Professional Documents
Culture Documents
Lupton 1988
Lupton 1988
Uploaded by
Amina GoharyCopyright:
Available Formats
You might also like
- Chapter 72. Case StudiesDocument40 pagesChapter 72. Case Studiesstawberry shortcake100% (1)
- Lesson Plan On Shock and HaemorrhageDocument35 pagesLesson Plan On Shock and HaemorrhageDr-Sanjay Singhania88% (16)
- Hasan 2021Document4 pagesHasan 2021Amina GoharyNo ratings yet
- Intravenous Immunoglobulin in Neonates With RhesusDocument9 pagesIntravenous Immunoglobulin in Neonates With RhesusGabriel BuftiaNo ratings yet
- Vries 2007Document6 pagesVries 2007BrîndușaPetcariuNo ratings yet
- Estudio de MariDocument6 pagesEstudio de MarianjidisNo ratings yet
- Pediatrics JournalDocument9 pagesPediatrics JournalDokter KarisNo ratings yet
- Etude Transf PQDocument10 pagesEtude Transf PQLincan RoxanaNo ratings yet
- Curley 2018 Platelet Transfusion Threshols in NeonatesDocument11 pagesCurley 2018 Platelet Transfusion Threshols in NeonatesEllya Latifah IlyasNo ratings yet
- DMV Cipe Di AtriaDocument6 pagesDMV Cipe Di AtriaAngélica ContrerasNo ratings yet
- Causes, Severity and Outcome of Neonatal Thrombocytopenia in Hi-Tech Medical College and Hospital, BhubaneswarDocument4 pagesCauses, Severity and Outcome of Neonatal Thrombocytopenia in Hi-Tech Medical College and Hospital, BhubaneswarInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyAlif ZainalNo ratings yet
- Articulo HICDocument6 pagesArticulo HICNelly GonzalezNo ratings yet
- Intraventricular HaemorrhageDocument9 pagesIntraventricular HaemorrhageTriponiaNo ratings yet
- Benson Multicentre 1986Document4 pagesBenson Multicentre 1986Dian NovitasariNo ratings yet
- Pediatric Outcome in Rhesus Hemolytic Disease Treated With and Without Intrauterine TransfusionDocument4 pagesPediatric Outcome in Rhesus Hemolytic Disease Treated With and Without Intrauterine TransfusionCatia CorreaNo ratings yet
- Normal Values For Mature and Immature in Very Preterm BabiesDocument3 pagesNormal Values For Mature and Immature in Very Preterm BabiesSukma EffendyNo ratings yet
- Noradrenalina en PrematurosDocument7 pagesNoradrenalina en PrematurosnzunaNo ratings yet
- Ultrasonido Doppler Temprano AMSDocument7 pagesUltrasonido Doppler Temprano AMSKaren Marbelly OrozcoNo ratings yet
- State University of New York, Downstate Medical Center, USADocument2 pagesState University of New York, Downstate Medical Center, USAronynoorNo ratings yet
- Transcranial Ultrasound Doppler Parameters in Cerebral Vessels May Predict Intracerebral Hemorrhage in Preterm NewbornsDocument7 pagesTranscranial Ultrasound Doppler Parameters in Cerebral Vessels May Predict Intracerebral Hemorrhage in Preterm Newbornsrezza mochamadNo ratings yet
- Transcranial Ultrasound Doppler Parameters in CereDocument7 pagesTranscranial Ultrasound Doppler Parameters in CereImin BuntaraNo ratings yet
- 1 s2.0 S1028455922001632 MainDocument4 pages1 s2.0 S1028455922001632 MainAditi SoniNo ratings yet
- Clinical StudyDocument6 pagesClinical StudyAndreiMunteanuNo ratings yet
- Thrombocytopenia in Late Preterm and Term Neonates After Perinatal AsphyxiaDocument10 pagesThrombocytopenia in Late Preterm and Term Neonates After Perinatal AsphyxiaTammy Utami DewiNo ratings yet
- Clinical Utility of Colour Doppler For Diagnosis of Adverse Perinatal Outcome in IUGR and PIHDocument4 pagesClinical Utility of Colour Doppler For Diagnosis of Adverse Perinatal Outcome in IUGR and PIHnjmdrNo ratings yet
- Importance of Ductus Venosus Doppler in Prediction of Perinatal Morbidity and MortalityDocument6 pagesImportance of Ductus Venosus Doppler in Prediction of Perinatal Morbidity and MortalityInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 1010 FTP PDFDocument5 pages1010 FTP PDFHerry SasukeNo ratings yet
- Irv 12375Document6 pagesIrv 12375Marella DevinaNo ratings yet
- Umbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialDocument5 pagesUmbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialAffah MustafaNo ratings yet
- J Journal of Pediatrics Volume 125 Issue 4 October 1994 Pages 603-606Document4 pagesJ Journal of Pediatrics Volume 125 Issue 4 October 1994 Pages 603-606ElaineNo ratings yet
- Early Enteral Feeding and Nosocomial Sepsis in Very Low Birthweight InfantsDocument4 pagesEarly Enteral Feeding and Nosocomial Sepsis in Very Low Birthweight InfantsaripbudiboyNo ratings yet
- Ultrasound in Obstet Gyne - 2002 - Senat - Management of Single Fetal Death in Twin To Twin Transfusion Syndrome A RoleDocument4 pagesUltrasound in Obstet Gyne - 2002 - Senat - Management of Single Fetal Death in Twin To Twin Transfusion Syndrome A RoleBramantyo Dwi HandjonoNo ratings yet
- Incidence of Periventricular/intraventricular Hemorrhage in Very Low Birth Weight Infants: A 15-Year Cohort StudyDocument7 pagesIncidence of Periventricular/intraventricular Hemorrhage in Very Low Birth Weight Infants: A 15-Year Cohort StudyGusBlomkvistSomocurioNo ratings yet
