Professional Documents
Culture Documents
Ec Nyeri
Ec Nyeri
Uploaded by
dramione shipperCopyright:
Available Formats
You might also like
- Clinical Anatomy of Spine, Spinal Cord & ANS PDFDocument680 pagesClinical Anatomy of Spine, Spinal Cord & ANS PDFMajda Bajramović100% (8)
- Operative Techniques in Foot and Ankle Surgery 2nd Edition Ebook PDFDocument61 pagesOperative Techniques in Foot and Ankle Surgery 2nd Edition Ebook PDFmaurice.honeycutt512100% (51)
- Cervical Total Disc Replacement: Long-Term OutcomesDocument12 pagesCervical Total Disc Replacement: Long-Term OutcomesKyle RobinNo ratings yet
- The Ligament Injury Connection To Osteoarthritis: Wonder Why?Document11 pagesThe Ligament Injury Connection To Osteoarthritis: Wonder Why?Saifuddin HaswareNo ratings yet
- Knee Pain July 2014Document10 pagesKnee Pain July 2014Naeemur RahmanNo ratings yet
- Diagnosis and Treatment of Patients With Patellofemoral PainDocument10 pagesDiagnosis and Treatment of Patients With Patellofemoral PainRuben CapelaNo ratings yet
- Effect of Cold Warm or Contrast Therapy On Controlling Knee Osteoarthritis Associated ProblemsDocument7 pagesEffect of Cold Warm or Contrast Therapy On Controlling Knee Osteoarthritis Associated ProblemsIneMeilaniNo ratings yet
- Assessment of Chronic PainDocument7 pagesAssessment of Chronic PainFranciscoGarciaNo ratings yet
- Osteochondroma Fracture in Young Athlete Bfe9f44bDocument4 pagesOsteochondroma Fracture in Young Athlete Bfe9f44bViona Ananda putriNo ratings yet
- JSS College of PhysiotherapyDocument8 pagesJSS College of PhysiotherapyDANIA NAJUA BINTI ZAINALNo ratings yet
- Kehlet2002 Article ChronicPostherniorrhaphyPainACDocument4 pagesKehlet2002 Article ChronicPostherniorrhaphyPainACHarutyun AlaverdyanNo ratings yet
- Injury: Theodoros H. Tosounidis, Hassaan Sheikh, Martin H. Stone, Peter V. GiannoudisDocument7 pagesInjury: Theodoros H. Tosounidis, Hassaan Sheikh, Martin H. Stone, Peter V. GiannoudisWanda AndiniNo ratings yet
- Comprehensive Approach To The Evaluation of Groin.7Document13 pagesComprehensive Approach To The Evaluation of Groin.7cooperorthopaedicsNo ratings yet
- THR Painful Pietrzak2017Document7 pagesTHR Painful Pietrzak2017Mohan DesaiNo ratings yet
- Hip Bone Marrow Edema Presenting As Low Back Pain A Case ReportDocument10 pagesHip Bone Marrow Edema Presenting As Low Back Pain A Case ReportVizaNo ratings yet
- Nursing Care For Ederly in Osteoarthritis Case With Cronic Pain ProblemDocument13 pagesNursing Care For Ederly in Osteoarthritis Case With Cronic Pain ProblemMitha Amelia PutriNo ratings yet
- Osteoarthritis and Arthroplasty of The Hip and Knee 2018 PDFDocument6 pagesOsteoarthritis and Arthroplasty of The Hip and Knee 2018 PDFMarcelo Ramirez SiñanizNo ratings yet
- Osteoarthritis of The Hip: Clinical PracticeDocument9 pagesOsteoarthritis of The Hip: Clinical PracticeMarina Tomasenco - DaniciNo ratings yet
- Is Extracorporeal Shockwave Therapy Effective Even in The Treatment of Partial Rotator Cuff TearDocument6 pagesIs Extracorporeal Shockwave Therapy Effective Even in The Treatment of Partial Rotator Cuff TearmitchelNo ratings yet
- Facet Joint SyndromeDocument17 pagesFacet Joint Syndromepaulvaso27100% (1)
- Plantar Fasciitis A Review of Treatments.4Document5 pagesPlantar Fasciitis A Review of Treatments.4diki Tri MardiansyahNo ratings yet
- Sebastian2014 PDFDocument8 pagesSebastian2014 PDFArchita AgarwalNo ratings yet
- Efeitos Da Maturacao BiologicaDocument12 pagesEfeitos Da Maturacao BiologicalucasNo ratings yet
- International Journal of Surgery OpenDocument11 pagesInternational Journal of Surgery OpenSaugi HudaNo ratings yet
- Anterior Knee PainDocument10 pagesAnterior Knee PainfreireortoNo ratings yet
- S32.Full (Tanda Kuning)Document11 pagesS32.Full (Tanda Kuning)ahmadheulwanNo ratings yet
- Postoperative Pain in Neurosurgery: A Pilot Study SurgeryDocument5 pagesPostoperative Pain in Neurosurgery: A Pilot Study SurgeryCuenta LastNo ratings yet
- Common Overuse Tendon ProblemsDocument8 pagesCommon Overuse Tendon ProblemsmircoNo ratings yet
- Journal Parkinson 2013Document5 pagesJournal Parkinson 2013widyakamrulNo ratings yet
- Shoulder 2 Ada MriDocument4 pagesShoulder 2 Ada MriNirmalasari AnirNo ratings yet
- Chemical Hip Denervation For Inoperable Hip FractureDocument6 pagesChemical Hip Denervation For Inoperable Hip Fracturemanuel torresNo ratings yet
- Osteosarcoma Clinical Case by SlidesgoDocument12 pagesOsteosarcoma Clinical Case by SlidesgoLwhynnNo ratings yet
- Managing The Patient With Heel PainDocument5 pagesManaging The Patient With Heel Painmh8m58brjnNo ratings yet
- Activity 1 Concepts of PainnDocument8 pagesActivity 1 Concepts of Painncrishara palomoNo ratings yet
- Nijs Et Al 2021 LANCET RheumatologyDocument10 pagesNijs Et Al 2021 LANCET RheumatologyVicaroNo ratings yet
- Groin Pain Syndrome Known As Sports Hernia A ReviewDocument9 pagesGroin Pain Syndrome Known As Sports Hernia A Review1541920001 LUIS GUILLERMO PAJARO FRANCO ESTUDIANTE ACTIVO ESPECIALIDAD MEDICINA INTERNANo ratings yet
- Lower Limb Evaluation Format Lower Limb Fracture Assesstment FormDocument12 pagesLower Limb Evaluation Format Lower Limb Fracture Assesstment FormsridharNo ratings yet
- Journal of Bodywork & Movement Therapies: Adi Dor, BPT, Leonid Kalichman, PT, PHDDocument6 pagesJournal of Bodywork & Movement Therapies: Adi Dor, BPT, Leonid Kalichman, PT, PHDLaura Espejo SalamancaNo ratings yet
- Fracture and Joint Injuries (Shalter-Chapter 15) - Kelompok C (Dr. Oktavianus, SP - Ot)Document69 pagesFracture and Joint Injuries (Shalter-Chapter 15) - Kelompok C (Dr. Oktavianus, SP - Ot)Heru ChrisNo ratings yet
- 2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDocument15 pages2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDavid Alejandro Cavieres AcuñaNo ratings yet
- Anterior Knee Pain: Remember To Look Up and Be Aware of Structural AnomaliesDocument3 pagesAnterior Knee Pain: Remember To Look Up and Be Aware of Structural AnomaliesDaniel G. A. C.No ratings yet
- Phantom Limb Pain: Moon Suk Bang, MD, PHD, and Se Hee Jung, MD, MsDocument4 pagesPhantom Limb Pain: Moon Suk Bang, MD, PHD, and Se Hee Jung, MD, MsIgnacio AndrésNo ratings yet
- Chinese Journal of Traumatology: Phantom Limb Pain: A Literature ReviewDocument3 pagesChinese Journal of Traumatology: Phantom Limb Pain: A Literature ReviewEva Nur MalaNo ratings yet
- Diagnostics and Management of TemporomanDocument6 pagesDiagnostics and Management of TemporomanDr. Zardasht N. BradostyNo ratings yet
