Professional Documents
Culture Documents
Questions
Questions
Uploaded by
shajitha.saji141Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Questions
Questions
Uploaded by
shajitha.saji141Copyright:
Available Formats
1.
A 67-year-old male patient is admitted to the postanesthesia care
unit (PACU) after abdominal surgery. Which assessment, if made by
the nurse, is the best indicator of respiratory depression?
Increased respiratory rate
Decreased oxygen saturation
Increased carbon dioxide pressure
Frequent premature ventricular contractions (PVCs)
Increased carbon dioxide pressure
Transcutaneous carbon dioxide pressure (PtcCO2) monitoring is a
sensitive indicator of respiratory depression. Increased CO2 pressures
would indicate respiratory depression. Clinical manifestations of
inadequate oxygenation include increased respiratory rate,
dysrhythmias (e.g., premature ventricular contractions), and decreased
oxygen saturation.
2.The nurse is caring for a 54-year-old unconscious female patient
who has just been admitted to the postanesthesia care unit after
abdominal hysterectomy. How should the nurse position the patient?
Left lateral position with head supported on a pillow
Prone position with a pillow supporting the abdomen
Supine position with head of bed elevated 30 degrees
Semi-Fowler's position with the head turned to the right
Left lateral position with head supported on a pillow
The unconscious patient should be placed in the lateral "recovery"
position to keep the airway open and reduce the risk of aspiration.
Once conscious, the patient is usually returned to a supine position
with the head of the bed elevated to maximize expansion of the thorax
by decreasing the pressure of the abdominal contents on the
diaphragm.
3.Which patient would be at highest risk for hypothermia after
surgery?
A 42-year-old patient who had a laparoscopic appendectomy
A 38-year-old patient who had a lumpectomy for breast cancer
A 20-year-old patient with an open reduction of a fractured radius
A 75-year-old patient with repair of a femoral neck fracture after a fall
A 75-year-old patient with repair of a femoral neck fracture after a fall
Patients at highest risk for hypothermia are those who are older,
debilitated, or intoxicated. Also, long surgical procedures and
prolonged anesthetic administration place the patient at increased risk
for hypothermia.
4.The nurse is providing discharge teaching to a 51-year-old female
patient who has had a laparoscopic cholecystectomy at an ambulatory
surgery center. Which statement, if made by the patient, indicates an
understanding of the discharge instructions?
"I will have someone stay with me for 24 hours in case I feel dizzy."
"I should wait for the pain to be severe before taking the medication."
"Because I did not have general anesthesia, I will be able to drive
home."
"It is expected after this surgery to have a temperature up to 102.4o
F."
"I will have someone stay with me for 24 hours in case I feel dizzy."
The nurse must assess understanding of discharge instructions and the
ability of the patient and caregiver to provide for home care needs.
The patient must be accompanied by a responsible adult caregiver.
The patient may not drive after receiving anesthetics or sedatives. The
patient should understand how to manage pain, and pain medication
should be taken before the pain becomes severe. The patient should
understand symptoms to be reported, such as a fever.
5.The nurse cares for a 72-year-old Native American male patient 2
days after a thoracotomy for tumor resection. What would be the most
appropriate action if the patient does not report any pain?
Contact the health care provider.
Identify possible reasons for denial of pain.
Administer the prescribed pain medication.
Assess the renal and liver function test results.
Identify possible reasons for denial of pain.
1.Unless contraindicated by the surgical procedure, which position is
preferred for the unconscious patient immediately postoperative?
Supine
Lateral
Semi-Fowler's
High-Fowler's
Lateral
2. The nurse is working on a surgical floor and is preparing to receive
a postoperative patient from the postanesthesia care unit (PACU).
What should the nurse's initial action be upon the patient's arrival?
Assess the patient's pain.
Assess the patient's vital signs.
Check the rate of the IV infusion.
Check the physician's postoperative orders.
Assess the patient's vital signs.
The highest priority action by the nurse is to assess the physiologic
stability of the patient. This is accomplished in part by taking the
patient's vital signs. The other actions can then take place in rapid
sequence.
3. When assessing a patient's surgical dressing on the first
postoperative day, the nurse notes new, bright-red drainage about 5
cm in diameter. In response to this finding, what should the nurse do
first?
Recheck in 1 hour for increased drainage.
Notify the surgeon of a potential hemorrhage.
Assess the patient's blood pressure and heart rate.
Remove the dressing and assess the surgical incision.
Assess the patient's blood pressure and heart rate.
The first action by the nurse is to gather additional assessment data to
form a more complete clinical picture. The nurse can then report all of
the findings. Continued reassessment will be done. Agency policy
determines whether the nurse may change the dressing for the first
time or simply reinforce it.
