Professional Documents
Culture Documents
Access Flow Reduction For Cardiac Failure
Access Flow Reduction For Cardiac Failure
Uploaded by
Luis Rodriguez PratoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Access Flow Reduction For Cardiac Failure
Access Flow Reduction For Cardiac Failure
Uploaded by
Luis Rodriguez PratoCopyright:
Available Formats
JVA
J Vasc Access 2016; 17 (Suppl 1): S60-S63
DOI: 10.5301/jva.5000517
ISSN 1129-7298 ORIGINAL ARTICLE
Access flow reduction for cardiac failure
Pierre Bourquelot
Angioaccess Surgery Department, Clinique Jouvenet, Paris - France
Abstract
High-flow in hemodialysis arteriovenous angioaccesses is frequent. It may result in high-output cardiac fail-
ure, which should be prevented by fistula flow reduction. The most frequently reported flow reduction pro-
cedure is banding but immediate and long-term results are questionable. Alternative techniques are related
here with personal results. Juxta-anastomosis “Proximal Radial Artery Ligation” (PRAL) is a very simple and
effective reduction technique for side-to-end radio-cephalic fistulas (82 patients; reduction rate [RR]: 54%
± 19%). For brachial artery-based fistulas flow reduction two variants of Revision Using Distal Inflow (RUDI)
procedures are used: 1) RUDI-1 using a polytetrafluoroethylene (PTFE) graft or a greater saphenous vein,
which we first described in 1989 as “Distal Report of the Arterial Inflow” (35 patients; RR: 53% ± 18%),
2) RUDI-2 procedure, “Transposition of the Radial Artery”, which we described in 2009 (47 patients; RR:
66% ± 14%).
Keywords: Arteriovenous fistula, Banding, Cardiac failure, Fistula ligation, Flow reduction, High-flow, RUDI,
Transposition of the radial artery
Introduction • Closure of the AVF when the creation of a more distal
AVF is possible, which is rare, or after successful kidney
Arteriovenous fistula (AVF) creation induces decreased transplantation.
peripheral resistance and increased cardiac output, blood • Banding of the vein to reduce its caliber, but this proce-
volume, pulmonary flow and pressure. dure rarely results in actual flow reduction.
Patients with large upper arm shunts are particularly at
risk of high-output cardiac failure (HOCF). With time, car- We routinely used the following methods (5, 6) to reduce high
diac hypertrophy and four chamber enlargement will take flow AVFs: juxta-anastomosis Proximal Radial Artery Ligation
place, and pulmonary hypertension will develop as well as (PRAL) for distal AVF (7), Distal Report of Arterial Inflow (RUDI-1)
AVF-related coronary hypoperfusion resulting in ischemic (5) and more recently, Transposition of the Radial Artery (RUDI-2)
cardiomyopathy. Treatment includes fistula flow reduction (8) for proximal AVF. These methods and their results are de-
or fistula ligation. scribed here.
For prevention of HOCF, access flow should be assessed
repeatedly and those with outputs >1.5 L/min should be AVF flow measurement
monitored closely for development of heart failure. Some
authors (1-2) consider surgical reduction of upper arm Although a flow rate of 300 to 500 mL/min is sufficient
shunts where flows average 1700 mL/min while others (3-4) to ensure proper hemodialysis, the actual AVF flow is usually
insist on the high predictive power for HOCF occurrence of much higher.
blood access flow (Qa) cut-off values >2.000 mL/min. Summarizing the current studies of Qa measurements
Apart from proceeding as distal as possible, there is no made with duplex scanning in upper arm fistula (cumulative
reliable way to limit blood flow when creating an AVF. total 227 patients) gives a mean Qa that ranges from 1,126
The standard procedures to reduce (Qa) are: to 1,722 mL/min. Based on these studies, at least 15% of
patients may have Qa greater than 2 to 2.5 L/min (9).
In a prospective evaluation of 45 autologous AVFs using
the ultrasound dilution technique (Transonic) the Qa of prox-
Accepted: December 25, 2015 imal cephalic AVFs was approximately twice as high as the
Published online: March 6, 2016 Qa of distal cephalic AVFs, 1,285 ± 652 vs 647 ± 331 mL/min,
respectively (10).
