Professional Documents
Culture Documents
WJG 22 4438
WJG 22 4438
Uploaded by
prasanna1047Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
WJG 22 4438
WJG 22 4438
Uploaded by
prasanna1047Copyright:
Available Formats
Submit a Manuscript: http://www.wjgnet.
com/esps/ World J Gastroenterol 2016 May 14; 22(18): 4438-4445
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 1007-9327 (print) ISSN 2219-2840 (online)
DOI: 10.3748/wjg.v22.i18.4438 © 2016 Baishideng Publishing Group Inc. All rights reserved.
TOPIC HIGHLIGHT
2016 Liver Transplantation: Global view
Liver transplantation: Current status and challenges
Caroline C Jadlowiec, Timucin Taner
Caroline C Jadlowiec, Timucin Taner, William J. von progress, however, also brings up the next set of
Liebig Transplantation Center, Division of Transplant Surgery, challenges: First, organ shortage remains a major
Department of Surgery, Mayo Clinic, Rochester, MN 55905, limitation, and accounts for a large proportion of wait
United States list mortality. While living donation has successfully
increased the total number of liver transplants done in
Author contributions: Jadlowiec CC and Taner T contributed
equally to the conception and design, writing of the article, and Asian countries, the total number of such transplants
critical revision. has been stagnant in the western hemisphere. As such,
there has been a significant effort over the past decade
Conflict-of-interest statement: The authors declare no conflicts to increase the existing deceased donor pool. This
of interest. effort has resulted in a greater use of liver allografts
following donation after cardiac death (DCD) along
Open-Access: This article is an open-access article which was with marginal and extended criteria donors. Improved
selected by an in-house editor and fully peer-reviewed by external understanding of the pathophysiology of liver allografts
reviewers. It is distributed in accordance with the Creative
procured after circulatory arrest has not only resulted
Commons Attribution Non Commercial (CC BY-NC 4.0) license,
which permits others to distribute, remix, adapt, build upon this in better selection and management of DCD donors,
work non-commercially, and license their derivative works on but has also helped in the development of mechanical
different terms, provided the original work is properly cited and perfusion strategies. Early outcomes demonstrating
the use is non-commercial. See: http://creativecommons.org/ the clinical applicability of both hypothermic and
licenses/by-nc/4.0/ normothermic perfusion and its potential to impact
patient survival and allograft function have generated
Correspondence to: Timucin Taner, MD, PhD, William J. von much interest. Second, long-term outcomes of liver
Liebig Transplantation Center, Division of Transplant Surgery, transplant recipients have not improved significantly,
Department of Surgery, Mayo Clinic, 200 Second Street South-
as recipients continue to succumb to complications
west, Rochester, MN 55905,
United States. taner.timucin@mayo.edu of long-term immunosuppression, such as infection,
Telephone: +1-507-2663117 malignancy and renal failure. Furthermore, recent
Fax: +1-507-2669806 evidence suggests that chronic immune-mediated
injury to the liver may also impact graft function.
Received: February 17, 2016
Peer-review started: February 18, 2016 Key words: donation after cardiac death; mechanical
First decision: March 21, 2016 perfusion; renal-sparing immunosuppression; antibody-
Revised: March 25, 2016 mediated rejection
Accepted: April 7, 2016
Article in press: April 7, 2016
© The Author(s) 2016. Published by Baishideng Publishing
Published online: May 14, 2016
Group Inc. All rights reserved.
Core tip: Organ shortage remains a major limitation
in liver transplantation, and there has been a
Abstract significant effort over the past decade to increase
Great progress has been made in the field of liver the existing deceased donor pool. Recent advances
transplantation over the past two decades. This have included better selection and management
WJG|www.wjgnet.com 4438 May 14, 2016|Volume 22|Issue 18|
Jadlowiec CC et al . Liver transplantation: Current status and challenges
of donors after circulatory arrest, application of non-function, hepatic artery thrombosis, ischemic
hypothermic and normothermic perfusion, minimization [2,3]
cholangiopathy, and allograft failure . With increasing
of standard immunosuppression and use of new experience, however, factors associated with improved
immunosuppressive medications. Additionally, there outcomes have been identified and more centers have
has been renewed emphasis and understanding of begun to use these donors .
[4-6]
liver immunology and the impact of antibody-mediated To date, there have been several large retrospective
rejection. Together, these advances have allowed for analyses which have identified DCD donor-related
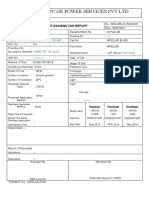
expansion of the donor pool with concurrent improved variables associated with recipient outcomes (Figure
patient outcomes.
1). Young age (45 ± 10 years old), short donor warm
ischemia time (less than thirty minutes), and limited
Jadlowiec CC, Taner T. Liver transplantation: Current status cold ischemia time (less than ten hours) have been
[4-6]
and challenges. World J Gastroenterol 2016; 22(18): 4438-4445 shown to improve allograft outcomes . In the Mayo
Available from: URL: http://www.wjgnet.com/1007-9327/full/ Clinic experience, every minute added to the warm
v22/i18/4438.htm DOI: http://dx.doi.org/10.3748/wjg.v22. ischemia period between asystole and cross-clamp was
i18.4438 found to be associated with a 16.1 percent increase
[6]
in the odds of ischemic cholangiopathy . Recipient
factors associated with improved DCD outcomes
generally concentrate on avoidance of sicker patients:
INTRODUCTION excluding patients requiring retransplantation, patients
with renal failure (creatinine > 2.0 mg/dL) and patients
Over the last several decades, the field of trans [5]
on life support . The correlation between these
plantation has witnessed much change yet, among
factors and outcomes is likely related to minimization
all solid organ transplants, arguably the greatest
of both cold ischemia time and further allograft injury
advances have been in liver transplantation. Today,
through recipient instability. As a result, by applying
liver transplantation is universally accepted as the only
these donor and recipient criteria, DCD outcomes
treatment option for end-stage liver disease, acute
have improved considerably with recipient survival and
fulminant hepatic failure, hepatocellular carcinoma, hilar
allograft function similar to that of donation after brain
cholangiocarcinoma and several metabolic disorders. [4-6]
death (DBD) donors .
Advancements in surgical technique, perioperative
management and immunosuppressive therapy have
yielded excellent short-term graft and patient survival Mechanical perfusion of deceased donor liver allografts
outcomes which have become the expected norm. With Despite these improved outcomes, many DCD livers
these advances comes the next set of challenges: organ continue to go unused as a result of unacceptable
shortage and improving long-term outcomes of the liver donor parameters and concern for poor allograft
transplant recipients. function. The concept of mechanical perfusion for
solid organ transplantation was originally introduced
[7]
in the late 1960s by Belzer et al and renewed
ORGAN SHORTAGE interest returned following a report by Moers et al
[8]
The disparity between the number of available liver in 2000 which, through a prospective randomized
allografts and transplant candidates continue to grow control trial, demonstrated a decreased incidence of
worldwide. In Asia, this problem has been successfully delayed graft function and improved graft survival in in
addressed by ever-increasing numbers of living- kidney transplant recipients. Since then, hypothermic
donor liver transplantation (LDLT). In the western machine perfusion in kidney transplantation has
countries, however, the number of LDLT has not seen a gained a widespread use. Although suboptimal, static
significant change for over a decade, and the demand hypothermic cold storage remains the primary method
for deceased donor liver allografts continue to increase. for liver preservation, largely because of its cost
Thus, substantial effort has been put in to expand the effectiveness, simplicity, and logistics. At present, there
existing deceased donor pool. is a large and apparent need to optimize preservation
particularly for DCD, marginal, and extended-criteria
Use of donation after cardiac death liver allografts donor organs. These allografts are subject to a greater
In the early 1990s, the use of livers procured from risk of ischemia-reperfusion injury which occurs as
donation after cardiac death (DCD) donors was an a result of donor warm ischemia time, aortic cross-
early attempt to narrow the disparity between organs clamping and initiation of cold ischemia, rewarming
[1]
and recipients in need . The early experience with during graft implantation, and finally full reperfusion
DCD livers was not favorable, as prolonged donor (Figure 1). It is here that the utility of mechanical
warm ischemia time and ischemia-reperfusion injury perfusion has emerged as potential solution to this
likely played a large role in the high rate of primary problem.