- Physiotherapy Management of Hip Osteoarthritis: Kim BennellDocument13 pagesPhysiotherapy Management of Hip Osteoarthritis: Kim BennellAndrei R LupuNo ratings yet
- Anterior Knee Pain in The Young AthleteDocument7 pagesAnterior Knee Pain in The Young AthleteAngelica GarciaNo ratings yet
- Reichenbach 2010Document6 pagesReichenbach 2010EriC. ChaN.No ratings yet
- 485-Article Text-605-1-10-20161227 PDFDocument10 pages485-Article Text-605-1-10-20161227 PDFJeg1No ratings yet
- JMT 23 162Document7 pagesJMT 23 162dark_PinchoNo ratings yet
- Clinical Review: OsteoarthritisDocument4 pagesClinical Review: OsteoarthritismarindadaNo ratings yet
- Joint Pain One PagerDocument3 pagesJoint Pain One PagermustafaNo ratings yet
- ArticlesDocument7 pagesArticlesSoha Arif ShaykhNo ratings yet
- Evaluation of Pain Levels and Management in Total Knee Replacement PatientsDocument10 pagesEvaluation of Pain Levels and Management in Total Knee Replacement PatientsBong Yi LinNo ratings yet
- Pain and Effusion and Quadriceps Activation and StrengthDocument6 pagesPain and Effusion and Quadriceps Activation and StrengthЯнь НгуенNo ratings yet
- Current Concept Management of Carpal Tunnel Syndrome: A Case ReportDocument17 pagesCurrent Concept Management of Carpal Tunnel Syndrome: A Case Reportwidiyah darmawanNo ratings yet
- Factores Que Afectan El Resultado Después de La Amputación Traumática de Una ExtremidadDocument14 pagesFactores Que Afectan El Resultado Después de La Amputación Traumática de Una Extremidadolalla de santosNo ratings yet
- OsteoartritisDocument9 pagesOsteoartritisWalter Espinoza CiertoNo ratings yet
- Mechanisms of Osteoarthritis (OA) PainDocument6 pagesMechanisms of Osteoarthritis (OA) Painedlinkusuma131No ratings yet
- Management L Low Back PainDocument7 pagesManagement L Low Back PainelsyamelindaNo ratings yet
- Plantar and Medial Heel Pain: Diagnosis and Management: Review ArticleDocument9 pagesPlantar and Medial Heel Pain: Diagnosis and Management: Review ArticleGhani AbdurahimNo ratings yet
- Sensibiliza o Central Nas Dores CR Nicas REVIEW LANCET 2021 - Open AccessDocument10 pagesSensibiliza o Central Nas Dores CR Nicas REVIEW LANCET 2021 - Open AccessRichard Mezadri ViebrantzNo ratings yet
- MRI of Degenerative Disease of the Spine: A Case-Based AtlasFrom EverandMRI of Degenerative Disease of the Spine: A Case-Based AtlasNo ratings yet
- National Hospital Insurance Fund PDFDocument292 pagesNational Hospital Insurance Fund PDFCargo ReeNo ratings yet
- Clinical Congress: ProgramDocument17 pagesClinical Congress: ProgramHassan HamzahNo ratings yet
- Orthotics - Ul & LLDocument48 pagesOrthotics - Ul & LLReena PremNo ratings yet
- Drexel University College of Medicine Department of AnesthesiologyDocument1 pageDrexel University College of Medicine Department of AnesthesiologydrexelanesthesiaNo ratings yet
- Recommended Reading List For EDAICDocument4 pagesRecommended Reading List For EDAICAna Belén Artero CastañoNo ratings yet
- MS - Foot and Toes - Slide10Document2 pagesMS - Foot and Toes - Slide10testNo ratings yet
- Airway Centric OrthoDocument6 pagesAirway Centric OrthoSrishti SyalNo ratings yet
- AO Surgery Reference Lenke ClassificationDocument1 pageAO Surgery Reference Lenke ClassificationFederico Nelson FreisNo ratings yet
- Session: I: Registration /breakfastDocument5 pagesSession: I: Registration /breakfastBhaskar BorgohainNo ratings yet
- Hospital Scorecard - DepartmentwiseDocument4 pagesHospital Scorecard - DepartmentwiseNatasha BhasinNo ratings yet
- Cosmetic Surgery EssayDocument7 pagesCosmetic Surgery Essayalisharenee0550% (2)
- Morphology of Cranial Sutures and RadiologicDocument6 pagesMorphology of Cranial Sutures and RadiologicEvans RodrigezNo ratings yet
- Mathogs Atlas of Craniofacial Trauma 2nd EditionDocument692 pagesMathogs Atlas of Craniofacial Trauma 2nd EditionCary Dee100% (1)
- EWMA Endorsements of Wound Centres Non Hospital Based ApplicationForm WordDocument17 pagesEWMA Endorsements of Wound Centres Non Hospital Based ApplicationForm WordCarlo BalzereitNo ratings yet
- 17 - Distal Radius FracturesDocument78 pages17 - Distal Radius FracturesFlorin Panduru100% (1)
- ACL Procedure & Tunnel Prep.: - Learning ObjectivesDocument17 pagesACL Procedure & Tunnel Prep.: - Learning ObjectivesIbrahim Syed MustafaNo ratings yet
- EVALUATION 1.1 THE ROLE OF NURSES IN THE OPERATING ROOM Unscramble SentencesDocument3 pagesEVALUATION 1.1 THE ROLE OF NURSES IN THE OPERATING ROOM Unscramble SentencesRonald Alfredo Gordillo PeraltaNo ratings yet
- The SAGES Safe Cholecystectomy ProgramDocument4 pagesThe SAGES Safe Cholecystectomy ProgramMikael AngelooNo ratings yet
- Comparative Study of Functional Outcome in Upper One Third Shaft Tibia Fractures With Suprapatellar and Infrapatellar Intramedullary Tibial NailingDocument8 pagesComparative Study of Functional Outcome in Upper One Third Shaft Tibia Fractures With Suprapatellar and Infrapatellar Intramedullary Tibial NailingakankshaNo ratings yet
- The Sample of PediatricsDocument47 pagesThe Sample of PediatricsWaseem UllahNo ratings yet
- Treatment of Supracondylar Femoral Fractures in Young Cats and Dogs Using "Arrow Pin" TechniqueDocument5 pagesTreatment of Supracondylar Femoral Fractures in Young Cats and Dogs Using "Arrow Pin" TechniqueVangelis PapachristosNo ratings yet
- Orthotics: A Report By: Kenneth Pierre M. LopezDocument94 pagesOrthotics: A Report By: Kenneth Pierre M. LopezAkbar AziziNo ratings yet
- Anchorage Considerations in Lingual OrthodonticsDocument4 pagesAnchorage Considerations in Lingual OrthodonticsSibi NairNo ratings yet
- Elbow Fractures: Distal Humerus: The American Society For Surgery of The Hand.)Document15 pagesElbow Fractures: Distal Humerus: The American Society For Surgery of The Hand.)Radu UrcanNo ratings yet
- The Flexion Gap in Normal Knees: An Mri StudyDocument4 pagesThe Flexion Gap in Normal Knees: An Mri StudyGERARDO TORRES RUIZNo ratings yet
- Norm Med TraumaDocument87 pagesNorm Med TraumaLibrería Médica PandoNo ratings yet
- PLX7100A BrochureDocument8 pagesPLX7100A Brochurealmotaz.khtNo ratings yet
Ec Nyeri
Ec Nyeri
Uploaded by
dramione shipperOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ec Nyeri
Ec Nyeri
Uploaded by
dramione shipperCopyright:
Available Formats
0353 5 Painful_Ferrata:- 15-09-2011 14:07 Pagina 19
Mini-review
Painful hip arthroplasty: definition
Paolo Ferrata significantly impaired in their daily activities by chronic pain (9).
