Professional Documents
Culture Documents
Jamacardiology Lopes 2021 BR 210002 1635348730.39399
Jamacardiology Lopes 2021 BR 210002 1635348730.39399
Uploaded by
Daniella AlarcónOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jamacardiology Lopes 2021 BR 210002 1635348730.39399
Jamacardiology Lopes 2021 BR 210002 1635348730.39399
Uploaded by
Daniella AlarcónCopyright:
Available Formats
Research
JAMA Cardiology | Brief Report
Effect of Exercise Training on Ambulatory Blood Pressure
Among Patients With Resistant Hypertension
A Randomized Clinical Trial
Susana Lopes, MSc; José Mesquita-Bastos, MD, PhD; Catarina Garcia, MSc; Susana Bertoquini, PhD;
Verónica Ribau, MSc; Manuel Teixeira, MSc; Ilda P. Ribeiro, PhD; Joana B. Melo, PhD; José Oliveira, PhD;
Daniela Figueiredo, PhD; Guilherme V. Guimarães, PhD; Linda S. Pescatello, PhD; Jorge Polonia, MD, PhD;
Alberto J. Alves, PhD; Fernando Ribeiro, PhD
Supplemental content
IMPORTANCE Limited evidence suggests exercise reduces blood pressure (BP) in individuals
with resistant hypertension, a clinical population with low responsiveness to drug therapy.
OBJECTIVE To determine whether an aerobic exercise training intervention reduces
ambulatory BP among patients with resistant hypertension.
DESIGN, SETTINGS, AND PARTICIPANTS The Exercise Training in the Treatment of Resistant
Hypertension (EnRicH) trial is a prospective, 2-center, single-blinded randomized clinical trial
performed at 2 hospital centers in Portugal from March 2017 to December 2019. A total of 60
patients with a diagnosis of resistant hypertension aged 40 to 75 years were prospectively
enrolled and observed at the hospitals’ hypertension outpatient clinic.
INTERVENTIONS Patients were randomly assigned in a 1:1 ratio to a 12-week moderate-
intensity aerobic exercise training program (exercise group) or a usual care control group. The
exercise group performed three 40-minute supervised sessions per week in addition to usual
care.
MAIN OUTCOMES AND MEASURES The powered primary efficacy measure was 24-hour
ambulatory systolic BP change from baseline. Secondary outcomes included daytime and
nighttime ambulatory BP, office BP, and cardiorespiratory fitness.
RESULTS A total of 53 patients completed the study, including 26 in the exercise group and 27
in the control group. Of these, 24 (45%) were women, and the mean (SD) age was 60.1 (8.7)
years. Compared with the control group, among those in the exercise group, 24-hour
ambulatory systolic BP was reduced by 7.1 mm Hg (95% CI, −12.8 to −1.4; P = .02).
Additionally, 24-hour ambulatory diastolic BP (−5.1 mm Hg; 95% CI, −7.9 to −2.3; P = .001),
daytime systolic BP (−8.4 mm Hg; 95% CI, −14.3 to −2.5; P = .006), and daytime diastolic BP
(−5.7 mm Hg; 95% CI, −9.0 to −2.4; P = .001) were reduced in the exercise group compared
with the control group. Office systolic BP (−10.0 mm Hg; 95% CI, −17.6 to −2.5; P = .01) and
cardiorespiratory fitness (5.05 mL/kg per minute of oxygen consumption; 95% CI, 3.5 to 6.6;
P < .001) also improved in the exercise group compared with the control group.
CONCLUSIONS AND RELEVANCE A 12-week aerobic exercise program reduced 24-hour and
daytime ambulatory BP as well as office systolic BP in patients with resistant hypertension.
These findings provide clinicians with evidence to embrace moderate-intensity aerobic
exercise as a standard coadjutant therapy targeting this patient population.
TRIAL REGISTRATION ClinicalTrials.gov Identifier: NCT03090529
Author Affiliations: Author
affiliations are listed at the end of this
article.
Corresponding Author: Fernando
Ribeiro, PhD, Institute of Biomedicine
(iBiMED), School of Health Sciences,
University of Aveiro, Bldg 30, Agras
do Crasto, Campus Universitário de
JAMA Cardiol. 2021;6(11):1317-1323. doi:10.1001/jamacardio.2021.2735 Santiago, 3810-193 Aveiro, Portugal
Published online August 4, 2021. (fernando.ribeiro@ua.pt).
(Reprinted) 1317
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 08/09/2023
Research Brief Report Effect of Exercise Training on Ambulatory Blood Pressure Among Patients With Resistant Hypertension
R
esistant hypertension persists as a clinical challenge,
as it is a puzzling problem without a clear solution.1 Key Points
The available treatment options to lower blood pres-
Question Is aerobic exercise training an effective
sure (BP) in these patients, namely antihypertensive medica- antihypertensive treatment in patients with resistant
tions and kidney denervation, have had limited success,2-4 hypertension?
while permanent implant-based therapies await appropriate
Findings In this randomized clinical trial including 53 patients, a
assessment.5 Despite the renewed clinical interest in kidney
12-week exercise training intervention promoted a clinically
denervation,6-8 the invasive nature and health care costs meaningful reduction in 24-hour and daytime ambulatory systolic
of this procedure along with the increasing prevalence of and diastolic blood pressure.
hypertension clearly demonstrate the need for other effec-
Meaning The findings show that aerobic exercise added to
tive treatment options, namely lifestyle strategies for the man-
optimized medical therapy reduces blood pressure in patients with
agement of treatment-resistant hypertension. low responsiveness to drug treatment and has the potential to be
Although exercise is recommended globally as a first-line incorporated in the standard care of these patients.
approach for the treatment of hypertension,9,10 specific rec-
ommendations for those with treatment-resistant hyperten-
sion are lacking. Two trials11,12 provide preliminary evidence Figure 1. Flow Diagram Depicting the Study Design
of the beneficial BP effects of exercise in individuals with treat-
ment-resistant hypertension. However, uncertainty persists 365 Assessed for eligibility
regarding the efficacy of exercise training for those with
resistant hypertension because of limitations of these 305 Excluded
271 Not meeting inclusion criteria
studies; they did not disclose the timing of the ambulatory BP
73 Secondary hypertension
assessments and important information regarding the 33 Evidence of target organ
damage
exercise training program, so the exercise dose cannot be
27 Heart failure
replicated.11 Furthermore, the exercise programs were very 19 Acute cardiovascular
event (≤1 y)
distinct in terms of exercise modality (treadmill exercise11
7 Peripheral artery disease
vs heated water–based exercise12) and intensity-monitoring strat- 27 Kidney failure
egies (target lactate concentrations11 vs perceived exertion12). The 16 Chronic obstructive
pulmonary disease
need for specialized personnel and infrastructures to conduct 37 Limitations to physical
activity
laboratory exercise assessments and deliver heated water–
3 Regular exercise training
based exercise is challenging and further complicates replica- 29 Change of antihypertensive
medication ≤3 mo
tion in a clinical setting. The Exercise Training in the Treatment
22 Declined to participate
of Resistant Hypertension (EnRicH) randomized clinical trial 12 Other reasons
was designed to overcome these methodological shortcom-
ings by testing with a rigorous design if exercise training com- 60 Randomized
pared with usual care indeed reduces ambulatory BP among
patients with resistant hypertension.
