Professional Documents
Culture Documents
DocScanner 29 May 2024 12-08 Am
DocScanner 29 May 2024 12-08 Am
Uploaded by
Sazia Begum0 ratings0% found this document useful (0 votes)
5 views34 pagesOriginal Title
DocScanner 29 May 2024 12-08 am
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
Download as pdf
0 ratings0% found this document useful (0 votes)
5 views34 pagesDocScanner 29 May 2024 12-08 Am
DocScanner 29 May 2024 12-08 Am
Uploaded by
Sazia BegumCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
Download as pdf
You are on page 1of 34
mes.
Lae
Moot Disorders ad Suicide
CHAPTER 7
the following case.
‘A Successful “Total Failure”
Margaret, a prominent businesswoman inher ate-oties,
noted for her energy and productivity, was unexpectedly
deserted by her husband fora younger woman. Following
her inital shock and rage, she began to have uncontrol
lable weeping spells and doubts about her business acu-
men. Decision making became an ordeal. Her spirits
rapidly sank, and she began to spend more and more
| time in bed, reusing to deal with anyone. Her alcohol
© consumption increased to the point where she was sel:
dom entirely sober. Within period of weeks, she had suf-
{fered serious financial losses owing to her inability, or
| refusal, to keep her affairs in order. She felt she was a
| total filur,” even when reminded of her considerable
“personal and professional achievements; indeed, her
-selfcricism gradually spread to all aspects of her life
andher persona history. Finally, alarmed members ofher
ily essentially forced her to accept an appointment
witha clinical psychologist.
‘Was something “wrong” with Margaret, ot was she merely
‘experiencing normal human emotions because of her hus-
band’s deserting her? The psychologist concluded that she
‘was suffering from a serious mood disorder and initiated
treatment. The diagnosis, based on the severity of the
symptoms and the degree of impairment, was. major
‘depressive disorder, Secondarily, she had also developed a
serious drinking problem—a condition that frequently co-
‘occurs with major depressive disorder.
exam, not getting into o,,
palling 2 o
seo ine NE yp th 9 ang
it depress rate school, ane 28 depressed Mood in man |
1 of us 8 :
ert enoice of colle that severe alterations in my
i a involv isturbances
ner are all ext igorders IV ch cases the disturbane of moog a]
people. However ‘ time, In UCT PT Gaptive, and often lead tose,
and for much Ln 5 cleat mace. In facts it as been ex
‘ istent e ;
intense and persistent ak peerage eal ond
gus problems in rlatlONST | ranked aMMOnE orld except Africa, and it vag
mated that 2000 OEP in all ats OF eg States, FMRI abOvE hag
terms of years lost R health condition in the roe Preease-burden” of depres
the numberone such Healt) <1" vera the rreatment 2 nding
direct costs ture deaths) —totalleg
fase and stroke (Ustll
: is, the total ee
‘ciety—that i, the and P
esha mised oe disap yr eo percent ofthe reported cos
: lone, :
$83.1 billion in ee Smonkplace (Greenbers, Kessler et al» 2003). Consider
resulting from problet
erse in nature, asisillustrated by
e gnized in the DSM-IV-TR
semanytypesof depression recognized int
thor we wll discus Nevertheless, int all mood disorders
ive disorders), extremes of emotion
v merly called affective disorders), extrem
ie ition or deep depression—dominate
cor affect soaring el
of Uisieal picture, other symptoms are also present, but
the abnormal mapd is the defining feature.
Wuat ARE Moop
DISORDERS?
“The two key moods involved in mood disorders are mania,
often characterized by intense and unrealistic feelings of
excitement and euphoria, and depression, which usually
involves feelings of extraordinary sadness and dejection.
Some people experience both of these kinds of moods at
‘one time or another, but other people experience only the
depression. These mood states are often conceived to beat
opposite ends of mood continuum, with normal mood
in the middle. although this concept is accurate t0 ¢
eres, sometimes patient may have symptoms pf manit
sed orion during the same time period (In thes
le cases, the person experiences rapidly altet~
‘aUingmoodssuchassadness, cuporia, and eabiy al
ren gime ead floes
the el ist discuss the unipolar disorders, in which
wwe wil diane ences only depressive episodes, and thet
xpress Cat bipolar disorders, in which the pero®
tinction is saaine ic and depressive episodes. This dis
tnpolerarereminent in DSM-1V-TR, and although the
holy co POL forms of mood disorder may not be
arate and distinct, there are notable difference
‘Mood disorders are div
cors,and treatm
~ yoms caus
flerentiate amor
rents. As
. “n Weill see,
iat costomiry te ng the mood ‘ior,
Perms OY Severin A tans
j ies the rau dete of impairment evi.