Serafino Carta The occurrence of pain following a technically satisfactory arthro-
Mattia Fortina plasty is of concern for both the orthopaedic surgeon and the pa-
Daniele Scipio tient. It’s one of the most difficult challenges for the surgeon to eval-
Alberto Riva uate and to treat. The difficulties in managing painful THA is due
to the heterogeneous nature of the disease. Pain related to the
Salvatore Di Giacinto
surgery itself can be associated with the implant, bone alterations
and soft tissue or nerve injuries. The situation complicates when his-
tory, clinical examination, and plain radiography fail to locate the ex-
Orthopaedics and Traumatology Clinic act origin of hip pain. In few cases patients were revised without hav-
University Hospital of Siena, Siena, Italy ing found the cause of pain. In the total 299,368 primary THAs re-
ported in the Swedish Hip Register that were performed from 1979
to 2008, the 0,03% was revised for pain as a single cause repre-
Address for correspondence: senting the 0,4% of all the reasons for revision in the 24,199 first
Dr. Mattia Fortina revision THAs (10).
Orthopaedics and Traumatology Clinic, In order that the source of the pain be accurately located, a systematic
University Hospital of Siena - V.le Bracci 1, 53100 Siena, Italy approach is required. Surgeons and physicians must contend with
Phone: +39 0577 585675 numerous factors that can affect the patient outcomes.
Fax: +39 0577 233400 We have analyzed the predisposing factors that could lead to a painful
E-mail: tia1974@alice.it hip arthroplasty and we have investigated the possible causes of
this pain.
Summary
Painful HIP predisposing factors
Total hip arthroplasty (THA) has been indicated as the surgi-
cal intervention with greatest improvement in pain and physical
Prognostic factors influence the probability of response, remission,
function. However some patients continue to experience hip
recurrence and duration of pain after the operation. Determining prog-
pain after elective surgery. We investigate prognostic factors
nostic factors that affect treatment effectiveness is essential to clin-
that negatively affect treatment effectiveness and the patient
icians and important to patients in their decision-making.
outcome. The “hip region” constitutes the groin, buttock, up-
Many factors can affect the patient outcome, like patients’ preop-
per lateral thigh, greater trochanteric area, and the iliac crest.
erative status and characteristics, timing of operation, type of op-
Pain originating from various sources and not directly linked
eration, type of prosthesis and length of hospital stay but only few
to prosthesis may be perceived here and includes the lum-
of these seems to have a correlation with pain (11,12).
bosacral spine, referred pain from abdominal organs and soft
Age and pain. Some studies that examined age as potential pre-
tissue sources such as trochanteric bursitis, tendinitis, hip ab-
dictors of pain reported more pain in younger patients (13). Better
ductor dysfunction, and inguinal hernia. An accurate asses-
pain outcomes in the more elderly compared to younger patients
sment of the pain cause is extremely difficult to construct and
may be due to higher pain tolerance, lower physical demands for
a complete differential diagnosis is fundamental. We assess
sports-related activities and lower prevalence of subclinical anxiety
all the possible causes of hip pain after THA and we divide them
and depression. When results were adjusted for covariates of in-
depending on the presence or absence of radiographic signs.
terest and potential confounders, including gender, BMI, comorbidity,
KEY WORDS: total hip arthroplasty; pain; epidemiology; complication; revision. ASA class, operative diagnosis, depression, and anxiety, age of the
patient seems to be more important for the improvement in phys-
ical function than for the improvement in the pain score (11). Clarke
Introduction et al. confirmed in a prospective double blind randomized study that
age do not influence the outcome of pain (14). McGuigan et al. (15)
Total hip arthroplasty (THA) is one of the most clinically success- and Nilsdotter et al. (16) found that older patients had a degree of
ful and cost-effective interventions in health care, with excellent long- pain improvement similar to that experienced by those younger. The
term results in terms of reducing pain and improving function and postoperative functional limitation in more elderly is likely related to
quality of life in patients with debilitating hip disease (1-3). greater severity of other comorbidity (back problems, vision, and bal-
Self reported patient satisfaction has been reported to be closer to ance problems) and higher risk of arthritis in other lower extremity
90% (4). Many authors reported on successfully relieved pain af- joints. The preoperative subjective status is the only significant pre-
ter THA also in cases where patients’ preoperative functional sta- dictor of the six months self-perceived functional status. In other
tus was poor (5,6). Physical function improvement is long lasting words, the worst pre-operative self-perceived status was also the
over 25 years (7) and is not affected by mild pain (8). worst post-operative self-perceived status will be (17).
However, despite remarkable developments in surgical technique Gender and pain. The relationship between gender and pain is not
and implant design, some patients continue to experience distressing clear. Some studies reported that women experienced less post-
pain after elective surgery. Results from a Danish nationwide study operative pain than men (18). Bogoch et al. (19) found that women
found that 12.1% of patients 12-18 months after hip arthroplasty were had more pain than men, both preoperatively and postoperative-
Clinical Cases in Mineral and Bone Metabolism 2011; 8(2): 19-22 19
0353 5 Painful_Ferrata:- 15-09-2011 14:07 Pagina 20
P. Ferrata et al.
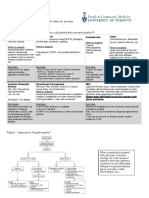
ly. However, equal proportions of women and men improved to good HIP pain causes
or excellent outcomes, such that women benefited from surgery slight-
ly more than men did. McGuigan et al. (15) and Halket et al. (16) Sequential plain radiographs is the universally used method for THA
noted that male gender was associated with a greater improvement evaluation and often reveals helpful features in diagnosing post-op-
after surgery with respect to pain scores than was female gender. erative pain. Surgeon directly face with x-rays at standard follow-
Singh et al. reported that at 2 and 5-years post-primary THA gen- up control so it is useful to divide the causes of hip pain in relation
der and age were not significantly associated with hip pain (17), but to the presence of radiographics sign.
female gender was associated with higher odds of NSAID and opi-
oid medication use. Positive X-rays
Commonly used outcome measures like VAS pain, SF-36 and WOM- 1. Aseptic Loosening: typical X-rays features are progressively in-
AC pain, stiffness, and function scores, can be flawed due to floor creasing lucent lines, cement fracture and component migra-
and ceiling effects. These effects are minimized in large cohort as tion, possible presence of osteolytic areas or even bone frac-
in the one reported in the Swedish Hip Register (10) with 21,804 tures. Pain characteristics: presence of a pain-free interval fol-
operations performed in 2004-2008. Women reported a greater pain lowing the operation, pain increased with activity or weight bear-
relief than men, measured on a VAS scale. However, women ex- ing and relieved with rest, pain that begins when starting to walk
perienced somewhat poorer satisfaction with the operation after one after sitting, sometimes pain presence at rest and at night also
year. Women reported a better effect of the intervention regarding (35). Tigh and leg pain indicate shaft mobilization, while groin
health-related quality of life and pain but are not as satisfied as men. and buttock symptoms are related to acetabular problems (36),
Obesity and pain. Body mass index (BMI) is regarded as one of even if totally mobilized cups can be completely asymptomatic.