WJG|www.wjgnet.com 4439 May 14, 2016|Volume 22|Issue 18|
Jadlowiec CC et al . Liver transplantation: Current status and challenges
Cessation of MAP < 50 until Incision to aortic
Waiting period
cardiopulmonary support cardiopulmonary cannulation and in situ
(2-5 min)
until MAP < 50 arrest cold preservation
Total warm ischemia time
Functional warm ischemia time
Ref.
Ref. Txp
Txp Period
Period No. Patients
No. Patients Donor Age
Donor Age WITWIT CIT CIT Asystole-to-cross
Asystole-to-crossclamp
clamp
44 1996-2006
1996-2006 874 874 ≤≤ 4545yryr ≤ 15min
≤ 15 min1 1
≤≤ 10 10 h
55 1996-2003
1996-2003 367 367 --- - << 30 min
30 min
1 1
< <1010hh
66 1998-2010
1998-2010 200 200 --- - --- - --- - Minimization
Minimization of asystole-to-
of asystole-to-
cross clamp time time
cross clamp (1 min ≈
16.1% (1
IC)min ≈ 16.1% IC)
Figure 1 Favorable donation after cardiac death donor criteria. 1From time of cessation of cardiopulmonary support to with loss of hemodynamic and respiratory
function up to the in situ initiation of cold preservation solution. MAP: Mean arterial pressure; WIT: Warm ischemia time; IC: Ischemia cholangiopathy.
Table 1 Comparison of hypothermic and normothermic mechanical perfusion
Hypothermic mechanical perfusion Normothermic mechanical perfusion
Temperature 4℃ 37 ℃
Pathophysiology Reduced cellular metabolism Continued cellular metabolism
Non-functioning liver during preservation Functioning liver during preservation
Perfusate No specific requirements, oxygen can be used Continuous delivery of nutrients and oxygen needs to be maintained
Logistics Similar to that of hypothermic mechanical perfusion More complex
currently used for renal allografts
Benefits Logistically easier Allows for the assessment of metabolic and synthetic function during
preservation
May provide benefit in marginal livers May provide benefit in marginal livers
Potential use in steatotic livers
Felt to reduce ischemia reperfusion injury
Hypothermic perfusion their results evaluating DCD livers treated with HOPE
Hypothermia slows cellular metabolism and prolongs along with matched static cold storage DCD livers. As
the amount of time an organ can be deprived of anticipated, results for DCD livers subjected to HOPE
oxygen without loss of viability (Table 1). In liver were superior with decreased graft injury, decreased
transplantation, hypothermic perfusion has shown intrahepatic cholangiopathy and biliary complications
[9] [13]
similar benefits. Authors Guarrera et al have and improved 1-year graft survival . Similarly,
demonstrated that hypothermic perfusion decreases hypothermic machine perfusion has also been applied
the extent of graft injury and subsequent clinical studies to extended criteria DBD donor liver allografts with
by the same group have shown improved allograft encouraging outcomes, such as decreased allograft
function, lower serum transaminases and decreased dysfunction (19% vs 30%), improved patient survival
hospital stay as compared to matched historic cold at one year (84% vs 80%) and a reduction in biliary
[11]
storage liver allografts from DBD donors
[10,11]
. Equally complications (13% vs 43%) .
beneficial results have been reported in DCD liver
Normothermic perfusion
[12,13]
allografts . In a trial using human DCD livers,
Hypothermic Oxygenated PErfusion (HOPE) was applied Normothermic perfusion is technically more deman
[12]
for 1 to 2 h prior to implantation . Functional warm ding, as it requires a continuous delivery of nutrients
ischemia time (MAP < 50 mmHg to cold flush) in this and oxygen in order to maintain ongoing cellular
[14]
group ranged from 22 to 41 min and postoperative metabolism . In theory, this setup reduces the
allograft function was normal in the entire cohort. In a ischemia-reperfusion injury and may thereby allow for
follow-up period of 8.5 mo, no evidence of intrahepatic the safe transplantation of marginal liver allografts.
biliary complications was noted. As a continuation to Normothermic mechanical perfusion can also allow
[13]
this study, authors Dutkowski et al recently published for the assessment of liver function during the pre-
WJG|www.wjgnet.com 4440 May 14, 2016|Volume 22|Issue 18|
Jadlowiec CC et al . Liver transplantation: Current status and challenges
[20]
implantation period (Table 1). Although these ad and higher ATP levels .
vantages are notable, historically, there have been
[15]
difficulties in maintaining stable perfusion . In a
[16]
preclinical work by op den Dries et al , discarded DCD IMPROVING LONG-TERM LIVER
human donor livers were subjected to normothermic TRANSPLANTATION OUTCOMES
mechanical perfusion following cold ischemia times
Although the short-term outcomes after liver trans
of 6.9 ± 1.9 h (WIT 15.5 ± 2.4 min). After six hours
plantation have been excellent worldwide, long-term
of normothermic perfusion (37 ℃ ), bile production
outcomes remain suboptimal. The top causes of late
was observed and histological examination showed
mortality after liver transplantation are allograft failure,
well-preserved liver morphology without signs of
cardiovascular events, infection, malignancy and renal
hepatocellular ischemia, biliary injury, or sinusoidal [21]
[16] failure . There is a clear and direct link between
damage . Currently, there are several human trials
these and the long-term use of immunosuppressive
underway comparing normothermic liver preservation
medications. As a result, in the past decade, a sig
with static cold storage. The first Phase I, non-
nificant effort has been put forth to minimize immuno
randomized, prospective trial using the normothermic
suppression in liver transplantation.
mechanical perfusion unit enrolled twenty transplanted
livers in United Kingdom and was completed in 2014.
Results from this trial demonstrated the safety and Renal sparing protocols
feasibility of normothermic machine preservation in Renal insufficiency is the strongest predictor of late
[21]
human liver allografts (personal communication). In mortality following liver transplantation . Because
the interim, a multicenter, randomized controlled trial of this, the use of renal sparing immunosuppression
with enrollment plan for 260 liver allografts (130 using protocols both during the induction and maintenance
©
OrganOx ; 130 using static cold storage) is under way. periods following liver transplantation has been
introduced into the clinical practice over the past
decade.
Steatotic liver allografts and mechanical perfusion
The application of mechanical perfusion to marginal
Mammalian target of rapamycin inhibitors: A
donors is foreseeable as hepatic steatosis has become
number of large trials evaluated the role of mammalian
increasingly common in the United States and the
target of rapamycin inhibitors (mTOR) in liver trans
incidence of deceased donors with steatotic livers
plantation. The Preservation of Renal Function in Liver
has concurrently increased. Allografts with severe
steatosis, defined as greater than sixty percent of the Transplant Recipients with Certican Therapy (PROTECT)
[22]
parenchyma, are known to carry a high risk of primary study , a randomized controlled trial sought to evaluate
non-function
[17,18]
. On the contrary, liver allografts with the effect of conversion from calcineurin inhibitors
mild steatosis (< 30%) yield results similar to those (CNI) to everolimus starting four weeks following liver
of non-steatotic liver allografts
[17,18]
. The outcomes of transplantation. Unfortunately, at one year, the study
liver allografts with moderate steatosis (30% to 60%) results proved to be inconclusive. No difference in
remain variable, and often depend upon additional glomerular filtration rater (GFR) was noted using the
factors such as recipient stability, ischemia time, and Cockcroft-Gault formula. Moreover, despite lack of clear
mechanism of donation (i.e., DBD vs DCD). Impaired benefit, the study did, however, observe a higher rate of
microcirculation secondary to increased hepatocyte infections, anemia, leukopenia and hyperlipidemia in the
[22]
volume is theorized to be responsible for the relative Everolimus treatment group .