Fhose areas and DY duration —whether thea,
4 esa clonic, of intermittent (with periods ot
BE oral functioning between the episodes of
| ei
080 ted, diagnosing unipolar or bipolar disorder
Jefe diagnosing what kind of mood episode the
ints with. The most common form of mood {
se Fiat people present with is a major depressi
le pressive
ge Pe dealed in the DSM-IV-TR table, Criteris for
Fypressive Episode, to receive this diagnosis, the
sfineest in pleasurable activities) for most of every
od for most days for at least 2 weeks. In addition, he
must show at least three or four other symptoms
ijt of five) that range from cognitive symptoms
(issteings of worthlessness or guilt and thoughts of
Gate to behavioral symptoms (such as fatigue or phy
‘agiation), to physical symptoms (such as changes in
setteand sleep patterns).
‘The other primary kind of mood episode is a manic
aiode, in which the person shows markedly elevated;
phair expansive mood, often interrupted by occa-
ged outbursts of intense irritability or even violence—
pialarly when others refuse to go along with the
‘atic person’s wishes and schemes. These extreme
sods ust persist for at least a week for this diagnosis to
txmale In addition, three or more additional symptoms
tzatoccurin the same time period, ranging from behav-
ial symptoms (such as a notable increase in goal-
Sxcted activity, often involving loosening of personal
‘odcaltural inhibitions as in multiple sexual, political, or
tgous activities), to mental symptoms where self-
xen becomes grossly inflated and mental activity may
sredup (uch as a “fight of ideas” or “racing thoughts”),
“»physical symptoms (such as a decreased need for sleep,
‘ythomotor agitation). (See the DSM-IV-TR table, Ci
‘ti fora Manic Episode on p. 228.)
Research suggests that mild mood disturbances are on
‘ame continuum as the more severe disorders. That is,
dferences seem to be chiefly of degree, not of kind, a
ion supported in several large studies examining
yt 8Kendler & Gardner, 1998; Ruscio & Ruscio,
However, there is also considerable heterogeneity in
sit it which the mood disorders manifest them-
yattthere are multiple different subtypes of both
i and bipolar disorders, and somewhat different
Nelyeand treatments are important for different
.
sg important to remember that suicide is a di
Sey) feguent outcome (and always a potential out,
Sue Bhificant depressions, both unipolar and
fact, as discussed in the latter part of this chap-
MS
ptf be markedly depressed (or show a marked fof
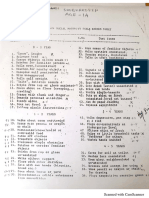
Criteria for Major Depressive Episode
A. Five (or more) ofthe fllowing symptoms have been
present dung the same 2-veek period and represent @
Change from previous functioning: atleast one of the
Symptoms is either 1) depressed mood or 2) loss of
les interest or pleasure.
WS SEiessed most of the day, nearly every day. as
Cis eo indented by ether subjective reports or observation
P29 made by thers,
(2) Markedly diminished interest or pleasure in all, or
almost al, activities most ofthe day, nearly every day.
(3) Significant weight loss (when not dieting) or weight
sain.
(@) Insomnia or hypersomnia nearly every day.
(5) Psychomotor agitation or retardation nearly every day.
(@ Fatigue or loss of energy nearly every day.
(7) Feelings of worthlessness or excessive or
guilt nearly every day.
shed ability to think or concentrate, oF
iveness, nearly every day.
(9) Recurrent thoughts of death or suicide, or recurrent
suicidal ideation without a plan, ora suicide attempt
or plan.
B. The symptoms do not meet criteria for a Mixed Episode,
C. The symptoms cause clinically significant distress or
impairment.
ter, depressive episodes are clearly the most common of the
predisposing causes leading to suicide.
The Prevalence of Mood Disorders
Major mood disorders occur with alarming frequency—at
least 15 to 20 times more frequently than schizophrenia,
for example, and at almost the same rate as all the anxiety
disorders taken together. Of the two types of serious mood
disorders, unipolar major depression is much more com-
mon, and its occurrence has apparently increased in recent
decades (Kaelber, Moul, & Farmer, 1995; Kessler, Berglund,
et al, 2003). The most recent epidemiological results from
the National Comorbidity Survey-Replication study found
lifetime prevalence rates of unipolar major depression at
nearly 17 percent (12-month prevalence rates were nearly
7 percent) (Kessler, Chiu, et al, 2005), Moreover, rates for
unipolar depression are always much higher for women
than for men (tisually about 2:1), similar to the sex differ.
ences for most anxiety disorders (see Chapter 6). The issue
of sex differences in unipolar depression will be discussed
ppropriate
Dysthymic Disorder
The point at which mood disturbance becomes a diagnos”
able mood disorder is a matter of clinical judgment and
usually concerns the degree of impairment in functioning
that the individual experiences. Dysthymic disorder is
considered to be of mild to moderate intensity, but its pri-
mary hallmark is its chronicity. To qualify for a diagnosis
of dysthymic disorder (or dysthymia), a person must have
a persistently depressed mood most of the day, for more
days than not, for at least 2 years (1 year for children and
adolescents). In addition, individuals with dysthymic dis-
order must have at least two of six additional symptoms
when depressed (see the DSM-IV-TR table, Criteria for
Dysthymic Disorder). Periods of normal mood may occur
briefly, but they usually last for only a few days to a few
weeks (and for a maximum of 2 months). These intermit-
tently normal moods are one of the most important char-
acteristics distinguishing dysthymic disorder from major
depressive disorder.