the most useful measures of obesity and has been shown to have 2. Septic loosening: typical X-rays features are endosteal scalloping
a direct relationship with morbidity and mortality (22). Ibrahim et and multilamellar periosteal new bone formation, sometimes fo-
al. compared 179 hip arthroplasties in 162 patients with an aver- cal lysis of bone is present (37). Pain characteristics: it may pre-
age BMI of 22.5 (18.6-24.9) with 164 hip arthroplasties in 151 age- sent after a pain-free interval following the operation or be per-
matched patients with an average BMI of 33.3 (30-39.6). Six out sistent since surgery in relation with late or early onset of infection
of 138 (4.3%) and five out of 157 (3.2%) patients recorded bad pain respectively, it compares usually at rest and during night (38).
following their total hip replacement in groups 1 and 2 respectively. Infection is the most difficult and the main exclusion diagnosis
The difference in proportion was not significant (23). Kessler et al. to do principally when there are no radiographics sings yet.
found that no significant differences in postoperative functional sta- 3. Osteolysis: Pain characteristics: presence of a pain-free inter-
tus, stiffness, and pain were found among patients with normal- val following the operation, osteolysis is often silent, but in cas-
weight (BMI 25 kg/m2, n 11), overweight (BMI 25 to 29.9 kg/m2, es of severe bone loss, pain may be related to an impending
n 36), and obese (BMI 30 kg/m2, n 20), either 10 days or 3 months fracture in the greater trochanter, in the acetabulum or in the
postoperatively (24). Similarly Bolland et al., in 28,068 THAs found femoral shaft. Lysis without looseness has been described as
that at 1 and 2 years there was a fall in anti-inflammatory use, stud- a cause of hip pain in both cemented and uncemented hip re-
ied as a marker of effective pain relief, with similar magnitude across placements (39).
all BMI groups (25). Conversely Singh et al. (17) reported that high- 4. Micromotion: X-ray features: initially negative, corticalis thick-
er body mass index (BMI: 35-40) was associated with significant- nessing, sclerotic lines that evolve in radiolucent lines. Micro-
ly higher odds of moderate-severe hip pain and use of NSAID med- motion lead to aseptic loosening during time. Pain character-
ications at 5-years. istics: pain that begins when starting to walk after sitting and dur-
Pre-operative scores and pain. If patients’ preoperative functional ing activity (40). In advanced stages pain has the same pattern
status was poor, they were more likely to have pain and need as- as in aseptic loosening.
sistance with walking postoperatively at one year compared with pa- 5. Heterotopic ossification: is the abnormal formation of lamellar
tients with better baseline status. Patients with low preoperative SF- bone in nonosseous soft tissues. Even if the radiographic preva-
36 pain and physical functioning scores were found to have lower lence is reported to be as high as 90% only the 8% of patients
scores postoperatively in comparison with patients with high pre- experience pain (40). Pain characteristics: is often an activity
operative scores (p < 0.01) (26). The baseline score, either SF-36 related pain (41).
or WOMAC pain, was always the most important predictor not only 6. Stress shielding and tip of stem effects: Stress shielding is the
of the six-month score (11, 27) but also at 7 years follow-up (28). adaptive bone remodeling in responses to load shift due to
Level of education. Patients with a higher level of education reported femoral stem presence and can be manifested radiographically
greater improvement in pain (28). MacWilliam et al. (26) found that as proximal bone resorption and distal bone hypertrophy. It was
a low level of education, and each additional comorbidity were as- reported with different implant design (42) and it is not corre-
sociated with a decrease in the change in the pain score (p < 0.01) lated with post-operative pain. When the modulus mismatch be-
and the change in the physical function score (p < 0.01). tween a stiff cementless femoral stem and the less stiff sur-
Patients’ expectation. Mahomed et al. (30) explored the role of pa- rounding bone fail to distribute equally the stress the load con-
tient expectation on postoperative outcome and showed that the ex- centrate at the tip of the stem (43). In this case pain may be pre-
pectation of complete pain relief was an independent predictor of sent also in absence of visible radiographic signs. Callaghan
greater improvement in the pain score (WOMAC) and physical func- et al. reported thigh pain in as many as 18% of patient with ex-
tioning score (SF-36 and WOMAC) (p < 0.05). On the other hand, tensively porous coated stem (44).
patients that hope for return or increase in nonessential activity were
less satisfied (31). Negative X-rays
Waiting Time for Surgery. Several studies concurred that there was 1. Reactive synovitis: MRI has been proposed to assess reactive
no association between the time that the patients waited for surgery synovitis and osteolysis due to particle debris. Osteolysis can
and postoperative pain (18, 32, 33). be detected before it comes evident on x-ray. Cooper et al. (45)
Mental Status. In a large retrospective study with 5,707 THAs at 2- studied with MRI a group of young patients (43-65 years) three
years and 3,289 THAs at 5-years associations of moderate-severe years after surgery. They found reactive synovitis in 39%, no
pain with depression were significant at 2-years, but not at 5-year signs of osteolysis and no correlation with synovitis and pain.
follow-up (17). Butler et al. (34) reported that poor preoperative sta- 2. Aseptic lymphocytic vasculitic associated lesion (ALVAL): is a
tus at Mental Component Score on the SF-12 is associated with a localized hypersensivity reaction and immunologic response to
higher incidence of thigh pain and a lower satisfaction score. metal wear debris (46). It may present as groin pain, or effusions
20 Clinical Cases in Mineral and Bone Metabolism 2011; 8(2): 19-22
0353 5 Painful_Ferrata:- 15-09-2011 14:07 Pagina 21
Painful hip arthroplasty: definition
or soft tissue masses, even with night sweats (47). Metal-on- new or persistent pain after surgery (9). Despite a better under-
metal THAs may present with pain due to hypersensitivity 1 to standing of the pathophysiology of pain in some cases is impossi-
3 years following arthroplasty (48). ble to understand the causes of persistent pain. We reviewed prog-
3. Prosthesis impingement: Nasser et al. (49) reported that 21 of nostic factors of pain finding that age (11, 14, 17) and waiting time
116 (18%) of the patients undergone hip resurfacing referred for surgery (18, 32, 33) is not significantly associated with hip pain.
persistent groin pain due to insufficient head/neck offset, an un- While poor pre-operative scores (11, 26-28), low level of education
covered acetabular component, or both. Possible explanations (26, 28), expectation of increase in nonessential activity with the op-
are ripetitive contact on the capsulae or friction over the ileop- eration (31) are all predictive of post-operative pain. Depression and
soas tendon. Also Bartelt et al. confirmed higher groin pain due poor mental status have a positive association with pain at 2 years
to impingement in resurfacing arthroplasty than conventional THA. follow-up (17, 34). Gender is weakly correlated with post-opera-
4. Ileopsoas tendinitis: Pain characteristics: activity related pain, tive pain as some studies reported more pain in woman (15, 16, 19),
pain that begins when starting to walk after sitting, the localization while a large cohort study referred more pain in men (10). BMI seems
is to the groin or to the buttock. Malposition of the acetabular not to influence postoperative pain only at early follow-up (23-25)
component may be associated with psoas tendon impingement while at 5 years more heavy patient (BMI > 35) complain more pain.
that becomes symptomatic with active flexion of the hip (51, 52). The widely variable nature of painful prostheses makes it extremely
The incidence of ileopsoas tendinitis in conventional THAs ranges difficult to construct criteria for assessment. Careful history taking,
between 0.3% and 4.3% (49). physical examination, and plain radiographs are believed to provide
5. Abductor muscle damage: Muller et al. (53) investigated with crucial information. Surgeon must keep in mind all the causes of
MRI patient one year post surgery. They found gluteus minus hip pain to make a correct differential diagnosis.
damages in 50% of patient but they didn’t found any correla- Many studies examined patient characteristics as potential predictors
tion with pain. Similar results are reported by Pfirrmann et al. of pain and function outcomes (11, 12), but were limited to small
(54). Instead gluteus medius tendon rupture after total hip arthro- samples of patients (<300 cases) (15, 18, 23, 24) and reported con-
plasty presented clinically with lateral pain, limp, and a positive tradictory results (13, 15-18). The small sample size makes them
Trendelenburg test secondary to severe abductor weakness (55). underpowered to detect significant associations, thereby leading to
6. Trochanteric bursitis: Pain characteristics: pain over the great false negative results. Additional research into pain characteristics
trochanter persistent for several months, described as neuro- needs to shift from retrospective cohort studies to longer-term large
pathic burning with dysesthesia and allodynia (56). Sometimes prospective investigations.
there is a correlation with radiographics signs of trochanteric pe-
riosteal remodeling or ossification. Acknowledgements
7. Lumbar spine disease: Patients with severe hip osteoarthritis Authors declare that they did not receive grants or outside fund-
often complain low back pain (LBP) due to abnormal spinal sagit- ing in support of their research or preparation of this manuscript.
tal alignment and wobbling gait configuring the hip spine syn- They did not receive payments or other benefits or a commitment
drome. Hip arthritis and lumbar spine arthritis coexist in 10% to or agreement to provide such benefits from a commercial entity.