Corresponding author:
Pierre Bourquelot
Clinique Jouvenet High blood flow AVF
6 Square Jouvenet
F75014 Paris, France The magnitude of AVF blood flow is dependent on the
pierre@bourquelot.fr following:
© 2016 Wichtig Publishing
Bourquelot S61
1. The initial diameter of the artery, while the role of the
initial caliber of the anteriovenous (AV) anastomosis re-
mains controversial, at least in the wrist. As known from
congenital AVF, the more proximal the AVF, the earlier
and more important is the cardiac overload. In fact, flow
of recently created accesses have been shown to be up
to twice as high in upper arm fistulas compared with low-
er arm fistulas (1,336 ± 689 vs. 645 ± 332 mL/min).
2. The ability of the artery to dilate with time. Among ther-
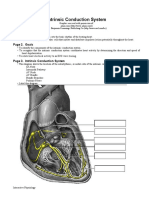
apeutic AVFs, the distal radial to cephalic AVF, which has Fig. 1 - Juxta-anastomosis Proximal Radial Artery Ligation (PRAL).
the longest life, may also be involved in high blood flow.
High flow appears infrequently in two kinds of angioaccesses: >2 L/min in 50 adult male patients were disappointing (14).
Access flow was initially reduced by >50% but a recurrent
• distal basilic-to-ulnar AVF, probably due to the small di- high flow (>2 L/min) developed in 52% of the patients during
ameter of the ulnar artery; the observation period (12 months). Young age and an access
• prosthetic arteriovenous bridge-graft: probably because flow >1 L/min immediately after banding were risk factors for
of the early venous anastomosis stenosis. recurrent high flow.
These factors, in addition to the failure of previous banding
Currently, there is no definition of when a fistula flow is too that we observed in referred high blood-flow AVF patients, led
high. According to the different authors the upper limit of us to abandon this technique.
flow that is tolerable varies between 1,500 and 2,000 mL/ Arterioarterial by-pass. We gave up early on the project
min. (1, 4, 11). to change high flow AVF into arterioarterial by-pass. The the-
oretical advantage would have been a marked reduction of
Standard flow reduction methods basic blood flow, capable to increase highly after cannulation
for hemodialysis. The 10 artery-to-artery by-passes which we
When high flow is important and/or when a cardiac over- had created in the upper arm were complicated with early
load is observed, a flow reduction is necessary. thrombosis, distal artery embolism and painful dialysis due to
Closure of the high flow AVF should be done after successful high pressure intra-arterial reinjection.
kidney transplantation or when it is possible to move to perito-
neal dialysis. Effective flow reduction methods
Replacement of a proximal AVF by a more distal perma-
nent access on either of both upper limbs is possible in a few Juxta-anastomosis proximal radial artery ligation
cases. Obviously in case of multiple fistulas, the ligation tech-
nique is also indicated. Juxta-anastomosis Proximal Radial Artery Ligation (PRAL)
The popular elbow side-to-side and the perforating vein (Fig. 1) that we have described in 1989 (5), applies to fore-
arteriovenous Gracz’s fistula deserves many criticisms: retro- arm side-to-end (radial-to-cephalic) high-flow AVFs. Results in
grade flow to the forearm may induce painful and ischemic adults and children were reported in 2010 (7).
distal venous hypertension; perfusion of the profunda brachial Anderson in 1977 was the first who observed that two-
veins via the perforating vein will not give any chance of vein thirds of the inflow in a side-to-end fistula at wrist is supplied
cannulation; the same applies to the basilic vein, which is not by the proximal artery, and that the remaining one-third
to be punctured without a serious risk of brachial artery dam- comes from retrograde flow through the distal artery. We
age, unless previous surgical superficialization; arterial distal observed similarly that a distal AVF could remain patent and
ischemia, occurring very frequently in diabetics and cardiac sufficient for hemodialysis, after spontaneous proximal artery
overload, are the major unrecognized risks of this technique. thrombosis.
Closure of the anastomosis straight above the artery is to be Before undertaking PRAL, it is necessary to check for out-
done and a new side-to-end “only one downstream cephalic or flow venous stenosis, which could lead to subsequent fistula
superficialized basilic vein anastomosis” is performed. thrombosis. Retrograde flow from the distal radial artery and
Banding was traditionally the method of choice to reduce the palmar arch is proved on the basis of a permanent, with
AVF flow. Objections to banding are multiple: systolic reinforcement, Doppler audible signal.
