Professional Documents
Culture Documents
6862-Article Text-48212-1-10-20230712
6862-Article Text-48212-1-10-20230712
Uploaded by
dradnanahmad82Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
6862-Article Text-48212-1-10-20230712
6862-Article Text-48212-1-10-20230712
Uploaded by
dradnanahmad82Copyright:
Available Formats
Original Article
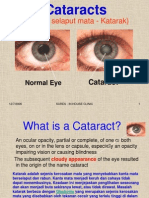
Comparison of the Efficacy of Diclofenac 0.1% and Nepafenac 0.1%
on anterior chamber cells in patients Undergoing Cataract Surgery:
t
A prospective clinical practice trial
Adnan Ahmad1, Shams Ul Haq2, Jamal Hussain3, Javed Rasul4
in
ABSTRACT
Objectives: To compare the efficacy of topical Nepafenac 0.1 % and Diclofenac 0.1% eye drops in reducing the aqueous
cells in the anterior chamber in an un-eventful post cataract surgery.
Methods: This prospective, clinical trial was conducted at an Eye OPD of Qazi Hussain Ahmad Medical Complex,
Nowshera from January till December 2021. Ophthalmic assessment included Visual acuity (VA), slit-lamp examination,
Intraocular pressure (IOP), Central macular thickness (CMT) by Optical coherence tomography (OCT) and anterior
pr
chamber-aqueous cells measurement pre-operatively and at day 1st, 2nd, 4th and 8th week post-operatively. Patients
were randomly allocated to topical diclofenac 0.1% (TD) four times a day and nepafenac 0.1% (TN) three times a day
for four weeks each along with topical steroids and antibiotics.
Results: Seventy patients (70) were randomly distributed into two treatment arms of 35 each. In both the arms
VA improved which achieved a level of statistical significance post-operatively, however statistically insignificant
difference was observed between the groups at 8th week follow up visit (p= 0.62). However, IOP and CMT values didn’t
achieve statistical significance between the arms pre and post operatively. In TN arm, level of AC-cells at 2nd and 4th
week post-operatively were significantly lower (10.54 ± 4.05 and 08.20 ± 4.44) than TD arm (11.28 ± 5.04 and 09. 66 ±
5.50) with statistically significant difference (p < 0.05).
of
Conclusions: Topical Nepafenac 0.1% was more effective in suppressing the anterior chamber inflammation as compared
to diclofenac during the early few post-operative weeks.
KEYWORDS: Anterior chamber inflammation, Aqueous cells, Cataract surgery, Topical nepafenac 0.1%, Topical
diclofenac 0.1%.
doi: https://doi.org/10.12669/pjms.39.5.6862
How to cite this: Ahmad A, Haq S, Hussain J, Rasul J. Comparison of the Efficacy of Diclofenac 0.1% and Nepafenac 0.1% on anterior chamber cells in patients
Undergoing Cataract Surgery: A prospective clinical practice trial. Pak J Med Sci. 2023;39(5):---------. doi: https://doi.org/10.12669/pjms.39.5.6862
ad
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted
use, distribution, and reproduction in any medium, provided the original work is properly cited.
1. Dr. Adnan Ahmad (FCPS, FRCS [UK], FICO (UK).
Associate Professor, Dept. of Eye, INTRODUCTION
Nowshera Medical College,
Qazi Hussain Medical Complex, Nowshera, Pakistan. Phacoemulsification is commonly employed procedure
2. Dr. Shams Ul Haq (FCPS). for cataract removal globally. The latest advancement in
3. Dr. Jamal Hussain (FCPS).
4. Dr. Javed Rasul (FCPS). the phacoemulsification mechanics have considerably
mitigated the adverse visual outcomes and enhanced its
he
Assistant Professor, Dept. of Eye,
Pak International Medical College, safety but still complications do occur. Cystoid macular
Peshawar, Pakistan.
edema (CME), with an estimated occurrence between 0.2
2,3: Consultant Ophthalmologist,District Headquarter Hospital, % and 4.1 %, causes of sub-optimal visual acuity (VA)
Timergara, Lower Dir, Pakistan. after an un-eventful cataract extraction1,2 post-operative
Correspondence: inflammatory reaction is one of the most important causes
Dr. Adnan Ahmad, for CME, mainly due to the disruption of the inner blood
Associate Professor, Department of Eye,
retinal barrier by the inflammatory mediators dispersed
Nowshera Medical College, Qazi Hussain Medical Complex,
inside the eye.3 There is release of inflammatory markers
A
Nowshera, Pakistan.
Postal Address: Eye Dept. Qazi Hussain Ahmad Medical Complex, during cataract surgery in the anterior chamber which
Near Kabul River, Mardan road, Nowshera. permeates into the vitreous and finally reaches the retinal
Email: dradnanahmad@hotmail.com
vascular bed. There is increased vascular permeability
* Received for Publication: July 8, 2022 especially in the peri-foveal zone, leading to build-up
* 1st Revision Received: August 20, 2022 of fluid in the region manifested in the form of post-op
* 2nd Revision Received: May 31, 2023 CME.4,5 There is a well-established relationship between
* Final Revision Accepted: June 15, 2023 the intensity of post-op (cataract) inflammation and the
Pak J Med Sci September - October 2023 Vol. 39 No. 5 www.pjms.org.pk 1
Adnan Ahmad et al.
development of severe CME reported in some studies.6 Inclusion and Exclusion Criteria: Patients’ ≥ 50 yrs.
The above statement signifies that by lowering the post- Both males and females with visually significant senile-
operative inflammation the occurrence of CME can be cataracts under-going phaco-emulsification with intra-
reduced. Topical non-steroidal anti-inflammatory drugs ocular implants were selected.
