Professional Documents
Culture Documents
Pocket-Card HEENT-Assessment January2024
Pocket-Card HEENT-Assessment January2024
Uploaded by
adnan MukhtarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pocket-Card HEENT-Assessment January2024
Pocket-Card HEENT-Assessment January2024
Uploaded by
adnan MukhtarCopyright:
Available Formats
January 2024
www.nursingcenter.com
Head, Eyes, Ears, Nose, Throat (HEENT) Assessment
Introduction
Most physical assessments begin at the top with the head, eyes, ears, nose, and throat (HEENT)
assessment. The patient is typically positioned sitting upright, allowing the examiner to systemically
work down through each body system. Many of these elements are included in the cranial nerve
assessment.
Assessing the Head
• Inspect the head and face for symmetry.
• Inspect the hair for color, distribution, and texture.
• Palpate the scalp and skull for tenderness and inspect for flaking, lesions, deformities, or
tenderness.
Assessing the Eyes
• Note position and alignment of the eyes and presence of discharge, irritation, and redness.
• Observe the eyelids.
o Check for drooping of the upper eyelids (ptosis).
o Check strength of upper eyelids by having patient squeeze their eyes shut. You should
not be able to open the patient’s eyelids (cranial nerve VII).
• Inspect sclera and conjunctiva of each eye; sclerae should be white and clear.
• Inspect each cornea, iris, and lens, checking for transparency.
• Compare the pupils and test each reaction to light.
o Pupils are normally round and vary in size.
o Use the mnemonic PERRLA (Pupils Equal, Round and Reactive to Light and
Accommodation) to test pupil reflexes.
§ Test for reactivity to light.
• Darken the room and shine a flashlight on each pupil. Normally, pupils
constrict with light and dilate in the dark.
§ Test for accommodation (ability of the lens to adjust to objects at varying
distances).
• When moving an object close to the eye, the pupil will constrict; when
moving an object away from the eye, the pupil will dilate.
• Assess extraocular movements for abnormalities.
o Assess the 6 cardinal positions of the gaze: right, right up, right down, left, left up, left
down.
o Check for conjugate gaze (ability of the eyes to move in the same direction at the same
time). Eyes normally move in unison, except when converging on an object that is
moving closer.
o Check for nystagmus, a condition in which the eyes move rapidly and uncontrollably side
to side (horizontal nystagmus), up and down (vertical nystagmus), or in a circle (rotary
nystagmus). This may be seen on lateral movement due to eye fatigue; watch for
vertical nystagmus or prolonged nystagmus.
• Screen visual fields in both eyes: medially/laterally, superiorly/inferiorly (cranial nerve II).
• Perform a visual acuity test with the Snellen Chart (cranial nerve II)
January 2024
www.nursingcenter.com
• For fundoscopic examination, use an ophthalmoscope to inspect the ocular fundi.
o Check transparency of the anterior and posterior chambers.
o Observe the red reflex of the retina; it can be observed by the clinician 1 foot from the
eye in a dimly lit room.
Assessing the Ears
• Examine each ear using an otoscope. Gently pull the pinna of the ear up and back to straighten
the external canal.
o Inspect the auricle, canal, and ear drum for color, symmetry, elasticity, tenderness, or
lesions.
o Inspect the external ear canal for color, drainage, cerumen (ear wax) buildup, canal
edema, erythema, or masses.
o Assess the tympanic membrane for color, shape, transparency, integrity, bulging, and
scarring.
• Test auditory acuity in each ear with the whisper test (cranial nerve VIII).
o Stand about 2 feet behind the seated patient.
o Occlude the non-test ear with a finger.
o Whisper a combination of three words of numbers and letters and ask the patient to
repeat them back to you.
o If acuity is decreased, perform the Weber and Rinne tests (cranial nerve VIII).
Assessing the Nose and Sinuses
• Inspect the external nose for color, size, shape, symmetry, and presence of drainage,
tenderness, and masses.
• Using a light and nasal speculum or otoscope, inspect the nasal passages for patency, nasal
mucosa for color, nasal septum for deviation, and turbinates for color and swelling.