15% of patients and often present with similar signs and symp-
toms (57). At 24 months follow-up after THA these patient re-
ferred a further improvement in hip function corresponded with References
continued improvement of spinal function and reduced LBP (58).
Some patients may find an initial worsening in their symptoms 1. Soderman P, Malchau H, Herberts P, et al. Outcome after total hip arthro-
after successful THA because of increased activity levels. Pain plasty: Part II. Disease-specific follow-up and the Swedish National To-
characteristics: pain that begins when starting to walk after sit- tal Hip Arthroplasty Register. Acta Orthop Scand. 2001;72:113-119.
ting. Severe osteoarthritis, spinal stenosis, lumbar degenera- 2. Berry DJ, Harmsen WS, Cabanela ME, et al. Twenty-five year survivorship
tive disk or disc herniation present with different pain pattern in of two thousand consecutive primary Charnley total hip replacements:
relation to the anatomic involvement, but all of them may pre- factors affecting survivorship of acetabular and femoral components. J
sent as referred hip pain and must be investigated during clin- Bone Joint Surg Am. 2002;84:171-177.
ical examination. 3. Ethgen O, Bruyere O, Richy F, et al. Health-related quality of life in to-
8. Nerve injuries: Neurologic complications following THA are usu- tal hip and total knee arthroplasty. A qualitative and systematic review
ally noted immediately after surgery, but delayed onset is pos- of the literature. J Bone Joint Surg Am. 2004;May 86-A(5):963-74.
sible even when due to intraoperative events. Nerve injury can 4. Arden NK, Kiran A, Judge A, et al. What is a good patient reported out-
manifest days after surgery as a result of direct pressure or for- come after total hip replacement? Osteoarthritis Cartilage 2010 (article
mation of a hematoma. Farrel et al. (59) reported a clinically ev- in press).
ident nerve injury incidence of 0,6-1,3%. The most compromised 5. Hayes JH, Cleary R, Gillespie WJ, et al. Are clinical and patient assessed
is the sciatic followed by the femoral, the obturator and the su- outcomes affected by reducing length of hospital stay for total hip arthro-
perior gluteal nerves. Brown et al. (60) reviewed the literature plasty? J Arthroplasty. 2000;15,448-452.
finding an incidence of 0.09%-3.7% and no association with sin- 6. Holtzman J, Saleh K, Kane R. Effect of baseline functional status and
pain on outcomes of total hip arthroplasty. J Bone Joint Surg Am.
gle risk factor.
2002;84,1942-1948.
9. Hernia femoral, inguinal, obturator: may present with groin pain.
7. Keener JD, Callaghan JJ, Goetz DD, et al. Long-term function after Charn-
In this case differential diagnosis is simple, an ecotomography
ley total hip arthroplasty. Clin Orthop Relat Res.2003;471,148-156.
may be helpful (35, 39).
8. Keisu KS, Orozco F, Sharkey PF, et al. Primary cementless total hip
10. Referred pain. Affections to internal organs may refer pain to arthroplasty in octogenarians. Two to eleven-years follow-up. J Bone
the hip region. Pain history and pattern must be taken in account Joint Surg Am. 2001;83,359-363.
to assess its true origin (38). 9. Nikolajsen L, Brandsborg B, Lucht U, et al. Chronic pain following to-
tal hip arthroplasty: a nationwide questionnaire study. Acta Anaesthe-
siol Scand. 2006;50:495-500.
Conclusion 10. Garellick G, Kärrholm J, Rogmarket C, et al. Swedish Hip Arthroplas-
ty Register. Annual Report 2008. Department of Ortopaedics, Sahlgren-
The aim of THA surgery is a satisfied patient with optimal pain re- ska University Hospital. October 2009. www.shpr.se, www.jru.or-
lief and satisfaction and an essentially normalized health-related qual- thop.gu.se.
ity of life. Despite the optimal results some patient may face with 11. Montin L, Leino-Kilpi H, Suominen T, et al. A systematic review of em-
Clinical Cases in Mineral and Bone Metabolism 2011; 8(2): 19-22 21
0353 5 Painful_Ferrata:- 15-09-2011 14:07 Pagina 22
P. Ferrata et al.
pirical studies between 1966 and 2005 of patient outcomes of total hip DOI 10.1007/s11999-010-1519-x.
arthroplasty and related factors. J Clin Nurs. 2008;17, 40-45. 35. Duffy P, Masri BA, Garbuz D, et al. Evaluation of patients with pain fol-
12. Santaguida PL, Hawker GA, Hudak PL, et al. Patient characteristics af- lowing total hip replacement. Instr Course Lect 2006;55:223-232.
fecting the prognosis of total hip and knee joint arthroplasty: a system- 36. Stavrev VP, Stavrev PV. Complications in total hip replacement. Folia
atic review. J can chir. 2008;51(6) décembre, 428-436. Med (Plovdiv). 2004;46(2):25-30.
13. Roder C, Parvizi J, Eggli S, et al. Demographic factors affecting long- 37. Garvin KL, Backstein D, Pellegrini Jr VD et al. Dealing with Complica-
term outcome of total hip arthroplasty. Clin Orthop Relat Res tions. J Bone Joint Surg Am. 2009 Aug;91(5):18-21.
2003;417:62-73. 38. Robbins GM, Masri BA, Garbutz DS et al. Evaluation of pain in patients
14. Clarke H, Kay J, Mitsakakis N, et al. Acute pain after total hip arthro- with apparently solidly fixed total hip arthroplasty components. J Am Acad
plasty does not predict the development of chronic postsurgical pain 6 Orthop Surg 2002;10:86-94.
months later. J Anesth. 2010;24:537-543. 39. Evans CA, Cuckler JM. Evaluation of the painful total hip arthroplasty.
15. McGuigan FX, Hozack WJ, Moriarty L, et al. Predicting quality-of-life out- Orthop Clin North Am. 1992;23:303-11.
comes following total joint arthroplasty. Limitations of the SF-36 Health 40. Pellegrini VD Jr. Management of heterotopic ossification. In: Lieberman
Status Questionnaire. J Arthroplasty. 1995;10:742-7. JR, Berry DJ, editors. Advanced reconstruction: hip. The Hip Society. Rose-
16. Halket A, Stratford PW, Kennedy DM, et al. Using Hierarchical Linear mont, IL: American Academy of Orthopaedic Surgeons; 2005. p 247-56.
