Professional Documents
Culture Documents
General Anesthesia
General Anesthesia
Uploaded by
dqnxfdw6bjOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
General Anesthesia
General Anesthesia
Uploaded by
dqnxfdw6bjCopyright:
Available Formats
Inhaled anesthetics properties
Inhaled anesthetics properties
Gas blood solubility / blood gas Gas lipid solubility / Oil/gas
partition coe cient partition coe cient
Check the e ectiveness of the To determine potency
anesthetics How much is the dose / determine
potency
Gas blood solubility / blood gas partition coe cient
High solubility Lowe solubility
Longer time to saturate blood Quickly saturate blood
Slower induction time Quick induction time
Slower washout Quick washout
- [blood]1.4>[alveoli]
The higher the number =
dissolve well in blood = slow
induction
Gas blood solubility: after blood saturated
here gas start being in it’s gas form because
it can’t dissolve anymore = measured by
partial pressure = more gas not dissolved the
higher the partial pressure
• Molecules dissolved in blood: No
anesthetic e ect
• Molecules NOT dissolved: Anesthetic e ect
• Need to saturate blood to generate
partial pressure
• So MORE solubility in blood = LONGER to
take e ect
Gas lipid solubility / oil/gas partition coe cient
↑lipid a nity = more potent (Meyer-Overton rule)
MAC / minimum alveolar concentration low = need small dose concentration of anesthetic to prevents
movement in 50% ( 1 MAC = 50% e cacy )
= high potency ( less dose ) and high lipid solubility
Bene t of MAC is drug combination: use multiple
drugs small doses and avoid side e ect
Determine multiple drugs potency: by adding the
MAC up
Take home points:
- ↑blood solubility = ↑blood / gas partition coe cient = slower induction
- ↓MAC = ↑oil / gas partition coe cient = ↑potent / low dose
- MAC = dose = lower MAC mean we need low dose of the drug to be e ective
fi
ff
ffi
ff
ff
ffi
ffi
ffi
ff
ffi
ff
ffi
ffi
ffi
ff
Special Side E ects of inhaled anesthesia
Halothane – Hepatotoxicity & malignant hyperthermia
• Liver tox: Rare, life-threatening
• Massive necrosis, increased AST/ALT
Methoxy urane – Nephrotoxicity
• Renal-toxic metabolite
En urane – Seizures
• Lowers seizure threshold
GABA Receptor Intravenous Anesthetics
• Etomidate
• Propofol
• Benzodiazepines
• Barbiturates ( thiopental / pentothal )
• GABA is largely inhibitory
• These drugs activate receptor→sedation
Clinical use scenarios of anesthesia:
Induction ( mostly IV drug ): Put patient to sleep
• Propofol
• Etomidate
• Ketamine
Maintenance – Keep patient asleep ( usually use inhaled
anesthesia )
• Propofol
• sevo urane
• des urane
Typical Open Heart Case
Induction
• Propofol, Midazolam ( give some amnesia)
Paralysis
• Rocuronium
Maintenance
• Sevo urane( to put the patient to sleep but don’t stop the
pain ), fentanyl ( to block pain )
Example of opioid overdose
Pharma equations
1. blood gas partition coe cient: [blood]1.4>[alveoli]
2. Lipid solubility or potency equation
fl
fl
fl
fl
fl
ff
ffi
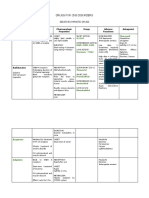
Intravenous anesthesia drugs:
Mechanism Uses and Potency Side e ect
Barbiturates Binding to GABA High potency from high lipid Myocardial / respiratory depression
( thiopental / receptor solubility easily cross BBB ↓ cerebral blood ow
Pentothal ) Ultra short acting because the drug
will redistribute / stored into muscle
and fat but is take long time to
washout