30 Allocated to 12 wk of aerobic 30 Allocated to 12 wk of
exercise training usual care
4 Lost to follow-up 3 Lost to follow-up
Methods 2 Family issues (severe health 1 Started a new medication
problems in close relatives) (not associated with
Study Design and Settings 2 Lack time to attend exercise hypertension) and asked to
The EnRicH trial is a prospective, 2-center, single-blinded ran- sessions be removed from the study
2 Refused to participate in
domized clinical trial with a parallel 2-arm group performed in follow-up assessment
Portugal from March 2017 to December 2019. Patients were ran-
domly assigned to a 12-week aerobic exercise training program 26 Analyzed 27 Analyzed
plus usual care (exercise group) or to usual care (control group).
The primary and secondary outcomes were assessed at base-
line and after the 12-week intervention, which was conducted tals’ hypertension outpatient clinics.1 On initial screening,
48 hours after the last exercise session. All patients provided writ- automated 24-hour ambulatory BP monitoring was per-
ten informed consent. The study was approved by the Ethics formed, adherence to medications was documented by the
Committee of the Centro Hospitalar do Baixo Vouga and regis- 8-item Morisky Medication Adherence Scale, and the diag-
tered on ClinicalTrials.gov. The trial protocol can be found in nosis of resistant hypertension was confirmed. Patients
Supplement 1. This study followed the Consolidated Standards were required to have a mean systolic BP of 130 mm Hg or
of Reporting Trials (CONSORT) reporting guideline. greater on 24-hour ambulatory BP monitoring and/or 135
mm Hg or greater during daytime hours while taking maxi-
Participants mally tolerated doses of at least 3 antihypertensive agents,
We prospectively enrolled patients with a diagnosis of resis- including a diuretic, or to have a controlled BP while taking
tant hypertension aged 40 to 75 years observed at the hospi- 4 or more antihypertensive agents.1 Exclusion criteria are
1318 JAMA Cardiology November 2021 Volume 6, Number 11 (Reprinted) jamacardiology.com
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 08/09/2023
Effect of Exercise Training on Ambulatory Blood Pressure Among Patients With Resistant Hypertension Brief Report Research
Table. Baseline Demographic and Clinical Characteristics
Mean (SD)
Characteristic Exercise group (n = 26) Control group (n = 27) P value
Age, y 59.3 (8.2) 60.8 (9.2) .53
Male, No. (%) 14 (54) 15 (56) .90
Weight, kg 81.5 (14.7) 83.0 (15.6) .70
Body mass indexa 29.8 (4.9) 30.4 (5.0) .64
Fat mass, % 34.3 (8.0) 35.0 (9.6) .80
Medical history, No. (%)
Currently smoking 5 (19) 3 (11) .41
Diabetes 3 (12) 6 (22) .30
Hyperlipidemia 20 (77) 21 (78) .94
Family history of hypertension 17 (65) 15 (56) .47
Obesity 11 (42) 14 (52) .49
Overweight 12 (46) 10 (37) .50
Stroke 3 (12) 1 (4) .28
Transient ischemic attack 1 (4) 2 (7) .58
Myocardial infarction 3 (12) 4 (15) .73
Medication, No. (%)
Antihypertensive drugs, mean (SD), No. 4.6 (0.9) 4.7 (0.6) .66
Controlled BP on ≥4 drugs 14 (54) 14 (52) .88
Diuretics 26 (100) 27 (100) NA
ACE inhibitors/angiotensin receptor antagonists 26 (100) 26 (96) .32
Calcium channel blockers 26 (100) 26 (96) .32
β-Blockers 16 (62) 16 (59) .87
Centrally acting sympatholytic agent 8 (31) 13 (48) .20
Direct-acting vasodilators 26 (100) 27 (100) NA
Aldosterone antagonist 10 (39) 11 (41) .87
Antiplatelet drug 4 (15) 7 (26) .34
Hypoglycemic drug 3 (12) 6 (22) .30
Lipid-lowering drugs 20 (77) 21 (78) .94
Lipid, metabolic, and urinary parameters
Fasting glucose, mg/dL 114.0 (41.7) 105.5 (17.5) .34
Total cholesterol, mg/dL 174.8 (36.5) 183.7 (52.2) .49
HDL cholesterol, mg/dL 48.9 (12.9) 49.8 (15.3) .84
LDL cholesterol, mg/dL 102.4 (30.1) 108.9 (39.9) .53
Triglycerides, mg/dL 117.4 (49.4) 126.2 (79.9) .64
Hemoglobin A1c, % 5.8 (1.1) 5.8 (0.5) .88
Urinary sodium excretion, mmol/24 h 168.2 (69.5) 166.2 (48.7) .91
Urinary potassium excretion, mmol/24 h 80.4 (25.8) 71.8 (24.6) .24
Microalbuminuria, median (IQR), mg/24 h 14.6 (6.9-19.2) 14.5 (10.5-115.2) .53
BP, mm Hg
24-h
Systolic BP 127.4 (12.2) 126.1 (17.2) .75
Diastolic BP 75.6 (7.8) 73.3 (10.2) .37
Mean BP 92.9 (8.0) 90.8 (11.6) .46
Daytime
Systolic BP 133.0 (12.3) 131.9 (18.0) .81
Diastolic BP 79.4 (8.1) 77.3 (10.5) .42
Mean BP 97.2 (8.0) 95.4 (12.0) .52
Nighttime
Systolic BP 115.0 (15.0) 115.4 (16.5) .93
Diastolic BP 67.3 (9.4) 66.2 (9.6) .69
(continued)
jamacardiology.com (Reprinted) JAMA Cardiology November 2021 Volume 6, Number 11 1319
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 08/09/2023
Research Brief Report Effect of Exercise Training on Ambulatory Blood Pressure Among Patients With Resistant Hypertension
Table. Baseline Demographic and Clinical Characteristics (continued)
Mean (SD)
Characteristic Exercise group (n = 26) Control group (n = 27) P value
Mean BP 83.1 (10.3) 82.7 (11.1) .89
Office
Systolic BP 140.7 (16.6) 141.1 (15.3) .94
Diastolic BP 84.3 (8.8) 84.4 (10.0) .96
Mean BP 103.0 (10.1) 103.2 (10.9) .95
Cardiorespiratory fitness, mL/kg per min of oxygen consumption 34.8 (5.6) 32.4 (6.8) .20
Abbreviations: ACE, angiotensin-converting enzyme; BP, blood pressure; 0.0555; cholesterol to millimoles per liter, multiply by 0.0259; and triglycerides
HDL, high-density lipoprotein; IQR, interquartile range; LDL, low-density to millimoles per liter, multiply by 0.0113.
