Professional Documents
Culture Documents
GPT 5.03 Pathology of The Adrenal Glands - v2 - 01.07.24
GPT 5.03 Pathology of The Adrenal Glands - v2 - 01.07.24
Uploaded by
Jonah Mae SampangOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
GPT 5.03 Pathology of The Adrenal Glands - v2 - 01.07.24
GPT 5.03 Pathology of The Adrenal Glands - v2 - 01.07.24
Uploaded by
Jonah Mae SampangCopyright:
Available Formats
GENERAL PATHOLOGY
Pathology of the Adrenal Glands Block 5
Jessica P. Abella, MD | December 4, 2023 GPT 5.03
OVERVIEW ● There is no distinct separation between the three cell types
I. Adrenal Glands ● Primary Chronic of the adrenal cortex. (Fig. 2)
II. Diseases of the Adrenal Adrenocortical ○ Glomerulosa
Cortex Insufficiency (Addison ➢ secretes mineralocorticoids mainly aldosterone
A. Adrenocortical Disease) ○ Fasciculata
Hyperfunction ● Secondary ➢ makes up 75% of the adrenal cortex layer
● Hypercortisolism Adrenocortical
➢ secretes glucocorticoids mainly cortisol
(Cushing Syndrome) Insufficiency
● Primary C. Adrenocortical
○ Reticularis
Hyperaldosteronism Neoplasms ➢ secretes sex steroids (androgens)
● Secondary ● Adrenocortical
Hyperaldosteronism Adenoma
● Adrenogenital III. Diseases of the Adrenal
Syndromes Medulla
B. Adrenocortical A. Pheochromocytoma
Insufficiency
● Primary Acute
Adrenocortical
Insufficiency
● Waterhouse
Friderichsen Syndrome
ABBREVIATIONS
ACTH Adrenocorticotropic hormone
MEN Multiple endocrine neoplasia
DM Diabetes mellitus
CRH Corticotropin-releasing hormone Figure 2. Histologic features of the adrenal glands. (●) adrenal medulla;
adrenal cortex: (+) reticularis, (■) fasciculata, (⬥) glomerulosa, (*) fibrous
AI Adrenocortical insufficiency
capsule, (□) adipose tissue.
DIC Disseminated intravascular coagulation
MSH Melanocyte-stimulating hormone
LEARNING OBJECTIVES
● To differentiate the pathogenesis of the different hypo- and
hyperfunctioning diseases of the adrenal cortex
● To understand the pathogenesis of pheochromocytoma
● To identify the morphological features of these diseases
I. ADRENAL GLANDS
A. Gross and Histologic Features
Figure 3. Histologic features of the adrenal cortex in higher magnification.
(A) glomerulosa, (B) fasciculata, (C) reticularis.
Figure 1. Gross anatomy of the right adrenal kidney (normal) located between
the liver and the kidney with visible adipose tissue.
● Paired endocrine organs located on the superior pole of each
kidney
Table 1. Parts of the adrenal gland[2026 Trans]
Adrenal Cortex Adrenal Medulla
● Outer layer ● Inner layer
● Mesodermally-derived ● Neuroectodermally-derived
● Secretes steroid hormones ● Secretes catecholamines
from cholesterol ● Darker color Figure 4. Gross view of adrenal glands. Top: atrophied, middle: normal,
bottom: hyperplastic.
● Yellowish
Page 1 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
II. DISEASES OF THE ADRENAL CORTEX
Table 2. Adrenocortical hyperfunction
Adrenal Cortex Hormone Produced Hyperfunctional Disease
Glomerulosa Aldosterone Hyperaldosteronism
Fasciculata Cortisol Cushing Syndrome
Androgens or Virilizing
Reticularis Androgens
Syndromes
A. Adrenocortical Hyperfunction
Hypercortisolism (Cushing Syndrome)
● Caused by elevation of glucocorticoid levels
● May be exogenous or endogenous
EXOGENOUS CAUSE
● Main cause of Cushing syndrome
● Caused by administration of steroidal or anti-inflammatory
medications to patients with impaired immune system
Figure 5. Crooke hyaline (→) change in the pituitary gland
● Ex: dexamethasone, beclomethasone, methylprednisolone
ADRENAL GLAND CHANGES
ENDOGENOUS CAUSE
● Abnormalities seen depend on the cause
● Divided into ACTH-dependent and -independent
● Exogenous cause: cortical atrophy
○ Administration of glucocorticoids → suppression of
Table 3. Endogenous causes of Cushing syndrome.
endogenous ACTH → cortical atrophy
ACTH-dependent ACTH-independent
● Endogenous cause: diffuse hyperplasia (Fig. 6)
● Increase in cortisol and ● Increase in cortisol but no
● Macronodular or micronodular hyperplasia
ACTH increase in ACTH
● Adenoma or carcinoma
● Usual cause (60-70%): ● Adenoma (10-20%) .
Cushing’s disease ● Carcinoma
○ Pituitary form of Cushing ● Marked hypercortisolism
syndrome ● McCune Albright Syndrome
○ Commonly seen in young ○ Rare genetic disorder
adult females ○ Recognized by fibrous
● Neuroendocrine tumors dysplasia, precocious
● Adenoma/hyperplasia puberty, and cafe au lait
● Ectopic ACTH (5-10%) spots
○ Small cell carcinoma of ○ Hyperthyroidism,
the lungs acromegaly, activating
Figure 6. Left: Diffuse hyperplasia of the adrenal (bottom) contrasted with
○ Pancreas or medullary mutation of GNAS1 gene
normal adrenal gland (top). The cross-section of the adrenal cortex is yellow
carcinoma ● Bilateral hyperplasia and thickened, and a subtle nodularity is seen. Right: Histology of diffuse
● Carney Complex hyperplasia showing expanded lipid-rich cells that represent the yellow
○ Rare genetic disorder formation in the cortex.
○ Associated with MEN
syndromes Clinical Presentation
○ Affects thyroid, pituitary,
and adrenals
○ Lead to cardiac myxoma,
skin pigmentation,
myxomas of the skin, and
other testicular tumors
Morphology
● Major lesions of Cushing’s syndrome are found in the
pituitary and adrenal glands.
PITUITARY GLAND CHANGES
● Changes are seen regardless of the cause (whether Figure 7. A patient with Cushing syndrome demonstrating central obesity,
moon facies, and abdominal striae.