- The Effects Aedv and RedvDocument7 pagesThe Effects Aedv and RedvTresa ivaniNo ratings yet
- Slide Obgyn Jurnal ReadingDocument18 pagesSlide Obgyn Jurnal Readingari naNo ratings yet
- 2016 Relacion ANEMIA Con NEC y TransfusionesDocument9 pages2016 Relacion ANEMIA Con NEC y TransfusionesnadisjaviNo ratings yet
- Leukopenia and Neutropenia As A Predictors of Neonatal SepsisDocument8 pagesLeukopenia and Neutropenia As A Predictors of Neonatal SepsisYandiNo ratings yet
- E548 FullDocument7 pagesE548 FullBimo Aryo TejoNo ratings yet
- BR J Haematol - 2017 - Rühle - Advances in Predicting Venous Thromboembolism Risk in ChildrenDocument12 pagesBR J Haematol - 2017 - Rühle - Advances in Predicting Venous Thromboembolism Risk in ChildrenKarina CamachoNo ratings yet
- Nej M 200009073431001Document8 pagesNej M 200009073431001Asri Ani NurchasanahNo ratings yet
- Neutro PhiliaDocument10 pagesNeutro PhiliaMARIA DE LOS ANGELES MARTINEZ VIRENo ratings yet
- NeutrophiliaDocument10 pagesNeutrophiliamaria martinezNo ratings yet
- Inferior Vena Cava Diameter A Useful Method For EsDocument5 pagesInferior Vena Cava Diameter A Useful Method For EsmalisalukmanNo ratings yet
- Cap 2023Document9 pagesCap 2023Neonatología HGO4No ratings yet
- Journal Medicine: The New EnglandDocument8 pagesJournal Medicine: The New EnglandHam jungNo ratings yet
- Journal 6Document18 pagesJournal 6Sebastian SetiahardjaNo ratings yet
- Murphy2002 Posthaemorrhagic Ventricular DilatationDocument6 pagesMurphy2002 Posthaemorrhagic Ventricular DilatationModou NianeNo ratings yet
- Fetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaDocument4 pagesFetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaMuhammad AdithiaNo ratings yet
- Am J Perinatol. 2007 Jun24 (6) 373-6Document4 pagesAm J Perinatol. 2007 Jun24 (6) 373-6Ivan Osorio RuizNo ratings yet
- Streptokinase in The Treatment of Pleural Controlled Trial of IntrapleuralDocument7 pagesStreptokinase in The Treatment of Pleural Controlled Trial of IntrapleuraltomgasoneNo ratings yet
- Management of Neonatal Hypotension and ShockDocument7 pagesManagement of Neonatal Hypotension and ShockntnquynhproNo ratings yet
- Management of Neonatal Hypotension and ShockDocument7 pagesManagement of Neonatal Hypotension and ShockntnquynhproNo ratings yet
- Nirs Preterm ScreeenDocument6 pagesNirs Preterm ScreeenLissaberti AmaliahNo ratings yet
- Andrea Surányi, Ábel Altorjay, László Kaiser, Tibor Nyári, Gábor NémethDocument9 pagesAndrea Surányi, Ábel Altorjay, László Kaiser, Tibor Nyári, Gábor NémethfujimeisterNo ratings yet
- Articles: BackgroundDocument10 pagesArticles: BackgroundKarina CamachoNo ratings yet
- NLR - Neonatal SepsisDocument6 pagesNLR - Neonatal SepsisGlen LazarusNo ratings yet
- 194 265 1 SMDocument5 pages194 265 1 SMAdkhiatul MuslihatinNo ratings yet
- 2009 DV Aortic Isthmus FGR Blood Flow GratacosDocument5 pages2009 DV Aortic Isthmus FGR Blood Flow GratacosRibeiro SáNo ratings yet
- Management and Complications of Intraventricular Hemorrhage in The NewbornDocument10 pagesManagement and Complications of Intraventricular Hemorrhage in The NewbornAnonymous Xmb6QQvRNo ratings yet
- Ductus Venosus Blood Velocity and The Umbilical Artery Circulation in The Seriously Growth Retarded FoetusDocument6 pagesDuctus Venosus Blood Velocity and The Umbilical Artery Circulation in The Seriously Growth Retarded FoetusSaikatBanerjeeNo ratings yet
- Diabetes in Children and Adolescents: A Guide to Diagnosis and ManagementFrom EverandDiabetes in Children and Adolescents: A Guide to Diagnosis and ManagementNo ratings yet
- Cureus 0015 00000038985Document6 pagesCureus 0015 00000038985Amina GoharyNo ratings yet
- PDF 8Document11 pagesPDF 8Amina GoharyNo ratings yet
- PDF 3Document5 pagesPDF 3Amina GoharyNo ratings yet
- Consensus Statement: The 16th Annual Western Canadian Gastrointestinal Cancer Consensus Conference Saskatoon, Saskatchewan September 5-6, 2014Document12 pagesConsensus Statement: The 16th Annual Western Canadian Gastrointestinal Cancer Consensus Conference Saskatoon, Saskatchewan September 5-6, 2014Amina GoharyNo ratings yet
- Prognostic Value of Metabolic Tumor Burden On F-FDG PET in Nonsurgical Patients With Non-Small Cell Lung CancerDocument12 pagesPrognostic Value of Metabolic Tumor Burden On F-FDG PET in Nonsurgical Patients With Non-Small Cell Lung CancerAmina GoharyNo ratings yet
- 4Document20 pages4Amina GoharyNo ratings yet
- Craniopharyngiomas of The Third Ventricle: Trans-Lamina Terminalis ApproachDocument9 pagesCraniopharyngiomas of The Third Ventricle: Trans-Lamina Terminalis ApproachAmina GoharyNo ratings yet
- CBU 5th Year Exam Paper 1 2017Document13 pagesCBU 5th Year Exam Paper 1 2017Homeground entertainment100% (3)
- Disseminated Intravascular Coagulopathy DICDocument24 pagesDisseminated Intravascular Coagulopathy DICMassimiliano MalerbaNo ratings yet