(NSAIDs), alone or in combination with topical steroids, We excluded patients with any past intra-ocular sur-
are widely used post-operatively in order to decrease the gery, any history of intra-ocular inflammatory diseases,
risk for CME development.7 traumatic globe injuries, corneal disorders impairing the
Anterior chamber aqueous cells (AC-cells) view, any glaucomatous diseases of eye, pseudo-exfolia-
measurement is used to grade the amount of the
t
tion and maculopathies such as macular edema due to oth-
inflammatory reaction in AC, the level of which signifies er etiologies or epi-retinal membranes or any age-related
the severity of blood aqueous barrier disruption.8,9 In this maculopathy. Those not willing to follow the study pro-
in
manner, AC-cells measurement may effectively evaluate tocols and requirements of follow up were also excluded.
the efficacy of topical Diclofenac and Nepafenac in Those who were pre-diabetics and confirmed diabetics,
altering the level of AC inflammation post-operatively with systemic autoimmune/inflammatory disorders or
and hence its impact on the CME development. To any history of allergic reaction to the study drugs or other
the best of our knowledge, limited studies have been NSAIDs were also excluded. Oral steroids or NSAIDs in-
conducted to date comparing two different NSAIDs by take was prohibited for the participants throughout the
pr
evaluating their responses on AC-cells.1,3 The rationale trial duration. Patients with eventful phaco surgery such
of the trial was to evaluate the therapeutic effectiveness as posterior-capsular tear, vitreous-prolapse or post-oper-
of both NSAIDs in suppressing the AC-cells and its
ative fibrinous reactions were not recruited for the study.
impact on preventing the development of post-op CME,
Methods: All subjects underwent baseline evaluation a
which is an important cause of reduced vision in post
week before surgery. Pre-operative evaluation comprised
cataract surgery patients.
of a detailed ophthalmic assessment including VA which
METHODS was converted in log MAR, slit lamp examination,
intra-ocular pressure (IOP) and biometry performed
A prospective, randomized control trial was con-
with Qantel Medical (France). AC-cells were counted
ducted, at an Ophthalmology department of Qazi Hus-
of
under slit lamp with 1.6* magnification brought in with
sain Ahmad Medical Complex, Nowshera from January
a slit beam of 1mm*1mm.8 Three consecutive readings
till December 2021. We included a total of 70 patients
in our trial, methodology of our study is shown in the were taken with the technique as mentioned above and
Fig.1. The trial was conducted in accordance with the average value was taken out as final measurement. The
tenets of Declaration of Helsinki and guidelines of good level of AC-cells was graded as shown in Table-I.8 Central
clinical practice. The trial had been registered with macular thickness (CMT) was measured by spectral
Iranian registry of clinical trials (IRCT) with trial id domain Optical coherence tomography (Topcon Inc.
IRCT20220607055097N2 at https://www.irct.ir. Written Japan) dense volume scan (15°×15°, approx. 5×5mm), 49
informed consent was acquired from all the participants B-scans each spaced 110 μ apart, were obtained with the
ad
of trial prior to the commencement of study. automatic real-time function operative.
Ethical Approval: The study was granted approval by the Table-I: Standardization of Uveitis Nomenclature (SUN)
Institutional ethical review board (IERB) with No.0283 Working Group Grading of Anterior chamber Cells
/R&D/IERB/NMC. (1mm by 1mm Slit Beam).
Grade Cells in field
0 0
he
0.5 1-5
1 6-15
2 16-25
3 26-50
4 > 50
* Bowling B. Kanski, Clinical Ophthalmology. A
systemic approach. In Uveitis. Elsevier publishing
Co. 9th ed; 2020; p 4278
A
At the day of the surgery, patients were randomly al-
located to one of the two treatment arms by computer-
generated randomization (topical diclofenac arm as TD
and topical nepafenac group as TN arm). All the surger-
ies were done under peri-bulbar LA and performed by a
single experienced senior surgeon, with the same phaco-
Fig.1: Flow chart showing the study methodology. emulsification machine and surgical technique and all the
Pak J Med Sci September - October 2023 Vol. 39 No. 5 www.pjms.org.pk 2
Efficacy of topical Diclofenac Vs Nepafenac in post-operative ocular inflammation
patients underwent hydrophilic foldable Intaocular Lens Table-III: Mean BC-VA in Log MAR at follow-ups
(IOL) implantation.
TD (N=35) TN (N=35) p-value
At the end of the procedure an intra-cameral injection of
0.5 mg of moxifloxacin was given, and 0.5% moxifloxacin Baseline 0.45 ± 0.4 0.46 ± 0.2 .246
and 0.1% dexamethasone combination eye-drops 2nd post-op week 0.03 ± 0.02 0.02± 0.05 .145
(Deximox, Allergan Inc. USA) were commenced. At the 4th post-op week 0.02 ± 0.04 0.02 ± 0.01 .562
time of discharge, all patients were put on Moxifloxacin 8th post-op week 0.01 ± 0.00 0.01 ± 0.02 .622
0.5% and dexamethasone 0.1% eye drops four times daily
for a week followed by reduction of one drop each week BC-VA= Best corrected-visual acuity, Log MAR= Log.
t
as a tapering regimen. Of minimum angle of resolution
Patients randomized to TD arm received diclofenac statistically significant between the groups. On 1st post-op
in
0.1% eye drops solution (DiclominR 0.1%, Schazoo day, AC-cells were significantly higher (20.15 ± 4.6 in TD
Inc. Pak) four times daily for four weeks, while TN and 19.44 ± 5.6 in TN) than before surgery (2.24 ± 1.5 in
arm received nepafenac 0.1% drops (CuranepR 0.1%, TD and 2.64 ± 1.6 in TN) in both arms (p<0.05). AC-cells
Schazoo Inc. Pak) three times/day for four weeks. Post- reduced in the 4th week (11.28 ± 5.04 in TD, 10.54 ± 4.05
operative full assessment was done by performing AC- in TN) and gradually reached pre-operative levels by 8th
cells measurement with slit lamp and CMT by spectral week in both treatment arms. We observed a statistically
significant difference (p<0.05) between the two arms in
pr
domain OCT on day 1st, 2nd, 4th and 8th week respectively.