exogenous or endogenous)
● Crooke hyaline (Fig. 5)
● May be subtle and develops slowly
○ Intermediate keratin filaments in the cytoplasm
● Hypertension
○ When they accumulate, they replace the basophilic
○ May be the initial presentation
cytoplasm of ACTH-producing cells in the pituitary
● Weight gain
○ Central pattern of fat distribution
○ Truncal obesity
○ Moon facies
○ Buffalo hump
Page 2 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
● Weakness Primary Hyperaldosteronism
○ Atrophy of proximal limb muscles ● Stems from an autonomous overproduction of aldosterone,
● Glucose intolerance / secondary DM with resultant hypertension, suppression of the
○ Excess glucocorticoids → gluconeogenesis → inhibition renin-angiotensin system, and decreased plasma renin
of glucose reuptake and stays in the blood → secondary activity[Robbins, p. 1118]
diabetes mellitus → polydipsia, polyuria ● Can be found in three conditions (3 causes):
● Thin fragile skin, easy bruising of the skin ○ Bilateral Idiopathic Hyperaldosteronism
○ Loss of collagen → abdominal striae ○ Adrenocortical neoplasm (Conn Syndrome)
● Suppression of immune system ○ Familial hyperaldosteronism (Glucocorticoid suppressible)
○ Lead to infections ● Increased aldosterone secretion manifests as hypertension
● Mental disturbances and hypokalemia
○ Psychosis, depression, mood swings ○ Through its effects on the renal mineralocorticoid
● Menstrual disturbances and hirsutism in females receptor, aldosterone promotes sodium reabsorption →
increases water reabsorption → expands the
Diagnosis extracellular fluid volume and elevates cardiac output
● Recall: Hypothalamic-Pituitary-Adrenal Axis ○ Other manifestations are effects of the
○ Helps maintain homeostatic function in the stress hyperaldosteronism-induced hypertension
response of the body ○ Primary hyperaldosteronism may be the most common
○ Neurons coming from the hypothalamus synthesizes cause of secondary hypertension
CRH → stimulates production of ACTH → stimulates the ➢ Long-term effects:
adrenal gland → zona fasciculata releases ↪ Cardiovascular compromise (e.g. left ventricular
glucocorticoids hypertrophy and reduced diastolic volumes)
● Unbound cortisol is filtered at the glomerulus and is ↪ Increased prevalence of adverse effects (e.g.
excreted stroke and myocardial infarction)
● 17-hydroxycorticosteroids: excretory products of ○ Hypokalemia was considered a mandatory feature of
corticosteroids primary hyperaldosteronism, but increasing numbers of
normokalemic patients are now diagnosed[Robbins, p. 1118]
DEXAMETHASONE SUPPRESSION TEST (DST) ➢ Renal potassium wasting → hypokalemia →
● Used in the evaluation of endogenous Cushing syndrome neuromuscular manifestations (e.g. weakness,
● Principles: paresthesias, visual disturbances, and occasionally
○ Assesses the lack of suppression of the HPA axis by frank tetany)
exogenous corticosteroids
○ Dexamethasone: a potent synthetic corticosteroid
➢ With high affinity for the receptors of the
glucocorticoid
➢ Has a long duration of action
○ Diurnal pattern: cortisol levels are higher in the morning
and decreases throughout the day
● Types:
○ Low dose: used for initial diagnosis (i.e. screening or
confirmatory) of Cushing syndrome
➢ After dexamethasone is given, the serum cortisol
levels are drawn the next morning
○ High dose: used to categorize into ACTH-dependent or
ACTH-independent after confirmatory diagnosis
● Expected Findings:
○ Pituitary Causes
➢ Low dose → ⬆ ACTH (no effect) → urinary excretion
still present
➢ High dose → feedback inhibition (⬇ ACTH) → no
urinary excretion
○ Ectopic ACTH
➢ Recall: Small cell lung carcinoma, pancreatic or
medullary carcinomas
➢ High or low dose: no effect on ACTH → fails to Figure 8. The major causes of primary hyperaldosteronism and its principal
effects on the kidney.
suppress excretion
○ Adrenal Tumor
● Diagnosis: confirmed by elevated ratios of plasma
➢ ⬆ cortisol → feedback inhibition → ⬇ ACTH
aldosterone concentration to plasma renin activity[Robbins]
○ If screening test is positive, a confirmatory aldosterone
Hyperaldosteronism
suppression test is performed, since many other
● Aldosterone: mineralocorticoid produced in the zona
disorders can alter the plasma aldosterone and renin
glomerulosa of the adrenal cortex in adrenal glands
● Hyperaldosteronism: general term grossly related group of ratios
conditions that present with chronic and excessive
aldosterone secretion
● May be primary or secondary to an extra-adrenal cause
Page 3 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
Bilateral Idiopathic Hyperaldosteronism
● Most common underlying cause (60% of cases), most of
which are sporadic
● Bilateral nodular hyperplasia of the aldosterone-secreting
zona glomerulosa cells
● Tend to affect the older age group
● Present with less severe hypertension compared to those
with an adrenal neoplasm
● Morphology [Robbins, p. 1119]
○ Diffuse and focal hyperplasia of cells resembling those
of the normal zona glomerulosa Figure 10. Adrenal cortical adenoma. Left: Gross appearance. The adenoma
○ The hyperplasia is often wedge-shaped, extending from is distinguished from nodular hyperplasia by its solitary, circumscribed nature.
the periphery toward the center of the gland Right: Histologic features. The neoplastic cells are vacuolated because of the
○ Enlargement may be subtle; adrenocortical adenoma presence of intracytoplasmic lipids with mild nuclear pleomorphism.
must be carefully excluded as the cause for
hyperaldosteronism Familial Hyperaldosteronism
● Treatment: aldosterone antagonist (e.g. spironolactone) [Robbins] ● Rare cause (5%)
● Have four distinct subtypes (FH-I to FH-IV)
Adrenocortical Neoplasm (Conn Syndrome) ○ FH-I (Glucocorticoid-remediable aldosteronism) is the
● Second most common cause (35%) most common
● Adrenocortical neoplasm is most commonly an ○ CYP11B2: the gene that encodes for aldosterone
aldosterone-producing adenoma (Conn syndrome) but, synthase, the enzyme in the last step in aldosterone
rarely, may also be an adrenocortical carcinoma [Robbins, p. 1119] synthesis [Robbins, p. 1119]
● Aldosterone-secreting adenoma (Conn syndrome) ○ Rearrangement in chromosome 8 → CYP11B2 under the
○ Almost always a solitary, small (<2cm in diameter), and control of the ACTH-responsive CYP11B1 gene
well-circumscribed lesion promoter → ACTH stimulates the synthesis of
○ Found usually on the left adrenal gland than on the right aldosterone synthase from the chimeric gene →
○ Often buried within the gland and do not produce visible aldosterone production is under the control of ACTH,
enlargement → difficult to locate via imaging which is suppressible by dexamethasone [Robbins, p. 1119]
○ More common in females than males
○ Commonly seen in adult patients (30-40 yrs old) Secondary Hyperaldosteronism
○ Characteristic feature: spironolactone bodies ⭐ ●
●
Usually an extra-adrenal cause
Release of aldosterone occurs in response to activation of
➢ Called such because they are found after treatment
the renin-angiotensin system
with the antihypertensive drug, spironolactone
○ No suppression of ACTH secretion → the adjacent ● Characterized by increased levels of plasma renin ⭐
adrenal cortex and that of the contralateral gland are not ● Seen in:
atrophic [Robbins p. 1119] ○ Decreased renal perfusion (due to arteriolar
○ Treatment: surgical excision[Robbins] nephrosclerosis, renal artery stenosis)
○ Arterial hypovolemia and edema (due to congestive
heart failure, cirrhosis, nephrotic syndrome)
○ Pregnancy (due to estrogen-induced increases in plasma
renin substrate)
● Treatment: correction of the underlying cause of the
hyperactivity of the renin-angiotensin system [Robbins, p. 1120]
Adrenogenital Syndromes
● Disorders of sexual differentiation (e.g. virilization or