Rapid - onset short - acting
Benzodiazepines • Bind to GABA Orally they are anti-anxiety and IV • Cause cardio-respiratory depression
Midazolam, receptors = increase they are anesthesia =↓BP
Lorazepam, frequency of GABA ion • Overdose: treated by Flumazenil
Diazepam, channel opening = • Low dose: anti-anxiety (anxiolytic) • Midazolam (Versed): Short
Alprazolam Increase level of CI • High dose: sedation, amnesia, procedures (endoscopy)
make muscle less anticonvulsant
likely to depolarize
Opioids Act on opioid (mu) Orally for chronic pain and high dose Side e ects:
Morphine,Fentan receptors in brain IV for anesthesia • ↓respiratory drive
yl, • opioids bind to Mu People who take them for chronic • ↓BP
Hydromorphone receptors pain over long term develop tolerance • Nausea/vomiting
• G-protein linked and decrease e ectiveness = major • Ileus
• 2nd messengers not problem with cancer pain • Urinary retention
clearly understood • No amnesia
• Increase K e ux Decreased e ect on
from cells causing • Pain Overdose:
HYPERpolarizes→l • Sedation Cause life threatening respiratory
ess pain • Nausea, vomiting depression treated by naloxone
transmission • Respiratory depression Opioid antidote / Mu antagonist
• Cough suppression Reverses e ects within minutes
Important to give drug • Urinary retention
Must be given IV/nasal→ because it’s
cause amnesia inactivated by liver if it given orally
because opioids are • No tolerance to constipation or
analgesics but have miosis
no amnesia e ect
Ketamine PCP / phencyclidine / It’s dissociative drug mean cause Good thing about ketamine it have few
angel dust derivative ( analgesia and amnesia ( they will not respiratory and cardiovascular side
abused by people but remember anything ) e ect
important side e ect
hallucination and Can cause ↑BP ↑HR
being violent ) When it’s abused as street drug it cause
hallucination and violent behaviors
Antagonist of NMDA
receptor ( NMDA are If ketamine used alone when the patient
receptor activated by wake up will have “Emergence
glutamate) Reactions” can stay for few hours
• Disorientation
• Dreams, hallucinations
•Can be frightening to patients
• Co-administer midazolam
( Benzodiazepines )
to help
Etomidate Modulates GABA Relatively hemodynamically neutral Blocks cortisol synthesis = cause acute
receptors / Blocks • Good for hypotensive patients adrenal insu ciency
neuro excitation
Used for Rapid sequence intubation Etomidate and succinglcholine both
Anesthesia but not for patient in severe respiratory washout very fast
analgesia = mean the distress and need emergency placed
patient can be sleep on a ventilator
but still feel pain Usually in this case it’s co-
administrated with succinglcholine
Propofol GABA modulator Used mostly for patient of ventilator Myocardial depression
Quick induction Sedation, amnesia Hypotension
ff
ff
ff
ff
ffi
ffl
ff
ff
ff
ff
fl
You might also like
- Adrenergic ReceptorsDocument1 pageAdrenergic ReceptorsBobet ReñaNo ratings yet
- USONA INSTITUTE - 2018 - Psilocybin Investigator BrochureDocument59 pagesUSONA INSTITUTE - 2018 - Psilocybin Investigator BrochureSandro RodriguesNo ratings yet
- Anesthesia PharmacologyDocument41 pagesAnesthesia PharmacologyHassan.shehri88% (8)
- General Anesthetics TRANSDocument15 pagesGeneral Anesthetics TRANSNikki Tuazon BartolomeNo ratings yet
- SNS and PNS Drugs (Cholinergics and Adrenergics)Document5 pagesSNS and PNS Drugs (Cholinergics and Adrenergics)Whitney Krabbenhoft100% (1)