Statistical Analysis: Statistical analysis was done by terms of AC-cells at two consecutive time points i.e., 2nd
using SPSS version 26.0 (IBM Corp. USA). Continuous/ and 4th week post-operatively. In fact, AC-cells values in
quantitative variables were expressed as mean and TN (10.54 ± 4.05 and 08.20 ± 4.44) were significantly lower
than in TD (11.28 ± 5.04 and 9. 66 ± 5.50) respectively.
standard deviation. As the data was not normally
(Table-IV). CMT didn’t change significantly throughout
distributed so non-parametric tests were conducted to
the length of study, with statistically insignificant
see for the significance of results.
difference between the two arms. (Table-V).
For within the group analysis Wilcoxon signed rank
test was performed and between the group analyses we DISCUSSION
used Mann Whitney test. For conducting correlational
of
analysis between AC-cells and BC-VA non-parametric In this trial, the comparative efficacy between TD 0.1% vs.
test Kendall’s tau-b was conducted. The statistical tests TN 0.1% in suppressing the AC-cells after un-complicated
Phacoemulsification revealed that both drugs were
were set at less than 5% for significance of analysis.
effective, but TN appeared to be more effective than TD
RESULTS at 2nd and 4th week post-op. Post-operative inflammation
Seventy patients were recruited for the trial. All the remained an important cause of delayed visual restoration
participants successfully completed the entire follow- among the patients who underwent cataract extraction.7
up. Two patients, one from TD and one from TN, Numerous studies have been published regarding the
developed CME with a markedly reduced VA. The mean efficacy of different agents utilized in suppression of
ad
age was 65.2 ± 6.4yrs. Forty were males (57.1%) and 30 Table-IV: Mean AC-cells in two treatment arms at follow-ups
were female patients (42.9%). (Table-II). Pre-operative
and post-operative mean-VA in both arms is shown in TD (N=35) TN (N=35) p-value
Table-II. BC-VA improved in both groups by achieving a
Baseline 2.24 ± 1.5 2.64 ± 1.6 .128
level of statistical significance (p <0.05), however, between
1st post-op day 20.15 ± 4.6 19.44 ± 5.6 .122
Table-II: Baseline characteristics of patients. 2nd post-op week 11.28 ± 5.04• 10.54 ± 4.05• <.05
4th post-op week 09. 66 ± 5.50• 08.20 ± 4.44• <.05
TD (N=35) TN (N=35) p-value
he
8th post-op week 2.20 ± 1.2 2.00 ± 1.5 .08
Mean age in- 64.6 ± 5.8 66.1 ± 5.4yrs .242
AC= Anterior Chamber, • p-value < 0.05
yrs. ± SD
Gender
Male 20 18 Table-V: Mean CMT measured by OCT in two
Female 15 17 treatment arms at follow-ups
BC-VA 0.45 ± 0.4 0.46 ± 0.2 .246
CMT 280.2 ± 30.1 281.1 ± 26.4 .166 TD (N=35) TN (N=35) p-value
A
AC-cells 2.24 ± 1.5 2.64 ± 1.6 .128 Baseline CMT in µm 280.2 ± 30.1 281.1 ± 26.4 .166
BC-VA= Best corrected-visual acuity, CMT= central 1st post-op day CMT 280.9 ± 26.2 279.8 ± 28.2 .174
macular thickness, AC= Anterior chamber 2nd post-op week CMT 280.5 ± 30.1 280.0 ± 26.2 .082
4th post-op week CMT 282.2 ± 24.5 281.8 ± 25.5 .106
the group analysis revealed statistically insignificant
8th post-op week CMT 284.1 ± 26.6 283.8 ± 24.2 .092
difference throughout the entire length of study (p>0.05).
In Table-III Difference between pre-operative and post- CMT= central macular thickness, OCT= optical
operative IOP values at 2nd, 4th and 8th week was not coherence tomography.
Pak J Med Sci September - October 2023 Vol. 39 No. 5 www.pjms.org.pk 3
Adnan Ahmad et al.
post-operative inflammation.1,3,4,6 Steroids are commonly findings should not underestimate the significance of
employed agents used post-operatively after intra-ocular controlling the post-operative (cataract) inflammation in
procedures to control the inflammation by inhibiting the 1st few weeks because this is the most likely factor for
the enzyme Phospholipase A2 that is elevated many the development of CME and visual deterioration.1-7,9,11-15
folds post-op, in this way the level of arachidonic acid is In corroboration with the above statement, two patients
reduced which acts as a potent inflammatory mediator.10 of our population developed CME with increased AC-
NSAIDs are also often prescribed post-operatively cells during the entire post-operative length of study. Our
and numerous studies have shown that they are more findings, are supported by the findings from other studies
effective than corticosteroids in preventing the disruption for stringent control of post-operative inflammation to
t
of blood retinal barrier post-op and hence it prevents the reduce the incidence of CME.9
development of post-operative CME.4,11,12 In contrast to our study observation, Ylinen et al.17
in
Numerous trials have been done to discover the reported no difference between nepafenac 0.1% and
effective therapy that helps prevent the development diclofenac 0.1% in controlling post-operative inflammation
of CME. Reports from various trials regarding the (post-op cataract surgery). The disagreement may be
effectiveness of the different topical NSAIDs are still not attributed to many factors like sample size, patient
yet clear and there are still gaps in the literature regarding demographics, methodology and frequency of doses (eye
the most effective topical NSAID which requires further drops) used in the subjects. Furthermore, he recruited
pr
comparative studies.12 patients with systemic/ocular diseases such as pseudo-
Duan et al.13 did a systematic review by comparing exfoliation syndrome (PXF), diabetes or sporadic use of
different NSAIDs in terms of their efficacy and safety
systemic anti-inflammatory drugs. However, we excluded
for the control of AC-cells post-operatively (cataract).