- Surgery: 1) Preoperative Assessment of HemostasisDocument13 pagesSurgery: 1) Preoperative Assessment of HemostasisIruthayanathar Andru NitharsanNo ratings yet
- Fluid Resuscitation in Haemorrhagic ShockDocument9 pagesFluid Resuscitation in Haemorrhagic ShockbashiruaminuNo ratings yet
- HEMA2 - Bleeding Time Written ReportDocument10 pagesHEMA2 - Bleeding Time Written ReportMarjorie GabalunosNo ratings yet
- Rle Skills Lab Rubrics GuidesDocument5 pagesRle Skills Lab Rubrics GuidesPrince Joshua Grande AngelesNo ratings yet
- B - Braun: Nutri Ex® Lipid SpecialDocument2 pagesB - Braun: Nutri Ex® Lipid SpecialAbhie Fajri MierzanNo ratings yet
- Bleeding After TonsillectomyDocument7 pagesBleeding After Tonsillectomyking_petarNo ratings yet
- First Year Complete Physiology MCQ Bank by Team DR Of2027-28Document284 pagesFirst Year Complete Physiology MCQ Bank by Team DR Of2027-28ammejan10100% (2)
- Jurnal 1Document7 pagesJurnal 1Nur WahyuniNo ratings yet
- NCP RosteDocument2 pagesNCP RosteRoyce Vincent TizonNo ratings yet
- Bleeding Disorders 1 - DR - Kamal MokbelDocument13 pagesBleeding Disorders 1 - DR - Kamal MokbelRawan E. SaeedNo ratings yet
- Nursing Care Plan Spontaneous AbortionDocument2 pagesNursing Care Plan Spontaneous AbortionAbigael Rubio de LeonNo ratings yet
- Medical History Report Medical Prescreen Questionnaire: Philippine National Police Health ServiceDocument4 pagesMedical History Report Medical Prescreen Questionnaire: Philippine National Police Health ServicejovelonderizaNo ratings yet
- Etamsylate DS Meppo2010 PDFDocument3 pagesEtamsylate DS Meppo2010 PDFAqmarlia PutriNo ratings yet
- Shock ChartsDocument2 pagesShock ChartsforminskoNo ratings yet
- Warf Side EffectsDocument6 pagesWarf Side EffectsPankaj SharmaNo ratings yet
- BleedingDocument14 pagesBleedingRhomizal MazaliNo ratings yet
- Chapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingDocument3 pagesChapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingKn VelasquezNo ratings yet
- Trauma Induced Coagulopathy What You Need To Know.1Document7 pagesTrauma Induced Coagulopathy What You Need To Know.1llucaspilonettoNo ratings yet
- Collection of Blood Sample From Experimental AnimalsDocument12 pagesCollection of Blood Sample From Experimental AnimalslovehopeNo ratings yet
- cc2851 (PDF - Io)Document15 pagescc2851 (PDF - Io)Aquardoleo ValentinoNo ratings yet
- Emcase 04 Feb 2019 Dr. KometDocument56 pagesEmcase 04 Feb 2019 Dr. KometKomet Rama DaudNo ratings yet
- Preparation For Giving First AidDocument11 pagesPreparation For Giving First AidLarisa HurtadoNo ratings yet
- StentsDocument11 pagesStentsIbrahim Ramadan Eltorky0% (2)
- 9 - Post-OP Management and ComplicationsDocument57 pages9 - Post-OP Management and ComplicationsThon JustineNo ratings yet
- Causes: Polycythemia VeraDocument15 pagesCauses: Polycythemia VeraMaria VisitacionNo ratings yet
- Blood Bank International Standard ISBT Science Series - 2008 - Hardwick - Blood ProcessingDocument29 pagesBlood Bank International Standard ISBT Science Series - 2008 - Hardwick - Blood ProcessingShan AhmadNo ratings yet
Lupton 1988
Lupton 1988
Uploaded by
Amina GoharyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lupton 1988
Lupton 1988
Uploaded by
Amina GoharyCopyright:
Available Formats
Reduced Platelet Count as a Risk Factor
for Intraventricular Hemorrhage
Brian A. Lupton, MB; Alan Hill, MD, PhD; Michael F. Whitfield, MD;
Cedric J. Carter, MB; Louis D. Wadsworth, MB; Elke H. Roland, MD
\s=b\ The role of thrombocytopenia as a occurrence of IVH,3-6 whereas others perinatal asphyxia, presence or absence of
risk factor for intraventricular hemor- have failed to demonstrate this asso¬ pneumothorax, and outcome. Perinatal as¬
rhage in infants of very low birth weight ciation.7·8 In the light of this contro¬ phyxia was defined as a fetal scalp or an
is unclear. This study investigates the umbilical cord pH of less than 7.2, or Apgar
versy, the purpose of this study is to
relationship between the lowest platelet determine the role of reduced platelet scores under 3 at one minute or under 6 at
count and the occurrence of intraven- five minutes, or all of these. Four patients
counts in the genesis of IVH in a large
tricular hemorrhage in 302 consecu- with platelet counts less than 20 x ÎO'/L
tively admitted infants with birth weights population of infants of very low birth received platelet transfusions. Indometha-
under 1500 g. Intraventricular hemor- weight (VLBW). cin sodium trihydrate was administered to
rhage, which occurred in 90 infants METHODS two patients only during the first 4 days of
(29.8%), was correlated with the lowest Patient Population life for the treatment of symptomatic pat¬
platelet count obtained during the first ent ductus arteriosus and was not used
4 days of life. In 27 infants with intraven- The patient population comprised 302
prophylactically.
