Professional Documents
Culture Documents
Chapter 2 Lesson 1 and 2
Chapter 2 Lesson 1 and 2
Uploaded by
helainemaeinesCopyright:
Available Formats
You might also like
- Wade AssessmentDocument5 pagesWade Assessmentapi-58457466550% (2)
- Launtop ManualDocument48 pagesLauntop ManualMatZancNo ratings yet
- Biobase Elisa Microplate Reader BK-EL10C User Manual 202103Document48 pagesBiobase Elisa Microplate Reader BK-EL10C User Manual 202103Victor BlancoNo ratings yet
- Framework For Maternal and Child Health NursingDocument7 pagesFramework For Maternal and Child Health NursingJan Oliver Yares100% (1)
- Baxter Storey BrochureDocument30 pagesBaxter Storey Brochurediv_anNo ratings yet
- The Ultimate Healthy Grocery List PDFDocument1 pageThe Ultimate Healthy Grocery List PDFHazwan Ariff HakimiNo ratings yet
- Physiology PF PuerperiumDocument34 pagesPhysiology PF PuerperiumKholoud Kholoud100% (4)
- Maternal & Child NUrsing SylabusDocument7 pagesMaternal & Child NUrsing Sylabusmarsan12No ratings yet
- Care of Mother, Child, Family and Population Group At-Risk or With ProblemsDocument52 pagesCare of Mother, Child, Family and Population Group At-Risk or With ProblemsMelchor Felipe Salvosa100% (1)
- CHN NotesDocument7 pagesCHN NotesAnvi Turingan PedronanNo ratings yet
- Fundamentals of NursingDocument29 pagesFundamentals of NursingThierd Cañete IIINo ratings yet
- Module 1 NCM 107 NewDocument44 pagesModule 1 NCM 107 NewAmethystNo ratings yet
- Module 1 NCM 100Document10 pagesModule 1 NCM 100ApRil Anne BalanonNo ratings yet
- Nursing Care During Normal Pregnancy Care of Dev FetusDocument5 pagesNursing Care During Normal Pregnancy Care of Dev FetusLuna Sang-anNo ratings yet
- Foundation For Maternal and Child Health NursingDocument18 pagesFoundation For Maternal and Child Health NursingChari RivoNo ratings yet
- Nursing Care of A Family With A ToddlerDocument37 pagesNursing Care of A Family With A ToddlerKarly Alissa TarubalNo ratings yet
- Maternal & Child Nursing Care: Lecture NotesDocument42 pagesMaternal & Child Nursing Care: Lecture NotesMidori San100% (1)
- Models of Health IllnessDocument3 pagesModels of Health Illnessjerikacorpuzmiranda100% (1)
- Maternal and Child Health Nursing (NCM 101 Lect) Part 1Document4 pagesMaternal and Child Health Nursing (NCM 101 Lect) Part 1yunjung0518100% (7)
- Brokenshire College Socsksargen, Inc.: NCM 100-Theorerical Foundations in NursingDocument8 pagesBrokenshire College Socsksargen, Inc.: NCM 100-Theorerical Foundations in NursingKeren Happuch EspirituNo ratings yet
- NCM 101 (Continuation) Postpartal Period and PediatricsDocument29 pagesNCM 101 (Continuation) Postpartal Period and PediatricsAudi Kyle SaydovenNo ratings yet
- Maternal and Child Nursing 1 Skills Lab Modele s1Document3 pagesMaternal and Child Nursing 1 Skills Lab Modele s1Crystal MaidenNo ratings yet
- Notes - MCHN - Chapter 1Document12 pagesNotes - MCHN - Chapter 1Jamaica mitalNo ratings yet
- 1.1. Concept of ManDocument27 pages1.1. Concept of ManTrisha SabaNo ratings yet
- Gravidity and ParityDocument11 pagesGravidity and ParityShahad HakimuddinNo ratings yet
- Module 3 Responsibilities of A Beginning Nurse ResearcherDocument9 pagesModule 3 Responsibilities of A Beginning Nurse ResearcherCaitlynNo ratings yet
- A. Goals and Philosophies of Maternal and Child Health Nursing The 2020 National Health GoalsDocument3 pagesA. Goals and Philosophies of Maternal and Child Health Nursing The 2020 National Health GoalsJoymae Olivares TamayoNo ratings yet
- Syllabus NCM 109 Care of Mother Child Adolescent at Risk or With ProblemDocument37 pagesSyllabus NCM 109 Care of Mother Child Adolescent at Risk or With Problembrilliant dumay100% (1)
- Nutri Lab 10Document38 pagesNutri Lab 10Carl Josef C. GarciaNo ratings yet
- Community Health NursingDocument23 pagesCommunity Health NursingMimi Vee100% (1)
- Ethico Legal Dilemmas in Critical Care NursingDocument36 pagesEthico Legal Dilemmas in Critical Care NursingNica Marie LumbaNo ratings yet
- Problems Associated With Chronic IllnessDocument8 pagesProblems Associated With Chronic IllnessMeryville JacildoNo ratings yet
- Finals TFN ReviewerDocument5 pagesFinals TFN ReviewerNicole Faith L. NacarioNo ratings yet
- MCHN Reviewer 1Document24 pagesMCHN Reviewer 1Steam LcNo ratings yet
- Ctu CCMC Level 3 NCM 1Document15 pagesCtu CCMC Level 3 NCM 1Divina VillarinNo ratings yet
- Prenatal Management (Part 5)Document36 pagesPrenatal Management (Part 5)Austine James Sabenicio PantiloNo ratings yet
- Professional Adjustment Final 2Document41 pagesProfessional Adjustment Final 2lielani_martinezNo ratings yet
- Funda Lec ReviewerDocument16 pagesFunda Lec ReviewerTricia Maxine DomingoNo ratings yet
- Advance Practice in Maternal and Child Nursing 1 High Risk Pregnancy: Nursing Care of A Family Experiencing A Pregnancy Complication From A Pre-Existing or Newly Acquired IllnessDocument31 pagesAdvance Practice in Maternal and Child Nursing 1 High Risk Pregnancy: Nursing Care of A Family Experiencing A Pregnancy Complication From A Pre-Existing or Newly Acquired Illnessallanrnmanaloto100% (2)
- Nursing Care of The Older Adult in Chronic IllnessDocument19 pagesNursing Care of The Older Adult in Chronic IllnessWen SilverNo ratings yet
- NCM 103 Syllabus ObeDocument20 pagesNCM 103 Syllabus Obeۦۦ JamesNo ratings yet
- HeheezjghDocument7 pagesHeheezjghDemiar Madlansacay QuintoNo ratings yet
- Transcultural Nursing TheoryDocument44 pagesTranscultural Nursing TheoryShweta KateNo ratings yet
- Care of The Mother and The Fetus During The Prenatal Period (Part 2)Document20 pagesCare of The Mother and The Fetus During The Prenatal Period (Part 2)Austine James Sabenicio PantiloNo ratings yet
- Maternal NewDocument30 pagesMaternal NewKhristine Rose Sanchez CaloNo ratings yet
- Concept of Man Health IllnessDocument12 pagesConcept of Man Health IllnessFrances Nicole FloresNo ratings yet
