Professional Documents
Culture Documents
Walter 2020
Walter 2020
Uploaded by
Sonia shitoleCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Walter 2020
Walter 2020
Uploaded by
Sonia shitoleCopyright:
Available Formats
Original Contributions
Clinical Dentistry
Utility of measuring anterior-posterior spread
to determine distal cantilever length off a
fixed implant-supported full-arch prosthesis
A review of the literature
Leora Walter, DDS; Gary Greenstein, DDS, MS
ABSTRACT
Background. Historically, anterior-posterior (AP) spread assessments were often used to determine
the length that a distal cantilever could be extended off an implant-supported fixed full-arch
prosthesis.
Types of Studies Reviewed. The authors searched the literature for articles that used AP spread
to calculate cantilever size to be constructed off implants bearing a fixed implant-supported full-arch
rehabilitation.
Results. The data indicate that the relationship between AP spread and cantilever length is not
linear and many influences (such as beam theory, cantilever size differences in the mandible versus
maxilla, number and distribution of placed implants, prosthetic materials, and framework design)
need to be considered when computing cantilever length with respect to fixed implant-supported
prostheses.
Practical Implications. Recommendations using AP spread assessments to compute cantilever
lengths have not been validated by means of prospective scientific evaluations. Therefore, AP
spread evaluation is just one of many issues that need to be considered when determining distal
cantilever length associated with a fixed full-arch implant-bearing prosthesis.
Key Words. Anterior-posterior spread; AP spread; cantilever; dental implants; prostheses.
JADA 2020:151(10):790-795
https://doi.org/10.1016/j.adaj.2020.06.016
A
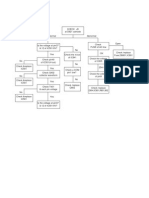
nterior-posterior (AP) spread measurements are often used to determine distal cantilever
length that extends from an implant-supported fixed full-arch restoration.1-4 The concept of
using AP spread to calculate cantilever size was first proposed by English1 in 1990. He stated
that biomechanical principles need to be applied to ensure a successful restorative outcome when a
cantilever is supported by means of a full-arch fixed implant-bearing prosthesis. AP spread was defined as
the distance between a line connecting the distal of the most distal implants of a full-arch implant-
supported prosthesis and a line through the center of the most anterior implant (Figure). English1
suggested that a cantilever’s span could be 1.5 times the AP spread in the mandible. This was his
opinion, and it did not evolve from a vigorous scientific assessment. Other clinicians also failed to
provide systematic prospective evaluations to validate that AP spread measurements could be used to
compute distal cantilever lengths.2-5 Questions arise as to what evidence there is that AP spread can be
used to determine cantilever size and what other factors need to be considered to calculate cantilever
length off implants that uphold a full-arch implant-supported prostheses. This is an important issue
because failure to adequately plan cantilever length and provide sufficient support for this type of
construct can result in stress on a prosthesis, which can cause screw loosening, screw breakage, prosthesis
fracture, implant fracture, and implant de-osseointegration.5-10 Therefore, it was deemed important to
Copyright ª 2020
critically appraise the relationship between AP spread and other factors (such as differences in cantilever
American Dental
Association. All rights size in the mandible versus maxilla, number and distribution of placed implants, prosthetic materials, and
reserved. framework design) that affect the cantilever length off an implant-supported fixed full-arch prostheses.
790 JADA 151(10) n http://jada.ada.org n October 2020
Figure. Anterior-posterior (AP) spread, as defined by English.1 The posterior line connects the distal-most portion of the
distal implants. The anterior line is placed in the center of the anterior-most implant and parallel to the posterior line. AP
spread is the distance between these 2 lines (blue arrow).
METHODS
Articles included in this critical analysis of the literature related to AP spread and biomechanics of
cantilevers were found by means of searching PubMed, Ovid, Embase, Dentistry and Oral Sciences
Source, and Cochrane using the following terms “AP spread,” “anteroposterior spread” with “fixed
prosthesis,” “cantilevers,” and “biomechanics of cantilevers.” Relevant articles were hand searched
to determine whether additional articles could be included in this analysis. All 11 human clinical
trials found in the literature related to AP spread were included in this literature analysis and
critiqued. Therefore, no exclusion criteria were used to negate the usefulness of studies; rather, each
study was addressed and critiqued directly.
DISCUSSION
AP spread to determine distal cantilever length
Numerous authors have suggested the following amounts of AP spread that could be used to
determine distal cantilever size off an implant-supported fixed full-arch prosthesis: less than 1,9 1.5,1
2,3 and 2.5.4 Misch and Misch-Dietsh4 suggested that a 2.5 AP spread was possible when force
influences (for example, parafunction or crown to root ratio) are low and the prosthesis is well
supported (that is, adequate number of implants). Others advised cantilever length could be a span
of 2 through 3 premolars,11 less than 15 mm,5,12 15 through 20 mm,2,13 and 20 mm.6 However,
these recommendations concerning cantilever length are grounded in clinical experience and
retrospective assessments with respect to decreased numbers of prosthetic complications and not
prospective scientific evaluations to determine a precise relationship between AP spread and
cantilever length.
