Professional Documents
Culture Documents
Grover M 2012
Grover M 2012
Uploaded by
afifahridhahumairahhCopyright:
Available Formats
You might also like
- Preopanc Trial - PancreasDocument20 pagesPreopanc Trial - PancreasRajalakshmi RadhakrishnanNo ratings yet
- 1 - Participate in Workplace CommunicaitonDocument38 pages1 - Participate in Workplace CommunicaitonSahlee Rose Falcunit GacaNo ratings yet
- ULSADO-JSA - Installation of Temporary Fence GateDocument2 pagesULSADO-JSA - Installation of Temporary Fence GateKelvin TanNo ratings yet
- GLP Vs 17025Document6 pagesGLP Vs 17025Nadhra HaligNo ratings yet
- Acupuncture-Based ModalitiesDocument9 pagesAcupuncture-Based ModalitiesFelipe MaiaNo ratings yet
- Grover 2011Document19 pagesGrover 2011afifahridhahumairahhNo ratings yet
- Pasricha 2008Document8 pagesPasricha 2008afifahridhahumairahhNo ratings yet
- FA - Metabolomic and Biochemical Characterization of A New Model of The Transition of Acute Kidney Injury To Chronic Kidney Disease Induced by Folic AcidDocument26 pagesFA - Metabolomic and Biochemical Characterization of A New Model of The Transition of Acute Kidney Injury To Chronic Kidney Disease Induced by Folic AcidCher IshNo ratings yet
- Pathophysiology, Diagnosis, and Management of Chronic Intestinal Pseudo-ObstructionDocument13 pagesPathophysiology, Diagnosis, and Management of Chronic Intestinal Pseudo-ObstructionJosealberto ArenasNo ratings yet
- Nihms 651235Document9 pagesNihms 651235afifahridhahumairahhNo ratings yet
- Nutrients 14 03959Document15 pagesNutrients 14 03959CrisNo ratings yet
- Nihms 1692401Document23 pagesNihms 1692401jim STAMNo ratings yet
- Harberson 2009Document12 pagesHarberson 2009afifahridhahumairahhNo ratings yet
- Reliability of Mini Nutritional Assessment in Hemodialysis Compared With Subjective Global AssessmentDocument6 pagesReliability of Mini Nutritional Assessment in Hemodialysis Compared With Subjective Global AssessmentyafanitaizzatiNo ratings yet
- Ajpgi 00190 2011 PDFDocument8 pagesAjpgi 00190 2011 PDFAnonymous CQSNUSNo ratings yet
- Acute Abdomen in The Medical Intensive Care Unit: ArticleDocument5 pagesAcute Abdomen in The Medical Intensive Care Unit: ArticleChiriţoiu AnamariaNo ratings yet
- Is Primary Sclerosing Cholangitis With Inflammatory Bowel Disease Different Between Patients in The East and West?Document2 pagesIs Primary Sclerosing Cholangitis With Inflammatory Bowel Disease Different Between Patients in The East and West?RobertVellaZammitNo ratings yet
- Advance Gastroparese DMDocument7 pagesAdvance Gastroparese DMAdis MahayanaNo ratings yet
- Jurnal Kel. 2Document11 pagesJurnal Kel. 2ho himmaNo ratings yet
- Penting PIIS0016508597004976Document5 pagesPenting PIIS0016508597004976afifahridhahumairahhNo ratings yet
- Nutrients 13 01628 v2Document23 pagesNutrients 13 01628 v2AnirisulNo ratings yet
- Loss of Muscle Strength in Patients Under Hemodialysis Evaluated by Dynamometry in The Mexican PopulationDocument6 pagesLoss of Muscle Strength in Patients Under Hemodialysis Evaluated by Dynamometry in The Mexican PopulationIsabel MarrugoNo ratings yet
- Review: Epidemiology, Mechanisms, and Management of Diabetic GastroparesisDocument8 pagesReview: Epidemiology, Mechanisms, and Management of Diabetic GastroparesisIrma KurniawatiNo ratings yet
- HHS Public Access: Author ManuscriptDocument20 pagesHHS Public Access: Author ManuscriptMarin GregurinčićNo ratings yet
- Gut Microbiota Is Altered in Patients With Alzheimer's DiseaseDocument10 pagesGut Microbiota Is Altered in Patients With Alzheimer's DiseaseaedrNo ratings yet
- (DR Dito Anurogo MSC) Materi Kuliah Biokimia - Jumat 17 Dec 2021Document61 pages(DR Dito Anurogo MSC) Materi Kuliah Biokimia - Jumat 17 Dec 2021Ziqriyah AfifahNo ratings yet
- Association Between The Level of Quality of Life and Nutritional Status in Patients Undergoing Chronic Renal HemodialysisDocument10 pagesAssociation Between The Level of Quality of Life and Nutritional Status in Patients Undergoing Chronic Renal HemodialysisVione rizkiNo ratings yet
- Effectiveness of Curry Leaf and Mint Decoction On Indigestion Among Geriatric Clients at Kondancherry Village, Thiruvallur DistrictDocument5 pagesEffectiveness of Curry Leaf and Mint Decoction On Indigestion Among Geriatric Clients at Kondancherry Village, Thiruvallur DistrictEditor IJTSRDNo ratings yet
- NIH Public Access: Author ManuscriptDocument15 pagesNIH Public Access: Author ManuscriptAdichita Khaira RidatasatriaNo ratings yet
- Petri 2020Document8 pagesPetri 2020afifahridhahumairahhNo ratings yet
- Narrative Review SampleDocument10 pagesNarrative Review SampleSvt Mscofficial2No ratings yet
- Nickel 2019Document14 pagesNickel 2019Bandac AlexandraNo ratings yet
- Probiotic Supplementation in CKD - Double-Blind, Randomized, Placebo TrialsDocument9 pagesProbiotic Supplementation in CKD - Double-Blind, Randomized, Placebo TrialsVinod KumarNo ratings yet
- He 2001Document8 pagesHe 2001afifahridhahumairahhNo ratings yet
- Ibs JurnalDocument11 pagesIbs JurnalimuhammadfahmiNo ratings yet
- SPW Diazoxide CholinDocument10 pagesSPW Diazoxide CholinlailagsazNo ratings yet
- Ulcer and HelicobacterDocument10 pagesUlcer and HelicobacterLiliana L SalazarNo ratings yet
- Ren 2020 Alteraciones MicrobiotaDocument14 pagesRen 2020 Alteraciones MicrobiotaMartin GomezNo ratings yet
- Am J Physiol Gastrointest Liver Physiol-2002-Wade-G489-95Document8 pagesAm J Physiol Gastrointest Liver Physiol-2002-Wade-G489-95Regina Marhadi SoniNo ratings yet
- Clinical Prognosis GI LymphomaDocument8 pagesClinical Prognosis GI LymphomaDasep Bambang PurnamaNo ratings yet
- Gastroenterology: World Journal ofDocument18 pagesGastroenterology: World Journal ofHana Nuraisa BasyaNo ratings yet
- Gastropaty Diabetic 4Document18 pagesGastropaty Diabetic 4Andi mayasari usmanNo ratings yet
- Desai 2018Document7 pagesDesai 2018afifahridhahumairahhNo ratings yet
- JCM 8071042Document17 pagesJCM 8071042Ma José EstébanezNo ratings yet
- Barret 2015.Document6 pagesBarret 2015.Elizabeth VegaNo ratings yet
- Chronic Kidney Disease: Christian Delles and Raymond VanholderDocument2 pagesChronic Kidney Disease: Christian Delles and Raymond VanholderYashinta MaharaniNo ratings yet
- WJG 23 6137Document16 pagesWJG 23 6137MUHAMMAD09No ratings yet
- Alteración de La Microbiota Intestinal en Pacientes Con Enfermedad de Alzheimer (Zhuang Et Al., 2018)Document10 pagesAlteración de La Microbiota Intestinal en Pacientes Con Enfermedad de Alzheimer (Zhuang Et Al., 2018)Centro integral del desarrollo LogrosNo ratings yet
- Functional Gastrointestinal Disorders 3: SeriesDocument14 pagesFunctional Gastrointestinal Disorders 3: SeriesDimas RizkyNo ratings yet
- Emerging Therapeutic Options For Non-Alcoholic Fatty Liver DiseaseDocument13 pagesEmerging Therapeutic Options For Non-Alcoholic Fatty Liver Diseasew57t4yrkt6No ratings yet
- BSN3J-3K G2 Peptic-UlcerDocument60 pagesBSN3J-3K G2 Peptic-UlcerCharisse CaydanNo ratings yet
- 09 Antigen Cancer 2017 DecDocument12 pages09 Antigen Cancer 2017 DecGabriela MilitaruNo ratings yet
- It Is Time To Review Concepts On Renal Involvement in Leprosy Pre and Post Treatment Evaluation of 189 PatientsDocument5 pagesIt Is Time To Review Concepts On Renal Involvement in Leprosy Pre and Post Treatment Evaluation of 189 PatientsAdhyt PratamaNo ratings yet
- Umeno2018 Article ClinicalFeaturesOfChronicEnterDocument9 pagesUmeno2018 Article ClinicalFeaturesOfChronicEnterzhe zhNo ratings yet
- Giglio 2018Document11 pagesGiglio 2018yafanitaizzatiNo ratings yet
- Clinical Guidelines Secondary Prevention of Gastric CancerDocument1 pageClinical Guidelines Secondary Prevention of Gastric Cancerhenrique.uouNo ratings yet
- Complex Gastrointestinal and Endocrine Sources ofDocument9 pagesComplex Gastrointestinal and Endocrine Sources ofBianca CaterinalisendraNo ratings yet
- Gastric Neuroendocrine Tumor: Review and UpdateDocument5 pagesGastric Neuroendocrine Tumor: Review and UpdateGonzalez ByronNo ratings yet
- Nutrigenomics Research: A ReviewDocument14 pagesNutrigenomics Research: A ReviewpuspitaNo ratings yet
- 2.1 Neurodegeneracion y Microbioma Intestinal 2021Document13 pages2.1 Neurodegeneracion y Microbioma Intestinal 2021ElizabethNo ratings yet
