Professional Documents
Culture Documents
Hospital File
Hospital File
Uploaded by
wasiman khanCopyright:
Available Formats
You might also like
- QC Tests For Oral Liquid Dosage FormsDocument13 pagesQC Tests For Oral Liquid Dosage FormsMitesh Jain100% (4)
- Laboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceFrom EverandLaboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceRating: 5 out of 5 stars5/5 (4)
- Updated Marketing Project For MBADocument99 pagesUpdated Marketing Project For MBAadamodharNo ratings yet
- Project Submitted To Osmania University Towards The Partial Fulfilment of The Award of Masters Degree in Hospital ManagementDocument59 pagesProject Submitted To Osmania University Towards The Partial Fulfilment of The Award of Masters Degree in Hospital ManagementAnkitChauhan100% (1)
- Reflection Paper SPEDDocument5 pagesReflection Paper SPEDMariecris Barayuga Duldulao-AbelaNo ratings yet
- Practice Writing A Report: Scenario 1Document2 pagesPractice Writing A Report: Scenario 1Olga100% (1)
- Clinical PharmacyDocument25 pagesClinical PharmacyHariom patelNo ratings yet
- Hos (1) - MergedDocument59 pagesHos (1) - Mergedanshulthestylorider2No ratings yet
- PithecellobiumDocument54 pagesPithecellobiummirahsanali69No ratings yet
- Dipak FinalDocument59 pagesDipak FinalMohammed Omar SharifNo ratings yet
- DHARSHINI R PDFDocument41 pagesDHARSHINI R PDFkesavanbsc17No ratings yet
- Samarjit Thesis-1Document16 pagesSamarjit Thesis-1himanshubehera73No ratings yet
- KAHKASHA Full ProjectsDocument113 pagesKAHKASHA Full Projectscity9848835243 cyber100% (1)
- DUE of PIPERACILLIN and TazobactumDocument73 pagesDUE of PIPERACILLIN and Tazobactumanup jagarlamudiNo ratings yet
- 86-90 GroupDocument30 pages86-90 GroupSai krishna PoojithaNo ratings yet
- 43 Shravan ParmarDocument30 pages43 Shravan Parmarsai projectNo ratings yet
- MaruffDocument4 pagesMaruffchoudhary25092000No ratings yet
- Project 115Document30 pagesProject 115Rushikesh PatilNo ratings yet
- 2022 Internship Manual PhysiotherapyDocument82 pages2022 Internship Manual PhysiotherapyRizwan KhanNo ratings yet
- Sachin Hospital 2 Training FinalDocument45 pagesSachin Hospital 2 Training Finaldevnishad985No ratings yet
- DALLUDocument15 pagesDALLUdalchandsahu74No ratings yet
- Project ReportDocument31 pagesProject ReportRamish KhanNo ratings yet
- Hospital Training ReportDocument26 pagesHospital Training ReportAlex GamingNo ratings yet
- Anti Inflammatory Prospective Study of Commiphora Mukul (Guggul) On Wistar Albino RatsDocument54 pagesAnti Inflammatory Prospective Study of Commiphora Mukul (Guggul) On Wistar Albino RatsKrish NalimelaNo ratings yet
- Prashant Pps Front PgesDocument6 pagesPrashant Pps Front PgesM. Shoeb Sultan100% (1)
- Artificial Intelligence: Mr. Hakim SinghDocument24 pagesArtificial Intelligence: Mr. Hakim SinghAman kumarNo ratings yet
- "Sugantha Malli Chooranam" "Sugantha Malli Chooranam" For The Treatment of "Lasuna Thabitham" "Sugantha Malli Chooranam"Document179 pages"Sugantha Malli Chooranam" "Sugantha Malli Chooranam" For The Treatment of "Lasuna Thabitham" "Sugantha Malli Chooranam"AzarudeenNo ratings yet
- Rajat Hopital ReportDocument29 pagesRajat Hopital ReportRajat Rastogi 143No ratings yet
- Industrial Training RecordDocument31 pagesIndustrial Training RecordPrint SolutionNo ratings yet
- Method Development and Validation For The Simultaneous Estimation of Lobeglitazone Sulphate and Glimepiride by HPLC MethodDocument113 pagesMethod Development and Validation For The Simultaneous Estimation of Lobeglitazone Sulphate and Glimepiride by HPLC MethodShikha MishraNo ratings yet
- Srilekha DeyDocument33 pagesSrilekha Deyunplugged ZoneNo ratings yet
- 8th Sem Project FinalDocument37 pages8th Sem Project FinalArsh DNo ratings yet
- Medication Disposal Household Practices in KarachiDocument8 pagesMedication Disposal Household Practices in KarachiFazal JalalNo ratings yet
- Hydrogel FrontDocument7 pagesHydrogel FrontVaibhav SharmaNo ratings yet
- Hospital Report 2 NDDocument83 pagesHospital Report 2 NDAbdul MannanNo ratings yet
- Hydrogel FrontDocument7 pagesHydrogel FrontVaibhav SharmaNo ratings yet
- ProjectDocument113 pagesProjectvishal sharmaNo ratings yet
- Vaishnavi Singh B.Pharm. Iiird Year, V Semester Roll No.1900560500097Document11 pagesVaishnavi Singh B.Pharm. Iiird Year, V Semester Roll No.1900560500097Vishnu SinghNo ratings yet
- Sustained Release Matrix Tablet of Diltiazem Hydrochloride It'S Formulation and EvaluationDocument10 pagesSustained Release Matrix Tablet of Diltiazem Hydrochloride It'S Formulation and EvaluationruriNo ratings yet
- Shri Govindram Seksaria Institute of Technology and ScienceDocument33 pagesShri Govindram Seksaria Institute of Technology and ScienceSunny Thakur17No ratings yet
- INDUSTRIAL TRANING - Garima SinghDocument17 pagesINDUSTRIAL TRANING - Garima SinghARVIND KUMARNo ratings yet
- Praveen ProjectDocument81 pagesPraveen Projectpraveen kumarNo ratings yet
- ANURAG Pharmaceutical-Industrial-Training-ReportDocument69 pagesANURAG Pharmaceutical-Industrial-Training-ReportRajat Rastogi 143No ratings yet
- Prospectus DipsarDocument36 pagesProspectus DipsarAnkit Arora0% (1)
- Sushma Verma BMWDocument37 pagesSushma Verma BMWPiaNo ratings yet
- Sapna 4th Yr 1newDocument23 pagesSapna 4th Yr 1newSAPNANo ratings yet
- A Clinical Study On: Diagnostic Methdology of PaanduDocument211 pagesA Clinical Study On: Diagnostic Methdology of PaanduThe logical humanNo ratings yet
- Pharmacy FRONTDocument4 pagesPharmacy FRONTSapna KumariNo ratings yet
- Ndds SK ProjectDocument72 pagesNdds SK ProjectShahnawaz khanNo ratings yet
- Formulation of An Instantly Dissolvable Solid Eye Drop Device For Topical Ocular DeliveryDocument243 pagesFormulation of An Instantly Dissolvable Solid Eye Drop Device For Topical Ocular DeliverystrauliaNo ratings yet
- Garima Project Report On Drug SafetyDocument27 pagesGarima Project Report On Drug SafetygariNo ratings yet
- Conference On Nanomedicine - Advances and ChallengesDocument6 pagesConference On Nanomedicine - Advances and Challengesrahulkrishna9019No ratings yet
- JMDH 400734 Application Benefits and Limitations of Telepharmacy For PDocument9 pagesJMDH 400734 Application Benefits and Limitations of Telepharmacy For PIrma RahmawatiNo ratings yet
- Practice School (Front Page)Document9 pagesPractice School (Front Page)adityaNo ratings yet
- Hospital Training ReportDocument89 pagesHospital Training ReportAbhishek SinghNo ratings yet
- Cosmetovigilance A ReviewDocument40 pagesCosmetovigilance A ReviewAnshulNo ratings yet