Class 1 lever system related to AP spread
There are biomechanical concepts that relate AP spread and cantilever length to lever systems. A
dental cantilever is a type 1 lever; the pivot (fulcrum) is between the applied biting force and the
occlusal load on a prosthesis.2 The occlusal load is computed by means of multiplying the biting
force times cantilever length. The fulcrum is the connector at the terminal abutment. The canti-
lever arm (effort arm) generates torque on the prosthesis and bending moments can form in 3
clinical axes (occlusoapical, mesiodistal, faciolingual).7,14,15
Researchers from several studies indicated that bending moments induced by means of load-
bearing cantilevers can increase forces 2 through 3 times on the supporting implants compared
with stresses normally detected on a single implant.7,14,15 As the length of the effort arm increases,
tensile, compressive, and shear forces increase stress on the prosthesis. To counteract these vectors, a
large resistance arm is needed (distance from the fulcrum to most anterior implant).2 To clinically ABBREVIATION KEY
accomplish this, anterior implants of a fixed full-arch restoration should be placed as anteriorly as AP: Anterior-posterior.
JADA 151(10) n http://jada.ada.org n October 2020 791
possible, thereby creating a large AP spread. Ideally, to reduce stress on a cantilevered prosthesis, a
short effort arm (cantilever) and a long AP spread (resistance arm) are desired.2
Cantilever lengths associated with full-arch reconstructions: maxilla versus mandible
Researchers have differentiated between cantilever lengths in the maxilla versus the mandible. For
example, English1 suggested that a cantilever length of 1.5 times AP spread should be used in the
mandible, but it should be shorter in the maxilla owing to diminished bone loading capacity in the
maxilla. Rasmussen16 indicated that a 20-mm cantilever in the mandible is appropriate, and a 15-
mm length was proper in the maxilla. Naert and colleagues17 agreed that a maximum of 20-mm
cantilever in the mandible was reasonable, but only 10 mm should be used in the maxilla. Ran-
gert and colleagues2 were more cautious and recommended a 15- through 20-mm cantilever in the
mandible and 10-mm in the maxilla. These authors disagree on cantilever length in the maxillary
and mandibular arches, however, they concur that mandibular cantilevers can be longer than in the
maxilla due to increased strength of mandibular cortical bone. It has been recorded that the
mandibular bone is 1.8 times denser than maxillary bone.18 However, none of these articles sys-
tematically assessed the utility of using AP spread to reliably predict what cantilever length would
result in successful prostheses in the mandible and the maxilla. Furthermore, confounding variables,
such as jaw and tooth size, occlusal forces, and different materials used, preclude defining a precise
AP calculation that would apply to all patients.
Number of implants supporting a cantilevered prosthesis
When English1 described the relationship between cantilever length and AP spread for a
mandibular reconstruction, the prosthesis included 5 implants placed intraforaminally. The center
implant was inserted as anteriorly as possible, thereby creating a large AP spread (1.5). In contrast,
other clinicians believed that the number of implants is the critical determinant with respect to
computing cantilever length and not the AP spread of implants.2,7,13 In this regard, Taylor and
Bergman13 stated that when 4 implants are inserted, a mandibular cantilever should not exceed
15 mm, and if 5 or 6 implants are used, then the cantilever can extend 20 mm. However, these were
empirical suggestions. Additional evidence underscored that the number of implants was more
important than AP spread for determining cantilever length was provided by McAlarney and
Stavropoulos.7 They simulated clinical conditions and applied load at various points along the
prosthesis and mathematically concluded that there is no linear relationship between AP spread and
cantilever length and that cantilever length was dependent on the number and distribution of
implants between the most anterior and posterior implants.
Spacing of implants, cross-arch stabilization, and arch form
Using mathematical equations, Skalak19 found that correct distribution of implants reduces the load
per implant and facilitates constructing a larger cantilever. Others agreed that appropriate spreading
of implants accommodates stress placed on cantilevers.14,20 Successful use of the “All-on-4” concept
has shown that bilateral cantilevers can be supported with a limited number of well-distributed
implants.21
In addition to positioning implants, turning the corner of the arch with a prosthesis is important
with respect to countering dislodging and lateral forces associated with a cantilever, and it enhances
prosthesis stability.19,22 This is referred to as cross-arch stabilization. Grossman and colleagues23
stated “a rigid cross-arch fixed prosthesis will distribute loads to several implants more effectively
than a similar prosthesis without cross-arch stabilization.” In our opinion, this concept appears to be
reasonable; however, there are no research data that assessed whether cross-arch stabilization fa-
cilitates creating a larger cantilever.
Edentulous arches are ovoid, tapered, or square. Ovoid arches are the most common,
followed by square and then tapered.24 A tapered or ovoid arch form allows for a more favorable AP
spread of implants than a square arch.4 A square arch results in implants being placed in a straight line,
and it therefore has a shorter AP spread.25 Owing to its effect on AP spread, arch form is a factor that
should to be considered when planning the size of a distal cantilever off a full-arch prosthesis.
Bone loss due to cantilevered prostheses
The effect a cantilever has on bone resorption is debatable. Lindquist and colleagues26 reported
that anterior implants had more bone loss than posterior implants after 1 year when they
792 JADA 151(10) n http://jada.ada.org n October 2020
supported a cantilever as part of a mandibular implant-supported fixed full-arch prosthesis.