- Unit 1 - Week (1) - Comprehensive Assessment: Intended Learning Outcomes (Week 1-ILO)Document28 pagesUnit 1 - Week (1) - Comprehensive Assessment: Intended Learning Outcomes (Week 1-ILO)John Van Dave TaturoNo ratings yet
- NCM114 - Learn Mat 1 2021Document32 pagesNCM114 - Learn Mat 1 2021jjNo ratings yet
- Rle 217... Typology of Nursing Problems in Family Nursing Practice MaglayaDocument6 pagesRle 217... Typology of Nursing Problems in Family Nursing Practice MaglayaMakspeyn del Valle - MoonNo ratings yet
- NCM 112-Mod2Document9 pagesNCM 112-Mod2Samantha BolanteNo ratings yet
- Intro To Psychiatric Mental HealthDocument75 pagesIntro To Psychiatric Mental HealthEryl Franz HerreraNo ratings yet
- Care of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManDocument26 pagesCare of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManLaurence Docog100% (1)
- NCMB314 Prelim ReadingsDocument77 pagesNCMB314 Prelim ReadingsNine SoleilNo ratings yet
- Course Outline-Ncm109Document10 pagesCourse Outline-Ncm109Charmagne Yanga EpantoNo ratings yet
- Pre Gestational GestationalDocument19 pagesPre Gestational GestationalRoger Jr PumarenNo ratings yet
- The Nursing Role in Genetic Assessment and Counseling The Nursing Role in Genetic Assessment and CounselingDocument35 pagesThe Nursing Role in Genetic Assessment and Counseling The Nursing Role in Genetic Assessment and CounselingBridget Shienne DaculaNo ratings yet
- Competency Appraisal 2 SyllabusDocument10 pagesCompetency Appraisal 2 SyllabusMary Janet Pinili100% (2)
- Maternal and Child HealthDocument7 pagesMaternal and Child HealthNessa Layos MorilloNo ratings yet
- NCM 119 - Rle (Prelim) Week 1: Immune Response Immunity: Natural and Acquired Immunity - Ma'am VAB Immune ResponseDocument13 pagesNCM 119 - Rle (Prelim) Week 1: Immune Response Immunity: Natural and Acquired Immunity - Ma'am VAB Immune ResponseJamaica Leslie Noveno100% (1)
- 1 Gerontology Nursing Concepts: Gloria P. de Leon, RN, RM, ManDocument211 pages1 Gerontology Nursing Concepts: Gloria P. de Leon, RN, RM, ManJohanine VillasantiagoNo ratings yet
- Concepts & Patterns of Human Behavior Mal Adap LecDocument4 pagesConcepts & Patterns of Human Behavior Mal Adap LecAshtua MandixNo ratings yet
- Eteeap - NCM 106 Page 1Document5 pagesEteeap - NCM 106 Page 1Marisol Jane JomayaNo ratings yet
- NCM103 (FUNDA) Module 1 CommunicationDocument6 pagesNCM103 (FUNDA) Module 1 CommunicationJohn Joseph Cruz100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- NCM09 Ob Lec ReviewerDocument36 pagesNCM09 Ob Lec ReviewerChelsea Keith Sollano BalasabasNo ratings yet
- Bfe2218 Lazourdy 500gpm@6bar PDFDocument117 pagesBfe2218 Lazourdy 500gpm@6bar PDFYazan Tamimi50% (2)
- RESA Tax 1410 Preweek 165Document21 pagesRESA Tax 1410 Preweek 165Fordan AntolinoNo ratings yet
- The New Cairo Mall: DWG-MF0202.03 DWG - MF0202.04Document1 pageThe New Cairo Mall: DWG-MF0202.03 DWG - MF0202.04Mahmud MaherNo ratings yet
- Oil Filled CTs (72!5!420 KV)Document65 pagesOil Filled CTs (72!5!420 KV)kunalan_79860100% (1)
- Hemp Herbicide Poster PDFDocument1 pageHemp Herbicide Poster PDFPintrijel LaurNo ratings yet
- Force and Pressure MCQDocument6 pagesForce and Pressure MCQnitikaNo ratings yet
- Test Bank Linux For Programmers and Users SolutionDocument4 pagesTest Bank Linux For Programmers and Users SolutionRichard1LauritsenNo ratings yet
- Issues N Chalenges in Health ManagementDocument133 pagesIssues N Chalenges in Health ManagementRachana Karki100% (1)
- Quiz Lu1 Y3 A PDFDocument3 pagesQuiz Lu1 Y3 A PDFWilfharry billyNo ratings yet
- Akhtamov A.A. - Reading Comprehension TestsDocument48 pagesAkhtamov A.A. - Reading Comprehension TestsKhalid TsouliNo ratings yet
- Unit 2 EVSDocument10 pagesUnit 2 EVSVenkatesh KumarNo ratings yet
- Goodhormonehealth News Jan16 PDFDocument10 pagesGoodhormonehealth News Jan16 PDFBrian CoxNo ratings yet
- Pre-Setting Manual Balancing Valves CIM 788: Technical InformationDocument7 pagesPre-Setting Manual Balancing Valves CIM 788: Technical InformationblindjaxxNo ratings yet
- Dowlex Lldpe 2645GDocument3 pagesDowlex Lldpe 2645GSalustraNo ratings yet
- Disability Report V03 SinglePagesDocument44 pagesDisability Report V03 SinglePagesAmerlia AdzianNo ratings yet
- Elephant MindDocument4 pagesElephant MindHardev SinghNo ratings yet
- Gas Exchange Mind MapDocument1 pageGas Exchange Mind MapWilliam karuniawan SentosaNo ratings yet
- Jayson Desear: 3. What Is The Importance of Legislation in The Development and Sustenance of Special Education Programs?Document2 pagesJayson Desear: 3. What Is The Importance of Legislation in The Development and Sustenance of Special Education Programs?Jayson Desear100% (3)
- July 12, 2019 Strathmore TimesDocument20 pagesJuly 12, 2019 Strathmore TimesStrathmore TimesNo ratings yet
- Ebp PosterDocument1 pageEbp Posterapi-340595961No ratings yet
- Your Habit Body A Better Model of The Unconscious For EveryoneDocument24 pagesYour Habit Body A Better Model of The Unconscious For EveryoneBubi Sutomo100% (1)
- Refex 134a SpecDocument15 pagesRefex 134a SpecSami ThirunavukkarasuNo ratings yet
- Quran MessageDocument1 pageQuran Messagekamallove7481No ratings yet
- Saudi Aramco Inspection ChecklistDocument22 pagesSaudi Aramco Inspection Checklistabdulgafoor54100% (2)
Chapter 2 Lesson 1 and 2
Chapter 2 Lesson 1 and 2
Uploaded by
helainemaeinesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 2 Lesson 1 and 2
Chapter 2 Lesson 1 and 2
Uploaded by
helainemaeinesCopyright:
Available Formats
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |1
CHAPTER 2. CARE OF AT-RISK/ HIGH-RISK AND SICK MOTHER
Several factors can make a pregnancy high risk, including existing health conditions, the
mother’s age, lifestyle, and health issues that happen before or during pregnancy.