Figure 9. Spironolactone bodies. Left: Observe the pink eosinophilic feminization) can be caused by primary gonadal disorders
cytoplasmic inclusions (↙). Right: Under higher magnification, observe the and several primary adrenal disorders
laminated cytoplasmic inclusions (⭘). ● The adrenal cortex secretes dehydroepiandrosterone and
androstenedione, both convertible to testosterone in
○ Bright yellow on cut section and are composed of peripheral tissues [Robbins, p. 1120]
lipid-laden cortical cells that more closely resemble ● Adrenal androgen formation is regulated by ACTH; excess
fasciculata cells than glomerulosa cells; cells have secretion may either be a “pure” syndrome or as a
uniform size and shape with occasional modest nuclear component of Cushing disease [Robbins, p. 1120]
and cellular pleomorphism [Robbins, p. 1119] ● Adrenal causes of androgen excess:
○ Adrenocortical Neoplasms (CA)
➢ More likely to be androgen-secreting adrenal
carcinomas than adenomas
➢ Associated with virilization and hypercortisolism
(“mixed syndrome”)
➢ Morphologically identical to other cortical neoplasms
○ Congenital Adrenal Hyperplasia (CAH)
➢ Group of disorders that stem from several autosomal
recessive, inherited metabolic errors
Page 4 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
➢ Each error is characterized by a deficiency of a
○ Block in cortisol synthesis and excess androgen production
particular enzyme involved in cortisol biosynthesis lead to virilization
➢ Most common cause: 21-hydroxylase deficiency ➢ Easily recognized in the female at birth or in utero
(caused by mutations of CYP21A2; 90% cases) ➢ Males come to clinical attention 5-15 days later because
➢ Morphology of CAH [Robbins, p. 1121] of salt loss, hypotension, and other abnormalities
↪ Adrenals are bilaterally hyperplastic (up to ● Simple virilizing adrenogenital syndrome without salt wasting
10-15x normal weight) due to sustained ○ Present as genital ambiguity
○ Generate sufficient mineralocorticoid to prevent salt-wasting
elevation of ACTH
○ Lowered glucocorticoid levels → reduction of feedback
↪ Adrenal cortex is thickened, nodular, and appears
inhibition of ACTH secretion → testosterone level
brown because of lipid depletion
increased → virilization
↪ The proliferating cells are mostly compact,
● “Nonclassic” or late-onset adrenal virilism
eosinophilic, lipid-depleted cells intermixed with ○ More common
lipid-laden clear cells ○ Partial 21-hydroxylase deficiency leads to later onset
↪ A subset of 21-hydroxylase–deficient patients ○ Present with mild manifestations (e.g. hirsutism, acne, and
also demonstrates adrenomedullary dysplasia menstrual irregularities)
● When there are blockages or defective steps in a certain ○ Cannot be diagnosed on routine newborn screening
pathway, the steroid precursors are channeled into other ○ Diagnosis: demonstration of biosynthetic defects in
steroidogenesis
pathways
○ Blockage in the pathways producing mineralocorticoids
and glucocorticoids (e.g. 21-hydroxylase deficiency) → B. Adrenocortical Insufficiency
steroid precursors channeled to the pathway producing ● or hypofunction
sex steroids → increased production of androgens → ● May be caused by:
virilization ○ Primary hypoadrenalism – primary adrenal disease
○ Simultaneously, mineralocorticoid and glucocorticoid ○ Secondary hypoadrenalism – decreased stimulation of
production are decreased the adrenals due to a deficiency of ACTH
➢ cortisol deficiency → reduced feedback inhibition →
increased ACTH secretion → adrenal cortex
hyperplasia
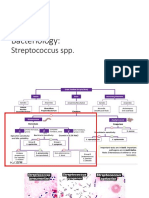
Figure 12. 3 Major Patterns of Adrenocortical Insufficiency
3 MAJOR PATTERNS OF ADRENOCORTICAL INSUFFICIENCY
1. Primary acute AI (adrenal crisis)
2. Primary chronic AI (Addison disease)
3. Secondary adrenocortical insufficiency
Primary Acute Adrenocortical Insufficiency
● Acute crisis in patients with chronic adrenocortical
insufficiency
○ May be precipitated by any form of stress that requires
Figure 11. Consequences of C-21 hydroxylase deficiency. 21-Hydroxylase an immediate increase in steroid output to maintain
deficiency impairs the synthesis of both cortisol and aldosterone at different
homeostasis [Robbins, p. 1122]
steps (“Blocks”). The resultant decrease in feedback inhibition (dashed line)
● Sudden withdrawal of steroids in patients maintained on
causes increased secretion of adrenocorticotropic hormone, resulting in
adrenal hyperplasia and increases testosterone synthesis. The sites of action exogenous corticosteroids
of 11-, 17-, and 21-hydroxylase are shown in numbers as circles. ○ or failure to increase steroid doses in response to an
acute stress → adrenal crisis because of the inability of
the atrophic adrenals to produce glucocorticoid
21-HYDROXYLASE DEFICIENCY SYNDROMES[Robbins & Cotran] hormones [Robbins, p. 1122]
● The consequences of the deficiency varies in severity depending on ● As a result of massive adrenal hemorrhage, which damages
the nature of the CYP21A2 mutation
the adrenal cortex sufficiently to cause acute AI
● Salt-wasting (“classic”) adrenogenitalism
○ Total lack of 21-hydroxylase → inability to convert
○ Occurs in
progesterone into deoxycorticosterone → no ➢ Newborns following prolonged and difficult delivery
mineralocorticoid synthesis and deficient cortisol synthesis with considerable trauma and hypoxia
○ Present with salt wasting, hyponatremia, and hyperkalemia, ➢ Some patients maintained on anticoagulant therapy
which induce acidosis, hypotension, cardiovascular collapse, ➢ Postsurgical patients who develop disseminated
and possibly death intravascular coagulation (DIC) and consequent
Page 5 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
hemorrhagic infarction of the adrenals Primary Chronic Adrenocortical Insufficiency (Addison Disease)
➢ Complication of disseminated bacterial infection ● Results from progressive destruction of adrenal cortex
(Waterhouse-Friderichsen syndrome) ● Uncommon disorder
● Symptoms described by Thomas Addison: changes of the
Table 4. Features of Waterhouse-Friderichsen Syndrome.
skin color & heart
Waterhouse-Friderichsen Syndrome ● Causes:
● Described by Waterhouse (English physician) ○ Autoimmune adrenalitis – inflammation of the adrenals
History
& Friderichsen (Danish pediatrician) ➢ More common
● Can occur at any age but is more common in ➢ 80% to 90% of cases of primary adrenal insufficiency
Epidemiology
children in high-income countries [Robbins, p. 1123]
● Basis for the adrenal hemorrhage is ○ Infections – e.g., TB, HIV
uncertain but may be due to direct bacterial ➢ Particularly by Mycobacterium tuberculosis
Etiology seeding of small vessels in the adrenal (Tuberculous Adrenalitis)
● Overwhelming bacterial infection, classically
Neisseria meningitidis septicemia ⭐ ➢ Fungi may also cause chronic AI [Robbins, p. 1123]
○ Metastatic neoplasms – more than primary carcinoma or
● Purpuric rash adenoma
● Rapidly progressive hypotension leading to ➢ Carcinomas of the lung and breast are the source of
shock a majority of metastases [Robbins, p. 1124]
● DIC
● Rapidly developing AI associated with
TUBERCULOUS ADRENALITIS
massive bilateral adrenal hemorrhage
Clinical
manifestations
Figure 13. Diffuse purpuric rash in a patient.
● Adrenal glands become shrunken,
hemorrhagic, and may appear infarcted
Figure 16. Tuberculous adrenalitis.
● Histology:
♦ = Central pinkish necrotic area, surrounded by lymphocytes,
Gross epithelioid macrophages, & Langhan giant cells (⭘)
⭘ = remaining intact adrenocortical cells
● Infection proceeds over months to years
● Destruction caused to the adrenal cortex leads to chronic AI
● ⬇ plasma cortisol → feedback inhibition → ⬆ ACTH
● Stimulates melanocyte production → skin hyperpigmentation
Figure 14. Adrenals are grossly hemorrhagic and
shrunken.