• Check the patency of each nare by asking the patient to occlude one nare and breathe through
the other.
• Assess the patient’s sense of smell (cranial nerve I) with an orange or lemon peel, coffee,
vinegar, or essence bottles of vanilla or peppermint.
• Palpate the frontal and maxillary sinuses for tenderness and assess for signs of infection.
Assessing the Throat (Mouth and Pharynx)
• Inspect:
o Lips for color, moisture, masses, cracks, sores, fissures, and symmetry.
o Oral mucosa for color, lesions, dryness/moisture, masses, and swelling.
o Tongue for color, thickness, moisture, symmetry of movement left and right, and
deviations from midline (cranial nerve XII). Palpate the tongue and floor of the mouth
for masses and swelling.
o Teeth for their general condition and evaluate if any are missing.
o Gums for color, texture, swelling, retraction, and bleeding.
o Uvula for movement, position, size, symmetry, and color.
o Pharynx (hard and soft palate) for color, redness, inflammation, exudate, masses, and
lesions.
o Tonsils for size, color, inflammation, and exudate.
o Salivary glands (parotid, sublingual, and submaxillary) for patency and signs of
inflammation or redness.
January 2024
www.nursingcenter.com
• Check the patient’s ability to swallow and their gag reflex (cranial nerves IX and X).
o The thyroid is typically not visible. Assess for an enlarged thyroid gland at the
suprasternal notch.
Assessing the Neck
• Check neck muscles for symmetry, masses, swelling, and range of motion.
• Palpate cervical lymph nodes for signs of swelling or tenderness; cervical lymph nodes should
not be fixed (unmovable) or palpable (unless the patient is very thin). Lymph nodes should be
small and freely moving.
• Assess head and neck range of motion.
• Check trapezius muscle strength. Ask the patient to shrug their shoulders against your hands as
you apply resistance (cranial nerve XI).
• Check cervical muscle strength. Ask the patient to turn their chin/jaw against your hand.
• Assess trachea for deviation; it should be midline.
• Evaluate thyroid gland noting enlargement or presence of nodules and masses; it should be
smooth.
• Examine the carotid arteries as part of the cardiac assessment, taking care to palpate the carotid
arteries one at a time, noting symmetry, strength, amplitude, and presence of an abnormal
thrill. Listen for bruits using the diaphragm of your stethoscope.
• Assess for cervical point tenderness along the posterior aspect of the neck.
PEARLS
• Compare any new findings with the patient’s past medical history.
• The elements of the HEENT assessment can be interwoven with the cranial nerve assessment.
• Ptosis may be congenital or caused by a disorder affecting the muscle tendon, muscle, or nerve
of the eyelid. Unilateral ptosis with impaired extraocular movement suggests a compressive
third cranial nerve palsy.
• A yellowish discoloration of the sclera indicates jaundice.
• Pain with movement of the auricle and tragus of the ear occurs in acute otitis externa
(inflammation of the ear canal), but not in otitis media (inflammation of the middle ear).
• In viral rhinitis, the nasal mucosa is often red and swollen; in allergic rhinitis, it may be pale,
bluish, or red.
• Tracheal deviation could be a serious sign of tension pneumothorax, pleural effusion, tumor, or
goiter.
References
Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bate’s Guide to Physical Examination and History Taking
(13th ed.). Wolters Kluwer Health: Philadelphia.
