Professional Documents
Culture Documents
First Article
First Article
Uploaded by
Muhammad ZamanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
First Article
First Article
Uploaded by
Muhammad ZamanCopyright:
Available Formats
DOI: https://doi.org/10.
53350/pjmhs22167811
ORIGINAL ARTICLE
Anemia in Patients with Ulcerative Colitis in Remission: A Cross-Sectional
Study from Pakistan
MUHAMMAD ARSALAN QAISAR1, SHERAZ SALEEM2, AISHAH ISHAQUE3, MUHAMMAD UBAID4, USMAN JAVAID5, MUHAMMAD
ZAMAN6
1
Medical Officer at Rehab Medical Clinic/ Ex House Officer Jinnah hospital, Lahore
2
Assistant Professor Department of Medicine/ Sargodha Medical College Sargodha/ DHQ Teaching Hospital, Sargodha
3
House Officer at PIMS Islamabad
4
Assistant Professor, Department of Medicine, Civil Hospital, Karachi
5
MBBS, MPH, Dip Gastro (UK), Assistant Director, Punjab Human Organ Transplantation Authority
6
M.Phil Pathology LUMHS Jamhsoro, Pathologist Civil Hospital, Naushahro Feroze
Corresponding author: Sheraz Saleem, Email: drsherazsaleem@yahoo.com
ABSTRACT
Background and Aim: Anemia is an extra intestinal manifestation of inflammatory bowel disease that frequently causes
complications. In inflammatory bowel disease (IBD) such as ulcerative colitis and Crohn’s disease, anemia is mostly caused by
iron deficiency which impacts the patient's quality of life [1, 2]. The present study aimed to assess the anemia in ulcerative colitis
patients in remission.
Methodology: A cross-sectional study was conducted on 82 ulcerative colitis patients at the Department of Medicine and
Gastroenterology, Jinnah hospital, Lahore from February 2021 to January 2022. All the patients were assessed for anemia
based on Mayo clinical score <3 for at least three months. Hemogram tests such as CBC, vitamin B12 serum levels, ferritin,
folic acid levels, concentration of C - reactive protein (CRP), and transferrin were performed for the initial screening. Further,
patients were evaluated for the determination of different causes of anemia. Patients were categorized into mild, moderate, and
severe anemia cases. Oral iron, intravenous iron, and blood transfusion were given to mild, moderate, and severe anemia
patients respectively. SPSS version 25 was used for data analysis.
Results: Of the total 82 ulcerative colitis patients, there were 48 (58.5%) male and 34 (41.5%) females. The prevalence of
anemia in ulcerative colitis patients and control was 51.2% (n=42) and 11.9% (n=5) respectively. The hemoglobin mean values
in UC patients and control was 11.95 g/dL and 13.21 g/dL respectively. Out of 42 ulcerative colitis patients, the prevalence of
mild, moderate, and severe anemia was 52.4% (n=22), 35.7% (n=15), and 11.9% (n=5) respectively. Iron deficiency was the
prevalent etiology of anemia found in 22 (52.4%) patients followed by chronic anemia disease with iron deficiency found in 8
(21.9%). Hemoglobin level has no association with ferritin level. Hemoglobin level has no association with ferritin level. The
hemoglobin level was increased with oral iron and intravenous iron by 1.6 g/dL and 2.3 g/dL respectively.
Conclusion: The present study concluded that prevalence of anemia was higher in ulcerative colitis patients. The most
common etiology of anemia was iron deficiency in both groups. Increased CRP and moderate activity associated to anemia
disease was significantly related with comorbid anemia. Oral iron and intravenous iron could increase hemoglobin levels in
ulcerative colitis associated anemia patients.
Keywords: Anemia, Ulcerative Colitis, Iron deficiency
INTRODUCTION remission and had normal limits of C-reactive protein level.
Anemia is an extra intestinal manifestation of inflammatory bowel Therefore, the aim of the current study was to assess the anemia
disease that frequently causes complications. In inflammatory in ulcerative colitis patients.