tricular hemorrhage, the lowest platelet infants with birth weights less than 1500 g
count was less than 100\m=x\109/L. Statis- who were admitted consecutively to the
tical analysis of the data demonstrated Neonatal Intensive Care Unit at British Diagnosis of IVH
that reduced platelet count was not as- Columbia's Children's Hospital, Vancouver,
sociated significantly with intraventric- during a period of 18 months. The mean Intraventricular hemorrhage was diag¬
ular hemorrhage. Similarly, the severity gestational age was 27.5 weeks (range, nosed by routine ultrasound scanning on
of intraventricular hemorrhage did not 23 to 35 weeks) and the mean (±SD) days 4 and 14 of life with a mechanical
correlate with the lowest platelet count. birth weight was 1076 ±246 g. Infants sector scanner (Diasonics ADA 400)
were admitted during the first day of equipped with a 7.5-MHz transducer. Scans
These data suggest that a reduced plate-
life and received standard treatment in were performed by a radiologist who was
let count does not play a major role in
the pathogenesis of intraventricular terms of ventilation, circulatory support, unaware of the infant's platelet count. The
and parenteral nutrition. The following IVH was graded as I to IV according to
hemorrhage in infants of very low birth
weight. variables, which have been implicated in the system of Papile et al,9 adapted for use
the pathogenesis of IVH, were recorded: with ultrasound scanning. Grades III and
(AJDC 1988;142:1222-1224)
birth weight, mode and location of delivery, IV were considered to represent severe
condition at delivery, respiratory distress, IVH.
TVTany factors have been implicated
in the pathogenesis of intraven¬
tricular hemorrhage (IVH) in the pre¬
term infant.1·2However, the role of
reduced platelet count in this context
remains unclear. Thus, several studies
have suggested a direct relationship
between low platelet count and the
Accepted for publication June 12, 1988.
From the Divisions of Neurology (Drs Lupton,
Hill, and Roland) and Neonatology (Dr Whit-
field), Department of Pediatrics, and the Division
of Hematopathology, Department of Pathology
(Drs Carter and Wadsworth), University of Brit-
ish Columbia, and the British Columbia's
Children's Hospital, Vancouver.
Presented in part at the meeting of the Amer-
ican Pediatric Society/Society for Pediatric Re-
search, Anaheim, Calif, May 1, 1987.
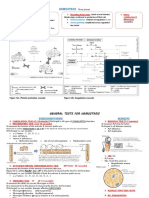
Reprint requests to Division of Neurology, Platelet Count 109/L
British Columbia's Children's Hospital, 4480 Oak
St, Vancouver, British Columbia, Canada Distribution of lowest platelet count and intraventricular hemorrhage. Solid bars indicate
V6H3V4 (Dr Hill). presence of, and striped bars, absence of, intraventricular hemorrhage.
Downloaded From: http://archpedi.jamanetwork.com/ by a Michigan State University User on 06/18/2015
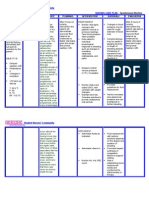
Table 1.—Correlation of Intraventricular Hemorrhage (IVH) With Lowest
the first day of life in all infants and
Platelet Count* were repeated between age 2 and 4
days in 215 infants (71%) who had
Lowest Platelet Count x 10VL medical complications. In 27 infants
No. of
Patients <100 100-150 151-200 >200 (9%), the LPC was less than
IVH (n 302)
=
(n 27)
=
(n 26)
=
(n 72)
=
(n 177)
= 100 109/L; in 26 infants (9%), the LPC
Present 90 7 9 27 47 was between 100 and 150 x 10VL; and
Absent 212 20 17 45 130 in 72 infants (24%), the LPC was
*X2 3.41,df=3;P
= =
.33. between 151 and 200xl09/L. In the
remaining 177 infants (59%), all
platelet counts were greater than
Table 2.—Correlation Between Grade of Intraventricular Hemorrhage (IVH) and 200 x 10VL.
Lowest Platelet Count* The distribution of the LPC in the
Lowest Platelet Count 10"/L
entire study population and in the
No. of infants who developed IVH is dis¬
IVH
Patients
(n 302)
=
<100
(n 27)
=
100-150
(n 26)
=
151-200
(n 72)
=
>200
(n 177)
=
played in the Figure. There was no
16 46
apparent difference between the inci¬
Absent 212 20 130
dence of IVH in infants with platelet
Present counts less than 100, 100 to 150, and
Grades I and II 40 2 11 23
150 to 200 x 109/L as compared with
Grades III and IV 50 5 15 24
the incidence in the remaining infants
0.47, df=1;P .5.
=
(Table 1). To avoid assumptions con¬
=
cerning a minimum "safe" platelet
count, variances of the LPC in infants
Table 3.—Correlation Between Birth Weight and Lowest Platelet Count* both with and without IVH were ex¬
Lowest Platelet Count 10»/L amined by the Student t test. There
No. of was a similarity of LPC in infants in
Patients <100 100-150 151-200 >200 each group (F' 1.23, P>f" .278),
= =
Birth Weight, g (n 302)
=
(n 27)
=
(n 26) =
(n=72) (n 177)
=
<750 32 6 5 4 17 indicating the absence of a direct re¬
750-999 84 7 7 23 47 lationship between the LPC and the
occurrence of IVH. A stepwise logistic
1000-1499 186 14 14 45 113
regression procedure was performed
V 8-57, df=6;P
= =
.199. to allow for interactions between de¬
pendent variables that might mask a
possible effect of thrombocytopenia on
Table 4.—Correlation Between Perinatal Asphyxia and Lowest Platelet Count* the risk of IVH due to other variables.
Lowest Platelet Count 10"/L Three variables (severity of respira¬
Perinatal
No. of
Patients <100 100-150 151-200 >200
tory distress, pneumothorax, and
birth weight) were found to have a
Asphyxia (n 302)
=
(n 27)
=
(n 27)
=
(n 69)
=
(n 179)
=
Present 88 12 9 21 46 significant influence on the incidence
Absent 214 15 18 48 133 of IVH. After allowing for the effect
of these factors, other variables, eg,
* * 4.15, df= 3; =.246.
=
LPC, perinatal asphyxia, serum so¬
dium level, and location of delivery,
Platelet Counts Statistical Analysis were not significant (P =
.05).