The chapter will entail the nursing care of at-risk and high-risk pregnant clients. You are going
to learn how to apply the nursing process in the care of the different disease processes as to the
identification of clients who are at risk, pre-gestational conditions, gestational conditions, and
gestational conditions.
The core concepts in maternal and child health nursing that you need to comprehend in this
chapter include the following:
Lesson 1: Identifying Clients at Risk
Lesson 2: Pre-gestational Conditions
Lesson 3: Gestational Conditions
LESSON 1: IDENTIFYING CLIENTS AT RISK
Introduction of the Lesson and Presentation of Outcomes
Most of the time having a baby is a natural process. After a full-term pregnancy, women go
into labor on or near their due date and give birth to a healthy baby. A day or two later they leave the
hospital to begin day-to-day life with their growing family. But not all pregnancies go smoothly. Some
women experience what doctors refer to as a high-risk pregnancy.
At the end of this lesson, you must have:
1. defined high-risk pregnancy;
2. defined at-risk individual;
3. defined risk factors; and
4. explained the different factors that may put the pregnancy at risk.
Warm-up Activity
Before you go to the learning inputs, try to list down five (5) factors that may put the
pregnancy at risk and explain. You discuss it with your classmates!
Learning Input
A pregnancy is considered high-risk when there are potential complications that could affect
the mother, the baby, or both. High-risk pregnancies require management by a specialist to help
ensure the best outcome for the mother and baby. A high-risk pregnancy is used to describe a situation
in which a mother, her fetus, or both are at higher risk for problems during pregnancy or delivery than
in a typical pregnancy.
Risk Pregnancy – is a pregnancy with a pre-existing or developing condition that threatens the
progression of the pregnancy, labor and delivery of a healthy term infant.
1
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |2
Risk Factors – are characteristics or circumstances of a person or group that are associated
with an increased risk of developing or being affected by a morbid process.
At-Risk Individual – is a person with an increased expectation of disease or complication.
Factors that may put the pregnancy at risk:
A. Personal-social factors
1. Maternal age (below 16 years old and above 35 years)
2. Birth interval
3. Weight is less than 100 pounds and more than 200 pounds
4. Height less than 5 feet
B. Socio-economic factors
1. Poor diet/ nutritional deficiencies
2. Low Income
3. Low educational level
C. Behavioral factors
1. Maternal behaviors
2. Smoking
3. Use of drugs
4. Use of alcohol
5. Intake of caffeine
D. Occupational factors
E. Health care delivery
Activity
For you to reflect on your learning in this lesson, watch this video and try to ponder on the
message.
https://www.youtube.com/watch?v=4mFvBQcyrLw
Wrap-up Activity
The care is given in family planning and gynecology centres provides a potential opportunity
to maximize maternal and fetal health benefits before conception. In the future, as a part of a health
institution, how can you contribute to the assessment of pregnant clients who are at-risk for high-risk?
Post-Assessment
Your instructor thru MVLE will give a summative test on the lessons of the chapter. Please
wait for further instructions. Good luck!
References
Silbert-Flagg, J. A., & Pillitteri, A. (2018). Maternal & child health nursing: Care of the childbearing &
childrearing family.
2
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |3
LESSON 2: PRE-GESTATIONAL CONDITIONS
Introduction of the Lesson and Presentation of Outcomes
When a woman enters pregnancy with a chronic condition such as cardiovascular or kidney
disease, both she and the fetus can be at risk for complications because either the pregnancy can
complicate the disease or the disease can complicate the pregnancy, affecting the baby or leaving a
woman less equipped to function in the future or undergo a future pregnancy. Nursing care for a
woman with a pre-existing illness focuses on close observation of maternal health and fetal well-being,
education of a woman and her family about special danger signs to watch for during pregnancy, and
actions to minimize complications whenever possible.
At the end of this lesson, you must have:
1. described common illnesses such as cardiovascular disease, diabetes mellitus, or renal
and blood disorders that can result in complications when they exist with pregnancy;
2. analyzed ways to provide nursing care can remain family-centred when a pre-existing or
newly acquired illness develops during pregnancy;
3. assessed a woman with an illness during pregnancy for changes occurring in the illness
because of the pregnancy or the pregnancy because of the illness;
4. formulated nursing diagnoses related to the effect of a pre-existing or newly acquired
illness on pregnancy;
5. identified expected outcomes that will contribute to a safe pregnancy outcome when
illness occurs with pregnancy;
6. formulated a plan of nursing care for a woman with an illness during pregnancy;
7. implemented nursing care for a woman when illness complicates the pregnancy; and
8. evaluated expected outcomes for achievement and effectiveness of care.
Warm-up Activity
Before you go to the learning inputs, try to list down five (5) pre-existing conditions that may
put pregnant clients that may put the pregnancy at risk and explain. You discuss it with your
classmates!
Learning Input
1. Pregnant client with preexisting or newly acquired illness
a. Diabetes mellitus-a hereditary endocrine disorder characterized by inadequate or lack of insulin
production that results in impaired glucose absorption and metabolism resulting in
hyperglycemia.
Classification of Diabetes mellitus:
1. Type 1- a state characterized by the destruction of the beta cells in the pancreas that
usually leads to absolute insulin deficiency.
2. Type 2- a state that usually arises because of insulin resistance combined with a relative
deficiency in the production of insulin.
3
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |4
3. Gestational Diabetes- a condition of abnormal glucose metabolism that arises during
pregnancy. Possible signal of an increased risk for type 2 diabetes later in life.
4. Impaired glucose homeostasis-a state between “normal” and “diabetes” in which the
body is no longer using and /or secreting insulin properly.