However, after 3 years, there was no difference between osseous resorption on anterior and
posterior implants. At 2 years, Ahlqvist and colleagues27 noted more bone loss in anterior than
posterior implants when supporting a cantilever in the mandible, but not in the maxilla of a
fixed full-arch restoration. In contrast, Naert and colleagues17 found no difference in the
amount of bone resorption among anterior and posterior implants associated with a canti-
levered prosthesis. Similarly, when the All-on-4 concept with bilateral cantilevers for full-arch
rehabilitation was used, no additional bone loss was noted compared with conventional
therapy.21,28 With respect to unilateral cantilevers, researchers from 2 5-year studies found no
additional bone loss when a short cantilever was present.29,30 These conflicting data preclude
making a determination as to whether there is a relationship between cantilever length and
bone loss adjacent to implants supporting a fixed full-arch restoration. Furthermore, no data
were found relating AP spread to bone loss.
Cantilever design related to beam theory
The flexibility of a cantilever can be computed using beam theory.31 A beam’s displacement
(movement) is dependent on the rigidity of the beam, which is a function of its length.31 Increasing
the length of a beam increases its flexibility and shortening the beam makes it more rigid. It can be
computed that if beam length is doubled or its thickness is cut in one-half, then the flexibility of the
beam (cantilever) is 8 times greater.8,32,33 These facts dictate that a cantilever should be limited in
size or be as small as possible because a beam will flex, resulting in increased stress on a prosthesis,
which can cause cantilever deformity and possible fracture of the luting media, porcelain, or
retaining screws.
To accommodate the flexibility of a cantilever, Worthington and colleagues34 and Sones35
recommended adequately bulking the material distal to the posterior abutment, as well as around
each cylinder. Contrastingly, Staab and Stewart36 reported that it was not the bulk of material but
the height of the connector that played a role in the success of a cantilever. Taylor and Bergman13
agreed that it was the height not the thickness of the connector that was important. To determine
the rigidity of a cantilever for occlusal loading, the following formula can be used: rigidity ¼
WH3/12.37 This relationship indicates that doubling the width (W) of the connector doubles its
strength, but doubling the height (H) increases its strength 8 times.37
There are situations in which the height of the framework is limited owing to anatomic con-
siderations. Accordingly, its cross-sectional design becomes important and needs to be adjusted to
allow for minimum height, while providing maximum resistance to flexion. Staab and Stewart36
studied the following 4 framework cross-sectional designs: L-, I-, and U-shaped and elliptical.
They reported that the I-beam was the most effective cross-sectional design to withstand occlusal
forces when there is minimum restorative height available. Others reached the same conclusion that
an I-beam design provides the most strength and rigidity and minimizes bulk and weight of a
framework.16,38,39
The above discussion indicates that there are numerous biomechanical factors that need to be
considered when determining cantilever length that could be extended off of a fixed full-arch
restoration. Cantilever length established solely on AP spread does not mathematically take into
account beam theory. Furthermore, calculations based on AP spread provide a wide-ranging general
estimate of possible cantilever lengths that can under- or overestimate the span of a cantilever that
could successfully be supported with an implant-supported fixed full-arch prosthesis.
Impact of materials used to construct prostheses
Vectors beyond biomaterial tolerances can cause technical problems (for example, screw loosening,
cantilever fracture, and damaged cemented bonds). In this regard, Drago9,40 conducted 2 studies
addressing materials used to construct cantilevers associated with implant-supported full-arch fixed
prostheses. Drago evaluated an interim prosthesis made from acrylic and a final prosthesis fabricated
from titanium. The prosthetic complication rate was greater with the interim acrylic prosthesis than
with the definitive metal prosthesis irrespective of AP spread.9,40 From another perspective,
Skalak19 stated that the distribution of load caused by means of a cantilever depends on the relative
stiffness of the material used to fabricate the restorative framework. The more rigid the prosthesis,
the more evenly distributed the forces, and therefore the cantilever is more resistant to deformation
JADA 151(10) n http://jada.ada.org n October 2020 793
and can be longer.16,41 Staab and Stewart36 agreed that survivability of a cantilevered prosthesis is
directly dependent on the fatigue life of the metal alloy framework. If a force exceeds two-thirds the
stress limit of a material (for example, metal), it fatigues and eventually fractures.31 Therefore, long
cantilevers should be avoided to reduce prosthetic complications. Additional evidence that the
material selected for a framework affects prosthesis survivability was provided by Zarb and Schmitt.6
After experiencing framework fractures, the constructs were remade, changing the silver palladium
alloy to one with higher yield and greater tensile strength. Subsequently, no additional framework
fractures occurred. They concluded that AP spread was not the determining factor for success of a
cantilevered prosthesis; rather, it was the rigidity of the framework material that was critically
important.
Other applications of AP spread assessments in the literature
This analysis discussed AP spread in relationship to the distal cantilever length off a fixed implant-
supported fixed full-arch prosthesis, it is apparent that many considerations for a fixed prosthesis can
apply to a removable prosthesis or unilateral cantilevered fixed implant prostheses. In this regard,
Kosinski42 suggested that cantilever length for removable implant retained overdentures can be
created distal to implants bilaterally by means of assessing the AP spread and multiplying it by 1.5.
Others mentioned the cantilever length could be 2.5 times the AP spread or 15 mm for over-
dentures.43 However, these numbers are based on literature addressing cantilever length associated
with fixed prostheses. These authors provided no scientific data using AP spread to determine
cantilever length for implant-bearing removable prostheses.