bowel disease (IBD) such as ulcerative colitis and Crohn’s disease,
anemia is mostly caused by iron deficiency which impacts the METHODOLOGY
patient's quality of life [1, 2]. A previous systematic review A cross-sectional study was conducted on 82 ulcerative colitis
reported 27% prevalence of anemia in Crohn’s disease patients patients at the Department of Medicine and Gastroenterology,
whereas 21% in ulcerative colitis patients with 95% confidence Jinnah hospital, Lahore from February 2021 to January 2022. All
interval [3]. Iron deficiency was the prevalent etiology for anemia the patients were assessed for anemia based on Mayo clinical
which comprised more than a half patients. Another study reported score <3 for at least three months. Hemogram tests such as CBC,
incidence of anemia to vary from 6.2% to 73.3% in inflammatory vitamin B12 serum levels, ferritin, folic acid levels, concentration of
bowel disease patients [4, 5]. Morbidity caused by anemia in C - reactive protein (CRP), and transferrin were performed for the
ulcerative colitis patients triggered different symptoms such as initial screening. Further, patients were evaluated for the
restless leg syndrome, easy fatigability, female infertility, sleeping determination of different causes of anemia. Patients were
disorders, and attention deficit impairing quality of life [6]. Other categorized into mild, moderate, and severe anemia cases. Oral
causes for anemia in ulcerative colitis patients are blood loss, iron, intravenous iron, and blood transfusion were given to mild,
nutritional deficiency, and medication used by the general moderate, and severe anemia patients respectively.
population [7]. Prior to study conduction, ethical approval was taken from
Comparing the prevalence of anemia in inflammatory bowel the institutional ethical committee. Written informed consent was
disease, it has been observed that hospitalized patients are more taken from each individual. All those patients with history of
susceptible to anemia than others [8]. The incidence of anemia in ulcerative colitis, had clinical remission, normal C-reactive protein
IBD hospitalized patients was reported to range from 44% by level, and no rectal bleeding were enrolled. Besides 82 ulcerative
Gonzalez et al [9] to 74% by Herrera [10]. However, advanced colitis patients that satisfied the inclusion criteria, 40 patients were
studies found lower prevalence of anemia in IBD patients due to in the control group as a functional dyspepsia. A detailed history
improving anemia treatment and outcome. Anemia successful regarding drug usage was taken. Hematinic user patients were
therapy could improve life’s quality in a better way than anti- excluded from the study. Based on WHO classification for anemia
inflammatory therapy [11]. Additionally, the most prevalent patients, hemoglobin cut off value was set 12 g/dL and 13 g/dL for
comorbid conditions related to IBD patient’s mortality was anemia females and males respectively. Ulcerative colitis patients with
[12]. However, in such patients, IBD severity was simply a factor anemia were further investigated. The range for counting red cell
that contributed to acute morbidity cases. The present study distribution width (RDW) and corrected reticulocyte count were
involved all the ulcerative colitis patients with at least 3 months 11.5% to 14.5% and 0.5% to 1.5% respectively. Patients were
P J M H S Vol. 16, No. 07, July 2022 811
Anemia in Patients with Ulcerative Colitis in Remission: A Cross-Sectional Study from Pakistan
assessed for anemia which had low/normal mean corpuscular Table-2: Association of iron deficiency and ferritin levels
volume (MCV), higher RDW, and low/normal reticulocyte count. Mgc/L Male n (%) Females’ n (%) Overall n (%)
Ferritin normal level and transferrin saturation were 30–300 <30 15 (48.4) 16 (51.6) 31 (73.8)
microgram per litre (mcg/L) and 15% to 50%. Anemia was 30-100 6 (66.7) 3 (33.4) 9 (21.4)
>100 1 (50%) 1 (50%) 2 (4.8)
considered to be present in patients having transferrin saturation
<20% and ferritin levels <30%. SPSS version 25 was used for data
analysis. Anemia prevalence was compared between two groups
using Chi-square test. Student’s t-test was used for comparing
hemoglobin values between study and control groups. P<0.05 was
considered of statistical significance.
RESULTS
Of the total 82 ulcerative colitis patients, there were 48 (58.5%)
male and 34 (41.5%) females. The prevalence of anemia in
ulcerative colitis patients and control was 51.2% (n=42) and 11.9%
(n=5) respectively. The hemoglobin mean values in UC patients
and control was 11.95 g/dL and 13.21 g/dL respectively. Out of 42
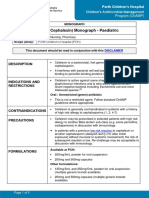
Figure-3: Different causes of anemia in ulcerative colitis patients
ulcerative colitis patients, the prevalence of mild, moderate, and
severe anemia was 52.4% (n=22), 35.7% (n=15), and 11.9% (n=5)
respectively. Iron deficiency was the prevalent etiology of anemia DISCUSSION
found in 22 (52.4%) patients followed by chronic anemia disease The present study demonstrated the prevalence of anemia in
with iron deficiency found in 8 (19.04%). Hemoglobin level has no ulcerative colitis patients. The results show that higher CRP and
association with ferritin level. The hemoglobin level was increased moderate disease activity has significant association with anemia.