Risk Factors in Developing Gestational Diabetes Mellitus:
1. Obesity
2. Age over 25 years
3. History of large babies (10 lbs or more)
4. History of unexplained fetal or perinatal loss
5. History of congenital anomalies in previous pregnancies
6. History of polycystic ovary syndrome
7. Family history of DM
8. Member of a population with a high risk for diabetes (Native American, Hispanic, Asian)
Signs and Symptoms of Diabetes Mellitus:
1. Hyperglycemia
2. Glycosuria
3. Polyuria
4. Polydipsia
5. Weight loss
6. Ketoacidosis
Effects of Diabetes on the Mother:
1. Increased tendency to preeclampsia and eclampsia, UTI and candidiasis
2. Higher incidence of dystocia because of a large infant
3. At increased risk for postpartum haemorrhage due to over distention of the uterus
4. Hydramnios
5. Maternal mortality
6. Diabetic retinopathy
7. Diabetic nephropathy
8. Preterm delivery
Effects of Diabetes on the infant:
1. Macrosomia refers to a baby that is considerably larger than normal.
2. Birth injury
3. Hypoglycemia
4. Respiratory distress
5. Prematurity
6. Predisposition to diabetes mellitus later in life
Prenatal Management:
1. Diagnosis: Suspect DM in women
a. With a family history of DM
b. With a history of unexplained repeated abortions and stillbirth
4
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |5
c. With glycosuria
d. Who are obese
e. Who has a history of giving birth to large infants over 10 pounds and in infants with
congenital anomaly
2. Screening Tests
a. Universal screening test-a 50-gram glucose challenge test between 24-48 weeks
gestation regardless of the time of the time of the day and meals is done to pregnant
clients to determine if they are at risk for gestational diabetes. If the result of the
test is 140 mg/dl or higher after one hour, 100 gram three hour glucose tolerance
test is performed to confirm if the woman is having hyperglycemia. In this test, after
a fasting glucose sample is obtained, the woman drinks an oral 100-g glucose
solution; a venous blood sample is then taken for glucose determination at 1, 2 and
3 hours later. If two of the blood samples collected for this test are abnormal, or the
fasting value is above 95 mg/dl, a diagnosis of diabetes is made.
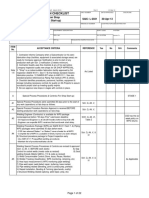
Table 2. Oral Glucose Challenge Test Values (Fasting Plasma Glucose Values) for
Pregnancy Following a 100-g Glucose Solution.
Test Type Pregnant Glucose Level
Fasting 95 mg/dl
1 hour 180 mg/dl
2 hours 155 mg/dl
3 hours 140 mg/dl
Other tests done to a pregnant woman with diabetes:
1. Glycosylated Hemoglobin (HbA1c)-measures the amount of glucose attached to
hemoglobin; used to detect the degree of hyperglycemia present; it reflects the
average blood glucose level over the past 4-6 weeks; this is used in monitoring
a woman with diabetes; upper normal level is 6% of the total hemoglobin.
2. Urine culture- done each trimester to detect asymptomatic UTIs as the increased
glucose concentration in urine may lead to increased infection.
3. Ophthalmic examination-done once to a woman with gestational diabetes and
at each trimester for women with known diabetes because common background
retinal changes that are common in diabetes such as increased exudate, dot
hemorrhage and macular edema can progress or originate during pregnancy.
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |6
3. Diet
a. Caloric intake should be enough to meet needs of fetus and mother (1, 800-2, 400
cal/day divided into 3 meals and three snacks to keep CHO evenly distributed during
the day so glucose remains constant); 20% of caloric intake should come from CHON
foods, 50% from CHOs, and 30% from fats.
b. Woman should be extremely nutrition conscious to maintain good control of glucose
and to keep her weight gain to a suitable amount (approximately 25-30 lbs) to limit
the size of the infant and make vaginal birth possible.
c. Teach and instruct to:
Reduce saturated fat
Reduce cholesterol
Increase dietary fiber
Avoid fasting and feasting
d. Have the woman become familiar with food exchange list and caloric values of foods
she usually eats to enable her to plan her diet properly and estimate her caloric intake
accurately.
e. The goal is to maintain a fasting blood sugar level of 90 mg/dl and postprandial blood
sugar level of 120 mg/dl.
4. Exercise
a. Aside from diet therapy, a liberal cardiovascular-conditioning exercise is the
management for gestational DM
b. ‘Exercise lowers blood glucose level and decreases the need for insulin
c. The exercise program should be individualized, performed regularly and under
supervision
d. Advise woman to eat complex carbohydrates before exercising to prevent
hypoglycemia.
5. Insulin Therapy
Insulin requirements increase during pregnancy.
Oral hypoglycemic such as Tolbutamide and Diamicron are contraindicated
during pregnancy because they are teratogenic for they can cross the placenta
and may cause fetal and newborn hypoglycemia.
Combined fast acting and intermediate insulin made up of human
derivative/humulin. Humulin is the insulin of choice during pregnancy because
it is the least allergenic.
2/3 in the morning, 1/3 at dinner administered SQ ½ hour before meals.
Insulin requirement is highest during the third trimester.
6. Home blood glucose monitoring
a. Done 4x a day-upon rising in the morning, before breakfast, lunch and dinner
b. Normal fasting: 90 mg/dl; postprandial: 120 mg/dl
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |7
7. Other nursing care:
a. Observe for urinary and vaginal tract infections particularly candidiasis
b. Assess for utero-placental functioning and fetal well-being
Serum alpha-feto protein- done at 15-17 weeks to assess for neural tube
defect
Ultrasound examination- performed at approximately 18-20 weeks to
detect gross abnormalities
Non-stress test or biophysical profile-to assess placental functioning
Fetal kick counts-to assess fetal well-being
Ultrasound examination-taken at 28 weeks then again at 36-38 weeks to
determine fetal growth, amniotic fluid volume, placental location and
biparietal diameter.
Lecithin/sphingomyelin ratio-done at 36 weeks to assess fetal maturity
Delivery:
1. Delivery is effected when the fetus is mature enough, after 38 weeks of gestation,
but not too large so as to cause cephalopelvic disproportion. Thus, early
hospitalization and labor induction is performed to deliver the baby before it
becomes too large to pass the birth canal
2. If cervix is not yet ripe, baby is macrosomic and fetal distress occurs, CS is
performed.
3. Regular insulin is given on the day of delivery not long acting insulin because insulin
requirement drops immediately after delivery. The woman may not require insulin
during the first 24 hours postpartum and her insulin requirements usually
fluctuates during the next few days.