For clinical manifestations of chronic AI to appear, at least
⭐
● Adrenals are converted to sacs of clotted ●
blood 90% of the adrenal cortex has been compromised
● Hemorrhage starts within the medulla near ● Clinical presentation:
thin-walled venous sinusoids, then suffuses ○ Weakness / easy fatigability – initial presentation
peripherally into the cortex, often leaving ➢ Insidious onset
islands of recognizable cortical cells ○ Patient may seek consult when glucocorticoids and
mineralocorticoids have significantly decreased:
➢ Volume depletion & hypotension due to potassium
retention and sodium loss
➢ GI disturbances (vomiting or diarrhea)
Histology
➢ Hyperpigmentation of the skin ⭐
↪ Occurs in those with primary adrenal lesions
↪ No hyperpigmentation for those with pituitary
lesions (secondary AI)
↪ Caused by stimulating the production of ACTH to
which it requires the ACTH precursor
pro-opiomelanocortin (POMC)
↪ ⬆ POMC → ⬆ ACTH & Melanocyte stimulating
Figure 15. Microscopically, little residual cortical
architecture is discernible.
hormone (MSH) → skin hyperpigmentation
Page 6 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
Secondary Adrenocortical Insufficiency Histological Morphology
● Any disorder of the hypothalamus and pituitary, such as:
○ Metastatic cancer
○ Infection
○ Infarction
○ Irradiation
● These disorders reduce the output of ACTH leading to a
syndrome of hypoadrenalism
○ Has many similarities to Addison disease [Robbins, p. 1124]
C. Adrenocortical Neoplasms
● Can be functioning or nonfunctioning
○ Functional adrenal neoplasms: mostly responsible for
various forms of hyperadrenalism
● In adults: adrenocortical adenoma and carcinomas are
equally common
Figure 18. Adrenocortical adenoma under a microscope, showing the
● In children: there is a predominance of adrenocortical
remaining compressed normal fasciculata cells (⭘) and the adenoma that is
carcinomas
well-differentiated, resembles the cells in the fasciculata layer, and has
minimal cellular pleomorphism (⭘). Since it resembles the fasciculata cells,
Adrenocortical Adenoma you expect the adenoma to produce cortisol.
● The most common primary lesion in the adrenal cortex
● Most are nonfunctional adenomas
○ clinically silent
○ only discovered during post-mortem examinations
● For functional adenomas: clinical manifestation depends on
the steroid hormones it produces (Refer to Table 5)
● Functional status of an adrenal cortical adenoma cannot be
distinguished on the basis of morphologic features[Robbin &
Cotrans]
○ Determination of functionality is based on clinical
evaluation & measurement of hormones or metabolites
in the blood.
Table 5. Functional adrenocortical adenomas and its manifestations
Functional adrenocortical
⭐
adenomas
Clinical Manifestations
Aldosterone ● Conn's syndrome
producing adenomas ● Hypertension, hypokalemia
● Cushing syndrome
Cortisol ● Moon facies, buffalo hump, truncal Figure 19. Adrenocortical adenoma under a microscope, showing eosinophilic
producing adenomas obesity, hypertension, secondary cytoplasms. The neoplastic cells are vacuolated because of the presence of
diabetes intracytoplasmic lipids (⭘). There is nuclear pleomorphism or endocrine atypia
● Virilization (⭘). Mitotic activity and necrosis are not seen.
Sex steroid hormone ● Feminization
producing adenomas ● Hirsutism, menstrual problems, sexual Adrenocortical Carcinoma
dysfunction ● Adrenocortical carcinomas are rare neoplasms that have a
bimodal distribution in the 1st and 5th decades of life [Robbins]
Gross Morphology ● More likely to be functional than adenomas and are often
● Very small, well-circumscribed, solitary lesion ⭐ associated with virilism or other clinical manifestations of
hyper-adrenalism
○ Often grow to a maximum of 2.5 cm
● Yellowish brown in the cut section ● Median patient survival is about 2 years
○ Due to the presence of lipid
Gross Morphology
●
●
For nonfunctional adenomas, the adjacent cortex is normal
For functional adenomas, the adjacent cortex is atrophic ● Large, invasive, ill-defined lesions ⭐
○ Many exceeding 20 cm in diameter, which efface the
native adrenal gland
● It can be variegated in the cut section
● Lesions tend to invade the vena cava, the adrenal vein, and
lymphatics
● Metastasis to periaortic or regional nodes are often seen,
giving to a distant hematogenous spread to the lungs or
other organs
Figure 17. (Left) Gross sample of an adrenocortical adenoma.
(Right) Cut section of the adrenocortical adenoma.
Page 7 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
III. DISEASES OF THE ADRENAL MEDULLA
● Adrenal medulla is structurally and functionally different
from the adrenal cortex because it is made up by specialized
neuroendocrine cells, such as the: ⭐
○ Chromaffin cells (NE markers)
➢ Produces catecholamines
↪ Epinephrine - systemic transmitter and is usually
associated with the α and β adrenergic receptors
↪ Norepinephrine - local transmitter that is
involved with the sympathetic postganglionic
Figure 20. Adrenal carcinoma, showing hemorrhagic (⭘), necrotic (⭘), and
neurons
cystic areas (⭘). The upper pole of the kidney (⭘) is being compressed by the ○ Sustentacular cells (S-100)
large adrenal lesion. ➢ Supports the chromaffin cells
➢ Spindly type of cells
● Immunohistochemical stains may help in distinguishing the
specialized cells
Neoplasms are the most important conditions found in the
⭐
●
adrenal medulla
Figure 21. Adrenal carcinoma. Large lesion (↙) that is poorly demarcated,
necrotic in some areas that is compressing the kidney (↙). The carcinoma has
a tendency to become very large because it is located in the retroperitoneum.
Histological Morphology
Figure 24. Adrenal medulla under the microscope,
containing chromaffin cells (↙) and sustentacular cells (↙).
● Paraganglion system is made up of the adrenal medulla
and other extra-adrenal organs that contains
neuroendocrine cells
● These extra-adrenal paraganglia are closely associated with
the autonomic nervous system and can be divided into three
groups based on their anatomic distribution
○ Branchiomeric group (located at the head and neck)
➢ Ex. carotid body (carotid paragangliomas)
Figure 22. Adrenocortical carcinoma (malignant) which shows the invasion of ○ Intravagal group (runs along the vagus nerve)
the adrenal vein (*) and focal hemorrhage (⬥). Some of the cells surrounding
○ Aortosympathetic group
the adrenal vein have pleomorphic nuclei and hyperchromasia. The cells are
➢ Ex. organs of Zuckerkandl
very disorganized. The cells resemble the cells in the reticularis zone.
Figure 23. Adrenocortical carcinoma. (Left) A very disorganized adrenal
cortex that resembles the reticularis zone (yellow circle). Some have lipid
content. (Right) Highly pleomorphic and atypical cells and hemorrhage are
observed.
