Professional Documents
Culture Documents
Srikantha 2009
Srikantha 2009
Uploaded by
filbertanswCopyright:
Available Formats
You might also like
- Neil v. Watson - The Mind's Machine - Foundations of Brain and Behavior-Sinauer AssociatesDocument622 pagesNeil v. Watson - The Mind's Machine - Foundations of Brain and Behavior-Sinauer AssociatesChumchum Kumar100% (12)
- BSBLDR511 Develop and Use Emotional IntelligenceDocument13 pagesBSBLDR511 Develop and Use Emotional IntelligenceLayla Correa da SilvaNo ratings yet
- Critical Care Goals and ObjectivesDocument28 pagesCritical Care Goals and ObjectivesjyothiNo ratings yet
- Short-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyDocument12 pagesShort-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyTJPRC PublicationsNo ratings yet
- SPIROMETRYDocument9 pagesSPIROMETRYaeyousefNo ratings yet
- Ijcp-5481 oDocument6 pagesIjcp-5481 oDebasis ChatterjeeNo ratings yet
- Adult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesDocument9 pagesAdult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesMutiara RizkyNo ratings yet
- Euro J of Neurology - 2023 - Doorn - European Academy of Neurology Peripheral Nerve Society Guideline On Diagnosis andDocument29 pagesEuro J of Neurology - 2023 - Doorn - European Academy of Neurology Peripheral Nerve Society Guideline On Diagnosis andjcr87No ratings yet
- Ijvm2014 531689 PDFDocument6 pagesIjvm2014 531689 PDFReka HariskianaNo ratings yet
- Lucas 2014Document8 pagesLucas 2014Prima YosiNo ratings yet
- Spirometry in Children: Clinical ReviewDocument9 pagesSpirometry in Children: Clinical ReviewMoonNo ratings yet
- Misra 2012Document7 pagesMisra 2012Carlos RiquelmeNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document4 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Riri KumalaNo ratings yet
- Chronic Kidney Disease : Hypertensive and Diabetic Retinopathy in PatientsDocument7 pagesChronic Kidney Disease : Hypertensive and Diabetic Retinopathy in PatientsAnonymous FgT04krgymNo ratings yet
- Effect of Prednisolone During Defervescence in Dengue Haemorrhagic Fever: An Open Label Controlled StudyDocument4 pagesEffect of Prednisolone During Defervescence in Dengue Haemorrhagic Fever: An Open Label Controlled StudyFabiola StellaNo ratings yet
- Red Blood Cell Transfusion: Decision Making in Pediatric Intensive Care UnitsDocument7 pagesRed Blood Cell Transfusion: Decision Making in Pediatric Intensive Care UnitsIndra AjaNo ratings yet
- A Clinical Study of Tuberculous Cervical LymphadenDocument5 pagesA Clinical Study of Tuberculous Cervical LymphadenAgung DewanggaNo ratings yet
- Gupta 2013Document5 pagesGupta 2013Dhruv MahajanNo ratings yet
- Benign Paroxysmal Positional Vertigo: Opportunities SquanderedDocument8 pagesBenign Paroxysmal Positional Vertigo: Opportunities SquanderedNia UtariNo ratings yet
- Subglottic Stenosis in Granulomatosis With Polyangiitis: The Role of Laryngotracheal ResectionDocument5 pagesSubglottic Stenosis in Granulomatosis With Polyangiitis: The Role of Laryngotracheal ResectionSamNo ratings yet
- Splenectomy in Children With Chronic ITP: Long-Term Efficacy and Relation Between Its Outcome and Responses To Previous TreatmentsDocument4 pagesSplenectomy in Children With Chronic ITP: Long-Term Efficacy and Relation Between Its Outcome and Responses To Previous TreatmentsVladimir Henry Triguero RosalesNo ratings yet
- Management Outcomes of Hydrocephalus Among Under Five Children in A Tertiary Hospital in Gombe North Eastern NigeriaDocument4 pagesManagement Outcomes of Hydrocephalus Among Under Five Children in A Tertiary Hospital in Gombe North Eastern NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Operative Versus Nonoperative Treatments For Legg-Calve - Perthes Disease: A Meta-AnalysisDocument9 pagesOperative Versus Nonoperative Treatments For Legg-Calve - Perthes Disease: A Meta-Analysisyarianna2No ratings yet
- Lovastatin For The Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled TrialDocument9 pagesLovastatin For The Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled TrialBpmStfbNo ratings yet
- 12 11 PBDocument168 pages12 11 PBYS NateNo ratings yet
- Claudia Craven VENTRICULOMEGALY CLASSIFICATIONDocument17 pagesClaudia Craven VENTRICULOMEGALY CLASSIFICATIONGUI VINCENo ratings yet
- Serum Thyroid-Stimulating Hormone Is An Independent Risk Factor of Recurrent Guillain-Barré SyndromeDocument41 pagesSerum Thyroid-Stimulating Hormone Is An Independent Risk Factor of Recurrent Guillain-Barré SyndromeDr NIVEDITHA CNo ratings yet
- Content ServerDocument8 pagesContent ServerG. Araya MoraNo ratings yet
- Clin Infect Dis. 2004 Tunkel 1267 84 Idsa MeningitiDocument18 pagesClin Infect Dis. 2004 Tunkel 1267 84 Idsa MeningitiJesus Salvador SerratoNo ratings yet
- Case Studies of Lower Respiratory Tract InfectionsDocument25 pagesCase Studies of Lower Respiratory Tract InfectionsMarianNo ratings yet
- Tourniquet TestingDocument6 pagesTourniquet TestingPatrick RamosNo ratings yet
- Tto Crup NatureDocument7 pagesTto Crup NatureCarolina Mora RuedaNo ratings yet
- Kwong 2012Document8 pagesKwong 2012Ke XuNo ratings yet
- To Study Hematological Profile in Covid-19 Patients in Relation With Prognosis and Outcome: - A Cross Sectional Observational StudyDocument7 pagesTo Study Hematological Profile in Covid-19 Patients in Relation With Prognosis and Outcome: - A Cross Sectional Observational StudyIJAR JOURNALNo ratings yet
- PESI Critical Care 2005Document6 pagesPESI Critical Care 2005Rocio Méndez FrancoNo ratings yet
- A Prospective Observational Study of Dengue Fever With Thrombocytopenia With Reference To TreatmentDocument6 pagesA Prospective Observational Study of Dengue Fever With Thrombocytopenia With Reference To Treatment-Tony Santoso Putra-No ratings yet
- Pediatric Hematology Oncology JournalDocument4 pagesPediatric Hematology Oncology JournalmitraNo ratings yet
- Long-Term Clinical Outcome of Fetal Cell Transplantation For Parkinson Disease Two Case ReportsDocument5 pagesLong-Term Clinical Outcome of Fetal Cell Transplantation For Parkinson Disease Two Case Reportsjust for download matterNo ratings yet
- Cerebral Venous Thrombosis: Clinical Predictors and Emerging TreatmentsDocument3 pagesCerebral Venous Thrombosis: Clinical Predictors and Emerging Treatmentschartreuse avonleaNo ratings yet
- Chest: Point/Counterpoint EditorialsDocument3 pagesChest: Point/Counterpoint Editorialsgiseladelarosa2006No ratings yet
- Comparison of Repositioning Maneuvers For Benign Paroxysmal Positional Vertigo of Posterior Semicircular Canal: Advantages of Hybrid ManeuverDocument6 pagesComparison of Repositioning Maneuvers For Benign Paroxysmal Positional Vertigo of Posterior Semicircular Canal: Advantages of Hybrid ManeuverFayza RihastaraNo ratings yet
