Professional Documents
Culture Documents
Prevalence of TB-HIV Co-Infection in Countries Except China
Prevalence of TB-HIV Co-Infection in Countries Except China
Uploaded by
Elizabeth AmezcuaCopyright:
Available Formats
You might also like
- Case Study of La Posta Mexican RestaurantsDocument1 pageCase Study of La Posta Mexican RestaurantsFatima Atiq80% (5)
- Power Wizard 2.1: CTA CTB CTCDocument2 pagesPower Wizard 2.1: CTA CTB CTCOsanebi Chukwudi Lucky80% (10)
- BS 57 (1951)Document23 pagesBS 57 (1951)dapsiduNo ratings yet
- Crochet Tunisian PrimerDocument7 pagesCrochet Tunisian PrimerVerónica Bertero100% (4)
- Astm E2352 - 1 (En) PDFDocument14 pagesAstm E2352 - 1 (En) PDFSainath AmudaNo ratings yet
- Prevalence and Determinants of Human Immunodeficiency Virus and Tuberculosis Co-Infection at Kampala International University Teaching HospitalDocument6 pagesPrevalence and Determinants of Human Immunodeficiency Virus and Tuberculosis Co-Infection at Kampala International University Teaching HospitalKIU PUBLICATION AND EXTENSIONNo ratings yet
- HZVDocument15 pagesHZVMarviane ThenNo ratings yet
- Jurnal 2Document16 pagesJurnal 2Edwin Pasha Jr.No ratings yet
- HCW Vs Adult Influenza IncidenceDocument9 pagesHCW Vs Adult Influenza Incidencereza_adrian_2No ratings yet
- Prognostic Score To Predict Mortality During TB Treatment in TBHIV Co-Infected PatientsDocument12 pagesPrognostic Score To Predict Mortality During TB Treatment in TBHIV Co-Infected PatientsGani ArlondNo ratings yet
- Ali2016 Article OutcomesOfTBTreatmentInHIVCo-iDocument9 pagesAli2016 Article OutcomesOfTBTreatmentInHIVCo-itishaNo ratings yet
- Njie-Khan2021 Article PrevalenceOfTuberculosisAndMenDocument7 pagesNjie-Khan2021 Article PrevalenceOfTuberculosisAndMenLinh NguyenNo ratings yet
- Ambo UniversityDocument12 pagesAmbo UniversityArarsa TolasaNo ratings yet
- Status of Tuberculosis-Related Stigma and Associated Factors: A Cross-Sectional Study in Central ChinaDocument7 pagesStatus of Tuberculosis-Related Stigma and Associated Factors: A Cross-Sectional Study in Central ChinaCharis MurwadiNo ratings yet
- J Infect Dis. 2022 Aug 12 - 226 - Suppl 1 - S17-S21.Document19 pagesJ Infect Dis. 2022 Aug 12 - 226 - Suppl 1 - S17-S21.HemerobibliotecaHospitalNo ratings yet
- RESEARCH ARTICLE Detecting Spatial Clusters of HIV and Hepatitis CoinfectionsDocument16 pagesRESEARCH ARTICLE Detecting Spatial Clusters of HIV and Hepatitis CoinfectionsDicky rahadianNo ratings yet
- Ofx 137Document7 pagesOfx 137Sheila Alcalde RNo ratings yet
- Re Ections On 40 Years of AIDS: PerspectiveDocument8 pagesRe Ections On 40 Years of AIDS: PerspectiveANGEL OMAR SANTANA AVILANo ratings yet
- Medi 102 E32811Document9 pagesMedi 102 E32811dani catriaNo ratings yet
- Co-Infection of Tuberculosis and Parasitic Diseases in Humans A Systematic ReviewDocument12 pagesCo-Infection of Tuberculosis and Parasitic Diseases in Humans A Systematic ReviewThamile CaetanoNo ratings yet
- Directly Observed TreatmentDocument9 pagesDirectly Observed TreatmentNovelia CarolinNo ratings yet
- Fetch ObjectDocument7 pagesFetch ObjectBilly UntuNo ratings yet
- Marzieh Shareizaei - Et.alDocument7 pagesMarzieh Shareizaei - Et.alkang.asep008No ratings yet
- Reference ThesisDocument13 pagesReference ThesisGhina SalsabilaNo ratings yet
- 2017 Article 2662Document11 pages2017 Article 2662Dhani KurniawanNo ratings yet
- The Global Epidemiology of Bacterial Vaginosis A Systematic ReviewDocument19 pagesThe Global Epidemiology of Bacterial Vaginosis A Systematic ReviewcheracapNo ratings yet
- Tuberculosis Vih EthiopiaDocument9 pagesTuberculosis Vih Ethiopiajulma1306No ratings yet
- Antiretroviral Therapy For Prevention of HIV Transmission: Implications For EuropeDocument23 pagesAntiretroviral Therapy For Prevention of HIV Transmission: Implications For EuropenukarevaNo ratings yet
- September CDC HAISDocument11 pagesSeptember CDC HAISnoval firdausNo ratings yet
- Syphilis Epidemic Among Men Who Have Sex With Men: A Global Systematic Review and Meta-Analysis of Prevalence, Incidence, and Associated FactorsDocument11 pagesSyphilis Epidemic Among Men Who Have Sex With Men: A Global Systematic Review and Meta-Analysis of Prevalence, Incidence, and Associated FactorsEldie RahimNo ratings yet
- HIV Prevalence in Suspected Ebola Cases During The 2014 - 2016 Ebola Epidemic in Sierra LeoneDocument4 pagesHIV Prevalence in Suspected Ebola Cases During The 2014 - 2016 Ebola Epidemic in Sierra LeoneJairo Castro MaestreNo ratings yet
- naturaleza y consecuencia de las coinfeccionesDocument7 pagesnaturaleza y consecuencia de las coinfeccionesSEVILLA RAMIREZ JOSE MANUELNo ratings yet
- WHO Position Paper Dengue 2016 ReferencesDocument17 pagesWHO Position Paper Dengue 2016 Referencessingularity24601_302No ratings yet
- HIV Epidemiology Among Female Sex Workers and Their Clients in The Middle East and North Africa: Systematic Review, Meta-Analyses, and Meta-RegressionsDocument30 pagesHIV Epidemiology Among Female Sex Workers and Their Clients in The Middle East and North Africa: Systematic Review, Meta-Analyses, and Meta-RegressionsLuís MiguelNo ratings yet
- Djimeu Published Replication PlanDocument17 pagesDjimeu Published Replication PlanVishalvishaldograNo ratings yet
- 19 Ninan EtalDocument6 pages19 Ninan EtaleditorijmrhsNo ratings yet
- CommunityViralLoadinHIV PDFDocument9 pagesCommunityViralLoadinHIV PDFIsaias PrestesNo ratings yet
- 10 1111@tbed 13621Document37 pages10 1111@tbed 13621onlyhyesun119No ratings yet
- Multidrug-Resistant Tuberculosis in Uzbekistan: Results of A Nationwide Survey, 2010 To 2011Document12 pagesMultidrug-Resistant Tuberculosis in Uzbekistan: Results of A Nationwide Survey, 2010 To 2011IsoqjonivichNo ratings yet
- Epidemiological Risk Factors For Adult Dengue in Singapore: An 8-Year Nested Test Negative Case Control StudyDocument9 pagesEpidemiological Risk Factors For Adult Dengue in Singapore: An 8-Year Nested Test Negative Case Control StudydouwesdNo ratings yet
- Epidemiology, Clinical Manifestations, and Outcomes of Streptococcus Suis Infection in HumansDocument10 pagesEpidemiology, Clinical Manifestations, and Outcomes of Streptococcus Suis Infection in HumansMark ReinhardtNo ratings yet
- Chapter II ReviewDocument5 pagesChapter II ReviewPardeepCharlyNo ratings yet
- Art GEBADocument8 pagesArt GEBAJhonathan Andres Garcia FiallosNo ratings yet
- Risk Factors For Herpes Zoster Infection: A Meta-Analysis: Review ArticleDocument8 pagesRisk Factors For Herpes Zoster Infection: A Meta-Analysis: Review Articleyenny handayani sihiteNo ratings yet
- Multidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceDocument7 pagesMultidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceAldy RinaldiNo ratings yet
- Spatial Analysis of TuberculosisDocument77 pagesSpatial Analysis of TuberculosisChrlzs BlgNo ratings yet
- HIV Systematic Review and Meta AnalysisDocument13 pagesHIV Systematic Review and Meta AnalysisSanti IskandarNo ratings yet
- Survival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorDocument10 pagesSurvival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorGetachew GemedaNo ratings yet