- Wis 1Document12 pagesWis 1Anonymous XOA037bAdXNo ratings yet
- 1 s2.0 S1051227619300020 MainDocument9 pages1 s2.0 S1051227619300020 MainRomário de Macedo EspíndolaNo ratings yet
- Management of Occult GI Bleeding: A Clinical GuideFrom EverandManagement of Occult GI Bleeding: A Clinical GuideMicheal TadrosNo ratings yet
- Essential Medical Disorders of the Stomach and Small Intestine: A Clinical CasebookFrom EverandEssential Medical Disorders of the Stomach and Small Intestine: A Clinical CasebookNo ratings yet
- Deboer 1992Document6 pagesDeboer 1992afifahridhahumairahhNo ratings yet
- Yang Shu 2017Document11 pagesYang Shu 2017afifahridhahumairahhNo ratings yet
- Camilleri 1984Document8 pagesCamilleri 1984afifahridhahumairahhNo ratings yet
- Malagelada 1980Document8 pagesMalagelada 1980afifahridhahumairahhNo ratings yet
- Regalia 2002Document8 pagesRegalia 2002afifahridhahumairahhNo ratings yet
- Aliment Pharmacol Ther - 2002 - de Block - Helicobacter Pylori Parietal Cell Antibodies and Autoimmune Gastropathy in TypeDocument9 pagesAliment Pharmacol Ther - 2002 - de Block - Helicobacter Pylori Parietal Cell Antibodies and Autoimmune Gastropathy in TypeafifahridhahumairahhNo ratings yet
- Barnett 1988Document6 pagesBarnett 1988afifahridhahumairahhNo ratings yet
- Gangula 2007Document10 pagesGangula 2007afifahridhahumairahhNo ratings yet
- 659 FullDocument6 pages659 FullafifahridhahumairahhNo ratings yet
- Guy 1984Document6 pagesGuy 1984afifahridhahumairahhNo ratings yet
- Meldgaard Et Al 2019 Pathophysiology and Management of Diabetic GastroenteropathyDocument17 pagesMeldgaard Et Al 2019 Pathophysiology and Management of Diabetic GastroenteropathyafifahridhahumairahhNo ratings yet
- Schmidt 2009Document12 pagesSchmidt 2009afifahridhahumairahhNo ratings yet
- Perdue 1988Document6 pagesPerdue 1988afifahridhahumairahhNo ratings yet
- Mark Feldman 1979Document6 pagesMark Feldman 1979afifahridhahumairahhNo ratings yet
- Lies 2014Document12 pagesLies 2014afifahridhahumairahhNo ratings yet
- Yarandi 2014Document14 pagesYarandi 2014afifahridhahumairahhNo ratings yet
- Harberson 2009Document12 pagesHarberson 2009afifahridhahumairahhNo ratings yet
- Raj K. Goyal 2018Document14 pagesRaj K. Goyal 2018afifahridhahumairahhNo ratings yet
- Iwasaki Hirohiko 2006Document12 pagesIwasaki Hirohiko 2006afifahridhahumairahhNo ratings yet
- s41598 023 42674 1Document14 pagess41598 023 42674 1afifahridhahumairahhNo ratings yet
- Duchen 1980Document3 pagesDuchen 1980afifahridhahumairahhNo ratings yet
- Analisa Risiko Kecelakaan Kerja Pada Proyek Konstruksi Jembatan Musi Vi PalembangDocument6 pagesAnalisa Risiko Kecelakaan Kerja Pada Proyek Konstruksi Jembatan Musi Vi PalembangRoraNo ratings yet
- Psychological Report: I. Personal Data / Identification DataDocument3 pagesPsychological Report: I. Personal Data / Identification DataRoger Jhon BravoNo ratings yet
- Week 5 The Global North and SouthDocument12 pagesWeek 5 The Global North and SouthAdrienne Joielle MartinezNo ratings yet
- HA Filler Injection and Skin Quality-Literature MiDocument9 pagesHA Filler Injection and Skin Quality-Literature MiEnt IMDCNo ratings yet
- OASIS Item Guidance Patient History & Diagnoses Oasis ItemDocument20 pagesOASIS Item Guidance Patient History & Diagnoses Oasis ItembiskwetNo ratings yet
- Lesson 4 Pe 1Document11 pagesLesson 4 Pe 1Maya RosarioNo ratings yet
- 1.preface The International Pharmacopoeia, Eleventh EditionDocument3 pages1.preface The International Pharmacopoeia, Eleventh EditionLIZ NORMA ARROYO TORRESNo ratings yet
- Detailed Lesson Plan in Physical Education Grade 4Document6 pagesDetailed Lesson Plan in Physical Education Grade 4Myca HernandezNo ratings yet
- Admit Card: Instructions To The CandidateDocument1 pageAdmit Card: Instructions To The CandidateGaurav YadavNo ratings yet
- CAPE Communication Studies 2009 P3BDocument4 pagesCAPE Communication Studies 2009 P3BRiaz JokanNo ratings yet
- Physical Exercise and Executive Functions in Preadolescent Children, Adolescents and Young Adults - A Meta-AnalysisDocument9 pagesPhysical Exercise and Executive Functions in Preadolescent Children, Adolescents and Young Adults - A Meta-AnalysisPedro J. Conesa CerveraNo ratings yet
- Epidemiology AssignmentDocument12 pagesEpidemiology AssignmentSagar ParajuliNo ratings yet
- Moh. Fahmi Suratinoyo - 0301777 - OsteomielitisDocument43 pagesMoh. Fahmi Suratinoyo - 0301777 - OsteomielitisFahmiNo ratings yet
- Cardio DrugsDocument58 pagesCardio DrugsMARIA ROWENA VIA J. LUCENANo ratings yet
- Muhammad Awais: ContactDocument1 pageMuhammad Awais: ContactMian AwaisNo ratings yet
- Lipo Contrast Cryo BrochureDocument5 pagesLipo Contrast Cryo BrochureSerenity ZhangNo ratings yet
- Routes of Admin (Cology1)Document35 pagesRoutes of Admin (Cology1)ROSENo ratings yet
- Biotechnology 8 Q4-Week1 LASDocument4 pagesBiotechnology 8 Q4-Week1 LASSean Maximus M. PanganibanNo ratings yet
- Improving Healthcare Warehouse Operations Through 5SDocument14 pagesImproving Healthcare Warehouse Operations Through 5SIbrahim SkakriNo ratings yet
- Midterm Quiz#1Document6 pagesMidterm Quiz#1AIRINI MAY L. GUEVARRANo ratings yet
- 1 s2.0 S2212443823000371 MainDocument11 pages1 s2.0 S2212443823000371 MainMirza GlusacNo ratings yet
- The Effects of Infant Massage On Maternal PostpartumDocument6 pagesThe Effects of Infant Massage On Maternal PostpartumopanocayNo ratings yet
- Lyceum of The Philippines UniversityDocument2 pagesLyceum of The Philippines UniversityVon Matthew BarcialNo ratings yet
- Hse Training MatrixDocument3 pagesHse Training Matrixjoenediath9345No ratings yet
- Hari KE Hari/Tgl Imam Kultum Badal BilalDocument4 pagesHari KE Hari/Tgl Imam Kultum Badal Bilalsyubban afifNo ratings yet
- HMB342 Course Syllabus Summer 2020Document5 pagesHMB342 Course Syllabus Summer 2020WangNo ratings yet
Grover M 2012
Grover M 2012
Uploaded by
afifahridhahumairahhCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Grover M 2012
Grover M 2012
Uploaded by
afifahridhahumairahhCopyright:
Available Formats
NIH Public Access
Author Manuscript
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Published in final edited form as:
NIH-PA Author Manuscript
Neurogastroenterol Motil. 2012 June ; 24(6): 531–e249. doi:10.1111/j.1365-2982.2012.01894.x.
Clinical-histological associations in gastroparesis: Results from
the Gastroparesis Clinical Research Consortium
The NIDDK Gastroparesis Clinical Research Consortium (GpCRC)*
Abstract
Background—Cellular changes associated with diabetic (DG) and idiopathic gastroparesis (IG)
have recently been described from patients enrolled in the Gastroparesis Clinical Research
Consortium. The association of these cellular changes with gastroparesis symptoms and gastric
emptying is unknown.
Aim—Relate cellular changes to symptoms and gastric emptying in patients with gastroparesis.
Methods—Earlier, using full thickness gastric body biopsies from 20 DG, 20 IG and 20 matched
NIH-PA Author Manuscript
controls, we found decreased interstitial cells of Cajal (ICC) and enteric nerves and an increase in
immune cells in both DG and IG. Here, demographic, symptoms (gastroparesis cardinal symptom
index score), and gastric emptying were related to cellular alterations using Pearson’s correlation
coefficients.
Results—ICC counts inversely correlated with 4 hours gastric retention in DG but not in IG (r=
−0.6, p=0.008, DG, r=0.2, p=0.4, IG). There was also a significant correlation between loss of ICC
and enteric nerves in DG but not in IG (r=0.5, p=0.03 for DG, r=0.3, p=0.16, IG). IG with a
myenteric immune infiltrate scored higher on the average GCSI (3.6±0.7 vs 2.7±0.9, p=0.05) and
nausea score (3.8±0.9 vs 2.6±1.0, p=0.02) as compared to those without an infiltrate.
Conclusions—In DG, loss of ICC is associated with delayed gastric emptying. ICC or enteric
nerve loss did not correlate with symptom severity. Overall clinical severity and nausea in IG is
associated with a myenteric immune infiltrate. Thus, full thickness gastric biopsies can help define
Send correspondence to: Gianrico Farrugia, MD, Mayo Clinic, 200 First Street SW, Rochester MN, 55905, Tel 507 284 4695, Fax 507
NIH-PA Author Manuscript
284 0266, farrugia.gianrico@mayo.edu.