Pertaining to unilateral cantilevers off an implant-supported fixed prosthesis, Greenstein and
Cavallaro44 used the term AP spread when discussing a single cantilever off 2 implants. They
reviewed numerous clinical trials and surmised that unilateral cantilevers were predictable
prosthetic constructs. The data in the article supported the concept that unilateral fixed pros-
theses could be constructed with a short cantilever (z8 mm) with an interimplant distance of
approximately 8 mm (AP spread). These findings were related to Brunski’s45 calculations with
respect to managing compressive forces on the terminal abutment and tensile vectors on the
anterior abutment. However, once again, no specific clinical trials were conducted to relate the
length of the cantilever to AP spread and ultimately to the clinical success of unilateral canti-
levered prostheses.
CONCLUSIONS
Historically, it has been suggested that the length of the cantilever extension associated with a full-
arch implant-supported restoration could be determined using AP spread.1 However, this was an
empirical decision rather than one established on rigorous scientific research. There are no scien-
tifically derived data that permit calculating cantilever length based solely on AP spread. Therefore,
cantilever length should be determined on a case-by-case basis, taking into consideration the
following factors: biomechanics, AP spread, bone quality in the maxilla versus the mandible,
number and distribution of implants, rehabilitation design, and prosthesis material.
With respect to fabricating a cantilever off implants supporting a full-arch fixed prosthesis the
following steps are suggested:
n consider the occlusal load when determining the size, number, thread design, and surface area of
implants to be placed and place enough implants to distribute the occlusal forces;
n maximize implant distribution to reduce the load per implant;
n maximize the AP spread;
n use a cross-arch splint design when working with a full-arch design;
n use rigid material for the framework;
n use an I-beam in cross-section for the framework;
n minimize cantilever length, especially in the maxilla.
The prosthesis should be monitored at regular recall visits to evaluate changes in the integrity of
the framework and the occlusion, especially at the cantilevered segment. Implants and surrounding
bone should be checked to ensure their osseous support has been maintained. Any anomalies to
prosthesis, bone, or implants should be treated accordingly. n
794 JADA 151(10) n http://jada.ada.org n October 2020
Dr. Walter is the course director and a clinical attending, Prosthodontics, Dr. Greenstein is a clinical professor, Department of Periodontics, College
Woodhull Hospital, Brooklyn, NY; and a dentist in private practice, of Dental Medicine, Columbia University, New York, NY; and a dentist in
Prosthodontic and Implant Associates, Mamaroneck, NY. Address private practice, Surgical Implantology and Periodontics, Freehold, NJ.
correspondence to Dr. Walter, Prosthodontic and Implant Associates, 745 Disclosure. Drs. Walter and Greenstein did not report any disclosures.
East Boston Post Rd, Mamaroneck, NY 10543, e-mail leora.walter@gmail.com.
1. English CE. Critical A-P spread. Implant Soc. 1990; 16. Rasmussen EJ. Alternative prosthodontic technique 30. Hälg GA, Schmid J, Hämmerle CH. Bone level
1(1):2-3. for tissue-integrated prostheses. J Prosthet Dent. 1987; changes at implants supporting crowns or fixed partial
2. Rangert B, Jemt T, Jörneus L. Forces and moments 57(2):198-204. dentures with or without cantilevers. Clin Oral Implants
on Brånemark implants. Int J Oral Maxillofac Implants. 17. Naert I, Quirynen M, van Steenberghe D, Darius P. Res. 2008;19(10):983-990.
1989;4(3):241-247. A study of 589 consecutive implants supporting complete 31. Lundgren D, Laurell L. Biomechanical aspects of
3. Takayama H. Biomechanical considerations in fixed prostheses, part II: prosthetic aspects. J Prosthet Dent. fixed bridgework supported by natural teeth and endo-
osseointegrated implants. In: Hobo S, Ichida E, Garcia L, 1992;68(6):949-956. sseous implants. Periodontology 2000. 1994;4:23-40.
eds. Osseiointegration and Occlusal Rehabilitation. Tokyo, 18. Kim YJ, Henkin J. Micro-computed tomography 32. Smyd ES. The mechanics of dental structures.
Japan: Quintessence Publishing; 1989:265-280. assessment of human alveolar bone: bone density and JADA. 1952;44(2):187-193.
4. Misch CE, Misch-Dietsh F. Preimplant prosthodon- three-dimensional micro-architecture. Clin Implant Dent 33. Rodriguez AM, Aquilino SA, Lund PS. Cantilever
tics. In: Misch CE, ed. Dental Implant Prosthetics. St. Louis, Relat Res. 2015;17(2):307-313. and implant biomechanics: a review of the literature, part
MO: Elsevier Mosby; 2005:168. 19. Skalak R. Biomechanical considerations in osseoin- 1. J Prosthodont. 1994;3(1):41-46.
5. Chapman RJ. Principles of occlusion for implant tegrated prostheses. J Prosthet Dent. 1983;49(6):843-848. 34. Worthington P, Bolender CL, Taylor TD. The
prostheses: guidelines for position, timing, and force of 20. Ogawa T, Dhaliwal S, Naert I, et al. Impact of Swedish system of osseointegrated implants: problems and
occlusal contacts. Quintessence Int. 1989;20(7): implant number, distribution and prosthesis material on complications encountered during a 4-year trial period. Int
473-480. loading on implants supporting fixed prostheses. J Oral J Oral Maxillofac Implants. 1987;2(2):77-84.
