesBiochemistry: Investigation Observed Value Unit Biological Reference IntervalAshutoshNo ratings yet
- Diabetic ProfileDocument3 pagesDiabetic ProfileAhmed EzzatNo ratings yet
- Babita DeviDocument4 pagesBabita Devitomofficialyt87No ratings yet
- Biochemistry CDCL CDCL-14403 17-18Document1 pageBiochemistry CDCL CDCL-14403 17-18Ashutosh SinghNo ratings yet
- Biochemistry CDCL CDCL-14403 17-18 PDFDocument1 pageBiochemistry CDCL CDCL-14403 17-18 PDFAshutosh SinghNo ratings yet
- 01 Altaf HossainDocument5 pages01 Altaf Hossainsumanbs8913No ratings yet
- Ap Land Titling ActDocument7 pagesAp Land Titling ActmurtyaretyNo ratings yet
- Multi Lab Id ReportDocument12 pagesMulti Lab Id ReportMayuresh NaikNo ratings yet
- PR1546497Document2 pagesPR1546497basavajsalagar1No ratings yet
- Department of Chemical Pathology: Liver Function TestsDocument3 pagesDepartment of Chemical Pathology: Liver Function TestsbabarchuhanNo ratings yet
- Lab ReportDocument7 pagesLab Reportabdulsamad202000No ratings yet
- LabReportNew - 2023-09-08T160827.328Document3 pagesLabReportNew - 2023-09-08T160827.328viraj kshirsagarNo ratings yet
- Test Name Result Biological Ref. Interval Method: SerumDocument5 pagesTest Name Result Biological Ref. Interval Method: SerumPranav SujayNo ratings yet
- LFT LalpathDocument2 pagesLFT Lalpathmoyic39272No ratings yet
- PdfText - 2024-03-15T191650.936Document1 pagePdfText - 2024-03-15T191650.936jayanthmahesh0403No ratings yet
- Test Results Units Biological Reference Range Hematology:::::: Ms. Farha MemonDocument5 pagesTest Results Units Biological Reference Range Hematology:::::: Ms. Farha MemonKM GASTRO CENTERNo ratings yet
- Date 16/feb/2020 02:12PM Unit Bio - Ref.Range: Laboratory Investigation ReportDocument1 pageDate 16/feb/2020 02:12PM Unit Bio - Ref.Range: Laboratory Investigation ReportBhupender SinghNo ratings yet
- Wa0002Document6 pagesWa0002swati_iabmNo ratings yet
- 09 Gouri Bala BagDocument5 pages09 Gouri Bala Bagsumanbs8913No ratings yet
- Department of Biochemistry Test Name Result Unit Bio. Ref. RangeDocument5 pagesDepartment of Biochemistry Test Name Result Unit Bio. Ref. RangeSudhanshuNo ratings yet
- Https2Ftdiagnostics Telangana Gov In2FViewFiles aspxReportId y7jhWHgPKAseGQIDocument8 pagesHttps2Ftdiagnostics Telangana Gov In2FViewFiles aspxReportId y7jhWHgPKAseGQIbhushanNo ratings yet
- Hba1C %Document10 pagesHba1C %Jatinder Singh (Sugar sales/HO)No ratings yet
- Clinical Biochemistry: Test Report Reg - No Age Name::: Reg - Date Collection:: Received: 15-Jul-2019 / 09:25 AMDocument8 pagesClinical Biochemistry: Test Report Reg - No Age Name::: Reg - Date Collection:: Received: 15-Jul-2019 / 09:25 AMAnuradha KommojuNo ratings yet
- Lab Report - ShivanandhamDocument7 pagesLab Report - ShivanandhamPO, ITDA BhadrachalamNo ratings yet
- Report 8b3a3101Document11 pagesReport 8b3a3101Pooja AgarwalNo ratings yet
- Apollo247 249052700 LabreportDocument7 pagesApollo247 249052700 LabreportASHWAQ JAANNo ratings yet
- Report of Mr. Amresh Kshirsagar PDFDocument4 pagesReport of Mr. Amresh Kshirsagar PDFSanket KathareNo ratings yet
- CD080524127_Vimlesh_7bb8Document9 pagesCD080524127_Vimlesh_7bb8shuklanarender66No ratings yet
- Biochemistry Test Name Result Bio. Ref. Range Method: C-Reactive Protein 0-5 Immuno Turbidometric AssayDocument10 pagesBiochemistry Test Name Result Bio. Ref. Range Method: C-Reactive Protein 0-5 Immuno Turbidometric AssayAnkur DeyNo ratings yet