- Butorphanol Tartrate (Drug Study)Document2 pagesButorphanol Tartrate (Drug Study)Franz.thenurse6888100% (2)
- Compare and Contrast Neostigmine and The Organophosphate CompoundsDocument1 pageCompare and Contrast Neostigmine and The Organophosphate CompoundsDonkeyManNo ratings yet
- Nitrous Oxide Isoflurane Halothane Enflurane Sevoflurane DesfluraneDocument3 pagesNitrous Oxide Isoflurane Halothane Enflurane Sevoflurane DesfluraneNariska CooperNo ratings yet
- Sedative-Hypnotic Drugs: Alprazolam Chlordiazepoxide Clonazepam ClorazepateDocument8 pagesSedative-Hypnotic Drugs: Alprazolam Chlordiazepoxide Clonazepam ClorazepateCas BuNo ratings yet
- Sedatives & HypnoticsDocument49 pagesSedatives & HypnoticsShubha DiwakarNo ratings yet
- Barbiturates Drug SummaryDocument5 pagesBarbiturates Drug SummarySydney JenningsNo ratings yet
- Clinical Pharmacology of Anesthetic Drugs: Dr. Waddah H. AwadDocument37 pagesClinical Pharmacology of Anesthetic Drugs: Dr. Waddah H. AwadwaddahawadNo ratings yet
- CNS DepressantsDocument69 pagesCNS DepressantsMicah Lou Calamba100% (1)
- Sedative HypnoticDocument60 pagesSedative HypnoticNeeraj KumarNo ratings yet
- MalnutritionDocument22 pagesMalnutritionkelvinamin12No ratings yet
- By Duy Thai, 1997: Pharmacology Semester 1 Page 1 of 5Document5 pagesBy Duy Thai, 1997: Pharmacology Semester 1 Page 1 of 5ravi2likeNo ratings yet
- General Anaesthesia: I Made Agus Kresna SucandraDocument38 pagesGeneral Anaesthesia: I Made Agus Kresna SucandraGianna GraciellaNo ratings yet
- Sedative HypnoticsDocument27 pagesSedative HypnoticsPrecious FulgarinasNo ratings yet
- Drugs For AsthmaDocument1 pageDrugs For Asthmakamil malikNo ratings yet
- Lecture 28 - 3rd Asessment - Sedatives, HypnoticsDocument32 pagesLecture 28 - 3rd Asessment - Sedatives, Hypnoticsapi-3703352100% (1)
- General Anaesthesia & Skeletal Muscle RelaxantDocument31 pagesGeneral Anaesthesia & Skeletal Muscle RelaxantDeepti SinglaNo ratings yet
- General Anesthesia For NursingDocument53 pagesGeneral Anesthesia For Nursingpuneetkumar7089No ratings yet
- Hypnotics and SedativesDocument22 pagesHypnotics and Sedativeskavya nainitaNo ratings yet
- Drugs Used For Treatment of Asthma - 1Document6 pagesDrugs Used For Treatment of Asthma - 1ireneNo ratings yet
- Impaired Gas ExchangeDocument1 pageImpaired Gas Exchangeruggero07No ratings yet
- General Anaesthesia: I Made Agus Kresna SucandraDocument37 pagesGeneral Anaesthesia: I Made Agus Kresna SucandraBakingpancakesNo ratings yet
- Local AnaestheticsDocument27 pagesLocal AnaestheticsRawand Ra'ed D.AlshawabkehNo ratings yet
- Patrick: An Introduction To Medicinal Chemistry 4e: Enzymes As Drug TargetsDocument43 pagesPatrick: An Introduction To Medicinal Chemistry 4e: Enzymes As Drug TargetsVishaka KashyapNo ratings yet
- General Anesthesia: by Dr. AnindyaDocument83 pagesGeneral Anesthesia: by Dr. Anindyaalhada azofit almaNo ratings yet
- Recent Advances of TDDS: The Ultra-Deformable Vesicle (UDV) : by Sarah AdindaputeriDocument21 pagesRecent Advances of TDDS: The Ultra-Deformable Vesicle (UDV) : by Sarah AdindaputeriClarence WorthingtonNo ratings yet
- General Anaesthesia: I Made Agus Kresna SucandraDocument39 pagesGeneral Anaesthesia: I Made Agus Kresna SucandraDoqaNo ratings yet
- Local AnestheticsDocument44 pagesLocal Anestheticsblack pink in ur area 21No ratings yet