Blood samples were obtained by punc¬ Results analyzed statistically in
were
The relationship between the LPC
ture of the prewarmed heel or from an terms of absolute platelet count and by and severity of IVH was examined
indwelling arterial catheter. Platelet counts stratification, using the 2 test, the Student (Table 2). Severe IVH, ie, grades III
were performed on all infants at the time t test, and progessive logistic regression. and IV was not associated with a
of admission and repeated daily on all sick higher incidence of reduced platelet
infants in whom the lowest platelet count RESULTS counts than mild IVH, ie, grades I
(LPC) had been noted between 2 and 4 Intraventricular hemorrhage oc¬ and II (x* 0.47, d/=l;
=
.5). Fur¬
=
days of age.6 Platelet counts were per¬ curred in 90 (29.8%) of the 302 infants. thermore, there was no significant
formed on an electronic cell counter (Coul¬
In 40 infants, the IVH was grade I or association between reduced platelet
ter S Plus IV). Platelet counts less than
30 x 109/L were confirmed by manual cham¬ II, and in 50 infants, it was grade III count and birth weight (Table 3). The
or IV As has been reported previously, relationship between the LPC and
ber counts using phase-contrast micros¬
copy. The LPC measured during the first 4 IVH occurred before age 4 days in perinatal asphyxia is demonstrated in
days of life was used in subsequent analy¬ most instances.2·10-12 Table 4. Although there was a trend
sis. Platelet counts were measured on toward lower platelet counts in infants
Downloaded From: http://archpedi.jamanetwork.com/ by a Michigan State University User on 06/18/2015
who sustained perinatal asphyxia, this Finally, in a study of VLBW infants after the first day of life. Thus, there
did not reach statistical significance. born in one year in whom the incidence is a greater likelihood of detecting
Assessment of the power of the of IVH was 56%, an increased inci¬ thrombocytopenia in the sickest in¬
study demonstrated that a 14% de¬ dence and severity of IVH was ob¬ fants, ie, those who are at highest risk
crease of low platelet counts in infants served in infants in whom platelet for IVH from any cause. Third, it has
with IVH would have been detected counts were less than 100 109/L been demonstrated that hemorrhage
with a ß error of 0.1 (a 0.05), indi¬
= within the first 2 weeks of life.6 How¬ itself may result in consumption of
cating that the study population was ever, in this study, thrombocytopenic platelets.16 Consequently, infants who
sufficiently large to detect any clini¬ infants were compared with "sick con¬ have sustained IVH may have lower
cally significant decrease in reduced trols." Thus, although two studies3·6 platelet counts following the hemor¬
platelet counts in infants with IVH. have identified major differences be¬ rhage.
tween infants with and without IVH The lack of association between IVH
COMMENT in terms of factors such as birth as¬ and reduced platelet count in our
These data do not demonstrate a phyxia and severity of respiratory dis¬ study population, despite various fac¬
clear association between reduced ease, multivariate analysis was not tors that would tend to emphasize a
platelet count and IVH, an observa¬ performed to determine whether positive relationship, argues against a
tion that is in contrast to several re¬ these variables could explain the ap¬ role for reduced platelet count in the
cent reports.3"6 Thus, Beverley et al,3 parent association between platelet pathogenesis of IVH. Because of the
in a study of coagulation status in 106 count and IVH. Our study, as well as small number of infants with an LPC
infants of less than 34 weeks' gesta¬ others that use multivariate analysis, of less than 50 x 109/L, we were unable
tion, observed significantly lower have failed to demonstrate a signifi¬ to establish whether such very low
platelet counts at 48 hours of age in cant association between IVH and counts are related causally to IVH.
infants with IVH. However, these data platelet counts.7·8 The conclusions Other variables, eg, methods of blood
do not permit conclusions as to from our data are similar whether or collection, location, and mode of deliv¬
whether the low platelet counts were not multivariate analysis is applied. ery, may explain the differences in
a cause or consequence of IVH. Simi¬ Additional factors may produce a incidence of thrombocytopenia be¬
larly, McDonald et al" reported a sig¬ noncausal association between throm¬ tween various studies.16
nificantly higher incidence of IVH in bocytopenia and IVH in this context. The lack of a causal relationship
50 infants of gestational ages less than Thus, an increased risk of IVH with between reduced platelet count and
33 weeks in whom platelet counts were perinatal asphyxia has been re¬ IVH suggests that treatment of mod¬
less than 150 x 109/L within the first 8 ported.5·1316 However, because perina¬ erate thrombocytopenia (>50 109/L)
hours of life. In a study of 58 VLBW tal asphyxia may cause a consumptive is unlikely to decrease the incidence
infants, Setzer et al5 observed a rela¬ coagulopathy, it may result in both of IVH in infants of VLBW
tionship between mean platelet counts IVH and thrombocytopenia, which
in the first day of life and IVH in 71%. may create an apparent association
between the two variables. Second, in We thank Sam Sheps, MD, and the Department
However, when adjusted for the effect of Clinical Epidemiology, University of British
of perinatal asphyxia, this relationship this study, platelet counts were re¬ Columbia, Vancouver, for assistance with statis¬
was no longer statistically significant. peated more often in the sicker infants tical analysis.
References
1. Volpe JJ: Neurology of the Newborn, ed 2. 7. Szymonowicz W, Yu VYH, Wilson FE: An- 1982;100:956-959.
Philadelphia, WB Saunders Co, 1987, pp 316\x=req-\ tecedents of periventricular hemorrhage in in- 12. Ment LR, Duncan CC, Ehrenkranz RA,
325. fants weighing 1250 g or less at birth. Arch Dis et al: Intraventricular hemorrhage in the preterm
2. Ment LR, Duncan CC, Ehrenkranz RA: Child 1984;59:13-17. neonate: Timing and cerebral blood flow changes.
Intraventricular hemorrhage of the preterm ne- 8. Szymonowicz W, Yu VYH, Walker A, et al: J Pediatr 1984;104:419-425.
onate. Semin Perinatol 1987;11:132-141. Reduction in periventricular hemorrhage in pre- 13. Reynolds ML, Evans CAN, Reynolds
3. Beverley DW, Chance GW, Inwood MJ, et al: term infants. Arch Dis Child 1986;61:661-665. EOR, et al: Intracranial hemorrhage in the pre-
Intraventricular hemorrhage and hemostasis de- 9. Papile LA, Burstein J, Burstein R, et al: term sheep fetus. Early Hum Dev 1979;3:163\x=req-\
fects. Arch Dis Child 1984;59:444-448. Incidence and evolution of subependymal and 186.