4.In planning postoperative interventions to promote repositioning,
ambulation, coughing, and deep breathing, which action should the
nurse recognize will best enable the patient to achieve the desired
outcomes?
Administering adequate analgesics to promote relief or control of pain
Asking the patient to demonstrate the postoperative exercises every 1
hour
Giving the patient positive feedback when the activities are performed
correctly
Warning the patient about possible complications if the activities are
not performed
Administering adequate analgesics to promote relief or
control of pain
5. Bronchial obstruction by retained secretions has contributed to a
postoperative patient's recent pulse oximetry reading of 87%. Which
health problem is the patient probably experiencing?
Atelectasis
Bronchospasm
Hypoventilation
Pulmonary embolism
Atelectasis
The most common cause of postoperative hypoxemia is atelectasis,
which may be the result of bronchial obstruction caused by retained
secretions or decreased respiratory excursion. Bronchospasm involves
the closure of small airways by increased muscle tone, whereas
hypoventilation is marked by an inadequate respiratory rate or depth.
Pulmonary emboli do not involve blockage by retained secretions.
You might also like
- Perioperative NursingDocument11 pagesPerioperative NursingMary Rias80% (5)
- Alexanders Care of The Patient in Surgery 16th Edition Rothrock Test BankDocument11 pagesAlexanders Care of The Patient in Surgery 16th Edition Rothrock Test Banklilykeva56r100% (37)
- The Biology of Being Frazzled (Arnsthen A., 1998)Document3 pagesThe Biology of Being Frazzled (Arnsthen A., 1998)JuanCarlosEspecializaciónNo ratings yet
- Case Study, Chapter 3, Critical Thinking, Ethical Decision Making, and The Nursing ProcessDocument2 pagesCase Study, Chapter 3, Critical Thinking, Ethical Decision Making, and The Nursing Processclyde i am0% (1)
- ReMyte Invisible Minerals II Carolyn Dean MD NDDocument100 pagesReMyte Invisible Minerals II Carolyn Dean MD NDBlake Conley100% (2)
- Anesthesiology Case PresDocument25 pagesAnesthesiology Case PresKirstin100% (1)
- Moderate Sedation PowerpointDocument68 pagesModerate Sedation PowerpointJames GarnerNo ratings yet
- Bariatric Case StudyDocument11 pagesBariatric Case Studyapi-346620455100% (3)
- Case Study Chapter 20 (Oct 16th)Document2 pagesCase Study Chapter 20 (Oct 16th)Anz MingNo ratings yet
- Anaesthesia 2018 10 Cases-PBLDocument12 pagesAnaesthesia 2018 10 Cases-PBLReddyNo ratings yet
- All Anthesia Cases SolvedDocument8 pagesAll Anthesia Cases SolvedHamdy GowefilNo ratings yet
- Module 2 PDFDocument13 pagesModule 2 PDFAlup MjhayNo ratings yet
- 4 - Post Operative Nursing ManagementDocument38 pages4 - Post Operative Nursing ManagementraghadNo ratings yet
- Care of The Older Adult - SAS 3Document4 pagesCare of The Older Adult - SAS 3Gia Lourdes Camille AustriaNo ratings yet
- 4 - Post Operative Phase 1Document39 pages4 - Post Operative Phase 1ننن نننن100% (5)
- MASTERY TEST 1 MedSurgDocument11 pagesMASTERY TEST 1 MedSurgHan NahNo ratings yet
- Week 6 DocsDocument18 pagesWeek 6 DocsSHERMINA HASANNo ratings yet
- (Osborn) Chapter 27: Learning Outcomes (Number and Title)Document16 pages(Osborn) Chapter 27: Learning Outcomes (Number and Title)KittiesNo ratings yet
- RN Targeted Medical Surgical Perioperative Online Practice 2Document6 pagesRN Targeted Medical Surgical Perioperative Online Practice 2Adriana RemedioNo ratings yet
- Care of Preoperative Patients 1 3 .Docx-1Document4 pagesCare of Preoperative Patients 1 3 .Docx-1mark OrpillaNo ratings yet
- MS Lec Notes Sas 1to 16Document25 pagesMS Lec Notes Sas 1to 16Noven CalambroNo ratings yet
- New Microsoft Office Word DocumentDocument6 pagesNew Microsoft Office Word DocumentMainak MajiNo ratings yet
- Medical Surgical NCLEX Test 2Document6 pagesMedical Surgical NCLEX Test 2mj078100% (1)