6. Zarb GA, Schmitt A. The longitudinal clinical Rehabil. 2010;37(7):525-531. 35. Sones AD. Complications with osseointegrated im-
effectiveness of osseointegrated dental implants: the Tor- 21. Taruna M, Chittaranjan B, Sudheer N, Tella S, plants. J Prosthet Dent. 1989;62(5):581-585.
onto study, part IIIdproblems and complications Abusaad M. Prosthodontic perspective to all-on-4® concept 36. Staab GH, Stewart RB. Theoretical assessment of
encountered. J Prosthet Dent. 1990;64(2):185-194. for dental implants. J Clin Diagn Res. 2014;8(10):ZE16-ZE19. cross sections for cantilevered implant-supported pros-
7. McAlarney ME, Stavropoulos DN. Determination of 22. Schweitzer JM, Schweitzer RD, Schweitzer J. Free- theses. J Prosthodont. 1994;3(1):23-30.
cantilever length-anterior-posterior spread ratio assuming end pontics used on fixed partial dentures. J Prosthet Dent. 37. English CE. Biomechanical concerns with fixed
failure criteria to be the compromise of the prosthesis 1968;20(2):120-138. partial dentures involving implants. Implant Dent. 1993;
retaining screw-prosthesis joint. Int J Oral Maxillofac Im- 23. Grossmann Y, Finger IM, Block MS. Indications for 2(4):221-242.
plants. 1996;11(3):331-339. splinting implant restorations. J Oral Maxillofac Surg. 2005; 38. von Gonten AS, Medina T Jr., Woolsey GD,
8. Adell R, Lekholm U, Rockler B, Brånemark PI. 63(11):1642-1652. Hill DR. Modifications in the design and fabrication of
A 15-year study of osseointegrated implants in the treat- 24. Celebi AA, Keklik H, Tan E, Ucar FI. Comparison mandibular osseointegrated fixed prostheses frameworks.
ment of the edentulous jaw. Int J Oral Surg. 1981;10(6): of arch forms between Turkish and North American. J Prosthodont. 1995;4(2):82-89.
387-416. Dental Press J Orthod. 2016;21(2):51-58. 39. Cox J, Zarb G. Alternative prosthodontic super-
9. Drago C. Ratios of cantilever lengths and anterior- 25. Kendrick S, Wong D. Vertical and horizontal di- structure designs. Swed Dent J Suppl. 1985;28:71-75.
posterior spreads of definitive hybrid full-arch, screw- mensions of implant dentistry: numbers every dentist 40. Drago C. Cantilever lengths and anterior-posterior
retained prostheses: results of a clinical study. J Prosthodont. should know. Inside Dent. 2009. July/August:2-5. spreads of interim, acrylic resin, full-arch screw-retained
2018;27(5):402-408. 26. Lindquist LW, Rockler B, Carlsson GE. Bone prostheses and their relationship to prosthetic complica-
10. McGlumphy EA, Robinson DM, Mendel DA. resorption around fixtures in edentulous patients treated tions. J Prosthodont. 2017;26(6):502-507.
Implant superstructures: a comparison of ultimate failure with mandibular fixed tissue-integrated prostheses. 41. Rodriguez AM, Aquilino SA, Lund PS. Cantilever
force. Int J Oral Maxillofac Implants. 1992;7(1):35-39. J Prosthet Dent. 1988;59(1):59-63. and implant biomechanics: a review of the literature,
11. Brånemark PI, Zarb GA, Albrektsson T. Tissue In- 27. Ahlqvist J, Borg K, Gunne J, Nilson H, Olsson M, part 2. J Prosthodont. 1994;3(2):114-118.
tegrated Prostheses. Chicago, IL: Quintessence; 1985:51-70, Astrand P. Osseointegrated implants in edentulous jaws: a 42. Kosinski TF. Overdenture design to maximize sta-
117-128. 2-year longitudinal study. Int J Oral Maxillofac Implants. bility and function. Dent Today. 2017;36(2):108-112.
12. Shackleton JR, Carr L, Slabbert JC, Becker PJ. Sur- 1990;5(2):155-163. 43. Sharma S, Makkar M, Teja SS, Singh P. Implant-
vival of fixed implant-supported prostheses related to 28. Hopp M, de Araújo Nobre M, Maló P. Comparison supported overdenture: a review. J Pharm Biomed Sci.
cantilever lengths. J Prosthet Dent. 1994;71:23-26. of marginal bone loss and implant success between axial 2017;07(7):270-277.
13. Taylor R, Bergman G. Laboratory Techniques for the and tilted implants in maxillary all-on-4 treatment 44. Greenstein G, Cavallaro J Jr. Cantilevers extending
Brånemark System. Chicago, IL: Quintessence; 1990, 34- concept rehabilitations after 5 years of follow-up. Clin from unilateral implant-supported fixed prostheses: a re-
26. Implant Dent Relat Res. 2017;19(5):849-859. view of the literature and presentation of practical
14. Brunski JB. Biomechanical factors affecting the 29. Wennström J, Zurdo J, Karlsson S, Ekestubbe A, guidelines. JADA. 2010;141(10):1221-1230.
bone-dental implant interface. Clin Mater. 1992;10: Gröndahl K, Lindhe J. Bone level change at implant- 45. Brunski J. Biomechanics. In: Worthington P,
153-201. supported fixed partial dentures with and without canti- Lang BR, Rubenstein JE, eds. Osseointegration in
15. Osier JF. Biomechanical load analysis of cantilevered lever extension after 5 years in function. J Clin Periodontol. Dentistry. 2nd ed., Hanover Park, IL: Quintessence;
implant systems. J Oral Implantol. 1991;17(1):40-47. 2004;31(12):1077-1083. 2003:49-84.