Figure 25. Paraganglion system
Page 8 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
A. Pheochromocytoma Histological Morphology
Tumors of the chromaffin cells, resulting in the release of Pheochromocytoma demonstrates a characteristic nests of
⭐
● ●
excessive catecholamines cells (Zellballen pattern) with abundant cytoplasm
● Rule of 10’s ⭐
○ 10% of pheochromocytoma are extra-adrenal
○ 10% of sporadic type of adrenal pheochromocytomas
are bilateral
➢ For the familial cases, it can go as high as 50%
○ 10% of pheochromocytoma are biologically malignant
➢ Malignancy are more common in the extra-adrenal
paragangliomas
○ 10% of pheochromocytoma are not associated with
hypertension
➢ Most of them present with paroxysmal episodes,
where patients would have a sudden rise of blood
pressure and also palpitation
Gross Morphology
● Roughly, it has a wide array of morphologic features
○ It can be presenting a very small lesion (1 gram) or to Figure 28. Pheochromocytoma (■) which is enclosed by the compressed 3
layers of the adrenal cortex (⬥). Higher magnification shows a nest of large
some extent, large hemorrhagic masses (kilograms)
polygonal chromaffin cells (pinkish cytoplasms) with surrounding capillaries.
Figure 26. (Left) Pheochromocytoma shows a gray tan color (⬥), while the
residual adrenal cortex shows a yellow cut surface (white arrow)
(Right) The tumor is well-circumscribed, enclosed by the connective tissue
and the remaining comma-shaped adrenal cortical portion below. In the cut
surface, there are lobulated areas because of the vascular fibrous network.
Figure 29. (Left) Pheochromocytoma with round, ovoid, spindled, and some
salt and pepper chromatin type of nuclei. (Right) Electron micrograph of
pheochromocytoma shows dark circles, which are membrane-bound
neurosecretory granules in which catecholamines are stored.
B. Neuronal Neoplasms
● Neuroblastic tumors
● Commonly found in children
*TG Note: Doc Abella mentioned that neuronal neoplasms will be further
discussed in the succeeding lectures.
Figure 27. Fresh pheochromocytoma sample. Using potassium dichromate
solution, tumor cells become dark brown (bottom specimen) because of the
oxidation of stored catecholamines found in pheochromocytoma.
Page 9 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
IV. REVIEW QUESTIONS
Adrenal Glands _____8. A patient presents with paroxysmal episodes or
hypertension, tachycardia, and headache. Your working diagnosis
_____1. Which of the following are paired correctly? is pheochromocytoma. Overgrowth of which type of cells are
A. Zona glomerulosa: glucocorticoids responsible for this presentation?
B. Zona fasciculata: aldosterone A. Chromaffin cells
C. Zona reticularis: androgens B. Sustentacular cells
D. All of the above C. Zellballen cells
D. All of the above
Diseases of the Adrenal Cortex
ANSWERS
_____2. A patient presents in the clinic with hypertension, truncal 1: C 2: A 3: C 4: A 5: C 6: B 7: D 8: A
obesity, and weakness. Which of the following findings are
expected? RATIONALE
A. Intermediate keratin filaments in the cytoplasm 1: Recall.
B. Bilateral nodular hyperplasia 2: Recall. Intermediate keratin filaments in the cytoplasm or
C. Solitary aldosterone-secreting adenoma crooke hyaline changes are seen in either endogenous or
D. Suppression of the HPA axis after low-dose exogenous Cushing syndrome. Lack of suppression of the
dexamethasone administration HPA axis is expected after DST.
3: Increased aldosterone secretion in primary
_____3. Which of the following conditions & characteristics are hyperaldosteronism manifests as hypertension and
paired incorrectly? hypokalemia. Hypokalemia was considered a mandatory
A. Aldosterone-secreting adenoma: spironolactone feature of primary hyperaldosteronism, but increasing
bodies numbers of normokalemic patients are now diagnosed.
B. Congenital adrenal hyperplasia: 21-hydroxylase 4: Recall.
deficiency 5: Recall.
C. Primary hyperaldosteronism: hypertension & 6: Recall.
hyperkalemia 7: Recall.
D. Secondary hyperaldosteronism: increased plasma 8: Pheochromocytomas are neoplasms composed of chromaffin
renin cells, which synthesize and release catecholamines & some
peptide hormones. These tumors are rare causes of surgically
_____4. A patient on chronic use of methylprednisolone correctable hypertension[Robbins & Cotran].
presented with weakness after he was unable to maintain his
prescribed dosage. Which pattern of adrenal insufficiency is
expected in the patient? REFERENCES
A. Primary acute adrenal insufficiency ● Jessica Abella, MD. Notes from Pathology of the Adrenal
B. Primary chronic adrenal insufficiency Glands.
C. Secondary acute adrenal insufficiency ● Kumar, V., Abbas, A. K., Aster, J. C., & Turner, J. R. (2021).
D. Secondary chronic adrenal insufficiency Robbins & Cotran pathologic basis of disease (10th ed.).
Elsevier Health Sciences.
_____5. Which of the following is expected in a patient with ● Xu, Simiao & Hu, Shuhong & Yu, Xuefeng & Zhang, Muxun &
primary chronic adrenal insufficiency? Yang, Yan. (2016). 17?-hydroxylase/17,20-lyase deficiency
A. At least 80% of the adrenal cortex has been in congenital adrenal hyperplasia: A case report. Molecular
compromised Medicine Reports. 15. 10.3892/mmr.2016.6029.
B. Volume retention & hypertension
C. Hyperpigmentation of the skin MNEMONICS
D. All of the above ● Pheochromocytoma: Rule of 10s
○ 10% are extra-adrenal
_____6. A small well-circumscribed, adrenocortical adenoma ○ 10% of sporadic type of adrenal pheochromocytomas
was observed on gross morphology. Which of the following will are bilateral
suggest a functional adenoma? ○ 10% are biologically malignant
A. The adjacent cortex is normal ○ 10% are not associated with hypertension
B. The adjacent cortex is atrophic
C. Presence of lipid
D. Yellowish brown
Diseases of the Adrenal Medulla
_____7. Which of the following is not true about
pheochromocytoma?