4. McDonald MM, Johnson ML, Rumack CM, intraventricular hemorrhage: A study of infants 14. Lou HC: Perinatal hypoxic-ischemic brain
et al: Role of coagulopathy in newborn intracra- with birth weight less than 1500 gm. J Pediatr damage and intraventricular hemorrhage. Arch
nial hemorrhage. Pediatrics 1984;74:24-31. 1978;92:529-534. Neurol 1980;37:383-397.
5. Setzer ES, Webb IB, Wassenaar JW, et al: 10. Rumack CM, Manco-Johnson ML, Manco\x=req-\ 15. Meidell R, Marinelli P, Pettett G: Perinatal
Platelet dysfunction and coagulopathy in intra- Johnson MJ, et al: Timing and course of neonatal factors associated with early-onset intracranial
ventricular hemorrhage in the premature infant. intracranial hemorrhage using real-time ultra- hemorrhage in premature infants. AJDC 1985;
J Pediatr 1982;100:599-605. sound. Radiology 1985;154:101-105. 139:160-163.
6. Andrew M, Castle V, Saigal S, et al: Clinical 11. Perlman JM, Volpe JJ: Cerebral blood flow 16. Preston FE: Disseminated intravascular
impact of neonatal thrombocytopenia. J Pediatr velocity in relation to intraventricular hemor- coagulation. J Hosp Med 1982;28:129-137.
1987;110:457-464. rhage in the premature newborn infant. J Pediatr
Downloaded From: http://archpedi.jamanetwork.com/ by a Michigan State University User on 06/18/2015
You might also like
- Chapter 72. Case StudiesDocument40 pagesChapter 72. Case Studiesstawberry shortcake100% (1)
- Lesson Plan On Shock and HaemorrhageDocument35 pagesLesson Plan On Shock and HaemorrhageDr-Sanjay Singhania88% (16)
- Hasan 2021Document4 pagesHasan 2021Amina GoharyNo ratings yet
- Intravenous Immunoglobulin in Neonates With RhesusDocument9 pagesIntravenous Immunoglobulin in Neonates With RhesusGabriel BuftiaNo ratings yet
- Vries 2007Document6 pagesVries 2007BrîndușaPetcariuNo ratings yet
- Estudio de MariDocument6 pagesEstudio de MarianjidisNo ratings yet
- Pediatrics JournalDocument9 pagesPediatrics JournalDokter KarisNo ratings yet
- Etude Transf PQDocument10 pagesEtude Transf PQLincan RoxanaNo ratings yet
- Curley 2018 Platelet Transfusion Threshols in NeonatesDocument11 pagesCurley 2018 Platelet Transfusion Threshols in NeonatesEllya Latifah IlyasNo ratings yet
- DMV Cipe Di AtriaDocument6 pagesDMV Cipe Di AtriaAngélica ContrerasNo ratings yet
- Causes, Severity and Outcome of Neonatal Thrombocytopenia in Hi-Tech Medical College and Hospital, BhubaneswarDocument4 pagesCauses, Severity and Outcome of Neonatal Thrombocytopenia in Hi-Tech Medical College and Hospital, BhubaneswarInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyAlif ZainalNo ratings yet
- Articulo HICDocument6 pagesArticulo HICNelly GonzalezNo ratings yet
- Intraventricular HaemorrhageDocument9 pagesIntraventricular HaemorrhageTriponiaNo ratings yet
- Benson Multicentre 1986Document4 pagesBenson Multicentre 1986Dian NovitasariNo ratings yet
- Pediatric Outcome in Rhesus Hemolytic Disease Treated With and Without Intrauterine TransfusionDocument4 pagesPediatric Outcome in Rhesus Hemolytic Disease Treated With and Without Intrauterine TransfusionCatia CorreaNo ratings yet
- Normal Values For Mature and Immature in Very Preterm BabiesDocument3 pagesNormal Values For Mature and Immature in Very Preterm BabiesSukma EffendyNo ratings yet
- Noradrenalina en PrematurosDocument7 pagesNoradrenalina en PrematurosnzunaNo ratings yet
- Ultrasonido Doppler Temprano AMSDocument7 pagesUltrasonido Doppler Temprano AMSKaren Marbelly OrozcoNo ratings yet
- State University of New York, Downstate Medical Center, USADocument2 pagesState University of New York, Downstate Medical Center, USAronynoorNo ratings yet
- Transcranial Ultrasound Doppler Parameters in Cerebral Vessels May Predict Intracerebral Hemorrhage in Preterm NewbornsDocument7 pagesTranscranial Ultrasound Doppler Parameters in Cerebral Vessels May Predict Intracerebral Hemorrhage in Preterm Newbornsrezza mochamadNo ratings yet
- Transcranial Ultrasound Doppler Parameters in CereDocument7 pagesTranscranial Ultrasound Doppler Parameters in CereImin BuntaraNo ratings yet
- 1 s2.0 S1028455922001632 MainDocument4 pages1 s2.0 S1028455922001632 MainAditi SoniNo ratings yet
- Clinical StudyDocument6 pagesClinical StudyAndreiMunteanuNo ratings yet
- Thrombocytopenia in Late Preterm and Term Neonates After Perinatal AsphyxiaDocument10 pagesThrombocytopenia in Late Preterm and Term Neonates After Perinatal AsphyxiaTammy Utami DewiNo ratings yet
- Clinical Utility of Colour Doppler For Diagnosis of Adverse Perinatal Outcome in IUGR and PIHDocument4 pagesClinical Utility of Colour Doppler For Diagnosis of Adverse Perinatal Outcome in IUGR and PIHnjmdrNo ratings yet