*Writing Committee: Madhusudan Grover (Mayo Clinic, Rochester, MN), Cheryl E. Bernard (Mayo Clinic, Rochester, MN), Pankaj
J. Pasricha (Stanford University, Palo Alto, CA), Matthew S. Lurken (Mayo Clinic, Rochester, MN), Maria Simonetta Faussone-
Pellegrini (University of Florence, Florence Italy), Thomas C Smyrk (Mayo Clinic, Rochester, MN), Henry P. Parkman (Temple
University, Philadelphia, PA), Thomas L. Abell (University of Mississippi, Jackson, MS), William J. Snape (California Pacific
Medical Center, San Francisco, CA), William L. Hasler (University of Michigan, Ann Arbor, MI), Richard W. McCallum (Texas
Tech University Health Sciences Center), Linda Nguyen (Stanford University, Palo Alto, CA), Kenneth L. Koch, Jorges Calles, MD
(Wake Forest University, Winston-Salem, NC), Linda Lee, James Tonascia, Aynur Ünalp-Arida (Johns Hopkins University,
Baltimore, MD), Frank A. Hamilton (National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD), and Gianrico
Farrugia (Mayo Clinic, Rochester, MN).
Authors contributions
Henry Parkman, Thomas Abell, William Snape, Pankaj J. Pasricha, Madhusudan Grover, Gianrico Farrugia: Acquisition of tissue and
drafting of manuscript, critical review of the manuscript for important intellectual content, study concept and design, analysis and
interpretation of data, critical revision of the data for important intellectual content, obtained funding.
Matthew Lurken, Cheryl Bernard, Maria Simonetta Faussone-Pellegrini, Thomas Smyrk: Study concept and design, analysis and
interpretation of data, critical revision of the data for important intellectual content.
William Hasler, Richard McCallum, Aynur Unalp-Arida, Linda Nguyen, Kenneth Koch, Jorges Calles, Linda Lee, James Tonascia,
Frank Hamilton: Analysis, interpretation of data, critical revision of the manuscript for important intellectual content.
Potential competing interests: None
Conflict of interest: None
Disclosures: There were no financial, professional or personal disclosures from any of the authors.
Page 2
specific cellular abnormalities in gastroparesis, some of which are associated with physiological
and clinical characteristics of gastroparesis.
NIH-PA Author Manuscript
Keywords
gastric emptying; gastroparesis; enteric nervous system; interstitial cells of Cajal; macrophages;
clinical symptoms
Introduction
Gastroparesis is a gastric motility disorder characterized by delayed gastric emptying (GE)
in the absence of mechanical obstruction 1. The clinical syndrome comprises of nausea,
vomiting, bloating, early satiety and abdominal pain 2 . It is an increasingly recognized
complication of both Type 1 and Type 2 diabetes.3 Other less common causes are post-
surgical and medication related, however, a cause remains unknown in a significant
proportion of patients characterized as idiopathic.4
Gastroparesis related morbidity seems to be on the rise. From 1995 to 2004, there has been a
158% increase in hospitalizations with gastroparesis with gastroparetics incurring higher
hospitalization costs compared to other upper gastrointestinal (GI) disorders.5 The age-
adjusted incidence of gastroparesis per 100,000 person-years was 2.4 for men and 9.8 for
NIH-PA Author Manuscript
women for years 1996–2006 from Olmsted County, Minnesota and corresponding
prevalence figures were 9.6 for men and 37.8 for women per 100,000 persons. In this study,
overall survival was found to be significantly lower than the age- and sex-specific survival
of general population.6 In spite of increasing recognition and morbidity associated with the
condition in last two decades, therapeutic options continue to remain limited at best. A
major limiting factor in the development of targeted therapy is the lack of understanding of
cellular etiopathogenesis in human gastroparesis.7
A few retrospective studies have defined abnormalities in cell types required for a normal
gastric function such as loss of interstitial cells of Cajal (ICC) and neuronal nitric oxide
synthase (nNOS).8–11 Loss of ICC has been associated with gastric dysrhythmias and worse
clinical symptoms.12, 13 Until recently, detailed analysis of various cell types, including the
extrinsic innervation to the stomach, enteric nerves, glia, smooth muscle cells, ICC and
immune cells was not available. In order to meet this need, the National Institutes of
Diabetes and Digestive and Kidney Diseases (NIDDK) Gastroparesis Clinical Research
Consortium(GpCRC) was established in 2006 to prospectively enroll patients, obtain
detailed clinical data and collect full thickness gastric tissue in a standardized approach. We
recently described the cellular changes associated with diabetic (DG) and idiopathic (IG)
NIH-PA Author Manuscript
gastroparesis from GpCRC patients.14 On quantitative comparisons, the most commonly
observed findings were loss of ICC and an immune infiltrate characterized by an increase in
CD45 and CD68 immunoreactivity in both DG and IG. A 14–17% decrease in the number
of enteric nerve fibers as defined by Protein Gene Product 9.5 (PGP9.5) immunoreactivity
was also seen. Less common were changes in nNOS, vasoactive intestinal peptide (VIP),
substance P (SP) and tyrosine hydroxylase (TH).
The primary aim of this study was to determine associations, in both DG and IG, between
specific histological markers of gastroparesis (ICC loss, nerve fiber loss and immune
infiltrate) and specific clinical features (scintigraphically determined impairment in GE and
worsening in standardized symptom scores). A secondary aim was to explore associations of
less commonly histological features such as nNOS, SP, VIP and TH expression with GE and
clinical symptoms.
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 3
Methods
Subject enrollment
NIH-PA Author Manuscript
The NIDDK GpCRC consists of a network of seven centers and one data coordinating
center collaborating for research on gastroparesis. The Gastroparesis Registry is an
observational study to clarify the epidemiology, natural history, clinical course and other
outcomes of gastroparesis (ClinicalTrials.gov identifier: NCT00398801). The Gastroparesis
Registry consists of patients > 18 years of age with symptoms of at least 12 week duration,
delayed GE on scintigraphy (> 60% retention at 2 hour or > 10% retention at 4 hour), and no
evidence of obstruction. Exclusion criteria included presence of active inflammatory bowel
disease, eosinophilic gastroenteritis, neurological conditions, acute liver or renal failure, and
history of total or subtotal gastric resection. Registry data at enrollment include detailed
history and physical examinations, validated symptom questionnaires, upper endoscopy, 4-
hour GE, and laboratory tests.
Clinical questionnaires
Patients were questioned about the onset of their symptoms and if they had an initial
infectious prodrome. Each patient filled out the 20-item Patient Assessment of Upper
Gastrointestinal Disorders Symptoms Severity Index (PAGI-SYM) questionnaire, which
assesses symptoms of gastroparesis, dyspepsia, and gastroesophageal reflux disease. It
NIH-PA Author Manuscript
includes the 9 symptoms consisting the Gastroparesis Cardinal Symptom Index (GCSI),
which asks about nausea, retching, vomiting, stomach fullness, inability to finish a meal,
excessive fullness, loss of appetite, bloating, and abdominal distention 15. The GCSI equals
the summation of the nausea/vomiting subscore (nausea, retching, and vomiting),
postprandial fullness/early satiety subscore (stomach fullness, inability to finish a meal,
excessive fullness, and loss of appetite), and bloating subscore (bloating and large stomach).
Patients were asked to assess the severity of their symptoms in previous 2 weeks on a 0 to 5
Likert scale (no symptoms = 0, very mild = 1, mild = 2, moderate = 3, severe = 4, very
severe = 5).
Gastric Emptying
Gastric emptying scintigraphy was performed using a low-fat egg white meal with imaging
at 0, 1, 2, and 4 hours after meal ingestion using the standardized protocol to estimate
percent gastric retention.16 This protocol ensures standardized information about delayed
GE across all participating sites. With this protocol, delayed GE is characterized by percent
gastric retention at any of the time points and can also be classified according to the gastric
retention at 4 hours as mild (≤20% gastric retention at 4 hours), moderate (>20 to 35%), and
severe (>35%).2
NIH-PA Author Manuscript
Laboratory studies
Laboratory tests obtained on each patient included complete blood cell count with
erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and glycosylated
hemoglobin (HbA1c).
Histology studies
Tissue was obtained from 20 DG and 20 IG patients undergoing surgery for placement of a
gastric stimulator and from 20 age and sex matched patients undergoing duodenal switch
gastric bypass surgery following IRB approved protocols. The full-thickness gastric biopsies
were collected in all subjects from the anterior aspect of the stomach, midway between the
greater and lesser curvatures where the gastroepiploic vessels meet. Details on tissue
acquisition and processing are provided elsewhere.14 Various components of the enteric
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 4
nervous system (ENS) were studied using antibodies to PGP9.5, nNOS, VIP (inhibitory
innervation), SP (excitatory inhibition), and TH (extrinsic motor innervation). For
examining ICC, c-Kit antibody was used and CD45 was used as a general cell marker for
NIH-PA Author Manuscript
immune infiltrate14.
Statistical Analysis
The histological markers for ICC (c-Kit), enteric nerves (PGP9.5) and immune infiltrate
(CD45) were used for clinical correlations as outlined in specific aim 1. Patients with marker
values ≥ 25% compared to normal were categorized as increased on that marker and those
with values ≤ 25% compared to normal were categorized as decreased on that marker.
Demographic and other characteristics were compared between those with and without
changes in these histological markers in both DG and IG using t-test (continuous
characteristics) and chi-square or Fisher’s exact test (categorical characteristics). For
continuous characteristics, groups with increased and decreased markers were expressed as
means ± standard deviations. Simple Pearson’s correlation analysis was done to relate the
histological markers (as measured) to the two key clinical variables indicative of symptoms
(average GCSI score) and delay in gastric emptying (% gastric retention at 4 hours). All
statistical analyses were carried out using GraphPad 4 software (GraphPad software Inc., La
Jolla, California. A p-value of <0.05 was considered statistically significant. Exact p-values
were used and these were not corrected for multiple comparisons.