[23]
[19]
susceptibility of steatotic livers to ischemia . Cellular By comparison, a second trial by Masetti et al in
edema accompanying ischemia-reperfusion likely 2010 showed some benefit in using mTOR inhibitors in
results in further obstruction of the sinusoids, thereby liver transplantation. In this randomized control trial,
exacerbating this injury. Accordingly, steatotic DCD cyclosporine (CsA) was used for ten days following
liver allografts are generally discarded as these liver transplantation. Patients were then randomized
scenarios combine several risk factors. As such, to Everolimus or cyclosporine plus mycophenolate
the application of mechanical perfusion may help mofetil (MMF). At twelve months, GFR was better
salvage steatotic livers. At present, preclinical and in the Everolimus group and no differences were
clinical studies are lacking however Bessems et al
[20]
noted in patient survival, acute rejection or hepatic
[23]
evaluated mechanical perfusion using a steatotic rat artery thrombosis . Among the patients with a GFR
2
model in which they compared static cold storage less than 60 mL/min per 1.73 m , the Everolimus
and hypothermic oxygenated mechanical perfusion. treatment group showed a benefit. Accordingly,
Results from this animal model found that preservation conclusions of the study were that early withdrawal
of steatotic livers stored in standard cold storage of CsA followed by Everolimus monotherapy in de
resulted in more cellular injury. By comparison, the novo liver transplant patients was associated with an
steatotic livers subjected to hypothermic oxygenated improvement in renal function, although, a criticism
mechanical perfusion showed improved bile production of the study has been the baseline difference between
WJG|www.wjgnet.com 4441 May 14, 2016|Volume 22|Issue 18|
Jadlowiec CC et al . Liver transplantation: Current status and challenges
the two groups with regard to the starting GFR. transplant recipients, 41 (40%) achieved operational
[24] [38]
In Spare-the-Nephron Trial , patients on CNI/ tolerance . At present, more information is needed
MMF for the first four weeks post-transplant were so as to better guide clinical decision making and
randomized to either continue the same regimen or similar trials with long-term follow-up will help
convert to Sirolimus/MMF. A mean increase in patient identify parameters with predictive and diagnostic
GFR was noted in the Sirolimus group, however the value regarding who could be successfully weaned
composite endpoint demonstrated non-inferiority of off IS. Longitudinal follow-up of operationally tolerant
[24]
Sirolimus to CNIs when used with MMF . Review of patients will also further demonstrate whether long-
other smaller studies evaluating the conversion from term outcomes improve with limiting the recipients’
CNI to mTOR inhibitors in liver transplant patients cumulative exposure to IS, particularly CNI.
with renal insufficiency reveals similar variable re
Chronic antibody-mediated injury
[25-28]
sults . A meta-analysis of the use of Sirolimus
in liver transplant recipients with CNI-induced renal Historically, liver allografts were thought to be spared
insufficiency found no significant improvement in from the HLA antibody-mediated injury, however
[29]
GFR, risk of death or graft failure . Findings were, recent findings have challenged this concept. The
however, significant for an increased risk of infection, Baylor group initially reported their observation in liver
[29]
mouth ulcers and treatment discontinuation . Given recipients with chronic rejection, who had circulating
this variability, the role of mTOR inhibitors continues to donor-specific HLA-antibody (DSA) more often than in
evolve with much indecision and hesitancy surrounding [39]
patients with no rejection . Subsequently, they found
their use for renal insufficiency. Newer roles, that multiple IgG subclasses were found in the sera
specifically with regard to benefit in hepatocellular of chronic rejection patients, and the IgG3 subclass
carcinoma, likewise remain to be fully realized. was associated with increased risk of graft loss .
[40]
A definitive cause-and-effect relationship remains
Induction therapy and delayed introduction to be demonstrated however, as these studies used
of calcineurin inhibitors: Delayed introduction of post-transplant DSA for analyses and did not include
CNI following liver transplantation may, theoretically, protocol biopsies. In our own observation at Mayo
help decrease the negative impact of CNI on renal Clinic, we did not find any DSA-mediated graft injury in
[30-33]
function . Among de novo liver transplant [41]
the first year after transplantation , and over the long
recipients who had pre-existing renal insufficiency, term, de novo DSA formation was preceded by liver
[42]
Thymoglobulin induction and delayed introduction allograft dysfunction (e.g., recurrent HCV cirrhosis) .
of CNI resulted in lower serum creatinine, a higher Based on these new observations, it appears
estimated GFR, and less dependence on dialysis that DSA may indeed cause chronic liver allograft
[30]
at twelve months . Similar strategies have been injury, although less frequently than in kidney or hear
employed using newer generation anti-interleukin- transplantation. In order to better understand the
2-receptor antibodies (Basiliximab, Daclizumab) for impact of DSA on both early and late outcomes in liver
[32,33]
induction . The ReSpECT trial, comparing standard transplantation, longitudinal prospective studies, similar
Tacrolimus vs reduced-dose Tacrolimus and Daclizumab to those done in kidney transplantation, correlating
[34]
induction and delayed reduced-dose Tacrolimus , DSA (both pre- and posttransplant at routine intervals)
demonstrated that the greatest decline in eGFR was with clinical outcomes and graft histology through
seen in the standard Tacrolimus group with the least protocol biopsies will need to be done. These studies
decline noted in the Daclizumab induction and delayed will ideally be designed to analyze DSA in detail, target
reduced-dose Tacrolimus group. Currently, at Mayo antigen expression in the allograft, and take into
Clinic, Basiliximab induction is used in patients with account immunosuppression and compliance issues
renal insufficiency so as to delay initiation of CNI post- in the recipients. In addition, histologic and genetic
transplant. evidence of endothelial cell injury and microvascular
inflammation (hallmark of DSA-mediated injury in
Immunosuppression minimization/withdrawal: kidney allografts) will need to be investigated in liver
[43-58]
Of all the solid organs that are transplanted routinely, transplant recipients with circulating DSA (Table 2) .
liver allograft appears to be unique, as approximately
19 percent of the recipients can achieve “operational”
tolerance (off immunosuppression incidentally or CONCLUSION
[35,36]
obligatorily) . Given these findings, several recent Along with the advances made in liver transplantation
trials investigated elective withdrawal of immunosup over the past thirty years have come a new set of
pression (IS) in liver transplant recipients. In one such challenges. As the demand for liver transplantation
trial, 12 out of 20 (60%) pediatric liver transplant continues to grow worldwide, more collaborative
recipients were successfully weaned off IS, with no or studies are needed to narrow the disparity between
[37]
minimal portal inflammation . In a large European the number of available deceased donor liver allografts
multi-center trial of 102 adult deceased donor liver and wait-listed patients, and to improve the long-term
WJG|www.wjgnet.com 4442 May 14, 2016|Volume 22|Issue 18|
Jadlowiec CC et al . Liver transplantation: Current status and challenges
Table 2 Current data for donor-specific HLA-antibody-associated injuries in kidney and liver transplantation
Kidney transplantation Liver transplantation
DSA specificity and levels ↑ risk hyperacute rejection[44]; ↑ DSA in new onset late ↑ DSA in recipients with CR, presence of IgG3 subclass
kidney allograft dysfunction[45]; acute AMR is associated associated with ↑ risk of graft loss[40]
with high posttransplant DSA levels[45]
C4d deposition in Graft failure significantly worse in the presence of C4d+ C4d+ staining nonspecific; In the presence of DSA, linear
microvasculature staining[44]; C4d+ is a marker of antibody-mediated portal capillary and sinusoidal staining observed in ACR;
injury[44,46] DSA negative C4d+ staining found in biliary strictures
and recurrent liver disease[47]
DSA subtypes, C1q binding ↓ graft survival and ↑ risk for AMR with C1q-binding Limited data[50]
DSA[48,49]
Microvascular inflammation Peritubular capillaritis is a possible predictor of chronic No current data
AMR[51]; subclinical AMR may contribute to development of
CAN[52]
EC activation by light EC and BM ultrastructural abnormalities in glomerular and No current data
microscopy peritubular capillaries are early markers of TXG[53]
Gene expression profile of Defined genetic profile in AMR[54,55] No current data
chronic AMR
Therapeutic-trials to prevent Bortezomib (plasma cell-targeted therapy) as a possible No current data
DSA-associated injury antihumoral therapy[56]; plasma exchange for AMR[57,58]
Modified from Ref. 43. AMR: Antibody-mediated rejection; CAN: Chronic allograft nephropathy; EC: Endothelial cell; BM: Basement membrane; DSA:
Donor-specific HLA-antibody; TXG: Transplant glomerulonephropathy.