- GBS PDTDocument8 pagesGBS PDTabdulkadirmunsyNo ratings yet
- VP Shunt For Meningitis TBDocument9 pagesVP Shunt For Meningitis TBNindi LizenNo ratings yet
- Emboli ParuDocument10 pagesEmboli Paruindry_purnamasariNo ratings yet
- 10.1007@s12098 020 03454 1Document6 pages10.1007@s12098 020 03454 1rayhantaswinNo ratings yet
- DIC in Abruptio 2Document5 pagesDIC in Abruptio 2HoneylynNo ratings yet
- Comparison of 3 Clinical Models For Predicting The Probability of Pulmonary EmbolismDocument8 pagesComparison of 3 Clinical Models For Predicting The Probability of Pulmonary EmbolismAlirio Rodrigo Bastidas GoyesNo ratings yet
- Fluctuaciones Relacionadas A Tratamiento GBDocument7 pagesFluctuaciones Relacionadas A Tratamiento GBOsvaldo CortésNo ratings yet
- Decompressive Hemicraniectomy and DuroplastyDocument5 pagesDecompressive Hemicraniectomy and DuroplastyAmy NilifdaNo ratings yet
- JHM 2112Document4 pagesJHM 2112senkonenNo ratings yet
- Achondroplasia Natural History Study (CLARITY)Document7 pagesAchondroplasia Natural History Study (CLARITY)jakelinelagoadvNo ratings yet
- Lung Ultrasound Dry WeightDocument16 pagesLung Ultrasound Dry WeightBhanu KumarNo ratings yet
- Restrictive Fluids in Septic Shock. NEJM 2022Document12 pagesRestrictive Fluids in Septic Shock. NEJM 2022neeraj SinghNo ratings yet
- Neutrophil To Lymphocyte Ratio in Diagnosis of Complicated and Non-Complicated AppendicitisDocument7 pagesNeutrophil To Lymphocyte Ratio in Diagnosis of Complicated and Non-Complicated AppendicitisHamza AhmedNo ratings yet
- Baca IniDocument9 pagesBaca IniRahmi Annisa MaharaniNo ratings yet
- Wetzel2020 Article Flow-regulatedVersusDifferentiDocument7 pagesWetzel2020 Article Flow-regulatedVersusDifferenticNo ratings yet
- Neurourology and Urodynamics - 2022 - Martin - Is Sacral Neuromodulation Effective in Patients With Parkinson S Disease ADocument7 pagesNeurourology and Urodynamics - 2022 - Martin - Is Sacral Neuromodulation Effective in Patients With Parkinson S Disease AElkin JNo ratings yet
- Kansal 2018Document1 pageKansal 2018Sheena Mae MansinadesNo ratings yet
- 1 s2.0 S074152140290621X MainDocument6 pages1 s2.0 S074152140290621X Main1751010307No ratings yet
- GBS European Guidelines 2023Document29 pagesGBS European Guidelines 2023Saurabh AgrawalNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Abdominal Acupuncture For DepressionDocument35 pagesAbdominal Acupuncture For DepressionAGNESE YOLOTZIN OLIVERA TORO REYESNo ratings yet
- Cannabis Legal Regulatory Update April June 2019Document19 pagesCannabis Legal Regulatory Update April June 2019stonerhinoNo ratings yet
- Research in Primary Dental Care 1 PDFDocument4 pagesResearch in Primary Dental Care 1 PDFMARIA NAENo ratings yet
- الإجازات المرضية - منصة صحةDocument2 pagesالإجازات المرضية - منصة صحةShatha miNo ratings yet
- Region of Waterloo Job DescriptionDocument4 pagesRegion of Waterloo Job Descriptionbeth aguirreNo ratings yet
- Ebsco Fulltext 2024 03 20Document17 pagesEbsco Fulltext 2024 03 20api-733905896No ratings yet
- MSDS GINKGOLON-24 (Ginkgo Biloba Ext)Document3 pagesMSDS GINKGOLON-24 (Ginkgo Biloba Ext)Selviani Dwi MuryantiNo ratings yet
- 2-NBDG As A Fluorescent Indicator For Direct Glucose Uptake MeasurementDocument9 pages2-NBDG As A Fluorescent Indicator For Direct Glucose Uptake MeasurementPili CárdenasNo ratings yet
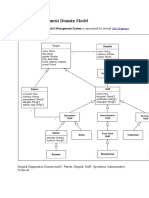
- Hospital Management Domain ModelDocument4 pagesHospital Management Domain Modelvinod kapateNo ratings yet
- PD Lesson 5 Coping With Stress in Middle and Late AdolescenceDocument16 pagesPD Lesson 5 Coping With Stress in Middle and Late AdolescenceEL FuentesNo ratings yet
- Developmental DelayDocument79 pagesDevelopmental DelayNaveen KumarNo ratings yet
- Glycolic Acid SdsDocument11 pagesGlycolic Acid SdsJuthi RahmanNo ratings yet
- Cardio DrugsDocument58 pagesCardio DrugsMARIA ROWENA VIA J. LUCENANo ratings yet
- Management Is Nothing More Than Motivating Other People GHEORGHE MDocument6 pagesManagement Is Nothing More Than Motivating Other People GHEORGHE MCristina PaliuNo ratings yet
- Buntis Congress Report 2021Document24 pagesBuntis Congress Report 2021Giselle ArenasNo ratings yet
- Antibiotic Prophylaxis OrthoDocument4 pagesAntibiotic Prophylaxis OrthoDonNo ratings yet
- Prosthesis For Long Span Kennedy's Class III Partially Edentulous Condition: A Case ReportDocument5 pagesProsthesis For Long Span Kennedy's Class III Partially Edentulous Condition: A Case ReportRiana WidiantyNo ratings yet
- HMB342 Course Syllabus Summer 2020Document5 pagesHMB342 Course Syllabus Summer 2020WangNo ratings yet
- Lifting Plan: Table of ContentDocument11 pagesLifting Plan: Table of ContentkhurramNo ratings yet
- ICN Framework of Disaster NursingDocument18 pagesICN Framework of Disaster NursingKRIZIA ANE A. SULONG100% (1)
- Element - 45 - 978-Design ReportDocument15 pagesElement - 45 - 978-Design ReportLeeNo ratings yet
- Product: A Product Is Anything That Can Be Offered To A Market To Satisfy A Want or NeedDocument12 pagesProduct: A Product Is Anything That Can Be Offered To A Market To Satisfy A Want or NeedSumon Das DasNo ratings yet
- Disability and Life Writing: Reports From The Nineteenth-Century AsylumDocument19 pagesDisability and Life Writing: Reports From The Nineteenth-Century AsylumHS22D001 MalavikaNo ratings yet
- UNIV144 Questions 2Document8 pagesUNIV144 Questions 2Clinton SmaugNo ratings yet
- Resume Igd Rsud PareDocument66 pagesResume Igd Rsud PareIqbalRazifNo ratings yet
- Pediatric Community Acquired PneumoniaDocument24 pagesPediatric Community Acquired PneumoniaJames Lagamayo JavierNo ratings yet
- PARENT AWARENESS SEMINAR-hand OutsDocument2 pagesPARENT AWARENESS SEMINAR-hand OutsLADY ANN GRACE LAGASNo ratings yet
- CPR Salbutamol+Ipratropium Neb (BRODIX PLUS) 35'sDocument2 pagesCPR Salbutamol+Ipratropium Neb (BRODIX PLUS) 35'sRacquel SolivenNo ratings yet
Srikantha 2009
Srikantha 2009
Uploaded by
filbertanswOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Srikantha 2009
Srikantha 2009
Uploaded by
filbertanswCopyright:
Available Formats
J Neurosurg Pediatrics 4:176–183,
4:000–000, 2009
Outcome of ventriculoperitoneal shunt placement in Grade
IV tubercular meningitis with hydrocephalus: a retrospective
analysis in 95 patients
Clinical article
Umesh Srikantha, M.B.B.S., M.Ch., Jagadeesh V. Morab, M.B.B.S., Savitr Sastry, M.S.,
Rojin Abraham, M.Ch., Anandh Balasubramaniam, M.Ch., Sampath Somanna, M.Ch.,
Indira Devi, M.Ch., Chandramouli A. Bangalore, M.Ch., and Paritosh Pandey, M.Ch.