NIH-PA Author Manuscript
Results
Diabetic Gastroparetics
Circular muscle ICC loss—There was a 48% decrease in overall quantification of ICC
in DG compared to controls (2.8±0.4 vs. 5.3±0.2 cells/ high power field, p<0.0001). Ten of
the twenty patients (50%) with DG were identified as having depleted number of ICC based
on a ≥ 25% drop. The group with depleted ICC was older than the group with normal ICC
(52.2±13.1 yr vs. 39.2±11.6 yr, p=0.03) but both groups were similar in terms of gender
distribution. There were no differences in terms of diabetes type (Type I or II), duration or
control (determined by HbA1c). The group with depleted ICC had significantly higher 4-
hour gastric retention as compared those with normal ICC (47.6±25.6% vs. 22±9.4%,
p=0.01) as shown in Table 1. ICC counts and gastric retention at 4 hours were inversely
correlated (r=−0.59, P=0.008, Fig. 1A). Within the group with depleted ICC, six patients
(60%) had severe gastric retention (> 35% at 4-hours) while 4 (40%) had mild to moderate
gastric retention. Of the ten patients with normal ICC bodies, only one (10%) had severe
gastric retention. There were no significant correlations between the average GCSI score and
ICC numbers (Fig. 1D)
NIH-PA Author Manuscript
Myenteric plexus immune cell infiltrate—There was an overall 25% increase in the
CD45 expression in DG when compared to controls (25.5±1.5 vs. 20.3±1.1 cells/high power
field, p=0.002). Nine of the twenty patients (45%) with DG were found to have ≥ 25%
increase in CD45 staining cells in the myenteric plexus. The groups with or without immune
infiltrate were similar in age, sex, or history of infectious prodrome. There were no
differences in terms of diabetes type, duration or control. Laboratory parameters such as
leukocyte count, CRP, and ESR were similar in both the groups. No significant correlations
were found between CD45 infiltrate and GE (Fig. 1B) or average GCSI (Fig. 1E). The
circular muscle CD45 expression was not different in DG when compared to controls
(16.9±0.8 vs. 14.3±0.7 cells/high power field, p=0.06).
Circular muscle enteric nerve fiber loss—There was a 17% overall decrease in the
expression of nerve fiber marker PGP9.5 (36.5±1.8 vs. 44.3±2.3 fibers/high power field,
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 5
p=0.01). Only four of the twenty patients (20%) with DG were found to have a PGP9.5
decrease of ≥ 25%. There were no differences in age, gender, diabetes type or duration
amongst the two groups. Furthermore, no correlations were found between PGP9.5 and GE
NIH-PA Author Manuscript
(Fig. 1C) or between PGP9.5 and average GCSI (Fig. 1F).
Correlation between ICC loss, nerve fiber loss and immune infiltrate—There
was a significant correlation between loss of ICC bodies and PGP9.5 fibers in DG (r=0.47,
p=0.03) (Fig. 2A). However, immune infiltrate was not correlated with ICC or nerve fiber
loss.
Inhibitory (nNOS, VIP) and excitatory (Substance P) enteric nervous system
and extrinsic innervation (Tyrosine hydroxylase)—Table 2 shows correlation
coefficients between nNOS positive myenteric neurons, nNOS positive nerve fibers, VIP,
SP, TH with GE and average GCSI. There were no significant correlations between these
markers and GE or average GCSI.
Idiopathic Gastroparetics
Circular muscle ICC loss—There was a 39% decrease in overall quantification of ICC
in IG when compared to controls (3.2±0.4 vs. 5.3±0.2 cells/high power field, p<0.0001).
Ten of the twenty patients with IG were characterized as having ICC loss (50%). There was
NIH-PA Author Manuscript
a similar age and sex distribution amongst those with or without ICC loss. ICC loss did not
correlate with gastric emptying as shown in figure 3A or average GCSI (Fig. 3D).
Myenteric plexus immune infiltrate—There was an overall 30% increase in the CD45
expression in IG when compared to controls (26.5±1.2 vs. 20.3±1.1 cells/high power field,
p=0.002). Fourteen of the twenty IG patients (70%) had ≥ 25% increase. The groups with
and without immune infiltrate did not differ in terms of age, sex, or history of infection.
Leukocyte count, CRP and ESR were similar in both the groups. Overall GCSI was higher
in individuals with myenteric plexus CD45 infiltrate (3.6±0.7 vs. 2.7±0.9, p=0.05). On
comparing the sub-scores, this was found to be predominantly secondary to higher nausea
score amongst those with CD45 infiltrate (3.8±0.9 vs. 2.6±1.0, p=0.02) as shown in Table 1.
However, the correlation between quantitative levels of CD45 and GE (Fig. 3B) or GCSI did
not reach statistical significance (Fig. 3E). The circular muscle CD45 expression was not
different in IG when compared to controls (16.5±0.8 vs. 14.3±0.7 cells/high power field,
p=0.06).
Circular muscle Nerve fiber loss—There was a 14% overall decrease in the PGP9.5
expression (38±1.5 vs. 44.3±2.3 fibers/high power field, p=0.01). Five of the twenty IG had
NIH-PA Author Manuscript
a ≥ 25% dropout. Age and sex were similar between those with and without PGP9.5 loss.
Furthermore, no correlations existed between PGP9.5 quantification and GE (Fig. 3C) and
GCSI (Fig. 3F).
Correlation between ICC loss, nerve loss and immune infiltrate—Unlike DG,
ICC and nerve fiber loss were not correlated with each other (Fig. 2D). There was no
correlation between ICC loss, nerve loss and immune infiltrate in IG.
Inhibitory (nNOS, VIP) and excitatory (Substance P) enteric nervous system
and extrinsic innervation (Tyrosine hydroxylase)—Table 2 shows correlation
coefficients between nNOS positive myenteric neurons, nNOS positive nerve fibers, VIP,
SP, TH with GE and average GCSI. There were no significant correlations between these
markers and GE or average GCSI.
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 6
Discussion
Gastroparesis continues to be a clinically challenging syndrome with limited insights into its
NIH-PA Author Manuscript
pathophysiology and no major breakthroughs in treatment options.17 The cellular defects in
human gastroparesis had not been comprehensively studied until recently and no substantive
data is available on correlations between various cellular defects and gastric function or
clinical symptoms. ICC are a key component of the gut control mechanisms.18 Loss of ICC
is the most common and most consistently reported cellular defect in animal models of DG
and in human gastroparesis. Significant loss of ICC at 12 weeks was observed in gastric
antrum of streptozotocin induced diabetic rats,19 and similar observations have been made in
the non obese diabetic (NOD) mice.20, 21 Amongst human studies, profound loss of ICC in
the antrum in a third of patients with refractory gastroparesis was seen.13 In another study,
intramuscular ICC were lost in eight patients with severe diabetes, along with loss of nNOS-
neurons.22 ICC loss correlated with development of delayed GE in NOD mice.20 In human
DG, ICC loss is associated with disruption in the generation and propagation of electrical
slow waves, resulting in gastric dysrhythmias12, 13 associated with abnormal GE.23, 24 Our
study, within the limitations of the relatively small sample size, is the first to describe a
positive correlation between ICC loss and severity of the delay in GE in human DG. The
group with ICC loss had more than twice gastric retention compared to those with normal
ICC.
NIH-PA Author Manuscript
Coordinated gastric motor function relies on intact intrinsic and extrinsic sensorimotor
innervation. It requires acetylcholine and purinergic mediated excitatory stimuli25 but also
VIP, carbon monoxide and nitric oxide (NO) mediated inhibitory stimuli.26 Abnormalities in
both of these ENS components have been described in animal models of DG and humans.
Most common being loss of expression of nNOS.7 Both nNOS knockout27 and
pharmacological inhibition28 have been associated with delayed GE in animal models.
Human data on abnormalities in nNOS and other components of ENS is sparse and is mostly
in form of case reports of diabetics with or without gastroparesis8, 10 with nearly no data on
whether these changes associate with gastric function and clinical symptoms. Even less is
known about ENS changes in IG11, 29. The current study provides the first comprehensive
description of associations between ENS defects and gastric function and symptoms in both
DG and IG. The decrease in pan-neuronal marker PGP9.514 did not correlate with either GE
or gastroparesis severity. This was perhaps not surprising considering relatively minor nerve
dropout in DG (17%) and IG (14%) when compared with controls. A study comparing
appendicial tissue of 6 diabetic patients with controls found no differences in PGP9.5
expression.30 Overall nerve loss as measured by PGP9.5 immunoreactivity may be less
common in gastroparesis than previously thought and it does not correlate with GE or
clinical symptoms. However, even minor neuronal losses when combined with other
NIH-PA Author Manuscript
abnormalities may result in physiological changes. Also it is possible that while the sample
size in the current study is the largest reported sample size may not have been sufficient to
achieve adequate power to detect differences for nerves and other markers. In accordance
with previous animal literature7, 9, 31, 32 and case reports,8, 10, 30 myenteric and muscle
nNOS expression trended to decrease in our DG and IG compared to controls, but this did
not reach significance. In addition, these changes did not correlate with GE or clinical
severity. It remains to be determined if measurement of other forms of nNOS such as
dimerized nNOS correlates better with clinical features.33 Likewise, Substance P
immunostain trended towards a decrease in gastroparetics compared to controls (p=0.06) but
was also not associated with clinical features or GE. Quantitative immunostaining for VIP or
extrinsic innervation (TH) were not different in gastroparetics as compared to controls and
were not associated with GE or symptom severity.
