Professional Documents
Culture Documents
Poster 29
Poster 29
Uploaded by
aamir6312Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Poster 29
Poster 29
Uploaded by
aamir6312Copyright:
Available Formats
IMPROVEMENT IN RECORDING, IDENTIFICATION AND
MANAGEMENT OF ORTHOSTATIC HYPOTENSION (CYCLE 3)
Dr Elinor Burn SpR1 , Dr Sooraj Mannil SHO 1, Dr Ethan Maltlyn F11, Dr Anu Thomas SHO1 (1)University Hospitals of Leicester, NHS Trust
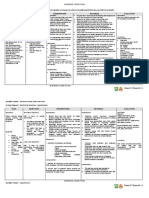
Quick Glance : Previous Audits / Interventions Note : Standards from previous samples were slightly different ; hence limiting direct comparison
Management of patients with falls and OH Improvement in recording and identification of LSBP
62% had LSBP measured when indicated
Supine for 5 mins 56 %
87.1 % did not had multiple BP recordings Creating an awareness card about standard guidelines of
1 min - 2nd BP 40 %
22.6 % had standing heart rate mentioned measuring LSBP
CYCLE 1
CYCLE 2
3 min - 3rd BP 33 %
Interventions Sharing information during HCA and Nurses meeting
Symptoms 27 %
To improve the electronic documentation in NerveCentre
Unified guidance for staff on ideal method for measuring LSBP Record and inform 25 %
or flowchart attached in bedside chart.
Proper training on measuring LSBP
Create a prompt card to attach to BP machine
Design a sticker/form to be placed in the notes
Interventions
Guidance for how & when to take action depending on results
Contributing authors from previous cycles : Dr Chan Nyein Khin, Dr Hay Mar Tun, Dr Nyein Aye Thu, Dr Hnin Oo Win, Dr Syed Ahmed, Dr Simon Biju, Dr D Lahhani, Dr George Ghaly, Dr James Reid
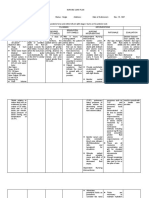
OBJECTIVES GUIDELINES
Review the management of Orthostatic Hypotension in acute medical admissions: RCP Guidelines : Measurement of lying and standing blood pressure
1. Interpret postural blood pressure readings The first BP should be taken after lying for at least 5 minutes.
2. Improve the recording of lying and standing blood pressure (LSBP) in acute The second BP should be taken after standing in the first minute.
medical admissions. A third BP should be taken after standing for 3 minutes.
3. Knowledge and confidence in assessment and management of OH
This recording can be repeated if the BP is still falling.
Symptoms of dizziness, light-headedness, vagueness, pallor, visual
METHODOLOGIES disturbance, feelings of weakness and palpitations should be documented.
Quantitative Qualitative
Patients admitted with falls, syncope, Questionnaire responses
orthostatic hypotension, or collapse gathered from 5 different
and aged 65+ admission wards from a
24 patients were reviewed. multidisciplinary team.
RESULTS
POSITIVE Results
Quantitative
The sample had 67% males, average age 82. a drop in systolic a drop to below 90 a drop in diastolic BP of
79% had LSBP measured; 42% experienced BP drop. BP of 20 mmHg or mmHg on standing even 10 mmHg with symptoms
84% had falls history; 58% reported presyncope. more (with or if the drop is less than (although clinically much
without symptoms) 20 mmHg (with or less significant than a
83% had polypharmacy (average 9.2 medications). Common medications:
without symptoms) drop in systolic BP)
antihypertensives (46%), analgesia (42%), diuretics (25%).
Advise patient of results, and if the result is positive:
Outcomes: 30-day mortality 17%, discharge to home 25%, rehab 21%.
inform the medical and nursing team
Qualitative take immediate actions to prevent falls and or unsteadiness
(Junior Doctors on average 0)
Only 9 members of staff were
able to recognise headache as an
atypical presentation of OH.