such patients from our study. Interestingly one study
They evaluated total of 12 studies, comparing the
reported that ocular as well as systemic inflammatory
efficacy of various topical NSAIDs. They found out that,
conditions can influence post-operative AC-cells value, as
Diclofenac-0.1% was more effective in improving AC
reaction post-op, whereas Nepafenac 0.1% was better at in cases of PXF.18
reducing the ocular pain. The pitfall of this review was A local study conducted by Sarfraz et al.19 on the efficacy
that AC reaction was measured with flare-meter only of topical Nepafenac 0.1% in prevention of pseudophakic
of
in two of the studies taken for analysis. In one of them cystoid macular edema in diabetic patients, concluded
diclofenac-Na 0.1% was compared to ketorolac 0.5%, that the incidence of macular edema was 3.3% as compare
in the second one diclofenac-Na 0.1% to flurbiprofen to those patients not receiving it i.e., 23.3%, this difference
0.03%, and indomethacin 0.1%.4,14 Our findings were was statistically significant, the author described this effect
opposite to their observations of Diclofenac efficacy in due the anti-inflammatory effect of nepafenac both in the
suppressing post-operative inflammation. In our study anterior as well as posterior chamber of the eye. Another
AC-cells were significantly reduced at 2nd and 4th week local study by Ullah et al.20 compared two groups one
post-op, in the TN treatment arm. Other researchers have was given topical nepafenac 0.1% along with standard
studied the incidence of post-operative CME and/or
ad
post-op medications (steroids and antibiotics) while
changes in CMT during the follow-ups.15 In these cases, other group was only given standard post op regimen
limitations can be due to the fact that there is still a lack of only in post phacoemulsification patients, the results
consensus in defining significant macular post-operative
showed that macular thickness was statistically less (p <
changes. Furthermore, macular thickness fluctuation is
0.01) in nepafenac group versus standard regimen only,
an indirect index of intra-ocular inflammation which can
the above two local studies support our study finding
be governed by many factors such as ocular diseases/
therapies, pre-operative and post-operative medications of reduced macular edema post operatively in topical
and systemic conditions.15,16 Another study reported the nepafenac due to its enhanced anti-inflammatory efficacy.
he
efficacy of topical nepafenac as post-operative therapy in Similar to the above two studies yet another study done
suppressing the AC inflammation as compared to other locally by Amjad et al.21 supporting the findings derived
classes of NSAIDs.3 We noted that during the 1st few from the above studies by showing the significance of
weeks, post-op TN appeared more effective than TD, topical nepafenac in reducing the macular thickness
which is widely used and safe NSAID. In support of other (edema) in post cataract surgery diabetic patients but
studies done we observed AC-cells level almost similar without retinopathy versus those patients not being given
eight weeks post-operatively to the baseline in both arms, nepafenac, the comparison was done at 1st and 4th week
with statistically insignificant difference between groups.
A
post operatively with statistically significant difference. It
In our study, different levels of AC-cells at the 4th week may be due to its better penetration, bio availability and
post-op didn’t have any clinical consequences. We didn’t pharmacokinetics as compared to diclofenac making it
notice any significant difference in VA and CMT during more effective in suppressing the inflammation.
the entire length of study between the two groups. These
findings are in agreement with other published studies, Limitations: It includes small sample size, lack of control
showing that reduced post-operative inflammation group, limited follow up period, lack of blinding in the
didn’t correlate with better VA.3,17 However, such study. Further prospective, multi-center randomized
Pak J Med Sci September - October 2023 Vol. 39 No. 5 www.pjms.org.pk 4
Efficacy of topical Diclofenac Vs Nepafenac in post-operative ocular inflammation
control trials are needed to further explore any gaps in 10. Vane JR, Botting RM. Mechanism of action of anti-inflammatory
drugs. Scand J Rheumatol Suppl. 1996;102:9-21. doi:
knowledge in this area to better understand the usefulness 10.3109/03009749609097226
of these agents in post-operative regimen. 11. Kessel L, Tendal B, Jørgensen KJ, Erngaard D, Flesner P, Andresen
JL, Hjortdal J: Postcataract Prevention of Inflammation and Macular
CONCLUSIONS Edema by Steroid and Nonsteroidal Anti-inflammatory Eye Drops
A Systematic Review. Ophthalmology. 2014;121(10):1915-1924. doi:
Topical Nepafenac 0.1% was more effective in 10.1016/j.ophtha.2014.04.035
suppressing the anterior chamber inflammation as 12. Sivaprasad S, Bunce C, Wormald R. Non-steroidal anti-
inflammatory agents for cystoid macular oedema following cataract
compared to diclofenac during the 1st few weeks post- surgery: a systematic review. Br J Ophthalmol. 2005;89:1420–1422.
t
operatively. It may be due to its better penetration, doi: 10.1136/bjo.2005.073817
bio availability and pharmacokinetics as compared to 13. Duan P, Liu Y, Li J: The comparative efficacy and safety of topical
diclofenac making it more effective in suppressing the non-steroidal anti-inflammatory drugs for the treatment of anterior
in
chamber inflammation after cataract surgery: a systematic review
inflammation and network meta-analysis. Graefes Arch Clin Exp Ophthalmol.