with oral iron and intravenous iron by 1.6 g/dL and 2.3 g/dL Till now, it has been observed for the first time that an important
respectively. Figure-1 shows the gender’s distribution. Baseline risk factor for anemia is moderate disease activity in ulcerative
characteristics are shown in Table-I. Anemia prevalence and colitis patients. Additionally, iron deficiency anemia was the
severity in ulcerative colitis patients are illustrated in Figure-2. prevalent etiology of anemia in inflammatory bowel disease
Table-II represents the association of iron deficiency and ferritin patients. Oral iron and intravenous iron could increase hemoglobin
levels. Figure-3 depicts the different causes of anemia in ulcerative levels in ulcerative colitis associated anemia patients. The
colitis patients. prevalence of anemia in ulcerative colitis patients and control was
51.2% found in the current study. A recent study conducted in
Europe reported the overall prevalence of anemia in IBD patients
was 24% (95% CI, 18-31) which is lower than our findings [13].
The prevalence of anemia range from 17% to 20% as reported by
various studies [14, 15] which is quite lower than the anemia
prevalence found in the current study.
The present study reported 5 cases of severe anemia. It,
however, due to the inclusion of severe IBD and anemia patients
34, 41.5% Male which needed high probability of hospitalization. Additionally, the
IBD patients were followed for continuous monitoring and
48, 58.5% Females achieving the target of intestinal inflammation tight control. The
underlying activity of disease was correlated with inflammatory
bowel disease patients who had anemia [16]. The anemia of
chronic disease, terminal ileitis due to vitamin B12 deficiency,
induced azathioprine, chronic blood loss, and folate deficiency
were attributable factors for anemia in ulcerative colitis patients
[17]. Chronic fatigue could results from anemia that blight the life’s
quality [18].
Figure-1: Gender’s distribution (n=82) Ulcerative colitis patients with remission were chosen for the
current study because certain anemia patients might go un-
Table-1: Baseline characterization recognized until tested specifically for anemia. Anemia was defined
Parameters Male (n=48) Females (n=34) Overall (n=82)
based on world health organization criteria set for hemoglobin level
Mean Hb (g/dL) 12.31 11.1 11.71
cut off value that is 12 g/dL and 13 g/dL for females and male
Mean MCV (fL) 83.62 76.92 80.27
Mean RDW (%) 16.9 22.9 19.9
respectively. According to the study conducted by Peyrin-Biroulet
et al [19] the incidence of anemia range from 16% to 74% in
inflammatory bowel disease patients [20].
14 12 The current study found the prevalence of mild, moderate,
12 severe anemia cases were 52 %, 35.7%, and 11.9% respectively.
10
10
A previous study reported that almost one third patients of
8 ulcerative colitis with anemia were not tested for anemia symptoms
8 7
like iron deficiency [21]. Nutritional deficiency was reported based
6 on indications such as high RWD and low reticulocyte count.
4 3
2 Microcytosis, macrocytosis, and normocytosis generally suggests
2 deficiency of iron, vitamin B12, and mix picture like disease of
0 chronic anemia. All the patients underwent flexible sigmoidoscopy
Mild (10-13 g/dL) Moderate (8-10 g/dL) Severe (g/dL) for the detection of endoscopic inflammation. In anemia patients.
Iron deficiency was the common etiology present in 52.4%.
Male Females Chronic anemia disease with iron deficiency was present in
19.04% ulcerative colitis patients. These findings almost resemble
Figure-2: association of anemia severity and gender’s distribution another study results according to which ulcerative colitis patients
812 P J M H S Vol. 16, No. 07, July 2022
M. A. Qaisar, S. Saleem, A. Ishaque et al
required iron supplementation, had blood loss, treatment intravenous treatment in iron deficiency anaemia in inflammatory
modification, and nutritional deficiency [22]. bowel disease: Early efficacy and impact on quality of life. Blood
The association of hemoglobin levels and ferritin levels were Transfus. 2016, 14, 199–205.
9. Gonzalez Alayon, C.; Pedrajas Crespo, C.; Marin Pedrosa, S.;
investigated for the gender’s difference in the present study. The Benítez, J.M.; Iglesias Flores, E.; Salgueiro Rodríguez, I.; Medina
acceptable limit for increasing the level of hemoglobin to be 2 g/dl Medina, R.; García-Sánchez, V. Prevalence of iron deficiency without
within four weeks were considered appropriate [23]. Another study anaemia in inflammatory bowel disease and impact on health-related
compared the oral iron to intravenous iron and found that the later quality of life. Gastroenterol. Hepatol. 2018, 41, 22–29.