- Ss - KPC Medical College Final ProjectDocument141 pagesSs - KPC Medical College Final ProjectSemanti SamantaNo ratings yet
- Vydehi Institute of Medical Sciences RC Department of Pharmacology NewsletterDocument6 pagesVydehi Institute of Medical Sciences RC Department of Pharmacology NewsletterPERFECT CLASSESNo ratings yet
- Finalset 1Document57 pagesFinalset 1Tahir BilalNo ratings yet
- Syccon S-4 - 20240518 - 172351 - 0000Document15 pagesSyccon S-4 - 20240518 - 172351 - 0000thiyagaswetha.r.2018.eceNo ratings yet
- The Initial Psychiatric Interview PDFDocument4 pagesThe Initial Psychiatric Interview PDFJoan ChoiNo ratings yet
- Sunflower Production (Final) PPT - Compressed PDFDocument27 pagesSunflower Production (Final) PPT - Compressed PDFMarijenLeaño88% (8)
- Teknistae Sulakkeista Englanti PDFDocument156 pagesTeknistae Sulakkeista Englanti PDFJosué Miranda da SilvaNo ratings yet
- Ic CCT15368Document2 pagesIc CCT15368Mohamed RadyNo ratings yet
- Blood Vessels: The Human Transport System: Sbi3UDocument15 pagesBlood Vessels: The Human Transport System: Sbi3UHelloworldasdtNo ratings yet
- Un Cisic E-Bulliten 5Document3 pagesUn Cisic E-Bulliten 5taha_basit2441No ratings yet
- Welcome Madison 2013 2014Document97 pagesWelcome Madison 2013 2014Alexander León PuelloNo ratings yet
- Dinner MenuDocument3 pagesDinner MenueatlocalmenusNo ratings yet
- Senate Hearing, 111TH Congress - Department of Defense Appropriations For Fiscal Year 2010Document610 pagesSenate Hearing, 111TH Congress - Department of Defense Appropriations For Fiscal Year 2010Scribd Government DocsNo ratings yet
- Barrier Free Design GuideDocument6 pagesBarrier Free Design GuideRamesh ArjunNo ratings yet
- Hot Dip Galvanization - FaboryDocument4 pagesHot Dip Galvanization - FaboryBrandon LimNo ratings yet
- Autism Spectrum and Open-MindednessDocument2 pagesAutism Spectrum and Open-MindednessJaime MontoyaNo ratings yet
- Updated DXN Presentation1Document56 pagesUpdated DXN Presentation1xs2vicky100% (1)
- Pipe Sizing GuideDocument4 pagesPipe Sizing GuideorganicspolybondNo ratings yet
- Lifting Supervisors Guidebook Revised 2014Document15 pagesLifting Supervisors Guidebook Revised 2014Abn BK100% (1)
- Parle AgroDocument3 pagesParle AgroKumar GautamNo ratings yet
- COVID-19 Vaccines and Fetal TissueDocument3 pagesCOVID-19 Vaccines and Fetal TissueAdim AresNo ratings yet
- Subsea Exercise No.6 PDFDocument16 pagesSubsea Exercise No.6 PDFEmmanuel Byensita100% (2)
- Soal Uts Kelas 9 MtsDocument5 pagesSoal Uts Kelas 9 Mtsindah sNo ratings yet
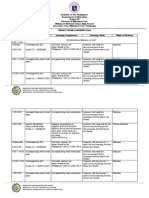
- Mabalacat National Senior High School Address: San Isidro, Dau, Mabalacat City, PampangaDocument5 pagesMabalacat National Senior High School Address: San Isidro, Dau, Mabalacat City, PampangaJel Louis LopezNo ratings yet
- Royal Wolf Product CatalogueDocument52 pagesRoyal Wolf Product Cataloguecadsifu100% (1)
- Components of A Gating System: VIT University 1Document11 pagesComponents of A Gating System: VIT University 1aryanNo ratings yet
- Quilt of Swami Stories English v8 Onlineversion PDFDocument50 pagesQuilt of Swami Stories English v8 Onlineversion PDFGaneshNo ratings yet
- Itp - For Heat ExchangerDocument3 pagesItp - For Heat ExchangerSuraj ShettyNo ratings yet
- Tape Mobil JVC.Document16 pagesTape Mobil JVC.EdisonNainggolanNo ratings yet
- 2022 - Executive Order - BADAC - BDODocument3 pages2022 - Executive Order - BADAC - BDOromulo sigaNo ratings yet
- Introduction To Labor Economics: Chapter 2 - The Labor MarketDocument37 pagesIntroduction To Labor Economics: Chapter 2 - The Labor Marketqulb abbasNo ratings yet
- Prodotti Manuali Documento 43Document16 pagesProdotti Manuali Documento 43whorne24No ratings yet
Hospital File
Hospital File
Uploaded by
wasiman khanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hospital File
Hospital File
Uploaded by
wasiman khanCopyright:
Available Formats
lOMoARcPSD|42080776
Hospital file
Bachelor of pharmacy (Dr. A.P.J. Abdul Kalam Technical University)
Scan to open on Studocu
Studocu is not sponsored or endorsed by any college or university
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
HOSPITAL TRAINING REPORT FILE
Submitted
In the partial fulfillment of the requirement for the degree of
BACHELOR OF PHARMACY
By
Name of Student
(Roll No :-21006605000)
Under the supervision of
Dr. Mayank Kulshreshtha Dr. Devender Pathak
(Professor) (Director & Dean)
Rajiv Academy for Pharmacy, Mathura
To the
Dr. A.P.J. ABDUL KALAM TECHNICAL UNIVERSITY
(Formerly Uttar Pradesh Technical University)
LUCKNOW
2024
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
CERTIFICATE
This is Certified that Name of Student , (Roll No -21006605000) has carried out
the hospital training as a part of the curriculum of Bachelor of Pharmacy (2023-
24). The report embodies results of training activities performed by the student
and the contents of report do not form the basis for the award of any other degree
to the candidate or to anybody else from this or any other University/Institution.
Dated:
Signature:
Dr. Mayank Kulshreshtha Dr. Devender Pathak
Professor Director & Dean
Rajiv Academy for Pharmacy, Mathura Rajiv Academy for
Pharmacy, Mathura
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
DECLARATION
I hereby declare that this project work entitled “Hospital Training Report File”
embodies my original work. It has not submitted in part on fully for any other
diploma or degree of any university. My indebtedness to other works has been
duly acknowledged at relevant places.
Place: Rajiv academy for pharmacy, Mathura Student Name –
Dr. A.P.J. Abdul Kalam Technical University, Lucknow (Roll No- 21006605000)
Date: …. /….. / 2024
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
ACKNOWLEDGEMENT
Today after completing such a major work, I look back, to find that it would not
have been possible without blessing, guidance and support of my family, teachers
and friends.
I express my sincere thanks to my project guide Dr. Mayank Kulshreshtha
(Professor), I sincerely acknowledge his for extending valuable guidance, support
for literature, critical reviews of project report and moral support provided at all
stage of project.
I am also thankful to entire faculty members like Dr. Himansu Chopra, R.K.
Chaudhary, Akash Garg, Shivendra Saxena for giving me their support during
my whole journey. The entire work is an outcome of the relentless and unfailing
endorsement of my parents who have been instrumental in pursuit.
I pay great tribute to my parents for being the constant source of love, concern,
strength, support and dedication in my life. It is always the blessings of parents
which makes us what we are today.