2017;255(4):639-649. doi: 10.1007/s00417-017-3599-8
Acknowledgement: I am thankful to my departmental 14. Diestelhorst M, Schmidl B, Konen W, Mester U, Raj PS: Efficacy
head for providing me guidance, general support and and tolerance of diclofenac sodium 0.1%, flurbiprofen 0.03%, and
providing conducive environment for conducting my indomethacin 1.0% in controlling post-operative inflammation. J
Cataract Refract Surg, 1996;22(Suppl1):788–793. doi: 10.1016/s0886-
trial. I would also like to acknowledge my ancillary and 3350(96)80163-5
paramedic staff of Eye dept. who helped me in arranging
pr
15. Cagini C, Fiore T, Iaccheri B, Piccinelli F, Ricci MA, Fruttini D:
necessary equipment and support throughout the Macular Thickness Measured by Optical Coherence Tomography
in a Healthy Population before and After Uncomplicated Cataract
duration of trial. Phacoemulsification Surgery. Current Eye Res. 2009;34(12):1036–
Conflicts of interest: None. 1041. doi: 10.3109/02713680903288937
Financial disclosure: None. 16. Kim SJ, Bressler NM. Optical coherence tomography and cataract
surgery. Curr Opin Ophthalmol. 2009;20:46–51. doi: 10.1097/
REFERENCES icu.0b013e3283199162
17. Ylinen P, Taipale C, Lindholm J, Laine I, Holmstrom E, Tuuminen
1. Kim SJ, Schoenberger SD, Thorne JE, Ehlers JP, Yeh S, Bakri SJ: Topical R. Postoperative management in cataract surgery: nepafenac
nonsteroidal anti-inflammatory drugs and cataract surgery: a report and preservative-free diclofenac compared. Acta Ophthalmol.
by the American Academy of Ophthalmology. Ophthalmology. 2018;96(8):853-859. doi: 10.1111/aos.13843
of
2015;122:2159–2168. doi: 10.1016/j.ophtha.2015.05.014 18. Coassin M, Iovieno A, Soldani A, Cavuto S, Cimino L, Sartori A, et
2. McCafferty S, Harris A, Kew C, Kassm T, Lane L, Levine J, Raven M. al. Bromfenac ophthalmic solution 0.09% as an adjunctive therapy
Pseudophakic cystoid macular edema prevention and risk factors; to topical steroids after cataract surgery in pseudoexfoliation
prospective study with adjunctive once daily topical nepafenac syndrome. J Cataract Refract Surg. 2016;42:1119–1125.
0.3% versus placebo. BMC Ophthalmol. 2017;17:16. doi: 10.1186/ doi: 10.1016/j.jcrs.2016.04.031
s12886-017-0405-7 19. Sarfraz MH, Intisar-ul-Haq R, Mehboob MA. Effect of topical
3. Sahu S, Ram J, Bansal R, Pandav SS, Gupta A: Effect of topical ketorolac nepafenac in prevention of macular edema after cataract surgery in
0.4%, nepafenac 0.1%, and bromfenac 0.09% on postoperative patients with non-proliferative diabetic retinopathy. Pak J Med Sci.
inflammation using laser flare photometry in patients having 2017;33(1):210-214. doi: 10.12669/pjms.331.11644
phacoemulsification. J Cataract Refract Surg. 2015;41:2043–2048. 20. Ullah W, Irfan M, Khan SAR. Ghalib A, Khalil ZU. Role of topical
doi: 10.1016/j.jcrs.2015.10.061 nepafenac in preventing increase in macular thickness after
4. Flach AJ, Dolan BJ, Donahue ME, Faktorovich EG, Gonzalez phacoemulsification. J Postgrad Med Inst. 2021;34(4):253-258.
ad
GA: Comparative Effects of Ketorolac 0.5% or Diclofenac 0.1% 21. Amjad A, Shaheer M, Tariq H, Rasheed A. Impact of Topical
Ophthalmic Solutions on Inflammation after Cataract Surgery. Nepafenac on Macular thickness after Phacoemulsification
Ophthalmology. 1998;105:1775–1779. doi: 10.1016/s0161- with Intraocular lens Implantation in Patients without Diabetic
6420(98)99053-4 Retinopathy. J Rawalpindi Med Coll. 2022;26(2):301-305. doi:
5. Miyake K. Four decades of topical nonsteroidal antiinflammatory 10.37939/jrmc.v26i2.1877
drugs use. Current issues and controversies. J Cataract Refract Surg.
2018;44(4):421-423 doi: 10.1016/j.jcrs.2018.02.021 Author’s Contribution:
6. Aliò JL, Sayans JA, Chipont E: Flare-cell meter measurement of AA: Study design, concept, data acquisition &
inflammation after uneventful cataract surgery with intraocular
lens implantation. J Cataract Refract Surg. 1997;23(6):935-939. doi: interpretation.
he
10.1016/s0886-3350(97)80256-8 SUH: Data acquisition & interpretation, critical revision
7. Wielders LHP, Schouten JSAG, Winkens B, van den Biggelaar and editing.
FJHM, Veldhuizen CA, Findl O, et al. European multicenter trial
of the prevention of cystoid macular edema after cataract surgery
JH: Statistical analysis, literature search, final draft
in nondiabetics: ESCRS PREMED study report 1. J Cataract Refract preparation.