- Importance of Ductus Venosus Doppler in Prediction of Perinatal Morbidity and MortalityDocument6 pagesImportance of Ductus Venosus Doppler in Prediction of Perinatal Morbidity and MortalityInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 1010 FTP PDFDocument5 pages1010 FTP PDFHerry SasukeNo ratings yet
- Irv 12375Document6 pagesIrv 12375Marella DevinaNo ratings yet
- Umbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialDocument5 pagesUmbilical Cord Milking in Term Infants Delivered by Cesarean Section: A Randomized Controlled TrialAffah MustafaNo ratings yet
- J Journal of Pediatrics Volume 125 Issue 4 October 1994 Pages 603-606Document4 pagesJ Journal of Pediatrics Volume 125 Issue 4 October 1994 Pages 603-606ElaineNo ratings yet
- Early Enteral Feeding and Nosocomial Sepsis in Very Low Birthweight InfantsDocument4 pagesEarly Enteral Feeding and Nosocomial Sepsis in Very Low Birthweight InfantsaripbudiboyNo ratings yet
- Ultrasound in Obstet Gyne - 2002 - Senat - Management of Single Fetal Death in Twin To Twin Transfusion Syndrome A RoleDocument4 pagesUltrasound in Obstet Gyne - 2002 - Senat - Management of Single Fetal Death in Twin To Twin Transfusion Syndrome A RoleBramantyo Dwi HandjonoNo ratings yet
- Incidence of Periventricular/intraventricular Hemorrhage in Very Low Birth Weight Infants: A 15-Year Cohort StudyDocument7 pagesIncidence of Periventricular/intraventricular Hemorrhage in Very Low Birth Weight Infants: A 15-Year Cohort StudyGusBlomkvistSomocurioNo ratings yet
- The Effects Aedv and RedvDocument7 pagesThe Effects Aedv and RedvTresa ivaniNo ratings yet
- Slide Obgyn Jurnal ReadingDocument18 pagesSlide Obgyn Jurnal Readingari naNo ratings yet
- 2016 Relacion ANEMIA Con NEC y TransfusionesDocument9 pages2016 Relacion ANEMIA Con NEC y TransfusionesnadisjaviNo ratings yet
- Leukopenia and Neutropenia As A Predictors of Neonatal SepsisDocument8 pagesLeukopenia and Neutropenia As A Predictors of Neonatal SepsisYandiNo ratings yet
- E548 FullDocument7 pagesE548 FullBimo Aryo TejoNo ratings yet
- BR J Haematol - 2017 - Rühle - Advances in Predicting Venous Thromboembolism Risk in ChildrenDocument12 pagesBR J Haematol - 2017 - Rühle - Advances in Predicting Venous Thromboembolism Risk in ChildrenKarina CamachoNo ratings yet
- Nej M 200009073431001Document8 pagesNej M 200009073431001Asri Ani NurchasanahNo ratings yet
- Neutro PhiliaDocument10 pagesNeutro PhiliaMARIA DE LOS ANGELES MARTINEZ VIRENo ratings yet
- NeutrophiliaDocument10 pagesNeutrophiliamaria martinezNo ratings yet
- Inferior Vena Cava Diameter A Useful Method For EsDocument5 pagesInferior Vena Cava Diameter A Useful Method For EsmalisalukmanNo ratings yet
- Cap 2023Document9 pagesCap 2023Neonatología HGO4No ratings yet
- Journal Medicine: The New EnglandDocument8 pagesJournal Medicine: The New EnglandHam jungNo ratings yet
- Journal 6Document18 pagesJournal 6Sebastian SetiahardjaNo ratings yet
- Murphy2002 Posthaemorrhagic Ventricular DilatationDocument6 pagesMurphy2002 Posthaemorrhagic Ventricular DilatationModou NianeNo ratings yet
- Fetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaDocument4 pagesFetomaternal Outcome in Pregnancy With Severe ThrombocytopeniaMuhammad AdithiaNo ratings yet
- Am J Perinatol. 2007 Jun24 (6) 373-6Document4 pagesAm J Perinatol. 2007 Jun24 (6) 373-6Ivan Osorio RuizNo ratings yet
- Streptokinase in The Treatment of Pleural Controlled Trial of IntrapleuralDocument7 pagesStreptokinase in The Treatment of Pleural Controlled Trial of IntrapleuraltomgasoneNo ratings yet
- Management of Neonatal Hypotension and ShockDocument7 pagesManagement of Neonatal Hypotension and ShockntnquynhproNo ratings yet
- Management of Neonatal Hypotension and ShockDocument7 pagesManagement of Neonatal Hypotension and ShockntnquynhproNo ratings yet
- Nirs Preterm ScreeenDocument6 pagesNirs Preterm ScreeenLissaberti AmaliahNo ratings yet
- Andrea Surányi, Ábel Altorjay, László Kaiser, Tibor Nyári, Gábor NémethDocument9 pagesAndrea Surányi, Ábel Altorjay, László Kaiser, Tibor Nyári, Gábor NémethfujimeisterNo ratings yet
- Articles: BackgroundDocument10 pagesArticles: BackgroundKarina CamachoNo ratings yet
- NLR - Neonatal SepsisDocument6 pagesNLR - Neonatal SepsisGlen LazarusNo ratings yet
- 194 265 1 SMDocument5 pages194 265 1 SMAdkhiatul MuslihatinNo ratings yet
- 2009 DV Aortic Isthmus FGR Blood Flow GratacosDocument5 pages2009 DV Aortic Isthmus FGR Blood Flow GratacosRibeiro SáNo ratings yet
- Management and Complications of Intraventricular Hemorrhage in The NewbornDocument10 pagesManagement and Complications of Intraventricular Hemorrhage in The NewbornAnonymous Xmb6QQvRNo ratings yet