Name Of Student
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Table of contents
Front page
Certificate 2
Declaration 3
Acknowledgement 4
Table of contents 5
Hospital Introduction 6-9
Activities Performed During Training 10
1. First Aid 11
i. Artificial Respiration 12
ii. Mouth to Mouth Resuscitation 12-13
iii. Mouth to Nose Resuscitation 13-14
2. Different Routes of Injection 15-16
i. Sub cutaneous (S.C.) 16-18
ii. Intra muscular (I.M.) 18-20
iii. Intra venous (I.V.) 20-22
iv. Intra Dermal (I.D.) 22-23
3. Patient Observation Chart 24-26
4. Prescription 27-29
5. Simple Diagnostic Reports 30-32
6. Blood Pressure measurement 33-35
7. Temperature measurement 36-37
8. Vaccination and Immunization 38-41
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
HOSPITAL INTRODUCTION
D.S HOSPITAL
Hospital name- D.S. Hospital
D.S. Hospital listed under Hospitals in Maholi Road, Mathura. D.S. Hospital in Maholi Road,
Mathura is one such reliable hospital that is committed to providing expert medical care. Having
established a firm presence as a trusted name in Hospitals, it is renowned for offering
specialised services and treatments like Ovarian Diseases, Myomectomy, Consultation, Spine
Surgery, etc.
Address and Overview- D.S. Hospital in Maholi Road, Mathura is one of the most renowned
Hospitals in the area. The practitioner holds qualification in the capacity of MBBS M, S. The
specialist has in-depth knowledge of related areas of specialization like Surgeon Doctors etc.
Countless locals in Maholi Road have placed immense trust in the practitioner over the years.
D.S. Hospital is situated at Plot No B-1/1 Industrial Area, Opposite Raman Lal Shorowala
School Near New Bus Stand, Maholi Road, Maholi Road-281001 near Opposite Raman Lal
Shorowala School Near New Bus Stand, which is easily accessible through various modes of
transport.
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
FACILITIES AVAILABLE IN HOSPITAL
There is a general ward consisting of 18 beds.
There is surgical ward consisting of 20 beds.
Round the clock water and electricity supply.
A canteen for both in and out patient.
24h security through CCTV and also manually.
24×7 service available.
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
FOLLOWING DEPARTMENTS/WARDS OF HOSPITAL
Medical Department
General I.C.U.
Semi I.C.U.
Emergency Department (M.O.T.)
Outpatient Department (O.P.D.)
Surgery Department (General)
Orthopaedic Department
X-Ray Department with C.R. System
Fully equipped pathology lab with modern equipments
2 operation theatres (O.T.) with all facilities.
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
S.NO Name of Doctor Qualification
1. Dr. Lalit Varshney M.B.B.S, M.S, FIAGES
2. Dr. Shefali S. Varshney M.B.B.S, M.D
3. Dr. Saurabh Bansal M.B.B.S, M.S (Ortho)
4. Dr . Megha Yadav M.B.B.S, D.G.O
(Obst & Gynae)
5. Dr. Arijit Singh Sikarwar M.B.B.S, M.D
6. Dr. Sambhav Yadav M.B.B.S, M.D (Paediatric)
7. Dr. Amit Varshney D.P.H, M.P.T (Ortho)
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
ACTIVITIES PERFORMED DURING TRAINING
The activities performed during training were: -
1. First Aid
i. Artificial Respiration
ii. Mouth to Mouth Resuscitation
iii. Mouth to Nose Resuscitation
2. Different routes of Injection
i. Sub cutaneous (S.C.)
ii. Intra muscular (I.M.)
iii. Intra venous (I.V.)
iv. Intra dermal (I.D)
3. Patient Observation Chart
4. Prescription
5. Simple Diagnostic Reports
6. Blood Pressure measurement
7. Temperature measurement
8. Vaccination and Immunization
10
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
FIRST AID
First aid is the assistance given to any person suffering a sudden illness or injury, with care
provided to preserve life, prevent the condition from worsening, and/or promote recovery. It
includes initial intervention in a serious condition prior to professional medical help being
available, such as performing CPR while awaiting an ambulance, as well as the complete
treatment of minor conditions, such as applying a plaster to a cut. First aid is generally
performed by the layperson, with many people trained in providing basic levels of first aid,
and others willing to do so from acquired knowledge. Mental health first aid is an extension of
the concept of first aid to cover mental health.
There are many situations which may require first aid, and many countries have legislation,
regulation, or guidance which specifies a minimum level of first aid provision in certain
circumstances. This can include specific training or equipment to be available in the
workplace (such as an Automated External Defibrillator), the provision of specialist first aid
cover at public gatherings, or mandatory first aid training within schools. First aid, however,
does not necessarily require any particular equipment or prior knowledge, and can involve
improvisation with materials available at the time, often by untrained persons.
First aid can be performed on all mammals, although this article relates to the care of human
patients.
Fig 01: The universal First Aid sign
11
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
i. Artificial Respiration
Without food a person can survive for 70 days, without water he can survive for 7 days but
without air a person cannot survive for more than 3 – 4 minutes. Therefore, whenever
breathing is stopped the patient should be immediately given artificial respiration also
known as pulmonary resuscitation to save his life.
ARTIFICIAL RESPIRATION
Fig 02: Steps in artificial respiration
ii. Mouth to Mouth Resuscitation
There are several methods of artificial respiration but mouth to mouth method is considered
as effective and easiest method to be used. During this method air is blown from the mouth of
first aider into the mouth of the victim who suffers from respiratory failure.
12
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Fig 03: Mouth to Mouth Resuscitation technique
Technique of Mouth-to-Mouth Respiration
a) Place the patient horizontally on his back on a hard flat surface.
b) Loosen clothing’s around his neck and remove any artificial teeth.
c) Clear the airway with a handkerchief. During this process the mouth of the victim
should be turned to a side so as to prevent entry of the particles into the respiratory
tract.
d) Tilt the head backwards with one hand and support the neck with other hand. This will
lift the tongue to its normal position. Thus, the airway will be cleared and the patient
may start breathing on his own.
e) If the breathing does not start, pinch the patient’s nostrils together, take a deep breath,
then seal the patient’s mouth tightly with your own mouth and breath out the air
forcefully into his lungs. Now move up your head and inhale more fresh air from the
atmosphere, again seal patient’s mouth with your own mouth and breath out the air
forcefully into his lungs. Repeat this process rapidly a number of times so as to
saturate the patient’s blood with oxygen. Afterwards 12 breathings per minute should
be given to an adult patient. Continue this procedure till the patient starts breathing on
his own.
Pinching the nose during mouth-to-mouth respiration is very important because the nose and
mouth are connected with each other by an air passage. If the nose is kept open, air would go
out through the nose and will not enter the lungs where it is needed.
iii. Mouth to Nose Resuscitation
When mouth to mouth respiration is not possible then mouth to nose respiration is given. In
this case the mouth is closed by the first aider’s palm.
Mouth to mouth respiration is not possible when
The face is damaged,
The jaw is damaged,
13
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Lips and mouth have been burned by a poison, or due to any other reason.
Fig 04: Mouth to Nose
Resuscitation technique
Technique of Mouth-to-Mouth Respiration
Close the victim mouth completely. Use your hand i.e., not on the victim’s forehead to
lift his jaw and close his mouth. It is important that no air escape through the victim’s
mouth when you perform ventilation.
Give two quick, full breath. Take a deep breath and seal your lips around the victim’s
nose and blow into his nose. (Be sure two quick are given with 3 seconds. Observe the
victim’s chest as you administer the two breath).
Remove your mouth from the victim’s nose. Either open his mouth or separate his lips
so
that he can exhale passively.
Watch the victim’s chest. When you see it rise, stop blowing, raise your mouth, turn
your head to the side and listen for exhalation.
DIFFERENT ROUTES OF INJECTION
14
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Parenteral Routes of Administration
(Par – beyond, enteral – intestinal)
Routes of drug administration other than oral route are known as Parenteral route. This refers
to administration by injection which takes the drug directly into the tissue fluid or blood
without having to cross the intestinal mucosa.
Advantages of parenteral route
Action is faster and surer.
Gastric irritation and vomiting are not provoked.
It can be employed even in unconscious, uncooperative and vomiting patient.
There are no chances of interference by food or digestive juices.
Liver is bypassed.
Disadvantages of parenteral route
The preparation has to be sterilized and is costlier.
The technique is invasive and painful.
Assistance of another person is mostly needed.
There are chances of local tissue injury and in general it is riskier.
The important parenteral routes are:
Subcutaneous (s.c.)