LSBPs performed in the last month (average)
1st BP recording 2nd BP recording 3rd BP recording
CONCLUSIONS
Orthostatic hypotension contributes to falls and morbidity. Though 79% of patients presenting with falls had LSBP recorded, documentation of heart rate and
symptoms needs improvement. Staff knowledge on LSBP measurement varied (38-42%). This indicates a need for ongoing education, through LSBP roadshow
events alongside reintroducing BP machine LSBP prompt cards and developing a trust based information leaflet for patient education for orthostatic hypotension
management.
References Abbreviations
Trust Guidelines, Orthostatic Hypotension (OH) UHL Emergency and Specialist Medicine Guideline (B45/2017) LSBP: Lying and Standing Blood Pressure HCA: Healthcare Assistant
RCP Standard Guidelines : Measurement of lying and standing blood pressure: A brief guide for clinical staff OH : Orthostatic Hypotension
You might also like
- ACLS Exam Version BDocument16 pagesACLS Exam Version BAhmed - Sawalha97% (65)
- ACLS Review TestDocument5 pagesACLS Review Testtostc60% (5)
- Cardiovascular Disorders Concept MapDocument4 pagesCardiovascular Disorders Concept MapZairaNo ratings yet
- SepsisDocument3 pagesSepsisPhilip Poerworahjono100% (3)
- Biomarkers Identifying Sepsis Phenotypes PDFDocument42 pagesBiomarkers Identifying Sepsis Phenotypes PDFjenaro heli Ardila CortesNo ratings yet
- Webminar: Hypertension and Diabetes Mellitus Management in Clinical PracticesDocument37 pagesWebminar: Hypertension and Diabetes Mellitus Management in Clinical PracticesSans 88No ratings yet
- Final NCP (Jannel)Document6 pagesFinal NCP (Jannel)Zed P. EstalillaNo ratings yet
- Kami Kagina, Gulpiyada Lang Siya Nadulaan Kusog Kag Gapukol Iya Hambalanon, Kag Nagakiwi Iya Nga Itsura." As VerbalizedDocument4 pagesKami Kagina, Gulpiyada Lang Siya Nadulaan Kusog Kag Gapukol Iya Hambalanon, Kag Nagakiwi Iya Nga Itsura." As VerbalizedKoleen Lhyte T. UYNo ratings yet
- Nursing Care Plan: Assessment Explanation of The Problem Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Assessment Explanation of The Problem Objectives Interventions Rationale EvaluationNelly CruzNo ratings yet
- dbs brainsense case study suboptimal programming(监测技术的介绍与患者案例)Document5 pagesdbs brainsense case study suboptimal programming(监测技术的介绍与患者案例)bg5hfcNo ratings yet
- KDIGO 2021 Clinical Practice Guideline For The Management of BP in CKD-p26-31Document6 pagesKDIGO 2021 Clinical Practice Guideline For The Management of BP in CKD-p26-31kieuchinhNo ratings yet
- Arp2018 1486261Document5 pagesArp2018 1486261Sheren ElinNo ratings yet
- HindawiDocument6 pagesHindawiTaufiqo Nugraha SjachrilNo ratings yet
- Starling Published StudiesDocument4 pagesStarling Published Studiesjobbathebutty mamamaNo ratings yet
- The Biology of Chronic Fatigue SyndromeDocument46 pagesThe Biology of Chronic Fatigue SyndromeAgustinus Benediktus Danang PutroNo ratings yet
- Changes in Control Status of COPD Over Time and T - 2021 - Archivos de BronconeuDocument8 pagesChanges in Control Status of COPD Over Time and T - 2021 - Archivos de BronconeuMomoh GaiusNo ratings yet
- Cirrhosis and Complications: Best of ILC 2019Document29 pagesCirrhosis and Complications: Best of ILC 2019Юлия ЦыгановаNo ratings yet
