Professional Documents
Culture Documents
Community Acquired Methicillin Resistant em Staph
Community Acquired Methicillin Resistant em Staph
Uploaded by
Brea WilleyCopyright:
Available Formats
You might also like
- Chapter 29 - Test: (60 Minutes)Document3 pagesChapter 29 - Test: (60 Minutes)Minh ThanhNo ratings yet
- UOP 304-08 Bromine Number and Bromine Index of Hydrocarbons by Potentiometric TitrationDocument13 pagesUOP 304-08 Bromine Number and Bromine Index of Hydrocarbons by Potentiometric TitrationMorteza SepehranNo ratings yet
- Anti Biotik 2015Document22 pagesAnti Biotik 2015cut herlindaNo ratings yet
- 3 - Acute InfectionsDocument44 pages3 - Acute InfectionsAlexa GabrielaNo ratings yet
- Risk Factors For Surgical Site InfectionDocument5 pagesRisk Factors For Surgical Site InfectionElizabeth Mautino CaceresNo ratings yet
- Bacterial and Fungal Contamination of Dental Hygienists' Hands With and Without Finger RingsDocument5 pagesBacterial and Fungal Contamination of Dental Hygienists' Hands With and Without Finger RingsAsniza AbasNo ratings yet
- Articulo Evaluacion Final Antimicrobianos 1 2020Document9 pagesArticulo Evaluacion Final Antimicrobianos 1 2020Juan BojacaNo ratings yet
- A Study of Skin Infection - How To Diagnosis and Its TherapyDocument7 pagesA Study of Skin Infection - How To Diagnosis and Its TherapyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Skin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus AureusDocument11 pagesSkin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus AureusFerdy RamadhanNo ratings yet
- The Health Professional's Role in Preventing Nosocomial InfectionsDocument5 pagesThe Health Professional's Role in Preventing Nosocomial InfectionsAbdo MohamedNo ratings yet
- Hand Osteomyelitis HudaDocument34 pagesHand Osteomyelitis HudaOrtho songoNo ratings yet
- Microbial Species Isolated From Infected Wounds and Antimicrobial Resistance Analysis: Data Emerging From A Three-Years Retrospective StudyDocument14 pagesMicrobial Species Isolated From Infected Wounds and Antimicrobial Resistance Analysis: Data Emerging From A Three-Years Retrospective StudyFawwaziNo ratings yet
- Free Research Papers On MrsaDocument8 pagesFree Research Papers On Mrsaafnhbijlzdufjj100% (1)
- Epidemiologia de Lesiones de Punta de Dedo en Hospital de PEMEXDocument14 pagesEpidemiologia de Lesiones de Punta de Dedo en Hospital de PEMEXOscar Cayetano Herrera RodríguezNo ratings yet
- Mrsa101 508Document45 pagesMrsa101 508Sam TullyNo ratings yet
- Sepsis in Trauma: A Deadly Complication: Fernanda Mas-Celis, Jimena Olea-López, and Javier Alberto Parroquin-MaldonadoDocument9 pagesSepsis in Trauma: A Deadly Complication: Fernanda Mas-Celis, Jimena Olea-López, and Javier Alberto Parroquin-MaldonadoMelissa JosephNo ratings yet
- 19.2 Antimicrobial Management of Complicated Skin and Soft Tissue KONAS PETRI BALI 2023-1Document34 pages19.2 Antimicrobial Management of Complicated Skin and Soft Tissue KONAS PETRI BALI 2023-1Eva RoswatiNo ratings yet
- Skin and Soft Tissue InfectionsDocument8 pagesSkin and Soft Tissue InfectionsciaranNo ratings yet
- MrsaDocument63 pagesMrsaRAHULNo ratings yet
- Life 13 01126Document14 pagesLife 13 01126s4cdbv4xjrNo ratings yet
- Disease ReportDocument2 pagesDisease Reportapi-511364141No ratings yet
- Empiric Antibiotics For Acute Infections of The HaDocument4 pagesEmpiric Antibiotics For Acute Infections of The HaBrea WilleyNo ratings yet
- Current Pathogens Infecting Open Fracture Tibia and Their Antibiotic Susceptibility at A Tertiary Care Teaching Hospital in South East AsiaDocument10 pagesCurrent Pathogens Infecting Open Fracture Tibia and Their Antibiotic Susceptibility at A Tertiary Care Teaching Hospital in South East AsiaFrancis RomanosNo ratings yet
- Chapter Two Literature ReviewDocument11 pagesChapter Two Literature ReviewKojo Adu100% (1)
- Surgical Site Infections: Epidemiology, Microbiology and PreventionDocument8 pagesSurgical Site Infections: Epidemiology, Microbiology and Preventionm8wyb2f6ngNo ratings yet
- SSI Webinar Series 1 PABIDocument18 pagesSSI Webinar Series 1 PABISafira Wahyu NurhardiyantiNo ratings yet
- Methicillin Resistant Staphylococcus Aureus: (MRSA)Document13 pagesMethicillin Resistant Staphylococcus Aureus: (MRSA)Adnan JourdanNo ratings yet
- Rab 9Document12 pagesRab 9Belia DestamaNo ratings yet
- Health NexusDocument3 pagesHealth NexusanupamaniroopNo ratings yet
- Wounds 313-323 PDFDocument12 pagesWounds 313-323 PDFTrong HieuNo ratings yet
- Missirlis, Katsikogianni, Missirlis. 2004. CONCISE REVIEW OF MECHANISMS OF BACTERIAL ADHESION TO BIOMATERIALS AND OF TECHNIQUES USED INDocument21 pagesMissirlis, Katsikogianni, Missirlis. 2004. CONCISE REVIEW OF MECHANISMS OF BACTERIAL ADHESION TO BIOMATERIALS AND OF TECHNIQUES USED INAzb 711No ratings yet
- Bone Graft SubstitutesDocument5 pagesBone Graft SubstitutessarraNo ratings yet
- Bali 2011Document4 pagesBali 2011ashkisaragiNo ratings yet
- Antibiotic Resistance in Malaysia and Its Public HDocument8 pagesAntibiotic Resistance in Malaysia and Its Public HNora LeeNo ratings yet
- MrsaDocument10 pagesMrsazia ul RahmanNo ratings yet
- Smart Central Venous Port For Early Detection of Bacterial Biofilm Related InfectionsDocument10 pagesSmart Central Venous Port For Early Detection of Bacterial Biofilm Related InfectionsGeneration GenerationNo ratings yet
- MRSA Case ReportDocument3 pagesMRSA Case ReportDr P.R. RaghavanNo ratings yet
- Luka 2 PDFDocument6 pagesLuka 2 PDFBarryNo ratings yet
- AAJIC Journal of QAC For SARS COV2Document2 pagesAAJIC Journal of QAC For SARS COV2ayuwinaNo ratings yet
- Field Wound Care: Prophylactic AntibioticsDocument13 pagesField Wound Care: Prophylactic AntibioticsAgstri Lestari PutriNo ratings yet
- Pepsi@u.washington - Edu: JA A DDocument1 pagePepsi@u.washington - Edu: JA A Disra navaNo ratings yet
- agm.j-3288.75-fDocument15 pagesagm.j-3288.75-fChandravadhana NarayananNo ratings yet
- 2022 Article 1123Document10 pages2022 Article 1123Achmad NurNo ratings yet
- Prevention of HAI IndonesienDocument208 pagesPrevention of HAI IndonesienLipun SethiNo ratings yet
- Are You and Your Patients in Safe HandsDocument8 pagesAre You and Your Patients in Safe Handsanis merahNo ratings yet
- Balancing Infection Control and Environmental.42Document4 pagesBalancing Infection Control and Environmental.42Alice MozerNo ratings yet