lipoprotein; NA, not applicable. a
Calculated as weight in kilograms divided by height in meters squared.
SI conversion factors: To convert glucose to millimoles per liter, multiply by
provided in the eMethods in Supplement 2. Medication sis and Shapiro-Wilk tests were performed to determine the
adherence and the antihypertensive medication regimen normality of the data distribution. Continuous variables are ex-
remained unchanged throughout the study. pressed as means with SDs or medians with interquartile
ranges; mean differences are expressed with their 2-sided 95%
Randomization and Allocation CIs. Between-group differences at baseline and in the change
Computer-based stratified randomization was generated (1: from baseline to the end of the study were tested with un-
1), with the strata defined by age (age 40 to 55 years, 56 to 65 paired t tests. Analysis of covariance was also used to adjust
years, and 66 to 75 years) and sex. Allocation was concealed for baseline BP measurements. Paired t tests were performed
in opaque envelopes until the beginning of the exercise or for within-group comparisons from baseline to the end of the
control intervention. study. For categorical variables, counts and percentages are
presented. Between-group comparisons at baseline in cat-
Outcomes egorical variables were tested with the χ2 test. The level of sig-
The primary efficacy end point was change in 24-hour nificance was set as a 2-sided P value less than .05. All analy-
ambulatory systolic BP from baseline to 3 months. Second- ses were conducted with SPSS version 24.0 (SPSS Inc). The
ary outcomes included mean changes in all other BP vari- eMethods in Supplement 2 includes further statistical analy-
ables, heart rate, body composition, cardiorespiratory fitness sis details, including the sample size calculation.
(maximum oxygen uptake; VO2 max), and adverse events
(eg, hypertensive crisis, being hospitalized, or death by any
cause), including adverse effects during or after the exercise
sessions (eg, severe hypotension). A detailed description of
Results
the assessment procedures is provided in the eMethods in Participants
Supplement 2. From the 94 patients who met the enrollment criteria, 60
patients agreed to participate. Seven terminated the study pre-
Study Treatment maturely; thus, 53 patients completed the follow-up assess-
Patients in the exercise group underwent a 12-week aerobic ments and were included in the analysis (Figure 1). Of these,
exercise training program composed of 3 supervised training 24 (45%) were women, and the mean (SD) age was 60.1 (8.7)
sessions per week. Each session included a 10-minute warm- years. Patients’ characteristics are shown in the Table.
up, 40 minutes of aerobic exercise consisting of cycling and/or
walking at 50% to 70% of VO2 max (11 to 14 on the Borg scale), BP Effects of Exercise Training
and a 10-minute cooldown. Patients started with 20 minutes The change in 24-hour ambulatory systolic BP was signifi-
of exercise at 50% of VO2 max, and progression occurred cantly different between groups by −7.1 mm Hg (95% CI, −12.8
weekly, alternating between a 5-minute increase in session to −1.4; P = .02), with a mean (SD) change of −6.2 (12.2) mm Hg
duration and a 5% of VO2 max increase in intensity, until in the exercise arm vs 0.9 (8.1) mm Hg in the control arm
achieving 40 minutes at 70% of VO2 max, if tolerated. The (Figure 2; eTable 1 in Supplement 2). Similarly, 24-hour ambu-
control group received usual care, including advice on appro- latory diastolic BP was significantly reduced in the exercise arm
priate lifestyle behavior and optimal or best-tolerated drug compared with the control arm (−5.1 mm Hg; 95% CI, −7.9 to
treatment provided by their physicians. −2.3; P = .001) (Figure 2; eTable 1 in Supplement 2).
Daytime ambulatory systolic BP (−8.4 mm Hg; 95% CI,
Statistical Analysis −14.3 to −2.5; P = .006) and diastolic BP (−5.7 mm Hg; 95% CI,
The EnRicH trial was powered for the primary outcome mea- −9.0 to −2.4; P = .001) as well as office systolic BP (−10.0 mm
sure of 24-hour ambulatory systolic BP. Exploratory data analy- Hg; 95% CI, −17.6 to −2.5; P = .01) were also significantly re-
1320 JAMA Cardiology November 2021 Volume 6, Number 11 (Reprinted) jamacardiology.com
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 08/09/2023
Effect of Exercise Training on Ambulatory Blood Pressure Among Patients With Resistant Hypertension Brief Report Research
Figure 2. Changes in Ambulatory and Office Blood Pressure (BP)
Baseline 12-wk
A 24-h Change in ambulatory systolic BP B 24-h Change in ambulatory diastolic BP
Difference, –7.1 mm Hg; 95% CI, –12.8 to –1.4; P = .02 Difference, –5.1 mm Hg; 95% CI, –7.9 to –2.3; P = .001
Change from baseline, Change from baseline, Change from baseline, Change from baseline,
180 –6.2 ± 12.2 mm Hg 0.9 ± 8.1 mm Hg 120 –4.4 ± 6.1 mm Hg 0.7 ± 3.9 mm Hg
24-h Ambulatory diastolic BP, mm Hg
P =.02 P =.57
24-h Ambulatory systolic BP, mm Hg
P =.001 P =.39
160
100
140
120 80
100
60
80
60 40
40
20
20
0 0
Exercise group Control group Exercise group Control group
C Change in daytime ambulatory systolic BP D Change in daytime ambulatory diastolic BP
Difference, –8.4 mm Hg; 95% CI, –14.3 to –2.5; P = .006 Difference, –5.7 mm Hg; 95% CI, –9.0 to –2.4; P = .001
Change from baseline, Change from baseline, Change from baseline, Change from baseline,
180 –7.3 ± 12.7 mm Hg 1.1 ± 8.2 mm Hg 120 –5.0 ± 6.9 mm Hg 0.7 ± 4.8 mm Hg
Daytime ambulatory diastolic BP, mm Hg
Daytime ambulatory systolic BP, mm Hg
P =.007 P =.51 P =.001 P =.44
160
100
140
120 80
100
60
80
60 40
40
20
20
0 0
Exercise group Control group Exercise group Control group
E Change in office systolic BP F Change in office diastolic BP
Difference, –10.0 mm Hg; 95% CI, –17.6 to –2.5; P = .01 Difference, –4.5 mm Hg; 95% CI, –10.1 to –1.2; P = .12
Change from baseline to the end of
Change from baseline, Change from baseline, Change from baseline, Change from baseline, treatment in 24-hour and daytime
–10.9 ± 15.2 mm Hg –0.9 ± 12.0 mm Hg –5.9 ± 11.1 mm Hg –1.4 ± 9.3 mm Hg ambulatory BP as well as office
180 P =.001 P =.70 120 P =.01 P =.45
systolic and diastolic BP in the
160 exercise and control groups.