The surgical procedure is very simple. A 3-weeks anticoag-
1) peroperative flowmeter is required but the previous sur- ulation therapy is recommended post-operatively to reduce
gical dissection frequently induces an arterial spasm, the risks of extensive thrombosis of the radial artery. Eighty-
2) reduction of vascular caliber must be important and two (mean age: 45 years, range: 5-82 years) whose high-flow
precise to avoid the risk of either persistent high flow or AVF was reduced by this method had 54 ± 19 (% ± SD) mean
thrombosis. reduction rate. Maximum reduction rate was observed on
highest flows.
Early successful results with banding have been published High flow had persisted or reappeared postoperatively in
by two different teams (12, 13), but recently the long-term a few cases. Associated ligation of the distal artery reducing
results of banding in brachial artery-based fistulas with flow AVF in-flow to small branches from ulnar and interosseous
© 2016 Wichtig Publishing
S62 Flow reduction for cardiac failure
Fig. 2 - Revision Using Distal Inflow (RUDI-1). Fig. 3 - Transposition of the Radial Artery (RUDI-2).
arteries was necessary in five cases: mean preoperative In a few cases, RUDI may be impossible, due to diabetic
flow was 920 ± 372 (mL/min ± SD), mean postoperative distal artery calcifications. Its drawback is eventual future
flow was 596 ± 271 (mL/min ± SD), mean reduction rate occurrence of a bridge-graft vein anastomosis stenosis.
was 34 ± 24%.
This method also applies in cases of proximal high-flow Transposition of the radial artery
AVF coexisting with high bifurcation of the brachial artery,
which is present in 14% of individuals. High bifurcation diag- Transposition of the Radial Artery (RUDI-2) (Fig. 3) (8)
nosis is made on the existence of a permanent, with systolic is also a surgical procedure to reduce excessive blood flow
reinforcement Doppler signal on both distal forearm arteries through a proximal AVF: the brachial artery which supplies
(retrograde in one). The AVF, although situated at the elbow, the vein is replaced by the radial artery which has a much
actually involves radial or ulnar artery which can be ligated smaller caliber. For that purpose, the radial artery is first dis-
proximally without any risk of distal ischemia. In fact, the sected from the forearm, divided at the wrist and then turned
surgical ligation could be a cumbersome procedure after a upwards to reach the vein at the elbow.
2-stage basilic vein superficialization, and a percutaneously No prosthesis, with its risk of vein anastomosis stenosis,
inserted plug may be preferred (15). is used. This method is useful in young patients with normal
forearm arteries, especially in children in which bridge-graft
Distal Report of the Arterial Inflow stenosis would appear early while life-long angioaccess is re-
quired. The new anastomosis is an end-to-side anastomosis
Revision Using Distal Inflow (RUDI-1) (Fig. 2) involves re- of the artery to the anterior aspect of the vein whose ex-
placing inflow from brachial artery of a proximal AVF by inflow tremity has previously been closed. The surgical procedure
from one of its smaller caliber distal branches. is greatly facilitated by the use of an operating microscope.
To our knowledge we were the first to describe this Forty-seven patients referred for flow reduction of their
technique in 1989 as “Distal report of the arterial inflow” elbow fistula (28 brachiobasilic and 19 brachiocephalic)
(5, 6). The original arteriovenous anastomosis was closed were treated with this technique. Mean patient age was
at the elbow; an arteriovenous by-pass (thin-wall polytetra- 41 years (range: 2-76 years). The indications for flow reduc-
fluoroethylene [PTFE] in adults, greater saphenous vein in tion were cardiac failure (n = 13), concerns about future car-
children) was connected between the radial artery or the diac dysfunction (n = 23), hand ischemia (n = 4), and chronic
ulnar artery at the forearm, as distal as possible using surgi- venous hypertension resulting in aneurysmal degeneration
cal microscope, and the out-flow tract (vein or prosthesis) of the vein (n = 7). Forearm arteries were checked by ultra-
at the elbow. Distal anastomosis was easier to perform with sound examination and/or angiography before intervention
greater saphenous vein interposition as compared to PTFE. to confirm the patency of the ulnar and radial arteries and
Secondary stenosis of the vein anastomosis in the elbow the palmar arch.
was observed in both grafts. A 60% ±18 mean postopera- Flow rates were calculated according to body surface area
tive reduction rate was observed in 35 patients (mean age in order to create a standard measure for patients, particu-
44 years, range 2-67 years). Similar technique was reported larly taking into account the differences between the mor-
by a different author in two patients in 2004 (16). phology of men, women and children. Follow-up ranged from
A variant of this technique was published in 2005 as “RUDI” 2 months to 15 years.