- Assessment of Psychosocial and Economic Adaptation Among People Living With Hivaids in NigeriaDocument74 pagesAssessment of Psychosocial and Economic Adaptation Among People Living With Hivaids in NigeriaDaniel ObasiNo ratings yet
- The Effectiveness and Cost-Effectiveness of Screening For HIV in Migrants in The EU/EEA: A Systematic ReviewDocument23 pagesThe Effectiveness and Cost-Effectiveness of Screening For HIV in Migrants in The EU/EEA: A Systematic ReviewAlexandra PaunNo ratings yet
- Plos Medicine /Article/Crossref/I /Article/Tw Itter/Info /Article/Metrics/Inf Info:Doi/10.1371/J Patient Adher 1185260400000Document25 pagesPlos Medicine /Article/Crossref/I /Article/Tw Itter/Info /Article/Metrics/Inf Info:Doi/10.1371/J Patient Adher 1185260400000khattak_i89No ratings yet
- Ofy 017Document9 pagesOfy 017Zakia DrajatNo ratings yet
- Interventions To Prevent Sexually Transmitted Infections, Including HIV InfectionDocument15 pagesInterventions To Prevent Sexually Transmitted Infections, Including HIV Infectionursula_ursulaNo ratings yet
- Paper TBDocument24 pagesPaper TBnachersNo ratings yet
- 1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1Document9 pages1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1dewi ayu wulandariNo ratings yet
- EpidemiologyDocument7 pagesEpidemiologyInoxcent MoonNo ratings yet
- Example of Research Paper About HivDocument6 pagesExample of Research Paper About Hivc9qb8gy7100% (3)
- Jurnal 10 HariantoDocument7 pagesJurnal 10 Hariantoaryzamelindah channelNo ratings yet
- Pamj 27 48Document7 pagesPamj 27 48JihanNo ratings yet
- Jia2 25392Document10 pagesJia2 25392Herpriiy BatukhNo ratings yet
- Captura de Pantalla 2024-01-23 A La(s) 11.26.43Document9 pagesCaptura de Pantalla 2024-01-23 A La(s) 11.26.43Dany MorBenNo ratings yet
- Awareness of Dengue and Practice of Dengue Control Among1Document6 pagesAwareness of Dengue and Practice of Dengue Control Among1rjohn 7No ratings yet
- HIV Screening USPTFDocument21 pagesHIV Screening USPTFhivpolicyyesNo ratings yet
- SSP Assignment Problems - FinalDocument2 pagesSSP Assignment Problems - FinalVadivelan AdaikkappanNo ratings yet
- Lesson Plan PatrickDocument4 pagesLesson Plan PatrickPatrick Jerome SilvanoNo ratings yet
- Electronics and Communication Engineering Sample ThesisDocument7 pagesElectronics and Communication Engineering Sample Thesiseifvhpugg100% (1)
- Research Methods For Commerce Lab Practical File "BRM Lab" BBA (M1) - BBA 213Document67 pagesResearch Methods For Commerce Lab Practical File "BRM Lab" BBA (M1) - BBA 213Mankeerat Singh ChannaNo ratings yet
- LIT - Sullair S-Energy 25-40hp Brochure - SAPSEN2540201904-6 - ENDocument8 pagesLIT - Sullair S-Energy 25-40hp Brochure - SAPSEN2540201904-6 - ENKrist San QNo ratings yet
- Persuasive Writing Assessment RubricDocument2 pagesPersuasive Writing Assessment Rubricapi-523656984No ratings yet
- PoonamDocument54 pagesPoonamCH Rajan GujjarNo ratings yet
- BeachesDocument32 pagesBeachesnympheasandhuNo ratings yet
- CiabattaDocument4 pagesCiabattaTarak ZayaniNo ratings yet
- WH2009 WaterHorseCatalogDocument132 pagesWH2009 WaterHorseCatalogAiko FeroNo ratings yet
- Gabet Response To Motion To CompelDocument13 pagesGabet Response To Motion To CompelKenan FarrellNo ratings yet
- Alim Knit (BD) LTD.: Recommended Process Flow DiagramDocument1 pageAlim Knit (BD) LTD.: Recommended Process Flow DiagramKamrul HasanNo ratings yet
- Roles of Physiotherapy in Intensive Care Unit (Document28 pagesRoles of Physiotherapy in Intensive Care Unit (Chukwuemeka ChidogoNo ratings yet
- Dvp-Es2 Ss2 Sa2 Sx2-Program o en 20110302Document609 pagesDvp-Es2 Ss2 Sa2 Sx2-Program o en 20110302puskyboyNo ratings yet
- SSC Gr10 ICT Q4 Module 2 WK 2 - v.01-CC-released-7June2021Document16 pagesSSC Gr10 ICT Q4 Module 2 WK 2 - v.01-CC-released-7June2021Vj AleserNo ratings yet
- PFW - Vol. 23, Issue 08 (August 18, 2008) Escape To New YorkDocument0 pagesPFW - Vol. 23, Issue 08 (August 18, 2008) Escape To New YorkskanzeniNo ratings yet
- Mother Gooses MelodyDocument49 pagesMother Gooses MelodyDominick GraceNo ratings yet
- Project WorkDocument6 pagesProject WorkNurbek YaxshimuratovNo ratings yet
- The Psychological Aspects of Cinematography and Its ImpactDocument21 pagesThe Psychological Aspects of Cinematography and Its Impactanastasiapiven7No ratings yet
- BUMA 20053 BUSINESS RESEARCH ModuleDocument59 pagesBUMA 20053 BUSINESS RESEARCH ModuleJanell Aganan100% (1)
- Rev29jan2019oftemplate OSHprogram Asof 290119Document12 pagesRev29jan2019oftemplate OSHprogram Asof 290119GelinaNo ratings yet
- VarahamihiraDocument6 pagesVarahamihiraSTAR GROUPS100% (1)
- SUBHIKSHADocument12 pagesSUBHIKSHAAkshat ChaturvediNo ratings yet
- ĐỀ 2Document4 pagesĐỀ 2Khôi Nguyên PhạmNo ratings yet
- 21st Century WeaponsDocument6 pages21st Century WeaponsSaqibMahmoodNo ratings yet
Prevalence of TB-HIV Co-Infection in Countries Except China
Prevalence of TB-HIV Co-Infection in Countries Except China
Uploaded by
Elizabeth AmezcuaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Prevalence of TB-HIV Co-Infection in Countries Except China
Prevalence of TB-HIV Co-Infection in Countries Except China
Uploaded by
Elizabeth AmezcuaCopyright:
Available Formats
Prevalence of TB/HIV Co-Infection in Countries Except
China: A Systematic Review and Meta-Analysis
Junling Gao, Pinpin Zheng, Hua Fu*
School of Public Health, Fudan University, Key Laboratory of Public Health Safety, Ministry of Education, Shanghai, China
Abstract
Background: TB and HIV co-epidemic is a major public health problem in many parts of the world. But the prevalence of TB/
HIV co-infection was diversified among countries. Exploring the reasons of the diversity of TB/HIV co-infection is important
for public policy, planning and development of collaborative TB/HIV activities. We aimed to summarize the prevalence of TB
and HIV co-infection worldwide, using meta-analysis based on systematic review of published articles.
Methods: We searched PubMed, Embase, and Web of Science for studies of the prevalence of TB/HIV co-infection. We also
searched bibliographic indices, scanned reference lists, and corresponded with authors. We summarized the estimates using
meta-analysis and explored potential sources of heterogeneity in the estimates by metaregression analysis.
Results: We identified 47 eligible studies with a total population of 272,466. Estimates of TB/HIV co-infection prevalence
ranged from 2.93% to 72.34%; the random effects pooled prevalence of TB/HIV co-infection was 23.51% (95% CI 20.91–
26.11). We noted substantial heterogeneity (Cochran’s x2 = 10945.31, p,0.0001; I2 = 99.58%, 95% CI 99.55–99.61).
Prevalence of TB/HIV co-infection was 31.25%(95%CI 19.30–43.17) in African countries, 17.21%(95%CI 9.97–24.46) in Asian
countries, 20.11%(95%CI 13.82–26.39) in European countries, 25.06%(95%CI 19.28–30.84) in Latin America countries and
14.84%(95%CI 10.44–19.24) in the USA. Prevalence of TB/HIV co-infection was higher in studies in which TB diagnosed by
chest radiography and HIV diagnosis based on blood analyses than in those which used other diagnostic methods, and in
countries with higher prevalence HIV in the general population than in countries with lower general prevalence.