Modeling to Explore Predictors of Pain After Total Hip and Knee Arthro- 41. Bozic KJ, Rubash HE. The painful total hip replacement. Clin Orthop
plasty as a Consequence of Osteoarthritis. J Arthroplasty. 2010;25(2 Feb- 2004;420:18-25.
ruary), 254-62. 42. Engh CA Jr, Young AM, Engh Sr CA et al. Clinical Consequnces of stress
17. Singh JA, Lewallen D. Predictors of pain and use of pain medications shielding after porous-coated total hip arthroplasty. Clin Orthop Rel Res
following primary Total Hip Arthroplasty (THA): 5,707 THAs at 2-years 2003;417:157-163.
and 3,289 THAs at 5-years. BMC Musculoskelet Disord 2010;May 43. Bulow JU, Scheller G, Arnold P et al. Uncemented total hip replacement
13;11:90. and thigh pain. Int Orthop. 1996;20:65-69.
18. Nilsdotter AK, Lohmander LS. Age and waiting time as predictors of out- 44. Callaghan JJ, Dysart SH, Savoy CG. The uncemented porous coated
come after total hip replacement for osteoarthritis. Rheumatology (Ox- anatomic total hip prosthesis: two year results of a prospective consecutive
ford). 2002;41:1261-7. series. J Bone Joint Surg 1988;70(A):337-346.
19. Caracciolo B, Giaquinto S. Determinants of the subjective functional out- 45. Cooper HJ, Ranawat AS, Potter HG et al. Early Reactive Synovitis and
come of total joint arthroplasty. Arch Gerontol Geriat. 2005;41:169-176. Osteolysis after Total Hip Arthroplasty. Clin Orthop Relat Res.
20. Visuri T, Koskenvuo M, Honkanen R. The influence of total hip re- 2010;468:3278-3285.
placement on hip pain and the use of analgesics. Pain 1985;23:19-26. 46. Watters TS, Cardona DM, Menon KS et al. Aseptic Lymphocyte-Dom-
21. Bogoch ER, Olschewski E, Zangger P, et al. Increased tender point counts inated Vasculitis-Associated Lesion: A Clinicopathologic Review of an
before and after total hip arthroplasty are associated with poorer out- Underrecognized Cause of Prosthetic Failure. Am J Clin Pathol. 2010
comes but are not individually predictive. J Arthroplasty. 2010;25(6 Sep- Dec;134(6):886-893.
tember), 945-950. 47. Molvik H, Hanna SA, de Roeck NJ. Failed Metal-on-Metal Total Hip Arthro-
22. Burton BT, Foster WR, Hirsch J, et al. Health implications of obesity: plasty Presenting as Painful Groin Mass With Associated Weight Loss
an NIH consensus development conference. Int J Obes.1985;9:155-170. and Night Sweats. Am J Orthop. 2010;39(5):E46-E49.
23. Ibrahim T, Hobson S, Beiri A, et al. No influence of body mass index 48. Cuckler JM. Unexplained Pain After THR: What Should I Do? Ortho-
on early outcome following total hip arthroplasty. Int Orthop.2005;29: pedics. September 2010;33(9):648.
359-361. 49. Nasser AB, Beaule´ PE, O’Neill M et al. Incidence of Groin Pain After
24. Kessler S, Kafer W. Overweight and Obesity: Two Predictors for Worse Metal-on-Metal Hip Resurfacing. Clin Orthop Relat Res. 2010;468:392-
Early Outcome in Total Hip Replacement? Obesity. 2007;15(11 No- 399.
vember), 2840-2845. 50. Bartelt RB, Yuan BJ, Trousdale RT et al. The Prevalence of Groin Pain
25. Bolland BJRF, Culliford DJ, Maskell J, et al. The effect of hip and knee After Metal-on-Metal Total Hip Arthroplasty and Total Hip Resurfacing.
arthroplasty on oral antiinflammatory use and the relationship to body Clin Orthop Relat Res. 2010;468:2346-2356.
mass index: results from the UK general practice research database, 51. Lachiewicz PF, Kauk JR. Anterior iliopsoas impingement and tendini-
Osteoarthritis Cartilage. 2010;doi:10.1016/j.joca.2010.10.012. tis after total hip arthroplasty. J Am Acad Orthop Surg. 2009;17(6):337-
26. MacWilliam CH, Yood MU, Verner JJ, et al. Patient-related risk factors 344.
that predict poor outcome after total hip replacement. Health Serv Res. 52. Jasani V, Richards P, Wynn-Jones C. Pain related to the psoas mus-
1996;31:623-38. cle after total hip replacement. J Bone Joint Surg Br.2002;84:991-993.
27. Fortin PR, Clarke AE, Joseph L, et al. Outcomes of total hip and knee 53. Müller M, Tohtz S, Winkler T et al. MRI Findings of gluteus minimus mus-
replacement: preoperative functional status predicts outcomes at six cle damage in primary total hip arthroplasty and the influence on clini-
months after surgery. Arthritis Rheum. 1999;42:1722-8. cal outcome. Arch Orthop Trauma Surg. 2010:130:927-935.
28. A Nilsdotter, F Isaksson. Patient relevant outcome 7 years after total hip 54. Pfirrmann CW, Notzli HP, Dora C et al. Abductor tendons and muscles
replacement for OA - a prospective study. BMC Musculoskelet Dis- assessed at MR imaging after total hip arthroplasty in asymptomatic and
ord.2010, 11:47 symptomatic patients. Radiology. 2005;235:969-976.
29. Rissanen P, Aro S, Sintonen H, et al. Quality of life and functional abil- 55. Fehm MN, Huddleston JI, Burke DW et al. Repair of a Deficient Abductor
ity in hip and knee replacements: a prospective study. Qual Life Res. Mechanism with Achilles Tendon Allograft After Total Hip Replacement.
1996;5:56-64.71. J Bone Joint Surg Am. 2010;92:2305-11.
30. Mahomed NN, Liang MH, Cook EF, et al. The importance of patient ex- 56. Yakovlev AE, Resch BE, Karasev SA. Treatment of intractable hip pain
pectations in predicting functional outcomes after total joint arthroplas- after THA and GTB using peripheral nerve field stimulation: a case se-
ty. J Rheumatol. 2002;29:1273-9. ries. Wisconsin Medical Journal. 2010;109(3):149-152.
31. Mancuso CA, Salvati EA, Johanson NA et al. Patients’ expectations and 57. Brown MD, Gomez-Martin O, Brookfield KF, et al. Differential diagno-
satisfaction with total hip arthroplasty. J Arthroplasty 1997;12:387-396. sis of hip disease versus spine disease. Clin Orthop 2004;1:280.
32. Williams JI, Llewellyn Thomas H, et al. The burden of waiting for hip and 58. Ben-Galim P, Ben-Galim T, Rand N et al. Hip-spine syndrome: the ef-
knee replacements in Ontario. Ontario Hip and Knee Replacement Pro- fect of total hip replacement surgery on low back pain in severe os-
ject Team. J Eval Clin Pract. 1997;3:59-68.64. teoarthritis of the hip. Spine. 2007 Sep 1;32(19):2099-2102.
33. Mahon JL, Bourne RB, Rorabeck CH, et al. Health-related quality of life 59. Farrell CM, Springer BD, Haidukewych GJ et al. Motor nerve palsy fol-
and mobility of patients awaiting elective total hip arthroplasty: a prospec- lowing primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2619-
tive study. CMAJ. 2002;167:1115-21. 25.
34. Butler RA, Rosenzweig S, Myers L, et al. The Impact of Socioeconomic 60. Brown GD, Swanson EA, Nercessian OA. Neurologic injuries after to-
Factors on Outcome After THA. A Prospective, Randomized Study. Pa- tal hip arthroplasty. Am J Orthop (Belle Mead NJ). 2008 Apr;37(4):191-
per presented at the Hip Society Meeting 2010. Clin Orthop Relat Res 7.