Dysthymia is also quite common, with a lifetime
prevalence estimated between 2.5 and 6 percent (Kessler
et al., 2005),
erglunds ne The aver
5 years, but it can persist gee
1, 1997) Chronic stress hash,
y of symptoms overa 7.5,
yx Klein, & Davila, 2004), Rd
n
cover from dysthymia wig
apse within an average of a,
h
half may Fel :
eat Swartz, Rose, & Leader, 2000), San
+ the teenage YeATS AME OVET 50 perce
before age 21-
g case is typi
1 of this disorder,
a as,yearold junior executive. ...complained of being
gepressed” about everyting: her job, her husband, and
her prospects forthe future...-Her complaints were of
vorsistent feelings of depressed mood, inferiority, and
pessimism, which she claims to have had since she was
fe or 27 years old. Although she did reasonably well in
‘college, she constantly ruminated about those students
‘who were “genuinely intelligent.” She dated during col-
lege and graduate school but claimed that she would
never go after a guy she thought was “special,” always
feeling inferior and intimidated...
Just after graduation, she had married the man she
‘was going out with at the time. She thought of him as rea-
sonably desirable, though not “special,” and married him
primarily because she felt she “needed a husband” for
‘companionship. Shortly after their marriage, the couple
started to bicker, She was very critical of his clothes, his
job, and his parents; and he, in turn, found her rejecting,
controlling, and moody. She began to feel that she had
made a mistake in marrying him.
Mes) she has also been having difficulties at
work She i assigned the most menial tasks atthe firm
Pecans Been sient importance
spore: She sis that she frequently does #
is required, an aA iat is given her, never does more en
ae tndmever demonstrates any assertiveness
her protesonne, 2 that she will never go very sary
nection oy acusese des not have the right "em
- otmoney cee tes does her husband, yet she dreams
band inohes eee Powe Her soil with her his
aoe Seater coupes, The man in te
ihe women yg ie of her husband. She i. sul
ath he peo oe interesting and urimpres
better offthan cae tne Seem 10 lke her are prob
Under the bur Ei ,
marriage, ee of her dissatisfaction with Nef
uninterested) ey on Ner Social life, feeling tired 2
fe" she now enters treatment for "
thi ti tie
me. (Spitzer eta, 2002, pp. sie)
1
i
;
|
| Sous of death or suc,
Major Depressive Disorder
The disgnostic criteria for major depressive disorder
esquire that the person exhibit more symptoms than are
ssquired for dysthymia and that the symptoms be more
sistent (not interwoven with periods of normal
rood). To receive a diagnosis of major depressive disoe-
éezaperson must be in a major depressive episode (initial
or single, or recurrent). An affected person must experi-
ace either markedly depressed moods or marked loss of
intrest in pleasurable activities most of every day, nearly
every day, for at least 2 consecutive weeks. In addition to
‘Saving one or both of these symptoms, the person must.
caperience at least three or four additional symptoms
daring the same period (for a total of at least five symp-
toms), as detailed in the DSM-IV-TR table, Criteria for
Major Depressive Episode. These symptoms include cog-
aitive symptoms (such as feelings of worthlessness or
gilt, and thoughts of suicide), behavioral symptoms
(uch as fatigue, or physical agitation), and physical
symptoms (such as changes in appetite and sleep pat-
terns).
Itshould be noted that few if any depressions—includ-
ingmilder ones—occur in the absence of significant ans
ty (¢g,, Akiskal, 1997; Merikangus et al., 2003; Mineka
al, 1998). Indeed, there is a high degree of overlap
seen measures of depressive and anxious symptoms in
‘eseports and in clinician ratings. At the diagnostic le
thee are very high levels of comorbidity between moo
‘8d anxiety disorders. As discussed later in this chapter
(ee Developments in Thinking 7.2 on p. 250), the issues
Ssttounding the co-occurrence of depression and anxiety,
‘hich have received a great deal of attention in recent years,
“every complex.
The following account illustrates a
f major depressive disorder.
moderately severe
Connie
Connie, a 33-year-old homemaker and mother of a 4-year-
old son, Robert, is referred ...to a psychiatric outpatient
rogram because ... she has been depressed and unable
to concentrate ever since she separated from her hus-
band 3 months previously. Connie left her husband, Don-
ald, after a 5-year marriage. Violent arguments between
them, during which Connie was beaten by her husband,
hhad occurred for the last 4 years oftheir marriage, begin:
when she became pregnant with Robert. There were
daily arguments during which Donald hit her hard enough
to leave bruises on her face and arms.
Before her marriage... she was close to her parents
{and} had many friends whom she also saw regularly...
Inhigh school she had been a popular cheerleader and a
‘good student, ... She had no personal history of depres-
sion and there was no family history of ... mental illness.
During the first year of marriage, Donald became
increasingly irritable and critical of Connie. He began to
request that Connie stop calling and seeing her friends
after work, and refused to allow them or his in-laws to visit
their apartment... Despite her misgivings about Donald's
behavior toward her, Connie decided to become preg-
nant. During the seventh month of the pregnancy...
