Professional Documents
Culture Documents
Medip, ISJ-7698 O
Medip, ISJ-7698 O
Uploaded by
researchnnnnOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medip, ISJ-7698 O
Medip, ISJ-7698 O
Uploaded by
researchnnnnCopyright:
Available Formats
International Surgery Journal
Tolpadi A et al. Int Surg J. 2021 Jul;8(7):2007-2011
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: https://dx.doi.org/10.18203/2349-2902.isj20212351
Original Research Article
Impact of interventions on the incidence of thrombophlebitis in
peripheral venous cannulation in a tertiary care teaching hospital
Anuradha Tolpadi1, Abhijeet Mane1*, Meera Modak1, Ashok Kumar Verma2,
Vishwas Ambekar3, Tanuja Shilawat3
1
Department of Microbiology, 2Department of Community Medicine, Bharati Vidyapeeth (DTU) Medical College, and
Hospital, Pune, Maharashtra, India
3
Department of Infection Control, Bharati Hospital and Research Centre, Pune, India
Received: 25 May 2021
Revised: 10 June 2021
Accepted: 11 June 2021
*Correspondence:
Dr. Abhijeet Mane,
E-mail: drakmane@yahoo.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: In hospitalized patients the use of intravenous devices like cannula are indispensable. Nearly about
80% of hospitalized patients require peripheral venous cannulation, as a part of therapy. Thrombophlebitis is one of
the prevalent complications of peripheral venous cannulation.
Method: The present study was aimed to find the incidence of thrombophlebitis after peripheral venous cannulations
in the patients admitted in a tertiary care teaching hospital. Impact of regular trainings and interventions on the
incidence and grades of thrombophlebitis was also studied. The study was conducted for period of 1 year.
Result: The total of 28850 cannulations carried out on 11686 patients was observed. Phlebitis was diagnosed in 1821
peripheral venous cannulations, giving the incidence of 6.3%. As per Visual Infusion Phlebitis (VIP) score, 1527
(83.86%) were grade 1 phlebitis, 274 (15.04%) were with grade 2 phlebitis and 20 (1.10 %) were grade 3 phlebitis.
Regular surveillance, training and timely interventions were carried out during this period and the effect of these
interventions was noted in the monthly phlebitis rate. Phlebitis rate reduced from 9.89% in January to 3.99% in the
month of December. There was also reduction in grade 2 thrombophlebitis (from 21.05% in January to 6.09% in
December). In the last 4 months of study period grade 3 phlebitis was not reported.
Conclusions: A significant reduction in the incidence of phlebitis associated with peripheral intravenous cannulations
may be achieved by regular surveillance, training and timely interventions.
Keywords: Cannulation, Thrombophlebitis, Visual infusion phlebitis score
INTRODUCTION thrombophlebitis with incidence varying according to
different settings. 2
Intravenous devices are indispensable and commonly
used among hospitalized patients. In the modern practice Thrombophlebitis is the inflammation of the vessel wall
of medicine around 80% of the hospitalized patients due to the formation of blood clot. There have been many
receive intravenous (IV) therapy at some time during theories on the pathophysiology of peripheral vein
their admission.1 The peripheral venous cannulation infusion thrombophlebitis. The currently accepted
(PVC) is a commonly used invasive procedure to concept suggests that catheterization of the vein leads to
administer medications, fluids and bio products. The inflammation and thrombus formation.3
most common complication associated with it is
International Surgery Journal | July 2021 | Vol 8 | Issue 7 Page 2007
Tolpadi A et al. Int Surg J. 2021 Jul;8(7):2007-2011
If the condition does not get resolved, this may lead to nurses. Bed side training was conducted on daily basis.
other complications like pulmonary embolism, deep vein This included PVC insertion and maintenance bundles,
thrombosis, septicemia, formation of nodule and diagnosis and grading of phlebitis (VIP score).
cellulitis. Due to this a need of insertion of new cannula PowerPoint presentations, videos and hands on training
at the site other than previous is required. These was used as training module.
complications of PVCs, followed by its therapy can have
catastrophic effect on the health as well as quality of life Interventions
of patients and on the other side increasing financial
burden with longer stay in hospital and treatment. 4 Monthly changes in the incidence and grades of
thrombophlebitis over a period of one year were
The present observational study was carried out to find recorded. The effect of training and various interventions
the incidence of thrombophlebitis in peripheral venous was noted on the incidence and grades of
cannulations. Regular surveillance, training and timely thrombophlebitis. Department wise presentation of
interventions were carried out and impact of these phlebitis was made in the monthly HICC meetings.