- Characteristics of Microbial Drug Resistance and Its Correlates in Chronic Diabetic Foot Ulcer InfectionsDocument9 pagesCharacteristics of Microbial Drug Resistance and Its Correlates in Chronic Diabetic Foot Ulcer InfectionsPutri Alif PermatasariNo ratings yet
- OM Stafilococo (Clase Observacionales)Document7 pagesOM Stafilococo (Clase Observacionales)Jairo Camilo Guevara FaríasNo ratings yet
- Occupational Hazards in DentistryDocument4 pagesOccupational Hazards in DentistrymonikaNo ratings yet
- 2021 Surgical Site Infection After Liver Transplantation in The Era of MultidrugDocument7 pages2021 Surgical Site Infection After Liver Transplantation in The Era of MultidrugInaldoNo ratings yet
- Capstone Apa Honors Prof 2Document7 pagesCapstone Apa Honors Prof 2api-543808198No ratings yet
- Wounds, Antimicrobial Resistance and Challenges of Implementing A Surveillance System in Myanmar: A Mixed-Methods StudyDocument15 pagesWounds, Antimicrobial Resistance and Challenges of Implementing A Surveillance System in Myanmar: A Mixed-Methods StudyKarina Dwi SwastikaNo ratings yet
- 1 - Name of The Candidate and AddressDocument19 pages1 - Name of The Candidate and AddressRini ThomasNo ratings yet
- Medi 97 E11097Document4 pagesMedi 97 E11097Lia FikayuniarNo ratings yet
- Necrotising Soft-Tissue InfectionsDocument14 pagesNecrotising Soft-Tissue Infectionssergio salazarNo ratings yet
- Current Concepts On The Virulence Mechanisms of Meticillin-Resistant Staphylococcus AureusDocument15 pagesCurrent Concepts On The Virulence Mechanisms of Meticillin-Resistant Staphylococcus AureusSeptiani HasibuanNo ratings yet
- Infection ControlDocument24 pagesInfection Controlsteffy christNo ratings yet
- Supra SobDocument34 pagesSupra SobZakaria NersNo ratings yet
- Promoting Asepsis and Infection Control: Teresa V. Hurley, MSN, RNDocument53 pagesPromoting Asepsis and Infection Control: Teresa V. Hurley, MSN, RNRoan DAlleNo ratings yet
- Such Ard 2011Document9 pagesSuch Ard 2011Jose MenesesNo ratings yet
- Resetting Healthcare Post-COVID-19 Pandemic: The Patient HandbookFrom EverandResetting Healthcare Post-COVID-19 Pandemic: The Patient HandbookNo ratings yet
- Viral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensFrom EverandViral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensNo ratings yet
- A High Proportion of Beta-Tocopherol In. 2019Document5 pagesA High Proportion of Beta-Tocopherol In. 2019Miguel Antonio CaicedoNo ratings yet
- Coalmine Monitoring SystemDocument65 pagesCoalmine Monitoring SystemTechnos_IncNo ratings yet
- Report On Reuse of Abandoned Quarries and Mine Pits in KeralaDocument90 pagesReport On Reuse of Abandoned Quarries and Mine Pits in KeralaDrThrivikramji Kyth100% (10)
- Button LoadcellDocument3 pagesButton LoadcellkshripNo ratings yet
- Datasheet Painel Solar 360W KuMax CS3U PDocument2 pagesDatasheet Painel Solar 360W KuMax CS3U PDenis SilvaNo ratings yet
- Integrity Management of Safety Critical Equipment and SystemsDocument10 pagesIntegrity Management of Safety Critical Equipment and SystemsLi QiNo ratings yet
- 04 - Rotational Motion - JEE PDFDocument124 pages04 - Rotational Motion - JEE PDFCefas Almeida50% (2)
- Projet de Partenariat Senegal Mat-Groupe Caparol Version AnglaiseDocument7 pagesProjet de Partenariat Senegal Mat-Groupe Caparol Version AnglaiseTaga DiopNo ratings yet
- Jobm 201800252Document14 pagesJobm 201800252leilany casillasNo ratings yet
- Contoh Soal Koordinasi Relay Ocr PDFDocument2 pagesContoh Soal Koordinasi Relay Ocr PDFEdi CarnediNo ratings yet
- Datasheet DiacDocument4 pagesDatasheet DiacOrlandoTobonNo ratings yet
- 7 TH Biology Worksheets Ls 8 Weather, Climate Animal AdaptationsDocument7 pages7 TH Biology Worksheets Ls 8 Weather, Climate Animal AdaptationsAysha Muhammad ShahzadNo ratings yet
- 50 Milisimal PotencyDocument8 pages50 Milisimal PotencyDr. Surendra Singh100% (3)
- Catalogue V2 - 2012 Final (Full Copy)Document132 pagesCatalogue V2 - 2012 Final (Full Copy)Richard PayneNo ratings yet
- TF65-67 Thermal Overload Relay: Product-DetailsDocument5 pagesTF65-67 Thermal Overload Relay: Product-DetailsSergio PartidaNo ratings yet
- Castrol 0w-30 German CastrolDocument2 pagesCastrol 0w-30 German CastrolTudor RatiuNo ratings yet
- Cloze Passage For SMP Kls 3Document7 pagesCloze Passage For SMP Kls 3DibaPertiwiNo ratings yet
- What Causes HallucinationsDocument2 pagesWhat Causes Hallucinationslook at meNo ratings yet
- Octamar LI 5 PDSDocument2 pagesOctamar LI 5 PDSfransleo.applicationNo ratings yet
- Manual Board 945GCT-M (2.0A)Document48 pagesManual Board 945GCT-M (2.0A)BalrogJoelNo ratings yet
- NIOEC-SP-00-72 (1) : Process Design of Hot Oil & Tempered Water CircuitsDocument28 pagesNIOEC-SP-00-72 (1) : Process Design of Hot Oil & Tempered Water CircuitsMohammad AminiNo ratings yet
- Wastage of Food in Indian WeddingsDocument9 pagesWastage of Food in Indian WeddingsThe United IndianNo ratings yet
- Week 4 - Stadelman-Cohen & Hillman (2014)Document22 pagesWeek 4 - Stadelman-Cohen & Hillman (2014)kehanNo ratings yet
- Girder - Arrangement 04 08 2023Document9 pagesGirder - Arrangement 04 08 2023sanyogitasawant5No ratings yet
- Soal USP BIG LMDocument56 pagesSoal USP BIG LMMoh. Aska FailandriNo ratings yet
- An Immunology-Inspired Network Security Architecture 2020Document12 pagesAn Immunology-Inspired Network Security Architecture 2020rgtreadsNo ratings yet
- CT-Demag Flyer InstrumentDocument2 pagesCT-Demag Flyer InstrumentKarthik SriramakavachamNo ratings yet
- The Evolution of Water Reverse Osmosis TechnologyDocument35 pagesThe Evolution of Water Reverse Osmosis TechnologyQassim LaouiraNo ratings yet
Community Acquired Methicillin Resistant em Staph
Community Acquired Methicillin Resistant em Staph
Uploaded by
Brea WilleyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Community Acquired Methicillin Resistant em Staph
Community Acquired Methicillin Resistant em Staph
Uploaded by
Brea WilleyCopyright:
Available Formats
SCIENTIFIC ARTICLE
Community-Acquired Methicillin-Resistant
Staphylococcus aureus in Surgically Treated
Hand Infections
Scott D. Imahara, MD, Jeffrey B. Friedrich, MD
Purpose An increase in the incidence of community-acquired methicillin-resistant Staphylo-
coccus aureus (CA-MRSA) infections has been observed. The purpose of this study is to
determine the change in proportion of surgically treated CA-MRSA hand infections over the
last decade and to identify associated risk factors.