Surg. 2018;44(4):429-439. doi: 10.1016/j.jcrs.2018.01.029 JR: Critical revision, editing of manuscript, final draft.
8. Bowling B. Kanski, Clinical Ophthalmology. A systemic approach. All of the above authors are responsible and accountable
Uveitis. Elsevier publishing Co. 9th ed; 2020;427.
9. Ersoy L, Caramoy A, Ristau T, Kirchhof B, Fauser S. Aqueous flare for the accuracy or integrity of the work.
is increased in patients with clinically significant cystoid macular
A
oedema after cataract surgery. Br J Ophthalmol. 2013;97:862–865.
doi: 10.1136/bjophthalmol-2012-302995
Pak J Med Sci September - October 2023 Vol. 39 No. 5 www.pjms.org.pk 5
You might also like
- Mcqs For Frcophth Part 2Document253 pagesMcqs For Frcophth Part 2Ophthalmology PLUS100% (4)
- Kuhn 2016Document548 pagesKuhn 2016Karan Kumarswamy100% (1)
- Transient Corneal Edema After Phacoemulsification: Original ArticleDocument5 pagesTransient Corneal Edema After Phacoemulsification: Original ArticlesarassashaNo ratings yet
- Comparison of The Outcomes of Phacoemulsification and Manual Small-IncisionDocument5 pagesComparison of The Outcomes of Phacoemulsification and Manual Small-Incisionkoas mr14No ratings yet
- M J Opht 1 1 004Document7 pagesM J Opht 1 1 004Pra BowoNo ratings yet
- Jcrs 48 1242Document6 pagesJcrs 48 1242ririen refrina sariNo ratings yet
- Emanuel 2017Document4 pagesEmanuel 2017Kimberly Ann SumbillaNo ratings yet
- MainDocument7 pagesMainiSee ClinicNo ratings yet
- Comparison of Ketorolac 0.4 and Nepafenac 0.1 For The Prevention of Cystoid Macular Oedema After PhacoemulsifiDocument6 pagesComparison of Ketorolac 0.4 and Nepafenac 0.1 For The Prevention of Cystoid Macular Oedema After PhacoemulsifiMinh NguyenNo ratings yet
- Clinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusDocument10 pagesClinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusPunam RazputriNo ratings yet
- Central Corneal Thickness Changes Following Manual Small Incision Cataract Surgery Versus Phacoemulsification For White CataractDocument7 pagesCentral Corneal Thickness Changes Following Manual Small Incision Cataract Surgery Versus Phacoemulsification For White CataractFadhila AnggariniNo ratings yet
- Prasanna Uday Patil, Supriya Sudhir Pendke, Mousumi Bandyopadhyay, Purban GangulyDocument4 pagesPrasanna Uday Patil, Supriya Sudhir Pendke, Mousumi Bandyopadhyay, Purban GangulyMinh NguyenNo ratings yet
- Recurrent Floaters Following Limited Vitrectomy For Vision Degrading MyodesopsiaDocument14 pagesRecurrent Floaters Following Limited Vitrectomy For Vision Degrading Myodesopsiamistic0No ratings yet
- Comparison of A Preservative Free Nonsteroidal.Document7 pagesComparison of A Preservative Free Nonsteroidal.Danty IndriastutyNo ratings yet
- Intracameral Mydriatics Versus Topical Mydriatics in Pupil Dilation For Phacoemulsification Cataract SurgeryDocument5 pagesIntracameral Mydriatics Versus Topical Mydriatics in Pupil Dilation For Phacoemulsification Cataract SurgeryGlaucoma UnhasNo ratings yet
- Evaluating The Therapeutic Response of Intra-Vitreal Moxifloxacin in Acute Post-Operative (Cataract) EndophthalmitisDocument6 pagesEvaluating The Therapeutic Response of Intra-Vitreal Moxifloxacin in Acute Post-Operative (Cataract) Endophthalmitisdradnanahmad82No ratings yet
- Jurding Mata JimmDocument8 pagesJurding Mata JimmNisia SetiabektiNo ratings yet
- Uploads PDF PDF 1768Document7 pagesUploads PDF PDF 1768nedimbali784883No ratings yet
- Deep Learning For Automatically Visual Evoked Potential Classification During Surgical Decompression of Sellar Region TumorDocument7 pagesDeep Learning For Automatically Visual Evoked Potential Classification During Surgical Decompression of Sellar Region TumoradityaNo ratings yet
- Randomized Clinical Trial of Topical Betaxolol For Persistent Macular Edema After Vitrectomy and Epiretinal Membrane RemovalDocument8 pagesRandomized Clinical Trial of Topical Betaxolol For Persistent Macular Edema After Vitrectomy and Epiretinal Membrane RemovalsiscaNo ratings yet
- Ahmed Glaucoma Valve and Single-Plate Molteno Implants in Treatment of Refractory Glaucoma: A Comparative StudyDocument10 pagesAhmed Glaucoma Valve and Single-Plate Molteno Implants in Treatment of Refractory Glaucoma: A Comparative StudyVlady BordaNo ratings yet
- Phacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearDocument6 pagesPhacoemulsification Versus Manual Small Incision Cataract Surgery in Hard NuclearRagni MishraNo ratings yet
- Conventional - Extracapsular - Cataract - Extraction - and CirugiaDocument4 pagesConventional - Extracapsular - Cataract - Extraction - and CirugiaPedro PeredaNo ratings yet