Postpartum:
1. Recurrence of diabetes may occur in subsequent pregnancies
2. Women who developed gestational DM have higher tendency to develop overt
diabetes later in life
3. Newborn Care:
a. Keep warm because of poor temperature control mechanisms
b. Observe respiration (since hydramnios inflates stomach which pushes up and
interferes with diaphragm and lung expansion)
c. Observe for signs of hypoglycemia (shrill cry, weakness)-give glucose water
d. Observe for signs of hypocalcemia (tetany, tremors)-give calcium gluconate
e. Observe for congenital anomalies: esophageal atresia, neural tube defect
4. Contraception
a. IUD and combined oral contraceptives are contraindicated
b. Norplant (progestin implant system) and progestin only pill (minipills) may be
used safely by diabetic women
b. Cardiac Disease
Classification of Functional Capacity for Clients with Cardiac Disease:
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |8
1. Class I (Uncompromised)- The patient is asymptomatic, with no limitation of physical
activity; does not experience angina pain or any discomfort with ordinary physical
activity
2. Class II (Slightly Compromised)-patient with slight limitation of physical activity since
ordinary/normal activity cause dyspnea, fatigue, chest pain and palpitations.
3. Class III (Markedly Compromised)-Patient with marked limitation of physical activity
because less than ordinary activity cause excessive fatigue, palpitations, chest pain
and dyspnea. The patient is comfortable only at rest.
4. Class IV (Severely Compromised)- Patient experience symptoms even at rest and is
unable to perform any physical activity without discomfort.
Signs and Symptoms:
1. Difficulty of breathing-dyspnea, orthopnea, nocturnal dyspnea
2. Hemoptysis
3. Syncope with exertion
4. Chest pain
5. Cyanosis
6. Clubbing of fingers
7. Neck vein distention
8. Systolic and diastolic murmurs
9. Cardiomegaly
10. Arrythmia
11. Persistent split second sound
12. Pulmonary hypertension
Remember: a pregnant woman with heart disease should avoid infection, excessive
weight gain, edema and anemia because these conditions increase the workload of
the heart.
Complications:
1. Heart failure
2. Abortion
3. Premature labor
4. Intrauterine growth retardation
Management:
1. Prenatal care
a. Promotion of rest (Class I and Class II)
Woman should sleep at least 8 hours during the night and have frequent
rest periods during the day
Lie down for 30 minutes after each meal
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) |9
Allowed only is light work in the house, no heavy work, no stair climbing
and no exhaustion
b. Diet
Diet is high in iron, CHON, minerals and vitamins
Limit sodium intake, avoid foods with high content
Weight gain of no more than 24 lbs-excessive weight gain further increase
cardiac workload
c. Avoid high altitudes, smoking areas, unpressurised planes, and overcrowded
areas. Cigarette smoking and alcoholic beverages are strictly prohibited.
d. Prevent infection
Avoid persons with infections: common colds
Early treatment of infection-instruct to report immediately to her HCP if
she experience any sign of infection
e. Provide instructions on danger sign of heart failure:
Cough with rales is usually the first sign of impending heart failure
Increasing dyspnea, tachycardia, rales, edema
f. Medications:
Iron supplementation to prevent anemia
Digitalis to strengthen myocardial contraction and slow down heart rate
Nitroglycerine to relieve chest pain
Antibiotics to prevent and treat infection
Diuretics may be prescribed in case of heart failure
2. Intrapartal care
a. Early hospitalization-woman is hospitalized before labor begins to promote
bed rest, for closer supervision and prevent infection
b. Woman in labor is put in semi-fowler’s position or left lateral recumbent
position. No lithotomy position.
c. Vital Signs-monitored continuously. Tachycardia and RR more than 24 are signs
of impending cardiac decompensation. During the first stage of labor, monitor
vital signs every 15 minutes and more frequently during the second stage.
d. Epidural anesthesia-is instituted for painless and pushless delivery. Forceps is
used to shorten the second stage. Pushing is contraindicated.
e. Women with heart disease are poor candidates for CS due to increased risk for
hemorrhage, infection and thromboembolism
3. Postpartum Care
a. The most dangerous period is the immediate postpartum because of the
sudden increase in circulatory blood volume.
b. Monitor vital signs
c. Promote rest-restrict visitors to allow patient to rest; let woman stay in the
hospital until cardiac status has stabilized
d. Early but gradual ambulation to prevent thrombophlebitis
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) | 10
e. Breastfeeding is allowed if there are no signs of cardiac decompensation during
pregnancy, labor and puerperium
f. Medications:
Antibiotics to prevent infection
Stool softeners to prevent straining at stool caused by constipation
c. Anemia – it is defined as hemoglobin level of less than 11 g/dl in the first and third trimester
and less than 10.5 g/dl in the 2nd trimester.
Different anemia during pregnancy:
1. Acquired anemia
a. Iron-deficiency anemia-most common during pregnancy
b. Anemia from acute blood loss
c. Anemia from inflammation and malignancy
d. Megaloblastic anemia
e. Acquired hemolytic anemia
f. Aplastic or hypoplastic anemia
2. Hereditary anemia
a. Thallasemia
b. Sickle cell hemolobinnopathies
c. Other hemoglobinopathies
d. Hereditary hemolytic anemia
A. Iron Deficiency Anemia-this is the most common type of anemia during pregnancy.
Most women enter pregnancy without enough iron reserve so that deficiency develops
particularly on the 2nd and 3rd trimesters when iron requirements increases.
The newborn of the severely anemic mother is not affected by iron deficiency
anemia because the amount of iron transported to the fetus of an anemic mother
is almost the same as the amount transported to the fetus of a mother without
anemia.
Predisposing Factors:
1. Poor diet and nutrition
2. Heavy menses
3. Pregnancies at close intervals, successive pregnancies
4. Unwise reducing programs
Signs and Symptoms:
1. Easy fatigability
2. Sensitivity to cold
3. Proneness to infection
4. Dizziness
5. Laboratory Findings:
a. Erythrocyte hypochromia
b. Microcytosis
10
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) | 11
c. Elevated serum iron binding capacity
d. No stainable bone marrow iron
Effects of Anemia to Pregnancy:
1. Decreased resistance to infection
2. Associated with prematurity and low birth weight infants
3. Predispose to heavy bleeding during labor and puerperium
4. May increase digestive discomfort of pregnancy
Management:
1. Oral Iron supplementation-200 mg of elemental iron daily in the form of:
a. Ferrous sulfate-the most absorbable form of iron
b. Ferrous fumarate
c. Ferrous gluconate
Inform the mother about the possible side effects like tarry stool,
constipation, GIT discomfort
Take one hour before or two hours after meal for better absorption
Never take with milk but with citrus juice
If given in liquid form, use straw to prevent staining the teeth. Tell
patient to rinse mouth.
If iron is to be given parenterally, give IM by Z tract technique to
prevent tissue staining. Do not massage after injection.