Methods A retrospective review was performed of all 159 hand infections treated in the
operating room over an 11-year period (1997–2007). Mean age overall was 40 years, mean
inpatient length of stay was 4.9 days, and 115 of the 159 patients were male. Examined data
included known risk factors for MRSA, including human immunodeficiency virus infection,
diabetes mellitus, intravenous drug use, incarceration, and homelessness.
Results Forty-eight patients had surgery for hand infections due to CA-MRSA. The yearly
proportion of CA-MRSA increased over the study period, and the risk of having an MRSA
infection was 41% higher with each progressive calendar year during the study period
relative to the apparent incidence of non-MRSA hand infections. Other factors associated
with CA-MRSA were intravenous drug use, felon-type infection, and prior hand infection.
Multivariable logistic regression identified intravenous drug use as a significant, independent
risk factor for CA-MRSA hand infection.
Conclusions The proportion of surgically treated hand infections due to CA-MRSA has
increased during the last decade. Intravenous drug use was the only independent risk factor
for CA-MRSA infections treated in the operating room at our institution. (J Hand Surg 2010;
35A:97–103. © 2010 Published by Elsevier Inc. on behalf of the American Society for
Surgery of the Hand.)
Key words Hand infection, methicillin-resistant Staphylococcus aureus.
RISE IN METHICILLIN-RESISTANT
Staphylococcus media.1–5 In the past, this type of drug-resistant infec-
A aureus (MRSA) infections has been observed
over the last decade, resulting in considerable
attention from both the medical community and the lay
tion was chiefly found to inhabit medical environments,
populations with recent antibiotic exposure or invasive
devices, or settings in which large numbers of people
were housed in close proximity.4,6,7 However, more
From the University of Washington, Seattle, WA. pediatric and adult patients who have had no prior
Received for publication January 5, 2009; accepted in revised form September 3, 2009.
exposure to these types of high-risk settings are pre-
senting with MRSA infections.2 This type of infection,
No benefits in any form have been received or will be received related directly or indirectly to the
subject of this article. known as community-acquired MRSA (CA-MRSA),
Corresponding author: Jeffrey B. Friedrich, MD, Division of Plastic and Reconstructive Surgery,
has been associated with a high incidence in certain at-risk
University of Washington, 325 9th Avenue, Box 359796, Seattle, WA 98104-2499; e-mail: populations, including extremes of age, contact sports,
jfriedri@uw.edu. shared athletic equipment, and immunosuppression.1,2,7–17
0363-5023/10/35A01-0018$36.00/0 Hand infections are common problems that fre-
doi:10.1016/j.jhsa.2009.09.004
quently warrant surgical treatment; however, existing
© Published by Elsevier, Inc. on behalf of the ASSH. 䉬 97
98 MRSA HAND INFECTIONS
TABLE 1. ICD-9 Procedure Codes and Diagnosis TABLE 2. Demographics, Surgical Treatment,
Codes Used to Identify Surgically Treated Hand and Comorbid Illness Among Surgically Treated
Infections Hand Infections
ICD-9 Procedure Codes Non- p
80.14 Arthrotomy—hand/finger Overall MRSA MRSA Value
82.01 Exploration tendon sheath, hand Total 159 (100) 111 48
82.03 Bursotomy of hand Male (%) 72.3 72.1 72.9 .999
82.04 Incision and drainage palmar/thenar space Mean age (y) 40.1 40.7 38.6 .311
82.09 Incision soft tissue hand NEC Mean inpatient length 4.9 4.9 5.0 .830
82.92 Aspiration bursa of hand of stay (d)
82.93 Aspiration soft tissue hand NEC No. of surgeries 1.2 1.2 1.3 .633
ICD-9 Diagnosis Codes ⬎1 surgery (%) 13.8 12.6 16.7 .617
680.30 Infection of skin and subcutaneous tissue, upper arm Second infection (%) 5.7 2.7 12.5 .023
and forearm Admit to final 707 784 541 .084
680.40 Infection of skin and subcutaneous tissue, hand follow-up (d)
681.00 Cellulitis and abscess, unspecified, finger Potential risk factors
681.01 Felon Homeless (%) 32.1 28.8 39.6 .199
681.02 Onychia and paronychia of finger Inmate (%) 6.9 5.4 10.4 .309
711.04 Pyogenic arthritis, hand Diabetes mellitus (%) 6.3 7.2 4.2 .724
727.05 Tenosynovitis, hand and wrist Human 4.4 2.7 8.3 .200
immunodeficiency
virus (%)
IVDU (%) 35.2 27.0 54.2 .002
studies describing CA-MRSA hand infections have had Any comorbidity (%) 3.8 4.5 2.1 .669
relatively short study periods and minimal description Any complication (%) 6.3 7.1 4.4 .720
of risk factors for MRSA.18 –20 The purposes of this
study are to determine the change in proportion of IVDU, intravenous drug use.
Boldface values indicate statistical significance.
surgically treated CA-MRSA hand infections over the
last decade (1997–2007) at a single urban level I trauma
center and to analyze the risk factors associated with
hand infections caused by this pathogen. During the 11-year period encompassed by this
study, 159 patients had surgical intervention in the
PATIENT POPULATION AND METHODS
operating room for a hand infection. There were 115
Demographic data male and 44 female patients, with an average age of 40
After the study was approved by the institutional review years (range, 11– 82 y; Table 2). Mean length of hos-
board, applicable patients were identified from the pital stay was 4.9 days (median, 4 days; range, 0 –22 d).
records of a level I trauma center. Using a discharge Mean follow-up was 21 months (range 0 days–10 y);
database from 1997 to 2007, patients were identified however, because the study was focused on pathogens
using the International Classification of Diseases, 9th and risk factors, the length of follow-up was not an
Edition/Revision (ICD-9) procedure codes for surgical inclusion criterion. Many patients had potential risk
drainage of an infection of the hand in the operating factors for community-acquired drug-resistant infec-
room (Table 1). Patients identified by ICD-9 procedure tion, including homelessness (51), incarceration (11),
codes were confirmed to have an infection by indepen- intravenous drug use (IVDU) (57), history of diabetes
dent chart review. Current procedural terminology mellitus (10), and documented history of human immu-
codes were not available for use in identifying patients. nodeficiency virus (5). Because of the retrospective
Bacterial pathogens were identified by microbiologic nature of the data, the authors were unable to determine
culture and susceptibility data obtained from each sur- whether patients lived in communal living quarters such
gery. In addition, patients were coded by specific diag- as barracks or dormitories. Patients who had drainage of
noses using ICD-9 diagnosis codes, which included a hand infection in the emergency department were
suppurative tenosynovitis, abscess, septic arthritis, excluded, chiefly because the fluid from these infections
felon, and paronychia. was not routinely sent for gram stain and culture. Pa-
JHS 䉬 Vol A, January
MRSA HAND INFECTIONS 99
tients with iatrogenic infections or a history of recent
TABLE 3. Discharge Antibiotic Usage Among
hospitalization were excluded.21 In addition, patients Patients With Surgically Treated Hand
with infections due to a human bite were excluded Infections
because these cases often involve flora intrinsic to the
Antibiotic Non-MRSA MRSA
oral cavity.