Conclusions: Our analyses suggest that it is necessary to attach importance to HIV/TB co-infection, especially screening of
TB/HIV co-infection using methods with high sensitivity, specificity and predictive values in the countries with high HIV/
AIDS prevalence in the general population.
Citation: Gao J, Zheng P, Fu H (2013) Prevalence of TB/HIV Co-Infection in Countries Except China: A Systematic Review and Meta-Analysis. PLoS ONE 8(5):
e64915. doi:10.1371/journal.pone.0064915
Editor: Jialin Charles Zheng, University of Nebraska Medical Center, United States of America
Received January 20, 2013; Accepted April 21, 2013; Published May 31, 2013
Copyright: ß 2013 Gao et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The study was sponsored by the Fundamental Research Funds for the Central Universities (grant number JJF201002). The funders had no role in study
design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing Interests: The authors have declared that no competing interests exist.
* E-mail: hfu@fudan.edu.cn
Introduction among HIV/AIDS population was 7.2% (4.2%–12.3%) [4]. So an
updated synthesis of the prevalence data from all other countries
The human immunodeficiency virus (HIV) pandemic presents a over the world would be important for public policy and planning
significant challenge to global tuberculosis (TB) control [1]. In and development of clinical services addressing the needs of TB
2011, 1.1 million (13%) of the 8.7 million people who developed and HIV/AIDS patients. It is also crucial to inform future projects
TB worldwide were HIV-positive [2]. TB is a leading killer among by identifying by identifying the reasons leading to the disparity of
people living with HIV. At least one in four deaths among people TB/HIV co-infection.
living with HIV can be attributed to TB [3]. To mitigate the dual We did a systematic review and meta-analysis to establish the
burden of TB/HIV in populations at risk of or affected by both prevalence of TB/HIV co-infection. We explored by meta
diseases, the World Health Organization (WHO) published a regression the reasons for variations between the primary studies
document on priority research questions in 2010 [3], and an and examined whether prevalence varied by year of publication,
updated policy on collaborative TB/HIV activities in 2012 [1], sex, study type, surveillance method, study size, study region, HIV
which emphasize the importance of surveillance of HIV among prevalence and TB prevalence of general population.
TB patients and surveillance of active TB patients among people
living with HIV in all countries. Methods
A wide range of estimates for the prevalence of TB/HIV co-
infection has been reported. However, to our knowledge, there Search Strategy and Selection Criteria
was only one study, which systematically evaluated the Chinese We searched PubMed, Embase and Web of Science with the
prevalence data of TB/HIV co-infection, indicated 0.9% (0.6%– term ‘‘co-infection and (tuberculosis or TB) and (HIV or AIDS or
1.4%) of TB patients were HIV infected, and the prevalence of TB human immunodeficiency virus or acquired immunodeficiency
PLOS ONE | www.plosone.org 1 May 2013 | Volume 8 | Issue 5 | e64915
Prevalence of TB/HIV Co-Infection: A Meta-Analysis
syndrome)’’ to identify English articles on studies of the prevalence infection among TB patients), place (by comparing population-
of TB/HIV co-infection until Dec 31, 2011. We also searched based studies with hospital-based studies), study type (by compar-
relevant reference lists and relevant journals by hand and ing cross-sectional studies with cohort studies), study size (as a
corresponded with authors. Our analyses accorded with the continuous variable),and estimates of HIV and TB prevalence in
preferred reporting items for systematic reviews and meta-analyses the general population of the study country (as a continuous
(PRISMA) guidelines (when appropriate) for a systematic review of variable). Information about the prevalence of TB and HIV
prevalence [5]. infection in the general population was obtained from the UN
Cross-sectional or cohort studies addressing the prevalence of Millennium Development Goals Database [12,13]. We chose the
HIV infection among TB patients or the prevalence of TB among national data that most closely matched the year of publication of
HIV/AIDS population were included. If the study was reported in the study. We entered only factors that we deemed significant
duplicate, the article published earlier was included. Investigations individually (p,0.05) into a multiple regression model to avoid
were included irrespective of diagnostic methods, but mostly model instability. We did all analyses in Stata (version 12.1) with
included chest radiography for tuberculosis and blood tests for the commands metan (for random-effects meta-analysis specifying
HIV. Diagnoses based on questionnaires (e.g. self-report of disease three variables: double-arcsine-transformed prevalence, Wilson
status) were also included. CIs, and prevalence ratios) and metareg (for meta regression).
Review articles, and studies in languages other than English or
studies conducted in China, with ,50 participants, focusing on Results
incidence rates, and addressing specific high risk populations (e.g.
injecting drug users or offenders), were excluded. Our searches returned a total of 8489 records. After removal of
Two reviewers (JLG and PPZ) independently extracted duplicates and initial screening, we reviewed 138 papers in full.
information about geographical location, year of publication, After exclusion of ineligible reports, our final sample was 47 studies
method of sample selection, sample size, mean age range, (n = 272,466) were included in this review [11,14–59] (Figure 1).
surveillance method, diagnostic method, and numbers diagnosed The characteristics of the included studies were shown in Table
with tuberculosis or HIV from every eligible study. Disagreement S1.
was resolved by consensus between the two reviewers or through Six reports each were from the USA (226,904)[11,17–19,22,54]
consultation with the corresponding author, when necessary. If and Brazil (4,841) [29,37,42,46,49,56], five were from Nigeria
needed, we sought further clarifications from the authors of (2,520) [21,32,47,52,55], four each were from Ethiopia (2,609)
relevant studies. [28,34,36,44] and Spain (10,809) [14,24,26,40], three were from
India (1,825) [27,45,59], two each were from Iran (721) [43,53],
Statistical Analysis South Africa (374) [23,50], Zambia (2,309) [16,35], and
We calculated prevalence estimates with the variance stabilizing Zimbabwe (2,049) [15,58], and one each was from Cambodia
double arcsine transformation [6]. Because the inverse variance (441) [25], Trinidad and Tobago (121) [41], Israel (1,059) [51],
weight in fixed-effects meta-analyses is suboptimum when dealing Netherland (13,269) [30], Singapore (184) [48], Tanzania (233)
with binary data with low prevalence. Additionally, the trans- [39], Thailand(54) [31], Togo(569) [57], UK(157) [20], Uk-
formed prevalence is weighted very slightly towards 50%, and raine(968) [33], and Vietnam(450) [38]. Twenty-nine reports
studies with prevalence of zero can thus be included in the screened HIV infection among TB patients (n = 22,884)[15–
analysis. We used the Wilson method [7] to calculate 95% CIs 17,19–23,26–28,31,33–36,38,41,42,48,50–52,54–59], and eleven
around these estimates because the asymptotic method produces reports screened TB patients among HIV/AIDS patients
intervals which can extend below zero [8]. We estimated (12,627)[14,25,32,39,40,43–47,53], and the screening method
heterogeneity between studies with Cochran’s Q (reported as x2 was unknown in the remaining seven (236,955)
and p values) and the I2 statistic, which describes the percentage of [11,18,24,29,30,37,49]. Tuberculosis was diagnosed by combina-
variation between studies that is due to heterogeneity rather than tion of chest radiography and sputum culture in 9 studies
chance [9,10]. Unlike Q, I2 does not inherently depend on the (n = 6,562) [15,28,31,34,36,39,42,50,58], by combination of chest
number of studies included; values of 25%, 50%, and 75% show radiography, sputum culture and PPD skin test in 1 studies (459)
low, moderate, and high degrees of heterogeneity, respectively. [43], by sputum culture in 17 studies (14,769)[14,16,17,22,25–
Because heterogeneity was high (I2.75%), we used random-effects 27,32,33,38,41,44,45,47,48,52,54], by PPD skin test in 1 study
models for summary statistics [10]. These models (in which the (262) [53], by chest radiography in 1 study (2072) [35], by
individual study weight is the sum of the weight used in a fixed- combination of chest radiography and PPD skin test in 1 studies
effects model and between-study variability) produce study weights (161) [23]; the method of diagnosis was unknown in the remaining
that mainly show between-study variation and thus provide close seventeen(248,181)[11,18–21,24,29,30,37,40,46,49,51,55–57,59].