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 7
Recent work has highlighted a potential role for immune cells in the pathophysiology of
gastroparesis. In an animal study, development of diabetes was associated with activation of
a population of heme oxygenase-1 (HO1) positive M2 macrophages (alternatively activated,
NIH-PA Author Manuscript
antiinflammatory).34 Mice that developed delayed GE showed selective loss of these
macrophages and activation of HO1 negative M1 macrophages (proinflammatory). In
addition to our report on myenteric CD45 immune cell infiltrate in both DG and IG,14
Parkman et al have also shown presence of immune infiltrate in a separate cohort of DG 35
and Zarate et al reported lymphocytic immune infiltrate in muscle layer of a single patient
with IG.11 In this study, we find that IG with an infiltrate scored higher on average GCSI,
especially the nausea subscale suggesting that these cells might be important in clinical
symptomatology of patients with IG. On visual grading, gastroparetics differed from
controls on staining for macrophages (CD68) and not T (CD3, CD4, CD8) or B lymphocytes
(CD79) suggesting that this infiltrate is from macrophages. A limitation is that CD68, the
most commonly used marker for human macrophages36–38 is not entirely specific. Future
studies are required to explore subpopulations of human macrophages and secreted
cytokines to determine if selective loss or gain of a subtype of these macrophages is more
commonly associated with gastroparesis.
This study highlights the difficulties in correlating symptoms with physiological or
pathophysiological end points. The association between symptoms and GE has been an area
of debate with several studies 39 finding no correlation while others correlating fullness,
NIH-PA Author Manuscript
upper abdominal pain and reduced hunger with delayed GE.40, 41 More recently data from
the GpCRC suggests an association, albeit not very strong, between the severity of GE and
symptoms.4 Given the central influence on symptom perception, the complex physiological
basis for GE and the presence of other factors such as visceral hypersensitivity,42 this is not
too surprising. Future studies will need to compare gastric segmental function and severity
of the GE defect as well as take into account central input on symptom generation in order to
decipher the relative contribution of each factor to symptoms. Also, the region of the human
stomach that is most appropriate to biopsy and the optimal size of the biopsy to account for
patchiness21 remains to be determined. This study also highlights potential differences in the
pathophysiology of DG and IG such as correlation between GE and ICC numbers in DG but
not IG and the stronger association between immune cells and symptoms in IG.
In conclusion, this study describes correlations between clinical, physiological and cellular
changes in a relatively large sample of prospectively enrolled gastroparetics. The main
findings of the paper are that loss of ICC is associated with development of delayed gastric
emptying in DG and that non-lymphocytic myenteric infiltrate correlates with overall
clinical severity and nausea in IG. Full thickness gastric biopsies may help define specific
cellular abnormalities in gastroparesis some of which are associated with physiological and
NIH-PA Author Manuscript
clinical characteristics of gastroparesis.
Acknowledgments
Financial support: The Gastroparesis Clinical Research Consortium (GpCRC) is supported by the National Institute
of Diabetes and Digestive and Kidney Diseases (NIDDK) (grants U01DK073983, U01DK073975, U01DK073985,
U01DK074007, U01DK073974, U01DK074008). This work was also supported by DK57061, DK84567, and PO1
DK68055.
Abbreviations not mentioned in the style guide
PGP9.5 Protein Gene Product 9.5
nNOS neuronal Nitric Oxide Synthase
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 8
VIP Vasoactive Intestinal Peptide
NIH-PA Author Manuscript
ICC interstitial cells of Cajal
GpCRC Gastroparesis Clinical Research Consortium
TH tyrosine hydroxylase
DAPI 4’,6-diamidino-2-phenylindole
SD standard deviation
Members of the Gastroparesis Clinical Research Consortium as of October
2010
Clinical Centers
Stanford University, Stanford, CA: Pankaj Jay Pasricha, MD (Principal Investigator);
Linda Nguyen, MD; Nighat Ullah, MD
California Pacific Medical Center, San Francisco, CA: William Snape, MD (Principal
Investigator); Robin Bishop (2008); Nata DeVole, RN; Mary Greene, MS; Sue Louiseau;
NIH-PA Author Manuscript
Shelly Parker, RN MSN ANP-C ANP; Eve Pillor, RN MSN FNP; Courtney Ponsetto, RN;
Katerina Shetler, MD
Mayo Clinic College of Medicine, Rochester, MN: Gianrico Farrugia, MD (Principal
Investigator); Madhusudan Grover, MD; Cheryl Bernard; Matt Lurken (2007–2009); K.
Robert Shen MD; Michael Sarr, MD; Michael Kendrick, MD
Temple University, Philadelphia, PA: Henry P. Parkman, MD (Principal
Investigator);Steven Kantor; Vanessa Lytes, CRNP; Amiya Palit, MD; Priyanka Sachdeva,
MD; Kellie Simmons, RN; Sean Harbison, MD
Texas Tech University Health Sciences Center: Richard W. McCallum, MD (Principal
Investigator); Reza Hejazi, MD; Irene Sarosiek, MD; Denise Vasquez; Natalia Vega
University of Michigan, Ann Arbor, MI: William Hasler, MD (Principal Investigator);
Michelle Atkinson
University of Mississippi Medical Center, Jackson, MS: Thomas Abell, MD (Principal
Investigator); JoAnne Fordham; Olivia Henry, RD; Archana Kedar, MD; Valerie McNair,
NIH-PA Author Manuscript
LPN II; Danielle Spree, CNP
Wake Forest University, Winston-Salem, NC: Kenneth Koch, MD (Principal
Investigator); Lynn Baxter; Jorge Calles, MD; Samantha Culler; Judy Hooker, RN; Paula
Stuart, PA
Resource Centers
National Institute of Diabetes, Digestive and Kidney Diseases, Bethesda, MD: Frank
Hamilton, MD, MPH (Project Scientist); Steven James, MD; Rebecca Torrance, RN, MSN;
Rebekah Van Raaphorst, MPH
Johns Hopkins University, Bloomberg School of Public Health (Data Coordinating
Center), Baltimore, MD: James Tonascia, PhD (Principal Investigator); Patricia Belt; ;
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 9
Michele Donithan, MHS; Mika Green, MA; Milana Isaacson; ; Linda Lee, MD; ; Kevin
Patrick May; Laura Miriel;Aynur Ünalp-Arida, MD, PhD; Mark Van Natta, MHS; Ivana
Vaughn, MPH; Laura Wilson, ScM; Katherine Yates, ScM
NIH-PA Author Manuscript
References
1. Parkman HP, Hasler WL, Fisher RS. American Gastroenterological A. American
Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis.
Gastroenterology. 2004; 127:1592–1622. [PubMed: 15521026]
2. Camilleri M. Clinical practice. Diabetic gastroparesis. N Engl J Med. 2007; 356:820–829. [PubMed:
17314341]
3. Bytzer P, Talley NJ, Leemon M, Young LJ, Jones MP, Horowitz M. Prevalence of gastrointestinal
symptoms associated with diabetes mellitus: a population-based survey of 15,000 adults. Arch
Intern Med. 2001; 161:1989–1996. [PubMed: 11525701]
4. Parkman HP, Yates K, Hasler WL, et al. Clinical features of idiopathic gastroparesis vary with, sex,
body mass, symptom onset, delay in gastric emptying, and gastroparesis severity. Gastroenterology.
140:101–115. [PubMed: 20965184]
5. Wang YR, Fisher RS, Parkman HP. Gastroparesis-related hospitalizations in the United States:
trends, characteristics, and outcomes, 1995–2004. Am J Gastroenterol. 2008; 103:313–322.
[PubMed: 18047541]
6. Jung HK, Choung RS, Locke GR 3rd, et al. The incidence, prevalence, and outcomes of patients
NIH-PA Author Manuscript
with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology. 2009;
136:1225–1233. [PubMed: 19249393]
7. Vittal H, Farrugia G, Gomez G, Pasricha PJ. Mechanisms of disease: the pathological basis of
gastroparesis--a review of experimental and clinical studies. Nat Clin Pract Gastroenterol Hepatol.
2007; 4:336–346. [PubMed: 17541447]
8. He CL, Soffer EE, Ferris CD, Walsh RM, Szurszewski JH, Farrugia G. Loss of interstitial cells of
cajal and inhibitory innervation in insulin-dependent diabetes. Gastroenterology. 2001; 121:427–
434. [PubMed: 11487552]
9. Choi KM, Gibbons SJ, Roeder JL, et al. Regulation of interstitial cells of Cajal in the mouse gastric
body by neuronal nitric oxide. Neurogastroenterol Motil. 2007; 19:585–595. [PubMed: 17593140]
10. Pasricha PJ, Pehlivanov ND, Gomez G, Vittal H, Lurken MS, Farrugia G. Changes in the gastric
enteric nervous system and muscle: a case report on two patients with diabetic gastroparesis. BMC
Gastroenterol. 2008; 8:21. [PubMed: 18513423]
11. Zarate N, Mearin F, Wang XY, Hewlett B, Huizinga JD, Malagelada JR. Severe idiopathic
gastroparesis due to neuronal and interstitial cells of Cajal degeneration: pathological findings and
management. Gut. 2003; 52:966–970. [PubMed: 12801952]
12. Forster J, Damjanov I, Lin Z, Sarosiek I, Wetzel P, McCallum RW. Absence of the interstitial cells
of Cajal in patients with gastroparesis and correlation with clinical findings. J Gastrointest Surg.
2005; 9:102–108. [PubMed: 15623450]
NIH-PA Author Manuscript
13. Lin Z, Sarosiek I, Forster J, Damjanov I, Hou Q, McCallum RW. Association of the status of
interstitial cells of Cajal and electrogastrogram parameters, gastric emptying and symptoms in
patients with gastroparesis. Neurogastroenterol Motil. 2010; 22:56–61. e10. [PubMed: 19614868]
14. Grover M, Farrugia G, Lurken MS, et al. Cellular changes in diabetic and idiopathic gastroparesis.
Gastroenterology. 2011; 140:1575–1585. e8. [PubMed: 21300066]
15. Rentz AM, Kahrilas P, Stanghellini V, et al. Development and psychometric evaluation of the
patient assessment of upper gastrointestinal symptom severity index (PAGI-SYM) in patients with
upper gastrointestinal disorders. Qual Life Res. 2004; 13:1737–1749. [PubMed: 15651544]
16. Abell TL, Camilleri M, Donohoe K, et al. Consensus recommendations for gastric emptying
scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the
Society of Nuclear Medicine. Am J Gastroenterol. 2008; 103:753–763. [PubMed: 18028513]
17. Kashyap P, Farrugia G. Diabetic gastroparesis: what we have learned and had to unlearn in the past
5 years. Gut. 59:1716–1726. [PubMed: 20871131]
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 10
18. Farrugia G. Interstitial cells of Cajal in health and disease. Neurogastroenterol Motil. 2008;
20(Suppl 1):54–63. [PubMed: 18402642]
19. Wang XY, Huizinga JD, Diamond J, Liu LW. Loss of intramuscular and submuscular interstitial
NIH-PA Author Manuscript
cells of Cajal and associated enteric nerves is related to decreased gastric emptying in
streptozotocin-induced diabetes. Neurogastroenterol Motil. 2009; 21 1095-e92.