Trimethoprim-sulfamethoxazole 8 26
Hospital course and infection characteristics Levofloxacin 7 7
The number of surgical procedures performed on each Clindamycin 16 8
patient was dictated by clinical circumstance and the Cephalexin 37 3
discretion of the treating surgeon. All patients had at Amoxicillin-clavulanate 42 2
least 1 surgical procedure for infection drainage. Twenty- Vancomycin 0 2
two patients required more than 1 surgery. Twenty-two Ciprofloxacin 0 2
patients had a second procedure; 10 patients, a third Rifampin 0 2
procedure; 5 patients, a fourth procedure; and 1 patient Linezolid 0 1
required a total of 10 procedures to obtain infection Nafcillin 1 0
control. Average follow-up time was 21 months (me- None 3 0
dian, 345 d; range, 1 d–10 y). Sixteen patients did not Penicillin VK 3 0
have follow-up after discharge from the hospital; there- Amoxicillin 1 0
fore, no assessment about their clinical results can be Trovafloxacin 1 0
made. Infection types requiring surgical drainage were Dicloxacillin 1 0
most commonly tenosynovitis (107), followed by ab- Metronidazole 1 0
scess (27), septic arthritis (19), felon (3), and 1 each of Doxycycline 1 0
paronychia, cellulitis and acute wound associated with
Total 122 53
phalangeal osteomyelitis, and laceration infection.
Eight patients had a second anatomically and tempo- Entries include patients who received more than 1 antibiotic.
rally distinct surgically treated hand infection after the
first infection was resolved.
accounted for 85% of the discharge antibiotics for the
Complications
group. Within the subgroup of patients who had CA-
Complications were assessed by presence of any resid- MRSA infections, trimethoprim/sulfamethoxazole was
ual dysfunction, arthritis, osteomyelitis, or other dis- the most commonly prescribed discharge agent, ac-
crete problems resulting from the infection or surgery. counting for 53% of the discharge antibiotics.
Because stiffness and edema of the affected part was
nearly universal, this was not counted as a complica- Statistical analysis
tion. A total of 9 patients had complications. Three
Bivariate analysis was conducted to determine which
patients required finger amputation due to digital isch-
variables were significantly associated with CA-MRSA.
emia following infection drainage. Three patients de-
Analysis was performed using a chi-square test for
veloped subsequent osteomyelitis, 1 of whom required
discrete variables and unpaired t-tests for continuous
ray amputation. Finally, 1 patient each had the follow- variables. Logistic regression analyses were used to
ing complications: delayed cutaneous wound healing, determine proportional risk for MRSA over the du-
mallet finger due to attritional rupture of the terminal ration of the study relative to the risk of being ad-
extensor tendon, and osteoarthritis of the proximal in- mitted for treatment of a non-MRSA infection. Non-
terphalangeal joint. MRSA infections were used as the comparison group
in all analyses because we did not have access to
Antibiotic usage population data. Because the numbers of people ad-
Antibiotic usage varied throughout the study cohort. mitted for treatment of non-MRSA hand infections
The 5 most common antibiotic regimens were single- remained stable over the course of the years evalu-
agent regimens and included amoxicillin/clavulanic ated, we determined that this comparison likely pro-
acid, cephalexin, trimethoprim/sulfamethoxazole, clin- vides an estimate of the change in the absolute inci-
damycin, and levofloxacin (Table 3). These 5 agents dence of CA-MRSA infections over the study period.
JHS 䉬 Vol A, January
100 MRSA HAND INFECTIONS
TABLE 4. Infection Type, Anatomic Location,
and Microbiology of Surgically Treated Hand
Infections
Non- p
Overall MRSA MRSA Value
n 159 111 48
Infection type
Tenosynovitis (%) 67.3 69.4 62.5 .462
Abscess (%) 17.0 13.5 25.0 .106
Septic arthritis (%) 11.9 15.3 4.2 .061
Felon (%) 1.9 0.0 6.3 .026
Paronychia (%) 0.6 0.0 2.1 .302
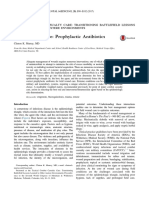
FIGURE 1: Proportion of patients with surgically treated hand
Cellulitis/osteomyelitis 0.6 0.9 0.0 .999
infections due to CA-MRSA over time. Values above each bar
(%)
represent the percentage of patients with CA-MRSA among
Infected laceration (%) 0.6 0.9 0.0 .999
the total number of patients each year.
Anatomic location
Finger and thumb (%) 2.5 2.7 2.1 .999
Hand (%) 13.8 13.5 14.6 .999
RESULTS
Forearm (%) 0.6 0.9 0.0 .999
During the 11-year period between 1997 and 2007, 48
Multiple sites (%) 11.3 11.7 10.4 .999
of 159 patients had cultures positive for CA-MRSA.
Wrist (%) 2.5 1.3 4.2 .585
The number of patients admitted with CA-MRSA in-
Finger joint (%) 6.9 7.2 6.3 .999
fections requiring surgical drainage rose significantly
Finger, no thumb (%) 73.0 74.8 68.8 .442
between 1997 and 2007. In contrast, the number of
Thumb only (%) 13.2 11.7 16.7 .447
patients admitted who required surgical drainage of
Non-MRSA microbiology
non-MRSA infections, although varying from year to
year, did not steadily increase (Fig. 1). Logistic regres- AHS (%) 3.8 5.4 0.0 .179
sion was used to compare the odds of being treated for GABHS (%) 29.6 36.9 12.5 .002
a CA-MRSA hand infection in each subsequent study MSSA (%) 31.4 45.0 0.0 ⬍.001
year during the period of study. The risk of having an N gonorrhea (%) 17.6 25.0 0.0 ⬍.001
MRSA infection was found to be 41% higher each Atypical (%) 6.3 9.0 0.0 .033
progressive calendar year during the study period rela- AHS, alpha-hemolytic Streptococcus; GABHS, group A beta-hemo-
tive to the risk of having a non-MRSA infection (odds lytic; MSSA, methicillin-sensitive Staphylococcus aureus; N gonor-
rhea, Neisseria gonorrhea.
ratio [OR], 1.41; 95% confidence interval [CI], 1.21– Boldface values indicate statistical significance.
1.64; p ⬍ .001).