- Jaundice (Summary)Document7 pagesJaundice (Summary)Sutirtha RoyNo ratings yet
- Acute Kidney Injury W/ Hyperkalemia NCPDocument5 pagesAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNo ratings yet
- Sink or Swim: New Waves in Fluid ResuscitationDocument55 pagesSink or Swim: New Waves in Fluid ResuscitationPhilip PoerworahjonoNo ratings yet
- 2019 - Evaluation of Procalcitonin in A Fluorescent Immunoassay AFIAS-6 AnalyzerDocument2 pages2019 - Evaluation of Procalcitonin in A Fluorescent Immunoassay AFIAS-6 AnalyzerTalent SackareNo ratings yet
- Ventriculo-Peritoneal Shunting Is A Safe and Effective Treatment For Idiopathic Intracranial HypertensionDocument10 pagesVentriculo-Peritoneal Shunting Is A Safe and Effective Treatment For Idiopathic Intracranial HypertensionTELHNo ratings yet
- EBM Therapy: DR - Edward Kosasih, MARS, PA, DKDocument26 pagesEBM Therapy: DR - Edward Kosasih, MARS, PA, DKReinsy NoviNo ratings yet
- CFR Bayes-Genis WEBDocument8 pagesCFR Bayes-Genis WEBTran Nguyen ChiNo ratings yet
- Sepsis and AnaesthesiaDocument44 pagesSepsis and AnaesthesiaFanny Ari SandyNo ratings yet
- Chronic Heart FailureDocument25 pagesChronic Heart FailureNeilavery WindaNo ratings yet
- Nursing Care Management of Systematic Lupus ErythematosusDocument53 pagesNursing Care Management of Systematic Lupus ErythematosusDana Marie LeanoNo ratings yet
- Blood Pressure Management in The Patient With Chronic Kidney DiseaseDocument3 pagesBlood Pressure Management in The Patient With Chronic Kidney DiseaseMahmoud AbouelsoudNo ratings yet
- Risperidone Induced Seizures After Cessation of ClozapineDocument1 pageRisperidone Induced Seizures After Cessation of ClozapineAttaufiq IrawanNo ratings yet
- Hiperparatiroidismo PsiquiatriaDocument3 pagesHiperparatiroidismo PsiquiatriaSamuel HernandezNo ratings yet
- Therapeutic Plasma Exchange Improves Short-Term, But Not Longterm, Outcomes in Patients With Acute-On-Chronic Liver Failure - A Propensity Score-Matched AnalysisDocument3 pagesTherapeutic Plasma Exchange Improves Short-Term, But Not Longterm, Outcomes in Patients With Acute-On-Chronic Liver Failure - A Propensity Score-Matched Analysisgwyneth.green.512No ratings yet
- 2021 Nguyen JAMA Effect of Osteopathic Manipulative Treatment Vs Sham Treatment On Activity Limitations in Patients With Nonspecific Subacute and Chronic Low Back PainDocument11 pages2021 Nguyen JAMA Effect of Osteopathic Manipulative Treatment Vs Sham Treatment On Activity Limitations in Patients With Nonspecific Subacute and Chronic Low Back PainLaurent FabreNo ratings yet
- Otorhinolaryngology: Clinical Characteristics of Patients With Persistent Postural-Perceptual DizzinessDocument7 pagesOtorhinolaryngology: Clinical Characteristics of Patients With Persistent Postural-Perceptual DizzinessFernando SalesNo ratings yet
- Prediction of Hypotension Using PerfusioDocument6 pagesPrediction of Hypotension Using PerfusioachyutsharmaNo ratings yet
- NCPDocument4 pagesNCPNurhaifa MocademaNo ratings yet
- Vital Sign Variations With Complications During Dialysis Among End-Stage Renal Disease PatientsDocument5 pagesVital Sign Variations With Complications During Dialysis Among End-Stage Renal Disease PatientsNanda Putri SeptianaNo ratings yet