JADA 151(10) n http://jada.ada.org n October 2020 795
You might also like
- Molar Ratio Practice ProblemsDocument2 pagesMolar Ratio Practice ProblemsMara M. LabanderoNo ratings yet
- Mitsubishi Lancer Evolution VII Workshop ManualDocument1,642 pagesMitsubishi Lancer Evolution VII Workshop ManualDiego Hernan PiñeiroNo ratings yet
- Comparison of Traditional RPE With Two Types of Micro I - 2019 - Seminars in OrtDocument9 pagesComparison of Traditional RPE With Two Types of Micro I - 2019 - Seminars in OrtOmy J. Cruz100% (1)
- Sears Owners Manual Model No 944.529181 Craftsman 1150 Series BS Engine 27in Two Stage Snow Thrower - SmallDocument43 pagesSears Owners Manual Model No 944.529181 Craftsman 1150 Series BS Engine 27in Two Stage Snow Thrower - Smalledahan64% (11)
- Analysis of Strain at Selected Bone Sites of A Cantilevered Implant-Supported ProsthesisDocument7 pagesAnalysis of Strain at Selected Bone Sites of A Cantilevered Implant-Supported ProsthesisMR GOKCHENNo ratings yet
- Prediction of Implant Loss and Marginal Bone Loss by Analysis of Dental Panoramic RadiographsDocument6 pagesPrediction of Implant Loss and Marginal Bone Loss by Analysis of Dental Panoramic RadiographsMuhammad RidwanNo ratings yet
- Am Journal 2009, Distal Jet Com MIDocument9 pagesAm Journal 2009, Distal Jet Com MIMariana SantosNo ratings yet
- 2020 Article 73180Document11 pages2020 Article 73180rachmadyNo ratings yet
- Short Term and LongDocument13 pagesShort Term and LongCARMEN ROSA AREVALO ROLDANNo ratings yet
- Guidelines For Treatment Planning of Mandibular Implant OverdentureDocument6 pagesGuidelines For Treatment Planning of Mandibular Implant OverdentureLia DietrichNo ratings yet
- J Arth 2015 09 001Document7 pagesJ Arth 2015 09 001Carlos Mauricio Salazar BedollaNo ratings yet
- Thanasrisuebwong - Influence of The Residual Ridge Widths and Implant Thread Designs OnDocument7 pagesThanasrisuebwong - Influence of The Residual Ridge Widths and Implant Thread Designs OnGustavo IsmaelNo ratings yet
- Concept of All On Four For Dental Implants A RevieDocument4 pagesConcept of All On Four For Dental Implants A RevieOumaima DabbouNo ratings yet
- Tips and Techniques For Optimal Stent Graft Placement in Angulated Aneurysm NecksDocument6 pagesTips and Techniques For Optimal Stent Graft Placement in Angulated Aneurysm NecksAhmed MohammedNo ratings yet
- Jomi 2018 04 s0815Document9 pagesJomi 2018 04 s0815S. BenzaquenNo ratings yet
- Clinical Outcomes of Ultrashort Sloping Shoulder Implant Design A Survival AnalysisDocument7 pagesClinical Outcomes of Ultrashort Sloping Shoulder Implant Design A Survival AnalysisBagis Emre GulNo ratings yet
- Journal 6Document7 pagesJournal 6JULIA SANFURGO VILLARROELNo ratings yet
- Bone Augmentation of The Edentulous Maxilla For Implant Placement: A Systematic ReviewDocument12 pagesBone Augmentation of The Edentulous Maxilla For Implant Placement: A Systematic ReviewJarvin Miguel Buitrago GalindezNo ratings yet
- Li 2011Document11 pagesLi 2011Hurāirāh ĐāřNo ratings yet
- 10 11607@jomi 8122Document8 pages10 11607@jomi 8122Marlene Kasumi Gantier TakanoNo ratings yet
- Implant-Retained Cantilever Fixed Prosthesis: Where and WhenDocument4 pagesImplant-Retained Cantilever Fixed Prosthesis: Where and WhenSitiKhadijahNo ratings yet
- Relaciones Voladizo Posterior en Prótesis HíbridaDocument7 pagesRelaciones Voladizo Posterior en Prótesis Híbridajdac.71241No ratings yet
- Marginal Bone Loss and Immediate DentureDocument14 pagesMarginal Bone Loss and Immediate DentureSupriya ShuklaNo ratings yet
- Sun Et Al 2023Document9 pagesSun Et Al 2023henriquetaranNo ratings yet
- ENG1 Effect of Different Clasps On Asymmetric Distal Extension Base Supporting Structures 1Document12 pagesENG1 Effect of Different Clasps On Asymmetric Distal Extension Base Supporting Structures 1Madalina BanarescuNo ratings yet
- Angled Abutment 2Document8 pagesAngled Abutment 2jotapintorNo ratings yet
- Clinical Outcome of The Altered Cast Impression Procedure Compared With Use of A One Piece Cast PDFDocument9 pagesClinical Outcome of The Altered Cast Impression Procedure Compared With Use of A One Piece Cast PDFNguyen Thi Minh HienNo ratings yet