to equal weighting. We did a sensitivity analyses by excluding one HIV/AIDS was diagnosed by blood in 25 studies (14,953)[15–
largest study [11]. 17,20,21,23,27,28,33–36,39,41,43,44,47,48,51,52,55–59], the
method of diagnosis was unknown in the remaining twenty-two
Heterogeneity studies (256,913) [11,14,18,19,22,24–26,29–
We further investigated potential sources of heterogeneity by 32,37,38,40,42,45,46,49,50,53,54].
arranging groups of studies according to potentially relevant For study types, four were prospective cohort studies (n = 9,561)
characteristics and by meta regression analysis, which attempts to [20,28,40,58], nine studies were retrospective cohort studies
relate differences in effect sizes to study characteristics. Factors (242,934)[11,18,22,30,42,49–51,54], and the remaining thirty four
examined both individually and in multiple-variable models were studies were cross sectional studies (19,971)[14–17,19,21,23–
year of publication, sex (by comparing male samples with female 27,29,31–39,41,43–48,52,53,55–57,59], fifteen studies were pop-
samples), diagnosis method (by comparing studies that diagnosed ulation-based (255,093)[11,18,24,26,29,30,36–40,42,49,54,58],
TB by chest radiography and HIV by blood with others studies), and the other 32 studies were hospital-based (17,373)[14–17,19–
screening method (by comparing studies that screening TB 23,25,27,28,31–35,41,43–48,50–53,55–57,59], twenty one report-
patients among HIV/AIDS population with screening HIV ed data for men and women respectively (men = 13,004 wom-
PLOS ONE | www.plosone.org 2 May 2013 | Volume 8 | Issue 5 | e64915
Prevalence of TB/HIV Co-Infection: A Meta-Analysis
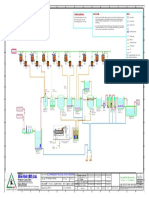
Figure 1. Study flow.
doi:10.1371/journal.pone.0064915.g001
en = 23,811) [15,17,18,20,28,30,33,36,38,39,44,46–48,52–55,57– prevalence did not change. Whereas the random-effects pooled
59]. TB/HIV co-infection prevalence raised to 23.89% (95% CI
Estimates of TB/HIV co-infection prevalence ranged from 20.21–27.56) with substantial heterogeneity (x2 = 10401.68,
2.93% to 72.34% (Figure 2); heterogeneity was substantial p,0.0001; I2 = 99.57%, 95% CI 99.53–99.60).
(x2 = 10945.31, p,0.0001; I2 = 99.58%, 95% CI 99.55–99.61). Meta regression analyses were used in order to explore source of
The random effects pooled prevalence of TB/HIV co-infection heterogeneity. In individual variable meta regression analysis, the
was 23.51% (95% CI 20.91–26.11). The random effects pooled prevalence of TB/HIV co-infection was higher in studies in which
TB/HIV co-infection prevalence among TB patients was chest radiography was used for TB diagnosis and HIV diagnosis
25.23%(95%CI 18.58–31.89) with substantial heterogeneity based on blood analyses (coefficient = 13.70, p = 0.001) than in
(x2 = 5478.67, p,0.0001; I2 = 99.49%, 95% CI 99.43–99.54). those in which other diagnostic methods were used; general
And the random effects pooled TB/HIV co-infection prevalence population prevalence of TB (coefficient = 0.03, p = 0.001) and
among HIV/AIDS patients was 23.30%(95%CI 16.69–29.91) HIV (coefficient = 1.76, p,0.001) were positively related to the
with substantial heterogeneity (x2 = 850.64, p,0.0001; prevalence of TB/HIV co-infection, but high general population
I2 = 98.82%, 95% CI 98.51–99.07). Prevalence of TB/HIV co- prevalence of TB was not related to the prevalence of TB/HIV co-
infection was 31.25%(95%CI 19.30–43.17) in African countries, infection after multivariate meta regression(Table 1).
17.21%(95%CI 9.97–24.46) in Asian countries, 20.11%(95%CI
13.82–26.39) in European countries, 25.06%(95%CI 19.28–30.84) Discussion
in Latin America countries and 14.84%(95%CI 10.44–19.24) in
the USA (Figure 3). Our systematic review and meta-analysis of TB/HIV co-
As part of our sensitivity analyses, we excluded one large infection identified 47 studies of 272,466 individuals except China.
tuberculosis study [11]; estimates of TB/HIV co-infection Our main findings were that, a high prevalence of TB/HIV co-
PLOS ONE | www.plosone.org 3 May 2013 | Volume 8 | Issue 5 | e64915
Prevalence of TB/HIV Co-Infection: A Meta-Analysis
Figure 2. Estimated prevalence of TB HIV co-infection by Screen methods.
doi:10.1371/journal.pone.0064915.g002
infection; TB/HIV co-infection prevalence was higher among TB patients and HIV/AIDS patients, especially in countries with high
patients than among HIV/AIDS patients, but which were not HIV prevalence or TB prevalence.
significantly different. Additionally, high general population Tuberculosis and HIV/AIDS can be worsened by each other.
prevalence of HIV/AIDS was related to higher prevalence of Tuberculosis is the most common opportunistic disease and cause
TB/HIV co-infection. These findings suggest that it should be of the death for those infected with HIV [60]. Similarly, HIV
paid more attention to screening TB/HIV co-infection among TB infection is one of the most important risk factors associated with
an increased risk of latent TB infection progressing to active TB
PLOS ONE | www.plosone.org 4 May 2013 | Volume 8 | Issue 5 | e64915
Prevalence of TB/HIV Co-Infection: A Meta-Analysis
Figure 3. Estimated prevalence of TB and HIV co-infection by Region.
doi:10.1371/journal.pone.0064915.g003
disease [61,62]. So the WHO’s Policy on collaborative TB/HIV prevalence of TB/HIV co-infection in our meta-analysis is
activities recommends a combination of measures to reduce the 23.51% (95% CI 20.91–26.11), which is higher than the rate
burden of TB among HIV-infected individuals [1]. These (13%) reported by WHO in 2011 [2]. The reasons may be that,
measures include intensified case finding, isoniazid preventive more than half studies (26 of 47 studies) were conducted in African
therapy, and infection control and antiretroviral therapy. The and Asian countries (Ethiopia, Nigeria, South Africa, Zambia,
PLOS ONE | www.plosone.org 5 May 2013 | Volume 8 | Issue 5 | e64915
Prevalence of TB/HIV Co-Infection: A Meta-Analysis
Table 1. Univariate and multivariate metaregression for prevalence of TB.
Metaregression coefficient (%)95%CI P
Univariate metaregression
Year of publication 20.27 20.88–0.34 0.381
Sex (male vs. female) 1.35 28.10–10.80 0.774
Diagnosis (TB by chest radiography and HIV by blood vs. other) 13.70 5.89–21.52 0.001
Screen (HIV from TB vs. TB from HIV) 24.34 212.65–3.97 0.302
Place (population-based vs. hospital-based) 25.24 212.45–1.97 0.152
Study type (cross-sectional vs. cohort) 1.43 23.61–6.46 0.575
Sample size ($500 vs. ,500) 20.21 27.09–6.67 0.952
Population prevalence of TB 0.03 0.01–0.05 0.001
Population prevalence of HIV/AIDS 1.76 1.14–2.37 ,0.001
Multivariate metaregression
Diagnosis (TB by chest radiography and HIV by blood vs. other) 3.32 2.46–12.10 0.035
Population prevalence of TB (per 100 000) 20.001 20.03–0.02 0.923
Population prevalence of HIV/AIDS (%) 1.62 0.71–2.53 0.001
doi:10.1371/journal.pone.0064915.t001
Zimbabwe, India and Thailand) with high general population associated with heterogeneity, such as history of TB and HIV/
prevalence of HIV and TB, while the HIV prevalence among AIDS, infectious routes of HIV or stages of AIDS, and future
people with TB is as high as 80% in some African countries [63]. research should describe samples in further detail.