one provides higher efficacy and better tolerability [24]. In our 10. Herrera-deGuise, C.; Casellas, F.; Robles, V.; Navarro, E.; Borruel,
study, we used ferric carboxymaltose. However, iron isomaltoside, N. Iron deficiency in the absence of anemia impairs the perception of
iron sucrose, ferric carboxymaltose, and even advanced health-related quality of life of patients with inflammatory bowel
disease. Inflamm. Bowel Dis. 2016, 22, 1450–1455.
ferumoxytol has been used for preparation of intravenous iron. We 11. Thuluvath, A.; Rayapati, D.; Limketkai, B.; Parian, A. Half of IBD
observed that the increase in hemoglobin level was higher in patients without anemia have iron deficiency leading to similar rates
intravenous iron users compared to oral iron. However, mostly of fatigue as iron deficiency anemia. Off. J. Am. Coll. Gastroenterol.
patients tolerated the oral iron compared to lower willingness for 2018, 113, S343.
injectable iron. As a result, we conclude that ulcerative colitis 12. Dignass, A.U.; Gasche, C.; Bettenworth, D.; Birgegård, G.; Danese,
patients treated for iron deficiency are only the tip of the iceberg, S.; Gisbert, J.P.; Gomollon, F.; Iqbal, T.; Katsanos, K.; Koutroubakis,
and the majority of patients with quiescent disease have underlying I.; et al. European consensus on the diagnosis and management of
iron deficiency and anaemia in inflammatory bowel diseases. J.
iron deficiency. These patients should be identified and screened Crohns’s Colitis 2015, 9, 211–222.
using a simple test, such as a hemogram, so that their iron 13. World Health Organization. Haemoglobin Concentrations for the
deficiency can be treated in a cost-effective manner. Diagnosis of Anaemia and Assessment of Severity; Vitamin and
Vitamin B12 deficiency was discovered in six patients, three Mineral Nutrition Information System; World Health Organization:
of whom were vegetarians and three of whom had pernicious Geneva, Switzerland, 2011.
anemia. Three patients were discovered to have celiac disease. 14. Soppi, E. Iron deficiency without anemia—Common, important,
Iron deficiency anemia persists in a significant proportion of neglected. Clin. Case. Rep. Rev. 2019, 5, 1–7.
15. Comin-Colet, J.; Enjuanes, C.; Gonzalez, G.; Torrens, A.; Cladellas,
ulcerative colitis patients in remission and must be treated M.; Meroño, O.; Ribas, N.; Ruiz, S.; Gómez, M.; Verdú, J.M.; et al.
appropriately. In IBD patients, intestinal inflammation plays a Iron deficiency is a key determinant of health-related quality of life in
critical role in the development of anemia. Particularly in the patients with chronic heart failure regardless of anaemia status. Eur.
presence of active disease and/or an elevated CRP level, the J. Heart Fail. 2013, 15, 1164–1172.
suspicion of underlying anemia should be raised, and it should be 16. Shepshelovich, D.; Rozen-Zvi, B.; Avni, T.; Gafter, U.; Gafter-Gvili, A.
carefully investigated. Intravenous versus oral iron supplementation for the treatment of
anemia in CKD: An updated systematic review and meta-analysis.
Am. J. Kidney Dis. 2016, 68, 677–690.
CONCLUSION 17. Çekiç, C.; Ipek, S.; Aslan, F.; Akpınar, Z.; Arabul, M.; Topal, F. The
The present study concluded that prevalence of anemia was effect of intravenous iron treatment on quality of life in inflammatory
higher in ulcerative colitis patients. The most common etiology of bowel disease patients with nonanemic iron deficiency.
anemia was iron deficiency in both groups. Increased CRP and Gastroenterol. Res. Pract. 2015, 2015, 582163.
moderate activity associated to anemia disease was significantly 18. Eliadou, E.; Kini, G.; Huang, J.; Champion, A.; Inns, S.J. Intravenous
iron replacement improves quality of life in hypoferritinemic
related with comorbid anemia. Oral iron and intravenous iron could inflammatory bowel disease patients with and without anemia. Dig.
increase hemoglobin levels in ulcerative colitis associated anemia Dis. 2017, 35, 444–448.
patients. 19. Peyrin-Biroulet, L.; Panes, J.; Sandborn, W.J.; Vermeire, S.; Danese,
S.; Feagan, B.G.; Colombel, J.F.; Hanauer, S.B.; Rycroft, B. Defining
REFERENCES disease severity in inflammatory bowel diseases: Current and future
1. Rubin DT, Ananthakrishnan AN, Siegel CA, et al. ACG clinical directions. Clin. Gastroenterol. Hepatol. 2016, 14, 348–354.e17.
guideline: ulcerative colitis in adults. Am J Gastroenterol. 20. Ponikowski, P.; van Veldhuisen, D.J.; Comin-Colet, J.; Ertl, G.;
Komajda, M.; Mareev, V.; McDonagh, T.; Parkhomenko, A.; Tavazzi,
2019;114:384–413.