- The Use of The Drug Visque in Age-Related Macular Degeneration of The RetinaDocument7 pagesThe Use of The Drug Visque in Age-Related Macular Degeneration of The RetinaCentral Asian StudiesNo ratings yet
- Ischemia Modified Albumin As A Useful Marker For Diagnoses and Management of Diabetic RetinopathyDocument5 pagesIschemia Modified Albumin As A Useful Marker For Diagnoses and Management of Diabetic RetinopathyMarcellia AngelinaNo ratings yet
- OpthalmologiDocument7 pagesOpthalmologirais123No ratings yet
- 2011 DelyferDocument8 pages2011 DelyferCitra Azma AnggitaNo ratings yet
- Intraocular Pressure 1Document6 pagesIntraocular Pressure 1Sher KhanNo ratings yet
- Jur DingDocument9 pagesJur DingLisa SariNo ratings yet
- The Effectiveness of Immediate Triamcinolone Acetonide Injection After Auricular Keloid Surgery: A Prospective Randomized Controlled TrialDocument8 pagesThe Effectiveness of Immediate Triamcinolone Acetonide Injection After Auricular Keloid Surgery: A Prospective Randomized Controlled TrialMarande LisaNo ratings yet
- Management of Pseudophakic Cystoid Macular Edema: SciencedirectDocument15 pagesManagement of Pseudophakic Cystoid Macular Edema: SciencedirectAnonymous TXkxLh138kNo ratings yet
- MataDocument16 pagesMataIslah NadilaNo ratings yet
- Jurnal Mata 5Document6 pagesJurnal Mata 5Dahru KinanggaNo ratings yet
- Outcomes of Deep Sclerectomy Following Failed XENDocument13 pagesOutcomes of Deep Sclerectomy Following Failed XENSagar ShahNo ratings yet
- Complication Rate in Preliminary Experience in Phacoemulsification Cataract SurgeryDocument5 pagesComplication Rate in Preliminary Experience in Phacoemulsification Cataract SurgeryimtiazbscNo ratings yet
- The Effectiveness of Laser Vitreolysis For Vitreous Floaters in Posterior Vitreous DetachmentDocument7 pagesThe Effectiveness of Laser Vitreolysis For Vitreous Floaters in Posterior Vitreous Detachmentmistic0No ratings yet
- Results of Staged Combined Laser Treatment of Neovascular GlaucomaDocument4 pagesResults of Staged Combined Laser Treatment of Neovascular GlaucomaCentral Asian StudiesNo ratings yet
- Jurnal 2Document5 pagesJurnal 2Asniar RNo ratings yet
- Ajphe v3 Id1036Document4 pagesAjphe v3 Id1036Amirah PaneNo ratings yet
- Bhargavaetal 17Document7 pagesBhargavaetal 17Flor ArenasNo ratings yet
- Incidence of Cystoid Macular Edema After Descemet Membrane Endothelial KeratoplastyDocument6 pagesIncidence of Cystoid Macular Edema After Descemet Membrane Endothelial KeratoplastynoonilNo ratings yet
- Ameerh Et Al., 2012Document5 pagesAmeerh Et Al., 2012vitor auzierNo ratings yet
- Editorial: The Management of Retinal Detachment: Techniques and PerspectivesDocument3 pagesEditorial: The Management of Retinal Detachment: Techniques and PerspectivesSarahNo ratings yet
- OmanJOphthalmol93150-4980548 135005Document7 pagesOmanJOphthalmol93150-4980548 135005ririen refrina sariNo ratings yet
- Comprehensive Management of Orbital Fractures: SummaryDocument7 pagesComprehensive Management of Orbital Fractures: SummaryDeng PanNo ratings yet
- Ijsrmjournal, Journal Manager, 17 IjsrmDocument9 pagesIjsrmjournal, Journal Manager, 17 IjsrmashishNo ratings yet
- 2005 Minimally Invasive Glaucoma SurgeryDocument9 pages2005 Minimally Invasive Glaucoma SurgeryJoseNo ratings yet
- Intravitreal Bevacizumab (Avastin) Therapy For Persistent Diffuse Diabetic Macular EdemaDocument7 pagesIntravitreal Bevacizumab (Avastin) Therapy For Persistent Diffuse Diabetic Macular EdemaJose Antonio Fuentes VegaNo ratings yet
- Retrospective Analysis of Sterile Corneal Infiltrates in Patients With Keratoconus After CrossLinking Procedure 2022Document10 pagesRetrospective Analysis of Sterile Corneal Infiltrates in Patients With Keratoconus After CrossLinking Procedure 2022fn_millardNo ratings yet
- Outcomes of Descemet Membrane Endothelial Keratoplasty in Patients With PreviouDocument6 pagesOutcomes of Descemet Membrane Endothelial Keratoplasty in Patients With PreviouRaúl Plasencia SaliniNo ratings yet
- Effect of Dexmedetomidine in Sub-Tenon's Block On Emergence Agitation in Pediatric Strabismus Surgery Under Sevoflurane Anesthesia - PMCDocument14 pagesEffect of Dexmedetomidine in Sub-Tenon's Block On Emergence Agitation in Pediatric Strabismus Surgery Under Sevoflurane Anesthesia - PMCamostafa.betaNo ratings yet
- Adminku Journal Manager ErlaniDocument7 pagesAdminku Journal Manager Erlanirm suryaubungNo ratings yet
- Mata 2Document4 pagesMata 2lala putriNo ratings yet
- Wound Healing After Photorefractive Keratectomy: Update/reviewDocument16 pagesWound Healing After Photorefractive Keratectomy: Update/reviewAngga WibowoNo ratings yet