Intramuscular (i.m.)
Intravenous (i.v.)
15
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Intradermal injection
Fig 05: Parenteral routes
i. Sub cutaneous injection
The drug is deposited in the loose subcutaneous tissue which is richly supplied by nerves
(irritant drug cannot be injected) but is less vascular (absorption is slower). Self-injection is
possible because deep penetration is not needed. This route should be avoided in shock
patients who are vasoconstricted – absorption will be delayed. Repository (depot)
preparations – oily solutions or aqueous suspensions can be injected for prolonged action.
Some special forms of this route are
a. Dermo jet: In this method needle is not used; a high velocity jet of drug solution is
projected from a micro fine orifice using a gun like implement. The solution passes
through the superficial layers and gets deposited in the subcutaneous tissue. It is
essentially painless and suited for mass inoculations.
b. Pellet implantation: The drug as solid pellet is introduced with a trocar and cannula.
This provides sustained release of the drug over week and months, e.g., DOCA,
testosterone.
c. Sialistic (non-biodegradable) and biodegradable implants: Crystalline drug is
packed in tubes made of suitable material and implanted under the skin. Slow and
uniform leaching of the drug occurs over months providing constant blood levels. The
16
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
non-biodegradable implant has to be removed later on but not the biodegradable one.
This have been tried for hormones and the contraceptives (e.g., NORPLANT).
17
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Fig 06: - Subcutaneous Injection Angle
Procedure
Subcutaneous injections are inserted at 45-90o angles, depending on amount of subcutaneous
tissue present and length of needle- a shorter, 3/8" needle is usually inserted 90 degrees and a
5/8" needle is usually inserted at 45 degrees. Medication is administered slowly, about 10
seconds/mL.
Wash the hands thoroughly and wear the gloves.
Choose the appropriate site for sub-cutaneous injection and skin should be inspected to
make sure there is no bruising, burns, swelling, hardness, or irritation in the area.
The skin must be cleansed with alcohol swab.
The skin should be held in a pinch between thumb and index finger. Thrust or inject the
needle into the skin quickly, but without great force at angle of 90° to 45°. (The angle is
varied on the body fat 2inches skin size use angle 90° and 1inch skin size use angle
45°).
Apply a gauge over the site of injection and needle is pulled out of the skin.
Subcutaneous injections are highly effective in administering vaccines and medications
such as
18
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Morphine,
Diacetylmorphine,
Goserelin, and
Insulin.
ii. Intra muscular injection
The drug is injected in one of the large skeletal muscles – deltoid, triceps, gluteus maximus,
rectus femoris, etc. Muscle is less richly supplied with sensory nerves (mild irritants can be
injected) and is more vascular (absorption is faster). It is less painful but self-injection is often
impracticable – deep penetration is needed. Depot preparations can be injected by this route.
Procedure
Wash hands properly and wear clear apron and gloves.
Withdraw the amount of drug required.
Remove any air bubble from the syringe.
Change the syringe needle to one of the correct sizes for the patient.
Clean the skin surface with spirit/antiseptic solution.
Insert the needle of syringe in the skin surface at 90º angle.
Withdraw the piston of syringe (to ensure that the needle has not penetrated into blood
vessel), observing for a flashback of blood into the syringe. If this occurs, do not inject the
drug.
If there is no blood flashback, slowly administer the drug and withdraw the needle
smoothly and quickly at 90º.
19
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
And rub that place with spirit cotton.
Fig 07: Intramuscular injection sites
Fig 08: Intramuscular injection angle
Examples of medications that are sometimes administered intramuscularly are
20
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Haloperidol
Chlorpromazine
Lorazepam
Diazepam
Morphine
Prednisone
Streptomycin
Penicillin
Ketamine
Naloxone
Vitamin B12
Sex hormones, such as testosterone, oestradiol valerate, and medroxyprogesterone
acetate (as Depo Provera).
In addition, some vaccines are administered intramuscularly
Gardasil
Hepatitis A vaccine
Rabies vaccine
Influenza vaccines
iii. Intra venous injection
The drug is injected as a bolus or infused slowly over hours in one of the superficial veins.
Intravenous simply means "within vein". The drug directly reaches into the blood stream and
effects are produced immediately. These can be minimized by diluting the drug or injecting it
into a running i.v. line. Only aqueous solutions (not suspensions) can be injected i.v. and
there are no depot preparations for this route. The dose of the drug required is smallest
(bioavailability is 100%) and even large volumes can be infused. One big advantage with this
route is – in case response is accurately measurable (e.g., BP) and the drug short acting (e.g.,
noradrenaline), titration of the dose with the response is possible.
21
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Fig 09: I.V. injection sites
Procedure
Wash your hands properly and wear the gloves.
Uncover the arm of patient completely.
Have the patient relax and support his arm below the vein to be used.
Apply tourniquet and look for a suitable vein.
Wait for the vein to swell and then, disinfect the place, stabilize the vein by pulling the
skin taut in the longitudinal direction of the vein.
Now, Insert the needle at an angle of around 35º.
Puncture the skin and move the needle slightly into the vein (3-5mm).
If blood appears hold the syringe steady, you are in the vein but if it not, try again.
Loosen tourniquet and inject the drug very slowly. Check for pain, swelling,
hematoma. If not, Withdraw the needle swiftly and press sterile cotton wool onto the
opening or secure with adhesive tape.
Fig 10: Intra venous therapy
Substances that may be infused intravenously include -
Volume expanders,
Blood-based products,
22
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Blood substitutes,
Medications and nutrition.
iv. Intra dermal injection
Intradermal injection is the injection of a substance into the dermis, just below the epidermis.
This route has the longest absorption time as compared to subcutaneous injections and
intramuscular injections. As a result, it is used for sensitivity tests, like Tuberculin and allergy
tests, and for local anaesthesia. Additionally, the body's reaction to substances is more easily
visible since it is closer to the surface.
Injection sites
Common injection sites include the inner surface of the forearm and the upper back, under the
scapula.
Fig 11: Intradermal injection
Procedure
The angle of administration is 5 to 15 degrees, almost against the skin. With bevel (opening)
side up, insert about 1/8" with entire bevel inside and inject while watching for small wheal or
blister to appear.
The injection site is rubbed vigorously with a cotton swab, and disinfectant is applied to
cleanse the area and increase the blood supply.
With the bevel of the needle facing upwards, the needle is inserted into the skin, parallel
with the forearm.
The syringe should then be pushed in steadily and slowly, releasing the solution into the
layers of the skin. This will cause the layers of the skin to rise slightly.
BCG vaccine and Small pox vaccine is administered by intra dermal route.
23
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
PATIENT OBSERVATION CHART
24
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
An observation and response chart are a document that allows the recording of patient
observations, and specifies the actions to be taken in response to deterioration from the norm.
The purpose of these charts is to support accurate and timely recognition of clinical
deterioration, and prompt action when deterioration is observed. The way in which
observation charts are designed and used can contribute to both the poor recording of
observations and failure to interpret them correctly.
Fig 12: Patient Observation Chart
Medical history of patient: It includes as-
Surgical history
The surgical history is a chronicle of surgery performed for the patient. It may have dates of
operations, operative reports, and/or the detailed narrative of what the surgeon did.
Obstetric history
The obstetric history lists prior pregnancies and their outcomes. It also includes any
complications of these pregnancies.
25
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Medications and medical allergies
The medical record may contain a summary of the patient's current and previous medications as
well as any medical allergies.
Family history
The family history lists the health status of immediate family members as well as their causes
of death (if known). It may also list diseases common in the family or found only in one sex or
the other. It may also include a pedigree chart. It is a valuable asset in predicting some
outcomes for the patient.
Social history
The social history is a chronicle of human interactions. It tells of the relationships of the patient,
his/her careers and trainings, and religious training. It is helpful for the physician to know what
sorts of community support the patient might expect during a major illness. It may explain the
behaviour of the patient in relation to illness or loss. It may also give clues as to the cause of an
illness (e.g., occupational exposure to asbestos).