L.; Levesque, V.; et al. Beneficial effects of long-term intravenous iron
2. Nakase H, Uchino M, Shinzaki S, et al. Evidence-based clinical
practice guidelines for inflammatory bowel disease 2020. J therapy with ferric carboxymaltose in patients with symptomatic heart
failure and iron deficiency. Eur. Heart J. 2015, 36, 657–668.
Gastroenterol. 2021;56:489–526.
21. van Veldhuisen, D.J.; Ponikowski, P.; van der Meer, P.; Metra, M.;
3. Magro F, Doherty G, Peyrin-Biroulet L, et al. ECCO position paper:
Böhm, M.; Doletsky, A.; Voors, A.A.; Macdougall, I.C.; Anker, S.D.;
harmonization of the approach to ulcerative colitis histopathology. J
Roubert, B.; et al. Effect of ferric carboxymaltose on exercise capacity
Crohns Colitis. 2020;14:1503–11.
in patients with chronic heart failure and iron deficiency. Circulation
4. Jonefjäll B, Simrén M, Lasson A, et al. Psychological distress, iron
2017, 136, 1374–1383.
deficiency, active disease and female gender are independent risk
factors for fatigue in patients with ulcerative colitis. United Eur 22. Peyrin-Biroulet, L.; Lopez, A.; Cummings, J.R.F.; Dignass, A.; Detlie,
Gastroenterol J. 2018;6:148–58. T.E.; Danese, S. Review article: Treating-to-target for inflammatory
5. Ratnakumaran R, Warren L, Gracie DJ, et al. Fatigue in inflammatory bowel disease-associated anaemia. Aliment. Pharmacol. Ther. 2018,
bowel disease reflects mood and symptom-reporting behavior rather 48, 610–617.
23. Auerbach, M.; Deloughery, T. Single-dose intravenous iron for iron
than biochemical activity or anemia. Clin Gastroenterol Hepatol.
2018;16:1165–7. deficiency: A new paradigm. Hematol. Am Soc Hematol Educ
Program 2016, 2016, 57–66
6. Goldenberg BA, Graff LA, Clara I, et al. Is iron deficiency in the
24. Chaparro, M.; Barreiro-de Acosta, M.; Benítez, J.M.; Cabriada, J.L.;
absence of anemia associated with fatigue in inflammatory bowel
Casanova, M.J.; Ceballos, D.; Esteve, M.; Fernández, H.; Ginard, D.;
disease? Am J Gastroenterol. 2013;108:1392–7.
Gomollón, F.; et al. Epidemiology, clinical characteristics, evolution
7. Gasche C, Berstad A, Befrits R, et al. Guidelines on the diagnosis
and treatments in newly diagnosed inflammatory bowel disease
and management of iron deficiency and anaemia in inflammatory
bowel diseases. Inflamm Bowel Dis. 2007; 13(12): 1545– 1553 (IBD): Results from the nationwide EpidemIBD study of GETECCU. J.
Crohns’s Colitis 2020, 14, S516–S517.