2. Oral iron should be continued until three months after anemia has been
corrected
3. Increase intake of Vitamin C to enhance iron absorption
4. Increase intake of iron rich foods
a. Lean meats
b. Liver
c. Dark green leafy vegetables
d. Legumes-lima beans and green peas
B. Megaloblastic Anemia- a group of hematologic diseases caused by impaired DNA
synthesis resulting in blood and bone marrow abnormalities.
Types:
1. Folic Acid Deficiency Anemia/Pernicious anemia
2. Vitamin B12Deficiency/Addison Pernicious Anemia
Folic Acid Deficiency Anemia:
- Folic acid is necessary for the normal formation and nutrition of red blood cells.
Deficiency in folic acid leads to the formation of large and immature blood cells that
have shorter life span than normal red blood cells. It usually develops in women
whose diet consists mostly of meat products and those who do not eat fresh green
11
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) | 12
leafy vegetables. Women who have folic acid deficiency during pregnancy are more
at risk of giving birth to babies with neural tube defects like spina bifida.
Effects on pregnancy:
1. Abortion
2. Abruptio placenta
3. Neural tube defects in fetus
Predisposing Factors:
1. Poor nutrition
2. Multiple pregnancies
3. Successive pregnancies
Management:
1. Folic acid supplementation of 1 mg/day accompanied by oral iron RDA for
women-0.4 mg/day
2. Vitamin supplements containing 400 micrograms of folic acid are now
recommended for all women of childbearing age and during pregnancy. These
supplements are needed because natural food sources of folate are poorly
absorbed and much of the vitamin is destroyed in cooking.
Food Sources of Folate:
Leafy, dark green vegetables
Dried beans and peas
Citrus fruits and juices and most berries
Fortified breakfast cereals
Enriched grain products
Vitamin B12 Deficiency Anemia:
-Addison Pernicious Anemia is a very rare type of anemia. It is an uncommon auto
immune disorder caused by failure to absorb vitamin B12 because of lack of
intrinsic factor. Its onset is usually at 40 years of age and unless treated, it may lead
to sterility. Breast fed infants of women with vitamin B12 deficiency may also
develop the disorder in infancy.
Causes:
1. Total gastrectomy- treated with monthly IM injection of 1000 ug of
cyanocobalamine
2. Crohn’s disease
3. Ilial resection
4. Bacterial over growth in the large intestine
Sickle Cell Anemia
- A recessive inherited hemolytic anemia caused by an abnormal amino acid ibn the
beta chain of hemoglobin
- Disease is characterized by sickling of the RBC in the presence of decreased
oxygenation
- Majority of the RBCs are irregular or sickle –shaped so cannot carry as much
hemoglobin as normally-shaped RBCs. When oxygen tension becomes reduced, as
12
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) | 13
happens at high altitudes, or blood becomes more viscid than usual (dehydration),
the cells tend to clump because of the irregular shape. This clumping can result in
vessel blockage with reduced blood flow to organs. The cells will undergo
hemolysis leading to severe anemia.
- Increased risk of: preeclampsia, UTI, pneumonia because of impaired immune
functioning
- Results to abortion, fetal death, prematurity and IUGR.
e. Thyroid Disorders
-diseases that affect four times more women than men
Kinds:
1. Hyperthyroidism or maternal thyrotoxicosis- the second most common endocrine
disorder of pregnancy. It is due to the elevated level of thyroxine which causes fast
metabolism in the body resulting in low birth weight infant.
Signs and Symptoms:
1. Tachycardia
2. Enlarged thyroid gland
3. Exopthalmos
4. Weakness
5. Sweating
6. Failure to gain weight normally
Thyroid Storm- a major complication of hyperthyroidism manifested by high fever,
tachycardia, severe dehydration and occasional cardiac decompensation.
Management:
1. Medical treatment with the use of thiomide drugs like propylthiouracil and
methimazole until the woman is euthyroid. These drugs however, crosses the
placenta and may cause fetal goiter and hypothyroidism
2. Thyroidectomy-Surgical removal of the thyroid gland carried out during
pregnancy. Best performed during 2nd trimester of pregnancy.
Complications:
1. Preeclampsia
2. Heart Failure
3. Abortion
4. Stillbirth
5. Low birth weight
2. Hypothyroidism- caused by very low thyroxine levels that cause slow metabolism
resulting in still birth. This disease is also associated with infertility.
Management: Thyroxine Replacement Therapy
Complications: Preeclampsia, abruptio placenta, low birth weight, stillbirth
13
Chapter 2: Care of At-Risk/High-Risk Sick Mother
Instructional Module in NCM 117a (Care of Clients with Maladaptive Patterns of Behavior, Acute and
Chronic) | 14
f. Rh and blood group sensitization
Rh sensitization- results from antigen-antibody immunologic reaction within the body. It
occurs when an Rh (-) woman carries Rh (+) fetus, either to term or terminated by
spontaneous or induced abortion; or if Rh (-) non-pregnant woman receives an Rh (+)
blood transfusion.
-First offspring is not affected. However, in subsequent pregnancy, Rh antibodies cross
the placenta and enter the fetal circulation causing severe hemolysis leading to anemia.
ABO incompatibility- limited to type “O” mothers with type “A” or “B” fetus.
-Once the woman becomes pregnant, the maternal serum anti-A and anti-B antibodies
cross the placenta and produce hemolysis of the fetal RBCs.
Fetal risks:
Infant death due to Rh hemolytic disease
Marked feta edema( hydrops fetalis) due to anemia
Severe hemolytic syndrome erythroblastosis fetalis
Neurologic damage(kernicterus)
Activity
After integrating the learning inputs, try to answer these situations accordingly to what you
have understood.
1. Angelina Gomez, the woman you met at the beginning of the chapter, has developed
congestive heart failure. She works at a job where she is on her feet almost all day. What
suggestions could you make to her to help her incorporate some rest periods into her day?
2. Angelina has also developed gestational diabetes. She’s resistant to learning about her
condition, though, because she knows her symptoms are only temporary and will fade at the
end of pregnancy. What type of teaching plan would you devise to help her learn in the face
of this attitude?
Wrap-up Activity
Based on the learning input, what is the most difficult pre-existing condition that has the
greatest impact on pregnancy? Why?
Post-Assessment
Your instructor thru MVLE will give a summative test on the lessons of the chapter. Please
wait for further instructions. Good luck!
References
Silbert-Flagg, J. A., & Pillitteri, A. (2018). Maternal & child health nursing: Care of the childbearing &
childrearing family.