Donald began complaining [and] began hitting her with
his fists. She left him and went to live with her parents for
a week. He expressed remorse....and...Connie returned
to her apartment. No further violence occurred until after
Robert's birth. At that time, Donald began using cocaine
every weekend and often became violent when he was
high.
In the 3 months since she left Donald, Connie has
become increasingly depressed. Her appetite has been
poor and she has lost 10 pounds. She cries alot and often
Wakes up at 5:00 Am. and is unable to get back to
(continued)
CHAP TEN 7 Mor tvanders and Suiile
Connie pale and thin... the speaks slowly,
i Her depressed mood and lack of enerBy. She.
‘/6 thal her only pleasure 1 In belng wth er son She
‘able to Lake care of him phystcally, but feels gully because
her preoccupation with hier own bad feelings prevents Her
{fom belng able to play with him, She now has no contacts
‘other than ith ho parents anderson he fols woth
les dnd blames hereel for her marital problems say
that if she had been a better wile, maybe Donald would
have been able (0 give up the cocalne,. (adapted fromm
Spl et al 300 9p, 414-43)
Note that Connie’ case nicely illustrates that perso
With major depresive disnrder shows not only mod
tymptoms of sade hut alo a variety of symptoms that
tre mote severe than in milder forms of depression, Cone
tle shows vars cognitive dlstonthons, including feeling
‘worthless and yuity. She complains ofa ack of energy anid
inability 1 play with her child, Her biological eymptoms
ippetite and
twill friends ko occurs commonly with
depression, i part becaue the person is unmotivated to
eck contact, Connie's cave aleo nicely ilusrates the mull
pplecompler Interacting factors that may be involved in the
tology of depression, Althouglt Connie did not have «
personal or a family history of depression, the experiences
from 5 years ofa very difficult mariage with a violent and
abusive husband were suliclent to finally precipitate her
major depression,
DEPRESSION THROUGHOUT THE LIFECYCLE Altho
he onset of unipolar mood disorder mut often oc
during, late adolewence up to middle wut
reactions may begin at any tine fron eatlycikdhoend to
Cold age, Depression was once thought not to vceur jn
dhildhood, hut more recent revearch hae found snajor
depressions in presdolewent children, and iti etinated
‘that about 2.0 4 percent of chuol-age children mect the
criteria for sone form of unipolar diorder, with perhaps
fanother 2 percent exhibiting chaonic mild depression (see
Garber 6 Horawits, 2002), ven infants may experience »
form of depression (commun knnwn as unaclitie depres
‘on or despait) if they ate separated for a prolonged
period from thelr attachient figure (usually thelr mother,
Havaloy, 1973, 19805 Speer eta, 1),
“rhe incidence of depression vies sharply during a
Jewence-# period of great tunnel for many people,
Sneed, ane review estimated that approximately 15 020
percent of adolescents experience nisior depresive dlsor-
der at some point ducting their wdotesrnt years (Lewine
“sohin 6 Vaan, 2002), nnd the wveraye ayy onset for
ws been decreas
solescenn depresion has Dee surg
pare Mea thevineon eta 1993 Speier ea, Pa
‘ perind that gx differences jy hk
fs during this tlie p
rye (Wankin& Abram, 4
depression first emerne mn, ay
qed ce, 20: Nolen Hore Gig
jn esearch 71 on p. 244) the
jor depressive divorder in adgte
eimat at eat hough youn. aduliond when yu
duals sow small but siicant psychoses jpe
rare in many donna, including helt Occupation
their interpersonal relationships, and ther general gyi."
Uf life (eqhe Vewinsohn, Hobe, et aly 2003), Seg!