- Course Case Studies - Viral HepatitisDocument5 pagesCourse Case Studies - Viral HepatitiswqmxmNo ratings yet
- Date 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalDocument11 pagesDate 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalAmit SinghNo ratings yet
- LIVER PROFILE LFT Test Report Format Example Sample Template Drlogy Lab ReportDocument1 pageLIVER PROFILE LFT Test Report Format Example Sample Template Drlogy Lab ReportM ShafiqNo ratings yet
- DR. Neelanjana SHARMADocument5 pagesDR. Neelanjana SHARMADr. Neelanjana SharmaNo ratings yet
- Saras 20231105033954957Document3 pagesSaras 20231105033954957Miracle of HornbillsNo ratings yet
- Erythrocytes: Reference: DR - NAINI SETALVAD Abhishek Khemka VID: 106191000857Document11 pagesErythrocytes: Reference: DR - NAINI SETALVAD Abhishek Khemka VID: 106191000857Abhishek KhemkaNo ratings yet
- Null 1Document3 pagesNull 1akshatbhandari08No ratings yet
- Geeta-Seth. 2404364Document4 pagesGeeta-Seth. 2404364BadAss GamingNo ratings yet
- Sample Hematology ResultDocument3 pagesSample Hematology ResultRaul ArranguezNo ratings yet
- Smart Full Body Checkup: Test Description Value(s) Unit(s) Reference RangeDocument13 pagesSmart Full Body Checkup: Test Description Value(s) Unit(s) Reference RangeShamsher SiddiqueNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Chamatkaram 2Document51 pagesChamatkaram 2muralinaiduNo ratings yet
- Cart Information - Reference Number: CHY0WR99LDWDocument1 pageCart Information - Reference Number: CHY0WR99LDWmuralinaiduNo ratings yet
- JeerapornKummabutr PaperDocument12 pagesJeerapornKummabutr PapermuralinaiduNo ratings yet
- Documents RequiredDocument1 pageDocuments RequiredmuralinaiduNo ratings yet
- Max Life - Comprehensive Accident Benefit Rider: UIN: 104B025V01Document7 pagesMax Life - Comprehensive Accident Benefit Rider: UIN: 104B025V01muralinaiduNo ratings yet
- Eleaflet Lifecover PDFDocument2 pagesEleaflet Lifecover PDFmuralinaiduNo ratings yet
- What A Song PDFDocument40 pagesWhat A Song PDFmuralinaiduNo ratings yet
- CostsOfSetting Up anSKADocument4 pagesCostsOfSetting Up anSKAmuralinaiduNo ratings yet
- Evaluation of Memory in Abacus LearnersDocument9 pagesEvaluation of Memory in Abacus LearnersmuralinaiduNo ratings yet
- Aha! Activities ExcerptsDocument10 pagesAha! Activities ExcerptsmuralinaiduNo ratings yet
- Old Adangal Application Form PDFDocument1 pageOld Adangal Application Form PDFmuralinaiduNo ratings yet
- Section 100-Index-Finally CorrectedDocument2 pagesSection 100-Index-Finally CorrectedmuralinaiduNo ratings yet
- NTPC Limited: Engineering Office Complex A-8A, SEC-24, NOIDA, U.P.201301 PH.:0120-2410333, FAX:0120-2410136Document2 pagesNTPC Limited: Engineering Office Complex A-8A, SEC-24, NOIDA, U.P.201301 PH.:0120-2410333, FAX:0120-2410136muralinaiduNo ratings yet
- BOQ For EarthworkDocument1 pageBOQ For EarthworkmuralinaiduNo ratings yet
- Annexure-100-A.1 (IS - IRC-List) - FINALLY CORRECTEDDocument14 pagesAnnexure-100-A.1 (IS - IRC-List) - FINALLY CORRECTEDmuralinaiduNo ratings yet
- Pulling Option ChainDocument317 pagesPulling Option ChainmuralinaiduNo ratings yet
- Bitumen Impregnated BoardDocument2 pagesBitumen Impregnated Boardmuralinaidu100% (1)
- Section-1000 (Materials For Structures)Document12 pagesSection-1000 (Materials For Structures)muralinaiduNo ratings yet