(17) reporting a short distalization to the proximal radial or Immediate success rate was 94%. Mean flow rate dropped
ulnar artery approximately 2-3 cm distal to the brachial artery from 1,999 ± 808 to 726 ± 467 mL/min per 1.73 m² corre-
bifurcation in four patients. Unfortunately the length of the dis- sponding to a mean flow rate reduction of 66%, with a low
talization may have been too short, and pre- and postoperative standard deviation of 14% and a clinical success in 29/31
flow rates were not reported. non-ischemic patients.
Nineteen patients treated by RUDI were recently report- The only two immediate failures were due to major tech-
ed (18). Mean preoperative access flow was reduced from nical difficulties in the making of the new anastomosis be-
3,080 ± 200 to 1,170 ± 160 mL/min (p = 0.001). Mean access tween a small caliber radial artery and a thick wall elbow
flow at 12 months was 1,580 ± 260 mL/min. Better results vein. This resulted in acute thrombosis requiring redo of the
were observed with greater saphenous vein interposition as previous brachial artery anastomosis, with no subsequent
compared with basilic vein interposition. ischemic complication.
© 2016 Wichtig Publishing
Bourquelot S63
Including initial failures, primary patency rates after inter- eds. Vascular Access for Hemodialysis. Hong Kong: Pluribus
vention were 75% at 1 year, 53% at 3 years. During follow- Press; 1989:124-130.
up nine patients were successfully treated by percutaneous 6. Bourquelot P. Hemodialysis access-induced distal ischemia
transluminal angioplasty, which included five anastomosis (HAIDI): surgical management. In: Asif A, Agarwal AK et al, eds.
angioplasties and 11 venous angioplasties. Secondary paten- Interventional Nephrology. New York: Mc Graw Hill Medical;
2012:601-614.
cy rates were 94% at 1 year, 87% at 3 years. No recurrence of
7. Bourquelot P, Gaudric J, Turmel-Rodrigues L, Franco G, Van
high-flow was observed at 48 months. Laere O, Raynaud A. Proximal radial artery ligation (PRAL) for
Finally, eight out of 13 patients with cardiac insufficiency reduction of flow in autogenous radial cephalic accesses for
were clearly improved after fistula flow reduction. haemodialysis. Eur J Vasc Endovasc Surg. 2010;40(1):94-99.
8. Bourquelot P, Gaudric J, Turmel-Rodrigues L, Franco G, Van
Conclusion Laere O, Raynaud A. Transposition of radial artery for reduction
of excessive high-flow in autogenous arm accesses for hemodi-
When distal end-to-side AVF flow must be reduced, juxta- alysis. J Vasc Surg. 2009;49(2):424-428, 428.e1.
anastomosis PRAL is the preferred method. 9. MacRae JM, Pandeya S, Humen DP, Krivitski N, Lindsay RM.
To reduce a proximal AVF high flow, Distal Report of the Arteriovenous fistula-associated high-output cardiac failure: a
review of mechanisms. Am J Kidney Dis. 2004;43(5):e17-e22.
Arterial Inflow (RUDI-1) or Transposition of the Radial Artery
10. Begin V, Ethier J, Dumont M, Leblanc M. Prospective evaluation
(RUDI-2) is performed. The former is simple and effective, of the intra-access flow of recently created native arteriove-
but could be complicated with a bridge-graft vein anastomo- nous fistulae. Am J Kidney Dis. 2002;40(6):1277-1282.
sis stenosis. The latter is our first choice especially for young 11. van Duijnhoven EC, Cheriex EC, Tordoir JH, Kooman JP, van
patients. Hooff JP. Effect of closure of the arteriovenous fistula on left
ventricular dimensions in renal transplant patients. Nephrol
Disclosures Dial Transplant. 2001;16(2):368-372.