20. Choi KM, Gibbons SJ, Nguyen TV, et al. Heme oxygenase-1 protects interstitial cells of Cajal
from oxidative stress and reverses diabetic gastroparesis. Gastroenterology. 2008; 135:2055–2064.
64 e1–2. [PubMed: 18926825]
21. Ordog T, Takayama I, Cheung WK, Ward SM, Sanders KM. Remodeling of networks of
interstitial cells of Cajal in a murine model of diabetic gastroparesis. Diabetes. 2000; 49:1731–
1739. [PubMed: 11016458]
22. Iwasaki H, Kajimura M, Osawa S, et al. A deficiency of gastric interstitial cells of Cajal
accompanied by decreased expression of neuronal nitric oxide synthase and substance P in patients
with type 2 diabetes mellitus. J Gastroenterol. 2006; 41:1076–1087. [PubMed: 17160518]
23. Chen JD, Lin Z, Pan J, McCallum RW. Abnormal gastric myoelectrical activity and delayed
gastric emptying in patients with symptoms suggestive of gastroparesis. Dig Dis Sci. 1996;
41:1538–1545. [PubMed: 8769276]
24. Koch KL. Diabetic gastropathy: gastric neuromuscular dysfunction in diabetes mellitus: a review
of symptoms, pathophysiology, and treatment. Dig Dis Sci. 1999; 44:1061–1075. [PubMed:
10389675]
25. Costa M, Glise H, Sjodahl R. The enteric nervous system in health and disease. Gut. 2000; 47:iv1.
NIH-PA Author Manuscript
[PubMed: 18668961]
26. Shah V, Lyford G, Gores G, Farrugia G. Nitric oxide in gastrointestinal health and disease.
Gastroenterology. 2004; 126:903–913. [PubMed: 14988844]
27. Mashimo H, Kjellin A, Goyal RK. Gastric stasis in neuronal nitric oxide synthase-deficient
knockout mice. Gastroenterology. 2000; 119:766–773. [PubMed: 10982771]
28. Plourde V, Quintero E, Suto G, Coimbra C, Tache Y. Delayed gastric emptying induced by
inhibitors of nitric oxide synthase in rats. Eur J Pharmacol. 1994; 256:125–129. [PubMed:
7519557]
29. Sokol H, Lavergne-Slove A, Mikol J, Sabate JM, Coffin B. Severe isolated myopathic
gastroparesis: a case report with pathological findings. Gut. 2006; 55:1662. [PubMed: 17047114]
30. Miller SM, Narasimhan RA, Schmalz PF, et al. Distribution of interstitial cells of Cajal and
nitrergic neurons in normal and diabetic human appendix. Neurogastroenterol Motil. 2008;
20:349–357. [PubMed: 18069951]
31. Takahashi T, Nakamura K, Itoh H, Sima AA, Owyang C. Impaired expression of nitric oxide
synthase in the gastric myenteric plexus of spontaneously diabetic rats. Gastroenterology. 1997;
113:1535–1544. [PubMed: 9352855]
32. Spangeus A, Suhr O, El-Salhy M. Diabetic state affects the innervation of gut in an animal model
of human type 1 diabetes. Histol Histopathol. 2000; 15:739–744. [PubMed: 10963118]
NIH-PA Author Manuscript
33. Gangula PR, Maner WL, Micci MA, Garfield RE, Pasricha PJ. Diabetes induces sex-dependent
changes in neuronal nitric oxide synthase dimerization and function in the rat gastric antrum. Am J
Physiol Gastrointest Liver Physiol. 2007; 292:G725–G733. [PubMed: 17347455]
34. Choi KM, Kashyap PC, Dutta N, et al. CD206-positive M2 macrophages that express heme
oxygenase-1 protect against diabetic gastroparesis in mice. Gastroenterology. 2010; 138:2399–
2409. 409 e1. [PubMed: 20178793]
35. Harberson J, Thomas RM, Harbison SP, Parkman HP. Gastric Neuromuscular Pathology in
Gastroparesis: Analysis of Full-Thickness Antral Biopsies. Dig Dis Sci. 2010; 10:359–370.
[PubMed: 19997975]
36. Horny HP, Ruck P, Xiao JC, Kaiserling E. Immunoreactivity of normal and neoplastic human
tissue mast cells with macrophage-associated antibodies, with special reference to the recently
developed monoclonal antibody PG-M1. Hum Pathol. 1993; 24:355–358. [PubMed: 8491475]
37. Holness CL, Simmons DL. Molecular cloning of CD68, a human macrophage marker related to
lysosomal glycoproteins. Blood. 1993; 81:1607–1613. [PubMed: 7680921]
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 11
38. Khazen W, M'Bika JP, Tomkiewicz C, et al. Expression of macrophage-selective markers in
human and rodent adipocytes. FEBS Lett. 2005; 579:5631–5634. [PubMed: 16213494]
39. Cassilly DW, Wang YR, Friedenberg FK, Nelson DB, Maurer AH, Parkman HP. Symptoms of
NIH-PA Author Manuscript
gastroparesis: use of the gastroparesis cardinal symptom index in symptomatic patients referred for
gastric emptying scintigraphy. Digestion. 2008; 78:144–151. [PubMed: 19033686]
40. Tack J, Bisschops R, Sarnelli G. Pathophysiology and treatment of functional dyspepsia.
Gastroenterology. 2004; 127:1239–1255. [PubMed: 15481001]
41. Sarnelli G, Caenepeel P, Geypens B, Janssens J, Tack J. Symptoms associated with impaired
gastric emptying of solids and liquids in functional dyspepsia. Am J Gastroenterol. 2003; 98:783–
788. [PubMed: 12738456]
42. Samsom M, Bharucha A, Gerich JE, et al. Diabetes mellitus and gastric emptying: questions and
issues in clinical practice. Diabetes Metab Res Rev. 2009; 25:502–514. [PubMed: 19610128]
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 12
NIH-PA Author Manuscript
NIH-PA Author Manuscript
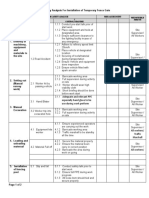
Figure 1.
Correlations between % gastric retention at 4 hours and average GCSI with ICC, CD45
positive myenteric plexus cells and PGP9.5 positive nerve fibers in diabetic gastroparesis A:
ICC and % gastric retention at 4 hours (r=−0.59, p=0.008*, slope=−7.3, 95% CI=−12.4 to
−2.2), B: CD45 positive cells and % gastric retention at 4 hours (r=0.05, p=0.83), C: PGP9.5
nerve fibers and % gastric retention at 4 hours (r=−0.19, p=0.43), D: ICC and GCSI-average
(r=0.10, p=0.69), E: CD45 positive cells and GCSI-average (r=0.13, p=0.63), F: PGP9.5
nerve fibers and GCSI-average (r=0.19, p=0.46).
NIH-PA Author Manuscript
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 13
NIH-PA Author Manuscript
NIH-PA Author Manuscript
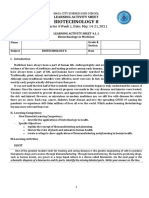
Figure 2.
Correlations between ICC, CD45 positive myenteric plexus cells and PGP9.5 positive nerve
fibers in Diabetic Gastroparesis- A: ICC-PGP9.5 positive nerve fibers (r=0.47, p=0.03*,
slope=0.11, 95% CI=0.008–0.2), B: ICC-CD45 positive myenteric cells (r=0.1, p=0.65), C:
PGP9.5 positive nerve fibers-CD45 positive myenteric cells (r=0.11, p=0.63). Correlations
between ICC, CD45 positive myenteric plexus cells and PGP9.5 positive nerve fibers in
Idiopathic Gastroparesis- D: ICC-PGP9.5 positive nerve fibers (r=0.32, p=0.16), E: ICC-
CD45 positive myenteric cells (r=−0.09, p=0.71), F: PGP9.5 positive nerve fibers-CD45
positive myenteric cells (r=0.06, p=0.78).
NIH-PA Author Manuscript
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 14
NIH-PA Author Manuscript
NIH-PA Author Manuscript
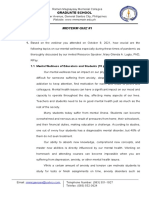
Figure 3.
Correlations between % gastric retention at 4 hours and average GCSI with ICC, CD45
positive myenteric plexus cells and PGP9.5 positive nerve fibers in idiopathic gastroparesis
A: ICC and % gastric retention at 4 hours (r=0.21, p=0.38), B: CD45 positive cells and %
gastric retention at 4 hours (r=−0.10, p=0.68), C: PGP9.5 nerve fibers and % gastric
retention at 4 hours (r=0.22, p=0.37), D: ICC and GCSI-average (r=−0.34, p=0.15), E: CD45
positive cells and GCSI-average (r=0.36, p=0.13), F: PGP9.5 nerve fibers and GCSI-average
(r=0.20, p=0.40).
* Some graphs have less than 20 data points because of missing data on either the counts,
GE or GCSI on these patients.
NIH-PA Author Manuscript
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Table 1
Comparisons of gastric retention and gastric symptoms (GCSI) in diabetic or idiopathic gastroparesis patients with and without cellular alterations: ICC
(Kit) loss, enteric nerves (PGP9.5) loss and increased immune infiltrate (CD45).