Department of Neurosurgery, National Institute of Mental Health and Neuro Sciences (NIMHANS),
Bangalore, Karnataka, India
Object. Hydrocephalus is the most common complication of tubercular meningitis (TBM). Relieving hydro-
cephalus by ventriculoperitoneal (VP) shunt placement has been considered beneficial in patients in Palur Grade II or
III. The role of VP shunt placement in those of Grade IV is controversial and the general tendency is to avoid its use.
Some authors have suggested that patients in Grade IV should receive a shunt only if their condition improves with a
trial placement of an external ventricular drain (EVD). In the present study, the authors assessed the outcome of VP
shunt placement in patients in Grade IV TBM with hydrocephalus to examine the factors predicting outcome and to
determine whether a trial with an EVD is absolutely necessary prior to shunt placement.
Methods. Ninety-five consecutive cases of TBM with hydrocephalus in which the patients underwent VP shunt
placement were retrospectively analyzed, and direct VP shunts were placed whenever possible. An EVD was placed
first only in the presence of deranged blood parameters. Outcomes were assessed both in the short and long term.
Results. The mean patient age was 17.5 years (range 1–55 years). Fifty-two patients underwent direct VP shunt
placement, and the remaining 43 received EVDs first. Overall, 33 and 45% of patients had favorable short- and long-
term outcomes, respectively. Age older than 3 years and duration of altered sensorium ≤ 3 days were predictive of a
favorable short-term outcome. Glasgow Coma Scale score at presentation was predictive of long-term outcome. Of
the patients who did not improve with placement of an EVD prior to VP shunt insertion, 24 and 18% had favorable
short- and long-term outcomes, respectively; this was not significantly different from the outcome in the patients who
underwent direct VP shunt placement.
Conclusions. Direct VP shunt placement is an effective option in patients with Grade IV TBM with hydrocepha-
lus. Age and duration of altered sensorium are predictive of short-term outcome, while Glasgow Coma Scale score at
presentation predicts long-term outcome. Ventriculoperitoneal shunts should be considered even in patients who do
not improve with an EVD. (DOI: 10.3171/2009.3.PEDS08308)
Key Words • tubercular meningitis • hydrocephalus •
ventriculoperitoneal shunt • external ventricular drainage • outcome
T
uberculosis is one of the most common chronic increased incidence of complications, and high morbidity
infections encountered in developing countries. It and mortality rate compared to other forms of tuberculo-
is also reported in developed countries because of sis.6
AIDS, organ transplantations, and the increasing use of Hydrocephalus is the most common complication of
immunosuppressant medications.6 Central nervous system TBM. Tandon et al.14 stated that hydrocephalus is nearly
tuberculosis accounts for only 5% of all tubercular infec- always present in patients who have had TBM for 4–6
tions,8 yet has received a lot of attention because of the weeks, and is more common and develops earlier in chil-
dren than in adults.4,8 Severity of TBM has been graded
Abbreviations used in this paper: ATT = antitubercular therapy; by different authors. The grading proposed by Palur and
EVD = external ventricular drain; GCS = Glasgow Coma Scale; colleagues,12 used in this study, recognizes 4 grades (Ta-
GOS = Glasgow Outcome Scale; TBM = tubercular meningitis; VP ble 1).
= ventriculoperitoneal. It is generally agreed that relieving hydrocephalus via
176 J Neurosurg: Pediatrics / Volume 4 / August 2009
Shunt placement in poor-grade TBM with hydrocephalus
TABLE 1: Palur grading system for TBM* Case Selection
GCS
Case records obtained in 95 consecutive patients who
Grade Clinical Features Score
met the inclusion criteria were retrospectively analyzed
and their demographic and clinical features, hematological
I no neurological deficit, normal sensorium 15 parameters, type of procedure done (direct VP shunt place-
II neurological deficit present, normal sensorium 15 ment or EVD first) were noted. The available follow-up and
III altered sensorium, easily arousable; neurological 9–14 the clinical status at follow-up were also recorded as noted
deficit present or absent in each patient’s file, as well as results of telephone inter-
IV deeply comatose; decerebrate or decorticate postur- 3–8
views or mailed questionnaires whenever possible.
ing present or absent Outcome Assessment
* Adapted from Palur et al., 1991. Outcome in patients with TBM with hydrocephalus
has been assessed in other studies in terms of GOS score
VP shunt placement is beneficial in patients in Grades II and at follow-up.10,12 We also used GOS score at follow-up as
III TBM.1,12 The general tendency is to avoid VP shunts in the criteria for assessing long-term outcome in our patients.
Grade IV TBM with hydrocephalus because these patients We felt that to truly evaluate the role of the VP shunt, we
are considered to have a poor outcome, with reported mor- would need to consider the short-term outcome, because
tality rates of 40–100%.1,7,10,12 Other authors have suggest- long-term outcome could be attributed to a combination of
ed that patients with Grade IV TBM with hydrocephalus the shunt, ATT, and steroid therapy. The short-term benefit
should receive a VP shunt only if their condition improves was attributed solely to the CSF diversion procedure. Be-
to Grade II or III with EVD placement.1,10 Although the cause of a lack of criteria in the literature for judging what
outcome of Grade IV TBM with hydrocephalus is consid- is considered immediate clinical improvement in these pa-
ered dismal, relieving the hydrocephalus is the only other tients who present with poor GCS scores, we considered
treatment we can offer these patients apart from ATT, ste- a cut-off of GCS score ≥ 12 at the time of discharge as a
roids, and supportive care. Thus, at our institution, we tend reasonable criterion for clinical improvement. According-
to undertake CSF diversion in most cases. ly, outcome was assessed in 2 forms: short-term and long-
Although patients in Grade IV TBM have on most oc- term outcome. Short-term outcome was assessed using the
casions received ATT and steroids alone—without a VP GCS score at discharge, with scores ≥ 12 considered a fa-
shunt—it is worthwhile to mention that to the best of our vorable outcome, and scores < 12 considered unfavorable.
knowledge, there has not been a single study solely dedi- Long-term outcome was assessed using the GOS score at
cated toward establishing the outcome or determining the follow-up, with scores of 4 or 5 considered favorable, and
prognostic factors in this set of patients. We therefore un- scores of 1–3 considered unfavorable. In children younger
dertook this study in Grade IV TBM with hydrocephalus than 2 years of age, the modified GOS score was used.
with 3 main objectives: 1) to examine the outcome of VP
shunts in Grade IV TBM with hydrocephalus; 2) to study Statistical Analysis
the factors predicting outcome; and 3) to assess whether a Statistical analysis was performed with commercially
trial of EVD is necessary prior to VP shunt placement. available software (SPSS 10.0; SPSS, Inc.). Cross-tabs with
chi-square tests were used for assessing outcome. Binary
Methods logistic regression analysis was used to test significance in
a multivariate model. Chi-square tests were used to show
This study was conducted at the National Institute of the similarity of the follow-up group to the whole popula-
Mental Health and Neurosciences, Bangalore, India, and tion.
is a retrospective analysis of all cases of Grade IV TBM Age, duration of symptoms, duration of altered sen-
with hydrocephalus for which VP shunts were placed be- sorium, GCS score at presentation, presence or absence of
tween January 2000 and December 2005. infarcts, and basal exudates were considered as variables
against which to assess outcome.