12. Schneider CG, Gawad KA, Strate T, Pfalzer B, Izbicki JR. T-banding:
Financial support: No grants or funding have been received for this a technique for flow reduction of a hyperfunctioning arteriove-
study. nous fistula. J Vasc Surg. 2006;43(2):402-405.
Conflict of interest: The author has no conflict of interest related to 13. Zanow J, Petzold K, Petzold M, Krueger U, Scholz H. Flow re-
this study to disclose.
duction in high-flow arteriovenous access using intraoperative
flow monitoring. J Vasc Surg. 2006;44(6):1273-1278.
References 14. Vaes RH, Wouda R, van Loon M, van Hoek F, Tordoir JH, Scheltinga
MR. Effectiveness of surgical banding for high flow in brachial ar-
1. Amerling R, Malostovker I, Dubrow A, Rosero H, Haveson S. tery-based hemodialysis vascular access. J Vasc Surg. 2015;61(3):
High output heart failure in patients with upper arm A-V fistu- 762-766.
lae: diagnosis and treatment. Abstracts from the 22nd Annual 15. Bourquelot P, Karam L, Raynaud A, Beyssen B, Ricco JB.
Meeting of International Society of Blood Purification (ISBP). Amplatzer vascular plug for occlusion or flow reduction of
London Sep 3-5, 2004. Blood Purif. 2004;A22:389. http://www. hemodialysis arteriovenous access. J Vasc Surg. 2014;59(1):
karger.com/Article/Pdf/80122 260-263.
2. Amerling R, Ronco C, Kuhlman M, Winchester JF. Arteriove- 16. Andrade JL, Paschôa AF, van Bellen B. Bridge graft to a small
nous fistula toxicity. Blood Purif. 2011;31(1-3):113-120. distal artery after fistula ligation for angioaccess-induced isch-
3. Basile C, Lomonte C, Vernaglione L, Casucci F, Antonelli M, emia: report of two cases. J Vasc Access. 2004;5(1):33-35.
Losurdo N. The relationship between the flow of arteriovenous 17. Minion DJ, Moore E, Endean E. Revision using distal inflow:
fistula and cardiac output in haemodialysis patients. Nephrol a novel approach to dialysis-associated steal syndrome. Ann
Dial Transplant. 2008;23(1):282-287. Vasc Surg. 2005;19(5):625-628.
4. Basile C, Lomonte C. Pro: the arteriovenous fistula is a blessing 18. Vaes RH, van Loon M, Vaes SM, Cuypers P, Tordoir JH, Scheltinga
of God. Nephrol Dial Transplant. 2012;27(10):3752-3756. MR. One-year efficacy of the RUDI technique for flow reduction
5. Bourquelot P, Corbi P, Cussenot O. Surgical improvement of in high-flow autologous brachial artery-based hemodialysis vas-
high-flow arteriovenous fistulas. In: Sommer BG, Henry ML, cular access. J Vasc Access. 2015;16(Suppl 9):S96-S101.
© 2016 Wichtig Publishing
You might also like
- Anatomic Exposure in Vascular Surgery, 3E (2013) (PDF) (UnitedVRG)Document605 pagesAnatomic Exposure in Vascular Surgery, 3E (2013) (PDF) (UnitedVRG)Rafael Castillo85% (13)
- Fetal Echocardiography Reporting FormatDocument1 pageFetal Echocardiography Reporting FormatMulugeta Abeneh100% (1)
- Cardiology Krok 2Document14 pagesCardiology Krok 2Suha AbdullahNo ratings yet
- Sabiston Textbook of Surgery 17th Ed 2005Document2,477 pagesSabiston Textbook of Surgery 17th Ed 2005Kyo Kusanagy38% (13)
- Intrinsic Conduction System: Page 1. IntroductionDocument5 pagesIntrinsic Conduction System: Page 1. IntroductionUta Provinsiana SukmaraNo ratings yet
- Estoya, Gen Paulo C. - Deep Vein Thrombosis NCP - NCM 112 LecDocument2 pagesEstoya, Gen Paulo C. - Deep Vein Thrombosis NCP - NCM 112 LecGen Paulo EstoyaNo ratings yet