100
Office diastolic BP, mm Hg
140 Significant changes from baseline to
Office systolic BP, mm Hg
the end of the intervention in
120 80
24-hour, daytime, and office systolic
100 and diastolic BP were observed in the
60
80 exercise group compared with the
60 40
control group. There was a significant
between-group difference in favor of
40 the exercise group for 24-hour and
20
20 daytime ambulatory systolic and
0 0 diastolic BP and for office systolic BP.
Exercise group Control group Exercise group Control group Error bars indicate standard
deviations.
duced in the exercise arm compared with the control arm Cardiorespiratory Fitness and Other
(Figure 2; eTable 1 in Supplement 2). Mean BP changes are Clinical Effects of Exercise Training
provided in eFigure 1 in Supplement 2. There were no differ- Individuals in the exercise arm improved cardiorespiratory fit-
ences in nighttime ambulatory BP and office diastolic BP ness by 14% (mean [SD] change of 4.7 [3.1] mL/kg per minute
between groups (eFigure 2 and eTable 1 in Supplement 2). of oxygen consumption; P < .001), while it remained un-
Individual BP changes from baseline to the end of the exer- changed in those in the control arm (eTable 2 in Supple-
cise and control interventions are provided in eFigure 3 in ment 2), resulting in a between-group difference of 5.05 mL/kg
Supplement 2. per minute of oxygen consumption (95% CI, 3.5 to 6.6;
jamacardiology.com (Reprinted) JAMA Cardiology November 2021 Volume 6, Number 11 1321
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 08/09/2023
Research Brief Report Effect of Exercise Training on Ambulatory Blood Pressure Among Patients With Resistant Hypertension
P < .001). There was also a significant between-group differ- nervation clinical trials. For instance, the SPYRAL HTN-ON
ence in the change in heart rate (24-hour and daytime) in fa- MED trial7 reported a decrease of 7.4 mm Hg for systolic BP and
vor of the exercise arm (eTable 2 in Supplement 2). There were 4.2 mm Hg for diastolic BP at 6 months after kidney denerva-
no between-group differences in body composition (eTable 2 tion compared with sham control.
in Supplement 2) or biochemical or urinary parameters From a public health perspective, the results of the En-
(eTable 3 in Supplement 2). RicH trial are quite promising. There is mounting evidence the
reduction of systolic BP is linearly associated with a lower risk
Safety and Compliance of cardiovascular morbidity and mortality in adults with
Patients in the exercise arm attended a mean (SD) of 98.8% hypertension.13 For instance, a reduction in systolic BP of 10
(3.2%) of the 36 total exercise sessions (median adherence rate, mm Hg or diastolic BP of 4 mm Hg is associated with approxi-
100%; minimum, 89%). There were no major adverse events mately 30% lower risk of stroke and approximately 20% lower
or complications registered during the study. Two patients risk of myocardial infarction.14 Altogether, the results of the
reported dizziness after 2 of the exercise sessions, and 2 EnRicH trial reaffirm the safety and efficacy of exercise train-
patients reported musculoskeletal complaints (knee and hip ing reported in previous trials among those with hypertension15
soreness) in the first weeks of the exercise intervention. and improve our understanding in the context of treatment-
resistant hypertension.
Limitations
Discussion Limitations of the EnRicH trial should be acknowledged. On
The EnRicH trial showed 12 weeks of moderate-intensity aero- average, our sample consisted of patients with baseline bio-
bic exercise training decreased the powered primary efficacy chemical parameters near or at the recommended levels,
end point of 24-hour systolic BP in patients with resistant hy- which limits the generalizability of our findings to patients
pertension by 7.1 mm Hg compared with usual care. Daytime with a more adverse cardiometabolic profile. Also, the
BP (systolic, −8.4 mm Hg; diastolic, −5.7 mm Hg), 24-hour dia- EnRicH trial was not powered to detect potential effects in
stolic BP (−5.1 mm Hg), and office systolic BP (−10.0 mm Hg) subgroups of interest (eg, men compared with women). Addi-
were also significantly reduced after exercise training com- tionally, results of the EnRicH trial are specific to aerobic
pared with usual care. The magnitude of these differences in exercise and may not be generalizable to other types of exer-
BP are clinically meaningful and associated with lower risk cise (eg, resistance exercise).
of cardiovascular morbidity and mortality in adults with
hypertension.13
From a clinical perspective, these results are encourag-
ing because the exercise prescription tested in the EnRicH trial
Conclusions
is easily reproducible and has the potential to be applied on a In conclusion, the EnRicH trial showed a significant reduc-
larger scale in a setting more representative of clinical prac- tion in systolic and diastolic BP in patients with resistant hy-
tice for which integrating drug treatment and exercise train- pertension after a 12-week moderate-intensity aerobic exer-
ing are recommended. Our results confirm that aerobic exer- cise program, both under ambulatory conditions and in the
cise training, which is already recommended as first-line office. In this study, when added to optimized medical therapy,
treatment for hypertension, should be extended to those with aerobic exercise reduced BP to clinically meaningful levels in
resistance to pharmacological treatment. The exercise inter- a patient population with a low responsiveness to drug treat-
vention resulted in a reduction in 24-hour ambulatory BP com- ment and has the potential to be incorporated into the stan-
parable with the reduction observed in successful kidney de- dard care of these patients.