Variables found by univariate analysis to be associ-
ated with CA-MRSA were IVDU (p ⫽ .002); a second
distinct, temporally unrelated hand infection (p ⫽ .01); p ⫽ .003) was independently associated with a higher
and felon-type hand infection (p ⫽ .026) (Tables 2 and risk of CA-MRSA hand infections (Table 5).
4). Factors not associated with CA-MRSA were age,
gender, other types of infection (tenosynovitis, abscess, DISCUSSION
etc.), location of infection on the hand, number of The proportion of methicillin-resistant Staphylococcus
surgeries, homelessness, incarceration, and other co- aureus infections continues to grow in hospital-
morbidities. Of the 143 patients for whom follow-up associated settings and, more recently, in community
data were available, there was no significant difference settings in the United States.4,22,23 Infection due to
in complication rates among the CA-MRSA and non- Staphylococcus aureus imposes a high and increasing
CA-MRSA groups (p ⫽ .72) (Table 2). Variables found burden on health care resources.4 A growing concern is
to be associated with CA-MRSA were analyzed by the emergence of MRSA infections among patient pop-
logistic regression to determine risk factors for CA- ulations with no apparent risk factors.21 Outbreaks of
MRSA. Only IVDU (OR, 3.58; 95% CI, 1.55– 8.29; CA-MRSA infections have emerged among healthy
JHS 䉬 Vol A, January
MRSA HAND INFECTIONS 101
TABLE 5. Logistic Regression for Potential Risk
MRSA ranging from 35% to 60% during 2003–2007.
Factors for CA-MRSA Among Surgically Another benefit of the current study, when compared
Treated Hand Infections to the earlier CA-MRSA hand infection studies men-
tioned, is an analysis of the risk factors thought to be
Variable Odds Ratio 95% CI p Value
associated with this pathogen.
Intravenous drug use 3.58 1.55–8.29 .003 Elucidating the risk factors for infection with CA-
Homelessness 1.03 0.42–2.51 .950 MRSA is an area of great research interest. Complicat-
Inmate 3.48 0.77–15.65 .104 ing these efforts are recent findings that the domains of
Diabetes mellitus 0.63 0.10–3.92 .616 CA-MRSA and HA-MRSA infection have been in-
Human immunodeficiency 2.89 0.48–17.37 .245
creasingly indistinct. LeBlanc’s group found that in
virus infection many patients with what appeared to be CA-MRSA, the
Second, separate hand 1.89 0.34–10.49 .469 particular MRSA strain was clonally similar to strains
infection of HA-MRSA.18,26 This spread of HA-MRSA beyond
Septic arthritis 0.32 0.05–1.88 .217 the hospital domain makes the elucidation of risk fac-
Felon ⬎10.0 0.00–⬎10.0 .999 tors even more difficult. Various risk factors for CA-
MRSA infection have been delineated; however, not all
Boldface values indicate statistical significance. studies have demonstrated agreement.21 A common
theory postulated that persons living in close quarters
(such as in jails, barracks, and dormitories) were at
individuals, including athletic teams, suggesting a higher risk of MRSA infection.6 However, the current
change in the evolving distribution apart from previ- analysis did not demonstrate incarceration to be a risk
ously identified high-risk populations.11,12,15–17 This factor. We were unable to reliably determine from the
emergence of antibiotic-resistant infections in the com- medical record whether patients lived in barracks or
munity has generated great concern in the early part of dormitories, and this could be considered a weakness of
this decade, as evidenced by extensive lay media cov- the study. In addition, 2 recent studies analyzing prior
erage.3,5 In addition, as many as 75% of soft tissue antibiotic usage found that antibiotic usage was associ-
infections observed in U.S. emergency rooms are due to ated with a higher risk of MRSA.6,24 The bivariate
CA-MRSA.24 Data also suggest that CA-MRSA has a analysis from the current study lends some credence to
more severe clinical course compared to hospital- this theory because prior hand infection had a stronger
acquired MRSA (HA-MRSA).25 association with presence of MRSA.
The treatment of hand infections comprises a sub- Intravenous drug use has been postulated to be
stantial proportion of many hand surgery practices. Re- linked to CA-MRSA infection.21 Earlier studies dem-
cent literature regarding CA-MRSA hand infections, onstrated IVDU to be a risk factor; however, Moran and
along with this institution’s recent experience, provided colleagues’ recent prospective emergency department
the impetus for this investigation. LeBlanc and col- study of soft tissue infections found only a modest
leagues provided one of the initial reports of CA- association between IVDU and presence of CA-
MRSA infections of the hand.18 This 3-year retrospec- MRSA.6,24 The current study found a significant asso-
tive analysis examined patients treated at a large, urban ciation between IVDU and CA-MRSA, on both biva-
hospital and found that a majority of patients (61%) riate and multivariate analyses. However, illicit drug
treated for hand infections had MRSA as the principal habits have regional variations, so this finding may not
pathogen. In a similar study, Bach and co-workers be generalizable.
conducted a 9-month study of patients treated for com- The majority of patients in this study had uncompli-
munity-acquired hand infections and found 73% cul- cated resolution of the infection following surgical
ture-positive for MRSA.19 In a 21-month retrospective drainage. This observation may indicate that with ap-
review, Kiran and co-workers found incidences of propriate surgical drainage, postoperative antibiotic ad-
MRSA hand infections that corroborated those of LeB- ministration is of secondary importance. Moran’s study
lanc and Bach.20 The more longitudinal nature of this of soft-tissue infections found that 96% of infections
study confirms the suspicion of an increasing propor- resolved after treatment in the emergency department.24
tion of CA-MRSA hand infections in recent years. Spe- In fact, Moran’s group suggests that drainage alone is
cifically, the proportion in the 5 most recent years was likely all that is necessary for treatment of soft-tissue
considerably higher than the first portion of the time period infections.24 Leblanc’s study of CA-MRSA hand infec-
(46.1%), with yearly proportions of patients with tions mentioned a trend toward increasing drug resis-
JHS 䉬 Vol A, January
102 MRSA HAND INFECTIONS
tance, but this finding has not been corroborated by and in better elucidating the characteristics of multi-
others.1,18 With surgically treated infections, multidrug drug-resistant bacterial infections.
resistance is probably less important to the final out-
come than adequate drainage. However, multidrug re- REFERENCES
sistance does have far-reaching implications for the 1. Eady EA, Cove JH. Staphylococcal resistance revisited: community-
acquired methicillin resistant Staphylococcus aureus—an emerging
treatment of infections in general. Finally, we found problem for the management of skin and soft tissue infections. Curr
that fully two-thirds of all patients in our series had Opin Infect Dis Apr 2003;16:103–124.
infections of the flexor tendon sheath. This observation 2. Frazee BW, Lynn J, Charlebois ED, Lambert L, Lowery D, Perd-
reau-Remington F. High prevalence of methicillin-resistant Staphy-
was different from Kiran’s findings in which most CA- lococcus aureus in emergency department skin and soft tissue infec-
MRSA hand infections were in the form of abscesses.20 tions. Ann Emerg Med 2005;45:311–320.
This may also reflect the fact that the current study 3. Berens M, Armstrong K. Culture of resistance. Seattle Times, Nov
16 –18, 2008.
concentrates on surgically treated infections, and sup- 4. National Nosocomial Infections Surveillance (NNIS) System Re-
purative flexor tenosynovitis is not amenable to emer- port, data summary from January 1992 through June 2004, issued
gency room treatment. October 2004. Am J Infect Control 2004;32:470 – 485.