Chapter 1)
ve occurrence of major Aepresion cantina,
Interlife,Ahough the I-year prevalence of major dep,
inlay ven ple we se
uner adults (Kessler etal 2003), major depression
pyar als are stil considered majong
Hic heath problenm today (Beekman, Deeg, etal, 2
Moree, esearch suggests hat rates of depression ag,
plyically ill residents of nursing homes or residential ae
facltes are substantially higher than among older adel,
living at home (see Powers et al 2002). Unfortu,
depression in ater life can be difficult wo diagnose becase
many of the symptoms averlap with those of veveral ma
ical nese anu dementia (Alexopoulos eta, 200) att
is very important to try and diagnose it elibly breve
depression in later life has many adverse consequences
8 person's health, including doubling the vsk of dah io
people who have had a heart attack or stoke (Suk
et a, 2002) (wee Chapter 10),
(ee Developmen
ter effects of 3
SPECIFIERS FOR Majon DEPRESSION Some ink
uals who meet the basic criteria for diagnosis of major
depreion an have adiional patterns of symptoms
features that are important to note when making dig”
sisbecause they have implications for understanding =
ahout the course of the disorder and/or its most effect
treatment, They: different patterns of symptoms off
tures are called specifiers in DSM-1V-TR. One such spe
fier is major depressiveepivode with melancholic featur
Thi designation sapped wen, in dition to meld
the criteria for major depression a patient either bas
interest or pleasure in almost all activities ar does not 4
10 usually pleasurable stimuli or desired events. In #4
tion, the patient must experience at least three of the
Sing early moringamaenings (2) depression
srs in the maming, (3) marked payhomotr =
tomato, spicata appetite a 2
(5) inapproprinte on excesive gui, and (6) 6
ited ‘ is qualitatively different from the sadnes
tlenced during a nonmelancholic depression. This
subtype of depression nasa wih a higher
Joading than other forms of depression (Kendler, 7"
}
atc ymptoms, characterized by loss of contac
ay and dslsions (Ge bei) or hllcintions
sits? erEELION) ay sometimes accompany
Srptoms of major depression. In such cares eh,
srg the diagnosis that is noted is neve
settee episode with psychotic features 0,
drresiions oF hallucinations present ar
ent-—that is they seem in some sense “appro
ne aris depression because the conten ier
oe, sch a8 themes of personal inadequacy cu
fred punishment, death, and disease. For example,
$etutisional idea that one’s internal organs have totally
forted—an idea sometimes held. by severly
ed people—ties in with the mood ofa despondiont
Feelings of worthlessness and guilt areakeo carne
apart of the clinical picture (Ohayon &e Shatrberg
Sha). Psychtically depressed individuals are likely
tne a pooret long-term prognosis than nonpsychotie
Spresives (Coryell, 1997), and any recurrent episodes
salikelyto be characterized by psychotic syreptome
ing et al, 2004). Treatment generally involves an
(psychotic medication as well as an antidepressant In
Ferre cass, psychotic depression occurs in the context
Mpospartum depression (Miller, 2002), where mothers
{uy Hl their babies because of the hallucinations or
{sions they have
‘Athird important specifier is used when the individ-
aul shows “atypical fentures” Major depressive episode
with aypical features includes a pattern of symptoms
Guacerized by mood reactvitys that is, the person's
‘ood brightens in response to potential positive evens. In
tition, the person must shove two or more of the follow
ificant weight gain or increase
(sleeping too much),
{leaden paralysis (heavy feelings in arms or legs), and
(#)along-standing pattern of being acutcly sensitive to
re major
edinarily,
fe mood-
int
fie
noe
weight, excessive gt
symptoms: wei
Characteristic Symptoms
‘Three of the following: Early morning awakening, depression worse in the
‘morning, marked psychomotor agitation or retardation, loss of appetite or
qualitatively different depressed mood.
Delusions or hallucinations (usually mood-congruent); feelings of guilt and
‘worthlessness common.
“Mood reactvity—brightens to positive events; 190 ofthe four following
1 gain or increase in appetite, hypersomnia, leaden paralysis,
being acutely sensitive t
Atleast two or more episodes in past2years that have ocurred at the sme ime
(usually fall or winter), and full remission at the same time (usually spring)
other nonseasonal episodes in same 2-year period. ie
Unipolar Mood Dieanders
nber of
imerpersonal rejection. & disproportionate number if
individuals who have atypical features are fernabes,
have an earlier-than-average age of onset and who are
more likely to show suicidal thoughts (Matra, Revicki
Davidson, & Stewart, 2003). This is also an important
specifier because there are indications that individuals
th atypical features may preferentially respond to a dif-
ferent class of antidepressants—the monoamine oxidave
inhibitors—than do most other depressed individuals, See
‘Table 7.1 fora summary of the major specifiers.
Although not recognized as an official specifier itis
not uncommon that major depression may coexist with
dysthymia in some people, a condition given the designa-
tion double depression (Holand & Keller, 2002; Keller,
Hirschfeld, & Hanks, 1997). People with double depression
are moderately depressed on a chronic basis (meeting,
symptom criteria for dysthymia) but undergo increaved
problems from time to time, during which they also mest
ria for a major depressive episode. Among, clinical
‘samples of people with dysthymia, the experience of dou-
ble depression appears to be common, although it may be
much less common in people with dysthymic disorder
who never seek treatment (Axiskal, 1997). For example,
one clinical sample of nearly 100 individuals with early
onset dysthymia (onset before age 21) were followed for
5 years, during which time 77 percent experienced at least
tone major depressive episode (see also Keller et al, 1997;
Klein et al, 2000). Although nearly all individuals with
double depression appear to recover from their major
depressive episodes (at least for a while), recurrence is
‘common (Boland & Keller, 2002; Klein etal. 2000).
DEPRESSION AS A RECURRENT DISORDER When a
diagnosis of major depressive disorder is made, itis usually
also specified whether this is a first and therefore single
terpersonal rejection.
~ a
CHAPTER 7 Mond Disonlersand Suicide
(initial) episode or a recurrent episode (preceded
by one or more previous episodes). This reflects the
fact that depressive episodes are usualy tive-lim=
iteds according to DSM-IV-TR, the average dura
tion of an untreated episode is about 6 months. In
2 large untreated sample of depressed women, cer
tain predictors pointed to a longer time to spon!