14
Chapter 2: Care of At-Risk/High-Risk Sick Mother
You might also like
- Wade AssessmentDocument5 pagesWade Assessmentapi-58457466550% (2)
- Launtop ManualDocument48 pagesLauntop ManualMatZancNo ratings yet
- Biobase Elisa Microplate Reader BK-EL10C User Manual 202103Document48 pagesBiobase Elisa Microplate Reader BK-EL10C User Manual 202103Victor BlancoNo ratings yet
- Framework For Maternal and Child Health NursingDocument7 pagesFramework For Maternal and Child Health NursingJan Oliver Yares100% (1)
- Baxter Storey BrochureDocument30 pagesBaxter Storey Brochurediv_anNo ratings yet
- The Ultimate Healthy Grocery List PDFDocument1 pageThe Ultimate Healthy Grocery List PDFHazwan Ariff HakimiNo ratings yet
- Physiology PF PuerperiumDocument34 pagesPhysiology PF PuerperiumKholoud Kholoud100% (4)
- Maternal & Child NUrsing SylabusDocument7 pagesMaternal & Child NUrsing Sylabusmarsan12No ratings yet
- Care of Mother, Child, Family and Population Group At-Risk or With ProblemsDocument52 pagesCare of Mother, Child, Family and Population Group At-Risk or With ProblemsMelchor Felipe Salvosa100% (1)
- CHN NotesDocument7 pagesCHN NotesAnvi Turingan PedronanNo ratings yet
- Fundamentals of NursingDocument29 pagesFundamentals of NursingThierd Cañete IIINo ratings yet
- Module 1 NCM 107 NewDocument44 pagesModule 1 NCM 107 NewAmethystNo ratings yet
- Module 1 NCM 100Document10 pagesModule 1 NCM 100ApRil Anne BalanonNo ratings yet
- Nursing Care During Normal Pregnancy Care of Dev FetusDocument5 pagesNursing Care During Normal Pregnancy Care of Dev FetusLuna Sang-anNo ratings yet
- Foundation For Maternal and Child Health NursingDocument18 pagesFoundation For Maternal and Child Health NursingChari RivoNo ratings yet
- Nursing Care of A Family With A ToddlerDocument37 pagesNursing Care of A Family With A ToddlerKarly Alissa TarubalNo ratings yet
- Maternal & Child Nursing Care: Lecture NotesDocument42 pagesMaternal & Child Nursing Care: Lecture NotesMidori San100% (1)
- Models of Health IllnessDocument3 pagesModels of Health Illnessjerikacorpuzmiranda100% (1)
- Maternal and Child Health Nursing (NCM 101 Lect) Part 1Document4 pagesMaternal and Child Health Nursing (NCM 101 Lect) Part 1yunjung0518100% (7)
- Brokenshire College Socsksargen, Inc.: NCM 100-Theorerical Foundations in NursingDocument8 pagesBrokenshire College Socsksargen, Inc.: NCM 100-Theorerical Foundations in NursingKeren Happuch EspirituNo ratings yet
- NCM 101 (Continuation) Postpartal Period and PediatricsDocument29 pagesNCM 101 (Continuation) Postpartal Period and PediatricsAudi Kyle SaydovenNo ratings yet
- Maternal and Child Nursing 1 Skills Lab Modele s1Document3 pagesMaternal and Child Nursing 1 Skills Lab Modele s1Crystal MaidenNo ratings yet
- Notes - MCHN - Chapter 1Document12 pagesNotes - MCHN - Chapter 1Jamaica mitalNo ratings yet
- 1.1. Concept of ManDocument27 pages1.1. Concept of ManTrisha SabaNo ratings yet
- Gravidity and ParityDocument11 pagesGravidity and ParityShahad HakimuddinNo ratings yet
- Module 3 Responsibilities of A Beginning Nurse ResearcherDocument9 pagesModule 3 Responsibilities of A Beginning Nurse ResearcherCaitlynNo ratings yet
- A. Goals and Philosophies of Maternal and Child Health Nursing The 2020 National Health GoalsDocument3 pagesA. Goals and Philosophies of Maternal and Child Health Nursing The 2020 National Health GoalsJoymae Olivares TamayoNo ratings yet
- Syllabus NCM 109 Care of Mother Child Adolescent at Risk or With ProblemDocument37 pagesSyllabus NCM 109 Care of Mother Child Adolescent at Risk or With Problembrilliant dumay100% (1)
- Nutri Lab 10Document38 pagesNutri Lab 10Carl Josef C. GarciaNo ratings yet
- Community Health NursingDocument23 pagesCommunity Health NursingMimi Vee100% (1)
- Ethico Legal Dilemmas in Critical Care NursingDocument36 pagesEthico Legal Dilemmas in Critical Care NursingNica Marie LumbaNo ratings yet
- Problems Associated With Chronic IllnessDocument8 pagesProblems Associated With Chronic IllnessMeryville JacildoNo ratings yet
- Finals TFN ReviewerDocument5 pagesFinals TFN ReviewerNicole Faith L. NacarioNo ratings yet
- MCHN Reviewer 1Document24 pagesMCHN Reviewer 1Steam LcNo ratings yet
- Ctu CCMC Level 3 NCM 1Document15 pagesCtu CCMC Level 3 NCM 1Divina VillarinNo ratings yet
- Prenatal Management (Part 5)Document36 pagesPrenatal Management (Part 5)Austine James Sabenicio PantiloNo ratings yet
- Professional Adjustment Final 2Document41 pagesProfessional Adjustment Final 2lielani_martinezNo ratings yet
- Funda Lec ReviewerDocument16 pagesFunda Lec ReviewerTricia Maxine DomingoNo ratings yet
- Advance Practice in Maternal and Child Nursing 1 High Risk Pregnancy: Nursing Care of A Family Experiencing A Pregnancy Complication From A Pre-Existing or Newly Acquired IllnessDocument31 pagesAdvance Practice in Maternal and Child Nursing 1 High Risk Pregnancy: Nursing Care of A Family Experiencing A Pregnancy Complication From A Pre-Existing or Newly Acquired Illnessallanrnmanaloto100% (2)
- Nursing Care of The Older Adult in Chronic IllnessDocument19 pagesNursing Care of The Older Adult in Chronic IllnessWen SilverNo ratings yet
- NCM 103 Syllabus ObeDocument20 pagesNCM 103 Syllabus Obeۦۦ JamesNo ratings yet
- HeheezjghDocument7 pagesHeheezjghDemiar Madlansacay QuintoNo ratings yet
- Transcultural Nursing TheoryDocument44 pagesTranscultural Nursing TheoryShweta KateNo ratings yet
- Care of The Mother and The Fetus During The Prenatal Period (Part 2)Document20 pagesCare of The Mother and The Fetus During The Prenatal Period (Part 2)Austine James Sabenicio PantiloNo ratings yet