interventions on the incidence and grade of
Weekly audits of insertion and Maintenance bundles
thrombophlebitis over a period of one year was studied.
were carried out and monthly feedback was shared with
concerned department. Feedback was given to individual
METHODS departments with names of the defaulters. Training was
intensified for the HCWs from the department showing
The present prospective observational study was carried
increase in phlebitis rate. Staff nurses and doctors who
out in a tertiary care teaching hospital, for a period of 1
did cannulations for more than second attempt were
year from January 2019 to December 2019. Study was
retrained. In the month of March use of 10 cm venous
approved by Institutional Ethics Committee.
extension (Ven-o-line, Romsons Disposable Medical
Devices, India) PVCs was implemeted all over hospital.
Patients admitted in the medical, surgical, obstetrics and
gynecology, pediatric wards and critical care unit with
peripheral venous cannulations were included in the Statistical analysis
study. Universal sampling was employed for the duration
from January 2019 to December 2019. Patients with PVC Data was entered in excel sheet and analysed using SPSS
done outside our hospital were excluded from the study. version 25. Categorical variables have been expressed as
Posters of VIP score were displayed at all the prominent frequencies and percentages.
places in the ward. Training on PVC was conducted on
regular basis for nurses and resident. RESULTS
From January 2019 record of all peripheral venous The study was carried out to observe the development of
cannulations was maintained in a register in individual phlebitis among the patients undergoing PVCs, admitted
wards. The demographic details of the patients along with in a tertiary care hospital over the period of 1 year, from
the date and time of insertion and removal of peripheral 1st January 2019 to 31st December 2019. Total 28850
venous cannula, number of attempts, and gauge of the PVCs carried out on 11686 patients, were monitored till
needle used were recorded. Record was also maintained the cannula was removed. When the patients were
in nurse’s care plan. divided on the basis of age there were 5142 (44%)
patients below the age of 45 years and 6544 (56%) were
Daily PVC site was monitored for the development of the above the age of 45 years. Out of all patients observed
signs and symptoms of thrombophlebitis in 3 shifts by number of females was (52%, n=6077), which was
infection control nurse and staff nurse till the cannula was significantly higher than males (48%, n=5609). Among
removed. Thrombophlebitis was graded using visual the total 28850 PVCs observed, phlebitis was developed
infusion phlebitis (VIP) score.5 Peripheral venous in 1821, giving the incidence of 6.3%. While no phlebitis
cannulation insertion and maintenance bundles were was seen in 27033 (93.70%) PVCs. When classified
formulated. Insertion bundles included, use of intracath according to the grades of phlebitis as per VIP score,
tray, hand hygiene, selection of vein, skin preparation 1527 (83.86%) were grade 1 phlebitis, 274 (15.04%)
with 2% chlorhexidine, aseptic non touch technique and were with grade 2 phlebitis and 20 (1.10%) were grade 3
correct sharp disposal. Maintenance bundle included phlebitis. Grade 1 was significantly more among the
daily PVC site assessment, dressing integrity checks, port phlebitis developed. The results are shown in Table 1.
disinfection, port capping, saline flushes, daily evaluation
for the continuation of cannula and hand hygiene before
The month wise distribution of the total PVCs and the
handling cannula.
phlebitis developed were calculated giving the month
wise incidence of its development. The highest incidence
Training (9.92%) was observed in the month of February, followed
by in January 9.89%, the least cases of phlebitis were
Training of staff nurses and junior doctors was conducted noted in August (3.84%) and December (3.99). The
by Microbiologist, infection control nurses and link incidence of grade I phlebitis was found to be higher
International Surgery Journal | July 2021 | Vol 8 | Issue 7 Page 2008
Tolpadi A et al. Int Surg J. 2021 Jul;8(7):2007-2011
compared to grade II and III. The distribution of all PVCs Variables N (%)
according to month and respective number of >45 5142 (44)
development of phlebitis and its grades with incidences Age (Years)
<45 6544 (56)
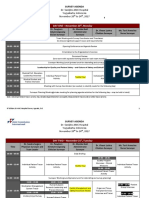
are shown in Table 2 and presented graphically in Figure
Males 5609 (48)
1. Gender
Females 6077 (52)
There was gradual reduction in grade II and grade III First 17310 (60)
Attempt of
phlebitis. In last 4 months of the study grade III phlebitis Second 10102 (35.02)
cannulation
was not seen (Table 2). Third 1438 (4.98)
Gauge 20 22587 (78.29)
Gauge of cannula
Gauge 22 4378 (15.18)
used
Gauge 24 1885 (6.83)
Hand 19906 (69%)
Location of PVC Forearm 8655 (30%)
Lower limb 289 (1%)
Duration of <72 18207 (63.11)
cannula (Hours) >72 10643 (36.89)
Medical 9304 (32.25)
Critical 6973 (24.17)
Surgical 6124 (21.23)
Location
(ward/unit) Gynecology and
3595 (12.45)
obstetrics
Pediatric 2854 (9.9)
Phlebitis Developed 1821 (6.30)
development Not developed 27029 (93.70)
Figure 1: Graphical presentation of month wise Grade 1 1527 (83.86)
incidence of phlebitis in patients underwent PVC in Grade of phlebitis Grade 2 274 (15.04)
the year 2019. Grade 3 20 (1.10)
Table 1: Characteristics of the participants.