ARTICLE INFORMATION Matosinhos, Portugal (Bertoquini, Polonia); Investigação de Cuidados de Suporte em Oncologia
Accepted for Publication: June 4, 2021. University of Coimbra, Cytogenetics and Genomics (AICSO), Vila Nova de Gaia, Portugal (Alves).
Laboratory, Institute of Cellular and Molecular Author Contributions: Ms Lopes and Dr Fernando
Published Online: August 4, 2021. Biology, Coimbra, Portugal (I. P. Ribeiro, Melo);
doi:10.1001/jamacardio.2021.2735 Ribeiro had full access to all of the data in the study
Coimbra Institute for Clinical and Biomedical and take responsibility for the integrity of the data
Author Affiliations: Institute of Biomedicine Research (iCBR) and Center of Investigation on and the accuracy of the data analysis.
(iBiMED), School of Health Sciences, University of Environment Genetics and Oncobiology (CIMAGO), Study concept and design: Lopes, Mesquita-Bastos,
Aveiro, Aveiro, Portugal (Lopes, Mesquita-Bastos, Faculty of Medicine and Clinical Academic Center of Oliveira, Figueiredo, Guimarães, Polonia, Alves, F.
Teixeira, F. Ribeiro); Cardiology Department, Coimbra (CACC), Coimbra, Portugal (I. P. Ribeiro, Ribeiro.
Hospital Infante D. Pedro, Centro Hospitalar do Melo); Research Centre in Physical Activity, Health Acquisition, analysis, or interpretation of data:
Baixo Vouga, Aveiro, Portugal (Mesquita-Bastos, and Leisure (CIAFEL), Faculty of Sport, University of All authors.
Ribau); Research Center in Sports Sciences, Health Porto, Porto, Portugal (Oliveira); Center for Health Drafting of the manuscript: Lopes, Mesquita-Bastos,
and Human Development (CIDESD), University Technology and Services Research (CINTESIS.UA), Garcia, Oliveira, Alves, F. Ribeiro.
Institute of Maia, Maia, Portugal (Garcia, Alves); School of Health Sciences, University of Aveiro, Critical revision of the manuscript for important
Centre for Health Technology and Services Aveiro, Portugal (Figueiredo); Heart Institute, intellectual content: Lopes, Mesquita-Bastos, Berto-
Research (CINTESIS), Faculty of Medicine, School of Medicine, University of São Paulo, quini, Ribau, Teixeira, I. Ribeiro, Melo, Oliveira,
University of Porto, Porto, Portugal (Bertoquini, São Paulo, Brazil (Guimarães); Department of Figueiredo, Guimarães, Pescatello, Polonia, Alves, F.
Polonia); Hypertension and Cardiovascular Risk Kinesiology, University of Connecticut, Storrs Ribeiro.
Unit, Unidade Local de Saúde Matosinhos, (Pescatello); OncoMove, Associação de
1322 JAMA Cardiology November 2021 Volume 6, Number 11 (Reprinted) jamacardiology.com
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 08/09/2023
Effect of Exercise Training on Ambulatory Blood Pressure Among Patients With Resistant Hypertension Brief Report Research
Statistical analysis: Lopes, Oliveira, Pescatello, Nursing; Council on Clinical Cardiology; Council on standardised antihypertensive treatment with or
Alves, F. Ribeiro. Genomic and Precision Medicine; Council on without renal denervation for resistant
Obtained funding: Lopes, Oliveira, Figueiredo, Peripheral Vascular Disease; Council on Quality of hypertension (DENERHTN): a multicentre,
Alves, F. Ribeiro. Care and Outcomes Research; and Stroke Council. open-label, randomised controlled trial. Lancet.
Administrative, technical, or material support: Resistant hypertension: detection, evaluation, and 2015;385(9981):1957-1965. doi:10.1016/
Lopes, Mesquita-Bastos, Garcia, Bertoquini, Ribau, management: a scientific statement from the S0140-6736(14)61942-5
Teixeira, I. Ribeiro, Melo, Oliveira, Guimarães. American Heart Association. Hypertension. 2018;72 9. Williams B, Mancia G, Spiering W, et al; ESC
Study supervision: Mesquita-Bastos, Oliveira, (5):e53-e90. doi:10.1161/HYP.0000000000000084 Scientific Document Group. 2018 ESC/ESH
Figueiredo, Alves, F. Ribeiro. 2. Bakris GL, Townsend RR, Liu M, et al; guidelines for the management of arterial
Conflict of Interest Disclosures: None reported. SYMPLICITY HTN-3 Investigators. Impact of renal hypertension. Eur Heart J. 2018;39(33):3021-3104.
Funding/Support: This work was funded by the denervation on 24-hour ambulatory blood doi:10.1093/eurheartj/ehy339
European Union through the European Regional pressure: results from SYMPLICITY HTN-3. J Am Coll 10. Whelton PK, Carey RM, Aronow WS, et al. 2017
Development Fund Operational Competitiveness Cardiol. 2014;64(11):1071-1078. doi:10.1016/ ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/
Factors Program (COMPETE) and by the j.jacc.2014.05.012 NMA/PCNA guideline for the prevention, detection,
Portuguese government through the Foundation 3. Agasthi P, Shipman J, Arsanjani R, et al. Renal evaluation, and management of high blood
for Science and Technology (grants P2020-PTDC/ denervation for resistant hypertension in the pressure in adults: a report of the American College
DTP-DES/1725/2014 and contemporary era: a systematic review and of Cardiology/American Heart Association Task
POCI-01-0145-FEDER-016710). Ms Lopes was meta-analysis. Sci Rep. 2019;9(1):6200. doi:10. Force on Clinical Practice Guidelines. Circulation.
awarded with a Portuguese Foundation for Science 1038/s41598-019-42695-9 2018;138(17):e484-e594.
and Technology PhD grant (grant 4. Bhatt DL, Kandzari DE, O’Neill WW, et al; 11. Dimeo F, Pagonas N, Seibert F, Arndt R, Zidek W,
SFRH/BD/129454/2017). The University of Aveiro SYMPLICITY HTN-3 Investigators. A controlled trial Westhoff TH. Aerobic exercise reduces blood
Institute of Biomedicine (iBiMED; reference No. of renal denervation for resistant hypertension. pressure in resistant hypertension. Hypertension.