- Geriatic Fluid and Electrolyte Imbalance NCPDocument4 pagesGeriatic Fluid and Electrolyte Imbalance NCPCA Candido JavierNo ratings yet
- Nursing Care Plan PT1Document2 pagesNursing Care Plan PT1Trexie ScattNo ratings yet
- Reduction in The Incidence of Awareness Using BIS MonitoringDocument7 pagesReduction in The Incidence of Awareness Using BIS MonitoringAlan Robinet VargasNo ratings yet
- AnaphylaxisDocument7 pagesAnaphylaxisDr. Sarthak MishraNo ratings yet
- Low Dose Levobupivacaıne 0.5% With Fentanyl in Spinal Anaesthesia For Transurethral Resection of Prostate SurgeryDocument6 pagesLow Dose Levobupivacaıne 0.5% With Fentanyl in Spinal Anaesthesia For Transurethral Resection of Prostate Surgeryblabarry1109No ratings yet
- TannenbaumDocument12 pagesTannenbaumayunda sherinaNo ratings yet
- Prediction 3Document21 pagesPrediction 3Adina Bîrsan-MarianNo ratings yet
- Sickle Cell - RahafDocument39 pagesSickle Cell - RahafgalalNo ratings yet
- HP For Sepsis and AKIDocument28 pagesHP For Sepsis and AKICordis SternumNo ratings yet
- Acute DyspneaDocument37 pagesAcute Dyspneaisnaira imamNo ratings yet
- Cues Nursing Diagnosis Analysis Goals/Objectives Intervention Rationale EvaluationDocument6 pagesCues Nursing Diagnosis Analysis Goals/Objectives Intervention Rationale EvaluationClarissa GuifayaNo ratings yet
- 2017-2018preparation For Safe PT Care 2017-218 1 FinalDocument20 pages2017-2018preparation For Safe PT Care 2017-218 1 Finalapi-450606407No ratings yet
- Study of The Role of Plasma Nt-Probnp in The Diagnosis of Heart FailureDocument5 pagesStudy of The Role of Plasma Nt-Probnp in The Diagnosis of Heart FailureMinerva Medical Treatment Pvt LtdNo ratings yet
- JCPT 46 585Document14 pagesJCPT 46 585Syam ChandrasekharanNo ratings yet
- The Effect of Photobiomodulation On Chemotherapy-Induced PeripheralDocument8 pagesThe Effect of Photobiomodulation On Chemotherapy-Induced PeripheralLizeth Arce100% (1)
- ENT 讀書報告Chapter74 C2 吳丞皓Document20 pagesENT 讀書報告Chapter74 C2 吳丞皓陳永杰No ratings yet
- Long-Term Efficacy of Shunt Therapy in Idiopathic Normal Pressure HydrocephalusDocument6 pagesLong-Term Efficacy of Shunt Therapy in Idiopathic Normal Pressure HydrocephalusLeoberto Batista Pereira SobrinhoNo ratings yet
- Obesity Hypoventilation SyndromeDocument88 pagesObesity Hypoventilation SyndromeakijismNo ratings yet
- EDTA Chelation-Hypertension Study - Clinical Patterns As Judged by The Cornell Medical Index QuestionnaireDocument5 pagesEDTA Chelation-Hypertension Study - Clinical Patterns As Judged by The Cornell Medical Index QuestionnaireFilipos ConstantinNo ratings yet
- "Mayroong Namuong Dugo Sa Utak Niya Kaya Hindi Maayos Ang Daloy NG Dugo Rito" As Verbalized by The Patient's MotherDocument6 pages"Mayroong Namuong Dugo Sa Utak Niya Kaya Hindi Maayos Ang Daloy NG Dugo Rito" As Verbalized by The Patient's MotherAllisson BeckersNo ratings yet
- Integration and Synergy of Infusion Pump and Patient Monitor (1Document39 pagesIntegration and Synergy of Infusion Pump and Patient Monitor (1ItalmarNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanMariel GamaloNo ratings yet
- Gi-Rle - NCP For Deficient Fluid VolumeDocument2 pagesGi-Rle - NCP For Deficient Fluid VolumeEvangeline Villa de Gracia100% (1)