Table 2: Month wise distribution of total PVC done, number of phlebitis occurred and its incidence.
Month Total PVC (n) Total phlebitis, n (%) Grade I Grade II Grade III
Jan 2306 228 (9.89) 176 (77.19) 48 (21.05) 4 (1.75)
Feb 2319 230 (9.92) 180 (78.26) 46 (20) 4 (1.74)
March 2250 218 (9.69) 175 (80.27) 40 (18.35) 3 (1.38)
April 3090 135 (4.37) 110 (81.48) 23 (17.04) 2 (1.48)
May 2093 126 (6.02) 112 (88.89) 12 (9.52) 2 (1.59)
June 2858 161 (5.63 131 (81.37) 28 (17.39) 2 (1.24)
July 1918 110 (5.74) 96 (87.27) 12 (10.91) 2 (1.82)
Aug 3231 124 (3.84) 104 (83.87) 19 (15.32) 1 (0.81)
Sept 1816 151 (8.31) 132 (87.42) 19 (12.58) 0 (0)
Oct 2038 117 (5.74) 105 (89.74) 12 (10.26) 0 (0)
Nov 2050 106 (5.17) 98 (92.45) 8 (7.54) 0 (0)
Dec 2881 115 (3.99) 108 (93.91) 7 (6.09) 0 (0)
Total 28850 1821 (6.30) 1527 (83.86) 274 (15.04) 20 (1.10)
DISCUSSION cost of some adverse effects like complications in this
case, which might be simple pain, or may develop into
Peripheral venous cannulation is commonly used in the severe thrombophlebitis and infections related to catheter
practice of medicine, and has revolutionized the practice infections.6
of drug administration, allowing infusion of medications,
hydration fluids, blood products and nutritional The present study was undertaken in a tertiary care
supplements.6 IV administration has almost become a teaching hospital over a period of one year to find out the
necessity in the indoor patient departments incidence and grades of thrombophlebitis in peripheral
today.1Anything which has benefits will also come at the venous cannulations. Various interventions were carried
out during this period and impact of these interventions
International Surgery Journal | July 2021 | Vol 8 | Issue 7 Page 2009
Tolpadi A et al. Int Surg J. 2021 Jul;8(7):2007-2011
on monthly incidence and grades of phlebitis were In our study as per the VIP score 1527 (83.86%) were
observed. 28850 peripheral venous cannulations were with grade I phlebitis, 274 (15.04%) with grade II
carried out on 11686 patients. Slightly higher but phlebitis and 20 (1.10 %) with grade III phlebitis. 5 Due to
significant patients were below the age of 45 years, and regular surveillance and increased awareness created
more than half of them were females. Majority of the through intense training, phlebitis was diagnosed at
cannulations were achieved in the 1stattempt, followed by earlier grades, so incidence of grade III phlebitis was very
2nd attempt and very few required 3rd attempts. The less. During the study period there was gradual reduction
commonest cannula gauge used was gauge 20, with the in grade II phlebitis (21.05% in Jan to 6.9% in
commonest location including hand, forearm and very December). Also, in the last 4 months of the study period
few in lower limbs. As a routine practice in our hospital grade III phlebitis was not reported. This was achieved
cannula was removed if not required after 72 hours, so due to continuous monitoring of cannulation site.