Study Protocol
All patients with a diagnosis of TBM were started on Results
weight-appropriate doses of 4-drug ATT (isoniazid, rifam-
picin, ethambutol, and pyrazinamide) and steroids (intrave- Ninety-five patients underwent VP shunt placement
nous dexamethasone). In patients in Grade IV (GCS score at our institution during the study period. The mean pa-
≤ 8) with hydrocephalus, the first choice for treatment was tient age was 17.5 years (range 1–55 years), with 57 pa-
VP shunt implantation. However, in the presence of hema- tients (60%) younger than 18 and 33 (35%) younger than
tological or biochemical abnormalities such as anemia or 3 years of age. There were 65 male and 30 female patients
hyponatremia requiring correction prior to general anes- (the male-to-female ratio was 1.7:1). The median duration
thesia (hemoglobin < 8 g or Na+ < 130 mEq/L), an EVD of symptoms prior to presentation was 21 days and the
was instituted until the anesthetist considered the patient fit median duration of altered sensorium prior to intervention
for shunt implantation surgery. The diagnosis of TBM was (either VP shunt or EVD placement) was 3 days. The GCS
confirmed in all cases by cytochemical analysis of CSF ob- score at presentation was 3–6 in 18 patients (19%), and was
tained by lumbar puncture.2 either 7 or 8 in the remaining 77 patients (81%). Infarcts
J Neurosurg: Pediatrics / Volume 4 / August 2009 177
U. Srikantha et al.
and basal exudates were present on preoperative CT scans TABLE 2: Results of the chi-square tests done to compare the
in 31 (32.6%) and 68 (71.6%) patients, respectively. Anemia groups with and without known outcomes*
and hyponatremia requiring correction was observed in 17
(18%) and 54 cases (57%), respectively. No. of Patients (%)
FU No FU
Duration of Follow-Up Variable (40 patients) (55 patients) p Value
A documented outcome was known in 40 cases (42%), age (yrs)
including 11 deaths (9 in-hospital deaths and 2 at follow- group 1 0.26
up). In these 40 cases, the median duration of follow-up
was 12 months (mean 18 months, range 3–65 months). ≤18 26 (46) 31 (54)
Chi-square tests were performed to compare these 40 >18 14 (37) 24 (63)
cases with the remaining 55 cases, and there were no sta- group 2 0.43
tistically significant differences between the groups with ≤3 13 (39) 20 (61)
respect to the variables analyzed (Table 2). This finding >3 27 (43) 35 (57)
implies that the follow-up group is not disparate from the duration of symptoms (days) 0.45
whole group.
≤21 21 (44) 27 (56)
Outcome of Grade IV TBM With Hydrocephalus After VP >21 19 (40) 28 (60)
Shunt Placement duration of altered sensorium
0.56
Outcome was assessed in terms of short-term out- (days)
come (GCS score at discharge in all 95 cases) and long- ≤3 22 (42) 30 (58)
term outcome (GOS score at follow-up in 40 patients in >3 18 (42) 25 (58)
whom follow-up was available). GCS score at presentation 0.31
The GCS score at discharge was ≥ 12 in 33% of pa- 3–6 9 (50) 9 (50)
tients, of whom 6% improved to a GCS score of 14 or 15.
The remaining 67% of patients had GCS scores ≤ 11 at 7 or 8 31 (40) 46 (60)
discharge (Fig. 1 upper). basal exudates 0.19
Of the 40 patients with documented follow-up, 18 present 31 (46) 37 (54)
(45%) had a GOS score of 4 or 5 at follow-up, which was absent 9 (33) 18 (67)
considered a favorable outcome (Fig. 1 lower). All 18 of infarcts 0.24
these patients were independent in their activities, and present 11 (35) 20 (65)
most children were attending school and playing. The to-
tal number of deaths in this study was 11 (28%). absent 29 (45) 35 (55)
procedure 0.43
Factors Influencing Outcome direct shunt 21 (40) 31 (60)
We analyzed the factors influencing short- and long- EVD followed by shunt 19 (44) 24 (56)
term outcomes separately. GCS score at discharge 0.24
Short-Term Outcomes. The patient population was ≥12 11 (36) 20 (64)
divided into 2 groups on the basis of age. Taking 18 years <12 29 (45) 35 (55)
as the cut off, we observed that a larger percentage of
* There were no statistically significant differences with respect to any
patients younger than 18 years had GCS scores ≥ 12 at
discharge; this finding showed only a trend toward statis- of the variables. Abbreviation: FU = follow-up.
tical significance (p = 0.08; Table 3). On further analysis,
we found that very young children (younger than 3 years) Long-Term Outcome. In contrast to short-term out-
had a statistically significant, worse short-term outcome come, GCS score at presentation was the sole predictor of
than older patients. Hence, there was a clear indication long-term outcome, assessed in terms of follow-up GOS
that younger patients have a worse outcome compared to score (Table 4). A significantly larger percentage of pa-
their older counterparts. This finding held true even on tients with a GCS scores of 7 or 8 at presentation had
multivariate analysis (binary logistic regression model) a favorable follow-up GOS score (4 or 5). More impor-
where only age (p = 0.03, OR 3.04) emerged as an inde- tantly, GCS score at presentation (p = 0.02, OR 26.47) re-
pendent predictor of outcome (see Table 5). tained its independent prognostic value in the multivari-
Furthermore, patients with a short duration of altered ate model (Table 5). On the other hand, age, duration of
sensorium (≤ 3 days) had a relatively better outcome than symptoms or altered sensorium, and presence or absence
those with a longer duration. This trended toward statisti- of infarcts or basal exudates did not correlate with long-
cal significance (p = 0.059). Presence or absence of in- term outcome.
farcts or basal exudates, duration of symptoms, and, sur-
Direct Shunt Placement Versus EVD First
prisingly, GCS score at presentation did not correlate with
short-term outcome. Imaging studies obtained in patients Of the 95 patients, 52 underwent direct VP shunt
with or without infarcts who had varying outcomes are placement and the remaining 43 received EVDs before
presented in Fig. 2 and discussed in the figure legend. VP shunt placement, for reasons discussed above. Corre-
178 J Neurosurg: Pediatrics / Volume 4 / August 2009
Shunt placement in poor-grade TBM with hydrocephalus
TABLE 3: Summary of the influence of various factors on
short-term outcome in all 95 patients
No. of Patients (%)
Discharge Discharge
No. of GCS Score GCS Score p
Variable Patients ≤11 ≥12 Value
age (yrs)
group 1 0.08
≤18 57 42 (74) 15 (26)
>18 38 22 (58) 16 (42)
group 2 0.02
≤3 33 27 (82) 6 (18)
>3 62 37 (60) 25 (40)
duration of symptoms 0.47
(days)
≤21 48 33 (69) 15 (31)
>21 47 31 (66) 16 (34)
duration of altered sen- 0.059
sorium (days)
≤3 52 31 (60) 21 (40)
>3 43 33 (77) 10 (23)
GCS score at presentation 0.22
3–6 18 14 (78) 4 (22)
Fig. 1. Upper: Bar graph showing short-term outcomes in terms of 7 or 8 77 50 (65) 27 (35)
GCS scores at discharge (GCS @ d/s) in all 95 patients. Lower: Bar
graph showing long-term outcomes in terms of follow-up GOS scores basal exudates 0.20
(GOS @ f/u) in the 40 patients in whom follow-up data were available. present 68 48 (71) 20 (29)
absent 27 16 (59) 11 (41)
lations for outcome were drawn with discharge GCS and
follow-up GOS scores. infarcts 0.11
Of the 52 patients who underwent direct VP shunt place- present 31 24 (77) 7 (23)
ment, 17 (33%) improved to a GCS score ≥ 12 at discharge. absent 64 40 (62) 24 (38)
Among the 43 who received EVDs first, 18 improved to
a GCS score > 8 prior to VP shunt placement. Neverthe-
less, the remaining 25 patients who remained in Grade IV TBM. Although VP shunts have generally been consid-
after EVD insertion also underwent VP shunt placement. ered beneficial in Grade II and III TBM with hydrocepha-
Of these, 12 (48%) had improved to Grade III at discharge. lus,1,10,12 their role in patients in Grade IV is controversial,
Most notably, 6 patients (24%) improved to discharge GCS with several studies recommending VP shunts in these
scores ≥ 12, a percentage not significantly different from cases only if the patient shows improvement after EVD
that in patients who improved to the same level after direct placement.1,10,12 This recommendation is because the un-
VP shunt placement (Fig. 3 upper). This observation stress- derlying cause of altered sensorium is multifactorial and
es the importance of VP shunt insertion even in patients cannot be attributed solely to the presence of hydrocepha-
who do not show improvement with a trial EVD. lus.10 Nevertheless, no study has compared the outcome
Among the 40 patients in whom follow-up was avail- after VP shunt placement in a large homogenous sample
able, 19 underwent EVD placement prior to receiving a VP of patients in Grade IV TBM with hydrocephalus.