However, this finding suggests case finding should be intensified Previous meta analysis of TB/HIV co-infection in China [4]
among TB patients and HIV/AIDS patients, because only 40% of reported a lower prevalence than that in our review, this may be
notified TB cases had a documented HIV test result in 2011 [2], because of low prevalence of HIV in China compared with that in
the percentage of people with TB who received an HIV test was countries where studies in our review were conducted. In addition,
just 26% in 2009 [63]. Gao and colleagues [4] reported lower summarized prevalence of
Our heterogeneity analyses generated several potentially HIV among TB patients for population-based studies. But our
important finding. Firstly, diagnostic method of chest radiography review didn’t find relationship between study place and prevalence
and blood was associated with significantly higher prevalence of of TB/HIV co-infection. An explanation could be demographic
TB/HIV co-infection than were other diagnostic methods. This factors of the study population, such as the gender and age
finding might be because of the higher sensitivity and specificity of distribution of subjects according to disease severity [66–68], but
chest radiography compared with sputum culture [64], which would need verification in future studies.
suggesting optimal TB algorithm to diagnose TB with high Because a meta-analysis has synthesized prevalence data of TB/
sensitivity, specificity and predictive values, that can be applied HIV co-infection in China [4],_ENREF_67 so we searched
across different settings and in patients with different TB and HIV prevalence data of TB/HIV co-infection in all other countries. But
disease burdens should be considered in the future. Secondly, only English articles were reviewed in our study, data published in
prevalence of TB/HIV co-infection was positively associated with other languages articles (e.g. French, Japanese) was unobtainable.
prevalence of HIV in the general population, which is consistent So collaboration of researchers from different language back-
with a previous study result that the rate of TB/HIV co-infection grounds is needed in the future. Second, due to the specific high-
depends on the prevalence of HIV infection in a community [36]. risk behaviors for TB and HIV infection, the selection of subjects
This result is potentially important from a public health might make results prone to potential selection bias even as we
perspective because it suggests it is should be paid more attention have excluded two studies performed among prisoners and
to screening TB/HIV co-infection among HIV/AIDS patients, injecting drug users. Another limitation of our systematic review
especially in countries with high HIV/AIDS prevalence of general is that, not all-necessary information, even age and HIV infection
population. This is also important from a preventive therapy routes stages of AIDS of the study population, could be obtained
because preventive TB therapy (any anti-TB drugs) reduces the from all included studies. Therefore, relevant stratified analyses
risk of active TB by 32% in people living with HIV [65], and could not be performed to disclose more detailed characteristics of
antiretroviral therapy reduces the individual risk of TB by 54% to the co-infection and its related risk factors.
92% and the population-based risk by 27% to 80% among people In conclusion, our analyses suggest that it is necessary to attach
living with HIV [1]. So HIV-infected patients should receive importance to HIV/TB co-infection, especially screening of TB/
antiretroviral therapy with optimal combination of antiretroviral HIV co-infection using methods with high sensitivity, specificity
and anti-TB therapy as early as possible. The substantial and predictive values in the countries with high HIV/AIDS
heterogeneity suggests that caution is necessary when pooled prevalence of general population. As prevalence of TB/HIV co-
estimates are used and emphasizes the need for careful description infection was positively associated with prevalence of HIV in the
of samples and diagnostic methods in surveys. Our sensitivity general population, and antiretroviral therapy is much helpful for
analyses showed that our overall results were not materially treatment of both diseases, so HIV-infected patients should receive
different when we excluded one study with largest sample size. antiretroviral therapy with as early as possible.
Other characteristics that we did not test might have been
PLOS ONE | www.plosone.org 6 May 2013 | Volume 8 | Issue 5 | e64915
Prevalence of TB/HIV Co-Infection: A Meta-Analysis
Supporting Information Author Contributions
Table S1 Studies of Prevalence of TB and HIV co- Conceived and designed the experiments: JLG PPZ HF. Performed the
experiments: JLG PPZ. Analyzed the data: JLG PPZ. Contributed
infection.
reagents/materials/analysis tools: JLG PPZ. Wrote the paper: JLG PPZ
(DOC) HF.
References
1. WHO (2012) WHO policy on collaborative TB/HIV activities: guidelines for 28. Yassin MA, Takele L, Gebresenbet S, Girma E, Lera M, et al. (2004) HIV and
national programmes and other stakeholders. Geneva: WHO Press. tuberculosis coinfection in the southern region of Ethiopia: a prospective
2. WHO (2012) Global tuberculosis report 2012. Geneva: WHO Press. epidemiological study. Scandinavian journal of infectious diseases 36: 670–673.
3. WHO TB/HIV Working Gropup (2010) Priority research questions for 29. De Carvalho LGM, Buani AZ, Zollner MSADC, Scherma AP (2006) Co-
TB:HIV in HIV-prevalent and resource-limited settings. Geneva: WHO Press. infection with Mycobacterium tuberculosis and human immunodeficiency virus:
4. Gao L, Zhou F, Li X, Jin Q (2010) HIV/TB co-infection in mainland China: a An epidemiological analysis in the city of Taubate, Brazil. 5 ed. Brazil:
meta-analysis. PloS one 5: e10736. Sociedade Brasileira de Pneumologia e Tisiologia. 424–429.
5. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, et al. (2009) The 30. Haar CH, Cobelens FG, Kalisvaart NA, Van der Have JJ, Van Gerven PJ, et al.
PRISMA statement for reporting systematic reviews and meta-analyses of studies (2006) HIV prevalence among tuberculosis patients in The Netherlands, 1993–
that evaluate health care interventions: explanation and elaboration. J Clin 2001: trends and risk factors. The international journal of tuberculosis and lung
Epidemiol 62: e1–34. disease : the official journal of the International Union against Tuberculosis and
6. Freeman MF, Tukey JW (1950) Transformations Related to the Angular and the Lung Disease 10: 768–774.
Square Root. Ann Math Stats 21: 607–611. 31. Jittimanee SX, Kateruttanakul P, Madigan EA, Jittimanee S, Phatkrathok S, et
7. Wilson EB (1927) Probable Inference, the Law of Succession, and Statistical al. (2006) Medical characteristics and tuberculosis treatment outcomes in an
Inference. J Am Stat Assoc 22: 209–212. urban tertiary hospital, Thailand. The Southeast Asian journal of tropical
8. Newcombe RG (1998) Two-Sided Confidence Intervals for The Single medicine and public health 37: 338–344.
Proportion: Comparison of Seven Methods. Stat Med 17: 857–872. 32. Salami AK, Katibi IA (2006) Human immunodeficiency virus-associated
9. Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. tuberculosis: pattern and trend in the University of Ilorin Teaching Hospital.
Stat Med 21: 1539–1558. African journal of medicine and medical sciences 35: 457–460.
10. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring 33. Van Der Werf MJ, Yegorova OB, Chentsova N, Chechulin Y, Hasker E, et al.
inconsistency in meta-analyses. BMJ 327: 557–560. (2006) Tuberculosis-HIV co-infection in Kiev City, Ukraine. 5 ed. United States:
11. Albalak R, O’Brien RJ, Kammerer JS, O’Brien SM, Marks SM, et al. (2007) Centers for Disease Control and Prevention (CDC). 766–768.
Trends in tuberculosis/human immunodeficiency virus comorbidity, United 34. Kassu A, Mengistu G, Ayele B, Diro E, Mekonnen F, et al. (2007) HIV and
States, 1993–2004. Archives of internal medicine 167: 2443–2452. intestinal parasites in adult TB patients in a teaching hospital in Northwest
12. UN. Millennium Development Goals database. Available: http://data.un.org/ Ethiopia. Tropical doctor 37: 222–224.
Data.aspx?d = MDG&f = seriesRowID%3a617. Accessed 2011 Dec 31. 35. Mwinga A, Mwananyambe N, Kanene C, Bultery M, Phiri C, et al. (2008)
13. UN. Millennium Development Goals database. Available: http://data.un.org/ Provider-initiated HIV testing and counseling of TB patients–Livingstone
Data.aspx?d = MDG&f = seriesRowID%3a729. Accessed 2011 Dec 31. District, Zambia, September 2004-December 2006. MMWR Morbidity and
14. Llibre JM, Tor J, Manterola JM, Carbonell C, Roset J (1992) Risk stratification mortality weekly report 57: 285–289.
for dissemination of tuberculosis in HIV-infected patients. The Quarterly 36. Datiko DG, Yassin MA, Chekol LT, Kabeto LE, Lindtjorn B (2008) The rate of
journal of medicine 82: 149–157. TB-HIV co-infection depends on the prevalence of HIV infection in a
15. Pozniak AL, MacLeod GA, Mahari M, Legg W, Weinberg J (1992) The community. United Kingdom. 266.
influence of HIV status on single and multiple drug reactions to antituberculous 37. Domingos MP, Caiaffa WT, Colosimo EA (2008) Mortality, TB/HIV co-
therapy in Africa. AIDS 6: 809–814. infection, and treatment dropout: Predictors of tuberculosis prognosis in Recife,
16. Chintu C, Bhat G, Luo C, Raviglione M, Diwan V, et al. (1993) Seroprevalence Pernambuco State, Brazil. 4 ed. Brazil: Fundacao Oswaldo Cruz. 887–896.
of human immunodeficiency virus type 1 infection in Zambian children with 38. Khue PM, Phuc TQ, Hung NV, Jarlier V, Robert J (2008) Drug resistance and
tuberculosis. The Pediatric infectious disease journal 12: 499–504. HIV co-infection among pulmonary tuberculosis patients in Haiphong City,
17. Greenberg BL, Weisfuse IB, Makki H, Adler J, el-Sadr W, et al. (1994) HIV-1 Vietnam. 7 ed. France: International Union against Tubercul. and Lung Dis.
seroprevalence in chest clinic and hospital tuberculosis patients in New York 763–768.