5. Graham J. Study paints picture of rampant “superbug”. Chicago
Our study has a number of important limitations. Tribune, June 25, 2007:1.
Retrospective medical record reviews are subject to 6. Skiest DJ, Brown K, Cooper TW, Hoffman-Roberts H, Mussa HR,
incomplete or incorrect information. In particular, we Elliott AC. Prospective comparison of methicillin-susceptible and
methicillin-resistant community-associated Staphylococcus aureus
found that many records lacked antibiotic susceptibility
infections in hospitalized patients. J Infect 2007;54:427– 434.
results for all cultures, which removed a potentially 7. Olesevich M, Kennedy A. Emergence of community-acquired me-
valuable source of information for this study. Although thicillin-resistant Staphylococcus aureus soft tissue infections. J Pe-
the inclusion of surgically treated infections alone al- diatr Surg 2007;42:765–768.
8. Herold BC, Immergluck LC, Maranan MC, Lauderdale DS, Gaskin
lowed some uniformity of the patient population, the RE, Boyle-Vavra S, et al. Community-acquired methicillin-resistant
lack of culture data from most of the patients treated in Staphylococcus aureus in children with no identified predisposing
our emergency department greatly reduced the avail- risk. JAMA 1998;279:593–598.
9. Archibald LK, Shapiro J, Pass A, Rand K, Southwick F. Methicillin-
able population of the study. Further, the need for resistant Staphylococcus aureus infection in a college football team:
surgical (versus bedside) drainage was entirely at the risk factors outside the locker room and playing field. Infect Control
discretion of the treating physician, thereby introducing Hosp Epidemiol 2008;29:450 – 453.
10. Begier EM, Frenette K, Barrett NL, Mshar P, Petit S, Boxrud DJ, et
another source of selection bias. Finally, CA-MRSA al. A high-morbidity outbreak of methicillin-resistant Staphylococ-
was defined among those patients without prior hospi- cus aureus among players on a college football team, facilitated by
talizations or hospital-acquired infections. Microbio- cosmetic body shaving and turf burns. Clin Infect Dis 2004;39:
1446 –1453.
logic identification of clonal strains associated with 11. Centers for Disease Control and Prevention (CDC). Methicillin-
CA-MRSA was not performed in this study, so the resistant Staphylococcus aureus among players on a high school
designation of CA-MRSA depends solely on social and football team—New York City, 2007. MMWR Morb Mortal Wkly
clinical criteria. Defining CA-MRSA by the absence of Rep. 2009;58:52–55.
12. Coronado F, Nicholas JA, Wallace BJ, Kohlerschmidt DJ, Musser K,
risk factors for health care exposure might underesti- Schoonmaker-Bopp DJ, et al. Community-associated methicillin-
mate the true number of CA-MRSA cases.26 resistant Staphylococcus aureus skin infections in a religious com-
This study presents a longitudinal analysis of the munity. Epidemiol Infect 2007;135:492–501.
13. Hall AJ, Bixler D, Haddy LE. Multiclonal outbreak of methicillin-
changing proportion of CA-MRSA hand infections and resistant Staphylococcus aureus infections on a collegiate football
the potential risk factors that are associated with this team. Epidemiol Infect 2009;137:85–93.
problem. Multivariable analysis demonstrated that 14. Lee MC, Rios AM, Aten MF, et al. Management and outcome of
children with skin and soft tissue abscesses caused by community-
more recent years of infection and admitted IVDU were acquired methicillin-resistant Staphylococcus aureus. Pediatr Infect
associated with increased odds of having MRSA as a Dis J 2004;23:123–127.
pathogen in the hand infection. Although we did not 15. Nguyen DM, Bancroft E, Mascola L, Guevara R, Yasuda L. Risk
factors for neonatal methicillin-resistant Staphylococcus aureus in-
find other risk factors such as homelessness and incar- fection in a well-infant nursery. Infect Control Hosp Epidemiol
ceration to be associated with a higher risk of CA- 2007;28:406 – 411.
MRSA, these factors should be taken into consideration 16. Cohen PR. Cutaneous community-acquired methicillin-resistant
Staphylococcus aureus infection in participants of athletic activities.
when initially providing empiric antibiotic treatment for
South Med J 2005;98:596 – 602.
hand infections. Fortunately, in cases of hand infections 17. Nguyen DM, Mascola L, Brancoft E. Recurring methicillin-resistant
involving fluid collection, drainage of the infected ma- Staphylococcus aureus infections in a football team. Emerg Infect
terial is usually adequate treatment. Future prospective Dis 2005;11:526 –532.
18. LeBlanc DM, Reece EM, Horton JB, Janis JE. Increasing incidence of
multi-institutional studies will be valuable in further methicillin-resistant Staphylococcus aureus in hand infections: a 3-year
refining the risk profile of CA-MRSA hand infections county hospital experience. Plast Reconstr Surg 2007;119:935–940.
JHS 䉬 Vol A, January
MRSA HAND INFECTIONS 103
19. Bach HG, Steffin B, Chhadia AM, Kovachevich R, Gonzalez MH. 23. Grundmann H, Aires-de-Sousa M, Boyce J, Tiemersma E. Emer-
Community-associated methicillin-resistant Staphylococcus aureus gence and resurgence of meticillin-resistant Staphylococcus aureus
hand infections in an urban setting. J Hand Surg 2007;32A:380 –383. as a public-health threat. Lancet 2006;368:874 – 885.
20. Kiran RV, McCampbell B, Angeles AP, Montilla RD, Medina C, 24. Moran G, Krishnadasan A, Gorwitz R, Fosheim GE, McDougal LK,
Mitra A, et al. Increased prevalence of community-acquired methi- Carey RB, et al. Methicillin-resistant S. aureus infections among
cillin-resistant Staphylococcus aureus in hand infections at an urban patients in the emergency department. N Engl J Med 2006;355:
medical center. Plast Reconstr Surg 2006;118:161–166; discussion 666 – 674.
167–169. 25. Davis SL, Perri MB, Donabedian SM, Manierski C, Singh A, Vager
21. Boucher H, Corey G. Epidemiology of methicillin-resistant Staphy- D, et al. Epidemiology and outcomes of community-associated me-
lococcus aureus. Clin Infect Dis 2008;46 Suppl 5:S344 –349. thicillin-resistant Staphylococcus aureus infection. J Clin Microbiol
22. Laupland K, Church D, Mucenski M, Sutherland L, Davies H. 2007;45:1705–1711.
Population-based study of the epidemiology of and the risk factors 26. David MZ, Glikman D, Crawford SE, Peng J, King KJ, Hostetler MA,
for invasive Staphylococcus aureus infections. J Infect Dis 2003; et al. What is community-associated methicillin-resistant Staphylococ-
187:1452–1459. cus aureus? J Infect Dis 2008;197:1235–1243.