shunt, and 21 received a direct VP shunt. Of the 21 patients
who underwent direct VP shunt placement, 13 (62%) had Outcome of VP Shunt Placement in Grade IV TBM With
improved to a GOS score of 4 or 5 at follow-up. Of the 19 Hydrocephalus
patients who received an EVD first, 8 improved to Grade In 1971, Bhagawati3 reported on his experience in a
II or III prior to VP shunt placement, and of these, 3 (38%) limited group of 5 patients with TBM and hydrocepha-
had GOS scores of 4 or 5 at follow-up. Of the 11 patients lus with altered sensorium who received ventriculoatrial
who did not improve after EVD placement, 2 (18%) had shunts. All 5 patients’ conditions improved, and their hemi-
GOS scores of 4 or 5 at follow-up (Fig. 3 lower). plegia, aphasia, and blindness almost completely resolved.
However, recent studies have not been able to duplicate
Discussion these results. In their series of 7 patients, Palur et al.12 re-
ported a mortality rate of 100%. Mathew and colleagues10
Ventriculoperitoneal shunt placement has been the also reported a high mortality rate in their 12 patients with
standard method to relieve hydrocephalus in patients with Grade IV TBM with hydrocephalus. The only patient who
J Neurosurg: Pediatrics / Volume 4 / August 2009 179
U. Srikantha et al.
TABLE 4: Summary of the influence of various factors on long-
term outcome*
No. of Patients (%)
FU GOS FU GOS
No. of Score Score p
Variable Patients 1–3 4 or 5 Value
age (yrs)
group 1 0.29
≤18 26 13 (50) 13 (50)
>18 14 9 (64) 5 (36)
group 2 0.59
≤3 13 7 (54) 6 (46)
>3 27 15 (56) 12 (44)
duration of symptoms (days) 0.51
≤21 21 12 (57) 9 (43)
>21 19 10 (53) 9 (47)
duration of altered sensorium
0.60
(days)
≤3 22 12 (55) 10 (45)
>3 18 10 (56) 8 (44)
GCS score at presentation 0.02
3–6 9 8 (89) 1 (11)
7 or 8 31 14 (45) 17 (55)
Fig. 2. Preoperative CT scans obtained in 4 different patients who
received VP shunts. All patients had hydrocephalus with periventricu- basal exudates 0.63
lar lucency. A: Scan in a patient with a favorable long-term outcome present 31 17 (55) 14 (45)
(follow-up GOS score of 5). B: Scan showing infarct in the right basal absent 9 5 (56) 4 (44)
ganglia. Despite this, the patient had a favorable outcome. C and D:
Scans obtained in patients who did not improve after VP shunt place- infarcts 0.37
ment. The patient shown in panel C had a poor follow-up GOS score, present 11 7 (64) 4 (36)
and the patient in panel D died of the disease. absent 29 15 (52) 14 (48)
survived in their series showed clinical deterioration in the * Follow-up data were available in 40 patients.
ward from Grade I to IV, and was successfully returned
to normal functional status because of early intervention.
Agrawal et al.1 reported a mortality rate of 40% among ed follow-up. The overall mortality rate among patients
their 6 patients, and all survivors were left with major with available follow-up was 28% (11 of 40), which could
disabilities. In the 28-case series of Karande et al.,7 40% be on the higher side as the follow-up rate was poor.
of patients died and 46% survived with severe disabili-
ties; only 14% made a complete recovery. The authors of Factors Predicting Outcome
another study concluded that although the results of VP Several factors have been identified as prognostic vari-
shunt placement are far from satisfactory, early shunt de- ables in TBM. In their multivariate analysis of prognostic
ployment still remains the best option to prevent long-term variables, Misra et al.,11 identified age, grade of TBM, pres-
neurological sequelae.13 Lamprecht and colleagues9 noted ence of cranial nerve palsies, and severity of hydrocephalus
good outcomes in 8.3% of their 36 patients with Medical as prognostic variables. Kalita et al.,6 in their multivariate
Research Council Grade III TBM, and no good outcomes analysis, have recognized the presence of focal motor defi-
among those who presented with GCS scores of 3–5. The cits as the most important predictor of delayed sequelae.
major limitations of the above series is obviously the small The other factors were GCS score, shunt surgery, and
number of included cases. bacille Calmette-Guérin vaccination. Karande and asso-
In the present study, we evaluated the outcome in 95 ciates7 identified clinical variables predictive of complete
cases of Grade IV TBM with hydrocephalus with known recovery, survival with disability, and death separately. In
outcomes at follow-up in 40 cases. A favorable short-term their study, only presence of deep coma and the absence of
outcome was demonstrated in 33% of our patients. More extrapyramidal movements at presentation were associated
importantly, 18 (45%) of the 40 patients with follow-up with death. Misra et al.11 and Kalita et al.5 identified pres-
information available had a favorable long-term outcome. ence of focal deficits and infarctions as important predic-
This might be an erroneously high percentage of good tors of outcome at 3 and 6 months, respectively. However,
long-term outcomes, however, as it is possible that people all of these factors have been identified in groups that in-
with worse outcomes or who died would not have attend- cluded only a small portion of Grade IV patients. No study
180 J Neurosurg: Pediatrics / Volume 4 / August 2009
Shunt placement in poor-grade TBM with hydrocephalus
TABLE 5: Summary of the influence of various factors on short- and long-term outcome in a multivariate model*
No. of Short-Term Outcome Long-Term Outcome
Variable Patients p Value Exp(B) 95% CI for Exp(B) p Value Exp(B) 95% CI for Exp(B)
age (yrs) 0.03 3.040 1.097–8.430 0.224 0.307 0.046–2.056
≤3 13
>3 27
duration of symptoms (days) 0.871 1.085 0.407–2.891 0.417 1.998 0.375–10.643
≤21 21
>21 19
duration of altered sensorium (days) 0.126 2.141 0.807–5.682 0.194 3.498 0.529–23.13
≤3 22
>3 18
GCS score at presentation 0.438 1.675 0.454–6.181 0.021 26.47 1.633–429.3
3–6 9
7 or 8 31
basal exudates 0.829 0.887 0.297–2.645 0.489 0.499 0.069–3.582
present 31
absent 9
infarcts 0.229 1.931 0.660–5.646 0.388 2.155 0.376–12.34
present 11
absent 29
* Short-term outcome data were available in 95 patients, and long-term outcome in 40.