UID/BIM/04501/2020), University of Porto N Engl J Med. 2014;370(15):1393-1401. doi:10.1056/ 2012;60(3):653-658. doi:10.1161/
Research Centre in Physical Activity, Health and NEJMoa1402670 HYPERTENSIONAHA.112.197780
Leisure (CIAFEL; reference No. UID/DTP/00617/
2020), University Institute of Maia Research Center 5. Gierthmuehlen M, Plachta DTT, Zentner J. 12. Guimaraes GV, de Barros Cruz LG,
in Sports Sciences, Health and Human Implant-mediated therapy of arterial hypertension. Fernandes-Silva MM, Dorea EL, Bocchi EA. Heated
Development (CIDESD; reference No. UID/DTP/ Curr Hypertens Rep. 2020;22(2):16. doi:10.1007/ water-based exercise training reduces 24-hour
04045/2020), and Center for Health Technology s11906-020-1019-7 ambulatory blood pressure levels in resistant
and Services Research (CINTESIS; reference No. 6. Böhm M, Kario K, Kandzari DE, et al; SPYRAL hypertensive patients: a randomized controlled trial
UID/IC/4255/2020) are research units supported HTN-OFF MED Pivotal Investigators. Efficacy of (HEx trial). Int J Cardiol. 2014;172(2):434-441.
by the Portuguese Foundation for Science and catheter-based renal denervation in the absence of doi:10.1016/j.ijcard.2014.01.100
Technology. antihypertensive medications (SPYRAL HTN-OFF 13. Bundy JD, Li C, Stuchlik P, et al. Systolic blood
Role of the Funder/Sponsor: The funders had no MED Pivotal): a multicentre, randomised, pressure reduction and risk of cardiovascular
role in the design and conduct of the study; sham-controlled trial. Lancet. 2020;395(10234): disease and mortality: a systematic review and
collection, management, analysis, and 1444-1451. doi:10.1016/S0140-6736(20)30554-7 network meta-analysis. JAMA Cardiol. 2017;2(7):
interpretation of the data; preparation, review, or 7. Kandzari DE, Böhm M, Mahfoud F, et al; SPYRAL 775-781. doi:10.1001/jamacardio.2017.1421
approval of the manuscript; and decision to submit HTN-ON MED Trial Investigators. Effect of renal 14. Staessen JA, Wang JG, Thijs L. Cardiovascular
the manuscript for publication. denervation on blood pressure in the presence of protection and blood pressure reduction:
Data Sharing Statement: See Supplement 3. antihypertensive drugs: 6-month efficacy and a meta-analysis. Lancet. 2001;358(9290):1305-1315.
safety results from the SPYRAL HTN-ON MED doi:10.1016/S0140-6736(01)06411-X
REFERENCES proof-of-concept randomised trial. Lancet. 2018; 15. Pescatello LS, Buchner DM, Jakicic JM, et al;
391(10137):2346-2355. doi:10.1016/ 2018 PHYSICAL ACTIVITY GUIDELINES ADVISORY
1. Carey RM, Calhoun DA, Bakris GL, et al; American S0140-6736(18)30951-6
Heart Association Professional/Public Education COMMITTEE. Physical activity to prevent and treat
and Publications Committee of the Council on 8. Azizi M, Sapoval M, Gosse P, et al; Renal hypertension: a systematic review. Med Sci Sports
Hypertension; Council on Cardiovascular and Stroke Denervation for Hypertension (DENERHTN) Exerc. 2019;51(6):1314-1323. doi:10.1249/
investigators. Optimum and stepped care MSS.0000000000001943
jamacardiology.com (Reprinted) JAMA Cardiology November 2021 Volume 6, Number 11 1323
© 2021 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ on 08/09/2023
You might also like
- Concept Paper Sex EducationDocument8 pagesConcept Paper Sex EducationYhazmin Iris Ilustrisimo100% (1)
- 10 1016@j JHT 2017 02 001 PDFDocument10 pages10 1016@j JHT 2017 02 001 PDFGusti Ayu KrisnayantiNo ratings yet
- Brazilian Journal of Physical TherapyDocument12 pagesBrazilian Journal of Physical TherapyKen ABNo ratings yet
- 1 s2.0 S1836955322001163 MainDocument2 pages1 s2.0 S1836955322001163 MainIhuoma AnaghaNo ratings yet
- Isometric Handgrip-1Document9 pagesIsometric Handgrip-1Adi PramonoNo ratings yet
- Aerobic Versus Isometric Handgrip Exercise in Hypertension: A Randomized Controlled TrialDocument8 pagesAerobic Versus Isometric Handgrip Exercise in Hypertension: A Randomized Controlled TrialROSANo ratings yet
- 2022 Strength Training For Arterial Hypertension Treatment A Systematic Review and Meta-Analysis of Randomize Clinical TrialsDocument15 pages2022 Strength Training For Arterial Hypertension Treatment A Systematic Review and Meta-Analysis of Randomize Clinical TrialsAntofa V EndeNo ratings yet
- 19417381221139343Document8 pages19417381221139343Thiago SartiNo ratings yet
- Inter HugoDocument10 pagesInter HugorizkaNo ratings yet
- Villelabeitia Jaureguizar 2016 Journal of Cardiopulmonary Rehabilitation and PreventionDocument10 pagesVillelabeitia Jaureguizar 2016 Journal of Cardiopulmonary Rehabilitation and PreventionPablo Damian LeivaNo ratings yet
- Decreased Blood Pressure Among Community Dwelling Older Adults Following Progressive Muscle Relaxation and Music Therapy (RESIK)Document6 pagesDecreased Blood Pressure Among Community Dwelling Older Adults Following Progressive Muscle Relaxation and Music Therapy (RESIK)Rara Mitha64No ratings yet
- Exercise Training For Blood Pressure: A Systematic Review and Meta-AnalysisDocument9 pagesExercise Training For Blood Pressure: A Systematic Review and Meta-AnalysisAnonymous 7dsX2F8nNo ratings yet
- IntervalexercisetrialAnnals2006 PDFDocument12 pagesIntervalexercisetrialAnnals2006 PDFrunmenNo ratings yet
- Sharman 2014Document12 pagesSharman 2014Jorge Valiente FernandezNo ratings yet