outcomes of the liver recipients. 9 Guarrera JV, Estevez J, Boykin J, Boyce R, Rashid J, Sun S,
Arrington B. Hypothermic machine perfusion of liver grafts for
transplantation: technical development in human discard and
REFERENCES miniature swine models. Transplant Proc 2005; 37: 323-325 [PMID:
15808631 DOI: 10.1016/j.transproceed.2004.12.094]
1 Casavilla A, Ramirez C, Shapiro R, Nghiem D, Miracle K, 10 Henry SD, Nachber E, Tulipan J, Stone J, Bae C, Reznik L,
Bronsther O, Randhawa P, Broznick B, Fung JJ, Starzl T. Experience Kato T, Samstein B, Emond JC, Guarrera JV. Hypothermic
with liver and kidney allografts from non-heart-beating donors. machine preservation reduces molecular markers of ischemia/
Transplantation 1995; 59: 197-203 [PMID: 7839441 DOI: 10.1097/ reperfusion injury in human liver transplantation. Am J Transplant
00007890-199501000-00008] 2012; 12: 2477-2486 [PMID: 22594953 DOI: 10.1111/
2 Merion RM, Pelletier SJ, Goodrich N, Englesbe MJ, Delmonico FL. j.1600-6143.2012.04086.x]
Donation after cardiac death as a strategy to increase deceased donor 11 Guarrera JV, Henry SD, Samstein B, Reznik E, Musat C, Lukose
liver availability. Ann Surg 2006; 244: 555-562 [PMID: 16998364 TI, Ratner LE, Brown RS, Kato T, Emond JC. Hypothermic machine
DOI: 10.1097/01.sla.0000239006.33633.39] preservation facilitates successful transplantation of “orphan”
3 Lee DD, Singh A, Burns JM, Perry DK, Nguyen JH, Taner CB. extended criteria donor livers. Am J Transplant 2015; 15: 161-169
Early allograft dysfunction in liver transplantation with donation [PMID: 25521639 DOI: 10.1111/ajt.12958]
after cardiac death donors results in inferior survival. Liver Transpl 12 Dutkowski P, Schlegel A, de Oliveira M, Müllhaupt B, Neff F,
2014; 20: 1447-1453 [PMID: 25179581 DOI: 10.1002/lt.23985] Clavien PA. HOPE for human liver grafts obtained from donors after
4 Lee KW, Simpkins CE, Montgomery RA, Locke JE, Segev DL, cardiac death. J Hepatol 2014; 60: 765-772 [PMID: 24295869 DOI:
Maley WR. Factors affecting graft survival after liver transplantation 10.1016/j.jhep.2013.11.023]
from donation after cardiac death donors. Transplantation 13 Dutkowski P, Polak WG, Muiesan P, Schlegel A, Verhoeven CJ,
2006; 82: 1683-1688 [PMID: 17198260 DOI: 10.1097/01. Scalera I, DeOliveira ML, Kron P, Clavien PA. First Comparison
tp.0000250936.73034.98] of Hypothermic Oxygenated PErfusion Versus Static Cold Storage
5 Mateo R, Cho Y, Singh G, Stapfer M, Donovan J, Kahn J, Fong of Human Donation After Cardiac Death Liver Transplants:
TL, Sher L, Jabbour N, Aswad S, Selby RR, Genyk Y. Risk factors An International-matched Case Analysis. Ann Surg 2015; 262:
for graft survival after liver transplantation from donation after 764-770; discussion 770-771 [PMID: 26583664 DOI: 10.1097/
cardiac death donors: an analysis of OPTN/UNOS data. Am J SLA.0000000000001473]
Transplant 2006; 6: 791-796 [PMID: 16539637 DOI: 10.1111/ 14 Brockmann J, Reddy S, Coussios C, Pigott D, Guirriero D,
j.1600-6143.2006.01243.x] Hughes D, Morovat A, Roy D, Winter L, Friend PJ. Normothermic
6 Taner CB, Bulatao IG, Willingham DL, Perry DK, Sibulesky perfusion: a new paradigm for organ preservation. Ann Surg 2009;
L, Pungpapong S, Aranda-Michel J, Keaveny AP, Kramer DJ, 250: 1-6 [PMID: 19561463 DOI: 10.1097/SLA.0b013e3181a63c10]
Nguyen JH. Events in procurement as risk factors for ischemic 15 Neuhaus P, Blumhardt G. Extracorporeal liver perfusion:
cholangiopathy in liver transplantation using donation after cardiac applications of an improved model for experimental studies of the
death donors. Liver Transpl 2012; 18: 100-111 [PMID: 21837741 liver. Int J Artif Organs 1993; 16: 729-739 [PMID: 8125621]
DOI: 10.1002/lt.22404] 16 op den Dries S, Karimian N, Sutton ME, Westerkamp AC, Nijsten
7 Belzer FO, Ashby BS, Gulyassy PF, Powell M. Successful MW, Gouw AS, Wiersema-Buist J, Lisman T, Leuvenink HG, Porte
seventeen-hour preservation and transplantation of human-cadaver RJ. Ex vivo normothermic machine perfusion and viability testing of
kidney. N Engl J Med 1968; 278: 608-610 [PMID: 4866541 DOI: discarded human donor livers. Am J Transplant 2013; 13: 1327-1335
10.1056/NEJM196803142781108] [PMID: 23463950 DOI: 10.1111/ajt.12187]
8 Moers C, Pirenne J, Paul A, Ploeg RJ; Machine Preservation Trial 17 Selzner M, Clavien PA. Fatty liver in liver transplantation and
Study Group. Machine perfusion or cold storage in deceased-donor surgery. Semin Liver Dis 2001; 21: 105-113 [PMID: 11296690 DOI:
kidney transplantation. N Engl J Med 2012; 366: 770-771 [PMID: 10.1055/s-2001-12933]
22356343 DOI: 10.1056/NEJMc1111038] 18 D’Alessandro AM, Kalayoglu M, Sollinger HW, Hoffmann RM,
WJG|www.wjgnet.com 4443 May 14, 2016|Volume 22|Issue 18|
Jadlowiec CC et al . Liver transplantation: Current status and challenges
Reed A, Knechtle SJ, Pirsch JD, Hafez GR, Lorentzen D, Belzer Transpl 2008; 14: 66-72 [PMID: 18161842 DOI: 10.1002/lt.21309]
FO. The predictive value of donor liver biopsies for the development 31 Soliman T, Hetz H, Burghuber C, Györi G, Silberhumer G,
of primary nonfunction after orthotopic liver transplantation. Steininger R, Mühlbacher F, Berlakovich GA. Short-term versus
Transplantation 1991; 51: 157-163 [PMID: 1987685 DOI: 10.1097/ long-term induction therapy with antithymocyte globulin in
00007890-199101000-00024] orthotopic liver transplantation. Transpl Int 2007; 20: 447-452
19 Teramoto K, Bowers JL, Kruskal JB, Clouse ME. Hepatic [PMID: 17343686 DOI: 10.1111/j.1432-2277.2007.00463.x]
microcirculatory changes after reperfusion in fatty and normal liver 32 Asrani SK, Kim WR, Pedersen RA, Charlton MR, Kremers WK,
transplantation in the rat. Transplantation 1993; 56: 1076-1082 Therneau TM, Rosen CB, Dean PG. Daclizumab induction therapy
[PMID: 8249103 DOI: 10.1097/00007890-199311000-00005] in liver transplant recipients with renal insufficiency. Aliment
20 Bessems M, Doorschodt BM, Kolkert JL, Vetelainen RL, van Pharmacol Ther 2010; 32: 776-786 [PMID: 20659283 DOI:
Vliet AK, Vreeling H, van Marle J, van Gulik TM. Preservation of 10.1111/j.1365-2036.2010.04408.x]
steatotic livers: a comparison between cold storage and machine 33 Lin CC, Chuang FR, Lee CH, Wang CC, Chen YS, Liu YW, Jawan
perfusion preservation. Liver Transpl 2007; 13: 497-504 [PMID: B, Chen CL. The renal-sparing efficacy of basiliximab in adult living
17394146 DOI: 10.1002/lt.21039] donor liver transplantation. Liver Transpl 2005; 11: 1258-1264
21 Watt KD, Pedersen RA, Kremers WK, Heimbach JK, Charlton [PMID: 16184544 DOI: 10.1002/lt.20520]
MR. Evolution of causes and risk factors for mortality post-liver 34 Neuberger JM, Mamelok RD, Neuhaus P, Pirenne J, Samuel D,
transplant: results of the NIDDK long-term follow-up study. Am J Isoniemi H, Rostaing L, Rimola A, Marshall S, Mayer AD. Delayed
Transplant 2010; 10: 1420-1427 [PMID: 20486907 DOI: 10.1111/ introduction of reduced-dose tacrolimus, and renal function in liver
j.1600-6143.2010.03126.x] transplantation: the ‘ReSpECT’ study. Am J Transplant 2009; 9:
22 Fischer L, Klempnauer J, Beckebaum S, Metselaar HJ, Neuhaus 327-336 [PMID: 19120077 DOI: 10.1111/j.1600-6143.2008.02493.x]
P, Schemmer P, Settmacher U, Heyne N, Clavien PA, Muehlbacher 35 Mazariegos GV, Reyes J, Marino IR, Demetris AJ, Flynn B, Irish W,
F, Morard I, Wolters H, Vogel W, Becker T, Sterneck M, Lehner McMichael J, Fung JJ, Starzl TE. Weaning of immunosuppression in
F, Klein C, Kazemier G, Pascher A, Schmidt J, Rauchfuss F, liver transplant recipients. Transplantation 1997; 63: 243-249 [PMID:
Schnitzbauer A, Nadalin S, Hack M, Ladenburger S, Schlitt HJ. 9020325 DOI: 10.1097/00007890-199701270-00012]
A randomized, controlled study to assess the conversion from 36 Assy N, Adams PC, Myers P, Simon V, Minuk GY, Wall W, Ghent
calcineurin-inhibitors to everolimus after liver transplantation- CN. Randomized controlled trial of total immunosuppression
-PROTECT. Am J Transplant 2012; 12: 1855-1865 [PMID: withdrawal in liver transplant recipients: role of ursodeoxycholic
22494671 DOI: 10.1111/j.1600-6143.2012.04049.x] acid. Transplantation 2007; 83: 1571-1576 [PMID: 17589339 DOI:
23 Masetti M, Montalti R, Rompianesi G, Codeluppi M, Gerring R, 10.1097/01.tp.0000266678.32250.76]
Romano A, Begliomini B, Di Benedetto F, Gerunda GE. Early 37 Feng S, Ekong UD, Lobritto SJ, Demetris AJ, Roberts JP, Rosenthal
withdrawal of calcineurin inhibitors and everolimus monotherapy P, Alonso EM, Philogene MC, Ikle D, Poole KM, Bridges ND, Turka
in de novo liver transplant recipients preserves renal function. Am J LA, Tchao NK. Complete immunosuppression withdrawal and
Transplant 2010; 10: 2252-2262 [PMID: 20486905 DOI: 10.1111/ subsequent allograft function among pediatric recipients of parental
j.1600-6143.2010.03128.x] living donor liver transplants. JAMA 2012; 307: 283-293 [PMID:
24 Teperman L, Moonka D, Sebastian A, Sher L, Marotta P, Marsh 22253395 DOI: 10.1001/jama.2011.2014]
C, Koneru B, Goss J, Preston D, Roberts JP; Spare-the-Nephron 38 Benítez C, Londoño MC, Miquel R, Manzia TM, Abraldes JG,
Trial Liver Transplantation Study Group. Calcineurin inhibitor- Lozano JJ, Martínez-Llordella M, López M, Angelico R, Bohne F,
free mycophenolate mofetil/sirolimus maintenance in liver Sese P, Daoud F, Larcier P, Roelen DL, Claas F, Whitehouse G, Lerut
transplantation: the randomized spare-the-nephron trial. Liver J, Pirenne J, Rimola A, Tisone G, Sánchez-Fueyo A. Prospective
Transpl 2013; 19: 675-689 [PMID: 23775875 DOI: 10.1002/ multicenter clinical trial of immunosuppressive drug withdrawal
lt.23658] in stable adult liver transplant recipients. Hepatology 2013; 58:
25 Eisenberger U, Sollinger D, Stickel F, Burckhardt B, Frey FJ. 1824-1835 [PMID: 23532679 DOI: 10.1002/hep.26426]
Relationship between renal resistance index and renal function in 39 O’Leary JG, Kaneku H, Susskind BM, Jennings LW, Neri MA,
liver transplant recipients after cessation of calcineurin inhibitor. Davis GL, Klintmalm GB, Terasaki PI. High mean fluorescence
Clin Transplant 2009; 23: 499-504 [PMID: 19486346 DOI: 10.1111/ intensity donor-specific anti-HLA antibodies associated with chronic
j.1399-0012.2009.00986.x] rejection Postliver transplant. Am J Transplant 2011; 11: 1868-1876
26 Shenoy S, Hardinger KL, Crippin J, Desai N, Korenblat K, Lisker- [PMID: 21672151 DOI: 10.1111/j.1600-6143.2011.03593.x]
Melman M, Lowell JA, Chapman W. Sirolimus conversion in 40 Kaneku H, O’Leary JG, Taniguchi M, Susskind BM, Terasaki PI,
liver transplant recipients with renal dysfunction: a prospective, Klintmalm GB. Donor-specific human leukocyte antigen antibodies
randomized, single-center trial. Transplantation 2007; 83: 1389-1392 of the immunoglobulin G3 subclass are associated with chronic
[PMID: 17519792 DOI: 10.1097/01.tp.0000261630.63550.41] rejection and graft loss after liver transplantation. Liver Transpl
27 Watson CJ, Gimson AE, Alexander GJ, Allison ME, Gibbs P, Smith 2012; 18: 984-992 [PMID: 22508525 DOI: 10.1002/lt.23451]
JC, Palmer CR, Bradley JA. A randomized controlled trial of late 41 Taner T, Gandhi MJ, Sanderson SO, Poterucha CR, De Goey SR,
conversion from calcineurin inhibitor (CNI)-based to sirolimus- Stegall MD, Heimbach JK. Prevalence, course and impact of HLA
based immunosuppression in liver transplant recipients with donor-specific antibodies in liver transplantation in the first year. Am
impaired renal function. Liver Transpl 2007; 13: 1694-1702 [PMID: J Transplant 2012; 12: 1504-1510 [PMID: 22420671 DOI: 10.1111/
18044728 DOI: 10.1002/lt.21314] j.1600-6143.2012.03995.x]
28 DuBay D, Smith RJ, Qiu KG, Levy GA, Lilly L, Therapondos 42 Taner T, Heimbach JK, Rosen CB, Nyberg SL, Park WD, Stegall
G. Sirolimus in liver transplant recipients with renal dysfunction MD. Decreased chronic cellular and antibody-mediated injury in
offers no advantage over low-dose calcineurin inhibitor regimens. the kidney following simultaneous liver-kidney transplantation.