has so far identified factors predicting outcome in Grade made by Mathew et al.10 in Grade III patients. These au-
IV TBM with hydrocephalus. thors placed EVDs in 13 patients with Grade III TBM
In our series including only Grade IV TBM with hy- with hydrocephalus, and irrespective of improvement
drocephalus, age and duration of altered sensorium corre- after EVD placement, they instituted VP shunts in all
lated with short-term outcome. A younger age was associ- patients. Mathew and colleagues observed that of the 6
ated with a worse short-term outcome, probably because patients with Grade III TBM with hydrocephalus who did
of the increased production of exudates and the formation not improve with an EVD, 4 were functionally normal at
of adhesive leptomeningitis in them.10 The GCS score at follow-up after VP shunt placement. These authors there-
presentation, although not predictive of short-term out- fore recommended that all patients in Grade III should
come, was the sole predictor of outcome in the long-term. be given the benefit of VP shunt placement, irrespective
Patients who presented with GCS scores of 7 or 8 fared of their response to a trial of EVD; these results were not
better than those who presented with a lower score. extrapolated to patients in Grade IV, however.
In the present study, all patients in Grade IV received
Role of Prior EVD VP shunts irrespective of their response to a trial of EVD.
Palur et al.12 treated all of their Grade IV patients with Moreover, EVDs were instituted only in the presence of se-
direct VP shunt placement and reported a 100% mortal- vere biochemical or hematological derangements requiring
ity rate. However, their sample size of 7 was very small. correction before the patient could receive general anesthe-
These authors proposed that patients in Grade IV TBM sia. We observed that among the patients who underwent
with hydrocephalus should undergo VP shunt placement direct VP shunt placement, 32.6% had favorable short-term
only if clinical improvement is shown after an EVD trial. outcomes, and 62% had favorable long-term outcomes.
Following this protocol, Mathew et al.10 instituted EVDs This observation, in itself, emphasizes the effectiveness
in 12 patients with Grade IV TBM with hydrocephalus, of direct VP shunt implantation in patients in Grade IV
and only 1 patient showed improvement. This patient’s without a trial of EVD. Moreover, even with no response to
condition deteriorated in the ward from Grade I to IV, EVD, 24% of patients had a favorable short-term outcome,
and he received immediate medical attention. The patient and 18% had a favorable long-term outcome after shunt
subsequently underwent VP shunt placement and was placement. This is similar to the observation of Mathew
neurologically normal at follow-up. The other patients et al.10 in Grade III cases, which we have shown holds true
died of TBM. Agrawal and colleagues1 performed VP in Grade IV TBM with hydrocephalus as well. We believe
shunt placements in 6 patients who showed improvement that a trial of EVD for a short duration (48–72 hours) is
after receiving EVDs, and reported a 40% mortality rate; inadequate to judge improvement. Cerebrospinal fluid di-
all surviving patients had severe disabilities. version is the only treatment we can offer these patients
An interesting point to note here is the observation apart from ATT, steroids, and supportive care. Hence, we
J Neurosurg: Pediatrics / Volume 4 / August 2009 181
U. Srikantha et al.
Fig. 3. Upper: Flowchart showing short-term outcomes in all 95 patients who underwent either direct VP shunt placement
or received an EVD first. Lower: Flowchart showing long-term outcomes in the 40 patients in whom follow-up was available.
Patients are grouped according to whether they received a VP shunt directly or an EVD first. V. = ventricular.
believe that unless there are major contraindications, VP even in Grade IV TBM with hydrocephalus managed with
shunts should be placed in these patients. However, caution VP shunt placement, ATT, and steroids. Age and duration
and clinical judgement should be exercised in patients with of altered sensorium predict short-term outcome, while
GCS scores of 3–6 and extensive infarcts, as the likelihood GCS score at presentation predicts long-term outcome.
of improvement in these patients is very small. Direct VP shunt placement is an effective option in pa-
There are obvious limitations to this study, including tients in Grade IV, and should be considered even in those
its retrospective nature and the relatively poor follow-up in who do not show improvement after EVD placement. A
the included cases. Although the follow-up group has been prior trial of EVD is not necessary in all cases, should be
shown not to be different from the entire group, whether used only as a temporary measure when necessary, and
the outcome can be projected onto the entire group can should be followed up with a VP shunt in most cases.
always be questioned. This is the only study to exclusively
examine Grade IV TBM with hydrocephalus with such a Disclaimer
large number of cases. In addition, we have unequivocally
shown the effectiveness of direct VP shunt placement in The authors report no conflict of interest concerning the mate-
terms of both short- and long-term outcome. rials or methods used in this study or the findings specified in this
paper.
Conclusions References
In summary, we demonstrated improved outcomes 1. Agrawal D, Gupta A, Mehta VS: Role of shunt surgery in pe-
182 J Neurosurg: Pediatrics / Volume 4 / August 2009
Shunt placement in poor-grade TBM with hydrocephalus
diatric tubercular meningitis with hydrocephalus. Indian Pe- 10. Mathew JM, Rajshekhar V, Chandy MJ: Shunt surgery in poor
diatr 42:245–250, 2005 grade patients with tuberculous meningitis and hydrocepha-
2. Ahuja GK, Mohan KK, Behari PM: Diagnostic criteria for tu- lus: effects of response to external ventricular drainage and
berculous meningitis and their validation. Tuber Lung Dis other variables on long term outcome. J Neurol Neurosurg
75:149–152, 1994 Psychiatry 65:115–118, 1998
3. Bhagwati SN: Ventriculoatrial shunt in tuberculous meningi- 11. Misra UK, Kalita J, Srivastava M, Mandal SK: Prognosis of
tis with hydrocephalus. J Neurosurg 35:309–313, 1971 tubercular meningitis: a multi-variate analysis. J Neurol Sci
4. Deshpande DH, Bharucha EP, Mondkar VP: Tuberculous 137:57–61, 1996
meningitis in adults: a clinico-pathological study of 18 cases. 12. Palur R, Rajshekhar V, Chandy MJ, Joseph T, Abraham J:
Neurol India 17:28–34, 1969 Shunt surgery for hydrocephalus in tuberculous meningitis: a
5. Kalita J, Misra UK: Outcome of tuberculous meningitis at 6 long-term follow-up study. J Neurosurg 74:64–69, 1991
and 12 months: a multivariate regression analysis. Int J Tu- 13. Sil K, Chatterji S: Shunting in tuberculous meningitis: a neuro-
berc Lung Dis 3:261–265, 1999 surgeons’s nightmare. Childs Nerv Syst 24:1029–1032, 2008
6. Kalita J, Misra UK, Ranjan P: Predictors of long-term neu- 14. Tandon PN, Bhatia R, Bhargava S: Tuberculous meningitis,
rological sequelae of tuberculous meningitis: a multivariate in Vinken PJ, Bruyn GW, Klawans HL (eds): Handbook of
analysis. Eur J Neurol 14:33–37, 2007 Clinical Neurology: Microbial Disease. Amsterdam: El-
7. Karande S, Gupta V, Kulkarni M, Joshi A: Prognostic clinical sevier, 1988, Vol 52, pp 195–226
variables in childhood tuberculous meningitis: an experience
from Mumbai, India. Neurol India 53:191–195, 2005
8. Kemalogu S, Ozkan U, Bukte Y, Ceviz A, Ozates M: Timing Manuscript submitted October 1, 2008.
of shunt surgery in childhood tuberculous meningitis with Accepted March 31, 2009.
hydrocephalus. Pediatr Neurosurg 37:194–198, 2002 Address correspondence to: Paritosh Pandey, M.Ch., Associate
9. Lamprecht D, Schoeman J, Donald P, Hartzenberg H: Ventric- Professor, Department of Neurosurgery, National Institute of Mental
uloperitoneal shunting in childhood tuberculous meningitis. Health and Neurosciences, Bangalore–29, India. email: paritosh2000
Br J Neurosurg 15:119–125, 2001 @gmail.com.