Reous remission of symptoms: having financial
iffculties, severe stressful life events, and high
‘genetic risk (Kendler, Walters, & Kessler, 1997). In
some cases major depression does not remit for
‘over 2 years, in which case chronic ‘major depres-
sive disorder is diagnosed,
Although most depressive episodes remit
(which is not said to occur until symptoms have
Femitted for at east 2 months), depressive episodes
‘usually recur at some future point. In recent years,
Fecurrence has been distinguished from relapse,
‘where the latter term refers to the return ‘of symp-
toms within a fairly short period of time and prob-
ably reflects the fact that the underlying episode of
depression has not yet run its course (Boland &
toe iil rte lites or thos n he
see empha mre eto eR scsonl eft day
rich dpesson ccs rina nthe llard winter months ndten
remit in the spring or sumer months.
Keller, 2002; Frank eta, 1991), Relapse may com-
monly occur, for example, when pharmacotherapy
is terminated prematurely after symptoms have remitted
but before the underlying episode is really over (Hollon
tal, 2002a, 2002b; 2008).
The proportion of patients who will exhibit a recur-
rence of major depression is very high (about 80 percent,
according to Judd, 1997), although the time period before
a recurrence occurs is highly variable. In one very large
national study of over 400 patients across 5 sites followed
for more than a decade, 25 to 40 percent had a recurrence
within 2 years, 60 percent within 5 years, 75 percent within
10 years, and 87 percent within 15 years (Boland & Keller,
2002; Keller & Boland, 1998). There is also evidence that
the probability of recurrence increases with the number of
prior episodes.
The traditional view was that between episodes, per-
son suffering from a recurrent major mood disorder is
‘essentially normal. However, as more research data on the
course of depression became available (e.g, Coryell &
Winokur, 1992; Judd et al, 1998), it became clear this is
frequently not the case. For example, in a large 5-site study
with over 400 patients, Judd et al, (1998) found that even
patients experiencing their first episode at the time the
study began showed no symptoms at all during only 54
percent of weeks during a 12-year follow-up period, rela-
tive to only 37 percent showing no symptoms among those
experiencing a second or later episode at the start of the
study. Moreover, people with some residual symptoms,
and/or with significant psychosocial impairment, follow-
jing an episode are even more likely to have recurrences
than’ those whose symptoms remit completely (Judd,
Paulus, Zeller, eta, 1999; Solomon et al, 2004).
SEASONAL AFFECTIVE DISORDER Some people who
experience recurrent depressive episodes show a seasonal
pattern commonly known as seasonal affective disorder,
‘To meet DSM-IV-TR criteria for recurrent major depres
sion with a seasonal pattern, the person must have hat
least two episodes of depression in the past 2 years occut+
ring at the same time of the year (most common; fallor
winter) and full remission must also have occured atthe
same time of the year (most commonly, the sprin
addition, the person cannot have had other, nons
depressive episodes in the same 2-year period, and most
of the person's lifetime depressive episodes must have
been of the seasonal variety. Prevalence rates suggest that
winter seasonal affective disorder is more common in
people living at higher latitudes (northern climates) and
in younger people.
> What are the major features that differentiate
dysthymic disorder and major depressive
disorder?
_| > What are three common specifiers of major
depressive disorder?
> Distinguish between “recurrence” and
“relapse,”
causal FAcTORs IN
‘x]POLAR Moop
pisORDERS
_paderag the development of unipolar mood disor
persion bee feed onthe pole roles of bo.
So sod sociocultural factors. Although
Sie cen Bas eal Been Tied separate at
koe gee sock! be to undentand how thes fer
factors are interrelated, in onder to
3 ppopnchosocal model,
soiogical Causal Factors
pus beg bees known that a variety of diseases and drugs
EBE= mood keading somtimes to depresion and
Boo daton or even bypomania Indeed, this idea
‘Shes w Hippocrates. who hypothesized that depres.
BB ssaassed by an cxcess of “black hile" in the system
spose As we will discuss, in the past half-century
szempting to establish a biological bass for
Sree cecrdess have considered a wide range of factors.
¢
GexETKC INFLUENCES Farsi studies have shown that
Sipsuence of mood disorders is approximately three
Sather emong blood relatives of persons with clini-
Sspesed unipolar depression than in the popula-
z= = ie (eg. Sullivan, Neale, & Kendler, 2000;
"ele Scineider, & McGuifin, 2002). More importantly,
tere: i mudies, which can provide much more con-
— netic influences on 2 disorder, also,
=e. “contribution to unipolar \
‘twin: Sollivan et al (2000) did a quantitative review —
Ftestin studies (the tral numberof tins sud
‘= sazorer 21,000) and found that monozygotic co-twins
¢apei with unipolar major depression ase about tice,
Bdywadevelop majordepressionas ( 7.) —W2-/.
seEzpticco-twins Averagingacross | 7
‘eral of these studies, this review
‘sags that about 31 to 42 percent
“fe variance in lability to major
‘ration was due to genetic influ-
‘adoption method
Canal Factors in Unipolar Mot Disorders
tion studies on mood disorders published thus far, the
most adequate one (Wender etal, 1986) found that wnipe~
lar depression nccttied about seven-timesmore offen in
EBs iwesof-the severely depressed adoptees
than in the biological relatives of control adoptees (Wal-
lace et a 2002; Wender etal, 1986).