8. Garcia-Lopez, S.; Bocos, J.M.; Gisbert, J.P.; Bajador, E.; Chaparro,
M.; Castaño, C.; García-Erce, J.A.; Gomollón, F. High-dose
P J M H S Vol. 16, No. 07, July 2022 813
You might also like
- Practical Atlas of Tung's Acupuncture - Acupuncture - BookshopDocument4 pagesPractical Atlas of Tung's Acupuncture - Acupuncture - BookshopEdmundo Cadilha0% (2)
- Association of Liver Cirrhosis Severity With AnemiaDocument5 pagesAssociation of Liver Cirrhosis Severity With Anemiamy accountNo ratings yet
- Comparison of Serum Iron TIBC Transferrin SaturatiDocument4 pagesComparison of Serum Iron TIBC Transferrin SaturatiAri Dwi PrasetyoNo ratings yet
- 21 - Prevalencia AnemiaDocument10 pages21 - Prevalencia AnemiaFernandoVignoloNo ratings yet
- DR T Dinesh Guide DR Baba YelkeDocument27 pagesDR T Dinesh Guide DR Baba YelkeDinesh AshwinNo ratings yet
- 1 Ajaz 2012Document4 pages1 Ajaz 2012Olivia Valentine LekiNo ratings yet
- 406-01. Manuscript (Article Text) - 1308-1-10-20130405Document4 pages406-01. Manuscript (Article Text) - 1308-1-10-20130405Jeffrey RamosNo ratings yet
- The Relationship Between Anemia, Liver Disease, and Hepcidin Levels in Hemodialysis Patients With HepatitisDocument4 pagesThe Relationship Between Anemia, Liver Disease, and Hepcidin Levels in Hemodialysis Patients With HepatitisDaitya Rangga SaputraNo ratings yet
- Relationship Between Malnutrition-Inflammation Complex Syndrome and Fluid Balance in Maintenance Hemodialysis PatientsDocument8 pagesRelationship Between Malnutrition-Inflammation Complex Syndrome and Fluid Balance in Maintenance Hemodialysis PatientsMaricic MilovanNo ratings yet
- Manuscript 1Document4 pagesManuscript 1maryNo ratings yet
- Prevalence of Anemia and Iron Deficiency in Romanian Patients With Inflammatory Bowel Disease: A Prospective Multicenter StudyDocument6 pagesPrevalence of Anemia and Iron Deficiency in Romanian Patients With Inflammatory Bowel Disease: A Prospective Multicenter StudyOcha24 TupamahuNo ratings yet
- JDR2019 7825804Document9 pagesJDR2019 7825804Anonymous Xc7NwZzoNo ratings yet
- MJCU_Volume 88_Issue December_Pages 2121-2129Document9 pagesMJCU_Volume 88_Issue December_Pages 2121-2129jihansalma00No ratings yet
- A Study To Assess Changes in The Hematological Profile in Chronic Kidney DiseaseDocument3 pagesA Study To Assess Changes in The Hematological Profile in Chronic Kidney Diseasemandhalanarshimlu48141No ratings yet
- Complication PDFDocument16 pagesComplication PDFDani ursNo ratings yet
- Prevalence of and Risk Factors For Anaemia in Patients With Advanced Chronic Liver DiseaseDocument11 pagesPrevalence of and Risk Factors For Anaemia in Patients With Advanced Chronic Liver Diseasemy accountNo ratings yet
- Low Alt CKDDocument5 pagesLow Alt CKDFebianti RukmanaNo ratings yet
- Comparative Evaluation of Blood Parameters in Chronic Periodontitis Patients and Healthy Patients For Signs of AnemiaDocument7 pagesComparative Evaluation of Blood Parameters in Chronic Periodontitis Patients and Healthy Patients For Signs of AnemiaInternational Organization of Scientific Research (IOSR)No ratings yet
- Study of Anemia and Its Correlation With Hematological Parameters in Patient of Various Age GroupDocument7 pagesStudy of Anemia and Its Correlation With Hematological Parameters in Patient of Various Age GroupIOSRjournal0% (1)
- Biopsias en DM2Document7 pagesBiopsias en DM2konqueNo ratings yet
- Use of Blood Product in SepsisDocument6 pagesUse of Blood Product in SepsisAditya IrawanNo ratings yet
- Lieshmeniasis IJPSIDocument3 pagesLieshmeniasis IJPSIdvenumohanNo ratings yet
- Pattern of Anemia in Elderly PatientsDocument6 pagesPattern of Anemia in Elderly PatientsMuhammad Shehr YarNo ratings yet
- Prevalence of Anaemia in Decompensated Chronic Liver DiseaseDocument5 pagesPrevalence of Anaemia in Decompensated Chronic Liver DiseaseElang SudewaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 16: HematologyFrom EverandComplementary and Alternative Medical Lab Testing Part 16: HematologyNo ratings yet
- Mon Anemia and AgingDocument7 pagesMon Anemia and AgingtyasNo ratings yet