J Neurosurg: Pediatrics / Volume 4 / August 2009 183
You might also like
- Neil v. Watson - The Mind's Machine - Foundations of Brain and Behavior-Sinauer AssociatesDocument622 pagesNeil v. Watson - The Mind's Machine - Foundations of Brain and Behavior-Sinauer AssociatesChumchum Kumar100% (12)
- BSBLDR511 Develop and Use Emotional IntelligenceDocument13 pagesBSBLDR511 Develop and Use Emotional IntelligenceLayla Correa da SilvaNo ratings yet
- Critical Care Goals and ObjectivesDocument28 pagesCritical Care Goals and ObjectivesjyothiNo ratings yet
- Short-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyDocument12 pagesShort-Term Outcome of Proliferative Lupus Nephritis A Single Center StudyTJPRC PublicationsNo ratings yet
- SPIROMETRYDocument9 pagesSPIROMETRYaeyousefNo ratings yet
- Ijcp-5481 oDocument6 pagesIjcp-5481 oDebasis ChatterjeeNo ratings yet
- Adult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesDocument9 pagesAdult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesMutiara RizkyNo ratings yet
- Euro J of Neurology - 2023 - Doorn - European Academy of Neurology Peripheral Nerve Society Guideline On Diagnosis andDocument29 pagesEuro J of Neurology - 2023 - Doorn - European Academy of Neurology Peripheral Nerve Society Guideline On Diagnosis andjcr87No ratings yet
- Ijvm2014 531689 PDFDocument6 pagesIjvm2014 531689 PDFReka HariskianaNo ratings yet
- Lucas 2014Document8 pagesLucas 2014Prima YosiNo ratings yet
- Spirometry in Children: Clinical ReviewDocument9 pagesSpirometry in Children: Clinical ReviewMoonNo ratings yet
- Misra 2012Document7 pagesMisra 2012Carlos RiquelmeNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document4 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Riri KumalaNo ratings yet
- Chronic Kidney Disease : Hypertensive and Diabetic Retinopathy in PatientsDocument7 pagesChronic Kidney Disease : Hypertensive and Diabetic Retinopathy in PatientsAnonymous FgT04krgymNo ratings yet
- Effect of Prednisolone During Defervescence in Dengue Haemorrhagic Fever: An Open Label Controlled StudyDocument4 pagesEffect of Prednisolone During Defervescence in Dengue Haemorrhagic Fever: An Open Label Controlled StudyFabiola StellaNo ratings yet
- Red Blood Cell Transfusion: Decision Making in Pediatric Intensive Care UnitsDocument7 pagesRed Blood Cell Transfusion: Decision Making in Pediatric Intensive Care UnitsIndra AjaNo ratings yet
- A Clinical Study of Tuberculous Cervical LymphadenDocument5 pagesA Clinical Study of Tuberculous Cervical LymphadenAgung DewanggaNo ratings yet
- Gupta 2013Document5 pagesGupta 2013Dhruv MahajanNo ratings yet
- Benign Paroxysmal Positional Vertigo: Opportunities SquanderedDocument8 pagesBenign Paroxysmal Positional Vertigo: Opportunities SquanderedNia UtariNo ratings yet
- Subglottic Stenosis in Granulomatosis With Polyangiitis: The Role of Laryngotracheal ResectionDocument5 pagesSubglottic Stenosis in Granulomatosis With Polyangiitis: The Role of Laryngotracheal ResectionSamNo ratings yet
- Splenectomy in Children With Chronic ITP: Long-Term Efficacy and Relation Between Its Outcome and Responses To Previous TreatmentsDocument4 pagesSplenectomy in Children With Chronic ITP: Long-Term Efficacy and Relation Between Its Outcome and Responses To Previous TreatmentsVladimir Henry Triguero RosalesNo ratings yet
- Management Outcomes of Hydrocephalus Among Under Five Children in A Tertiary Hospital in Gombe North Eastern NigeriaDocument4 pagesManagement Outcomes of Hydrocephalus Among Under Five Children in A Tertiary Hospital in Gombe North Eastern NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Operative Versus Nonoperative Treatments For Legg-Calve - Perthes Disease: A Meta-AnalysisDocument9 pagesOperative Versus Nonoperative Treatments For Legg-Calve - Perthes Disease: A Meta-Analysisyarianna2No ratings yet
- Lovastatin For The Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled TrialDocument9 pagesLovastatin For The Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled TrialBpmStfbNo ratings yet
- 12 11 PBDocument168 pages12 11 PBYS NateNo ratings yet
- Claudia Craven VENTRICULOMEGALY CLASSIFICATIONDocument17 pagesClaudia Craven VENTRICULOMEGALY CLASSIFICATIONGUI VINCENo ratings yet
- Serum Thyroid-Stimulating Hormone Is An Independent Risk Factor of Recurrent Guillain-Barré SyndromeDocument41 pagesSerum Thyroid-Stimulating Hormone Is An Independent Risk Factor of Recurrent Guillain-Barré SyndromeDr NIVEDITHA CNo ratings yet
- Content ServerDocument8 pagesContent ServerG. Araya MoraNo ratings yet
- Clin Infect Dis. 2004 Tunkel 1267 84 Idsa MeningitiDocument18 pagesClin Infect Dis. 2004 Tunkel 1267 84 Idsa MeningitiJesus Salvador SerratoNo ratings yet
- Case Studies of Lower Respiratory Tract InfectionsDocument25 pagesCase Studies of Lower Respiratory Tract InfectionsMarianNo ratings yet
- Tourniquet TestingDocument6 pagesTourniquet TestingPatrick RamosNo ratings yet
- Tto Crup NatureDocument7 pagesTto Crup NatureCarolina Mora RuedaNo ratings yet
- Kwong 2012Document8 pagesKwong 2012Ke XuNo ratings yet
- To Study Hematological Profile in Covid-19 Patients in Relation With Prognosis and Outcome: - A Cross Sectional Observational StudyDocument7 pagesTo Study Hematological Profile in Covid-19 Patients in Relation With Prognosis and Outcome: - A Cross Sectional Observational StudyIJAR JOURNALNo ratings yet
- PESI Critical Care 2005Document6 pagesPESI Critical Care 2005Rocio Méndez FrancoNo ratings yet
- A Prospective Observational Study of Dengue Fever With Thrombocytopenia With Reference To TreatmentDocument6 pagesA Prospective Observational Study of Dengue Fever With Thrombocytopenia With Reference To Treatment-Tony Santoso Putra-No ratings yet
- Pediatric Hematology Oncology JournalDocument4 pagesPediatric Hematology Oncology JournalmitraNo ratings yet
- Long-Term Clinical Outcome of Fetal Cell Transplantation For Parkinson Disease Two Case ReportsDocument5 pagesLong-Term Clinical Outcome of Fetal Cell Transplantation For Parkinson Disease Two Case Reportsjust for download matterNo ratings yet
- Cerebral Venous Thrombosis: Clinical Predictors and Emerging TreatmentsDocument3 pagesCerebral Venous Thrombosis: Clinical Predictors and Emerging Treatmentschartreuse avonleaNo ratings yet