the duration of cannula<72 hours was significantly more Cannula was removed and resited as per VIP score
in the 63.11 % patients compared to 36.89% with>72 guidelines. With decrease in the incidence of phlebitis the
hours. significant decrease in the number of grades I, grade II
and grade III phlebitis noted from the month January to
A study from Chitwan medical college by Thapa et al December. Similar result of incidence of
reported highest incidence of phlebitis among the patients thrombophlebitis was reported by Rai et al, they also
with durations of cannula ranging between 48-72 hours.7 noted predominantly grade I phlebitis, followed by grade
According to Rai et al an average time of IV cannulation II and very few grades III.8 In a study by Saji et al out of
was 5 days, with use of 20-gauge cannula for all total 82 patients recruited 50% incidence of
patients.8 thrombophlebitis was reported.6 61% of them were with
grade 1 thrombophlebitis and remaining grade 2 was in
The present study reported phlebitis incidence of 6.3% 39% of patients without any incidence of grade 3
among 28850 PVCs observed. In the initial months thrombophlebitis, with no association of thrombophlebitis
(January, February and March) the incidence of phlebitis incidence and risk factors considered. Thapa et al
was high (9.89%,9.92% and 9.69 respectively). Due to reported the overall incidence of phlebitis to be 33.44%
increased awareness created through training sessions the and early-stage phlebitis was 88.26%.7
reporting was increased. In March venous extension of 10
cm was used in all PVCs. This minimized chances of Performing peripheral venous cannulation is an invasive
mechanical irritation and infection by taking the procedure and requires an experienced clinician or nurse,
administration site away from insertion site. Due to this local aseptic methods and knowledge of common
intervention the phlebitis rate reduced in the month of precautions that need to be taken while giving the
April and in subsequent months. Emphasis was given on therapy. Due to lack of knowledge, reasonable care and
aseptic technique during insertion. Use of intracath tray skill, thrombophlebitis has emerged as a very common
was made compulsory. Hand hygiene and use of gloves complication in hospitalized patients. The reason why
during insertion was monitored. Aseptic handling of the more lighter needs to be shed on this subject is that it
ports was implemented. Also, regular surveillance, increases the nursing cost and time, along with putting
training and sharing of phlebitis data of individual wards the patient’s safety at risk.4
in the monthly meetings contributed towards achieving
reduction in the phlebitis at the end of the study period. Limitations
Purushothaman et al analyzed the data of
thrombophlebitis before and after the training of the We could not compare all the risk factors between
nursing staff over the period of 4 years.9 They also phlebitis and non-phlebitis group. Further study is needed
reported significant reduction in numbers of in this regard to highlight risk factors.
thrombophlebitis in the post training period.
CONCLUSION
Similar reduction in phlebitis rate was noted by Sriupaya
et al in 2014.10 They observed reduction in phlebitis from Regular surveillance of phlebitis helps in planning
0.6% to 0.02%. They could achieve this with interventions to reduce phlebitis due to peripheral venous
implementation of hand hygiene and dressing integrity cannulation. Knowledge about the anatomy of venous
checks, while Yagnik et al in 2017 achieved reduction structure, diagnosis as per visual Infusion Phlebitis score
from 3.7% phlebitis in pre intervention to 0% in post and early diagnosis of phlebitis is crucial to reduce its
intervention phase.11 They stressed on documentation incidence in patients undergoing peripheral venous
during insertion and aseptic non-touch technique during cannulations.
insertion. Duncan et al in 2018 could achieve reduction in
phlebitis rate from 8% to 2%.12 Few of their bundle Regular training of the staff and doctors involved in
components were-PIVC site assessment, alcohol caps and peripheral cannulation should be an integral part of
minimization of tubing disconnect. infection control activities.
International Surgery Journal | July 2021 | Vol 8 | Issue 7 Page 2010
Tolpadi A et al. Int Surg J. 2021 Jul;8(7):2007-2011
ACKNOWLEDGEMENTS Catheter Related Phlebitis among Patients at a
Teaching Hospital, Chitwan. Int J Sci Res.
The authors would like to thank the Medical Director for 2019;8(4):1019-24.
constant support and encouragement throughout the 8. Rai P, Thati V, Ghag G, Nandu V. Post-injection
duration of this study. thrombophlebitis in patients undergoing peripheral
IV catheterization in a tertiary care hospital:
Funding: No funding sources incidence and risk factors. Int J Sci Rep.
Conflict of interest: None declared 2020;6(4):154-62.
Ethical approval: The study was approved by the 9. Purushothaman S, Patel KP, Dalal DN, Carwal TN,
Institutional Ethics Committee Gawali VP. Impact of rigorous nursing training and
reinforcement on incidence of thrombophlebitis at
REFERENCES tertiary care centre. Int J Adv Med. 2020;7:1260-3.