Liver Transpl 2008; 14: 651-659 [PMID: 18433069 DOI: 10.1002/ Kidney Int 2016; 89: 909-917 [PMID: 26924059 DOI: 10.1016/
lt.21429] j.kint.2015.10.016]
29 Asrani SK, Leise MD, West CP, Murad MH, Pedersen RA, Erwin 43 Taner T, Stegall MD, Heimbach JK. Antibody-mediated rejection
PJ, Tian J, Wiesner RH, Kim WR. Use of sirolimus in liver transplant in liver transplantation: current controversies and future directions.
recipients with renal insufficiency: a systematic review and meta- Liver Transpl 2014; 20: 514-527 [PMID: 24470340 DOI: 10.1002/
analysis. Hepatology 2010; 52: 1360-1370 [PMID: 20815021 DOI: lt.23826]
10.1002/hep.23835] 44 Patel R, Terasaki PI. Significance of the positive crossmatch test in
30 Bajjoka I, Hsaiky L, Brown K, Abouljoud M. Preserving renal kidney transplantation. N Engl J Med 1969; 280: 735-739 [PMID:
function in liver transplant recipients with rabbit anti-thymocyte 4886455]
globulin and delayed initiation of calcineurin inhibitors. Liver 45 Gaston RS, Cecka JM, Kasiske BL, Fieberg AM, Leduc R, Cosio
WJG|www.wjgnet.com 4444 May 14, 2016|Volume 22|Issue 18|
Jadlowiec CC et al . Liver transplantation: Current status and challenges
FC, Gourishankar S, Grande J, Halloran P, Hunsicker L, Mannon R, 52 Haas M, Montgomery RA, Segev DL, Rahman MH, Racusen LC,
Rush D, Matas AJ. Evidence for antibody-mediated injury as a major Bagnasco SM, Simpkins CE, Warren DS, Lepley D, Zachary AA,
determinant of late kidney allograft failure. Transplantation 2010; Kraus ES. Subclinical acute antibody-mediated rejection in positive
90: 68-74 [PMID: 20463643 DOI: 10.1097/TP.0b013e3181e065de] crossmatch renal allografts. Am J Transplant 2007; 7: 576-585
46 Burns JM, Cornell LD, Perry DK, Pollinger HS, Gloor JM, [PMID: 17229067 DOI: 10.1111/j.1600-6143.2006.01657.x]
Kremers WK, Gandhi MJ, Dean PG, Stegall MD. Alloantibody 53 Wavamunno MD, O’Connell PJ, Vitalone M, Fung CL, Allen
levels and acute humoral rejection early after positive crossmatch RD, Chapman JR, Nankivell BJ. Transplant glomerulopathy:
kidney transplantation. Am J Transplant 2008; 8: 2684-2694 [PMID: ultrastructural abnormalities occur early in longitudinal analysis
18976305 DOI: 10.1111/j.1600-6143.2008.02441.x] of protocol biopsies. Am J Transplant 2007; 7: 2757-2768 [PMID:
47 Ali S, Ormsby A, Shah V, Segovia MC, Kantz KL, Skorupski S, 17924997]
Eisenbrey AB, Mahan M, Huang MA. Significance of complement 54 Dean PG, Park WD, Cornell LD, Gloor JM, Stegall MD. Intragraft
split product C4d in ABO-compatible liver allograft: diagnosing gene expression in positive crossmatch kidney allografts: ongoing
utility in acute antibody mediated rejection. Transpl Immunol 2012; inflammation mediates chronic antibody-mediated injury. Am J
26: 62-69 [PMID: 21907804 DOI: 10.1016/j.trim.2011.08.005] Transplant 2012; 12: 1551-1563 [PMID: 22335458 DOI: 10.1111/
48 Loupy A, Lefaucheur C, Vernerey D, Prugger C, Duong van Huyen j.1600-6143.2011.03964.x]
JP, Mooney N, Suberbielle C, Frémeaux-Bacchi V, Méjean A, 55 Sis B, Jhangri GS, Riopel J, Chang J, de Freitas DG, Hidalgo L,
Desgrandchamps F, Anglicheau D, Nochy D, Charron D, Empana Mengel M, Matas A, Halloran PF. A new diagnostic algorithm
JP, Delahousse M, Legendre C, Glotz D, Hill GS, Zeevi A, Jouven for antibody-mediated microcirculation inflammation in kidney
X. Complement-binding anti-HLA antibodies and kidney-allograft transplants. Am J Transplant 2012; 12: 1168-1179 [PMID: 22300601
survival. N Engl J Med 2013; 369: 1215-1226 [PMID: 24066742 DOI: 10.1111/j.1600-6143.2011.03931.x]
DOI: 10.1056/NEJMoa1302506] 56 Everly MJ, Everly JJ, Susskind B, Brailey P, Arend LJ, Alloway
49 Yabu JM, Higgins JP, Chen G, Sequeira F, Busque S, Tyan DB. RR, Roy-Chaudhury P, Govil A, Mogilishetty G, Rike AH,
C1q-fixing human leukocyte antigen antibodies are specific for Cardi M, Wadih G, Tevar A, Woodle ES. Bortezomib provides
predicting transplant glomerulopathy and late graft failure after effective therapy for antibody- and cell-mediated acute rejection.
kidney transplantation. Transplantation 2011; 91: 342-347 [PMID: Transplantation 2008; 86: 1754-1761 [PMID: 19104417 DOI:
21116220 DOI: 10.1097/TP.0b013e318203fd26] 10.1097/TP.0b013e318190af83]
50 Del Bello A, Congy-Jolivet N, Danjoux M, Muscari F, Lavayssière 57 Bentall A, Tyan DB, Sequeira F, Everly MJ, Gandhi MJ, Cornell
L, Esposito L, Cardeau-Desangles I, Guitard J, Dörr G, Milongo D, LD, Li H, Henderson NA, Raghavaiah S, Winters JL, Dean PG,
Suc B, Duffas JP, Alric L, Bureau C, Guilbeau-Frugier C, Rostaing Stegall MD. Antibody-mediated rejection despite inhibition of
L, Kamar N. De novo donor-specific anti-HLA antibodies mediated terminal complement. Transpl Int 2014; 27: 1235-1243 [PMID:
rejection in liver-transplant patients. Transpl Int 2015; 28: 1371-1382 24990476 DOI: 10.1111/tri.12396]
[PMID: 26303035 DOI: 10.1111/tri.12654] 58 Stegall MD, Gloor J, Winters JL, Moore SB, Degoey S. A
51 Lerut E, Naesens M, Kuypers DR, Vanrenterghem Y, Van Damme comparison of plasmapheresis versus high-dose IVIG desensitization
B. Subclinical peritubular capillaritis at 3 months is associated with in renal allograft recipients with high levels of donor specific
chronic rejection at 1 year. Transplantation 2007; 83: 1416-1422 alloantibody. Am J Transplant 2006; 6: 346-351 [PMID: 16426319
[PMID: 17565313 DOI: 10.1097/01.tp.0000266676.10550.70] DOI: 10.1111/j.1600-6143.2005.01178.x]
P- Reviewer: Bramhall S, Liu QD, Makisalo H S- Editor: Gong ZM
L- Editor: A E- Editor: Wang CH
WJG|www.wjgnet.com 4445 May 14, 2016|Volume 22|Issue 18|
Published by Baishideng Publishing Group Inc
8226 Regency Drive, Pleasanton, CA 94588, USA
Telephone: +1-925-223-8242
Fax: +1-925-223-8243
E-mail: bpgoffice@wjgnet.com
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx
http://www.wjgnet.com
I S S N 1 0 0 7 - 9 3 2 7
18
9 7 7 10 0 7 9 3 2 0 45
© 2016 Baishideng Publishing Group Inc. All rights reserved.