JHS 䉬 Vol A, January
You might also like
- Chapter 29 - Test: (60 Minutes)Document3 pagesChapter 29 - Test: (60 Minutes)Minh ThanhNo ratings yet
- UOP 304-08 Bromine Number and Bromine Index of Hydrocarbons by Potentiometric TitrationDocument13 pagesUOP 304-08 Bromine Number and Bromine Index of Hydrocarbons by Potentiometric TitrationMorteza SepehranNo ratings yet
- Anti Biotik 2015Document22 pagesAnti Biotik 2015cut herlindaNo ratings yet
- 3 - Acute InfectionsDocument44 pages3 - Acute InfectionsAlexa GabrielaNo ratings yet
- Risk Factors For Surgical Site InfectionDocument5 pagesRisk Factors For Surgical Site InfectionElizabeth Mautino CaceresNo ratings yet
- Bacterial and Fungal Contamination of Dental Hygienists' Hands With and Without Finger RingsDocument5 pagesBacterial and Fungal Contamination of Dental Hygienists' Hands With and Without Finger RingsAsniza AbasNo ratings yet
- Articulo Evaluacion Final Antimicrobianos 1 2020Document9 pagesArticulo Evaluacion Final Antimicrobianos 1 2020Juan BojacaNo ratings yet
- A Study of Skin Infection - How To Diagnosis and Its TherapyDocument7 pagesA Study of Skin Infection - How To Diagnosis and Its TherapyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Skin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus AureusDocument11 pagesSkin and Soft-Tissue Infections Caused by Methicillin-Resistant Staphylococcus AureusFerdy RamadhanNo ratings yet
- The Health Professional's Role in Preventing Nosocomial InfectionsDocument5 pagesThe Health Professional's Role in Preventing Nosocomial InfectionsAbdo MohamedNo ratings yet
- Hand Osteomyelitis HudaDocument34 pagesHand Osteomyelitis HudaOrtho songoNo ratings yet
- Microbial Species Isolated From Infected Wounds and Antimicrobial Resistance Analysis: Data Emerging From A Three-Years Retrospective StudyDocument14 pagesMicrobial Species Isolated From Infected Wounds and Antimicrobial Resistance Analysis: Data Emerging From A Three-Years Retrospective StudyFawwaziNo ratings yet
- Free Research Papers On MrsaDocument8 pagesFree Research Papers On Mrsaafnhbijlzdufjj100% (1)
- Epidemiologia de Lesiones de Punta de Dedo en Hospital de PEMEXDocument14 pagesEpidemiologia de Lesiones de Punta de Dedo en Hospital de PEMEXOscar Cayetano Herrera RodríguezNo ratings yet
- Mrsa101 508Document45 pagesMrsa101 508Sam TullyNo ratings yet
- Sepsis in Trauma: A Deadly Complication: Fernanda Mas-Celis, Jimena Olea-López, and Javier Alberto Parroquin-MaldonadoDocument9 pagesSepsis in Trauma: A Deadly Complication: Fernanda Mas-Celis, Jimena Olea-López, and Javier Alberto Parroquin-MaldonadoMelissa JosephNo ratings yet
- 19.2 Antimicrobial Management of Complicated Skin and Soft Tissue KONAS PETRI BALI 2023-1Document34 pages19.2 Antimicrobial Management of Complicated Skin and Soft Tissue KONAS PETRI BALI 2023-1Eva RoswatiNo ratings yet
- Skin and Soft Tissue InfectionsDocument8 pagesSkin and Soft Tissue InfectionsciaranNo ratings yet
- MrsaDocument63 pagesMrsaRAHULNo ratings yet
- Life 13 01126Document14 pagesLife 13 01126s4cdbv4xjrNo ratings yet
- Disease ReportDocument2 pagesDisease Reportapi-511364141No ratings yet
- Empiric Antibiotics For Acute Infections of The HaDocument4 pagesEmpiric Antibiotics For Acute Infections of The HaBrea WilleyNo ratings yet
- Current Pathogens Infecting Open Fracture Tibia and Their Antibiotic Susceptibility at A Tertiary Care Teaching Hospital in South East AsiaDocument10 pagesCurrent Pathogens Infecting Open Fracture Tibia and Their Antibiotic Susceptibility at A Tertiary Care Teaching Hospital in South East AsiaFrancis RomanosNo ratings yet
- Chapter Two Literature ReviewDocument11 pagesChapter Two Literature ReviewKojo Adu100% (1)
- Surgical Site Infections: Epidemiology, Microbiology and PreventionDocument8 pagesSurgical Site Infections: Epidemiology, Microbiology and Preventionm8wyb2f6ngNo ratings yet
- SSI Webinar Series 1 PABIDocument18 pagesSSI Webinar Series 1 PABISafira Wahyu NurhardiyantiNo ratings yet
- Methicillin Resistant Staphylococcus Aureus: (MRSA)Document13 pagesMethicillin Resistant Staphylococcus Aureus: (MRSA)Adnan JourdanNo ratings yet
- Rab 9Document12 pagesRab 9Belia DestamaNo ratings yet
- Health NexusDocument3 pagesHealth NexusanupamaniroopNo ratings yet
- Wounds 313-323 PDFDocument12 pagesWounds 313-323 PDFTrong HieuNo ratings yet
- Missirlis, Katsikogianni, Missirlis. 2004. CONCISE REVIEW OF MECHANISMS OF BACTERIAL ADHESION TO BIOMATERIALS AND OF TECHNIQUES USED INDocument21 pagesMissirlis, Katsikogianni, Missirlis. 2004. CONCISE REVIEW OF MECHANISMS OF BACTERIAL ADHESION TO BIOMATERIALS AND OF TECHNIQUES USED INAzb 711No ratings yet
- Bone Graft SubstitutesDocument5 pagesBone Graft SubstitutessarraNo ratings yet
- Bali 2011Document4 pagesBali 2011ashkisaragiNo ratings yet
- Antibiotic Resistance in Malaysia and Its Public HDocument8 pagesAntibiotic Resistance in Malaysia and Its Public HNora LeeNo ratings yet
- MrsaDocument10 pagesMrsazia ul RahmanNo ratings yet
- Smart Central Venous Port For Early Detection of Bacterial Biofilm Related InfectionsDocument10 pagesSmart Central Venous Port For Early Detection of Bacterial Biofilm Related InfectionsGeneration GenerationNo ratings yet
- MRSA Case ReportDocument3 pagesMRSA Case ReportDr P.R. RaghavanNo ratings yet
- Luka 2 PDFDocument6 pagesLuka 2 PDFBarryNo ratings yet
- AAJIC Journal of QAC For SARS COV2Document2 pagesAAJIC Journal of QAC For SARS COV2ayuwinaNo ratings yet
- Field Wound Care: Prophylactic AntibioticsDocument13 pagesField Wound Care: Prophylactic AntibioticsAgstri Lestari PutriNo ratings yet
- Pepsi@u.washington - Edu: JA A DDocument1 pagePepsi@u.washington - Edu: JA A Disra navaNo ratings yet
- agm.j-3288.75-fDocument15 pagesagm.j-3288.75-fChandravadhana NarayananNo ratings yet
- 2022 Article 1123Document10 pages2022 Article 1123Achmad NurNo ratings yet
- Prevention of HAI IndonesienDocument208 pagesPrevention of HAI IndonesienLipun SethiNo ratings yet