- Journal Club - FinishedDocument2 pagesJournal Club - Finishedapi-508122123No ratings yet
- Severe Dengue and Pocus EditedDocument44 pagesSevere Dengue and Pocus EditedMaarveen RajNo ratings yet
- Hemodynamic Alteration DSSDocument18 pagesHemodynamic Alteration DSSAbdul ChairyNo ratings yet
- Atlas of High-Resolution Manometry, Impedance, and pH MonitoringFrom EverandAtlas of High-Resolution Manometry, Impedance, and pH MonitoringNo ratings yet
- OSCE Checklist Blood Pressure MeasurementDocument2 pagesOSCE Checklist Blood Pressure MeasurementRohullah QasimiNo ratings yet
- Electrogram Recording and Analyzing Techniques ToDocument14 pagesElectrogram Recording and Analyzing Techniques ToTanah PantaiNo ratings yet
- Cardiac Risk Stratification - CardiologyDocument10 pagesCardiac Risk Stratification - CardiologyDaniel A. Velarde LópezNo ratings yet
- 1 SM PDFDocument6 pages1 SM PDFFina NANo ratings yet
- Ecg Interpretation: Presented by:-ROHINI RAI M SC Nursing Part I, C.O.N, N.B.M.C.HDocument69 pagesEcg Interpretation: Presented by:-ROHINI RAI M SC Nursing Part I, C.O.N, N.B.M.C.HRohini RaiNo ratings yet
- Hyperthyroidism and ComplicationsDocument15 pagesHyperthyroidism and ComplicationsrosianaNo ratings yet
- ACSDocument56 pagesACSGabriel CalderónNo ratings yet
- Jadwal Sympo Edit1Document3 pagesJadwal Sympo Edit1reyNo ratings yet
- Emergency Nursing M8.2 Unit TaskDocument6 pagesEmergency Nursing M8.2 Unit TaskMaria Leonie Dela CruzNo ratings yet
- 6086 24900 1 PBDocument13 pages6086 24900 1 PBSalwiyadiNo ratings yet
- Syok NeurogenikDocument12 pagesSyok NeurogenikFreddy PanjaitanNo ratings yet
- EKG Taki-Bradi AritmiaDocument47 pagesEKG Taki-Bradi Aritmiamithaa octoviagnesNo ratings yet
- AED DesignDocument17 pagesAED DesignAlina BarkovaNo ratings yet
- Omron RS6 Wrist Blood Pressure Monitor Instruction Manual (English)Document8 pagesOmron RS6 Wrist Blood Pressure Monitor Instruction Manual (English)Geza LevaiNo ratings yet
- Physiology Practical 2: Toad HeartDocument10 pagesPhysiology Practical 2: Toad HeartAdams OdanjiNo ratings yet
- Angina PostprandialDocument10 pagesAngina PostprandialJoaquín SosaNo ratings yet
- Ecg Basic ConceptsDocument18 pagesEcg Basic ConceptsDaniel SolonyaNo ratings yet
- Electrocardiograms (ECG) : Figure 1 12 Lead ECG PerspectivesDocument8 pagesElectrocardiograms (ECG) : Figure 1 12 Lead ECG Perspectivessarb100% (1)
- Vasopressors in Septic Shock - Which, When, and How MuchDocument10 pagesVasopressors in Septic Shock - Which, When, and How Muchemres11No ratings yet
- AHA PALS AlgorithmsDocument2 pagesAHA PALS AlgorithmsGulrejNo ratings yet
- Zoll-1200-Op USUARIO PDFDocument57 pagesZoll-1200-Op USUARIO PDFbiomedikarmandoNo ratings yet
- 12 Lead EKG Interpretation PDFDocument251 pages12 Lead EKG Interpretation PDFRobert So JrNo ratings yet
- My TMTDocument22 pagesMy TMTJegadeeswari EswarNo ratings yet
- Hemodynamic Monitoring For NursesDocument29 pagesHemodynamic Monitoring For NursesMahalakshmi Prabhu100% (1)
- Cvs BP Monitor 271245 Wrong UmDocument31 pagesCvs BP Monitor 271245 Wrong UmDarlaNo ratings yet
- Heart Failure Cheat SheetDocument2 pagesHeart Failure Cheat SheetNicolle GaleNo ratings yet
- Manual InstrDocument19 pagesManual InstrAnonymous jDLm5eNjNo ratings yet