ICC ICC P CD45 CD45 P PGP9.5 PGP9.5 P
Low Normal Increased Normal Low (n=4) Normal
(n=10) (n=10) (n=9) (n=11) (n=16)
Diabetic Gastroparesis
% Gastric Retention at 4 hrs (mean±SD) 47.6±25.6 22±9.4 0.01 39.8±26.5 31.6±20.5 0.46 40.2±20.5 34.2±24.4 0.66
GCSI average score (mean±SD) 2.9±1.4 2.8±1.5 0.83 2.8±1.5 2.9±1.4 0.83 2.7±1.6 2.9±1.4 0.79
Idiopathic Gastroparesis
% Gastric Retention at 4 hrs (mean±SD) 17.5±16.8 28.8±16.6 0.17 19.8±15.0 29.6±22.2 0.29 11.2±9.1 26.8±17.8 0.08
GCSI average score (mean±SD) 3.7±1.2 3.2±1.0 0.39 3.6±0.7 2.7±0.9 0.05 3.2±0.6 3.3±0.9 0.88
-Nausea 3.6±1.2 3.2±1.0 0.38 3.8±0.9 2.6±1.0 0.02 3.3±1.2 3.5±1.1 0.80
-Fullness 3.6±1.0 3.6±1.2 0.93 3.8±0.9 3.2±1.4 0.31 3.4±1.0 3.7±1.2 0.58
-Bloating 3.3±1.6 2.2±1.8 0.18 2.9±1.6 2.4±1.9 0.54 3.0±1.6 2.7±1.8 0.76
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 15
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Table 2
Correlations between Inhibitory (nNOS, VIP), excitatory (Substance P) enteric nervous system and extrinsic innervation (Tyrosine hydroxylase) and 4
hour gastric retention and GCSI score.
nNOS nNOS positive VIP positive SP positive TH positive
positive nerve fibers nerve fibers nerve fibers labeling
neurons
Diabetic Gastroparesis
% Gastric Retention at 4 hrs, Correlation coefficient (r) −0.32(p=0.18) −0.03 (p=0.89) −0.13 (p=0.58) −0.35 (p=0.15) −0.12 (p=0.61)
GCSI average score, Correlation coefficient (r) 0.17 (p=0.48) 0.21 (p=0.45) 0.22 (p=0.37) 0.20 (p=0.47) −0.14 (p=0.56)
Idiopathic Gastroparesis
% Gastric Retention at 4 hrs, Correlation coefficient (r) 0.13 (p=0.61) −0.14 (p=0.56) 0.22 (p=0.34) 0.006 (p=0.97) 0.25 (p=0.31)
GCSI average score, Correlation coefficient (r) 0.17 (p=0.45) 0.40 (p=0.06) −0.27 (p=0.26) 0.35 (p=0.13) −0.14 (p=0.56)
Neurogastroenterol Motil. Author manuscript; available in PMC 2013 June 01.
Page 16
You might also like
- Preopanc Trial - PancreasDocument20 pagesPreopanc Trial - PancreasRajalakshmi RadhakrishnanNo ratings yet
- 1 - Participate in Workplace CommunicaitonDocument38 pages1 - Participate in Workplace CommunicaitonSahlee Rose Falcunit GacaNo ratings yet
- ULSADO-JSA - Installation of Temporary Fence GateDocument2 pagesULSADO-JSA - Installation of Temporary Fence GateKelvin TanNo ratings yet
- GLP Vs 17025Document6 pagesGLP Vs 17025Nadhra HaligNo ratings yet
- Acupuncture-Based ModalitiesDocument9 pagesAcupuncture-Based ModalitiesFelipe MaiaNo ratings yet
- Grover 2011Document19 pagesGrover 2011afifahridhahumairahhNo ratings yet
- Pasricha 2008Document8 pagesPasricha 2008afifahridhahumairahhNo ratings yet
- FA - Metabolomic and Biochemical Characterization of A New Model of The Transition of Acute Kidney Injury To Chronic Kidney Disease Induced by Folic AcidDocument26 pagesFA - Metabolomic and Biochemical Characterization of A New Model of The Transition of Acute Kidney Injury To Chronic Kidney Disease Induced by Folic AcidCher IshNo ratings yet
- Pathophysiology, Diagnosis, and Management of Chronic Intestinal Pseudo-ObstructionDocument13 pagesPathophysiology, Diagnosis, and Management of Chronic Intestinal Pseudo-ObstructionJosealberto ArenasNo ratings yet
- Nihms 651235Document9 pagesNihms 651235afifahridhahumairahhNo ratings yet
- Nutrients 14 03959Document15 pagesNutrients 14 03959CrisNo ratings yet
- Nihms 1692401Document23 pagesNihms 1692401jim STAMNo ratings yet
- Harberson 2009Document12 pagesHarberson 2009afifahridhahumairahhNo ratings yet
- Reliability of Mini Nutritional Assessment in Hemodialysis Compared With Subjective Global AssessmentDocument6 pagesReliability of Mini Nutritional Assessment in Hemodialysis Compared With Subjective Global AssessmentyafanitaizzatiNo ratings yet
- Ajpgi 00190 2011 PDFDocument8 pagesAjpgi 00190 2011 PDFAnonymous CQSNUSNo ratings yet
- Acute Abdomen in The Medical Intensive Care Unit: ArticleDocument5 pagesAcute Abdomen in The Medical Intensive Care Unit: ArticleChiriţoiu AnamariaNo ratings yet
- Is Primary Sclerosing Cholangitis With Inflammatory Bowel Disease Different Between Patients in The East and West?Document2 pagesIs Primary Sclerosing Cholangitis With Inflammatory Bowel Disease Different Between Patients in The East and West?RobertVellaZammitNo ratings yet
- Advance Gastroparese DMDocument7 pagesAdvance Gastroparese DMAdis MahayanaNo ratings yet
- Jurnal Kel. 2Document11 pagesJurnal Kel. 2ho himmaNo ratings yet
- Penting PIIS0016508597004976Document5 pagesPenting PIIS0016508597004976afifahridhahumairahhNo ratings yet
- Nutrients 13 01628 v2Document23 pagesNutrients 13 01628 v2AnirisulNo ratings yet
- Loss of Muscle Strength in Patients Under Hemodialysis Evaluated by Dynamometry in The Mexican PopulationDocument6 pagesLoss of Muscle Strength in Patients Under Hemodialysis Evaluated by Dynamometry in The Mexican PopulationIsabel MarrugoNo ratings yet
- Review: Epidemiology, Mechanisms, and Management of Diabetic GastroparesisDocument8 pagesReview: Epidemiology, Mechanisms, and Management of Diabetic GastroparesisIrma KurniawatiNo ratings yet
- HHS Public Access: Author ManuscriptDocument20 pagesHHS Public Access: Author ManuscriptMarin GregurinčićNo ratings yet
- Gut Microbiota Is Altered in Patients With Alzheimer's DiseaseDocument10 pagesGut Microbiota Is Altered in Patients With Alzheimer's DiseaseaedrNo ratings yet
- (DR Dito Anurogo MSC) Materi Kuliah Biokimia - Jumat 17 Dec 2021Document61 pages(DR Dito Anurogo MSC) Materi Kuliah Biokimia - Jumat 17 Dec 2021Ziqriyah AfifahNo ratings yet
- Association Between The Level of Quality of Life and Nutritional Status in Patients Undergoing Chronic Renal HemodialysisDocument10 pagesAssociation Between The Level of Quality of Life and Nutritional Status in Patients Undergoing Chronic Renal HemodialysisVione rizkiNo ratings yet
- Effectiveness of Curry Leaf and Mint Decoction On Indigestion Among Geriatric Clients at Kondancherry Village, Thiruvallur DistrictDocument5 pagesEffectiveness of Curry Leaf and Mint Decoction On Indigestion Among Geriatric Clients at Kondancherry Village, Thiruvallur DistrictEditor IJTSRDNo ratings yet
- NIH Public Access: Author ManuscriptDocument15 pagesNIH Public Access: Author ManuscriptAdichita Khaira RidatasatriaNo ratings yet
- Petri 2020Document8 pagesPetri 2020afifahridhahumairahhNo ratings yet
- Narrative Review SampleDocument10 pagesNarrative Review SampleSvt Mscofficial2No ratings yet
- Nickel 2019Document14 pagesNickel 2019Bandac AlexandraNo ratings yet
- Probiotic Supplementation in CKD - Double-Blind, Randomized, Placebo TrialsDocument9 pagesProbiotic Supplementation in CKD - Double-Blind, Randomized, Placebo TrialsVinod KumarNo ratings yet
- He 2001Document8 pagesHe 2001afifahridhahumairahhNo ratings yet
- Ibs JurnalDocument11 pagesIbs JurnalimuhammadfahmiNo ratings yet
- SPW Diazoxide CholinDocument10 pagesSPW Diazoxide CholinlailagsazNo ratings yet
- Ulcer and HelicobacterDocument10 pagesUlcer and HelicobacterLiliana L SalazarNo ratings yet
- Ren 2020 Alteraciones MicrobiotaDocument14 pagesRen 2020 Alteraciones MicrobiotaMartin GomezNo ratings yet
- Am J Physiol Gastrointest Liver Physiol-2002-Wade-G489-95Document8 pagesAm J Physiol Gastrointest Liver Physiol-2002-Wade-G489-95Regina Marhadi SoniNo ratings yet
- Clinical Prognosis GI LymphomaDocument8 pagesClinical Prognosis GI LymphomaDasep Bambang PurnamaNo ratings yet
- Gastroenterology: World Journal ofDocument18 pagesGastroenterology: World Journal ofHana Nuraisa BasyaNo ratings yet
- Gastropaty Diabetic 4Document18 pagesGastropaty Diabetic 4Andi mayasari usmanNo ratings yet
- Desai 2018Document7 pagesDesai 2018afifahridhahumairahhNo ratings yet
- JCM 8071042Document17 pagesJCM 8071042Ma José EstébanezNo ratings yet
- Barret 2015.Document6 pagesBarret 2015.Elizabeth VegaNo ratings yet
- Chronic Kidney Disease: Christian Delles and Raymond VanholderDocument2 pagesChronic Kidney Disease: Christian Delles and Raymond VanholderYashinta MaharaniNo ratings yet