- Cerebrovascular Disease MCQDocument25 pagesCerebrovascular Disease MCQDr. Kishore Kumar Ubrangala85% (13)
- 37 1Document3 pages37 1MoneymakerNo ratings yet
- Vascular and Peritoneal AccessDocument91 pagesVascular and Peritoneal AccessFrida AtallahNo ratings yet
- Vascular Access For Dialytic Therapies: Jan H. M. TordoirDocument1 pageVascular Access For Dialytic Therapies: Jan H. M. TordoirYuliastuti Mamah ChelseaNo ratings yet
- Eriko Shibata, Kojiro Nagai, Risa Takeuchi, (2015)Document3 pagesEriko Shibata, Kojiro Nagai, Risa Takeuchi, (2015)Aufa AdliaNo ratings yet
- Jeac 239Document4 pagesJeac 239Spam MailerNo ratings yet
- (CVP Journal) Vallo, Josef Dale T.Document2 pages(CVP Journal) Vallo, Josef Dale T.Josef ValloNo ratings yet
- Portal Hypertension SurgeryDocument6 pagesPortal Hypertension SurgeryjackSNMMCNo ratings yet
- Dialysis Access and Recirculation: Toros Kapoian Jeffrey L. Kaufman John Nosher Richard A. ShermanDocument14 pagesDialysis Access and Recirculation: Toros Kapoian Jeffrey L. Kaufman John Nosher Richard A. ShermanaeleandrosNo ratings yet
- Fistula USGDocument20 pagesFistula USGsamuelNo ratings yet
- AVF NewDocument81 pagesAVF NewBasit AliNo ratings yet
- Overview of Hemodialysis Access and Assessment - PMCDocument17 pagesOverview of Hemodialysis Access and Assessment - PMCvwyldrNo ratings yet
- Dr. Farsana - TK Junior ResidentDocument30 pagesDr. Farsana - TK Junior ResidentKmct Radiology Dpt.No ratings yet
- Arterial LineDocument2 pagesArterial LineRaghav Goyal100% (1)
- Aneurysm Abdominal AortaDocument8 pagesAneurysm Abdominal AortaMochammad Halim NNo ratings yet
- Original ArticlesDocument8 pagesOriginal ArticlesHugoNo ratings yet
- A Review Article: Access Recirculation Among End Stage Renal Disease Pa-Tients Undergoing Maintenance HemodialysisDocument6 pagesA Review Article: Access Recirculation Among End Stage Renal Disease Pa-Tients Undergoing Maintenance HemodialysisIrma HermaliaNo ratings yet
- Conduits For Coronary Bypass: Vein Grafts: Hendrick B Barner, M.D., Emily A Farkas, M.DDocument12 pagesConduits For Coronary Bypass: Vein Grafts: Hendrick B Barner, M.D., Emily A Farkas, M.DGaetano Di GiovanniNo ratings yet
- HarrisDocument25 pagesHarrisHafiz AlfarizieNo ratings yet
- ImpellaDocument5 pagesImpellapuspaNo ratings yet
- Tumor Kanker TiroidDocument9 pagesTumor Kanker TiroidyuliantoNo ratings yet
- Prospective Evaluation of Factors Associated With Early Failure of Arteriovenous Fistulae in Hemodialysis PatientsDocument5 pagesProspective Evaluation of Factors Associated With Early Failure of Arteriovenous Fistulae in Hemodialysis PatientsIvor WilopoNo ratings yet
- Manajemen Transfusi Perioperatif Pada Pasien Bedah Jantung Dewasa DenganDocument18 pagesManajemen Transfusi Perioperatif Pada Pasien Bedah Jantung Dewasa DenganGambar DoangNo ratings yet
- Fontan Operation: DR Hussain BuxDocument62 pagesFontan Operation: DR Hussain BuxMujeeb Ur RehmanNo ratings yet
- Malgor 2013Document4 pagesMalgor 2013vas25No ratings yet
- Management Acute Variceal BleedingDocument7 pagesManagement Acute Variceal BleedingSilminaNo ratings yet
- Cateteres Arteriaes, Central y Arteria PulmonarDocument13 pagesCateteres Arteriaes, Central y Arteria PulmonarmmsNo ratings yet
- Carotid PSV Song YDocument6 pagesCarotid PSV Song YthunderparthNo ratings yet