Hinkle, J. (2021). Brunner & Suddarth’s Textbook of Medical-Surgical Nursing (15th ed.). Wolters Kluwer
Health. https://wolterskluwer.vitalsource.com/books/9781975161057
Mankowski, N.L. & Raggio, B.S. (2022, January 24). Otoscope exam. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK553163/
You might also like
- Head To Toe Assessment Normal FindingsDocument13 pagesHead To Toe Assessment Normal FindingsDanica May Corpuz Comia-Enriquez100% (3)
- World Lit Presentation Daydream of A Drunk WomanDocument4 pagesWorld Lit Presentation Daydream of A Drunk WomanAgnes Sugut100% (1)
- Baby One More Time Chords by Blink-182 @Document4 pagesBaby One More Time Chords by Blink-182 @Eva Magdalena PardedeNo ratings yet
- Head Neck Assesment and Technique of Physical AssesmentDocument4 pagesHead Neck Assesment and Technique of Physical AssesmentFitriani PratiwiNo ratings yet
- EO/IO Exam CriteriaDocument3 pagesEO/IO Exam CriteriaTaylor100% (1)
- Physical AssessmentDocument5 pagesPhysical AssessmentIsabel DizonNo ratings yet
- Physical Head-To-Toe AssessmentDocument138 pagesPhysical Head-To-Toe AssessmentCRISELLE KHATE TABAGO PAGATPATANNo ratings yet
- Head (Skull, Scalp, Hair) : Head-To-Toe Assessment (C. Eyebrows, Eyes and Eyelashes)Document15 pagesHead (Skull, Scalp, Hair) : Head-To-Toe Assessment (C. Eyebrows, Eyes and Eyelashes)anne002No ratings yet
- WEEK 3 - Head and NeckDocument22 pagesWEEK 3 - Head and NeckHashley CastellyNo ratings yet
- 3 - HEENT Physical ExminationDocument56 pages3 - HEENT Physical ExminationXtylish Bacha 8bpNo ratings yet
- Cranial NervesDocument9 pagesCranial NervesRabin TacderNo ratings yet
- Head To Toe AssessmentDocument22 pagesHead To Toe AssessmentNessa Layos MorilloNo ratings yet
- Head To Toe Assessment ToolDocument19 pagesHead To Toe Assessment ToolJeah Mae CastroNo ratings yet
- Head To Toe Physical AssessmentDocument27 pagesHead To Toe Physical AssessmentLarmay dcsnNo ratings yet
- Cranial Nerves ExaminationDocument25 pagesCranial Nerves Examinationnaveenarageson4No ratings yet
- Conduct of Physical Examination: I. General SurveyDocument10 pagesConduct of Physical Examination: I. General SurveyWeng RamojalNo ratings yet
- Scalp: Normal Findings: SkullDocument13 pagesScalp: Normal Findings: SkullfranlynNo ratings yet
- Physical Assessment (Normal Findings)Document31 pagesPhysical Assessment (Normal Findings)Rinki SinghNo ratings yet
- Head To Toe Physical AssessmentDocument9 pagesHead To Toe Physical Assessmentthe studentNo ratings yet
- Conduct of Physical Examination RemindersDocument23 pagesConduct of Physical Examination RemindersJazer DairoNo ratings yet
- Physical Examination of Heent & LgsDocument34 pagesPhysical Examination of Heent & Lgstsehay asratNo ratings yet
- Head Face Neck Eyes Ears ThroatDocument9 pagesHead Face Neck Eyes Ears ThroatDale Ros CollamatNo ratings yet
- Oral Surgery Lec 5&6Document14 pagesOral Surgery Lec 5&6Mohammad RaadNo ratings yet
- Performance Evaluation Checklist PaDocument4 pagesPerformance Evaluation Checklist PaRitchie Mae Espinosa DumapitNo ratings yet
- Checklist Head To Toe AssessDocument6 pagesChecklist Head To Toe AssessMira senalNo ratings yet
- Physical AssessmentDocument6 pagesPhysical AssessmentDonna Flor NabuaNo ratings yet
- Head and NeckkkkkkDocument7 pagesHead and NeckkkkkkJoey A. RumbaoaNo ratings yet
- PX NN CranialDocument35 pagesPX NN CranialZenithaMeidaNo ratings yet