- Pharmacology - Drugs For CNS DisordersDocument4 pagesPharmacology - Drugs For CNS DisordersJireh MejinoNo ratings yet
- Cocaine Corneal Sloughing: Low Potency (Short DOA)Document4 pagesCocaine Corneal Sloughing: Low Potency (Short DOA)Thulasi tootsieNo ratings yet
- Pharmacology IV L5Document4 pagesPharmacology IV L5سلطان القلحNo ratings yet
- Drugs Acting On CNSDocument19 pagesDrugs Acting On CNSAditya sagarNo ratings yet
- Chapter 22 Sedative HypnoticsDocument7 pagesChapter 22 Sedative HypnoticsChristine Annmarie TapawanNo ratings yet
- SioooDocument4 pagesSioooanonymousNo ratings yet
- Basic Pharmacology PDFDocument27 pagesBasic Pharmacology PDFVizit DubeyNo ratings yet
- Farmako AnastesiaDocument4 pagesFarmako AnastesiaMuhammad Dafa Tira Pratista AkbarNo ratings yet
- Intravenous Anaesthetics: Thiopentone Methohexitone Propofol KetamineDocument9 pagesIntravenous Anaesthetics: Thiopentone Methohexitone Propofol KetamineTomNo ratings yet
- Name: Enjel Fanecha Difa NIM: 21117049 Major: Psik BDocument5 pagesName: Enjel Fanecha Difa NIM: 21117049 Major: Psik BEnjelNo ratings yet
- (Local Anaesthetics) : Dr. MizajDocument17 pages(Local Anaesthetics) : Dr. MizajaliNo ratings yet
- Jenis ShockDocument6 pagesJenis ShockMUHAMAD PATHU ROHMANNo ratings yet
- Sedative & HypnoticsDocument60 pagesSedative & HypnoticsDr Nilesh Patel100% (1)
- ANS DrugsDocument68 pagesANS DrugsROSEMARIE ONGNo ratings yet
- BenzodiazepinesDocument35 pagesBenzodiazepinesanaeshklNo ratings yet
- Leanna R. Miller: LRM ConsultingDocument20 pagesLeanna R. Miller: LRM ConsultingreneecolemanNo ratings yet
- Wsop Asma - Prof Bambang SDocument67 pagesWsop Asma - Prof Bambang SSiti Arieanni KesumaNo ratings yet
- Simplified ACLS AlgorithmDocument1 pageSimplified ACLS AlgorithmBrianNo ratings yet
- Hypnotic and SedativeDocument16 pagesHypnotic and SedativeAnim 2499No ratings yet
- Sedative-Hypnotics (SeH) and AnxiolyticsDocument101 pagesSedative-Hypnotics (SeH) and Anxiolyticsmatchees-gone rogueNo ratings yet
- Learning Objectives: Drugs That Enhance Cholinergic TransmissionDocument3 pagesLearning Objectives: Drugs That Enhance Cholinergic TransmissionSamer FarhanNo ratings yet
- Ek Ah YG EIA: Page 4 Out of 11 PagesDocument1 pageEk Ah YG EIA: Page 4 Out of 11 PagesRebekah EquizNo ratings yet
- Assignment AnesthesiaDocument9 pagesAssignment AnesthesiaRavi PatelNo ratings yet
- Pre Anesthetics Local AnestheticsDocument45 pagesPre Anesthetics Local AnestheticsDR AbidNo ratings yet
- Hydrophobic Ion PairingDocument14 pagesHydrophobic Ion PairingSilvia Argelia Peraza KuNo ratings yet
- (Surg2) 5.1b Introduction To Anesthesia-Part 2Document16 pages(Surg2) 5.1b Introduction To Anesthesia-Part 2AlloiBialbaNo ratings yet
- Recreational Drugs and Sleep: DR Claire Durant Imperial College London, UKDocument24 pagesRecreational Drugs and Sleep: DR Claire Durant Imperial College London, UKSantiago Urzúa SaldívarNo ratings yet
- LOCAL ANESTHETICS and EMERGENCY DRUGSDocument7 pagesLOCAL ANESTHETICS and EMERGENCY DRUGSrosheanne0913No ratings yet
- Anti EmeticsDocument7 pagesAnti EmeticsPatricia BuzonNo ratings yet
- Autonomic SystemDocument5 pagesAutonomic Systemdqnxfdw6bjNo ratings yet
- MeningitisDocument5 pagesMeningitisdqnxfdw6bjNo ratings yet
- Pharma and GraphDocument2 pagesPharma and Graphdqnxfdw6bjNo ratings yet
- Crazy Laura Printable Pack JournalDocument65 pagesCrazy Laura Printable Pack Journaldqnxfdw6bjNo ratings yet