You might also like
- Kitchenbrigade 120821195157 Phpapp02Document25 pagesKitchenbrigade 120821195157 Phpapp02Conrado AreolaNo ratings yet
- Strategic Plan-4Document9 pagesStrategic Plan-4Bryan VillarezNo ratings yet
- Massive Transfusion - An Update For The Anesthesiologist 2017Document9 pagesMassive Transfusion - An Update For The Anesthesiologist 2017JOSENo ratings yet
- Meta 6 - Khizar - 2023Document11 pagesMeta 6 - Khizar - 2023matheus.verasNo ratings yet
- Efek HDDocument10 pagesEfek HDAdi SuciptoNo ratings yet
- JCM 12 06173Document20 pagesJCM 12 06173Taulant MukaNo ratings yet
- WarshawDocument11 pagesWarshawJuan RamirezNo ratings yet
- Nair Et Al. 2016 - Frequent Home Haemodialysis, A Review of The EvidenceDocument8 pagesNair Et Al. 2016 - Frequent Home Haemodialysis, A Review of The EvidenceShareDialysisNo ratings yet
- Conrad Et Al-2017-Journal of Hepato-Biliary-Pancreatic SciencesDocument14 pagesConrad Et Al-2017-Journal of Hepato-Biliary-Pancreatic SciencesAndra CiocanNo ratings yet
- Hepatic Steatosis and Fibrosis Non-Invasive AssessDocument19 pagesHepatic Steatosis and Fibrosis Non-Invasive Assessehsanulazim50buetNo ratings yet
- Biomedicines 10 01013Document15 pagesBiomedicines 10 01013Anshika yadavNo ratings yet
- HDX by Ronco 2017Document8 pagesHDX by Ronco 2017lizzaNo ratings yet
- Protective Mechanisms and Current Clinical EvidencDocument18 pagesProtective Mechanisms and Current Clinical EvidencCláudia SilvaNo ratings yet
- WJGS 8 376Document7 pagesWJGS 8 376Inamullah FurqanNo ratings yet
- PIIS1053077023003403Document12 pagesPIIS1053077023003403lxluizNo ratings yet
- Breakthroughs in Hepatology JhepatDocument2 pagesBreakthroughs in Hepatology JhepatCláudia SilvaNo ratings yet
- Clinical Transplantation - 2022 - Alconchel - Are Short Term Complications Associated With Poor Allograft and PatientDocument14 pagesClinical Transplantation - 2022 - Alconchel - Are Short Term Complications Associated With Poor Allograft and PatientlucianapcariusNo ratings yet
- Neoadjuvant Chemotherapy Vs Upfront Surgery For Gastric Signet Ring Cell Carcinoma A Retrospective, Propensity Score-Matched StudyDocument11 pagesNeoadjuvant Chemotherapy Vs Upfront Surgery For Gastric Signet Ring Cell Carcinoma A Retrospective, Propensity Score-Matched StudyLITTLESWEETKILLERNo ratings yet
- Clinicopathological Study of Varicose Veins (Descriptive Study)Document10 pagesClinicopathological Study of Varicose Veins (Descriptive Study)Vlad DraculaNo ratings yet
- DOACs in Cirrhotic Patients With Portal Vein Thrombosis - The EvidenceDocument15 pagesDOACs in Cirrhotic Patients With Portal Vein Thrombosis - The EvidencelabertoNo ratings yet
- Joacp 35 29Document6 pagesJoacp 35 29kenjiNo ratings yet
- Hemodialysis Internal Jugular Vein Versus Subclavian Vein Catheters: Complications, Patients' Comfort, Tolerance and Cost-EffectivenessDocument5 pagesHemodialysis Internal Jugular Vein Versus Subclavian Vein Catheters: Complications, Patients' Comfort, Tolerance and Cost-EffectivenessYolanda IrawatiNo ratings yet
- AnemiaDocument7 pagesAnemiaAttilio Del RossoNo ratings yet
- Changing Trends in Liver Transplantation .14Document14 pagesChanging Trends in Liver Transplantation .14Pablo Henrique Alves TelesNo ratings yet
- 2016 - Long-Term Donor Outcomes After Pure Laparoscopic Versus Open Living Donor NephrectomyDocument7 pages2016 - Long-Term Donor Outcomes After Pure Laparoscopic Versus Open Living Donor Nephrectomynarutota181No ratings yet
- A Review of Liver Transplantation For The Dentist and Guidelines For Dental ManagementDocument7 pagesA Review of Liver Transplantation For The Dentist and Guidelines For Dental ManagementLujainNo ratings yet
- Revisiting Donor Risk Over Two Decades of Single-Center Experience: More Attention On The Impact of OverweightDocument8 pagesRevisiting Donor Risk Over Two Decades of Single-Center Experience: More Attention On The Impact of Overweightyerich septaNo ratings yet
- Clinical Efficacy of Enhanced Recovery After Surgery in Percutaneous Nephrolithotripsy: A Randomized Controlled TrialDocument8 pagesClinical Efficacy of Enhanced Recovery After Surgery in Percutaneous Nephrolithotripsy: A Randomized Controlled TrialfaundraNo ratings yet
- Timing of Initiation of Renal-ReplacementDocument12 pagesTiming of Initiation of Renal-Replacementchamwick4567No ratings yet
- Pi is 0085253820309054Document11 pagesPi is 0085253820309054Chavalit ChotruangnapaNo ratings yet
- World Journal of Gastroenterology, Hepatology and Endoscopy: Article InformationDocument4 pagesWorld Journal of Gastroenterology, Hepatology and Endoscopy: Article Informationscience world publishingNo ratings yet
- MKW 070Document6 pagesMKW 070Dashhh RamirezNo ratings yet
- Wjgo 14 1199Document12 pagesWjgo 14 1199juan uribeNo ratings yet
- Resuscitation Fluid Composition in Acute Kidney Injury in Critical IllnessDocument2 pagesResuscitation Fluid Composition in Acute Kidney Injury in Critical IllnessDe Frede EditoreNo ratings yet
- Posthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)Document12 pagesPosthepatectomy Liver Failure: A Definition and Grading by The International Study Group of Liver Surgery (ISGLS)drsubramanianNo ratings yet
- s43678 021 00126 7Document5 pagess43678 021 00126 7Hugo EspinozaNo ratings yet
- Thesis On Chronic Kidney DiseaseDocument5 pagesThesis On Chronic Kidney Diseasebrendahigginsarlington100% (2)
- 10 Carcinomatoza PeritonealaDocument9 pages10 Carcinomatoza PeritonealaGabriela MilitaruNo ratings yet
- Acute Allograft Rejection in Liver Transplant Recipients: Incidence, Risk Factors, Treatment Success, and Impact On Graft FailureDocument12 pagesAcute Allograft Rejection in Liver Transplant Recipients: Incidence, Risk Factors, Treatment Success, and Impact On Graft Failurenathalialusman98No ratings yet
- DRC Kdigo CanadenseDocument29 pagesDRC Kdigo CanadensePaulo RigaudNo ratings yet
- Recommendations For The Use of Tolvaptan in AutosoDocument13 pagesRecommendations For The Use of Tolvaptan in AutosoBeth EnriquezNo ratings yet
- BaliJAnaesthesiol5126-1251569 032835Document7 pagesBaliJAnaesthesiol5126-1251569 032835Yunita Kristiana DewiNo ratings yet
- 1 s2.0 S105122762300105X MainDocument11 pages1 s2.0 S105122762300105X MainJulia KhaerunisaNo ratings yet