- Focused AssessmentDocument5 pagesFocused AssessmentPiyali SahaNo ratings yet
- EARSEYESDocument93 pagesEARSEYESZen Gesner Kenneth G. EganaNo ratings yet
- Physical Assessment Mid-Term Evaluation Fall23Document6 pagesPhysical Assessment Mid-Term Evaluation Fall23Anna DrakeNo ratings yet
- Cranial Nerves: Remembering The Order and Function of The Cranial NervesDocument4 pagesCranial Nerves: Remembering The Order and Function of The Cranial NervesNatalia OrtizNo ratings yet
- Examination of The Head and Neck Is A Fundamental Part of The Standard Physical ExaminationDocument5 pagesExamination of The Head and Neck Is A Fundamental Part of The Standard Physical ExaminationDavidNo ratings yet
- PictureDocument11 pagesPictureLaiba FatimaNo ratings yet
- Head To Toe AssessmentDocument21 pagesHead To Toe AssessmentZahra jane A.100% (1)
- Cranialnerve 180324181201 PDFDocument44 pagesCranialnerve 180324181201 PDFArwah FerozeNo ratings yet
- Head and Neck Assessment: ChecklistDocument2 pagesHead and Neck Assessment: ChecklistLucky Dela cruz100% (1)
- Head and Neck Assessment NursingDocument10 pagesHead and Neck Assessment Nursingflorian layuganNo ratings yet
- Physical Assessment Script FinalDocument9 pagesPhysical Assessment Script FinalArabiah AbdullahNo ratings yet
- Box 10Document2 pagesBox 10stx863No ratings yet
- IPPA Physical AssxDocument4 pagesIPPA Physical Assxkimglaidyl bontuyanNo ratings yet
- Peads AssessmentDocument63 pagesPeads AssessmentSrinivas MohanNo ratings yet
- Physical Examination: Presented To Mrs. Nisha Mane Assistant Professor D.Y.P.S.O.NDocument41 pagesPhysical Examination: Presented To Mrs. Nisha Mane Assistant Professor D.Y.P.S.O.NNilakshi Barik MandalNo ratings yet
- Assessing Cranial Nerve FunctionDocument1 pageAssessing Cranial Nerve FunctionSITTIE JOBAISAH TOMINAMAN ALINo ratings yet
- Ears, Mouth, Throat Nose, and Sinuses AssessmentDocument8 pagesEars, Mouth, Throat Nose, and Sinuses Assessmentshannon c. lewisNo ratings yet
- Health Assessment Lesson 1Document44 pagesHealth Assessment Lesson 1Bernice EbbiNo ratings yet
- SodaPDF Merged Merging Result 1Document203 pagesSodaPDF Merged Merging Result 1nonelNo ratings yet
- Neurological AssessmentDocument76 pagesNeurological Assessmentjcabatit3No ratings yet
- FINAL Genral Ward ADULT PHYSICAL ASSESSMENT CompressedDocument59 pagesFINAL Genral Ward ADULT PHYSICAL ASSESSMENT CompressedDustin AgsaludNo ratings yet
- Head and Neck 3Document51 pagesHead and Neck 3Diran TerzyanNo ratings yet
- Lymphadenopathy: Examination ProcedureDocument9 pagesLymphadenopathy: Examination ProcedureBeenish IqbalNo ratings yet
- Advanced Assessments Final ExamDocument57 pagesAdvanced Assessments Final ExamBreanna BeckfordNo ratings yet
- Head-To-Toe Assessment A. Head (Skull, Scalp, Hair)Document35 pagesHead-To-Toe Assessment A. Head (Skull, Scalp, Hair)Kris_Hilyn_9815No ratings yet
- Session 4 Skills.......Document18 pagesSession 4 Skills.......Harry ChauhanNo ratings yet
- Ent History Taking and Examination-1Document16 pagesEnt History Taking and Examination-1Jyotirmayee100% (6)
- Head and Neck Assessment NursingDocument8 pagesHead and Neck Assessment NursingNicks NacarioNo ratings yet
- Head and Neck Assessment NursingDocument8 pagesHead and Neck Assessment NursingNicks NacarioNo ratings yet
- Cranial-Nerve-Examination Copy Copy-1Document27 pagesCranial-Nerve-Examination Copy Copy-1cvmqx7yppdNo ratings yet