10. Sriupayo A, Inta N, Boonkongrat S, Kaphan K,
1. Sharifi J, Ghavami F, Nowrouzi Z, Fouladvand B, Uttama J, Budsabongphiwan S et al. Effectiveness of
Malek M, Rezaeian M et al. Oral versus intravenous peripheral vascular catheter care bundle in the
rehydration therapy in severe gastroenteritis. Arch pediatric nursing service, Chiang Mai university
Dis Child. 1985;60:856-60. hospital, Thailand. Chiang Mai Med J.
2. Oliveria AS, Parreira PM. Nursing intervention and 2014;53(2):63-73.
peripheral venous catheter related phlebitis. Systemic 11. Yagnik L, Graves A, Thong K. Plastic in patient
literature review. Referencia: Scientific J Health Sci study: prospective audit of adherence to peripheral
Res Unit: Nursing. 2010;3(2):137-47. intravenous cannula monitoring and documentation
3. Tagalakis V, Kahn S, Libman M, Blostein M. The guidelines, with the aim of reducing future rates of
epidemiology of peripheral vein infusion intravenous cannula-related complications. Am J
thrombophlebitis: A critical review. Am J Med. Infect Control. 2017;45(1):34-8.
2002;113:146-51. 12. Duncan M, Warden P, Bernatchez SF, Morse D. A
4. Saji J, KorulaSV, Mathew A, Mohan L. Peripheral bundled approach to decrease the rate of primary
Intravenous Cannula in Post-Operative Patients a bloodstream infections related to peripheral
Prospective Observational Study. J Dental Med Sci. intravenous catheters. J Assoc Vasc Access.
2015;14(6(I)):1-4. 2018;23(1):15-22.
5. Jackson A. Infection control: a battle in vein infusion
phlebitis. Nursing Times. 1998; 94(4):68-71.
6. Singh S, Gupta A, Handa P, Aggarwal N, Gupta S, Cite this article as: Tolpadi A, Mane A, Modak M,
Kalyani VC et al. Peripheral venous cannulation Verma AK, Ambekar V, Shilawat T. Impact of
associated thrombophlebitis and its management. Eur interventions on the incidence of thrombophlebitis in
J Med Health Sci. 2020;2(3):1-3. peripheral venous cannulation in a tertiary care
7. Thapa B, Rajbanshi L, Dhungana GP, Dahal BD. teaching hospital. Int Surg J 2021;8:2007-11.
Contributing Factors of Peripheral Intravenous
International Surgery Journal | July 2021 | Vol 8 | Issue 7 Page 2011
You might also like
- 484 Qi Project ClabsiDocument13 pages484 Qi Project Clabsiapi-338133673No ratings yet
- HB 260-2003 Hospital Acquired Infections - Engineering Down The RiskDocument10 pagesHB 260-2003 Hospital Acquired Infections - Engineering Down The RiskSAI Global - APACNo ratings yet
- Outline Prog NoteDocument3 pagesOutline Prog NoteSetya Gon FreccssNo ratings yet
- Assessing and Managing IntravenousDocument22 pagesAssessing and Managing Intravenousirshad ahmedNo ratings yet
- البحث السادس PDFDocument32 pagesالبحث السادس PDFايمان عمرانNo ratings yet
- Inter Plebitis 1Document25 pagesInter Plebitis 1Bella FebriantiNo ratings yet
- Contributing Factors in Increasing Health Care Associated Infection (Hai's) in Phlebitis CasesDocument8 pagesContributing Factors in Increasing Health Care Associated Infection (Hai's) in Phlebitis CasesJenny MaulidyaNo ratings yet
- NigerJClinPract217827-2343919 063039Document5 pagesNigerJClinPract217827-2343919 063039dkprsmdr.yapNo ratings yet
- The Incidence of Peripheral IntravenousDocument5 pagesThe Incidence of Peripheral IntravenousAlvin Josh CalingayanNo ratings yet
- Knowledge and Practice Towards Care and MaintenancDocument7 pagesKnowledge and Practice Towards Care and MaintenancyunishaNo ratings yet
- Positive Effect of Care Bundles On Patients With Central Venous Catheter Insertions at A Tertiary Hospital in Beijing, ChinaDocument10 pagesPositive Effect of Care Bundles On Patients With Central Venous Catheter Insertions at A Tertiary Hospital in Beijing, ChinaElfina NataliaNo ratings yet