- Locoregional Treatments Obsolete For Patients With Cancer With Liver MetastasesDocument18 pagesLocoregional Treatments Obsolete For Patients With Cancer With Liver MetastasesDR. SUMANTRA RAYNo ratings yet
- Cancer Res-2011-Kawada-0008-5472.CAN-10-3277Document16 pagesCancer Res-2011-Kawada-0008-5472.CAN-10-3277Nolie Lovarya HarukaNo ratings yet
- Donor Management and Organ Preservation Transplant - International 2016 974-984Document11 pagesDonor Management and Organ Preservation Transplant - International 2016 974-984Marisol Gallego DuqueNo ratings yet
- 10.1007@s11897 019 00432 3Document7 pages10.1007@s11897 019 00432 3diogofc123No ratings yet
- New England Journal Medicine: The ofDocument14 pagesNew England Journal Medicine: The ofFajar PramaduNo ratings yet
- Fluid Management During Kidney TransplantationDocument8 pagesFluid Management During Kidney Transplantationgiancarlor368No ratings yet
- Radiology & Medical ImagingDocument6 pagesRadiology & Medical ImagingRizka Ramadhani AbrarNo ratings yet
- KDIGO Onconeph PT 1 Kidney Impairment and Solid Organ CancerDocument12 pagesKDIGO Onconeph PT 1 Kidney Impairment and Solid Organ CancerMaría MartínezNo ratings yet
- Criteria For Continuous Kidney Replacement Therapy Cessation in ICU PatientsDocument9 pagesCriteria For Continuous Kidney Replacement Therapy Cessation in ICU PatientszeravoneNo ratings yet
- Application of Various Surgical Techniques in Liver TransplantDocument12 pagesApplication of Various Surgical Techniques in Liver TransplantPaula AlmeidaNo ratings yet
- Uncontrolled Donation After Circulatory Death CompDocument9 pagesUncontrolled Donation After Circulatory Death CompKaffal TwoNo ratings yet
- Surgery of The Liver Pancreas and Biliary Tract (Dragged) 79Document17 pagesSurgery of The Liver Pancreas and Biliary Tract (Dragged) 79Nguyen Hai NamNo ratings yet
- Fish OilDocument18 pagesFish OilninukNo ratings yet
- ACO Peripro 2016Document10 pagesACO Peripro 2016Philippe Bocanegra FernándezNo ratings yet
- Surgery: SciencedirectDocument6 pagesSurgery: SciencedirectabrarkhanmdcmNo ratings yet
- Renal Cell Carcinoma A Case Series With Integrative Treatment 2329 6771 S1 002Document5 pagesRenal Cell Carcinoma A Case Series With Integrative Treatment 2329 6771 S1 002VanroNo ratings yet
- Hagedorn 2019Document10 pagesHagedorn 2019Cinthya Añazco RomeroNo ratings yet
- Long-Term Outcomes of Hepatitis B Virus-Related Cirrhosis Treated With Nucleos (T) Ide AnalogsDocument10 pagesLong-Term Outcomes of Hepatitis B Virus-Related Cirrhosis Treated With Nucleos (T) Ide AnalogsZulfiana NabilaNo ratings yet
- Critical Care for Potential Liver Transplant CandidatesFrom EverandCritical Care for Potential Liver Transplant CandidatesDmitri BezinoverNo ratings yet
- Sword and Sorcery 5eDocument5 pagesSword and Sorcery 5eConstantine PaleologusNo ratings yet
- Waterfront Boundaries For Grants of Public Crown Lands - MNR - E000074 - 2001Document3 pagesWaterfront Boundaries For Grants of Public Crown Lands - MNR - E000074 - 2001Sen HuNo ratings yet
- IBA Gas Field QuestionsDocument19 pagesIBA Gas Field Questionssazzadmunna5950% (1)
- Undergraduate Scholarships Application FormDocument3 pagesUndergraduate Scholarships Application FormAbdul Rehman ShejwalkarNo ratings yet
- Primemotiontraining Beeptest GuideDocument6 pagesPrimemotiontraining Beeptest GuideCristian NechitaNo ratings yet
- MIP 2021 (Budget Proposal)Document215 pagesMIP 2021 (Budget Proposal)Yanny ManggugubatNo ratings yet
- A Study of Factors Affecting Travel Decision Making of TouristsDocument10 pagesA Study of Factors Affecting Travel Decision Making of TouristsAmmarah Rajput ParhiarNo ratings yet
- Instruments NotesDocument116 pagesInstruments Notesprithvih4No ratings yet
- MPKDocument15 pagesMPKghaliyahalmiraNo ratings yet
- Metropolis 3 EdgesDocument12 pagesMetropolis 3 Edgesapi-264020285No ratings yet
- $ROW9KSXDocument18 pages$ROW9KSXRoberto SangregorioNo ratings yet
- Unit 1 - Introduction & Number Theory: Dr.S.Kalaivani Assistant Professor/ Dept. of CSE IrttDocument87 pagesUnit 1 - Introduction & Number Theory: Dr.S.Kalaivani Assistant Professor/ Dept. of CSE IrttRishikaa RamNo ratings yet
- Bahasa Inggris Kelas 5Document2 pagesBahasa Inggris Kelas 5Bimbeldec Depok100% (1)
- Test Bank For e Commerce 2019 Business Technology and Society 15th by LaudonDocument21 pagesTest Bank For e Commerce 2019 Business Technology and Society 15th by LaudonCecil Johnson100% (42)
- Fly & Drive Albania-UpdatedDocument5 pagesFly & Drive Albania-UpdatedBarbara CsécseiNo ratings yet
- OTC Asia 2024 Conference PreviewDocument20 pagesOTC Asia 2024 Conference PreviewAmmirul AzmanNo ratings yet
- Chapter 1 - History of NeuropsychologyDocument29 pagesChapter 1 - History of Neuropsychologymacue96No ratings yet
- Lloyd P. Gerson, PlotinusDocument9 pagesLloyd P. Gerson, PlotinusPrendasNo ratings yet
- NTPC Ge Power Services PVT LTD: Liquid Penetrant Examination ReportDocument2 pagesNTPC Ge Power Services PVT LTD: Liquid Penetrant Examination ReportBalkishan DyavanapellyNo ratings yet
- Mastermind 2 Unit 1 Grammar and Vocabulary Test ADocument7 pagesMastermind 2 Unit 1 Grammar and Vocabulary Test ARolando Guzman Martinez100% (1)
- Dissertation Binding DallasDocument8 pagesDissertation Binding DallasINeedSomeoneToWriteMyPaperOlathe100% (1)
- Chap002 2019 Fall Assignment 2Document6 pagesChap002 2019 Fall Assignment 2Taranom BakhtiaryNo ratings yet
- Teklehaimanot Abreham Job Application Letter: To: Heineken Breweries Share Company Dear Recruitment Manager!Document2 pagesTeklehaimanot Abreham Job Application Letter: To: Heineken Breweries Share Company Dear Recruitment Manager!Curios cornerNo ratings yet
- BABOK - Techniques by KADocument1 pageBABOK - Techniques by KABenhar Masahod BLM-VLOGNo ratings yet
- South Dakota State Treasurer Unclaimed Property: Claim FormDocument2 pagesSouth Dakota State Treasurer Unclaimed Property: Claim FormMiguel Paz100% (1)
- Survey of Philippine Literature in English: Shepherdville CollegeDocument9 pagesSurvey of Philippine Literature in English: Shepherdville CollegeMary Rose GuerreroNo ratings yet
- Conservative Management of Talon's Cusp-A Case ReportDocument22 pagesConservative Management of Talon's Cusp-A Case ReportHarees Shabir100% (1)
- Capital and RevenueDocument20 pagesCapital and RevenueDr Sarbesh Mishra100% (1)