- review.plaglessDocument8 pagesreview.plaglesshaadiiNo ratings yet
- Jurnal 1 Beby NefroDocument14 pagesJurnal 1 Beby NefroAndri SunataNo ratings yet
- Diabetic Ketoacidosis in A Hospital Based Population in PakistanDocument6 pagesDiabetic Ketoacidosis in A Hospital Based Population in Pakistanhasnainhamid668No ratings yet
- TransfusiDocument9 pagesTransfusiabbhyasa5206No ratings yet
- 4768 10572 1 PBDocument8 pages4768 10572 1 PBNovianus Ummah SanyNo ratings yet
- Journal of Microscopy and Ultrastructure: Nora Nasir Al HassanDocument4 pagesJournal of Microscopy and Ultrastructure: Nora Nasir Al HassanAnis RanisNo ratings yet
- Jurnal Reading 4Document29 pagesJurnal Reading 4Maya SariNo ratings yet
- Serum Albumin Level Adjusted With C-Reactive Protein Predicts Hemodialysis Patient SurvivalDocument9 pagesSerum Albumin Level Adjusted With C-Reactive Protein Predicts Hemodialysis Patient Survivalmelda lestari haidirNo ratings yet
- Clinical Manifestation in Sickle Cell Anemia: A Study in Chhattisgarh Institute of Medical Sciences (CIMS) Bilaspur, Chhattisgarh, India.Document4 pagesClinical Manifestation in Sickle Cell Anemia: A Study in Chhattisgarh Institute of Medical Sciences (CIMS) Bilaspur, Chhattisgarh, India.IOSRjournalNo ratings yet
- 25rakshitha EtalDocument8 pages25rakshitha EtaleditorijmrhsNo ratings yet
- DD 22Document5 pagesDD 22siska dwiNo ratings yet
- A Comparison of The Pattern of Liver Involvement in Dengue Hemorrhagic Fever With Classic Dengue FeverDocument5 pagesA Comparison of The Pattern of Liver Involvement in Dengue Hemorrhagic Fever With Classic Dengue FeverMichelle Rayvi J. SumampouwNo ratings yet
- To Study The Hematological Profile in Patients With Alcoholic Liver Cirrhosis in A Tertiary Care Hospital in ManipurDocument9 pagesTo Study The Hematological Profile in Patients With Alcoholic Liver Cirrhosis in A Tertiary Care Hospital in ManipurIJAR JOURNALNo ratings yet
- AnnGastroenterol 30 217 PDFDocument8 pagesAnnGastroenterol 30 217 PDFhusni gunawanNo ratings yet
- Hypertension and Chronic Kidney Disease in Asian PopulationsDocument6 pagesHypertension and Chronic Kidney Disease in Asian PopulationsBIETRIS WARISYUNo ratings yet
- Faysal Bas It,+161 54-57Document4 pagesFaysal Bas It,+161 54-57Irvin MarcelNo ratings yet
- Cuidados Paliativos en Enf Hepatica TerminalDocument19 pagesCuidados Paliativos en Enf Hepatica Terminalcarlos ujedaNo ratings yet
- Sesuai JudulDocument6 pagesSesuai JudulNurazrah AzridadNo ratings yet
- Association of Anaemia in Primary Care Patients With Chronic Kidney Disease: Cross Sectional Study of Quality Improvement in Chronic Kidney Disease (QICKD) Trial DataDocument9 pagesAssociation of Anaemia in Primary Care Patients With Chronic Kidney Disease: Cross Sectional Study of Quality Improvement in Chronic Kidney Disease (QICKD) Trial DatahanifahrafaNo ratings yet
- Jurnal 6Document8 pagesJurnal 6OziNo ratings yet
- Sirosis Dan ESRDDocument9 pagesSirosis Dan ESRDdevidanthonyNo ratings yet
- Iron Deficiency Anemia and Associated Risk Factors Among Teenagers in Najran Saudi ArabiaDocument9 pagesIron Deficiency Anemia and Associated Risk Factors Among Teenagers in Najran Saudi ArabiaZkdlin kaiNo ratings yet
- An Etiological Reappraisal of Pancytopenia - LargestDocument9 pagesAn Etiological Reappraisal of Pancytopenia - LargestKaye Antonette AntioquiaNo ratings yet
- Sharawey2011 PDFDocument7 pagesSharawey2011 PDFIkram DibNo ratings yet
- Lipid Profile in CKDDocument4 pagesLipid Profile in CKDAmiyanshu BeheraNo ratings yet
- Factors Predicting Malnutrition in Hemodialysis Patients: A Cross-Sectional StudyDocument10 pagesFactors Predicting Malnutrition in Hemodialysis Patients: A Cross-Sectional StudyMarco TolentinoNo ratings yet
- DR - Mukesh Dassani Synopsis 20 SepDocument20 pagesDR - Mukesh Dassani Synopsis 20 SepMukesh DassaniNo ratings yet
- 2019 Article 1596Document9 pages2019 Article 1596Arina FitrianiNo ratings yet
- Electrolyte Imbalance in CKD PatientsDocument4 pagesElectrolyte Imbalance in CKD PatientsEditor IJTSRDNo ratings yet