- Class-14 - Plasma Lipoproteins - EnzymesDocument39 pagesClass-14 - Plasma Lipoproteins - EnzymesAyi FurqonNo ratings yet
- CA2005 User Manual 1.3-Custom-FDocument34 pagesCA2005 User Manual 1.3-Custom-FDinesh SreedharanNo ratings yet
- Sarah Ding 3 PDFDocument108 pagesSarah Ding 3 PDFEdd NoddNo ratings yet
- Reflotron Plus Training ManualDocument54 pagesReflotron Plus Training ManualtransilvanpopNo ratings yet
- Comparative Hepatotoxicity of Fluconazole Ketocona PDFDocument10 pagesComparative Hepatotoxicity of Fluconazole Ketocona PDFPERMATASARI BKUNo ratings yet
- Clinical Chemistry 2 First GradingDocument25 pagesClinical Chemistry 2 First GradingMHEKAELLA SAMSONNo ratings yet
- Clinical EnzymologyDocument25 pagesClinical Enzymologyaminata6No ratings yet
- Aspartate Aminotransferase (Ast/Got)Document2 pagesAspartate Aminotransferase (Ast/Got)Ivana BajunovicNo ratings yet
- ENZYMOLOGYDocument2 pagesENZYMOLOGYCarla Lagar FloresNo ratings yet
- CC2 2Document13 pagesCC2 2Aedren TrillanaNo ratings yet
- Fahmida Nasrin: ID No: 1030883070 MS in Biotechnology Dept. of Biochemistry & Microbiology North South UniversityDocument28 pagesFahmida Nasrin: ID No: 1030883070 MS in Biotechnology Dept. of Biochemistry & Microbiology North South UniversitySadia Sharmin NilimaNo ratings yet
- Enzymes of Clinical SignificanceDocument65 pagesEnzymes of Clinical SignificancepaulaOrialNo ratings yet
- 1379 PDFDocument7 pages1379 PDFbalusaichanduNo ratings yet
- FRM Patient View All ReportDocument6 pagesFRM Patient View All ReportShailesh KumarNo ratings yet
- EN AST BAOSR6x09 USDocument2 pagesEN AST BAOSR6x09 UScarineNo ratings yet
- Chest InjuryDocument52 pagesChest InjuryJeyaganesh SellvarajuNo ratings yet
- CC 2 Lab - Amylase and LipaseDocument7 pagesCC 2 Lab - Amylase and LipaseAngelaAmmcoNo ratings yet
- KrushKrokMnemonics 1 1Document23 pagesKrushKrokMnemonics 1 1Fianyo DavidNo ratings yet
- Claudio Case Study of Pregnancy Induced HypertensionDocument78 pagesClaudio Case Study of Pregnancy Induced HypertensionTanya Victoria Lean ClaudioNo ratings yet
- Elitech Fully Automatic Chemistry AnalyzerDocument7 pagesElitech Fully Automatic Chemistry AnalyzerOmerNo ratings yet
- Topic: Protein Metabolism: Biochemistry & Biophysics: Paper-V, Unit-9Document14 pagesTopic: Protein Metabolism: Biochemistry & Biophysics: Paper-V, Unit-9aayushi tejwaniNo ratings yet
- Guillain Barre SyndromeDocument19 pagesGuillain Barre SyndromeCrisMartAgullanaNo ratings yet
- Hospi Clin ReviewDocument349 pagesHospi Clin ReviewCatherine AlduezaNo ratings yet
- CC1 Lab Fin V2Document22 pagesCC1 Lab Fin V2Melody PardilloNo ratings yet
- Laboratory Investigation Report: HaematologyDocument3 pagesLaboratory Investigation Report: HaematologyHarshitNo ratings yet
- Executive Health Check Up Package - RSPI - Pondok Indah - 2023Document20 pagesExecutive Health Check Up Package - RSPI - Pondok Indah - 2023stephanymelody123No ratings yet
- Liver Function TestsDocument3 pagesLiver Function TestsdanielazimzadehNo ratings yet
- Unit One Enzymes: General PropertiesDocument24 pagesUnit One Enzymes: General PropertiesHUAWEI HUAWEINo ratings yet
- Kaplan: Clinical Chemistry, 5 Edition: Clinical References - Methods of AnalysisDocument11 pagesKaplan: Clinical Chemistry, 5 Edition: Clinical References - Methods of AnalysispudjoNo ratings yet
- Clinical Enzymology-4th LevelDocument29 pagesClinical Enzymology-4th Leveltony maxxNo ratings yet