City, 1989–1991. AIDS 8: 957–962. 39. Ngowi BJ, Mfinanga SG, Bruun JN, Morkve O (2008) Pulmonary tuberculosis
18. CDC (1995) Co-incidence of HIV/AIDS and tuberculosis–Chicago, 1982– among people living with HIV/AIDS attending care and treatment in rural
1993. MMWR Morbidity and mortality weekly report 44: 227–231. northern Tanzania. BMC public health 8: 341.
19. Gampper SNR, George JA, Carter EJ, Jesdale BM, Flanigan TP, et al. (1998) 40. Velasco M, Castilla V, Cervero M, Sanz J, Condes E, et al. (2008) The changing
Co-infection with Mycobacterium tuberculosis and HIV in high risk clinical care pattern of tuberculosis and HIV co-infection in immigrants and Spaniards in the
settings in Rhode Island. 2 ed. United Kingdom. 221–229. last 20 years. 4 ed. United Kingdom: Blackwell Publishing Ltd. 227–233.
20. Marshall BG, Mitchell DM, Shaw RJ, Marais F, Watkins RM, et al. (1999) HIV 41. Baboolal S, Millet J, Akpaka PE, Ramoutar D, Rastogi N (2009) First insight
and tuberculosis co-infection in an inner London hospital–a prospective into Mycobacterium tuberculosis epidemiology and genetic diversity in Trinidad
anonymized seroprevalence study. The Journal of infection 38: 162–166. and Tobago. Journal of clinical microbiology 47: 1911–1914.
21. Onipede AO, Idigbe O, Ako-Nai AK, Omojola O, Oyelese AO, et al. (1999) 42. Coelho AG, Zamarioli LA, Perandones CA, Cuntiere I, Waldman EA (2009)
Sero-prevalence of HIV antibodies in tuberculosis patients in Ile-Ife, Nigeria. Characteristics of pulmonary tuberculosis in a hyperendemic area: the city of
East African medical journal 76: 127–132. Santos, Brasil. Jornal brasileiro de pneumologia : publicacao oficial da Sociedade
22. Sotir MJ, Parrott P, Metchock B, Bock NN, McGowan JE Jr, et al. (1999) Brasileira de Pneumologia e Tisilogia 35: 998–1007.
Tuberculosis in the inner city: impact of a continuing epidemic in the 1990s. 43. Davarpanah MA, Rafiee GH, Mehrabani D (2009) The prevalence of M.
Clinical infectious diseases : an official publication of the Infectious Diseases tuberculosis infection and disease in HIV positive individuals in Shiraz, Southern
Society of America 29: 1138–1144. Iran. 2 ed. United Arab Emirates: Iranian Red Crescent Society (PO Box: 2330,
23. Madhi SA, Huebner RE, Doedens L, Aduc T, Wesley D, et al. (2000) HIV-1 co- Dubai, UAE, United Arab Emirates). 199–202.
infection in children hospitalised with tuberculosis in South Africa. 5 ed. France: 44. Deribew A, Tesfaye M, Hailmichael Y, Negussu N, Daba S, et al. (2009)
International Union against Tubercul. and Lung Dis. 448–454. Tuberculosis and HIV co-infection: its impact on quality of life. Health and
24. Mayoral Cortes JM, Garcia Fernandez M, Varela Santos MC, Fernandez quality of life outcomes 7: 105.
Merino JC, Garcia Leon J, et al. (2001) Incidence of pulmonary tuberculosis and 45. Ghiya R, Naik E, Casanas B, Izurieta R, Marfatia Y (2009) Clinico-
HIV coinfection in the province of Seville, Spain, 1998. European journal of epidemiological profile of HIV/TB coinfected patients in Vadodara, Gujarat.
epidemiology 17: 737–742. Indian journal of sexually transmitted diseases 30: 10–15.
25. Kimerling ME, Schuchter J, Chanthol E, Kunthy T, Stuer F, et al. (2002) 46. Gutierrez EB, Gomes V, Picone CM, Suga H, Atomiya AN (2009) Active
Prevalence of pulmonary tuberculosis among HIV-infected persons in a home tuberculosis and Mycobacterium tuberculosis latent infection in patients with
care program in Phnom Penh, Cambodia. The international journal of HIV/AIDS. HIV medicine 10: 564–572.
tuberculosis and lung disease : the official journal of the International Union 47. Iliyasu Z, Babashani M (2009) Prevalence and predictors of tuberculosis
against Tuberculosis and Lung Disease 6: 988–994. coinfection among HIV-seropositive patients attending the Aminu Kano
26. Godoy P, Dominguez A, Alcaide J, Camps N, Jansa JM, et al. (2004) Teaching Hospital, northern Nigeria. Journal of epidemiology/Japan Epidemi-
Characteristics of tuberculosis patients with positive sputum smear in Catalonia, ological Association 19: 81–87.
Spain. European journal of public health 14: 71–75. 48. Low SY, Eng P (2009) Human immunodeficiency virus testing in patients with
27. Gothi D, Joshi JM (2004) Clinical and laboratory observations of tuberculosis at newly-diagnosed tuberculosis in Singapore. Singapore medical journal 50: 479–
a Mumbai (India) clinic. Postgraduate medical journal 80: 97–100. 481.
PLOS ONE | www.plosone.org 7 May 2013 | Volume 8 | Issue 5 | e64915
Prevalence of TB/HIV Co-Infection: A Meta-Analysis
49. Santos Mde L, Ponce MA, Vendramini SH, Villa TC, Santos NS, et al. (2009) Harare, Zimbabwe. The international journal of tuberculosis and lung disease :
The epidemiological dimension of TB/HIV co-infection. Revista latino- the official journal of the International Union against Tuberculosis and Lung
americana de enfermagem 17: 683–688. Disease 15: 1390–1396.
50. van Well GT, Paes BF, Terwee CB, Springer P, Roord JJ, et al. (2009) Twenty 59. Sawant SS, Agrawal SR, Shastri JS, Pawaskar M, Kadam P (2011) Human
years of pediatric tuberculous meningitis: a retrospective cohort study in the immunodeficiency virus infection among tuberculosis patients in mumbai.
western cape of South Africa. Pediatrics 123: e1–8. Journal of laboratory physicians 3: 12–14.
51. Bendayan D, Littman K, Polansky V (2010) Active tuberculosis and human 60. Friedland G, Churchyard GJ, Nardell E (2007) Tuberculosis and HIV
immunodeficiency virus co-infection in Israel: a retrospective study. The Israel coinfection: current state of knowledge and research priorities. J Infect Dis
Medical Association journal : IMAJ 12: 100–103. 196 Suppl 1: S1–3.
52. Erhabor O, Jeremiah ZA, Adias TC, Okere C (2010) The prevalence of human 61. Meya DB, McAdam KP (2007) The TB pandemic: an old problem seeking new
immunodeficiency virus infection among TB patients in Port Harcourt Nigeria. solutions. J Intern Med 261: 309–329.
HIV/AIDS 2: 1–5. 62. Girardi E, Raviglione MC, Antonucci G, Godfrey-Faussett P, Ippolito G (2000)
53. Jam S, Sabzvari D, SeyedAlinaghi S, Fattahi F, Jabbari H, et al. (2010) Impact of the HIV epidemic on the spread of other diseases: the case of
Frequency of Mycobacterium tuberculosis infection among Iranian patients with tuberculosis. Aids 14 Suppl 3: S47–56.