- Change in Crown-to-Implant Ratio of Implants Placed in Grafted and Nongrafted Posterior Maxillary Sites: A 5-Year Prospective Randomized StudyDocument6 pagesChange in Crown-to-Implant Ratio of Implants Placed in Grafted and Nongrafted Posterior Maxillary Sites: A 5-Year Prospective Randomized StudyValeria CrespoNo ratings yet
- Factors Affecting Retention of Post SystemsDocument6 pagesFactors Affecting Retention of Post SystemsDonanguyenNo ratings yet
- Sousa2016 PDFDocument11 pagesSousa2016 PDFEsme ValenciaNo ratings yet
- kjod-49-150Document11 pageskjod-49-150RANIK DUTTANo ratings yet
- Occlusion For Implant Suppported CDDocument4 pagesOcclusion For Implant Suppported CDpopat78No ratings yet
- Densit Osoasa A Palatului DurDocument8 pagesDensit Osoasa A Palatului DurDiana DrutaNo ratings yet
- Immediate Versus Conventional Loading of Implant-Supported Maxillary Overdentures: A Finite Element Stress AnalysisDocument7 pagesImmediate Versus Conventional Loading of Implant-Supported Maxillary Overdentures: A Finite Element Stress AnalysisMr OdontologiaNo ratings yet
- (2010 Birdi) Crown-to-Implant Ratios of Short-Length ImplantsDocument9 pages(2010 Birdi) Crown-to-Implant Ratios of Short-Length Implantsyena1010No ratings yet
- Ret 3Document7 pagesRet 3train.with.asadhamoodNo ratings yet
- 5 PDFDocument6 pages5 PDFalejandra_baltaza_17No ratings yet
- Tent-Pole in Regeneration TechniqueDocument4 pagesTent-Pole in Regeneration TechniqueangelicapgarciacastilloNo ratings yet
- Short ImplantsFrom EverandShort ImplantsBoyd J. TomasettiNo ratings yet
- Sagat2010 2Document11 pagesSagat2010 2James Alexander Toruño GordonNo ratings yet
- (2020) Effects of Overdenture Attachment Systems With Different Working Principles On Stress Transmission A Three-Dimensional Finite Element StudyDocument10 pages(2020) Effects of Overdenture Attachment Systems With Different Working Principles On Stress Transmission A Three-Dimensional Finite Element StudyafrickarmNo ratings yet
- Anterior Cable Reconstruction Using Autologous Long Head of The Biceps Tendon For Massive Irreparable Rotator Cuff TearsDocument11 pagesAnterior Cable Reconstruction Using Autologous Long Head of The Biceps Tendon For Massive Irreparable Rotator Cuff TearsjulioNo ratings yet
- Selection of Factors For Mini-Implant Selection Protocol Applied To MARPEDocument9 pagesSelection of Factors For Mini-Implant Selection Protocol Applied To MARPEGAURAV VARMANo ratings yet
- Toti 2017Document40 pagesToti 2017gbaez.88No ratings yet
- Amak JurnalDocument8 pagesAmak Jurnalpratamayossi41No ratings yet
- 01.01 Able, 2018Document7 pages01.01 Able, 2018Daniel IbarraNo ratings yet
- 1 s2.0 S088954060901155X MainDocument8 pages1 s2.0 S088954060901155X Mainbruno mañonNo ratings yet
- Preoperative Planning For Primary Total Hip ArthroplastyDocument8 pagesPreoperative Planning For Primary Total Hip Arthroplastyanon_683301094No ratings yet
- Clinical Behavior of Short Dental Implants - Systematic Review and Meta-Analysis. J Clin Med, 2020Document16 pagesClinical Behavior of Short Dental Implants - Systematic Review and Meta-Analysis. J Clin Med, 2020Marlene Kasumi Gantier TakanoNo ratings yet
- Mandibular Implat RetainedDocument6 pagesMandibular Implat RetainedMaria Fernanda Samaniego MorochoNo ratings yet
- Dr. Uzair Synopsis (Latest)Document14 pagesDr. Uzair Synopsis (Latest)Muhammad UzairNo ratings yet
- And Of: Topics of Interest Cantilever Implant Biomechanics: Review Literature, 1Document6 pagesAnd Of: Topics of Interest Cantilever Implant Biomechanics: Review Literature, 1harshita parasharNo ratings yet
- Dental Implant Navigation System Guide The Surgery Future: SciencedirectDocument9 pagesDental Implant Navigation System Guide The Surgery Future: SciencedirectrachmadyNo ratings yet
- (2013 Hasan) Biomechanics and Load Resistance of Short Dental Implants A Review of The LiteratureDocument6 pages(2013 Hasan) Biomechanics and Load Resistance of Short Dental Implants A Review of The Literatureyena1010No ratings yet
- Septal Extension Graft ArticlesDocument7 pagesSeptal Extension Graft Articlesjose orlando sturla pelleranoNo ratings yet
- Aaid Joi D 11 00068Document8 pagesAaid Joi D 11 00068Hema SinghNo ratings yet
- (2007 Verri) Verri - Et - Al - 2007 - Lenght - and - Diameter - ImpDocument11 pages(2007 Verri) Verri - Et - Al - 2007 - Lenght - and - Diameter - Impyena1010No ratings yet