Taken together, the results from family, twin, and
adoption studies make a steongcase for amoderategenctis
sal patterns of-unipolar major,
ution as
for bipolar disorder (Farmer Eley. Met
lace etal, 2002), However, the evidence for a genetic con=
tribution is much less consistent for milder but chronic
forms of unipolar depression such as dysthymia, with
some studies finding no evidence of genetic contributions
(Roth & Mountjoy, 1997; Wallace et al, 2002), Finally
attempts tg identify specifi genes that may be responsible
for these genetic luences have not yt been success
although there are some promising leads (Plomin et aly
2001; Wallace et al, 2002).
gene involved in the trans
toni, which is one ofthe key neurotransmitters involved
in depression, There are two different kinds of versions or
alleles involwed—the short allele (5) and the tong allele (Dy
and people have two short alleles (5s), two long alleles (12),
oF onc of each (sl). Prior work with animals had suggested
that having ssalleles might predispose to depression rela~
tive to having alleles, but human work on this iste had
provided mixed results. In 2003, Caspi, Sugden, Mofit,
and colleagues published a landmark study in which they
tested for the possibilty ofa gene-environn
involving this erotonin-transporter gene (see Chapter 3).
‘They used 847 people in New Zealand who had been fol-
lowed fom birth until 26 years of age, at which time the
researchers assessed diagnoses of major depression in the
past year, and the occurrence of stressful life events in the
previous 5 years. Their results were very
Hiking: fadviduals who possesed the
ssalleles Were twice as likely to develop
lepression following four ér more stress-
ful life events in the past 5 years as those
Who possessed the Ilalleles and had four
interaction
‘=e The estimate was even higher for
‘bac serere, recurrent depressions.
‘Scubly however, the same review con-
ued that even more variance in the
‘SSiey to major depression is due to
‘
interact with other disturbed hormonal and nexroptrs
logical patterns and biological ripthms (2. Gaiow
Nemeroff, 2003).An interesting new focus of some o>
Fewearch is on understanding how interactocs <=
these different neurobiological stems ax EOE
resilience in the face of major stress (a very comico
Gipitant for depreuion}, which in num may bee Fo
why only a suet of people undersoing mice
depression (Southwick et al 2005).
MAUTIES OF HORMONAL REGULAT:
hormonal causes or correlates of some for
rater i ss a
10044 aly 2002). The tnajority of attention has bec,
jon the ypothalamic-pituitary-adrenal (HPA) aie
‘p particular on the hormone which is
2% gel bythe outermost portion ofthe adrenal glands
aig regulated through 9 complex feedback loop (ace
we! in Chapter 3 68 Howland & Thase, 1990). As
Fie yedin Chapters 3,5,and 6 the human stress response
Sociated with clevated activity of the HDA axis, which
ly controlled by horepinephrine and serotonin. The
n of stress or threat can lead to norepinephrine
re :
ity inthe hypothalamus, causing the release of conte
Sossamon CRE fo thel poe
Srvbich in turn triggers release of adrenocorticatrophie
pomane (ACTH) from the pituitary. The ACTH then typ=
JAllrtravels through the blood to the adrenal cortex of the.»
‘areal gands where etal is released. Blood plasiita
els of cortisol are known to be elevated in som to 40 ~
Fit of severely depressed hospitalized patients (Thase
al, 2002). Sustained elevations in cortisol can result
from increased CRH activation (for example, during sus-
no8!
i
isp
‘Causal Factors in Unipolar Mood Disorders
tained stress or threat), increased secretion of ACTH, oF
the failure of feedback mechanisms. See Figure 7.2.
‘One line of evidence that implicates the failure of
feedback mechanisms in some depressed patients comes
from robust findings that in about 45 percent of seriously
depressed patients, a potent suppressor of plasma cortisol
in normal individuals, dexamethasone, either fails entirely
to suppress cortisol or fails to sustain its suppression
(Thase et al., 2002). This means that the HPA axis is not
‘operating properly in these “dexamethasone nonsuppres-
sors” It was initially thought that DST nonsuppressor
Patients constituted a distinct subgroup of people with
severe or melancholic depression (Holsboer, 1992). How-
ever, subsequent research showed that several other groups
of psychiatric patients, such as those with panic disorder,
also exhibit high rates of nonsuppression. This suggests
that nonsuppression may merely be a nonspecific indica-
tor of generalized mental distress.
Recent findings have revealed that depressed patients
with elevated cortisol also tend to show memory impair-
‘ments and problems with abstract thinking and complex
problem solving (Belanoff et al., 2001). Some of these
cognitive problems may be related to other findings
showing that prolonged elevations in cortisol such as seen
in moderate to severe depression result in cell death in the
Patient with Major Depression
Other
regulatory
factors
Normal Subject
Other
regulatory
FIGURE 7.2
Response to Stress in a Normal
Subject and a Patient with Major
Depressive Disorder
In normal subjects and in patients with
‘major depression, periods of stress are
‘typically associated with increased
levels of both cortisol and carticotropin-
releasing factor. Corticotropin-releasing
{actor stimulates the production of
corticotropin, which in turn stimulates
the production of cortisol. Cortsal
Inhibits the release of corticotropin from
the pituitary and the release of -
Whatis the role of stressful life events in
inipolar depression, and what kinds of
datheses have been proposed to interact
vith them?