22 Clinical Cases in Mineral and Bone Metabolism 2011; 8(2): 19-22
You might also like
- Clinical Anatomy of Spine, Spinal Cord & ANS PDFDocument680 pagesClinical Anatomy of Spine, Spinal Cord & ANS PDFMajda Bajramović100% (8)
- Operative Techniques in Foot and Ankle Surgery 2nd Edition Ebook PDFDocument61 pagesOperative Techniques in Foot and Ankle Surgery 2nd Edition Ebook PDFmaurice.honeycutt512100% (51)
- Cervical Total Disc Replacement: Long-Term OutcomesDocument12 pagesCervical Total Disc Replacement: Long-Term OutcomesKyle RobinNo ratings yet
- The Ligament Injury Connection To Osteoarthritis: Wonder Why?Document11 pagesThe Ligament Injury Connection To Osteoarthritis: Wonder Why?Saifuddin HaswareNo ratings yet
- Knee Pain July 2014Document10 pagesKnee Pain July 2014Naeemur RahmanNo ratings yet
- Diagnosis and Treatment of Patients With Patellofemoral PainDocument10 pagesDiagnosis and Treatment of Patients With Patellofemoral PainRuben CapelaNo ratings yet
- Effect of Cold Warm or Contrast Therapy On Controlling Knee Osteoarthritis Associated ProblemsDocument7 pagesEffect of Cold Warm or Contrast Therapy On Controlling Knee Osteoarthritis Associated ProblemsIneMeilaniNo ratings yet
- Assessment of Chronic PainDocument7 pagesAssessment of Chronic PainFranciscoGarciaNo ratings yet
- Osteochondroma Fracture in Young Athlete Bfe9f44bDocument4 pagesOsteochondroma Fracture in Young Athlete Bfe9f44bViona Ananda putriNo ratings yet
- JSS College of PhysiotherapyDocument8 pagesJSS College of PhysiotherapyDANIA NAJUA BINTI ZAINALNo ratings yet
- Kehlet2002 Article ChronicPostherniorrhaphyPainACDocument4 pagesKehlet2002 Article ChronicPostherniorrhaphyPainACHarutyun AlaverdyanNo ratings yet
- Injury: Theodoros H. Tosounidis, Hassaan Sheikh, Martin H. Stone, Peter V. GiannoudisDocument7 pagesInjury: Theodoros H. Tosounidis, Hassaan Sheikh, Martin H. Stone, Peter V. GiannoudisWanda AndiniNo ratings yet
- Comprehensive Approach To The Evaluation of Groin.7Document13 pagesComprehensive Approach To The Evaluation of Groin.7cooperorthopaedicsNo ratings yet
- THR Painful Pietrzak2017Document7 pagesTHR Painful Pietrzak2017Mohan DesaiNo ratings yet
- Hip Bone Marrow Edema Presenting As Low Back Pain A Case ReportDocument10 pagesHip Bone Marrow Edema Presenting As Low Back Pain A Case ReportVizaNo ratings yet
- Nursing Care For Ederly in Osteoarthritis Case With Cronic Pain ProblemDocument13 pagesNursing Care For Ederly in Osteoarthritis Case With Cronic Pain ProblemMitha Amelia PutriNo ratings yet
- Osteoarthritis and Arthroplasty of The Hip and Knee 2018 PDFDocument6 pagesOsteoarthritis and Arthroplasty of The Hip and Knee 2018 PDFMarcelo Ramirez SiñanizNo ratings yet
- Osteoarthritis of The Hip: Clinical PracticeDocument9 pagesOsteoarthritis of The Hip: Clinical PracticeMarina Tomasenco - DaniciNo ratings yet
- Is Extracorporeal Shockwave Therapy Effective Even in The Treatment of Partial Rotator Cuff TearDocument6 pagesIs Extracorporeal Shockwave Therapy Effective Even in The Treatment of Partial Rotator Cuff TearmitchelNo ratings yet
- Facet Joint SyndromeDocument17 pagesFacet Joint Syndromepaulvaso27100% (1)
- Plantar Fasciitis A Review of Treatments.4Document5 pagesPlantar Fasciitis A Review of Treatments.4diki Tri MardiansyahNo ratings yet
- Sebastian2014 PDFDocument8 pagesSebastian2014 PDFArchita AgarwalNo ratings yet
- Efeitos Da Maturacao BiologicaDocument12 pagesEfeitos Da Maturacao BiologicalucasNo ratings yet
- International Journal of Surgery OpenDocument11 pagesInternational Journal of Surgery OpenSaugi HudaNo ratings yet
- Anterior Knee PainDocument10 pagesAnterior Knee PainfreireortoNo ratings yet
- S32.Full (Tanda Kuning)Document11 pagesS32.Full (Tanda Kuning)ahmadheulwanNo ratings yet
- Postoperative Pain in Neurosurgery: A Pilot Study SurgeryDocument5 pagesPostoperative Pain in Neurosurgery: A Pilot Study SurgeryCuenta LastNo ratings yet
- Common Overuse Tendon ProblemsDocument8 pagesCommon Overuse Tendon ProblemsmircoNo ratings yet
- Journal Parkinson 2013Document5 pagesJournal Parkinson 2013widyakamrulNo ratings yet
- Shoulder 2 Ada MriDocument4 pagesShoulder 2 Ada MriNirmalasari AnirNo ratings yet
- Chemical Hip Denervation For Inoperable Hip FractureDocument6 pagesChemical Hip Denervation For Inoperable Hip Fracturemanuel torresNo ratings yet
- Osteosarcoma Clinical Case by SlidesgoDocument12 pagesOsteosarcoma Clinical Case by SlidesgoLwhynnNo ratings yet
- Managing The Patient With Heel PainDocument5 pagesManaging The Patient With Heel Painmh8m58brjnNo ratings yet
- Activity 1 Concepts of PainnDocument8 pagesActivity 1 Concepts of Painncrishara palomoNo ratings yet
- Nijs Et Al 2021 LANCET RheumatologyDocument10 pagesNijs Et Al 2021 LANCET RheumatologyVicaroNo ratings yet
- Groin Pain Syndrome Known As Sports Hernia A ReviewDocument9 pagesGroin Pain Syndrome Known As Sports Hernia A Review1541920001 LUIS GUILLERMO PAJARO FRANCO ESTUDIANTE ACTIVO ESPECIALIDAD MEDICINA INTERNANo ratings yet
- Lower Limb Evaluation Format Lower Limb Fracture Assesstment FormDocument12 pagesLower Limb Evaluation Format Lower Limb Fracture Assesstment FormsridharNo ratings yet
- Journal of Bodywork & Movement Therapies: Adi Dor, BPT, Leonid Kalichman, PT, PHDDocument6 pagesJournal of Bodywork & Movement Therapies: Adi Dor, BPT, Leonid Kalichman, PT, PHDLaura Espejo SalamancaNo ratings yet
- Fracture and Joint Injuries (Shalter-Chapter 15) - Kelompok C (Dr. Oktavianus, SP - Ot)Document69 pagesFracture and Joint Injuries (Shalter-Chapter 15) - Kelompok C (Dr. Oktavianus, SP - Ot)Heru ChrisNo ratings yet
- 2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDocument15 pages2014 The Pain of Tendinopathy - Physiological or PathophysiologicalDavid Alejandro Cavieres AcuñaNo ratings yet
- Anterior Knee Pain: Remember To Look Up and Be Aware of Structural AnomaliesDocument3 pagesAnterior Knee Pain: Remember To Look Up and Be Aware of Structural AnomaliesDaniel G. A. C.No ratings yet
- Phantom Limb Pain: Moon Suk Bang, MD, PHD, and Se Hee Jung, MD, MsDocument4 pagesPhantom Limb Pain: Moon Suk Bang, MD, PHD, and Se Hee Jung, MD, MsIgnacio AndrésNo ratings yet
- Chinese Journal of Traumatology: Phantom Limb Pain: A Literature ReviewDocument3 pagesChinese Journal of Traumatology: Phantom Limb Pain: A Literature ReviewEva Nur MalaNo ratings yet