- Predictors of Outcome in Fungal KeratitisDocument6 pagesPredictors of Outcome in Fungal KeratitisAl NaifNo ratings yet
- Pars Plana VitrekDocument8 pagesPars Plana VitrekAnggisari Danastri DharmaNo ratings yet
- Ringkasan Pustaka Edema Kornea 7Document6 pagesRingkasan Pustaka Edema Kornea 7B OriestoNo ratings yet
- European Multicenter Trial of The Prevention of Cystoid Macular Edema After Cataract Surgery in Nondiabetics: ESCRS PREMED Study Report 1Document11 pagesEuropean Multicenter Trial of The Prevention of Cystoid Macular Edema After Cataract Surgery in Nondiabetics: ESCRS PREMED Study Report 1salvadorNo ratings yet
- None 3Document11 pagesNone 3Yehiel FlaviusNo ratings yet
- Scheimpflug Corneal Densitometry Changes After TrabeculectomyDocument7 pagesScheimpflug Corneal Densitometry Changes After TrabeculectomyFernando MartínezNo ratings yet
- General Anesthesia Versus Local Anesthesia For Penetrating Keratoplasty: A Prospective StudyDocument5 pagesGeneral Anesthesia Versus Local Anesthesia For Penetrating Keratoplasty: A Prospective StudyhandykaaaNo ratings yet
- Choroidal NeovascularizationFrom EverandChoroidal NeovascularizationJay ChhablaniNo ratings yet
- Phacoemulsification Versus Small Incision Cataract Surgery For Treatment ofDocument7 pagesPhacoemulsification Versus Small Incision Cataract Surgery For Treatment ofRagni MishraNo ratings yet
- Cataract Surgery EvolutionDocument2 pagesCataract Surgery EvolutionIa BezhashviliNo ratings yet
- Price Frimen 2021 TerbaruDocument23 pagesPrice Frimen 2021 TerbaruRisty AnnaNo ratings yet
- Annexure-I: Revised Rate List Under The West Bengal Health Scheme, 2008 (Notification No. 796-F (MED) Dated 31-01-2011)Document51 pagesAnnexure-I: Revised Rate List Under The West Bengal Health Scheme, 2008 (Notification No. 796-F (MED) Dated 31-01-2011)tanmoyNo ratings yet
- Phacoemulsification & Extra Capsular Cataract ExtractionDocument7 pagesPhacoemulsification & Extra Capsular Cataract ExtractionJo-anne CorderoNo ratings yet
- Associate 6000Document12 pagesAssociate 6000avastfNo ratings yet
- 25 - Corneal Edema After PhacoemulsificationDocument10 pages25 - Corneal Edema After PhacoemulsificationOphthalmology Resident UNSRAT manado 2017No ratings yet
- My Experience in FRCS Ophthalmology Glasgow June 2017Document5 pagesMy Experience in FRCS Ophthalmology Glasgow June 2017LalNo ratings yet
- PgfgfygDocument3 pagesPgfgfygCrypto DocNo ratings yet
- Ophtha TMC Lec3Document16 pagesOphtha TMC Lec3Anonymous ic2CDkFNo ratings yet
- Khusbu Keyal 2017 PDFDocument10 pagesKhusbu Keyal 2017 PDFFelicia SutarliNo ratings yet
- Cataract and Eye Care DCaDocument26 pagesCataract and Eye Care DCaSamuil SumpalNo ratings yet
- Nylon LoopDocument4 pagesNylon LooporlandgpicadoNo ratings yet
- (123doc) - Opthalmic-Microsurgical-Suturing-Techniques-Part-3-PpsxDocument15 pages(123doc) - Opthalmic-Microsurgical-Suturing-Techniques-Part-3-PpsxTEODORA MIHAELA PELEASANo ratings yet
- Case Review - EndophthalmitisDocument4 pagesCase Review - EndophthalmitisDr Shawgat Ul Karim KhanNo ratings yet
- Jurnal IOL - PDF'Document4 pagesJurnal IOL - PDF'Noni RahmawatiNo ratings yet
- International Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR)Document4 pagesInternational Council of Ophthalmology's Ophthalmology Surgical Competency Assessment Rubrics (ICO-OSCAR)zaidoonys1No ratings yet
- Senile Cataract (Age-Related Cataract) Treatment & Management - Medical Care, Surgical Care, ConsultationsDocument5 pagesSenile Cataract (Age-Related Cataract) Treatment & Management - Medical Care, Surgical Care, ConsultationsAhmad FahroziNo ratings yet
- Opth 13 1877Document9 pagesOpth 13 1877Nurulia RizkiNo ratings yet
- CataractDocument38 pagesCataractruhulcoc1No ratings yet
- 2012 Katalyst Surgical Catalog PDFDocument69 pages2012 Katalyst Surgical Catalog PDFDien Doan QuangNo ratings yet
- Cat Surg GreenhornsDocument83 pagesCat Surg GreenhornsumakantsinghNo ratings yet
- Birth of The Intraocular LensDocument198 pagesBirth of The Intraocular LensNurul Ramadhani MustafaNo ratings yet
- Advances in OphthalmologyDocument618 pagesAdvances in OphthalmologyirinaNo ratings yet
- MUHS Question BankDocument23 pagesMUHS Question BanksuhasNo ratings yet
- Sukruthi Rate List 2020Document2 pagesSukruthi Rate List 2020Dr PrashanthNo ratings yet
- The Basics of Fluidics: A Thorough Understanding Is Essential For Successful PhacoemulsificationDocument3 pagesThe Basics of Fluidics: A Thorough Understanding Is Essential For Successful PhacoemulsificationMohammad A. BawtagNo ratings yet
- Surgical Glove Perforation Among Nurses in Ophthalmic SurgeryDocument8 pagesSurgical Glove Perforation Among Nurses in Ophthalmic SurgeryAdel AdielaNo ratings yet