- Emergence and Postoperative Anesthetic Management: Prepared By: Serkalem Teshome Advised by Instructor WosneyelehDocument85 pagesEmergence and Postoperative Anesthetic Management: Prepared By: Serkalem Teshome Advised by Instructor WosneyelehagatakassaNo ratings yet
- Exams MedsurgDocument29 pagesExams MedsurgUy Jezrielle MicahNo ratings yet
- ExamDocument7 pagesExamRhabdoNo ratings yet
- Preop & Postop Nursing InterventionsDocument8 pagesPreop & Postop Nursing InterventionsLizethNo ratings yet
- RespiDocument1 pageRespiBeverlyn AsparoNo ratings yet
- OR Medsurg Shifting ExamDocument23 pagesOR Medsurg Shifting ExamEya BaldostamonNo ratings yet
- Admission Posttest EditedDocument22 pagesAdmission Posttest EditedBryan DorosanNo ratings yet
- CardiovascularDocument46 pagesCardiovascularHamza NejibNo ratings yet
- Postoperative Care SWEETDocument4 pagesPostoperative Care SWEETHans Dayag MallillinNo ratings yet
- Sas 3 Cabahug, Victoria Mae IDocument3 pagesSas 3 Cabahug, Victoria Mae Ibekbekk cabahugNo ratings yet
- ICC2 (008) Perioperative Care WorkbookDocument99 pagesICC2 (008) Perioperative Care WorkbookMariam Mokhtar ZedanNo ratings yet
- Post Op CareDocument7 pagesPost Op CareJeraldien Diente TagamolilaNo ratings yet
- Final Exam Questions 3Document40 pagesFinal Exam Questions 3clarke skaikruNo ratings yet
- Prometric 2 PDFDocument24 pagesPrometric 2 PDFKatherine Joy ApquisNo ratings yet
- N105 - Quizlet Finals ReviewerDocument28 pagesN105 - Quizlet Finals ReviewerJustine Charles UbaldeNo ratings yet
- Safe Recovery From AnaesthesiaDocument7 pagesSafe Recovery From AnaesthesiaKarthikNo ratings yet
- Cardio QuestionsDocument18 pagesCardio QuestionsTrisha ArizalaNo ratings yet
- Ch. 19. Postoperative Nursing CareDocument51 pagesCh. 19. Postoperative Nursing Careمحمد الحواجرةNo ratings yet
- 1Document7 pages1YolieEspejo100% (2)
- (Osborn) Chapter 41: Learning Outcomes (Number and Title)Document19 pages(Osborn) Chapter 41: Learning Outcomes (Number and Title)KittiesNo ratings yet
- OLA HA LecDocument4 pagesOLA HA LecBetina De JesusNo ratings yet
- ReviewerDocument10 pagesReviewerCharlene RepolloNo ratings yet
- HESI SampleDocument4 pagesHESI SampleTerex ManualNo ratings yet
- UntitledDocument15 pagesUntitledstuffednurseNo ratings yet
- Hypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumDocument5 pagesHypertension NCLEX Quiz Questions: A. I Will Make Sure I Consume Foods High in PotassiumMelodia Turqueza GandezaNo ratings yet
- Critical Thinking ExerciseDocument5 pagesCritical Thinking ExerciseRey Teofilo ArnadoNo ratings yet
- Concept On Surgery: Postoperative CareDocument44 pagesConcept On Surgery: Postoperative CareMelisa ClaireNo ratings yet
- NCP Gouty ArthritisDocument21 pagesNCP Gouty ArthritisArianne Kamille Andes67% (3)
- Alterations in The Surgical Patient Updated 2010Document122 pagesAlterations in The Surgical Patient Updated 2010hkellyrnNo ratings yet
- 50items Funda Part 1Document52 pages50items Funda Part 1clobregas100% (3)
- Fundamental of Nursing 3Document7 pagesFundamental of Nursing 3Atom AtomicNo ratings yet
- Perioperative NursingDocument8 pagesPerioperative NursinglovethestarNo ratings yet
- P2 Funda LecDocument8 pagesP2 Funda LecAira Mae R. AndradaNo ratings yet
- Nursing Diagnosis Impaired Gas ExchangeDocument7 pagesNursing Diagnosis Impaired Gas ExchangeZycon Rodney Ae'zecquel Gachallan50% (2)
- Top 10 Care Essentials in Ventilated PtsDocument3 pagesTop 10 Care Essentials in Ventilated PtsAdel HamadaNo ratings yet
- NCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!From EverandNCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!Rating: 5 out of 5 stars5/5 (4)
- Textbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyFrom EverandTextbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyNo ratings yet