- CLP Surgical GuideDocument3 pagesCLP Surgical GuideAmit SadhwaniNo ratings yet
- The Journal of ArthroplastyDocument4 pagesThe Journal of ArthroplastyFrancisco J DominguezNo ratings yet
- C As The Use ofDocument20 pagesC As The Use ofVenkat MarakalaNo ratings yet
- A Long-Term Study of 370 Autotransplanted Premolars. Part IV. Root Development Subsequent To TransplantationDocument13 pagesA Long-Term Study of 370 Autotransplanted Premolars. Part IV. Root Development Subsequent To TransplantationAdriana BragaNo ratings yet
- A New Geometric AP SpreadDocument8 pagesA New Geometric AP SpreadGerard GonzalezNo ratings yet
- Is The Size of The Acetabular Bone Lesion A Predictive Factor For Failure in Revisions of Total Hip Arthroplasty Using An Impacted Allograft?Document6 pagesIs The Size of The Acetabular Bone Lesion A Predictive Factor For Failure in Revisions of Total Hip Arthroplasty Using An Impacted Allograft?abass elananiNo ratings yet
- Iit Jee Study MaterialDocument3 pagesIit Jee Study MaterialIit - PulseNo ratings yet
- PLL CBDocument28 pagesPLL CBEugenio Verdinelli100% (2)
- RETScreen Combined Heat and Power CogenerationDocument24 pagesRETScreen Combined Heat and Power CogenerationArul SankaranNo ratings yet
- DES 606: Watershed Modeling With Hec-Hms: Theodore G. Cleveland, PH.D., P.E 29 June 2011Document35 pagesDES 606: Watershed Modeling With Hec-Hms: Theodore G. Cleveland, PH.D., P.E 29 June 2011CHEL TAKNo ratings yet
- Various Types of Shear ConnectorsDocument6 pagesVarious Types of Shear Connectorssilverware1No ratings yet
- Offer For Panasonic Welding Machine Model 400RX1Document2 pagesOffer For Panasonic Welding Machine Model 400RX1eaNo ratings yet
- Induction Cooker Ic1600 Instruction Manual Pn40 50704 00 200621154438Document12 pagesInduction Cooker Ic1600 Instruction Manual Pn40 50704 00 200621154438Vicky TanNo ratings yet
- Labsheet Translation Mechanical SystemDocument33 pagesLabsheet Translation Mechanical SystemMuhammad Ehsan Abdul Halim0% (1)
- ETEEAP - MemorazonDocument18 pagesETEEAP - MemorazonRAP & GAB TVNo ratings yet
- Activated Sludge Rheology A Critical Review On Data Collection and ModellingDocument20 pagesActivated Sludge Rheology A Critical Review On Data Collection and ModellingZohaib Ur RehmanNo ratings yet
- D&H-301 Rev 4 Golite XXX & XXX GMDocument1 pageD&H-301 Rev 4 Golite XXX & XXX GMخربوش سماعينNo ratings yet
- ABB Outdoor 1 OverviewDocument3 pagesABB Outdoor 1 OverviewVictor GuzmanNo ratings yet
- Capacities and Specifications: MaintenanceDocument22 pagesCapacities and Specifications: MaintenanceAlexander the greatNo ratings yet
- Containers in Non-Cellular ShipsDocument7 pagesContainers in Non-Cellular ShipschildofheavenNo ratings yet
- Ullmanns Encyclopedia of Industrial Chemistry Filtration 1 Fundamentals PDFDocument38 pagesUllmanns Encyclopedia of Industrial Chemistry Filtration 1 Fundamentals PDFHervéNo ratings yet
- Used Water Submission ProceduresDocument26 pagesUsed Water Submission Procedurescloud6521100% (1)
- Brochure Rectifier Sg825863ben c00!09!2016 LRDocument8 pagesBrochure Rectifier Sg825863ben c00!09!2016 LRsubhashkpn86No ratings yet
- Product Blending CalculationsDocument23 pagesProduct Blending CalculationsCatlinhbk08100% (1)
- Fact-Sheet-No.-28-Aug-2018 Oxyfuel Safety - Check Valves and Flashback ArrestorsDocument3 pagesFact-Sheet-No.-28-Aug-2018 Oxyfuel Safety - Check Valves and Flashback ArrestorsCarlos BustamanteNo ratings yet
- Goddstar Cb21t20s Pc-81aDocument19 pagesGoddstar Cb21t20s Pc-81aedisonic2000No ratings yet
- Pen Picture of Ata-ul-GhalibDocument2 pagesPen Picture of Ata-ul-Ghalibata_ghalib100% (2)
- Design and Research On The LCL Filter in Three-Phase PV Grid-Connected InvertersDocument4 pagesDesign and Research On The LCL Filter in Three-Phase PV Grid-Connected InvertersJong Hee LeeNo ratings yet
- W - 8-10ab Mole-Mass Problems Wkst-Key and QDocument4 pagesW - 8-10ab Mole-Mass Problems Wkst-Key and QR RenegadeNo ratings yet
- General Specification For Materials, Fabrication and Installation of StructureDocument74 pagesGeneral Specification For Materials, Fabrication and Installation of StructureOrlando Fang75% (4)
- Choosing Bandsaw Guides PDFDocument8 pagesChoosing Bandsaw Guides PDFgortonm1100% (1)
- Csi Section 270553Document16 pagesCsi Section 270553Rafael Nuñez HernandezNo ratings yet