- science: Auditing Urinary Catheter CareDocument7 pagesscience: Auditing Urinary Catheter CareNissa ErLinaNo ratings yet
- Assessment of Risk Factors of Phlebitis Amongst PDFDocument9 pagesAssessment of Risk Factors of Phlebitis Amongst PDFwindysandyNo ratings yet
- Ebp UtiDocument7 pagesEbp Utiapi-234511817No ratings yet
- Jurnal 10Document14 pagesJurnal 10adika negaraNo ratings yet
- 13-2 Collated 3 (3) - 149-155Document7 pages13-2 Collated 3 (3) - 149-155Inas AzharNo ratings yet
- Assess The Practice of Aseptic Techniques On Starting A Peripheral Intravenous Cannula by Staff Nurses at Tertiary Teaching Hospital PuducherryDocument6 pagesAssess The Practice of Aseptic Techniques On Starting A Peripheral Intravenous Cannula by Staff Nurses at Tertiary Teaching Hospital PuducherryMalarvizhi SureshNo ratings yet
- 50 ReferDocument6 pages50 ReferUsha DeviNo ratings yet
- Urinary CatheterDocument22 pagesUrinary Catheterايمان عمرانNo ratings yet
- Establish A Perioperative Check Forum For Peripheral Intravenous Access To Prevent The Occurrence of PhlebitisDocument7 pagesEstablish A Perioperative Check Forum For Peripheral Intravenous Access To Prevent The Occurrence of Phlebitismohamad malikul mulkiNo ratings yet
- Chiu 2015Document7 pagesChiu 2015retta tataNo ratings yet
- PlebitisDocument7 pagesPlebitisrizkidwifNo ratings yet
- Rba 0 AheadOfPrint 6036c54fa95395582f07f644Document5 pagesRba 0 AheadOfPrint 6036c54fa95395582f07f644STRMoch Hafizh AlfiansyahNo ratings yet
- Video 4 PDFDocument9 pagesVideo 4 PDFMirza RisqaNo ratings yet
- Children: Nebulizer Care and Inhalation Technique in Children With Cystic FibrosisDocument9 pagesChildren: Nebulizer Care and Inhalation Technique in Children With Cystic FibrosisyukihannaNo ratings yet
- Use of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes WorldwideDocument7 pagesUse of Short Peripheral Intravenous Catheters: Characteristics, Management, and Outcomes WorldwidemochkurniawanNo ratings yet
- Nurses Knowledge Regarding Intravenous Fluid - 2021 - International Journal ofDocument5 pagesNurses Knowledge Regarding Intravenous Fluid - 2021 - International Journal ofRonald QuezadaNo ratings yet
- Prevalence of Phlebitis Among Patients Receiving Peripheral Intravenous Therapy in A Tertiary Care Hospital in IndiaDocument6 pagesPrevalence of Phlebitis Among Patients Receiving Peripheral Intravenous Therapy in A Tertiary Care Hospital in IndiaIJAR JOURNALNo ratings yet
- Article 1Document8 pagesArticle 1Sherlaz EfhalNo ratings yet
- The Incidence of Thrombophlebitis Following The Use of Peripheral Intravenous Cannula in Post-Operative Patients A Prospective Observational StudyDocument4 pagesThe Incidence of Thrombophlebitis Following The Use of Peripheral Intravenous Cannula in Post-Operative Patients A Prospective Observational StudyIOSRjournalNo ratings yet
- Analisis Jurnal: Disusun Dalam Rangka Memenuhi Tugas Stase Keperawatan DasarDocument6 pagesAnalisis Jurnal: Disusun Dalam Rangka Memenuhi Tugas Stase Keperawatan DasarNur FitriNo ratings yet
- Jurnal Uro 2Document8 pagesJurnal Uro 2Lisa HikmawanNo ratings yet
- Infection Related Catheter Complications in Patients Undergoing Prone Positioning For Acute Respiratory Distress Syndrome: An Exposed/unexposed StudyDocument9 pagesInfection Related Catheter Complications in Patients Undergoing Prone Positioning For Acute Respiratory Distress Syndrome: An Exposed/unexposed Studyluandry medinaNo ratings yet
- Prevention of Central Venous Catheter-Related Bloodstream Infections: Is It Time To Add Simulation Training To The Prevention Bundle?Document6 pagesPrevention of Central Venous Catheter-Related Bloodstream Infections: Is It Time To Add Simulation Training To The Prevention Bundle?Jonatan ortizNo ratings yet