- Hysterectomy, (Removal of Uterus) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHysterectomy, (Removal of Uterus) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- TÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANOFrom EverandTÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANONo ratings yet
- نموذج انقاذ حياة الجديدDocument2 pagesنموذج انقاذ حياة الجديدraad_alghamdi_10% (1)
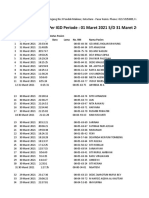
- Triase IGD Maret 2021Document33 pagesTriase IGD Maret 2021IRAYANANo ratings yet
- Đề Cương Giữa Kì 1 Lớp 11 (2023-2024) Ban HsDocument10 pagesĐề Cương Giữa Kì 1 Lớp 11 (2023-2024) Ban Hsmyorange9277No ratings yet
- Wet To Damp DressingDocument2 pagesWet To Damp DressingCarrie TranNo ratings yet
- Acute Coronary SyndromeDocument8 pagesAcute Coronary SyndromeMohammad Neyazur RahamanNo ratings yet
- Enhancement of Antimicrobial Potential Of: Phyllanthus Niruri by FermentationDocument9 pagesEnhancement of Antimicrobial Potential Of: Phyllanthus Niruri by FermentationZil ArdiNo ratings yet
- 4Document19 pages4engineering_readerNo ratings yet
- Infertility: Kindu Y, LecturerDocument77 pagesInfertility: Kindu Y, LecturerCHALIE MEQUNo ratings yet
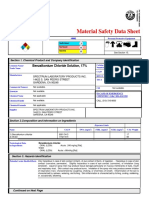
- Benzalkonium Chloride Solution, 17% MSDS - Revision 09-09-08Document7 pagesBenzalkonium Chloride Solution, 17% MSDS - Revision 09-09-08New TubeNo ratings yet
- Chemical Product and Company Information: Material Safety Data SheetDocument5 pagesChemical Product and Company Information: Material Safety Data Sheetkirandas_mullasseryNo ratings yet
- Amphotericin B: Component Mg/liter Mol. Wt. Mol. (MM)Document7 pagesAmphotericin B: Component Mg/liter Mol. Wt. Mol. (MM)Echa Alifyanty SyarifNo ratings yet
- Bhat. Et Al. - 2014 - Coriander (Coriandrum Sativum L.) Processing, Nutritional and Functional AspectsDocument9 pagesBhat. Et Al. - 2014 - Coriander (Coriandrum Sativum L.) Processing, Nutritional and Functional AspectsirfanNo ratings yet
- Housing and Health: Time Again For Public Health ActionDocument11 pagesHousing and Health: Time Again For Public Health ActionDiogo CostaNo ratings yet
- HERU SETIAWAN-Week-4 Assigment Gene InteractionDocument2 pagesHERU SETIAWAN-Week-4 Assigment Gene InteractionHeru SetiawanNo ratings yet
- Bender Gestalt TestDocument3 pagesBender Gestalt TestAleena ThakurtaNo ratings yet
- 50 Items HADocument7 pages50 Items HAToni Marie Buenconsejo PunzalanNo ratings yet
- Neuroanatomy NotesDocument26 pagesNeuroanatomy Notesdeyar janblyNo ratings yet
- Aioh Position Paper Rcs Update Sep2018 Final Unmarked DraftDocument19 pagesAioh Position Paper Rcs Update Sep2018 Final Unmarked Drafthitman1363No ratings yet
- Washing Raw Chicken Increases Risk of Food Poisoning: Campylobacter Causes An InfectiousDocument3 pagesWashing Raw Chicken Increases Risk of Food Poisoning: Campylobacter Causes An InfectioussecretNo ratings yet
- FIFe EMS System User GuidelinesDocument3 pagesFIFe EMS System User GuidelinesAlexanderSmithNo ratings yet
- Evaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisDocument5 pagesEvaluation of Antibiotic Sensitivity Pattern in Acute TonsillitisyoanaNo ratings yet
- Diabetes Comprehensive T2DM Management: Hemi SinoritaDocument55 pagesDiabetes Comprehensive T2DM Management: Hemi SinoritaJipeeZedNo ratings yet
- Stiles Et Al (2020) Impact of COVID 19 On Health and Safety in The Construction SectorDocument13 pagesStiles Et Al (2020) Impact of COVID 19 On Health and Safety in The Construction SectorCeline DupontNo ratings yet
- Home Remedies For Ringworm - 11 Natural TreatmentsDocument11 pagesHome Remedies For Ringworm - 11 Natural TreatmentsHenz FreemanNo ratings yet
- Epworth Richmond - Agency Staff Orientation Booklet MAY 2016Document33 pagesEpworth Richmond - Agency Staff Orientation Booklet MAY 2016Anonymous BaD9jQNo ratings yet
- Concepts of ProsthoDocument22 pagesConcepts of ProsthoKirti SharmaNo ratings yet
- The Omnivores Dilemma Chapter 4Document2 pagesThe Omnivores Dilemma Chapter 4api-239466415No ratings yet