- Maternal NewDocument30 pagesMaternal NewKhristine Rose Sanchez CaloNo ratings yet
- Concept of Man Health IllnessDocument12 pagesConcept of Man Health IllnessFrances Nicole FloresNo ratings yet
- Unit 1 - Week (1) - Comprehensive Assessment: Intended Learning Outcomes (Week 1-ILO)Document28 pagesUnit 1 - Week (1) - Comprehensive Assessment: Intended Learning Outcomes (Week 1-ILO)John Van Dave TaturoNo ratings yet
- NCM114 - Learn Mat 1 2021Document32 pagesNCM114 - Learn Mat 1 2021jjNo ratings yet
- Rle 217... Typology of Nursing Problems in Family Nursing Practice MaglayaDocument6 pagesRle 217... Typology of Nursing Problems in Family Nursing Practice MaglayaMakspeyn del Valle - MoonNo ratings yet
- NCM 112-Mod2Document9 pagesNCM 112-Mod2Samantha BolanteNo ratings yet
- Intro To Psychiatric Mental HealthDocument75 pagesIntro To Psychiatric Mental HealthEryl Franz HerreraNo ratings yet
- Care of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManDocument26 pagesCare of Mother, Child, and Adolescent: Prepared by Donna Belle Sumugat RN ManLaurence Docog100% (1)
- NCMB314 Prelim ReadingsDocument77 pagesNCMB314 Prelim ReadingsNine SoleilNo ratings yet
- Course Outline-Ncm109Document10 pagesCourse Outline-Ncm109Charmagne Yanga EpantoNo ratings yet
- Pre Gestational GestationalDocument19 pagesPre Gestational GestationalRoger Jr PumarenNo ratings yet
- The Nursing Role in Genetic Assessment and Counseling The Nursing Role in Genetic Assessment and CounselingDocument35 pagesThe Nursing Role in Genetic Assessment and Counseling The Nursing Role in Genetic Assessment and CounselingBridget Shienne DaculaNo ratings yet
- Competency Appraisal 2 SyllabusDocument10 pagesCompetency Appraisal 2 SyllabusMary Janet Pinili100% (2)
- Maternal and Child HealthDocument7 pagesMaternal and Child HealthNessa Layos MorilloNo ratings yet
- NCM 119 - Rle (Prelim) Week 1: Immune Response Immunity: Natural and Acquired Immunity - Ma'am VAB Immune ResponseDocument13 pagesNCM 119 - Rle (Prelim) Week 1: Immune Response Immunity: Natural and Acquired Immunity - Ma'am VAB Immune ResponseJamaica Leslie Noveno100% (1)
- 1 Gerontology Nursing Concepts: Gloria P. de Leon, RN, RM, ManDocument211 pages1 Gerontology Nursing Concepts: Gloria P. de Leon, RN, RM, ManJohanine VillasantiagoNo ratings yet
- Concepts & Patterns of Human Behavior Mal Adap LecDocument4 pagesConcepts & Patterns of Human Behavior Mal Adap LecAshtua MandixNo ratings yet
- Eteeap - NCM 106 Page 1Document5 pagesEteeap - NCM 106 Page 1Marisol Jane JomayaNo ratings yet
- NCM103 (FUNDA) Module 1 CommunicationDocument6 pagesNCM103 (FUNDA) Module 1 CommunicationJohn Joseph Cruz100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- NCM09 Ob Lec ReviewerDocument36 pagesNCM09 Ob Lec ReviewerChelsea Keith Sollano BalasabasNo ratings yet
- Bfe2218 Lazourdy 500gpm@6bar PDFDocument117 pagesBfe2218 Lazourdy 500gpm@6bar PDFYazan Tamimi50% (2)
- RESA Tax 1410 Preweek 165Document21 pagesRESA Tax 1410 Preweek 165Fordan AntolinoNo ratings yet
- The New Cairo Mall: DWG-MF0202.03 DWG - MF0202.04Document1 pageThe New Cairo Mall: DWG-MF0202.03 DWG - MF0202.04Mahmud MaherNo ratings yet
- Oil Filled CTs (72!5!420 KV)Document65 pagesOil Filled CTs (72!5!420 KV)kunalan_79860100% (1)
- Hemp Herbicide Poster PDFDocument1 pageHemp Herbicide Poster PDFPintrijel LaurNo ratings yet
- Force and Pressure MCQDocument6 pagesForce and Pressure MCQnitikaNo ratings yet
- Test Bank Linux For Programmers and Users SolutionDocument4 pagesTest Bank Linux For Programmers and Users SolutionRichard1LauritsenNo ratings yet
- Issues N Chalenges in Health ManagementDocument133 pagesIssues N Chalenges in Health ManagementRachana Karki100% (1)
- Quiz Lu1 Y3 A PDFDocument3 pagesQuiz Lu1 Y3 A PDFWilfharry billyNo ratings yet
- Akhtamov A.A. - Reading Comprehension TestsDocument48 pagesAkhtamov A.A. - Reading Comprehension TestsKhalid TsouliNo ratings yet
- Unit 2 EVSDocument10 pagesUnit 2 EVSVenkatesh KumarNo ratings yet
- Goodhormonehealth News Jan16 PDFDocument10 pagesGoodhormonehealth News Jan16 PDFBrian CoxNo ratings yet
- Pre-Setting Manual Balancing Valves CIM 788: Technical InformationDocument7 pagesPre-Setting Manual Balancing Valves CIM 788: Technical InformationblindjaxxNo ratings yet
- Dowlex Lldpe 2645GDocument3 pagesDowlex Lldpe 2645GSalustraNo ratings yet
- Disability Report V03 SinglePagesDocument44 pagesDisability Report V03 SinglePagesAmerlia AdzianNo ratings yet
- Elephant MindDocument4 pagesElephant MindHardev SinghNo ratings yet
- Gas Exchange Mind MapDocument1 pageGas Exchange Mind MapWilliam karuniawan SentosaNo ratings yet
- Jayson Desear: 3. What Is The Importance of Legislation in The Development and Sustenance of Special Education Programs?Document2 pagesJayson Desear: 3. What Is The Importance of Legislation in The Development and Sustenance of Special Education Programs?Jayson Desear100% (3)
- July 12, 2019 Strathmore TimesDocument20 pagesJuly 12, 2019 Strathmore TimesStrathmore TimesNo ratings yet
- Ebp PosterDocument1 pageEbp Posterapi-340595961No ratings yet
- Your Habit Body A Better Model of The Unconscious For EveryoneDocument24 pagesYour Habit Body A Better Model of The Unconscious For EveryoneBubi Sutomo100% (1)
- Refex 134a SpecDocument15 pagesRefex 134a SpecSami ThirunavukkarasuNo ratings yet
- Quran MessageDocument1 pageQuran Messagekamallove7481No ratings yet
- Saudi Aramco Inspection ChecklistDocument22 pagesSaudi Aramco Inspection Checklistabdulgafoor54100% (2)