A. 10% are extra-adrenal
B. 10% of sporadic type of adrenal pheochromocytomas
are bilateral
C. 10% are biologically malignant
D. 10% are associated with hypertension
Page 10 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
SUMMARY
ADRENAL GLANDS
General Information Adrenal Cortex Adrenal Medulla
● Paired endocrine organs ● Outer layer ● Inner layer
● Located on the superior pole of each ● Mesodermally derived ● Neuroectodermally derived
kidney ● Secretes steroid hormones from cholesterol ● Secretes catecholamines
○ Zona Glomerulosa: Mineralocorticoids (Aldosterone) ● Darker color
○ Zona Fasciculata: Glucocorticoids (Cortisol)
○ Zona Reticularis: Sex steroids (Androgens)
● Yellowish
DISEASES OF THE ADRENAL CORTEX
ADRENOCORTICAL HYPERFUNCTION
General Information Morphology & Clinical Presentation Dexamethasone Suppression Test
● ⬆ glucocorticoids ● Pituitary changes: seen regardless of ● Assesses lack of suppression of the
● Exogenous cause: steroidal or cause HPA axis by exogenous
anti-inflammatory drugs ○ Crooke hyaline corticosteroids
○ ex. dexamethasone, ● Adrenal changes: depends on cause Types:
dexamethasone, ○ Exogenous: cortical atrophy ● Low dose: for screening or
methylprednisolone ○ Endogenous: diffuse hyperplasia confirmatory diagnosis
● Endogenous cause: ● Clinical Manifestation ● High dose: to categorize into
○ ACTH-dependent ○ Weight gain ACTH-dependent or -independent
➢ NE tumors ○ Truncal obesity Expected Findings:
Hypercortisolism
➢ Adenoma ○ Moon facies ● Pituitary Causes
(Cushing Syndrome)
➢ Cushing’s disease ○ Buffalo hump ○ Low dose → ⬆ ACTH (no effect)
➢ Ectopic ACTH ○ Abdominal striae → ⊕ urinary excretion
○ ACTH-independent ○ Weakness ○ High dose → feedback inhibition
➢ Adenoma ○ Hypertension (⬇ ACTH) → ⊖ urinary excretion
➢ Carcinoma ○ Glucose intolerance / secondary ● Ectopic ACTH: High or low dose: no
➢ McCline Albright DM effect on ACTH → fails to suppress
➢ Bilateral hyperplasia ○ Immunosuppression → infection excretion
➢ Carney complex ○ Mental disturbances ● Adrenal Tumor: ⬆ cortisol →
○ Menstrual disturbances, hirsutism feedback inhibition → ⬇ ACTH
in females
Bilateral Idiopathic Adrenocortical Neoplasm Familial hyperaldosteronism
Hyperaldosteronism (Conn Syndrome) (Glucocorticoid suppressible)
● Most common cause (60%) ● Second most common cause (35%) ● Rare underlying cause (5%)
● Bilateral nodular hyperplasia of the ● Commonly Conn Syndrome, but may ● Has four distinct subtypes (FH-I to
aldosterone-secreting zona also be an adrenocortical carcinoma FH-IV)
glomerulosa ● Aldosterone-secreting adenoma ● FH-I is the most common
● Diffuse and focal hyperplasia of (Conn Syndrome): ● Rearrangement in chromosome 8 →
Primary
cells resembling those of the ○ solitary, small (< 2cm diameter), CYP11B2 under the control of the
Hyperaldosteronism
normal zona glomerulosa and well-circumscribed; ACTH-responsive CYP11B1 gene
● Treatment: aldosterone antagonist ○ usually on the left gland; promoter → ACTH stimulates the
○ difficult to locate via imaging synthesis of aldosterone synthase
○ Characteristic feature: from the chimeric gene →
spironolactone bodies aldosterone production is under the
● Treatment: surgical excision control of ACTH, which is
suppressible by dexamethasone
● Usually an extra-adrenal cause ● Conditions:
● Response to activation if the ➢ Decreased renal perfusion
Secondary renin-angiotensin system ➢ Arterial hypovolemia
Hyperaldosteronism ● Characterized by increased levels of ➢ Pregnancy
plasma renin ● Treatment: correction of the underlying cause of the
hyperactivity of the renin-angiotensin system
Adrenocortical Neoplasms (CA) Congenital Adrenal Hyperplasia (CAH)
● More likely to be androgen-secreting ● Group of disorders that stem from several autosomal recessive, inherited
adrenal carcinomas than adenomas metabolic errors
● Morphologically identical to other ● Most common: 21-hydroxylase deficiency
Adrenogenital cortical neoplasms ● Blockage in mineralocorticoid and glucocorticoid pathways → steroid
Syndromes precursors channeled to sex steroid pathway → increased androgen
production and cortisol deficiency (which reduces feedback inhibition → ACTH
secretion → adrenal cortex hyperplasia)
● Morphology: adrenals are bilaterally hyperplastic; adrenal cortex is thickened,
nodular, and appears brown due to lipid depletion
Page 11 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
ADRENOCORTICAL INSUFFICIENCY / HYPOFUNCTION
Major Patterns Etiology Clinical Presentation Morphology
● Acute crisis in patients with chronic Waterhouse-Friderichsen syndrome Waterhouse-Friderichsen syndrome
adrenocortical insufficiency ● Overwhelming bacterial infection, ● Gross: Shrunken and hemorrhagic
● Sudden withdrawal of steroids in classically Neisseria meningitidis adrenal glands
patients maintained on exogenous septicemia ● Histology: Hemorrhage starts
corticosteroids ● Rapidly progressive hypotension within the medulla near thin-walled
Primary Acute AI
● As a result of massive adrenal leading to shock venous sinusoids, then suffuses
hemorrhage, which damages the ● DIC associated with purpuric rash peripherally into the cortex, often
adrenal cortex sufficiently of the skin leaving islands of recognizable
○ Waterhouse-Friderichsen cortical cells
syndrome ⭐
● Autoimmune adrenalitis ● Weakness / easy fatigability Tuberculous adrenalitis
○ more common ● Volume depletion & hypotension ● Histology: Central pinkish necrotic
Infections (TB, HIV, fungi) ● GI disturbances (vomiting or area, surrounded by lymphocytes,
⭐
●
Primary Chronic AI ○ Tuberculous adrenalitis diarrhea) epithelioid macrophages, &
(Addison Disease) ● Metastatic neoplasms ● Hyperpigmentation of the skin ⭐ Langhan giant cells
NOTE: For clinical manifestations of AI
to appear, at least 90% of the adrenal
cortex has been compromised ⭐
● Any disorder of the hypothalamus and pituitary, such as:
○ Metastatic cancer
Secondary AI ○ Infection
○ Infarction
○ Irradiation
ADRENOCORTICAL NEOPLASMS
Type Description Gross Morphology Histological Morphology
● Most common primary lesion in the ● Very small, well-circumscribed, ● Well-differentiated
adrenal cortex solitary lesion ● Eosinophilic cytoplasms
● Most are nonfunctional adenomas ● Yellowish brown in the cut section ● Vacuolated (intracytoplasmic lipids)
● Manifestations of functional ● For functional adenomas, the ● Nuclear pleomorphism
adenomas depend on the hormones adjacent cortex is atrophic
○ Aldosterone producing
Adrenocortical
adenomas
Adenoma
➢ Conn’s syndrome
○ Cortisol producing adenomas
➢ Cushing syndrome
○ Sex steroid hormone producing
adenomas
➢ Virilization, feminization
● More likely to be functional than ● Large, invasive, ill-defined lesions ● Cells are very disorganized
adenomas and are often associated ● Variegated in the cut section ● Pleomorphic nuclei and
with virilism or other clinical ● Hemorrhage, necrosis, and cysts hyperchromasia
Adrenocortical
manifestations of hyper-adrenalism ● Compresses the kidney ● Metastasis (ex. invasion of adrenal
Carcinoma
● Lesions tend to invade the vena vein)
cava, the adrenal vein, and ● Hemorrhage
lymphatics
DISEASES OF THE ADRENAL MEDULLA
Description Gross Morphology Histological Morphology
● Tumors of the chromaffin cells, ● It has a wide array of morphologic ● Nests of cells (Zellballen pattern)
resulting in the release of excessive features (can be very small lesion or with abundant cytoplasm
catecholamines to large hemorrhagic masses) ● Compressed adrenal cortex
● Rule of 10’s ⭐ ● Compressed adrenal cortex ● Electron micrograph shows
Pheochromocytoma ○ 10% are extra-adrenal ● Gray tan color membrane-bound neurosecretory
○ 10% of sporadic type of adrenal ● Well-circumscribed granules
pheochromocytomas are bilateral ● Dark brown using potassium
○ 10% are biologically malignant dichromate solution
○ 10% are not associated with
hypertension
Page 12 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
GPT 5.02 Pathology of the Adrenal Gland
APPENDIX
Appendix A: Schematic diagram of the adrenal steroidogenesis biosynthesis pathway.