- Cardiac Complications of Arteriovenous Fistulas in Patients With End-Stage Renal DiseaseDocument12 pagesCardiac Complications of Arteriovenous Fistulas in Patients With End-Stage Renal Diseasetenty isniNo ratings yet
- JUMDC 6 Arterio VenousDocument6 pagesJUMDC 6 Arterio VenousMudassar SaeedNo ratings yet
- Flow Ands Cardiac ComplicationsDocument4 pagesFlow Ands Cardiac ComplicationsRenov OmpusungguNo ratings yet
- Ateriovenous FistulaDocument31 pagesAteriovenous Fistulaapi-265849428No ratings yet
- Potri Hafisah B. Macadaya Group 2 BSN 3Document26 pagesPotri Hafisah B. Macadaya Group 2 BSN 3Marivic Diano100% (2)
- Vascular Access HemodialysisDocument19 pagesVascular Access Hemodialysisplethoraldork100% (1)
- Endoscopicmanagementof Portalhypertension-Related Bleeding: Andrew Nett,, Kenneth F. BinmoellerDocument17 pagesEndoscopicmanagementof Portalhypertension-Related Bleeding: Andrew Nett,, Kenneth F. BinmoellerAlonso CayaniNo ratings yet
- Emborrhoid Technique Performed On A Patient With Portal Hypertension and Chronic Hemorrhoidal Bleeding As A Salvage TherapyDocument4 pagesEmborrhoid Technique Performed On A Patient With Portal Hypertension and Chronic Hemorrhoidal Bleeding As A Salvage TherapydianisaindiraNo ratings yet
- Fluid Management in Acute Kidney InjuryDocument8 pagesFluid Management in Acute Kidney InjuryHGZ 83 MoreliaNo ratings yet
- Assessment of Av FistulaDocument49 pagesAssessment of Av Fistulaatul_desai_3100% (1)
- Vascular Access For HemodialysisDocument25 pagesVascular Access For HemodialysisKartika JuwitaNo ratings yet
- Adenosine-Induced Transient Asystole: Gavin W. Britz, M.D., M.P.HDocument4 pagesAdenosine-Induced Transient Asystole: Gavin W. Britz, M.D., M.P.HAnkitaNo ratings yet
- What Is FFR?: How Can FFR Affect Treatment of The Patient?Document3 pagesWhat Is FFR?: How Can FFR Affect Treatment of The Patient?Anonymous 2wt1RiNo ratings yet
- 2016 - Mukhtar - Modulation of Splanchnic CirculationDocument12 pages2016 - Mukhtar - Modulation of Splanchnic CirculationJZNo ratings yet
- AAAkateDocument5 pagesAAAkateprem kotiNo ratings yet
- Arterial DopplerDocument29 pagesArterial DopplerAudrey100% (20)
- Phlebology 2012 Gloviczki 2 9Document9 pagesPhlebology 2012 Gloviczki 2 9Peet UpNo ratings yet
- I1524-5012-16-3-243 IMPELLADocument7 pagesI1524-5012-16-3-243 IMPELLAzairakuri32No ratings yet
- Robertson 2017Document10 pagesRobertson 2017tnsourceNo ratings yet
- CVP Evaluation Interpretation PDFDocument3 pagesCVP Evaluation Interpretation PDFMegan LewisNo ratings yet
- The Role of Color Doppler Ultrasound in Living Donor Liver Transplantation 2008 Journal of Medical UltrasoundDocument11 pagesThe Role of Color Doppler Ultrasound in Living Donor Liver Transplantation 2008 Journal of Medical UltrasoundIman Ru-ancaNo ratings yet
- Doppler-Atlas VasospasmDocument5 pagesDoppler-Atlas VasospasmdanielNo ratings yet
- mn58 Pleno Dialysis UnumaDocument2 pagesmn58 Pleno Dialysis UnumaBashir AhmedNo ratings yet
- Arteriovenous FistulasDocument21 pagesArteriovenous FistulasDragos GarofilNo ratings yet
- Venous Congestion ChapterDocument8 pagesVenous Congestion ChapterpcarrascoeNo ratings yet
- Blalock Taussig Shunt PDFDocument4 pagesBlalock Taussig Shunt PDFzuraini_mdnoorNo ratings yet
- Brain HemorrhagesDocument9 pagesBrain HemorrhagesAyashopia AyaNo ratings yet