> Descibe the following theories of depression:
Beck's cognitive theory, the helplessness and
ss theories, and interpersonal
\BIPOLAR DISORDERS
‘plr disorders are distinguished from unipolar disorders
‘nthe presence of manic or hypomanic symptoms. A pet-
‘a who experiences a manic episode has a markedly cle~
‘ed, cuphoric,and expansive mood, often interrupted by
fis outbursts of intense irritability oF even ve>
particularly when others refuse to go along with
bipolar Disorders
person's wishes and schemes. These extreme
‘moods must persis for at least a week for this diagnosis 10
bbe made, In addition, three or more additional symptoms
must occur inthe same time period. There must ako be
significant impairment of occupational ancl social func
sind. hospitalization is often necessary during
manic episodes.
In milder forms, st
10 a diagnosis of hypon
experiences abnormally elev
‘mood for at least 4 days. In addi
at least three other symptoms simi
mania but to a lesser degree (cf inflated self-esteem,
decreased need for sleep lights of ideas, pressured speech,
etc.) Although the symptoms listed are the same for manic
and hypomanic episodes, there is much less impairment in
social and occupational functioning in hypomania, and
hospitalization is not required.
1 kinds of symptoms can lead
nic episode, in which a person
rated, expansive, of irritable
n,the person must have
lar to those involved in
Cyclothymic Disorder
It has tong been recognized that some people ae subject
to cyclic mood changes les severe than the mood
SSvngs see in bipolar disorder These are the symptoms
Of the disorder known as eyeothymic disorder. In
DSM-iv-TR, eyclothymia is defined asa less serious ver~
Sion of major bipolar disorder, minus certain extreme
Symptom and payehotie features, such as delusions, and
aimee the marked ‘impairment caused. by fallblown
tmanie or major depresive episodes.
Inthe depressed phase of eyclothymic disordes a per-
sons mood iusjsted an he o sh experiencesa dstinet
loss of interest or pleasure in customary activities and pas-
times n aio the person may show other symptoms
Aah as Tow energy, feelings of inadequacy, socal with-
tawal and » pessimistic, brooding atitude. Essential
the symptoms are similar to those in someone with dys-
thymfa except without the duration criterion
Symptoms of the hypomanic phase of cyclothymia
arecatentally the opposite of the symptoms of d)sthymia.
Inthis phase ofthe disorder, the person may become espe
Gilly creative and productive because of increased phy
Gal and mental energy. There may be significant pes
treween episodes in which the person vith eyelothyi
functions ina elatively adaptive manner. For a diagnosis
(feyelothymia, there mast beat least a 2-year span during
sihigh there are numerous periods with hypomanic and
depressed symptoms (1 year for adolescents and. ch
deen) and the symptoms must cause clinlly significant
istres or Impairment in functioning (although not as
Severe ain bipolar disorder). (Sethe DSM-IV-TR table,
Giteria for Cyelothymic Divorder) Because individuals
with epelothymia ate a increased tisk of later developing
full-biown bipolar disorder (eg Akiskal & Pinto, 1999),
DSM-IV-TR recommend that they be treated
“The following case illustrates cylothymia.
1253
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5834)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (852)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (903)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (541)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (349)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (823)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (405)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- epqDocument9 pagesepqSazia BegumNo ratings yet
- Adobe Scan Apr 30, 2023Document19 pagesAdobe Scan Apr 30, 2023Sazia BegumNo ratings yet
- PersonalityDocument5 pagesPersonalitySazia BegumNo ratings yet
- DAT VR ReportDocument2 pagesDAT VR ReportSazia BegumNo ratings yet
- SocialMediaandYoungPeopleEmotion JMIW2019Document16 pagesSocialMediaandYoungPeopleEmotion JMIW2019Sazia BegumNo ratings yet
- Professional Make-Up CourseDocument9 pagesProfessional Make-Up CourseSazia BegumNo ratings yet
- New Doc 2023-03-28 12.10.05Document2 pagesNew Doc 2023-03-28 12.10.05Sazia BegumNo ratings yet
- DocScanner 18-May-2023 4-37 PMDocument5 pagesDocScanner 18-May-2023 4-37 PMSazia BegumNo ratings yet
- Scientific Information System: Network of Scientific Journals From Latin America, The Caribbean, Spain and PortugalDocument9 pagesScientific Information System: Network of Scientific Journals From Latin America, The Caribbean, Spain and PortugalSazia BegumNo ratings yet
- Family Pathology ScaleDocument4 pagesFamily Pathology ScaleSazia BegumNo ratings yet
- Assignment-1 Sazia BegumDocument4 pagesAssignment-1 Sazia BegumSazia BegumNo ratings yet