Source: Xu, et al (2016)
Page 13 of 13 | TH: SOTTO, N. | GPT TG 6 | REGALA, SY, G., TENG, TIDOSO
You might also like
- Pathophysiology in Liver CirrhosisDocument4 pagesPathophysiology in Liver CirrhosisCyrus Ortalla RobinNo ratings yet
- Fundamentals of Nursing NCLEX Practice Quiz 9 (25 Questions) - NurseslabsDocument26 pagesFundamentals of Nursing NCLEX Practice Quiz 9 (25 Questions) - NurseslabsCHINGANGBAM ANJU CHANUNo ratings yet
- Adrenal ColorDocument35 pagesAdrenal ColorAnonymous oOofKbmPTiNo ratings yet
- Endocrine Disorders Cont... (For ADRENAL GLAND)Document4 pagesEndocrine Disorders Cont... (For ADRENAL GLAND)Ernie G. Bautista II, RN, MD100% (3)
- L46 - Adrenal DisordersDocument30 pagesL46 - Adrenal DisordersCharles AntonyNo ratings yet
- Adrenal Glands Clinical Chemistry (Laboratory) : Lesson 7Document5 pagesAdrenal Glands Clinical Chemistry (Laboratory) : Lesson 7Cherry Ann ColechaNo ratings yet
- Title of Lecture: AY 2018-2019 1 Shifting Exam Instructor's Name (Name, MD, Other-Post-Nominals) Mm/Dd/YyyyDocument5 pagesTitle of Lecture: AY 2018-2019 1 Shifting Exam Instructor's Name (Name, MD, Other-Post-Nominals) Mm/Dd/YyyyMarielle MalabananNo ratings yet
- Pedia-Adrenal Gland DisordersDocument5 pagesPedia-Adrenal Gland DisordersEmerson QuimbaNo ratings yet
- Endocrine DisordersDocument27 pagesEndocrine DisordersHsay AyitehgNo ratings yet
- What Are Adrenal Glands?: NCM 116: Medical Surgical Nursing Adrenal DisordersDocument9 pagesWhat Are Adrenal Glands?: NCM 116: Medical Surgical Nursing Adrenal DisordersGabrielle AcaboNo ratings yet
- Adrenal Hyperfunction: Cushing'S SyndromeDocument10 pagesAdrenal Hyperfunction: Cushing'S SyndromeJoaquim RodriguezNo ratings yet
- Adrenal Gland PathologyDocument6 pagesAdrenal Gland PathologyRami ShishanNo ratings yet
- Kuliah AdrenalDocument32 pagesKuliah AdrenalNindhyana Diwaratri R100% (1)
- AdrenalDocument9 pagesAdrenalNada MuchNo ratings yet
- Tertiary Adrenocortical InsufficiencyDocument8 pagesTertiary Adrenocortical InsufficiencysarathNo ratings yet
- Adrenal Disorders in ChildrenDocument39 pagesAdrenal Disorders in ChildrenCorina OngNo ratings yet
- Chem+Path +adrenal+2021 H+VreedeDocument39 pagesChem+Path +adrenal+2021 H+VreedeKamogelo AlbertNo ratings yet
- Gangguan Kel. AdrenalDocument16 pagesGangguan Kel. AdrenalInna Nur Fitri DahliyantiNo ratings yet
- AdrenocorticosteroidsDocument25 pagesAdrenocorticosteroidsAbdullah RawashdehNo ratings yet
- Kelompok 3 Casing SindromeDocument9 pagesKelompok 3 Casing SindromeChristinaTriAstutiPauNo ratings yet
- Principles of Clinical EndocrinologyDocument127 pagesPrinciples of Clinical EndocrinologyMNo ratings yet
- Anatomy & Physiology: CRH ActhDocument6 pagesAnatomy & Physiology: CRH ActhAmoroso, Marian Corneth D.No ratings yet
- Cushing SyndromeDocument12 pagesCushing SyndromeAmoroso, Marian Corneth D.No ratings yet
- Addison's Disease FileDocument25 pagesAddison's Disease FileZyla KrisshaNo ratings yet
- Addison's Disease (Primary Adrenal Insufficiency)Document5 pagesAddison's Disease (Primary Adrenal Insufficiency)sunnnydayNo ratings yet
- Week 11. Endocrinology 3Document17 pagesWeek 11. Endocrinology 3MACOB, ETHELHYN JHANENo ratings yet
- (MS II Lec) Endocrine System2Document8 pages(MS II Lec) Endocrine System2IlawNo ratings yet
- A Dre No CorticoidsDocument2 pagesA Dre No CorticoidsAlbert CorderoNo ratings yet
- 2021 COMET Krisis Adrenal (Compatibility Mode) (1) - Pages-1-27Document27 pages2021 COMET Krisis Adrenal (Compatibility Mode) (1) - Pages-1-27Octo IndradjajaNo ratings yet
- Insuficiencia AdrenalDocument5 pagesInsuficiencia AdrenalLuciana RafaelNo ratings yet
- Endocrine System: THE Adrenal GlandsDocument50 pagesEndocrine System: THE Adrenal GlandsAbdel Aziz NazihNo ratings yet
- Adrenal Gland NUBDocument21 pagesAdrenal Gland NUBpvsmj5kdk4No ratings yet
- Adrenal InsufficiencyDocument25 pagesAdrenal InsufficiencyMustafa Salam M.NooriNo ratings yet
- Adrenal GlandDocument22 pagesAdrenal GlandSurvey IndiaNo ratings yet
- Adrenal Diseases: Types Aetiology Diagnosis Complications TreatmentDocument29 pagesAdrenal Diseases: Types Aetiology Diagnosis Complications Treatmentgani7222No ratings yet
- Investigation and Management of Adrenal Disease: The Adrenal Medulla Synthesizes The Catecholamines AdrenalineDocument6 pagesInvestigation and Management of Adrenal Disease: The Adrenal Medulla Synthesizes The Catecholamines AdrenalineMarlin Berliannanda TawayNo ratings yet
- Adrenal Function: T. Creighton Mitchell, A. Wayne MeikleDocument19 pagesAdrenal Function: T. Creighton Mitchell, A. Wayne MeikleWho KnowsNo ratings yet
- Pituitary Tumor & AcromegalyDocument32 pagesPituitary Tumor & Acromegalysam840720No ratings yet
- Cushingssyndrome 180217104318Document14 pagesCushingssyndrome 180217104318Zakaria FarahNo ratings yet
- CUSHINGDocument12 pagesCUSHINGCarlos alvarezNo ratings yet
- Adrenal Gland Gonadocorticoids AtfDocument2 pagesAdrenal Gland Gonadocorticoids Atf2ymyccmvfcNo ratings yet
- Cushing Syndrome Addisons 1Document6 pagesCushing Syndrome Addisons 1Czarena Ysabelle PayotNo ratings yet
- Canine Hypoadrenocorticism Overvew Diagnosis and Treatment LolattiDocument6 pagesCanine Hypoadrenocorticism Overvew Diagnosis and Treatment LolattiAna Clara SevasteNo ratings yet
- Adrenal Gland: by M. Jyotirmayee Sister Tutor, N.T.IDocument23 pagesAdrenal Gland: by M. Jyotirmayee Sister Tutor, N.T.IlindaNo ratings yet
- Endocrine Drugs by JIS DumbriqueDocument10 pagesEndocrine Drugs by JIS DumbriqueYangyang R. AzradNo ratings yet
- Screenshot 2023-04-26 at 12.52.44 PMDocument1 pageScreenshot 2023-04-26 at 12.52.44 PMRenadNo ratings yet
- DM by AsheDocument73 pagesDM by Asheabduljewad arageNo ratings yet