Habits
Various habits which impact health, such as tobacco use, alcohol intake, exercise, and diet are
chronicled, often as part of the social history. This section may also include more intimate
details such as sexual habits and sexual orientation.
Immunization history
The history of vaccination is included. Any blood tests proving immunity will also be included
in this section.
Growth chart and developmental history
26
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
For children and teenagers, charts documenting growth as it compares to other children of the
same age is included, so that health-care providers can follow the child's growth over time.
Many diseases and social stresses can affect growth, and longitudinal charting can thus provide
a clue to underlying illness. Additionally, a child's Behavior (such as timing of talking,
walking, etc.) as it compares to other children of the same age is documented within the
medical record for much the same reasons as growth.
PRESCRIPTION
27
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Fig 13: Prescription Symbol
Prescription is a written order from a registered medical practitioner, or other properly licensed
practitioners, such as dentist, veterinarian etc. to a pharmacist to compound and dispense a
specific medication for the patient. The order is accompanied by directions for the pharmacist
to prepare a specific type and quantity of preparation for the patient, the prescription also
includes the direction for the patient regarding the mode of administration of drugs, which is
dispensed for him. Thus, prescription is a media through which treatment is provided for a
patient by the combined skill and services of both the physician and the pharmacist.
The prescription is generally written in the English language but Latin words or abbreviations
are frequently used in order to save time. So, it becomes necessary for a pharmacist, t become
28
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
familiar with the common Latin terms and abbreviations used by the prescriber while writing
the prescription.
Parts of a prescription
Prescription is generally written on a typical format which are usually kept as pads. A typical
prescription consists of following parts –
Date;
Name, age, sex and address of the patient;
Superscription;
Inscription;
Subscription;
Signature;
Renewal instructions;
Signature, address and registration number of the prescriber.
I Date – It helps a pharmacist to find out the date of prescribing and date of presentation
for filling the prescription. The prescription which prescribes narcotic or other habit-
forming drugs, must bear the date, so as to avoid the misuse of prescription if it is
presented by the patient, a number of times for dispensing.
II Name, age, sex and address of the patient – It must be written in the prescription
because it serves to identify the prescription. In case, if any of this information is
missing in the prescription, the same may be included by the pharmacist after proper
enquiry from the patient. Age and sex of the patient, especially in case of children, help
the pharmacist to check the prescribe dose of medication.
III Superscription – It is represented by a symbol Rx which is written before writing the
prescription. Rx is an abbreviation of the Latin word recipe, meaning ‘you take’ (Take
thou). In olden days, the symbol was considered to be originated from the sign of
Jupiter, God of healing. This symbol was employed by the ancient in requesting God for
the quick recovery of the patient.
IV Inscription – this is the main part of the prescription order, contains the name and the
quantities of the prescribed ingredients. The names of the ingredients are generally
written in the English language but common abbreviation used can be written in both
English and Latin languages.
29
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Extreme care should be taken by the pharmacist in interpreting the abbreviations; otherwise, it
can lead to serious errors.
The medicament may be prescribed as an official preparation, a proprietary product, a non-
proprietary product (generic), not official or a specific or individual formula. In case of special
or individual formula, the quantity of each ingredient will be stated together with a description
of the type of the preparation, e.g., cream, mixture, lotion etc.
The name of each ingredient is written on the separate line along with its quantity. In complex
prescriptions containing several ingredients the inscription is divided into following parts:
i Base: The active medicaments which are intended to produce the therapeutic effects.
ii Adjuvant: It is included either to enhance the action of medicament or to improve the
palatability of the preparation
iii Vehicle: It is included in the prescription either to dissolve the solid ingredients or to
increase the volume of the preparation.
Now a days, the majority of the drugs are prescribed which are already in a suitable
formulation. The pharmacist is required to dispense the readymade form of drugs. So,
compounding of prescription is almost eliminated.
V Subscription: This comprises direction to the pharmacist for preparing the prescription
and number of doses to be dispensed. These days, the prescribers are omitting the
specific instructions to the pharmacist because the majority of the prescriptions are not
compounded and dispensed.
VI Signature: This consists of the direction to be given to the patients regarding the
administration of the drug. It is usually written as ‘Sig’ on the prescription. The
instructions given in the prescription are required to be transferred to the label of the
container in which the medicament is to be dispensed, so that the patient can follow it.
The instructions may include:
a) The quantity to be taken or amount to be used.
b) The frequency and timing of administration or application.
c) The route of administration.
d) The special instructions such as dilution direction.
30
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
VII Renewal instructions: The prescriber indicate on every prescription order, whether it
may be renewed or if so, how many times. It is very important particularly in the
prescription containing the narcotic and other habit-forming drugs to prevent its misuse.
VIII Signature, address and registration number of the prescriber: The prescription
must bear the signature of the prescriber along with its registration number and address.
SIMPLE DIAGNOSTIC REPORT READING
This report may include as follows
HAEMOGBLOBIN TEST: - Haemoglobin is the iron containing oxygen transport
metalloprotein in the red blood cells of all vertebrates.
This test is often used to check for anaemia, usually along with haematocrit or as part of
complete blood count.
TOTAL LEUKOCYTE COUNT (TLC): - White blood cells are also known as
leukocytes. These are cells of the immune system that are involved in protecting body
against both infectious disease and foreign invaders. WBC are of 2 types as-
a. Agranulocyte (Further of two type lymphocyte and monocyte).
b. Granulocytes (Further of three types eosinophil, basophil, and neutrophil).
Eosinophils are increase in response to allergies, parasitic infection and disease of
central nervous system, spleen and collagen.
Basophils are chiefly responsible for allergic and antigen response by releasing the
chemical histamine.
Neutrophils re increase when the bacterial and fungal infection occurs in the body.
Monocytes are responsible for phagocytosis.
31
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
TLC test count the number of white blood cells in the body. Any deviation from the normal
range implies to disease process. Decrease in white blood cells count is called leukopenia.
And high WBC count is known as leucocytosis.
DLC (Different leukocyte count) This blood test measures the percentage of each type
of WBC in your blood.
PCV (packed cell volume) The PCV test is used to measure the number of cells in the
blood. MCV (Mean corpuscular volume) MCV test is a measure of the average
volume of RBCS. MCH (Mean cell haemoglobin) it is the average of haemoglobin per
RBCs in a sample of blood.
MCHC (Mean cell haemoglobin concentration) It is the measure of the concentration
of haemoglobin in a given volume of packed RBCS.
TOTAL RBCS COUNT Total RBCS count test measure that how many RBCs you have.
TOTAL PLATE LETS COUNT TEST It is a diagnostic test that determine the
number of platelets in the blood. Platelets are the cells which are present in blood and
responsible for the blood clotting. Platelets are also known as thrombocyte.
S. GLUCOSE(Random) TEST This is the type of blood test used to determine the
amount of glucose in the blood. In this amount of glucose is measured in the serum.
S. UREA TEST This test involves measurement of urea in the serum. When the
amount of urea is increase it indicates misfunctioning of kidney.
S.CREATININE TEST In this test the amount of creatinine is determined in the
serum. If the creatinine level is deviated from the normal level, it indicates impaired
kidney function.
S.G.O.T(Serum glutamic oxaloacetic transaminase)TEST Serum glutamic
oxaloacetic transaminase is an enzyme. In this test its amount is measured. This
enzyme is present in the liver and heart cells. This enzyme releases into the blood when
the liver or heart is damaged.
S.G.P.(Serum glutamic pyruvic transaminase) TEST This test measures an enzyme
called Serum glutamic pyruvic transaminase. This enzyme made in liver, these releases
when liver is damage.
S.BILRUBIN TEST(TOTAL) This test is used to detect bilirubin increased level in
the blood. It may be used to help determine the cause of jaundice, liver disease, and
haemolytic. And also, for blockage of the bile ducts.
32
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
S.SODIUM (Na+) TEST This test is performed to measure the amount of sodium in
the serum. Decrease or increase amount of sodium show dis functioning of adrenal
gland and other reason.