- Diagnostics and Management of TemporomanDocument6 pagesDiagnostics and Management of TemporomanDr. Zardasht N. BradostyNo ratings yet
- Physiotherapy Management of Hip Osteoarthritis: Kim BennellDocument13 pagesPhysiotherapy Management of Hip Osteoarthritis: Kim BennellAndrei R LupuNo ratings yet
- Anterior Knee Pain in The Young AthleteDocument7 pagesAnterior Knee Pain in The Young AthleteAngelica GarciaNo ratings yet
- Reichenbach 2010Document6 pagesReichenbach 2010EriC. ChaN.No ratings yet
- 485-Article Text-605-1-10-20161227 PDFDocument10 pages485-Article Text-605-1-10-20161227 PDFJeg1No ratings yet
- JMT 23 162Document7 pagesJMT 23 162dark_PinchoNo ratings yet
- Clinical Review: OsteoarthritisDocument4 pagesClinical Review: OsteoarthritismarindadaNo ratings yet
- Joint Pain One PagerDocument3 pagesJoint Pain One PagermustafaNo ratings yet
- ArticlesDocument7 pagesArticlesSoha Arif ShaykhNo ratings yet
- Evaluation of Pain Levels and Management in Total Knee Replacement PatientsDocument10 pagesEvaluation of Pain Levels and Management in Total Knee Replacement PatientsBong Yi LinNo ratings yet
- Pain and Effusion and Quadriceps Activation and StrengthDocument6 pagesPain and Effusion and Quadriceps Activation and StrengthЯнь НгуенNo ratings yet
- Current Concept Management of Carpal Tunnel Syndrome: A Case ReportDocument17 pagesCurrent Concept Management of Carpal Tunnel Syndrome: A Case Reportwidiyah darmawanNo ratings yet
- Factores Que Afectan El Resultado Después de La Amputación Traumática de Una ExtremidadDocument14 pagesFactores Que Afectan El Resultado Después de La Amputación Traumática de Una Extremidadolalla de santosNo ratings yet
- OsteoartritisDocument9 pagesOsteoartritisWalter Espinoza CiertoNo ratings yet
- Mechanisms of Osteoarthritis (OA) PainDocument6 pagesMechanisms of Osteoarthritis (OA) Painedlinkusuma131No ratings yet
- Management L Low Back PainDocument7 pagesManagement L Low Back PainelsyamelindaNo ratings yet
- Plantar and Medial Heel Pain: Diagnosis and Management: Review ArticleDocument9 pagesPlantar and Medial Heel Pain: Diagnosis and Management: Review ArticleGhani AbdurahimNo ratings yet
- Sensibiliza o Central Nas Dores CR Nicas REVIEW LANCET 2021 - Open AccessDocument10 pagesSensibiliza o Central Nas Dores CR Nicas REVIEW LANCET 2021 - Open AccessRichard Mezadri ViebrantzNo ratings yet
- MRI of Degenerative Disease of the Spine: A Case-Based AtlasFrom EverandMRI of Degenerative Disease of the Spine: A Case-Based AtlasNo ratings yet
- National Hospital Insurance Fund PDFDocument292 pagesNational Hospital Insurance Fund PDFCargo ReeNo ratings yet
- Clinical Congress: ProgramDocument17 pagesClinical Congress: ProgramHassan HamzahNo ratings yet
- Orthotics - Ul & LLDocument48 pagesOrthotics - Ul & LLReena PremNo ratings yet
- Drexel University College of Medicine Department of AnesthesiologyDocument1 pageDrexel University College of Medicine Department of AnesthesiologydrexelanesthesiaNo ratings yet
- Recommended Reading List For EDAICDocument4 pagesRecommended Reading List For EDAICAna Belén Artero CastañoNo ratings yet
- MS - Foot and Toes - Slide10Document2 pagesMS - Foot and Toes - Slide10testNo ratings yet
- Airway Centric OrthoDocument6 pagesAirway Centric OrthoSrishti SyalNo ratings yet
- AO Surgery Reference Lenke ClassificationDocument1 pageAO Surgery Reference Lenke ClassificationFederico Nelson FreisNo ratings yet
- Session: I: Registration /breakfastDocument5 pagesSession: I: Registration /breakfastBhaskar BorgohainNo ratings yet
- Hospital Scorecard - DepartmentwiseDocument4 pagesHospital Scorecard - DepartmentwiseNatasha BhasinNo ratings yet
- Cosmetic Surgery EssayDocument7 pagesCosmetic Surgery Essayalisharenee0550% (2)
- Morphology of Cranial Sutures and RadiologicDocument6 pagesMorphology of Cranial Sutures and RadiologicEvans RodrigezNo ratings yet
- Mathogs Atlas of Craniofacial Trauma 2nd EditionDocument692 pagesMathogs Atlas of Craniofacial Trauma 2nd EditionCary Dee100% (1)
- EWMA Endorsements of Wound Centres Non Hospital Based ApplicationForm WordDocument17 pagesEWMA Endorsements of Wound Centres Non Hospital Based ApplicationForm WordCarlo BalzereitNo ratings yet
- 17 - Distal Radius FracturesDocument78 pages17 - Distal Radius FracturesFlorin Panduru100% (1)
- ACL Procedure & Tunnel Prep.: - Learning ObjectivesDocument17 pagesACL Procedure & Tunnel Prep.: - Learning ObjectivesIbrahim Syed MustafaNo ratings yet
- EVALUATION 1.1 THE ROLE OF NURSES IN THE OPERATING ROOM Unscramble SentencesDocument3 pagesEVALUATION 1.1 THE ROLE OF NURSES IN THE OPERATING ROOM Unscramble SentencesRonald Alfredo Gordillo PeraltaNo ratings yet
- The SAGES Safe Cholecystectomy ProgramDocument4 pagesThe SAGES Safe Cholecystectomy ProgramMikael AngelooNo ratings yet
- Comparative Study of Functional Outcome in Upper One Third Shaft Tibia Fractures With Suprapatellar and Infrapatellar Intramedullary Tibial NailingDocument8 pagesComparative Study of Functional Outcome in Upper One Third Shaft Tibia Fractures With Suprapatellar and Infrapatellar Intramedullary Tibial NailingakankshaNo ratings yet
- The Sample of PediatricsDocument47 pagesThe Sample of PediatricsWaseem UllahNo ratings yet
- Treatment of Supracondylar Femoral Fractures in Young Cats and Dogs Using "Arrow Pin" TechniqueDocument5 pagesTreatment of Supracondylar Femoral Fractures in Young Cats and Dogs Using "Arrow Pin" TechniqueVangelis PapachristosNo ratings yet
- Orthotics: A Report By: Kenneth Pierre M. LopezDocument94 pagesOrthotics: A Report By: Kenneth Pierre M. LopezAkbar AziziNo ratings yet
- Anchorage Considerations in Lingual OrthodonticsDocument4 pagesAnchorage Considerations in Lingual OrthodonticsSibi NairNo ratings yet
- Elbow Fractures: Distal Humerus: The American Society For Surgery of The Hand.)Document15 pagesElbow Fractures: Distal Humerus: The American Society For Surgery of The Hand.)Radu UrcanNo ratings yet
- The Flexion Gap in Normal Knees: An Mri StudyDocument4 pagesThe Flexion Gap in Normal Knees: An Mri StudyGERARDO TORRES RUIZNo ratings yet
- Norm Med TraumaDocument87 pagesNorm Med TraumaLibrería Médica PandoNo ratings yet
- PLX7100A BrochureDocument8 pagesPLX7100A Brochurealmotaz.khtNo ratings yet