- Coronary Heart DiseaseDocument10 pagesCoronary Heart DiseaseMauludin BilaleyaNo ratings yet
- Intradialytic Exercise Is Medicine For.1Document7 pagesIntradialytic Exercise Is Medicine For.1Christian Tobar FredesNo ratings yet
- Abdominal and Auricular Acupuncture For Blood PressureDocument7 pagesAbdominal and Auricular Acupuncture For Blood PressureitensorNo ratings yet
- Evidence-Based Medical Treatment of Peripheral Arterial Disease: A Rapid ReviewDocument14 pagesEvidence-Based Medical Treatment of Peripheral Arterial Disease: A Rapid ReviewLeo OoNo ratings yet
- Interval Endurance and Resistance Training As Part of A Community-Based Secondary Prevention Program For Patients With Diabetes Mellitus and Coronary Artery DiseaseDocument7 pagesInterval Endurance and Resistance Training As Part of A Community-Based Secondary Prevention Program For Patients With Diabetes Mellitus and Coronary Artery DiseaseMarcos Túlio de SáNo ratings yet
- Diferent Exercise TrainingDocument9 pagesDiferent Exercise TrainingRenan Carraro RosaNo ratings yet
- Antihypertensives in HDDocument6 pagesAntihypertensives in HDamanyNo ratings yet
- Physical Therapy in Critically Ill Adult Patients PDFDocument17 pagesPhysical Therapy in Critically Ill Adult Patients PDFSoledad Cayupi TrafilafNo ratings yet
- 888 FullDocument5 pages888 FullZurya 12No ratings yet
- Risom 2020Document10 pagesRisom 2020drewantaNo ratings yet
- The Journal of Physiology - 2024 - Brito - Evening But Not Morning Aerobic Training Improves Sympathetic Activity andDocument15 pagesThe Journal of Physiology - 2024 - Brito - Evening But Not Morning Aerobic Training Improves Sympathetic Activity andAnnah MeeloNo ratings yet
- Jamacardiology Wang 2023 BR 230003 1681999274.03492 PDFDocument6 pagesJamacardiology Wang 2023 BR 230003 1681999274.03492 PDFFernando DominguezNo ratings yet
- Preprints202206 0017 v3 PDFDocument10 pagesPreprints202206 0017 v3 PDFSathish Candy BoyNo ratings yet
- Brazilian Journal of Physical TherapyDocument9 pagesBrazilian Journal of Physical TherapyWahdina PratamaNo ratings yet
- J Cjca 2012 07 744Document2 pagesJ Cjca 2012 07 744khadesakshi55No ratings yet
- 7 Effect of Specific Exercise Strategy On Need For Surgery in Patients With Subacromial Impingement Syndrome-Randomised Controlled StudyDocument3 pages7 Effect of Specific Exercise Strategy On Need For Surgery in Patients With Subacromial Impingement Syndrome-Randomised Controlled StudyJefferson James Dos SantosNo ratings yet
- Indian Heart Journal: Original ArticleDocument5 pagesIndian Heart Journal: Original ArticleRendi KurniawanNo ratings yet
- High Intensity Interval Training Versus Moderate Intensity Continuous Training Within Cardiac Rehabilitation A Systematic Review and Meta AnalysisDocument18 pagesHigh Intensity Interval Training Versus Moderate Intensity Continuous Training Within Cardiac Rehabilitation A Systematic Review and Meta AnalysisAnatomska CentralaNo ratings yet
- VHRM 7 085Document11 pagesVHRM 7 085AldiKurosakiNo ratings yet
- Home-Based Telehealth Exercise Training Program inDocument9 pagesHome-Based Telehealth Exercise Training Program inarwitarahayuNo ratings yet
- New England Journal Medicine: The ofDocument14 pagesNew England Journal Medicine: The ofIMNo ratings yet
- Educational Program Patients With HypertensionDocument9 pagesEducational Program Patients With HypertensionRoy martadi NurmansyahNo ratings yet
- AcupressureDocument9 pagesAcupressureFebi Tria KurniasariNo ratings yet
- Current InsightsDocument7 pagesCurrent InsightschandrusaiNo ratings yet
- A Study To Assess The Effectiveness of Abdominal Breathing Exercise in Reduction of Blood Pressure Among Hypertensive Patients in Selected Hospitals at BhopalDocument6 pagesA Study To Assess The Effectiveness of Abdominal Breathing Exercise in Reduction of Blood Pressure Among Hypertensive Patients in Selected Hospitals at BhopalEditor IJTSRDNo ratings yet
- Treatment Options For Patellar Tendinopathy: A Systematic ReviewDocument12 pagesTreatment Options For Patellar Tendinopathy: A Systematic ReviewEstefa Roldan RoldanNo ratings yet
- Physiotherapy 3 1 2Document4 pagesPhysiotherapy 3 1 2AjiNo ratings yet
- Am J Hypertens 2015 Sharman 147 58Document12 pagesAm J Hypertens 2015 Sharman 147 58yusnadiNo ratings yet
- The Polypill in Cardiovascular Prevention EvidenceDocument8 pagesThe Polypill in Cardiovascular Prevention EvidenceAn-Nisa Khoirun UmmiNo ratings yet
- Adsett Et Al. - 2015 - Aquatic Exercise Training and Stable Heart Failure A Systematic Review and Meta-AnalysisDocument7 pagesAdsett Et Al. - 2015 - Aquatic Exercise Training and Stable Heart Failure A Systematic Review and Meta-AnalysisErnesto Isaac Tlapanco RiosNo ratings yet
- Abstract BookDocument222 pagesAbstract BookArkesh PatnaikNo ratings yet
- Effects of Inspiratory Muscle Training Using An Electronic Device On Patients Undergoing Cardiac Surgery: A Randomized Controlled TrialDocument9 pagesEffects of Inspiratory Muscle Training Using An Electronic Device On Patients Undergoing Cardiac Surgery: A Randomized Controlled TrialDaniel Lago BorgesNo ratings yet
- International Journal of Trend in Scientific Research and Development (IJTSRD)Document5 pagesInternational Journal of Trend in Scientific Research and Development (IJTSRD)Editor IJTSRDNo ratings yet