- ENDOCRINE DISORDERS- Adrenal Gland DisordersDocument19 pagesENDOCRINE DISORDERS- Adrenal Gland Disordersalwanh878No ratings yet
- Adrenal Gland Cushing Disease Adrenal Crisis: SectionDocument44 pagesAdrenal Gland Cushing Disease Adrenal Crisis: SectioniikNo ratings yet
- EndocrineDocument46 pagesEndocrineMike GNo ratings yet
- AdrenalpathologyDocument81 pagesAdrenalpathologyjoavchNo ratings yet
- Insuficiencia AdrenalDocument24 pagesInsuficiencia Adrenalalejandro.marglez97No ratings yet
- Addison's Disease - Diabetes Insipidus 116Document3 pagesAddison's Disease - Diabetes Insipidus 116Rose Ann BollerosNo ratings yet
- Adrenal Gland DisordersDocument24 pagesAdrenal Gland Disorderssimona mariana dutuNo ratings yet
- Congenital Adrenal Hyperplasia:: Diagnosis, Evaluation, and ManagementDocument11 pagesCongenital Adrenal Hyperplasia:: Diagnosis, Evaluation, and Managementsabachannel456No ratings yet
- Safety of Medications and Hormones UsedDocument12 pagesSafety of Medications and Hormones UsedandreNo ratings yet
- Chap3 The Adrenal GlandDocument20 pagesChap3 The Adrenal GlandSharon GabrielNo ratings yet
- Adrenal DiseasesDocument35 pagesAdrenal Diseasesmy Lord JesusNo ratings yet
- 052 - Endocrinology Physiology) Adrenal Gland OverviewDocument2 pages052 - Endocrinology Physiology) Adrenal Gland Overviewیوسف رمضانNo ratings yet
- Midterms - NCMB 316 Disorders PDFDocument21 pagesMidterms - NCMB 316 Disorders PDFLouise TorresNo ratings yet
- Addison’s Disease, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandAddison’s Disease, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Clinical Simulation Feb. 20 J 2024Document4 pagesClinical Simulation Feb. 20 J 2024Jonah Mae SampangNo ratings yet
- Magis Notes Pre-Week Day 2Document209 pagesMagis Notes Pre-Week Day 2Jonah Mae SampangNo ratings yet
- 2022 Alf LMT - Labor LawDocument31 pages2022 Alf LMT - Labor LawJonah Mae SampangNo ratings yet
- Doctrine Pool SPL FinalsDocument25 pagesDoctrine Pool SPL FinalsJonah Mae SampangNo ratings yet
- 2 - (2022 UP LAW BOC) Labor Law LMTsDocument10 pages2 - (2022 UP LAW BOC) Labor Law LMTsJonah Mae SampangNo ratings yet
- 1 - (2022 UP LAW BOC) Political Law LMTsDocument13 pages1 - (2022 UP LAW BOC) Political Law LMTsJonah Mae Sampang50% (2)
- Agra Election Law 05.22.2021Document81 pagesAgra Election Law 05.22.2021Jonah Mae SampangNo ratings yet
- Plague in Early Islamic History - Michael W. DolsDocument14 pagesPlague in Early Islamic History - Michael W. DolsAminodin SaripNo ratings yet
- Ebook Goodman Gilmans The Pharmacological Basis of Therapeutics PDF Full Chapter PDFDocument67 pagesEbook Goodman Gilmans The Pharmacological Basis of Therapeutics PDF Full Chapter PDFyolanda.dulle942100% (34)
- E Sports NeurotrackerDocument1 pageE Sports Neurotrackeralbercarpio89No ratings yet
- Chapter 3 Levenson. Coping With IllnessDocument40 pagesChapter 3 Levenson. Coping With Illnessjodalo.jdlrNo ratings yet
- Antiparasitic DrugsDocument7 pagesAntiparasitic DrugsPeter MjeeNo ratings yet
- Introduction To ECG RhythmsDocument59 pagesIntroduction To ECG RhythmsIvona RagužNo ratings yet
- Path Endocrine OutlineDocument46 pagesPath Endocrine Outlineaya derweshNo ratings yet
- Ultrasonography of The Neck: O. Taeymans, DVM, Dip ECVDIDocument73 pagesUltrasonography of The Neck: O. Taeymans, DVM, Dip ECVDIKSNo ratings yet
- Aplastic Anemia: Edited: Dr. Dairion Gatot SP - PD-KHOMDocument11 pagesAplastic Anemia: Edited: Dr. Dairion Gatot SP - PD-KHOMrubyniNo ratings yet
- Chiari MalformationDocument3 pagesChiari MalformationAloysius RodriguesNo ratings yet
- The Persistent Stigma and Disregard For Mental Health in Sri LankaDocument3 pagesThe Persistent Stigma and Disregard For Mental Health in Sri Lankadevmini herathNo ratings yet
- Oral Anticoagulation in Patients With Chronic Liver DiseaseDocument23 pagesOral Anticoagulation in Patients With Chronic Liver DiseaseSophia PapathanasiouNo ratings yet
- Quiz Mrs DallowayDocument4 pagesQuiz Mrs DallowayAna100% (1)
- Baseer Price ListDocument2 pagesBaseer Price ListUmarkNo ratings yet
- Mps Individual Temp PermitsDocument5 pagesMps Individual Temp PermitspsetoNo ratings yet
- Vol5 Issue4 02 PDFDocument3 pagesVol5 Issue4 02 PDFRyan RachmawanNo ratings yet
- SUMAOANG - Maalox Drug StudyDocument4 pagesSUMAOANG - Maalox Drug StudyMina SumaoangNo ratings yet
- NCP Systemic Viral Infection SVIDocument4 pagesNCP Systemic Viral Infection SVIPavel Kolesnikov100% (1)
- Mental RetardationDocument2 pagesMental RetardationAman SahaNo ratings yet
- MicroPara Lecture 6Document24 pagesMicroPara Lecture 6Pearl NoconNo ratings yet
- EPISTAXISDocument2 pagesEPISTAXISRUTH RosilinNo ratings yet
- 4 - 26 - 32 - Ibrahim Et AlDocument7 pages4 - 26 - 32 - Ibrahim Et AlUMYU Journal of Microbiology Research (UJMR)No ratings yet
- Empirical Antibiotic Therapy in Children: Clinical GuidelineDocument2 pagesEmpirical Antibiotic Therapy in Children: Clinical GuidelineAna-Mihaela BalanuțaNo ratings yet
- MOPH Guideline - Skin and Soft Tissue Infections v0.3 - Quality CheckDocument68 pagesMOPH Guideline - Skin and Soft Tissue Infections v0.3 - Quality CheckEmna DerbelNo ratings yet
- Chapter 4 - Servsafe - 6e Edited PDFDocument4 pagesChapter 4 - Servsafe - 6e Edited PDFdevvy anneNo ratings yet
- Preterm Labour (Prematurity) : DR - Abdulkarim Ahmed Mohamud MBCHB (Ust), Mmed (Uon)Document17 pagesPreterm Labour (Prematurity) : DR - Abdulkarim Ahmed Mohamud MBCHB (Ust), Mmed (Uon)PeterNo ratings yet
- Home Nursing and CaregivingDocument78 pagesHome Nursing and CaregivingJake Arizapa100% (2)
- NACC Practice Exam - Answer (PDF) - Course SidekickDocument107 pagesNACC Practice Exam - Answer (PDF) - Course SidekickeguasglobalresourcesltdNo ratings yet