- Ductus Venosus Blood Velocity and The Umbilical Artery Circulation in The Seriously Growth Retarded FoetusDocument6 pagesDuctus Venosus Blood Velocity and The Umbilical Artery Circulation in The Seriously Growth Retarded FoetusSaikatBanerjeeNo ratings yet
- Diabetes in Children and Adolescents: A Guide to Diagnosis and ManagementFrom EverandDiabetes in Children and Adolescents: A Guide to Diagnosis and ManagementNo ratings yet
- Cureus 0015 00000038985Document6 pagesCureus 0015 00000038985Amina GoharyNo ratings yet
- PDF 8Document11 pagesPDF 8Amina GoharyNo ratings yet
- PDF 3Document5 pagesPDF 3Amina GoharyNo ratings yet
- Consensus Statement: The 16th Annual Western Canadian Gastrointestinal Cancer Consensus Conference Saskatoon, Saskatchewan September 5-6, 2014Document12 pagesConsensus Statement: The 16th Annual Western Canadian Gastrointestinal Cancer Consensus Conference Saskatoon, Saskatchewan September 5-6, 2014Amina GoharyNo ratings yet
- Prognostic Value of Metabolic Tumor Burden On F-FDG PET in Nonsurgical Patients With Non-Small Cell Lung CancerDocument12 pagesPrognostic Value of Metabolic Tumor Burden On F-FDG PET in Nonsurgical Patients With Non-Small Cell Lung CancerAmina GoharyNo ratings yet
- 4Document20 pages4Amina GoharyNo ratings yet
- Craniopharyngiomas of The Third Ventricle: Trans-Lamina Terminalis ApproachDocument9 pagesCraniopharyngiomas of The Third Ventricle: Trans-Lamina Terminalis ApproachAmina GoharyNo ratings yet
- CBU 5th Year Exam Paper 1 2017Document13 pagesCBU 5th Year Exam Paper 1 2017Homeground entertainment100% (3)
- Disseminated Intravascular Coagulopathy DICDocument24 pagesDisseminated Intravascular Coagulopathy DICMassimiliano MalerbaNo ratings yet
- Surgery: 1) Preoperative Assessment of HemostasisDocument13 pagesSurgery: 1) Preoperative Assessment of HemostasisIruthayanathar Andru NitharsanNo ratings yet
- Fluid Resuscitation in Haemorrhagic ShockDocument9 pagesFluid Resuscitation in Haemorrhagic ShockbashiruaminuNo ratings yet
- HEMA2 - Bleeding Time Written ReportDocument10 pagesHEMA2 - Bleeding Time Written ReportMarjorie GabalunosNo ratings yet
- Rle Skills Lab Rubrics GuidesDocument5 pagesRle Skills Lab Rubrics GuidesPrince Joshua Grande AngelesNo ratings yet
- B - Braun: Nutri Ex® Lipid SpecialDocument2 pagesB - Braun: Nutri Ex® Lipid SpecialAbhie Fajri MierzanNo ratings yet
- Bleeding After TonsillectomyDocument7 pagesBleeding After Tonsillectomyking_petarNo ratings yet
- First Year Complete Physiology MCQ Bank by Team DR Of2027-28Document284 pagesFirst Year Complete Physiology MCQ Bank by Team DR Of2027-28ammejan10100% (2)
- Jurnal 1Document7 pagesJurnal 1Nur WahyuniNo ratings yet
- NCP RosteDocument2 pagesNCP RosteRoyce Vincent TizonNo ratings yet
- Bleeding Disorders 1 - DR - Kamal MokbelDocument13 pagesBleeding Disorders 1 - DR - Kamal MokbelRawan E. SaeedNo ratings yet
- Nursing Care Plan Spontaneous AbortionDocument2 pagesNursing Care Plan Spontaneous AbortionAbigael Rubio de LeonNo ratings yet
- Medical History Report Medical Prescreen Questionnaire: Philippine National Police Health ServiceDocument4 pagesMedical History Report Medical Prescreen Questionnaire: Philippine National Police Health ServicejovelonderizaNo ratings yet
- Etamsylate DS Meppo2010 PDFDocument3 pagesEtamsylate DS Meppo2010 PDFAqmarlia PutriNo ratings yet
- Shock ChartsDocument2 pagesShock ChartsforminskoNo ratings yet
- Warf Side EffectsDocument6 pagesWarf Side EffectsPankaj SharmaNo ratings yet
- BleedingDocument14 pagesBleedingRhomizal MazaliNo ratings yet
- Chapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingDocument3 pagesChapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingKn VelasquezNo ratings yet
- Trauma Induced Coagulopathy What You Need To Know.1Document7 pagesTrauma Induced Coagulopathy What You Need To Know.1llucaspilonettoNo ratings yet
- Collection of Blood Sample From Experimental AnimalsDocument12 pagesCollection of Blood Sample From Experimental AnimalslovehopeNo ratings yet
- cc2851 (PDF - Io)Document15 pagescc2851 (PDF - Io)Aquardoleo ValentinoNo ratings yet
- Emcase 04 Feb 2019 Dr. KometDocument56 pagesEmcase 04 Feb 2019 Dr. KometKomet Rama DaudNo ratings yet
- Preparation For Giving First AidDocument11 pagesPreparation For Giving First AidLarisa HurtadoNo ratings yet
- StentsDocument11 pagesStentsIbrahim Ramadan Eltorky0% (2)
- 9 - Post-OP Management and ComplicationsDocument57 pages9 - Post-OP Management and ComplicationsThon JustineNo ratings yet
- Causes: Polycythemia VeraDocument15 pagesCauses: Polycythemia VeraMaria VisitacionNo ratings yet
- Blood Bank International Standard ISBT Science Series - 2008 - Hardwick - Blood ProcessingDocument29 pagesBlood Bank International Standard ISBT Science Series - 2008 - Hardwick - Blood ProcessingShan AhmadNo ratings yet