- Evidence-Based Drug Therapy For Chronic Heart Failure: ZannadDocument7 pagesEvidence-Based Drug Therapy For Chronic Heart Failure: ZannadA5BNi Gusti Ketut Purnami Putri AdnyaniNo ratings yet
- 10 1016@j Arthro 2019 06 017Document17 pages10 1016@j Arthro 2019 06 017Ines Riera MoyaNo ratings yet
- gardner2019 - Changes in vascular and inflammatory biomarkers after exercise rehabilitation in patients with symptomatic peripheral artery diseaseDocument11 pagesgardner2019 - Changes in vascular and inflammatory biomarkers after exercise rehabilitation in patients with symptomatic peripheral artery diseasemutialailaniNo ratings yet
- Tendão, ExercícioDocument8 pagesTendão, ExercícioFabiano LacerdaNo ratings yet
- 1 s2.0 S1836955320300217 MainDocument3 pages1 s2.0 S1836955320300217 Mainjaxad78743No ratings yet
- Treatment Options For Patellar Tendinopathy A Systematic ReviewDocument12 pagesTreatment Options For Patellar Tendinopathy A Systematic ReviewRonny Araya AbarcaNo ratings yet
- Cardiovascular Disease and Exercise 2008Document5 pagesCardiovascular Disease and Exercise 2008OscarDavidGordilloGonzalezNo ratings yet
- Literature Review Cardiac RehabilitationDocument5 pagesLiterature Review Cardiac Rehabilitationafmzitaaoxahvp100% (1)
- Bukan RCT 1Document6 pagesBukan RCT 1Resky Ika Sah PutriNo ratings yet
- Hypertension Improvement Project: Clinical TrialDocument8 pagesHypertension Improvement Project: Clinical Trialneway workuNo ratings yet
- WH Elton 1998Document9 pagesWH Elton 1998cifa parinussaNo ratings yet
- Complementary Therapies in Clinical PracticeDocument6 pagesComplementary Therapies in Clinical PracticenurindahwarNo ratings yet
- Exercise and Other Non-Pharmaceutical Interventions 2018Document10 pagesExercise and Other Non-Pharmaceutical Interventions 2018storm.ghirlandoNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Sample Safety Health and Environmental ManualDocument13 pagesSample Safety Health and Environmental Manualtony s100% (1)
- Nliu Bhopal-University Reopening Guidelines-DraftDocument21 pagesNliu Bhopal-University Reopening Guidelines-DraftRashi BakshNo ratings yet
- FCP Hazard FallDocument6 pagesFCP Hazard FallChrissa Mae Aranilla MayoNo ratings yet
- Respiratory System Mechanics: Pulmonary Function TestsDocument3 pagesRespiratory System Mechanics: Pulmonary Function Testschaira nisaaNo ratings yet
- Case Study 1 PediaDocument7 pagesCase Study 1 PediaXeyanNo ratings yet
- Identification and Risk Reduction of Ebola Exposure: Guidance For Law Enforcement, First Responders and CorrectionsDocument8 pagesIdentification and Risk Reduction of Ebola Exposure: Guidance For Law Enforcement, First Responders and CorrectionsTy UsikNo ratings yet
- Hope Act1Document2 pagesHope Act1Mark Ian BellezaNo ratings yet
- mHIMSS Roadmap-Executive SummaryDocument1 pagemHIMSS Roadmap-Executive SummarySteveEpsteinNo ratings yet
- ANGARA DISEASE Inclusion Body Hepatitis Hydropericarditis Litchi Heart Syndrome in Broiler ChickenDocument42 pagesANGARA DISEASE Inclusion Body Hepatitis Hydropericarditis Litchi Heart Syndrome in Broiler Chickenkedar karki100% (2)
- McKenzie Explained PDFDocument4 pagesMcKenzie Explained PDFItai IzhakNo ratings yet
- 014 Milicevic JovanovicDocument13 pages014 Milicevic Jovanovicsintya dewiNo ratings yet
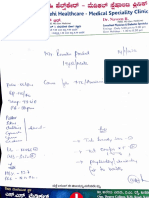
- L/Ylok: Janasnehi Healthcare Medical SpecialityDocument2 pagesL/Ylok: Janasnehi Healthcare Medical SpecialityRenukaprasad K RNo ratings yet
- Hse360 2023 - NewDocument19 pagesHse360 2023 - Newadrian.zurawieckiNo ratings yet
- Battisti Exercices PediatrieDocument197 pagesBattisti Exercices Pediatrieahkrab100% (1)
- Kuhas Syllabus 2021Document279 pagesKuhas Syllabus 2021Ansu MaliyakalNo ratings yet
- Chapter 9 Dengue Fever 1Document9 pagesChapter 9 Dengue Fever 1Kyla BalboaNo ratings yet
- Home Prescribing Course PP PDFDocument177 pagesHome Prescribing Course PP PDFAy Nine Dişi BilgeliğiNo ratings yet
- 9 Condor Assessment SignoffDocument8 pages9 Condor Assessment SignoffAbhishek SrivastavaNo ratings yet
- Review Article On Acharya TechDocument5 pagesReview Article On Acharya Techrahul yadavNo ratings yet
- Trauma Atls 2009Document2 pagesTrauma Atls 2009Jennifer IdrisNo ratings yet
- Update of FNSA 2022 Chapter Handbook eDocument89 pagesUpdate of FNSA 2022 Chapter Handbook eFNSANo ratings yet
- Sterilization and Disinfection For Bds 2nd YearDocument33 pagesSterilization and Disinfection For Bds 2nd YearLaiba IkramNo ratings yet
- Almaghrabi Resp ExaminationDocument33 pagesAlmaghrabi Resp ExaminationSagit Nauman81No ratings yet
- 1 en Act Part1 v8 0Document24 pages1 en Act Part1 v8 0Tara ReashaNo ratings yet
- Root Cause AnalysisDocument6 pagesRoot Cause Analysisapi-448506260No ratings yet
- Meeting Room Hazard Inspection ChecklistDocument3 pagesMeeting Room Hazard Inspection ChecklistAshishKiran SinghNo ratings yet
- Chronic Fatigue Syndrome Caused by Electromagnetic Fields (EMF) ?Document6 pagesChronic Fatigue Syndrome Caused by Electromagnetic Fields (EMF) ?SwissTeslaNo ratings yet
- H-1-Contractor HCT EHSMS Agreement FormDocument2 pagesH-1-Contractor HCT EHSMS Agreement FormRex SantosNo ratings yet
- 1 s2.0 S1360859220301704 MainDocument6 pages1 s2.0 S1360859220301704 MainJuan David Arenas MendozaNo ratings yet