- Spinal Cord LesionDocument3 pagesSpinal Cord Lesiondqnxfdw6bjNo ratings yet
- تدبر في القرآن و ادعيهDocument27 pagesتدبر في القرآن و ادعيهdqnxfdw6bjNo ratings yet
- العون الإلهيDocument3 pagesالعون الإلهيdqnxfdw6bjNo ratings yet
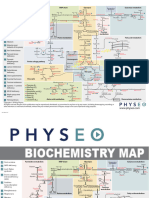
- Bio MapDocument2 pagesBio Mapdqnxfdw6bjNo ratings yet
- 6-Month UFABB With FA 2021Document16 pages6-Month UFABB With FA 2021dqnxfdw6bjNo ratings yet
- Jurnal EBCRDocument13 pagesJurnal EBCRDestry AryantyNo ratings yet
- Full Download PDF of Pharmacology For Medical Graduates, 4th Updated Edition Shanbhag - Ebook PDF All ChapterDocument69 pagesFull Download PDF of Pharmacology For Medical Graduates, 4th Updated Edition Shanbhag - Ebook PDF All Chaptermawlwdszende100% (6)
- HBI Blacklist Journals 2018Document123 pagesHBI Blacklist Journals 2018pptpptNo ratings yet
- Dr. Naitik D Trivedi & Dr. Upama N. Trivedi: Multiple Choice Questions (Pharmacology)Document65 pagesDr. Naitik D Trivedi & Dr. Upama N. Trivedi: Multiple Choice Questions (Pharmacology)Lokesh Mahata100% (1)
- 05 Paeds Drug Doses-1Document4 pages05 Paeds Drug Doses-1JunaidahMubarakAliNo ratings yet
- Puente PiedraDocument6 pagesPuente PiedraBotica Super FarmaNo ratings yet
- Bahasa Inggris Iii: 6. Giving InjectionDocument15 pagesBahasa Inggris Iii: 6. Giving InjectionErlangga PratamaNo ratings yet
- Magnesium Hydroxide (Milk of Magnesia)Document1 pageMagnesium Hydroxide (Milk of Magnesia)ENo ratings yet
- Pharmacology MnemonicsDocument17 pagesPharmacology MnemonicsJuvenis SampangNo ratings yet
- Steroid Tapering and Supportive Treatment Guidance V1.0 PDFDocument1 pageSteroid Tapering and Supportive Treatment Guidance V1.0 PDFPatricia MaisekaNo ratings yet
- Final ColistinDocument3 pagesFinal ColistinGwyn RosalesNo ratings yet
- Soal KpbiDocument5 pagesSoal KpbiTiffany Sabilla RamadhaniNo ratings yet
- Pharmacology ScrapbookDocument89 pagesPharmacology ScrapbookJesell France PlanaNo ratings yet
- 3.2 TheophyllineDocument3 pages3.2 TheophyllinesarahabdullahNo ratings yet
- Price ListDocument39 pagesPrice ListHarloXsiNo ratings yet
- Farmakologi KlinikDocument29 pagesFarmakologi KlinikMaria elisabethNo ratings yet
- SemaglutideDocument95 pagesSemaglutideShigma Putra Mahaley100% (1)
- Hydroxy ZineDocument2 pagesHydroxy ZineSharmaine Grace FlorigNo ratings yet
- Good Practice in CompoundingDocument53 pagesGood Practice in Compoundingvicky_law_2100% (1)
- PharmacologyDocument3 pagesPharmacologyVISHAKHANo ratings yet
- CCIM MD Dravyaguna Final SyllabusDocument12 pagesCCIM MD Dravyaguna Final SyllabusGiridhar VedantamNo ratings yet
- Clinical Trials and Drug DevelopmentDocument109 pagesClinical Trials and Drug DevelopmentYasimini RamadhaniNo ratings yet
- GuidelinesDocument94 pagesGuidelinesMichael PiducaNo ratings yet
- The Extract of Mucuna Pruriens Possesses Histamine Activity: Asian Pacific Journal of Tropical MedicineDocument3 pagesThe Extract of Mucuna Pruriens Possesses Histamine Activity: Asian Pacific Journal of Tropical MedicineSergio Andres Salas CoronelNo ratings yet
- Item Baru Klinik Pekanbaru 2022Document12 pagesItem Baru Klinik Pekanbaru 2022Listia NingsihNo ratings yet
- Fitri BHPDocument3 pagesFitri BHPekadwiyantiNo ratings yet
- Cms High Risk MedicationsDocument8 pagesCms High Risk MedicationsMihai VladescuNo ratings yet
- SPC - Ma130 00201Document6 pagesSPC - Ma130 00201Cassia FistulaNo ratings yet