S.POTASSIUM(K+) TEST This test is performed to measure the amount of
potassium in the serum. Decrease or increase amount of sodium show dis functioning
of adrenal gland and other reason.
S.CALCIUM (Ca2+) TEST This test is used to measure the amount of calcium in
serum. If the calcium is high then its leads to various misfunctioning of body like
hyperthyroidism, osteomalacia, etc. And if the amount is low due to kidney failure,
pancreatitis etc.
33
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Table 01: Different diagnostic test values
TEST NAME STANDARD VALUE
Hemoglobin(Hb) Male 15±2gm%, Female 13.5±2gm%
Total leucocyte count 4000-11,000/cumm
Different leucocyte count:-
Polymorphs 45-75%
Lymphocyte 20-40%
Eosinophils 1-6%
Monocytes 02-10%
Basophils 00-01%
PCV Male 45±5%, female 40±5%
MCV 76-96Ft/dl
MCH 27-32Pg/dl
Total RBCs count Male 5±0.5mill/cumm, female 4.5±0.5mill/cumm
Platelets count 1.5-4.5 lakh/cumm
S.Glucose(R) 60-150mg/dl
S,Urea 10-40 mg/dl
S.Creatinine 0.6-1.4 mg/dl
S .G.O.T. 08-40IU/L
S. G.P.T. 08-40IU/L
S. BILIRUBIN(Total) 02-1.2mg/dl
S.SODIUM(Na+) 136-150meq/L
S. POTASSIUM(K+) 3.5-5.0 meq/L
BLOOD PRESSURE MEASUREMENT
34
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Blood pressure (BP) is the pressure of circulating blood on the walls of blood vessels. When
used without further specification, "blood pressure" usually refers to the arterial pressure in the
systemic circulation. Blood pressure is usually expressed in terms of the systolic (maximum
during one heart beat) pressure over diastolic (minimum in between two heart beats) pressure
and is measured in milli-meters of mercury (mmHg).
It is one of the vital signs, along with respiratory rate, heart rate, oxygen saturation, and body
temperature. Normal resting systolic (diastolic) blood pressure in an adult is approximately 120
mmHg (80 mmHg), abbreviated "120/80 mmHg".
Blood pressure is determined, moment by moment, by the balance between heart output
versus total peripheral resistance and varies depending on situation, emotional state,
activity, and relative health/disease states. It is regulated by the brain via both the nervous
and endocrine systems.
Blood pressure that is low due to a disease state is called hypotension, and pressure that is
consistently high is hypertension. Both have many causes which can range from mild to severe.
Both may be of sudden onset or of long duration. Long term hypertension is a risk factor for
many diseases, including heart disease, stroke and kidney failure. Long term hypertension is more
common than long term hypotension in Western countries. Long term hypertension often goes
undetected because of infrequent monitoring and the absence of symptoms.
Table 02: Classification of blood pressure for adults
35
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Table 03: Classification of blood pressure for children
Stage Approximate Systolic Diastolic
age
Infants 1 to 12 months 75–100 50–70
Toddlers and 1 to 5 years 80–110 50–80
preschoolers
School age 6 to 12 years 85–120 50–80
Adolescents 13 to 18 years 95–140 60–90
Measurement of blood pressure
Arterial pressure is most commonly measured via a sphygmomanometer, which uses the height of
a column of mercury to reflect the circulating pressure. Blood pressure values are generally
reported in millimetres of mercury (mmHg).
For each heartbeat, blood pressure varies between systolic and diastolic pressures. Systolic
pressure is peak pressure in the arteries, which occurs near the end of the cardiac cycle when the
ventricles are contracting. Diastolic pressure is minimum pressure in the arteries, which occurs
near the beginning of the cardiac cycle when the ventricles are filled with blood. An example of
normal measured values for a resting, healthy adult human is 120 mmHg systolic and 80 mmHg
diastolic (written as 120/80 mmHg, and spoken as "one-twenty over eighty").
Systolic and diastolic arterial blood pressures are not static but undergo natural variations from
one heartbeat to another and throughout the day (in a circadian rhythm). They also change in
response to stress, nutritional factors, drugs, disease, exercise, and momentarily from standing up.
Sometimes the variations are large.
36
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Fig 14: Mercury manometer
Procedure
Firstly, Wrap the cuff around the upper arm with the cuff’s lower edge one inch above the
antecubital fossa.
Lightly press the stethoscope’s bell over the branchial artery just below the cuff’s edge.
Rapidly inflate the cuff to 180mmHg or maximum upto 250mmhg.Now, release the air
from the cuff at a moderate rate (3mm/sec) and try to listen first knocking sound with
stethoscope and simultaneously observe the sphygmomanometer.
The first knocking sound (Korotkoff) is the subject’s systolic pressure. When this knocking
sound get disappears that is the diastolic pressure (such as 120/80mmHg).
Record the observed blood pressure and note the difference or filed it into patient
observation chart.
37
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
TEMPERATURE MEASUREMENT
Normal human body temperature, also known as normothermia or euthermia, is a narrow
temperature range indicating optimal health and thermoregulation. Individual body temperature
depends upon the age, exertion, infection, sex, time of day, and reproductive status of the
subject, the place in the body at which the measurement is made, the time of day, the subject’s
state of consciousness (waking or sleeping), activity level, and emotional state.
The body temperature of a healthy person varies during the day by about 0.5 °C (0.9 °F) with
lower temperatures in the morning and higher temperatures in the late afternoon and evening, as
the body’s needs and activities change. Other circumstances also affect the body’s temperature.
The core body temperature of an individual tends to have the lowest value in the second half of
the sleep cycle; the lowest point, called the nadir, is one of the primary markers for circadian
rhythms. The body temperature also changes when a person is hungry, tired, sick, or cold.
Taking a person’s temperature is an initial part of a full clinical examination. There are various
types of medical thermometers, as well as sites used for measurement, including:
In the anus (rectal temperature)
In the mouth (oral temperature)
Under the arm (axillary temperature)
In the ear (tympanic temperature)
In the vagina (vaginal temperature)
In the bladder
On the skin of the forehead over the temporal artery
Thermometer:
A thermometer is a device that measures temperature or a temperature gradient. A
thermometer has two important elements:
1. A temperature sensor (e.g. the bulb of a mercury-in-glass thermometer) in which some
physical change occurs with temperature.
2. Some means of converting this physical change into a numerical value (e.g., the visible
scale that is marked on a mercury-in-glass thermometer).
38
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Fig 15: A mercury thermometer
Procedure
Firstly, wash the thermometer with antiseptic solution / spirit.
Now place the thermometer below the tongue or other suitable place (such as under arm)
and leave for 1min. to gain the accurate temperature of patient.
Remove out the thermometer and observe the level of mercury in thermometer.
Note the temperature and differentiate from standard value and filed into patient
observation chart.
39
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
VACCINATION AND IMMUNIZATION
Vaccination is the administration of antigenic material (a vaccine) to stimulate an individual's
immune system to develop adaptive immunity to a pathogen.
The effectiveness of vaccination has been widely studied and verified; for example, the influenza
vaccine, the HPV vaccine, and the chicken pox vaccine.
Vaccination is the most effective method of preventing infectious diseases.
A vaccine administration may be oral, by injection (intramuscular, intradermal, subcutaneous),
by puncture, transdermal or intranasal.
Some of the vaccines are
Tetanus vaccine
BCG vaccine
Hepatitis B vaccine
Pentavalent vaccine
Polio vaccine
DPT vaccine
Measles vaccine
i Tetanus vaccine
Tetanus vaccine, also known as tetanus toxoid (TT), is a vaccine used to prevent tetanus.[1]
During childhood five doses are recommended, followed by additional doses every ten years.
After three doses almost everyone is immune.
The vaccine is very safe including during pregnancy and in those with HIV/AIDS.