- VExUS Nexus Bedside Assessment of Venous CongestiDocument10 pagesVExUS Nexus Bedside Assessment of Venous Congestilegap27No ratings yet
- AvfrdingDocument4 pagesAvfrdingyelisha05No ratings yet
- Aortic RegurgitationFrom EverandAortic RegurgitationJan VojacekNo ratings yet
- Diagnostic and Interventional Radiology of Arteriovenous Accesses for HemodialysisFrom EverandDiagnostic and Interventional Radiology of Arteriovenous Accesses for HemodialysisNo ratings yet
- T3 - Pack Code DetailsDocument302 pagesT3 - Pack Code DetailskiranNo ratings yet
- Atrial Septal Defect: Presented By:-Dr Kunwar Sidharth SaurabhDocument60 pagesAtrial Septal Defect: Presented By:-Dr Kunwar Sidharth SaurabhKunwar Sidharth SaurabhNo ratings yet
- Anatomy of The Ventricular Septal Defect in Congenital Heart DefectDocument8 pagesAnatomy of The Ventricular Septal Defect in Congenital Heart DefectFajar YuniftiadiNo ratings yet
- CVS Tables FranzDocument7 pagesCVS Tables FranzCole GoNo ratings yet
- Matsushita 2010Document7 pagesMatsushita 2010Arankesh MNo ratings yet
- THROMBOSISDocument11 pagesTHROMBOSISChandan DebbarmaNo ratings yet
- Basic Coronary Angiography All SlidesDocument55 pagesBasic Coronary Angiography All SlidesSaud ShirwanNo ratings yet
- Waksman 2018Document7 pagesWaksman 2018harry pribadiNo ratings yet
- Moya MoyaDocument5 pagesMoya MoyaNick Junior100% (1)
- Do Any Supplements Help For Varicose Veins or Chronic Venous Insufficiency?Document2 pagesDo Any Supplements Help For Varicose Veins or Chronic Venous Insufficiency?PeterNo ratings yet
- Cardiovascular Pathology 1:: Blood VesselsDocument48 pagesCardiovascular Pathology 1:: Blood VesselsRaiver CadenNo ratings yet
- Blood CirculationDocument42 pagesBlood CirculationAshu kumar100% (1)
- Tissues and Intro To Circulation 2014 2Document51 pagesTissues and Intro To Circulation 2014 2Chantae JulienNo ratings yet
- Basic EcmoDocument62 pagesBasic EcmoBasantkumar SinghNo ratings yet
- Biochemical Markers For Clinical Monitoring of Tissue PerfusionDocument14 pagesBiochemical Markers For Clinical Monitoring of Tissue PerfusionTrọng MPNo ratings yet
- Congestive Cardiac FailureDocument38 pagesCongestive Cardiac FailureSalman KhanNo ratings yet
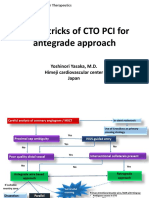
- Tips & Tricks of CTO PCI For Antegrade Approach: Yoshinori Yasaka, M.D. Himeji Cardiovascular Center JapanDocument21 pagesTips & Tricks of CTO PCI For Antegrade Approach: Yoshinori Yasaka, M.D. Himeji Cardiovascular Center JapanEll KlazureNo ratings yet
- Tim Gilbert and Nicola Rudge Chief of Medicine 1 Service and Chief PharmacistDocument39 pagesTim Gilbert and Nicola Rudge Chief of Medicine 1 Service and Chief PharmacistjellyjohnNo ratings yet
- Congestive Heart FailureDocument1 pageCongestive Heart Failuredr_654737902No ratings yet
- Measurement of CENTRAL VENOUS PRESSURE Via A TransducerDocument22 pagesMeasurement of CENTRAL VENOUS PRESSURE Via A TransducerJasleen KaurNo ratings yet
- A Simple and Fast Experimental Model: Laboratory InvestigationDocument4 pagesA Simple and Fast Experimental Model: Laboratory InvestigationAjay PeddiNo ratings yet
- Management of Acute Limb Ischemia in The Pediatric PopulationDocument5 pagesManagement of Acute Limb Ischemia in The Pediatric PopulationPendidikan Dokter Unsyiah 2015No ratings yet
- DobutaminDocument15 pagesDobutaminInnocence AmandaNo ratings yet