- WJG 23 6137Document16 pagesWJG 23 6137MUHAMMAD09No ratings yet
- Alteración de La Microbiota Intestinal en Pacientes Con Enfermedad de Alzheimer (Zhuang Et Al., 2018)Document10 pagesAlteración de La Microbiota Intestinal en Pacientes Con Enfermedad de Alzheimer (Zhuang Et Al., 2018)Centro integral del desarrollo LogrosNo ratings yet
- Functional Gastrointestinal Disorders 3: SeriesDocument14 pagesFunctional Gastrointestinal Disorders 3: SeriesDimas RizkyNo ratings yet
- Emerging Therapeutic Options For Non-Alcoholic Fatty Liver DiseaseDocument13 pagesEmerging Therapeutic Options For Non-Alcoholic Fatty Liver Diseasew57t4yrkt6No ratings yet
- BSN3J-3K G2 Peptic-UlcerDocument60 pagesBSN3J-3K G2 Peptic-UlcerCharisse CaydanNo ratings yet
- 09 Antigen Cancer 2017 DecDocument12 pages09 Antigen Cancer 2017 DecGabriela MilitaruNo ratings yet
- It Is Time To Review Concepts On Renal Involvement in Leprosy Pre and Post Treatment Evaluation of 189 PatientsDocument5 pagesIt Is Time To Review Concepts On Renal Involvement in Leprosy Pre and Post Treatment Evaluation of 189 PatientsAdhyt PratamaNo ratings yet
- Umeno2018 Article ClinicalFeaturesOfChronicEnterDocument9 pagesUmeno2018 Article ClinicalFeaturesOfChronicEnterzhe zhNo ratings yet
- Giglio 2018Document11 pagesGiglio 2018yafanitaizzatiNo ratings yet
- Clinical Guidelines Secondary Prevention of Gastric CancerDocument1 pageClinical Guidelines Secondary Prevention of Gastric Cancerhenrique.uouNo ratings yet
- Complex Gastrointestinal and Endocrine Sources ofDocument9 pagesComplex Gastrointestinal and Endocrine Sources ofBianca CaterinalisendraNo ratings yet
- Gastric Neuroendocrine Tumor: Review and UpdateDocument5 pagesGastric Neuroendocrine Tumor: Review and UpdateGonzalez ByronNo ratings yet
- Nutrigenomics Research: A ReviewDocument14 pagesNutrigenomics Research: A ReviewpuspitaNo ratings yet
- 2.1 Neurodegeneracion y Microbioma Intestinal 2021Document13 pages2.1 Neurodegeneracion y Microbioma Intestinal 2021ElizabethNo ratings yet
- Wis 1Document12 pagesWis 1Anonymous XOA037bAdXNo ratings yet
- 1 s2.0 S1051227619300020 MainDocument9 pages1 s2.0 S1051227619300020 MainRomário de Macedo EspíndolaNo ratings yet
- Management of Occult GI Bleeding: A Clinical GuideFrom EverandManagement of Occult GI Bleeding: A Clinical GuideMicheal TadrosNo ratings yet
- Essential Medical Disorders of the Stomach and Small Intestine: A Clinical CasebookFrom EverandEssential Medical Disorders of the Stomach and Small Intestine: A Clinical CasebookNo ratings yet
- Deboer 1992Document6 pagesDeboer 1992afifahridhahumairahhNo ratings yet
- Yang Shu 2017Document11 pagesYang Shu 2017afifahridhahumairahhNo ratings yet
- Camilleri 1984Document8 pagesCamilleri 1984afifahridhahumairahhNo ratings yet
- Malagelada 1980Document8 pagesMalagelada 1980afifahridhahumairahhNo ratings yet
- Regalia 2002Document8 pagesRegalia 2002afifahridhahumairahhNo ratings yet
- Aliment Pharmacol Ther - 2002 - de Block - Helicobacter Pylori Parietal Cell Antibodies and Autoimmune Gastropathy in TypeDocument9 pagesAliment Pharmacol Ther - 2002 - de Block - Helicobacter Pylori Parietal Cell Antibodies and Autoimmune Gastropathy in TypeafifahridhahumairahhNo ratings yet
- Barnett 1988Document6 pagesBarnett 1988afifahridhahumairahhNo ratings yet
- Gangula 2007Document10 pagesGangula 2007afifahridhahumairahhNo ratings yet
- 659 FullDocument6 pages659 FullafifahridhahumairahhNo ratings yet
- Guy 1984Document6 pagesGuy 1984afifahridhahumairahhNo ratings yet
- Meldgaard Et Al 2019 Pathophysiology and Management of Diabetic GastroenteropathyDocument17 pagesMeldgaard Et Al 2019 Pathophysiology and Management of Diabetic GastroenteropathyafifahridhahumairahhNo ratings yet
- Schmidt 2009Document12 pagesSchmidt 2009afifahridhahumairahhNo ratings yet
- Perdue 1988Document6 pagesPerdue 1988afifahridhahumairahhNo ratings yet
- Mark Feldman 1979Document6 pagesMark Feldman 1979afifahridhahumairahhNo ratings yet
- Lies 2014Document12 pagesLies 2014afifahridhahumairahhNo ratings yet
- Yarandi 2014Document14 pagesYarandi 2014afifahridhahumairahhNo ratings yet
- Harberson 2009Document12 pagesHarberson 2009afifahridhahumairahhNo ratings yet
- Raj K. Goyal 2018Document14 pagesRaj K. Goyal 2018afifahridhahumairahhNo ratings yet
- Iwasaki Hirohiko 2006Document12 pagesIwasaki Hirohiko 2006afifahridhahumairahhNo ratings yet
- s41598 023 42674 1Document14 pagess41598 023 42674 1afifahridhahumairahhNo ratings yet
- Duchen 1980Document3 pagesDuchen 1980afifahridhahumairahhNo ratings yet
- Analisa Risiko Kecelakaan Kerja Pada Proyek Konstruksi Jembatan Musi Vi PalembangDocument6 pagesAnalisa Risiko Kecelakaan Kerja Pada Proyek Konstruksi Jembatan Musi Vi PalembangRoraNo ratings yet
- Psychological Report: I. Personal Data / Identification DataDocument3 pagesPsychological Report: I. Personal Data / Identification DataRoger Jhon BravoNo ratings yet
- Week 5 The Global North and SouthDocument12 pagesWeek 5 The Global North and SouthAdrienne Joielle MartinezNo ratings yet
- HA Filler Injection and Skin Quality-Literature MiDocument9 pagesHA Filler Injection and Skin Quality-Literature MiEnt IMDCNo ratings yet
- OASIS Item Guidance Patient History & Diagnoses Oasis ItemDocument20 pagesOASIS Item Guidance Patient History & Diagnoses Oasis ItembiskwetNo ratings yet
- Lesson 4 Pe 1Document11 pagesLesson 4 Pe 1Maya RosarioNo ratings yet
- 1.preface The International Pharmacopoeia, Eleventh EditionDocument3 pages1.preface The International Pharmacopoeia, Eleventh EditionLIZ NORMA ARROYO TORRESNo ratings yet
- Detailed Lesson Plan in Physical Education Grade 4Document6 pagesDetailed Lesson Plan in Physical Education Grade 4Myca HernandezNo ratings yet
- Admit Card: Instructions To The CandidateDocument1 pageAdmit Card: Instructions To The CandidateGaurav YadavNo ratings yet
- CAPE Communication Studies 2009 P3BDocument4 pagesCAPE Communication Studies 2009 P3BRiaz JokanNo ratings yet
- Physical Exercise and Executive Functions in Preadolescent Children, Adolescents and Young Adults - A Meta-AnalysisDocument9 pagesPhysical Exercise and Executive Functions in Preadolescent Children, Adolescents and Young Adults - A Meta-AnalysisPedro J. Conesa CerveraNo ratings yet
- Epidemiology AssignmentDocument12 pagesEpidemiology AssignmentSagar ParajuliNo ratings yet
- Moh. Fahmi Suratinoyo - 0301777 - OsteomielitisDocument43 pagesMoh. Fahmi Suratinoyo - 0301777 - OsteomielitisFahmiNo ratings yet
- Cardio DrugsDocument58 pagesCardio DrugsMARIA ROWENA VIA J. LUCENANo ratings yet
- Muhammad Awais: ContactDocument1 pageMuhammad Awais: ContactMian AwaisNo ratings yet
- Lipo Contrast Cryo BrochureDocument5 pagesLipo Contrast Cryo BrochureSerenity ZhangNo ratings yet
- Routes of Admin (Cology1)Document35 pagesRoutes of Admin (Cology1)ROSENo ratings yet
- Biotechnology 8 Q4-Week1 LASDocument4 pagesBiotechnology 8 Q4-Week1 LASSean Maximus M. PanganibanNo ratings yet
- Improving Healthcare Warehouse Operations Through 5SDocument14 pagesImproving Healthcare Warehouse Operations Through 5SIbrahim SkakriNo ratings yet
- Midterm Quiz#1Document6 pagesMidterm Quiz#1AIRINI MAY L. GUEVARRANo ratings yet
- 1 s2.0 S2212443823000371 MainDocument11 pages1 s2.0 S2212443823000371 MainMirza GlusacNo ratings yet
- The Effects of Infant Massage On Maternal PostpartumDocument6 pagesThe Effects of Infant Massage On Maternal PostpartumopanocayNo ratings yet
- Lyceum of The Philippines UniversityDocument2 pagesLyceum of The Philippines UniversityVon Matthew BarcialNo ratings yet
- Hse Training MatrixDocument3 pagesHse Training Matrixjoenediath9345No ratings yet
- Hari KE Hari/Tgl Imam Kultum Badal BilalDocument4 pagesHari KE Hari/Tgl Imam Kultum Badal Bilalsyubban afifNo ratings yet
- HMB342 Course Syllabus Summer 2020Document5 pagesHMB342 Course Syllabus Summer 2020WangNo ratings yet