Fig 16: Tetanus vaccine
40
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Schedule
The first vaccine is administered at infancy. The baby is injected with the DTaP vaccine which is 3
inactive toxins in one injection. DTaP protects against diphtheria, pertussis, and tetanus. This
vaccine is safer than the previously used DTP.
Another option for infants is DT which is a vaccine that is a combination of diphtheria and tetanus
vaccines. This is given as an alternative to infants who have conflicts with the DTaP vaccine.
TD and TDaP are to be administered to older children, adolescents, and adults so it can therefore be
injected into the deltoid muscle. These are boosters and are therefore to be administered at least
every ten years. And it is safe to have shorter intervals between a single dose of Tdap and a dose of
the Td booster.
ii. BCG vaccine
Bacillus Calmette–Guérin (BCG) vaccine is a vaccine primarily used against tuberculosis.
It is also often used as part of the treatment of bladder cancer.
Serious side effects are rare. Often there is redness, swelling, and mild pain at the site of injection.
A small ulcer may also form with some scarring after healing. . It is not safe for use during
pregnancy. The vaccine was originally developed from Mycobacterium bovis which is commonly
found in cows.
BCG vaccination is recommended to be given intradermally.
Some BCG vaccines are freeze dried and become fine powder. Such a glass ampoule has to be
opened slowly to prevent the airflow from blowing out the powder. Then the powder has to be
diluted with saline water before injecting.
41
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Fig 17: BCG vaccine
Schedule
In countries where tuberculosis is common one dose is recommended in healthy babies as close to
the time of birth as possible.[1] Babies with HIV/AIDS should not be vaccinated.[2] In areas where
tuberculosis is not common, only babies at high risk are typically immunized while suspected cases
of tuberculosis are individually tested for and treated.
Method of Administration
Except in neonates, a tuberculin skin test should always be done before administering BCG. A
reactive tuberculin skin test is a contraindication to BCG. Someone with a positive tuberculin
reaction is not given BCG, because the risk of severe local inflammation and scarring is high, not
because of the common misconception that tuberculin reactors "are already immune" and therefore
do not need
BCG is given as a single intradermal injection at the insertion of the deltoid. If BCG is accidentally
given subcutaneously, then a local abscess may form (a "BCG-Oma") that can sometimes ulcerate,
and may require treatment with antibiotics immediately, otherwise without treatment it could spread
the infection causing severe damage to vital organs.
iii. Hepatitis B vaccine
Hepatitis B vaccine is a vaccine that prevents hepatitis B.[1] The first dose is recommended within
24 hours of birth with either two or three more doses given after that.
Serious side effects from the hepatitis B vaccine are very uncommon. Pain may occur at the site of
injection. It is safe for use during pregnancy or while breastfeeding.
Babies born to mothers infected with HBV are vaccinated with hepatitis B vaccine and injected
with hepatitis B immunoglobulin (HBIG).
42
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
lOMoARcPSD|42080776
Fig 18: Hepatitis B vaccine
iv Polio vaccine
Polio vaccines are vaccines used to prevent poliomyelitis (polio).[1] One type uses inactivated
poliovirus and is given by injection (IPV), while the other type uses weakened poliovirus and is
given by mouth (OPV). The World Health Organization recommends all children be vaccinated
against polio.
The inactivated polio vaccines are very safe. Mild redness or pain may occur at the site of injection.
Oral polio vaccines result in vaccine-associated paralytic poliomyelitis in about three per million
doses.
Fig 19: Polio vaccine
Schedule
The World Health Organization recommends three or four doses starting at two months of age.
43
Downloaded by PHARMA CRACKERS (pharmacrackerswill2win@gmail.com)
You might also like
- QC Tests For Oral Liquid Dosage FormsDocument13 pagesQC Tests For Oral Liquid Dosage FormsMitesh Jain100% (4)
- Laboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceFrom EverandLaboratory Total Quality Management for Practitioners and Students of Medical Laboratory ScienceRating: 5 out of 5 stars5/5 (4)
- Updated Marketing Project For MBADocument99 pagesUpdated Marketing Project For MBAadamodharNo ratings yet
- Project Submitted To Osmania University Towards The Partial Fulfilment of The Award of Masters Degree in Hospital ManagementDocument59 pagesProject Submitted To Osmania University Towards The Partial Fulfilment of The Award of Masters Degree in Hospital ManagementAnkitChauhan100% (1)
- Reflection Paper SPEDDocument5 pagesReflection Paper SPEDMariecris Barayuga Duldulao-AbelaNo ratings yet
- Practice Writing A Report: Scenario 1Document2 pagesPractice Writing A Report: Scenario 1Olga100% (1)
- Clinical PharmacyDocument25 pagesClinical PharmacyHariom patelNo ratings yet
- Hos (1) - MergedDocument59 pagesHos (1) - Mergedanshulthestylorider2No ratings yet
- PithecellobiumDocument54 pagesPithecellobiummirahsanali69No ratings yet
- Dipak FinalDocument59 pagesDipak FinalMohammed Omar SharifNo ratings yet
- DHARSHINI R PDFDocument41 pagesDHARSHINI R PDFkesavanbsc17No ratings yet
- Samarjit Thesis-1Document16 pagesSamarjit Thesis-1himanshubehera73No ratings yet
- KAHKASHA Full ProjectsDocument113 pagesKAHKASHA Full Projectscity9848835243 cyber100% (1)
- DUE of PIPERACILLIN and TazobactumDocument73 pagesDUE of PIPERACILLIN and Tazobactumanup jagarlamudiNo ratings yet
- 86-90 GroupDocument30 pages86-90 GroupSai krishna PoojithaNo ratings yet
- 43 Shravan ParmarDocument30 pages43 Shravan Parmarsai projectNo ratings yet
- MaruffDocument4 pagesMaruffchoudhary25092000No ratings yet
- Project 115Document30 pagesProject 115Rushikesh PatilNo ratings yet
- 2022 Internship Manual PhysiotherapyDocument82 pages2022 Internship Manual PhysiotherapyRizwan KhanNo ratings yet
- Sachin Hospital 2 Training FinalDocument45 pagesSachin Hospital 2 Training Finaldevnishad985No ratings yet
- DALLUDocument15 pagesDALLUdalchandsahu74No ratings yet
- Project ReportDocument31 pagesProject ReportRamish KhanNo ratings yet
- Hospital Training ReportDocument26 pagesHospital Training ReportAlex GamingNo ratings yet
- Anti Inflammatory Prospective Study of Commiphora Mukul (Guggul) On Wistar Albino RatsDocument54 pagesAnti Inflammatory Prospective Study of Commiphora Mukul (Guggul) On Wistar Albino RatsKrish NalimelaNo ratings yet
- Prashant Pps Front PgesDocument6 pagesPrashant Pps Front PgesM. Shoeb Sultan100% (1)
- Artificial Intelligence: Mr. Hakim SinghDocument24 pagesArtificial Intelligence: Mr. Hakim SinghAman kumarNo ratings yet
- "Sugantha Malli Chooranam" "Sugantha Malli Chooranam" For The Treatment of "Lasuna Thabitham" "Sugantha Malli Chooranam"Document179 pages"Sugantha Malli Chooranam" "Sugantha Malli Chooranam" For The Treatment of "Lasuna Thabitham" "Sugantha Malli Chooranam"AzarudeenNo ratings yet