- Pemeriksaan Fisik Kepala Dan LeherDocument39 pagesPemeriksaan Fisik Kepala Dan LeherdokteraanNo ratings yet
- Physical AsessmentDocument15 pagesPhysical AsessmentnonelNo ratings yet
- Neck Assessment - WPS OfficeDocument20 pagesNeck Assessment - WPS OfficeTricia Denise EstabilloNo ratings yet
- Complete Thesis... VarquezDocument59 pagesComplete Thesis... VarquezrodielimNo ratings yet
- Job Description For Hse AdvisorDocument2 pagesJob Description For Hse AdvisorSam JoseNo ratings yet
- How Does Marijuana Affect The BrainDocument3 pagesHow Does Marijuana Affect The BrainWanNurAtikahNo ratings yet
- Chanchreek Ameta QADocument4 pagesChanchreek Ameta QAQa TutorNo ratings yet
- HEMOPHILIA CausesDocument4 pagesHEMOPHILIA CausesJhoanelle MalgapoNo ratings yet
- Eng 316 Resume and Cover Letter 2019Document1 pageEng 316 Resume and Cover Letter 2019api-476963060No ratings yet
- Multiple Access Techniques in Wireless Communication PPT AyazDocument28 pagesMultiple Access Techniques in Wireless Communication PPT AyazAyaz Ahmad100% (1)
- Manila Int Climate PDFDocument3 pagesManila Int Climate PDFLevy SorianoNo ratings yet
- Quick Reference Guide: An Assertiveness FormulaDocument2 pagesQuick Reference Guide: An Assertiveness FormulaAhmadNo ratings yet
- ADE 420 Spring 2015 Assignment #1 GuidelinesDocument2 pagesADE 420 Spring 2015 Assignment #1 Guidelinesapi-20975547No ratings yet
- Sme Loan From SabincoDocument12 pagesSme Loan From Sabincotipu1sultan_1No ratings yet
- Anna GorskaDocument10 pagesAnna GorskaRey-ann Kyle L. ManansalaNo ratings yet
- Movie Worksheet TED - Reporting Crisis Via TextingDocument1 pageMovie Worksheet TED - Reporting Crisis Via TextingAdam SzymaszekNo ratings yet
- Financial Results For The Year 2019 20Document35 pagesFinancial Results For The Year 2019 20Akshaya SwaminathanNo ratings yet
- Liste Jeux PS Vita Boites PALDocument1 pageListe Jeux PS Vita Boites PALDenis Alibor MajhenNo ratings yet
- 2 - Cebu Institute of Technology vs. OpleDocument1 page2 - Cebu Institute of Technology vs. OpleChristine JungoyNo ratings yet
- Thesis (Live in Relationship)Document20 pagesThesis (Live in Relationship)Shaynie Tañajura DuhaylungsodNo ratings yet
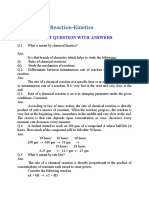
- Chapter 11 .Reaction-Kinetics: Short Question With AnswersDocument6 pagesChapter 11 .Reaction-Kinetics: Short Question With AnswersAasim AliNo ratings yet
- The Marketing of BarbieDocument8 pagesThe Marketing of BarbieКристина БеляеваNo ratings yet
- DBT in ASDDocument9 pagesDBT in ASDCarregan AlvarezNo ratings yet
- Social StructureDocument11 pagesSocial StructureabbiecdefgNo ratings yet
- Silahis Marketing Corp. v. IAC (1989)Document2 pagesSilahis Marketing Corp. v. IAC (1989)Fides DamascoNo ratings yet
- Ucla PGP Pro BrochureDocument28 pagesUcla PGP Pro BrochureTarapada MishraNo ratings yet
- Hydro Resources Contractors Corp. v. Pagaliluan G.R. No. 62909. April 18, 1989Document28 pagesHydro Resources Contractors Corp. v. Pagaliluan G.R. No. 62909. April 18, 1989Acel RamirezNo ratings yet
- The Trolley ProblemDocument2 pagesThe Trolley ProblemAngelina SuterNo ratings yet
- Module 1 LO3a & LO3b Prepare Basic Instructional MaterialsDocument15 pagesModule 1 LO3a & LO3b Prepare Basic Instructional Materialsjonellambayan100% (1)
- PLD 1990 SC 28Document8 pagesPLD 1990 SC 28Ali HussainNo ratings yet
- LAW - ON - SALES CH 4 Sec 3Document4 pagesLAW - ON - SALES CH 4 Sec 3MaricrisNo ratings yet