- Comparison The Effect of High Flux and Low Flux Dialyzer On Quality of Life in Hemodialysis Patients A Clinical TrialDocument8 pagesComparison The Effect of High Flux and Low Flux Dialyzer On Quality of Life in Hemodialysis Patients A Clinical TrialMrQmonkNo ratings yet
- Nutrients: Nutritional Adequacy and Latent Tuberculosis Infection in End-Stage Renal Disease PatientsDocument8 pagesNutrients: Nutritional Adequacy and Latent Tuberculosis Infection in End-Stage Renal Disease PatientsMarwa AmrangNo ratings yet
- Paternostro 2020Document9 pagesPaternostro 2020my accountNo ratings yet
- Fluid Overload in Peritoneal Dialysis PatientsDocument11 pagesFluid Overload in Peritoneal Dialysis PatientsHaryonoNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderFrom EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Intestinal ObstructionDocument74 pagesIntestinal Obstructionmehroksukhwinder439No ratings yet
- Classification and Spectrum of Bipolar Disorder: Moderator: Dr. Navkiran S. MahajanDocument46 pagesClassification and Spectrum of Bipolar Disorder: Moderator: Dr. Navkiran S. MahajanAarti GuptaNo ratings yet
- Coronavirus Covid 19 Presentation Free Template by Slidecore 87pusdDocument24 pagesCoronavirus Covid 19 Presentation Free Template by Slidecore 87pusdHASSANNo ratings yet
- Cefalexin (Cephalexin) Monograph - Paediatric: DescriptionDocument5 pagesCefalexin (Cephalexin) Monograph - Paediatric: Descriptioneinas omerNo ratings yet
- Inter-Orient Maritime Enterprises, Inc. v. Creer IIIDocument10 pagesInter-Orient Maritime Enterprises, Inc. v. Creer IIIoabeljeanmoniqueNo ratings yet
- PreeclamsiaDocument22 pagesPreeclamsiaJosé DomínguezNo ratings yet
- Sepsis Fact SheetDocument4 pagesSepsis Fact SheetJoana MoreiraNo ratings yet
- BillaDocument5 pagesBillaZeeshan AfzalNo ratings yet
- Clinico - Hematological Analysis of Pancytopenia: A Bone Marrow StudyDocument6 pagesClinico - Hematological Analysis of Pancytopenia: A Bone Marrow StudySrinath M VNo ratings yet
- The Flesh CompositionDocument18 pagesThe Flesh CompositionMuhammad Irwan SetiawanNo ratings yet
- Anemia and Pregnancy: Sunil Kumar DahaDocument43 pagesAnemia and Pregnancy: Sunil Kumar DahaBhawna JoshiNo ratings yet
- Pir March18Document84 pagesPir March18María Cristina RomanoNo ratings yet
- Dka TogDocument25 pagesDka TogMelNo ratings yet
- Lipase Vs AmylaseDocument6 pagesLipase Vs AmylaseLuis AcevedoNo ratings yet
- Case Study (Appendicitis)Document8 pagesCase Study (Appendicitis)Jobelle AcenaNo ratings yet
- Key Points SurgeryDocument2 pagesKey Points SurgeryVyom ShrigodNo ratings yet
- Case Study 3 (Botulism)Document1 pageCase Study 3 (Botulism)Fariz LukmanNo ratings yet
- PR Bedah Onkologi - Dyah Putri Mentari Ginting - I4A013043Document3 pagesPR Bedah Onkologi - Dyah Putri Mentari Ginting - I4A013043Andrian SitompulNo ratings yet
- SPONDILOARTROPATIDocument8 pagesSPONDILOARTROPATIImam HakikiNo ratings yet
- Antenatal High Risk CaseDocument1 pageAntenatal High Risk CasesjamilmdfauzieNo ratings yet
- Chapter 50 Vision and HearingDocument7 pagesChapter 50 Vision and HearingAlmer OstreaNo ratings yet
- Pediatrics QuestionsDocument22 pagesPediatrics QuestionsShaik AmreenNo ratings yet
- Top 20 Bodyweight Exercises For Building Muscle & Strength - How To Build Muscle - Strength Training Workouts - Mass Gain DietDocument28 pagesTop 20 Bodyweight Exercises For Building Muscle & Strength - How To Build Muscle - Strength Training Workouts - Mass Gain DietDamonDanskyNo ratings yet
- PDFDocument152 pagesPDFAyu Putri Firda NNo ratings yet
- Inside The Criminal Mind.: Gonzalo B. Roman JR.,MD.,FPSP, MBAHDocument47 pagesInside The Criminal Mind.: Gonzalo B. Roman JR.,MD.,FPSP, MBAHAnonymous IJah4mNo ratings yet
- What Is Turner SyndromeDocument7 pagesWhat Is Turner SyndromeTiara Ramadhani100% (1)
- UNICORNDocument3 pagesUNICORNbrothersaleNo ratings yet
- Food Safety IssueDocument2 pagesFood Safety IssueDivine De GraciaNo ratings yet
- IM Case ReportDocument5 pagesIM Case ReportGurungSurajNo ratings yet