- Chest: Point/Counterpoint EditorialsDocument3 pagesChest: Point/Counterpoint Editorialsgiseladelarosa2006No ratings yet
- Comparison of Repositioning Maneuvers For Benign Paroxysmal Positional Vertigo of Posterior Semicircular Canal: Advantages of Hybrid ManeuverDocument6 pagesComparison of Repositioning Maneuvers For Benign Paroxysmal Positional Vertigo of Posterior Semicircular Canal: Advantages of Hybrid ManeuverFayza RihastaraNo ratings yet
- GBS PDTDocument8 pagesGBS PDTabdulkadirmunsyNo ratings yet
- VP Shunt For Meningitis TBDocument9 pagesVP Shunt For Meningitis TBNindi LizenNo ratings yet
- Emboli ParuDocument10 pagesEmboli Paruindry_purnamasariNo ratings yet
- 10.1007@s12098 020 03454 1Document6 pages10.1007@s12098 020 03454 1rayhantaswinNo ratings yet
- DIC in Abruptio 2Document5 pagesDIC in Abruptio 2HoneylynNo ratings yet
- Comparison of 3 Clinical Models For Predicting The Probability of Pulmonary EmbolismDocument8 pagesComparison of 3 Clinical Models For Predicting The Probability of Pulmonary EmbolismAlirio Rodrigo Bastidas GoyesNo ratings yet
- Fluctuaciones Relacionadas A Tratamiento GBDocument7 pagesFluctuaciones Relacionadas A Tratamiento GBOsvaldo CortésNo ratings yet
- Decompressive Hemicraniectomy and DuroplastyDocument5 pagesDecompressive Hemicraniectomy and DuroplastyAmy NilifdaNo ratings yet
- JHM 2112Document4 pagesJHM 2112senkonenNo ratings yet
- Achondroplasia Natural History Study (CLARITY)Document7 pagesAchondroplasia Natural History Study (CLARITY)jakelinelagoadvNo ratings yet
- Lung Ultrasound Dry WeightDocument16 pagesLung Ultrasound Dry WeightBhanu KumarNo ratings yet
- Restrictive Fluids in Septic Shock. NEJM 2022Document12 pagesRestrictive Fluids in Septic Shock. NEJM 2022neeraj SinghNo ratings yet
- Neutrophil To Lymphocyte Ratio in Diagnosis of Complicated and Non-Complicated AppendicitisDocument7 pagesNeutrophil To Lymphocyte Ratio in Diagnosis of Complicated and Non-Complicated AppendicitisHamza AhmedNo ratings yet
- Baca IniDocument9 pagesBaca IniRahmi Annisa MaharaniNo ratings yet
- Wetzel2020 Article Flow-regulatedVersusDifferentiDocument7 pagesWetzel2020 Article Flow-regulatedVersusDifferenticNo ratings yet
- Neurourology and Urodynamics - 2022 - Martin - Is Sacral Neuromodulation Effective in Patients With Parkinson S Disease ADocument7 pagesNeurourology and Urodynamics - 2022 - Martin - Is Sacral Neuromodulation Effective in Patients With Parkinson S Disease AElkin JNo ratings yet
- Kansal 2018Document1 pageKansal 2018Sheena Mae MansinadesNo ratings yet
- 1 s2.0 S074152140290621X MainDocument6 pages1 s2.0 S074152140290621X Main1751010307No ratings yet
- GBS European Guidelines 2023Document29 pagesGBS European Guidelines 2023Saurabh AgrawalNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Abdominal Acupuncture For DepressionDocument35 pagesAbdominal Acupuncture For DepressionAGNESE YOLOTZIN OLIVERA TORO REYESNo ratings yet
- Cannabis Legal Regulatory Update April June 2019Document19 pagesCannabis Legal Regulatory Update April June 2019stonerhinoNo ratings yet
- Research in Primary Dental Care 1 PDFDocument4 pagesResearch in Primary Dental Care 1 PDFMARIA NAENo ratings yet
- الإجازات المرضية - منصة صحةDocument2 pagesالإجازات المرضية - منصة صحةShatha miNo ratings yet
- Region of Waterloo Job DescriptionDocument4 pagesRegion of Waterloo Job Descriptionbeth aguirreNo ratings yet
- Ebsco Fulltext 2024 03 20Document17 pagesEbsco Fulltext 2024 03 20api-733905896No ratings yet
- MSDS GINKGOLON-24 (Ginkgo Biloba Ext)Document3 pagesMSDS GINKGOLON-24 (Ginkgo Biloba Ext)Selviani Dwi MuryantiNo ratings yet
- 2-NBDG As A Fluorescent Indicator For Direct Glucose Uptake MeasurementDocument9 pages2-NBDG As A Fluorescent Indicator For Direct Glucose Uptake MeasurementPili CárdenasNo ratings yet
- Hospital Management Domain ModelDocument4 pagesHospital Management Domain Modelvinod kapateNo ratings yet
- PD Lesson 5 Coping With Stress in Middle and Late AdolescenceDocument16 pagesPD Lesson 5 Coping With Stress in Middle and Late AdolescenceEL FuentesNo ratings yet
- Developmental DelayDocument79 pagesDevelopmental DelayNaveen KumarNo ratings yet
- Glycolic Acid SdsDocument11 pagesGlycolic Acid SdsJuthi RahmanNo ratings yet
- Cardio DrugsDocument58 pagesCardio DrugsMARIA ROWENA VIA J. LUCENANo ratings yet
- Management Is Nothing More Than Motivating Other People GHEORGHE MDocument6 pagesManagement Is Nothing More Than Motivating Other People GHEORGHE MCristina PaliuNo ratings yet
- Buntis Congress Report 2021Document24 pagesBuntis Congress Report 2021Giselle ArenasNo ratings yet
- Antibiotic Prophylaxis OrthoDocument4 pagesAntibiotic Prophylaxis OrthoDonNo ratings yet
- Prosthesis For Long Span Kennedy's Class III Partially Edentulous Condition: A Case ReportDocument5 pagesProsthesis For Long Span Kennedy's Class III Partially Edentulous Condition: A Case ReportRiana WidiantyNo ratings yet
- HMB342 Course Syllabus Summer 2020Document5 pagesHMB342 Course Syllabus Summer 2020WangNo ratings yet
- Lifting Plan: Table of ContentDocument11 pagesLifting Plan: Table of ContentkhurramNo ratings yet
- ICN Framework of Disaster NursingDocument18 pagesICN Framework of Disaster NursingKRIZIA ANE A. SULONG100% (1)
- Element - 45 - 978-Design ReportDocument15 pagesElement - 45 - 978-Design ReportLeeNo ratings yet
- Product: A Product Is Anything That Can Be Offered To A Market To Satisfy A Want or NeedDocument12 pagesProduct: A Product Is Anything That Can Be Offered To A Market To Satisfy A Want or NeedSumon Das DasNo ratings yet
- Disability and Life Writing: Reports From The Nineteenth-Century AsylumDocument19 pagesDisability and Life Writing: Reports From The Nineteenth-Century AsylumHS22D001 MalavikaNo ratings yet
- UNIV144 Questions 2Document8 pagesUNIV144 Questions 2Clinton SmaugNo ratings yet
- Resume Igd Rsud PareDocument66 pagesResume Igd Rsud PareIqbalRazifNo ratings yet
- Pediatric Community Acquired PneumoniaDocument24 pagesPediatric Community Acquired PneumoniaJames Lagamayo JavierNo ratings yet
- PARENT AWARENESS SEMINAR-hand OutsDocument2 pagesPARENT AWARENESS SEMINAR-hand OutsLADY ANN GRACE LAGASNo ratings yet
- CPR Salbutamol+Ipratropium Neb (BRODIX PLUS) 35'sDocument2 pagesCPR Salbutamol+Ipratropium Neb (BRODIX PLUS) 35'sRacquel SolivenNo ratings yet