- Are You and Your Patients in Safe HandsDocument8 pagesAre You and Your Patients in Safe Handsanis merahNo ratings yet
- Balancing Infection Control and Environmental.42Document4 pagesBalancing Infection Control and Environmental.42Alice MozerNo ratings yet
- Characteristics of Microbial Drug Resistance and Its Correlates in Chronic Diabetic Foot Ulcer InfectionsDocument9 pagesCharacteristics of Microbial Drug Resistance and Its Correlates in Chronic Diabetic Foot Ulcer InfectionsPutri Alif PermatasariNo ratings yet
- OM Stafilococo (Clase Observacionales)Document7 pagesOM Stafilococo (Clase Observacionales)Jairo Camilo Guevara FaríasNo ratings yet
- Occupational Hazards in DentistryDocument4 pagesOccupational Hazards in DentistrymonikaNo ratings yet
- 2021 Surgical Site Infection After Liver Transplantation in The Era of MultidrugDocument7 pages2021 Surgical Site Infection After Liver Transplantation in The Era of MultidrugInaldoNo ratings yet
- Capstone Apa Honors Prof 2Document7 pagesCapstone Apa Honors Prof 2api-543808198No ratings yet
- Wounds, Antimicrobial Resistance and Challenges of Implementing A Surveillance System in Myanmar: A Mixed-Methods StudyDocument15 pagesWounds, Antimicrobial Resistance and Challenges of Implementing A Surveillance System in Myanmar: A Mixed-Methods StudyKarina Dwi SwastikaNo ratings yet
- 1 - Name of The Candidate and AddressDocument19 pages1 - Name of The Candidate and AddressRini ThomasNo ratings yet
- Medi 97 E11097Document4 pagesMedi 97 E11097Lia FikayuniarNo ratings yet
- Necrotising Soft-Tissue InfectionsDocument14 pagesNecrotising Soft-Tissue Infectionssergio salazarNo ratings yet
- Current Concepts On The Virulence Mechanisms of Meticillin-Resistant Staphylococcus AureusDocument15 pagesCurrent Concepts On The Virulence Mechanisms of Meticillin-Resistant Staphylococcus AureusSeptiani HasibuanNo ratings yet
- Infection ControlDocument24 pagesInfection Controlsteffy christNo ratings yet
- Supra SobDocument34 pagesSupra SobZakaria NersNo ratings yet
- Promoting Asepsis and Infection Control: Teresa V. Hurley, MSN, RNDocument53 pagesPromoting Asepsis and Infection Control: Teresa V. Hurley, MSN, RNRoan DAlleNo ratings yet
- Such Ard 2011Document9 pagesSuch Ard 2011Jose MenesesNo ratings yet
- Resetting Healthcare Post-COVID-19 Pandemic: The Patient HandbookFrom EverandResetting Healthcare Post-COVID-19 Pandemic: The Patient HandbookNo ratings yet
- Viral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensFrom EverandViral Vistas: Insights into Infectious Diseases: The Invisible War: Decoding the Game of Hide and Seek with PathogensNo ratings yet
- A High Proportion of Beta-Tocopherol In. 2019Document5 pagesA High Proportion of Beta-Tocopherol In. 2019Miguel Antonio CaicedoNo ratings yet
- Coalmine Monitoring SystemDocument65 pagesCoalmine Monitoring SystemTechnos_IncNo ratings yet
- Report On Reuse of Abandoned Quarries and Mine Pits in KeralaDocument90 pagesReport On Reuse of Abandoned Quarries and Mine Pits in KeralaDrThrivikramji Kyth100% (10)
- Button LoadcellDocument3 pagesButton LoadcellkshripNo ratings yet
- Datasheet Painel Solar 360W KuMax CS3U PDocument2 pagesDatasheet Painel Solar 360W KuMax CS3U PDenis SilvaNo ratings yet
- Integrity Management of Safety Critical Equipment and SystemsDocument10 pagesIntegrity Management of Safety Critical Equipment and SystemsLi QiNo ratings yet
- 04 - Rotational Motion - JEE PDFDocument124 pages04 - Rotational Motion - JEE PDFCefas Almeida50% (2)
- Projet de Partenariat Senegal Mat-Groupe Caparol Version AnglaiseDocument7 pagesProjet de Partenariat Senegal Mat-Groupe Caparol Version AnglaiseTaga DiopNo ratings yet
- Jobm 201800252Document14 pagesJobm 201800252leilany casillasNo ratings yet
- Contoh Soal Koordinasi Relay Ocr PDFDocument2 pagesContoh Soal Koordinasi Relay Ocr PDFEdi CarnediNo ratings yet
- Datasheet DiacDocument4 pagesDatasheet DiacOrlandoTobonNo ratings yet
- 7 TH Biology Worksheets Ls 8 Weather, Climate Animal AdaptationsDocument7 pages7 TH Biology Worksheets Ls 8 Weather, Climate Animal AdaptationsAysha Muhammad ShahzadNo ratings yet
- 50 Milisimal PotencyDocument8 pages50 Milisimal PotencyDr. Surendra Singh100% (3)
- Catalogue V2 - 2012 Final (Full Copy)Document132 pagesCatalogue V2 - 2012 Final (Full Copy)Richard PayneNo ratings yet
- TF65-67 Thermal Overload Relay: Product-DetailsDocument5 pagesTF65-67 Thermal Overload Relay: Product-DetailsSergio PartidaNo ratings yet
- Castrol 0w-30 German CastrolDocument2 pagesCastrol 0w-30 German CastrolTudor RatiuNo ratings yet
- Cloze Passage For SMP Kls 3Document7 pagesCloze Passage For SMP Kls 3DibaPertiwiNo ratings yet
- What Causes HallucinationsDocument2 pagesWhat Causes Hallucinationslook at meNo ratings yet
- Octamar LI 5 PDSDocument2 pagesOctamar LI 5 PDSfransleo.applicationNo ratings yet
- Manual Board 945GCT-M (2.0A)Document48 pagesManual Board 945GCT-M (2.0A)BalrogJoelNo ratings yet
- NIOEC-SP-00-72 (1) : Process Design of Hot Oil & Tempered Water CircuitsDocument28 pagesNIOEC-SP-00-72 (1) : Process Design of Hot Oil & Tempered Water CircuitsMohammad AminiNo ratings yet
- Wastage of Food in Indian WeddingsDocument9 pagesWastage of Food in Indian WeddingsThe United IndianNo ratings yet
- Week 4 - Stadelman-Cohen & Hillman (2014)Document22 pagesWeek 4 - Stadelman-Cohen & Hillman (2014)kehanNo ratings yet
- Girder - Arrangement 04 08 2023Document9 pagesGirder - Arrangement 04 08 2023sanyogitasawant5No ratings yet
- Soal USP BIG LMDocument56 pagesSoal USP BIG LMMoh. Aska FailandriNo ratings yet
- An Immunology-Inspired Network Security Architecture 2020Document12 pagesAn Immunology-Inspired Network Security Architecture 2020rgtreadsNo ratings yet
- CT-Demag Flyer InstrumentDocument2 pagesCT-Demag Flyer InstrumentKarthik SriramakavachamNo ratings yet
- The Evolution of Water Reverse Osmosis TechnologyDocument35 pagesThe Evolution of Water Reverse Osmosis TechnologyQassim LaouiraNo ratings yet