- Post Extubation Stridor UHL Paediatric Intensive Care GuidelineDocument6 pagesPost Extubation Stridor UHL Paediatric Intensive Care Guidelineandreea.spasenieNo ratings yet
- J Clinic Periodontology - 2023 - StieschDocument22 pagesJ Clinic Periodontology - 2023 - StieschtzulinNo ratings yet
- Jurnal Kritis ICU Bundle Vap PneumoniaDocument6 pagesJurnal Kritis ICU Bundle Vap PneumoniaAdzkia PintaNo ratings yet
- Successful Strategy To Decrease Indwelling Catheter Utilization Rates inDocument7 pagesSuccessful Strategy To Decrease Indwelling Catheter Utilization Rates inWardah Fauziah El SofwanNo ratings yet
- Predictive Value of The Negative Inspiratory ForceDocument8 pagesPredictive Value of The Negative Inspiratory ForceTam HmNo ratings yet
- 6887 25815 1 PB PDFDocument7 pages6887 25815 1 PB PDFmochkurniawanNo ratings yet
- The Risk Factors of Phlebitis in The Installation of Intravent CatalystsDocument13 pagesThe Risk Factors of Phlebitis in The Installation of Intravent CatalystsvanesaNo ratings yet
- Running Head: Research Proposal 1Document24 pagesRunning Head: Research Proposal 1Hogan ObiNo ratings yet
- Shaffer2017-Tutku MacBook ProDocument6 pagesShaffer2017-Tutku MacBook ProMEKSELINA KALENDERNo ratings yet
- Vanc Article 5BTDocument7 pagesVanc Article 5BTLeslie AdamsNo ratings yet
- Antibiotics 10 00608Document10 pagesAntibiotics 10 00608Marketable StudioNo ratings yet
- Prevent BsaiDocument8 pagesPrevent BsaiSaifuddinNo ratings yet
- Hasan 2020Document6 pagesHasan 2020Ananth BalakrishnanNo ratings yet
- 30-Article Text-43-1-10-20190213Document10 pages30-Article Text-43-1-10-20190213Miz UuzNo ratings yet
- Impact Vap Bundle 2017Document6 pagesImpact Vap Bundle 2017Elisya KharuniawatiNo ratings yet
- O-JPAM Vol 13 Issue1 P 591-597 PDFDocument7 pagesO-JPAM Vol 13 Issue1 P 591-597 PDFMarcela Rios HernandezNo ratings yet
- Factors Contributing To Phlebitis Among Adult Patients Admitted in The Medical-Surgical Units of A Central Hospital in Harare, ZimbabweDocument7 pagesFactors Contributing To Phlebitis Among Adult Patients Admitted in The Medical-Surgical Units of A Central Hospital in Harare, Zimbabweretta tataNo ratings yet
- ASGE Infection Control During GI EndosDocument10 pagesASGE Infection Control During GI Endosmonir61No ratings yet
- Artículo InteresanteDocument8 pagesArtículo InteresanteadaloraNo ratings yet
- JCM 11 04997Document11 pagesJCM 11 04997Omran AzzamNo ratings yet
- International Journal of Health Sciences and ResearchDocument4 pagesInternational Journal of Health Sciences and Researchwound and ostomy careNo ratings yet
- Journal Pone 0185369Document11 pagesJournal Pone 0185369madilaNo ratings yet
- Telemonitoringin Cystic Fibrosis A4 Year Assessmentand Simulationforthe Next 6 YearsDocument10 pagesTelemonitoringin Cystic Fibrosis A4 Year Assessmentand Simulationforthe Next 6 Yearsk.durantoislamNo ratings yet
- Effect of Educational Program On Nurses' Practice Regarding Care of Adult Patients With Endotracheal TubeDocument28 pagesEffect of Educational Program On Nurses' Practice Regarding Care of Adult Patients With Endotracheal TubeadultnursingspecialtyNo ratings yet
- Implementing An Evidence-Based Practice Protocol For Prevention of Catheterized Associated Urinary Tract Infections in A Progressive Care UnitDocument9 pagesImplementing An Evidence-Based Practice Protocol For Prevention of Catheterized Associated Urinary Tract Infections in A Progressive Care UnitLina Mahayaty SembiringNo ratings yet
- SJMPS 36B608 614Document7 pagesSJMPS 36B608 614Nadeeka GamageNo ratings yet
- A National Survey of The Diagnosis and Management of Suspected Ventilator-Associated PneumoniaDocument12 pagesA National Survey of The Diagnosis and Management of Suspected Ventilator-Associated PneumoniamochkurniawanNo ratings yet