HIV/AIDS by PPD test. Acta medica Iranica 48: 67–71. 63. UNAIDS (2010) Global report: UNAIDS report on the global AIDS epidemic
54. Rodwell TC, Barnes RF, Moore M, Strathdee SA, Raich A, et al. (2010) HIV- 2010. Geneva: WHO Press.
tuberculosis coinfection in Southern California: evaluating disparities in disease 64. van’t Hoog AH, Meme HK, Laserson KF, Agaya JA, Muchiri BG, et al. (2012)
burden. American journal of public health 100 Suppl 1: S178–185. Screening strategies for tuberculosis prevalence surveys: the value of chest
55. Pennap G Fau - Makpa S, Makpa S Fau - Ogbu S, Ogbu S (2010) Sero- radiography and symptoms. Plos One 7: e38691.
prevalence of HIV infection among tuberculosis patients in a rural tuberculosis 65. Akolo C, Adetifa I, Shepperd S, Volmink J (2010) Treatment of latent
referral clinic in northern Nigeria. tuberculosis infection in HIV infected persons. Cochrane Database Syst Rev:
56. Brunello ME, Chiaravalloti Neto F, Arcencio RA, Andrade RL, Magnabosco CD000171.
GT, et al. (2011) Areas of vulnerability to HIV/TB co-infection in Southeastern 66. Carvalho BM, Monteiro AJ, Pires Neto Rda J, Grangeiro TB, Frota CC (2008)
Brazil. Revista de saude publica 45: 556–563. Factors related to HIV/tuberculosis coinfection in a Brazilian reference hospital.
57. Dagnra AY, Adjoh K, Tchaptchet Heunda S, Patassi AA, Sadzo Hetsu D, et al. Braz J Infect Dis 12: 281–286.
(2011) Prevalence of HIV-TB co-infection and impact of HIV infection on 67. Girardi E, Goletti D, Antonucci G, Ippolito G (2001) Tuberculosis and HIV: a
pulmonary tuberculosis outcome in Togo. 5 ed. France: Societe de Pathologie deadly interaction. J Biol Regul Homeost Agents 15: 218–223.
Exotique (25 rue du Docteur Roux, Paris 75724, France). 342–346. 68. Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, et al. (2003) The
58. Macpherson P, Dimairo M, Bandason T, Zezai A, Munyati SS, et al. (2011) Risk growing burden of tuberculosis: global trends and interactions with the HIV
factors for mortality in smear-negative tuberculosis suspects: a cohort study in epidemic. Archives of internal medicine 163: 1009–1021.
PLOS ONE | www.plosone.org 8 May 2013 | Volume 8 | Issue 5 | e64915
You might also like
- Case Study of La Posta Mexican RestaurantsDocument1 pageCase Study of La Posta Mexican RestaurantsFatima Atiq80% (5)
- Power Wizard 2.1: CTA CTB CTCDocument2 pagesPower Wizard 2.1: CTA CTB CTCOsanebi Chukwudi Lucky80% (10)
- BS 57 (1951)Document23 pagesBS 57 (1951)dapsiduNo ratings yet
- Crochet Tunisian PrimerDocument7 pagesCrochet Tunisian PrimerVerónica Bertero100% (4)
- Astm E2352 - 1 (En) PDFDocument14 pagesAstm E2352 - 1 (En) PDFSainath AmudaNo ratings yet
- Prevalence and Determinants of Human Immunodeficiency Virus and Tuberculosis Co-Infection at Kampala International University Teaching HospitalDocument6 pagesPrevalence and Determinants of Human Immunodeficiency Virus and Tuberculosis Co-Infection at Kampala International University Teaching HospitalKIU PUBLICATION AND EXTENSIONNo ratings yet
- HZVDocument15 pagesHZVMarviane ThenNo ratings yet
- Jurnal 2Document16 pagesJurnal 2Edwin Pasha Jr.No ratings yet
- HCW Vs Adult Influenza IncidenceDocument9 pagesHCW Vs Adult Influenza Incidencereza_adrian_2No ratings yet
- Prognostic Score To Predict Mortality During TB Treatment in TBHIV Co-Infected PatientsDocument12 pagesPrognostic Score To Predict Mortality During TB Treatment in TBHIV Co-Infected PatientsGani ArlondNo ratings yet
- Ali2016 Article OutcomesOfTBTreatmentInHIVCo-iDocument9 pagesAli2016 Article OutcomesOfTBTreatmentInHIVCo-itishaNo ratings yet
- Njie-Khan2021 Article PrevalenceOfTuberculosisAndMenDocument7 pagesNjie-Khan2021 Article PrevalenceOfTuberculosisAndMenLinh NguyenNo ratings yet
- Ambo UniversityDocument12 pagesAmbo UniversityArarsa TolasaNo ratings yet
- Status of Tuberculosis-Related Stigma and Associated Factors: A Cross-Sectional Study in Central ChinaDocument7 pagesStatus of Tuberculosis-Related Stigma and Associated Factors: A Cross-Sectional Study in Central ChinaCharis MurwadiNo ratings yet
- J Infect Dis. 2022 Aug 12 - 226 - Suppl 1 - S17-S21.Document19 pagesJ Infect Dis. 2022 Aug 12 - 226 - Suppl 1 - S17-S21.HemerobibliotecaHospitalNo ratings yet
- RESEARCH ARTICLE Detecting Spatial Clusters of HIV and Hepatitis CoinfectionsDocument16 pagesRESEARCH ARTICLE Detecting Spatial Clusters of HIV and Hepatitis CoinfectionsDicky rahadianNo ratings yet
- Ofx 137Document7 pagesOfx 137Sheila Alcalde RNo ratings yet
- Re Ections On 40 Years of AIDS: PerspectiveDocument8 pagesRe Ections On 40 Years of AIDS: PerspectiveANGEL OMAR SANTANA AVILANo ratings yet
- Medi 102 E32811Document9 pagesMedi 102 E32811dani catriaNo ratings yet
- Co-Infection of Tuberculosis and Parasitic Diseases in Humans A Systematic ReviewDocument12 pagesCo-Infection of Tuberculosis and Parasitic Diseases in Humans A Systematic ReviewThamile CaetanoNo ratings yet
- Directly Observed TreatmentDocument9 pagesDirectly Observed TreatmentNovelia CarolinNo ratings yet
- Fetch ObjectDocument7 pagesFetch ObjectBilly UntuNo ratings yet
- Marzieh Shareizaei - Et.alDocument7 pagesMarzieh Shareizaei - Et.alkang.asep008No ratings yet
- Reference ThesisDocument13 pagesReference ThesisGhina SalsabilaNo ratings yet
- 2017 Article 2662Document11 pages2017 Article 2662Dhani KurniawanNo ratings yet
- The Global Epidemiology of Bacterial Vaginosis A Systematic ReviewDocument19 pagesThe Global Epidemiology of Bacterial Vaginosis A Systematic ReviewcheracapNo ratings yet
- Tuberculosis Vih EthiopiaDocument9 pagesTuberculosis Vih Ethiopiajulma1306No ratings yet
- Antiretroviral Therapy For Prevention of HIV Transmission: Implications For EuropeDocument23 pagesAntiretroviral Therapy For Prevention of HIV Transmission: Implications For EuropenukarevaNo ratings yet
- September CDC HAISDocument11 pagesSeptember CDC HAISnoval firdausNo ratings yet
- Syphilis Epidemic Among Men Who Have Sex With Men: A Global Systematic Review and Meta-Analysis of Prevalence, Incidence, and Associated FactorsDocument11 pagesSyphilis Epidemic Among Men Who Have Sex With Men: A Global Systematic Review and Meta-Analysis of Prevalence, Incidence, and Associated FactorsEldie RahimNo ratings yet
- HIV Prevalence in Suspected Ebola Cases During The 2014 - 2016 Ebola Epidemic in Sierra LeoneDocument4 pagesHIV Prevalence in Suspected Ebola Cases During The 2014 - 2016 Ebola Epidemic in Sierra LeoneJairo Castro MaestreNo ratings yet
- naturaleza y consecuencia de las coinfeccionesDocument7 pagesnaturaleza y consecuencia de las coinfeccionesSEVILLA RAMIREZ JOSE MANUELNo ratings yet
- WHO Position Paper Dengue 2016 ReferencesDocument17 pagesWHO Position Paper Dengue 2016 Referencessingularity24601_302No ratings yet
- HIV Epidemiology Among Female Sex Workers and Their Clients in The Middle East and North Africa: Systematic Review, Meta-Analyses, and Meta-RegressionsDocument30 pagesHIV Epidemiology Among Female Sex Workers and Their Clients in The Middle East and North Africa: Systematic Review, Meta-Analyses, and Meta-RegressionsLuís MiguelNo ratings yet