- Rajat Hopital ReportDocument29 pagesRajat Hopital ReportRajat Rastogi 143No ratings yet
- Industrial Training RecordDocument31 pagesIndustrial Training RecordPrint SolutionNo ratings yet
- Method Development and Validation For The Simultaneous Estimation of Lobeglitazone Sulphate and Glimepiride by HPLC MethodDocument113 pagesMethod Development and Validation For The Simultaneous Estimation of Lobeglitazone Sulphate and Glimepiride by HPLC MethodShikha MishraNo ratings yet
- Srilekha DeyDocument33 pagesSrilekha Deyunplugged ZoneNo ratings yet
- 8th Sem Project FinalDocument37 pages8th Sem Project FinalArsh DNo ratings yet
- Medication Disposal Household Practices in KarachiDocument8 pagesMedication Disposal Household Practices in KarachiFazal JalalNo ratings yet
- Hydrogel FrontDocument7 pagesHydrogel FrontVaibhav SharmaNo ratings yet
- Hospital Report 2 NDDocument83 pagesHospital Report 2 NDAbdul MannanNo ratings yet
- Hydrogel FrontDocument7 pagesHydrogel FrontVaibhav SharmaNo ratings yet
- ProjectDocument113 pagesProjectvishal sharmaNo ratings yet
- Vaishnavi Singh B.Pharm. Iiird Year, V Semester Roll No.1900560500097Document11 pagesVaishnavi Singh B.Pharm. Iiird Year, V Semester Roll No.1900560500097Vishnu SinghNo ratings yet
- Sustained Release Matrix Tablet of Diltiazem Hydrochloride It'S Formulation and EvaluationDocument10 pagesSustained Release Matrix Tablet of Diltiazem Hydrochloride It'S Formulation and EvaluationruriNo ratings yet
- Shri Govindram Seksaria Institute of Technology and ScienceDocument33 pagesShri Govindram Seksaria Institute of Technology and ScienceSunny Thakur17No ratings yet
- INDUSTRIAL TRANING - Garima SinghDocument17 pagesINDUSTRIAL TRANING - Garima SinghARVIND KUMARNo ratings yet
- Praveen ProjectDocument81 pagesPraveen Projectpraveen kumarNo ratings yet
- ANURAG Pharmaceutical-Industrial-Training-ReportDocument69 pagesANURAG Pharmaceutical-Industrial-Training-ReportRajat Rastogi 143No ratings yet
- Prospectus DipsarDocument36 pagesProspectus DipsarAnkit Arora0% (1)
- Sushma Verma BMWDocument37 pagesSushma Verma BMWPiaNo ratings yet
- Sapna 4th Yr 1newDocument23 pagesSapna 4th Yr 1newSAPNANo ratings yet
- A Clinical Study On: Diagnostic Methdology of PaanduDocument211 pagesA Clinical Study On: Diagnostic Methdology of PaanduThe logical humanNo ratings yet
- Pharmacy FRONTDocument4 pagesPharmacy FRONTSapna KumariNo ratings yet
- Ndds SK ProjectDocument72 pagesNdds SK ProjectShahnawaz khanNo ratings yet
- Formulation of An Instantly Dissolvable Solid Eye Drop Device For Topical Ocular DeliveryDocument243 pagesFormulation of An Instantly Dissolvable Solid Eye Drop Device For Topical Ocular DeliverystrauliaNo ratings yet
- Garima Project Report On Drug SafetyDocument27 pagesGarima Project Report On Drug SafetygariNo ratings yet
- Conference On Nanomedicine - Advances and ChallengesDocument6 pagesConference On Nanomedicine - Advances and Challengesrahulkrishna9019No ratings yet
- JMDH 400734 Application Benefits and Limitations of Telepharmacy For PDocument9 pagesJMDH 400734 Application Benefits and Limitations of Telepharmacy For PIrma RahmawatiNo ratings yet
- Practice School (Front Page)Document9 pagesPractice School (Front Page)adityaNo ratings yet
- Hospital Training ReportDocument89 pagesHospital Training ReportAbhishek SinghNo ratings yet
- Cosmetovigilance A ReviewDocument40 pagesCosmetovigilance A ReviewAnshulNo ratings yet
- Ss - KPC Medical College Final ProjectDocument141 pagesSs - KPC Medical College Final ProjectSemanti SamantaNo ratings yet
- Vydehi Institute of Medical Sciences RC Department of Pharmacology NewsletterDocument6 pagesVydehi Institute of Medical Sciences RC Department of Pharmacology NewsletterPERFECT CLASSESNo ratings yet
- Finalset 1Document57 pagesFinalset 1Tahir BilalNo ratings yet
- Syccon S-4 - 20240518 - 172351 - 0000Document15 pagesSyccon S-4 - 20240518 - 172351 - 0000thiyagaswetha.r.2018.eceNo ratings yet
- The Initial Psychiatric Interview PDFDocument4 pagesThe Initial Psychiatric Interview PDFJoan ChoiNo ratings yet
- Sunflower Production (Final) PPT - Compressed PDFDocument27 pagesSunflower Production (Final) PPT - Compressed PDFMarijenLeaño88% (8)
- Teknistae Sulakkeista Englanti PDFDocument156 pagesTeknistae Sulakkeista Englanti PDFJosué Miranda da SilvaNo ratings yet
- Ic CCT15368Document2 pagesIc CCT15368Mohamed RadyNo ratings yet
- Blood Vessels: The Human Transport System: Sbi3UDocument15 pagesBlood Vessels: The Human Transport System: Sbi3UHelloworldasdtNo ratings yet
- Un Cisic E-Bulliten 5Document3 pagesUn Cisic E-Bulliten 5taha_basit2441No ratings yet
- Welcome Madison 2013 2014Document97 pagesWelcome Madison 2013 2014Alexander León PuelloNo ratings yet
- Dinner MenuDocument3 pagesDinner MenueatlocalmenusNo ratings yet
- Senate Hearing, 111TH Congress - Department of Defense Appropriations For Fiscal Year 2010Document610 pagesSenate Hearing, 111TH Congress - Department of Defense Appropriations For Fiscal Year 2010Scribd Government DocsNo ratings yet
- Barrier Free Design GuideDocument6 pagesBarrier Free Design GuideRamesh ArjunNo ratings yet
- Hot Dip Galvanization - FaboryDocument4 pagesHot Dip Galvanization - FaboryBrandon LimNo ratings yet
- Autism Spectrum and Open-MindednessDocument2 pagesAutism Spectrum and Open-MindednessJaime MontoyaNo ratings yet
- Updated DXN Presentation1Document56 pagesUpdated DXN Presentation1xs2vicky100% (1)
- Pipe Sizing GuideDocument4 pagesPipe Sizing GuideorganicspolybondNo ratings yet
- Lifting Supervisors Guidebook Revised 2014Document15 pagesLifting Supervisors Guidebook Revised 2014Abn BK100% (1)
- Parle AgroDocument3 pagesParle AgroKumar GautamNo ratings yet
- COVID-19 Vaccines and Fetal TissueDocument3 pagesCOVID-19 Vaccines and Fetal TissueAdim AresNo ratings yet
- Subsea Exercise No.6 PDFDocument16 pagesSubsea Exercise No.6 PDFEmmanuel Byensita100% (2)
- Soal Uts Kelas 9 MtsDocument5 pagesSoal Uts Kelas 9 Mtsindah sNo ratings yet
- Mabalacat National Senior High School Address: San Isidro, Dau, Mabalacat City, PampangaDocument5 pagesMabalacat National Senior High School Address: San Isidro, Dau, Mabalacat City, PampangaJel Louis LopezNo ratings yet
- Royal Wolf Product CatalogueDocument52 pagesRoyal Wolf Product Cataloguecadsifu100% (1)
- Components of A Gating System: VIT University 1Document11 pagesComponents of A Gating System: VIT University 1aryanNo ratings yet
- Quilt of Swami Stories English v8 Onlineversion PDFDocument50 pagesQuilt of Swami Stories English v8 Onlineversion PDFGaneshNo ratings yet
- Itp - For Heat ExchangerDocument3 pagesItp - For Heat ExchangerSuraj ShettyNo ratings yet
- Tape Mobil JVC.Document16 pagesTape Mobil JVC.EdisonNainggolanNo ratings yet
- 2022 - Executive Order - BADAC - BDODocument3 pages2022 - Executive Order - BADAC - BDOromulo sigaNo ratings yet
- Introduction To Labor Economics: Chapter 2 - The Labor MarketDocument37 pagesIntroduction To Labor Economics: Chapter 2 - The Labor Marketqulb abbasNo ratings yet
- Prodotti Manuali Documento 43Document16 pagesProdotti Manuali Documento 43whorne24No ratings yet