- Interventional Radiological Treatment of Renal AngiomyolipomaDocument2 pagesInterventional Radiological Treatment of Renal Angiomyolipomarajesh.shirwal382No ratings yet
- ALS Regulations - January 2016 PDFDocument8 pagesALS Regulations - January 2016 PDFAnonymous 3O0J2YYNo ratings yet
- Large Samples AssignmentDocument4 pagesLarge Samples AssignmentHunny VermaNo ratings yet
- Ayaz Ahmed C.VDocument3 pagesAyaz Ahmed C.VSaima TabbasumNo ratings yet
- OtsmDocument2 pagesOtsmjonchkNo ratings yet
- Emrgency Guidelines 3 RD EditionDocument123 pagesEmrgency Guidelines 3 RD EditionMitz MagtotoNo ratings yet
- Diane Weis Curriculum VitaeDocument8 pagesDiane Weis Curriculum Vitaeapi-363602776No ratings yet
- Aria Guidelines 2016 Revision PDFDocument9 pagesAria Guidelines 2016 Revision PDFSiska HarapanNo ratings yet
- Electrical Injury in Relation To Voltage, "No Let Go" Phenomenon, Symptoms and Perceived Safety Culture: A Survey of Swedish Male ElectriciansDocument11 pagesElectrical Injury in Relation To Voltage, "No Let Go" Phenomenon, Symptoms and Perceived Safety Culture: A Survey of Swedish Male ElectriciansYopa Riyanda PuteriNo ratings yet
- Luchie CV17 V 20Document4 pagesLuchie CV17 V 20Luchie Roa NopmatNo ratings yet
- Vadesignguide: First DraftDocument11 pagesVadesignguide: First Drafteng_waleed2008No ratings yet
- Assessment of PWD Checklist Rev 7-19-17Document2 pagesAssessment of PWD Checklist Rev 7-19-17riddhiNo ratings yet
- New York-Presbyterian Q2 2019 Financial StatementsDocument57 pagesNew York-Presbyterian Q2 2019 Financial StatementsJonathan LaMantia0% (1)
- Standards For Post Anesthesia CareDocument2 pagesStandards For Post Anesthesia Carenicolasmoreno03No ratings yet
- Time Table Test Centres of Written Test For Recruitment of Various Posts of Churachandpur Medical CollegeDocument1 pageTime Table Test Centres of Written Test For Recruitment of Various Posts of Churachandpur Medical CollegeYumkhaibam PamchaNo ratings yet
- AssessmentDocument2 pagesAssessmentPau-pau BasiNo ratings yet
- Effectiveness of Self Instructional Module (Sim) On Knowledge Regarding The Prevention of Hiv/aids Among Students Studying in Selected Degree CollegeDocument24 pagesEffectiveness of Self Instructional Module (Sim) On Knowledge Regarding The Prevention of Hiv/aids Among Students Studying in Selected Degree CollegeAnshul Nandi100% (2)
- Faye Glenn AbdellahDocument1 pageFaye Glenn AbdellahJammel DayudayNo ratings yet
- India's Healthcare SectorDocument24 pagesIndia's Healthcare SectoraNo ratings yet
- Jadwal Survey Jci 20-24 Nov 2017Document5 pagesJadwal Survey Jci 20-24 Nov 2017Erdananda HaryosuwanditoNo ratings yet
- 03 VenipuncturebySyringeDocument7 pages03 VenipuncturebySyringemaryjo ostreaNo ratings yet
- Provisional List of Colleges (M.Sc. Nursing) For Counselling Purpose Session 2019-20 Rajasthan University of Health Sciences, JaipurDocument2 pagesProvisional List of Colleges (M.Sc. Nursing) For Counselling Purpose Session 2019-20 Rajasthan University of Health Sciences, JaipurDeepshikhaNo ratings yet
- Soal Uji Coba Bahasa Inggris 2 08Document8 pagesSoal Uji Coba Bahasa Inggris 2 08Poeza Setiawan100% (1)
- JOYCE TRAVELBEE and DOROTHY JOHNSONDocument5 pagesJOYCE TRAVELBEE and DOROTHY JOHNSONRaya MesiasNo ratings yet
- Micu Case Study d1Document28 pagesMicu Case Study d1jmarc_2180% (5)
- Mental Health Care in India: Old Aspirations Renewed HopeDocument973 pagesMental Health Care in India: Old Aspirations Renewed HopeVaishnavi JayakumarNo ratings yet
- Advanced Life Support Training and Assessment PDFDocument6 pagesAdvanced Life Support Training and Assessment PDFwilmaNo ratings yet
- D An Introduction: Physical Medicine and RehabilitationDocument33 pagesD An Introduction: Physical Medicine and RehabilitationChadNo ratings yet