- Djimeu Published Replication PlanDocument17 pagesDjimeu Published Replication PlanVishalvishaldograNo ratings yet
- 19 Ninan EtalDocument6 pages19 Ninan EtaleditorijmrhsNo ratings yet
- CommunityViralLoadinHIV PDFDocument9 pagesCommunityViralLoadinHIV PDFIsaias PrestesNo ratings yet
- 10 1111@tbed 13621Document37 pages10 1111@tbed 13621onlyhyesun119No ratings yet
- Multidrug-Resistant Tuberculosis in Uzbekistan: Results of A Nationwide Survey, 2010 To 2011Document12 pagesMultidrug-Resistant Tuberculosis in Uzbekistan: Results of A Nationwide Survey, 2010 To 2011IsoqjonivichNo ratings yet
- Epidemiological Risk Factors For Adult Dengue in Singapore: An 8-Year Nested Test Negative Case Control StudyDocument9 pagesEpidemiological Risk Factors For Adult Dengue in Singapore: An 8-Year Nested Test Negative Case Control StudydouwesdNo ratings yet
- Epidemiology, Clinical Manifestations, and Outcomes of Streptococcus Suis Infection in HumansDocument10 pagesEpidemiology, Clinical Manifestations, and Outcomes of Streptococcus Suis Infection in HumansMark ReinhardtNo ratings yet
- Chapter II ReviewDocument5 pagesChapter II ReviewPardeepCharlyNo ratings yet
- Art GEBADocument8 pagesArt GEBAJhonathan Andres Garcia FiallosNo ratings yet
- Risk Factors For Herpes Zoster Infection: A Meta-Analysis: Review ArticleDocument8 pagesRisk Factors For Herpes Zoster Infection: A Meta-Analysis: Review Articleyenny handayani sihiteNo ratings yet
- Multidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceDocument7 pagesMultidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceAldy RinaldiNo ratings yet
- Spatial Analysis of TuberculosisDocument77 pagesSpatial Analysis of TuberculosisChrlzs BlgNo ratings yet
- HIV Systematic Review and Meta AnalysisDocument13 pagesHIV Systematic Review and Meta AnalysisSanti IskandarNo ratings yet
- Survival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorDocument10 pagesSurvival Analysis of Adult Tuberculosis Disease: Olurotimi Bankole Ajagbe, Zubair Kabair, Terry O'ConnorGetachew GemedaNo ratings yet
- Assessment of Psychosocial and Economic Adaptation Among People Living With Hivaids in NigeriaDocument74 pagesAssessment of Psychosocial and Economic Adaptation Among People Living With Hivaids in NigeriaDaniel ObasiNo ratings yet
- The Effectiveness and Cost-Effectiveness of Screening For HIV in Migrants in The EU/EEA: A Systematic ReviewDocument23 pagesThe Effectiveness and Cost-Effectiveness of Screening For HIV in Migrants in The EU/EEA: A Systematic ReviewAlexandra PaunNo ratings yet
- Plos Medicine /Article/Crossref/I /Article/Tw Itter/Info /Article/Metrics/Inf Info:Doi/10.1371/J Patient Adher 1185260400000Document25 pagesPlos Medicine /Article/Crossref/I /Article/Tw Itter/Info /Article/Metrics/Inf Info:Doi/10.1371/J Patient Adher 1185260400000khattak_i89No ratings yet
- Ofy 017Document9 pagesOfy 017Zakia DrajatNo ratings yet
- Interventions To Prevent Sexually Transmitted Infections, Including HIV InfectionDocument15 pagesInterventions To Prevent Sexually Transmitted Infections, Including HIV Infectionursula_ursulaNo ratings yet
- Paper TBDocument24 pagesPaper TBnachersNo ratings yet
- 1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1Document9 pages1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1dewi ayu wulandariNo ratings yet
- EpidemiologyDocument7 pagesEpidemiologyInoxcent MoonNo ratings yet
- Example of Research Paper About HivDocument6 pagesExample of Research Paper About Hivc9qb8gy7100% (3)
- Jurnal 10 HariantoDocument7 pagesJurnal 10 Hariantoaryzamelindah channelNo ratings yet
- Pamj 27 48Document7 pagesPamj 27 48JihanNo ratings yet
- Jia2 25392Document10 pagesJia2 25392Herpriiy BatukhNo ratings yet
- Captura de Pantalla 2024-01-23 A La(s) 11.26.43Document9 pagesCaptura de Pantalla 2024-01-23 A La(s) 11.26.43Dany MorBenNo ratings yet
- Awareness of Dengue and Practice of Dengue Control Among1Document6 pagesAwareness of Dengue and Practice of Dengue Control Among1rjohn 7No ratings yet
- HIV Screening USPTFDocument21 pagesHIV Screening USPTFhivpolicyyesNo ratings yet
- SSP Assignment Problems - FinalDocument2 pagesSSP Assignment Problems - FinalVadivelan AdaikkappanNo ratings yet
- Lesson Plan PatrickDocument4 pagesLesson Plan PatrickPatrick Jerome SilvanoNo ratings yet
- Electronics and Communication Engineering Sample ThesisDocument7 pagesElectronics and Communication Engineering Sample Thesiseifvhpugg100% (1)
- Research Methods For Commerce Lab Practical File "BRM Lab" BBA (M1) - BBA 213Document67 pagesResearch Methods For Commerce Lab Practical File "BRM Lab" BBA (M1) - BBA 213Mankeerat Singh ChannaNo ratings yet
- LIT - Sullair S-Energy 25-40hp Brochure - SAPSEN2540201904-6 - ENDocument8 pagesLIT - Sullair S-Energy 25-40hp Brochure - SAPSEN2540201904-6 - ENKrist San QNo ratings yet
- Persuasive Writing Assessment RubricDocument2 pagesPersuasive Writing Assessment Rubricapi-523656984No ratings yet
- PoonamDocument54 pagesPoonamCH Rajan GujjarNo ratings yet
- BeachesDocument32 pagesBeachesnympheasandhuNo ratings yet
- CiabattaDocument4 pagesCiabattaTarak ZayaniNo ratings yet
- WH2009 WaterHorseCatalogDocument132 pagesWH2009 WaterHorseCatalogAiko FeroNo ratings yet
- Gabet Response To Motion To CompelDocument13 pagesGabet Response To Motion To CompelKenan FarrellNo ratings yet
- Alim Knit (BD) LTD.: Recommended Process Flow DiagramDocument1 pageAlim Knit (BD) LTD.: Recommended Process Flow DiagramKamrul HasanNo ratings yet
- Roles of Physiotherapy in Intensive Care Unit (Document28 pagesRoles of Physiotherapy in Intensive Care Unit (Chukwuemeka ChidogoNo ratings yet
- Dvp-Es2 Ss2 Sa2 Sx2-Program o en 20110302Document609 pagesDvp-Es2 Ss2 Sa2 Sx2-Program o en 20110302puskyboyNo ratings yet
- SSC Gr10 ICT Q4 Module 2 WK 2 - v.01-CC-released-7June2021Document16 pagesSSC Gr10 ICT Q4 Module 2 WK 2 - v.01-CC-released-7June2021Vj AleserNo ratings yet
- PFW - Vol. 23, Issue 08 (August 18, 2008) Escape To New YorkDocument0 pagesPFW - Vol. 23, Issue 08 (August 18, 2008) Escape To New YorkskanzeniNo ratings yet
- Mother Gooses MelodyDocument49 pagesMother Gooses MelodyDominick GraceNo ratings yet
- Project WorkDocument6 pagesProject WorkNurbek YaxshimuratovNo ratings yet
- The Psychological Aspects of Cinematography and Its ImpactDocument21 pagesThe Psychological Aspects of Cinematography and Its Impactanastasiapiven7No ratings yet
- BUMA 20053 BUSINESS RESEARCH ModuleDocument59 pagesBUMA 20053 BUSINESS RESEARCH ModuleJanell Aganan100% (1)
- Rev29jan2019oftemplate OSHprogram Asof 290119Document12 pagesRev29jan2019oftemplate OSHprogram Asof 290119GelinaNo ratings yet
- VarahamihiraDocument6 pagesVarahamihiraSTAR GROUPS100% (1)
- SUBHIKSHADocument12 pagesSUBHIKSHAAkshat ChaturvediNo ratings yet
- ĐỀ 2Document4 pagesĐỀ 2Khôi Nguyên PhạmNo ratings yet
- 21st Century WeaponsDocument6 pages21st Century WeaponsSaqibMahmoodNo ratings yet