Professional Documents
Culture Documents
Urinary Incontinence
Urinary Incontinence
Uploaded by
ipadmed99Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Urinary Incontinence
Urinary Incontinence
Uploaded by
ipadmed99Copyright:
Available Formats
Obstetrics & Gynecology
Anatomy
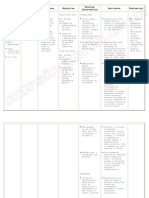
o Normal Urethral Closure must be higher than vesical pressure.
Intrinsic Factors Extrinsic Factors
Striated muscle Levator ani muscles.
(external sphincter). Endopelvic fascia.
Vascular congestion Attachments to the
of submucosal pelvic sidewalls &
venous plexus. urethra.
Smooth muscle
(circular & longitud).
Epithelial coaptation
of the folds of the
urethral lining.
o Bladder:
-pressure system that expands to
Definition accommodate volumes of urine
without appreciable in pressure.
❖ Bladder filling muscle
fiber recruitment of pelvic
floor & urethra outlet
resistance.
❖ Bladder muscle (detrusor)
should remain inactive
during filling.
Micturition
❖ Certain volume is filled
tension-stretch receptors
signal brain micturition
reflex cortical control
mechanisms depend on
social circumstances & the
state of the patient's NS.
Voluntary relaxation of pelvic floor &
Urinary Incontinence Voiding
urethra + Contraction of detrusor.
o Innervation:
Sympathetic NS Parasympathetic NS Somatic NS
T11 – (L2-L3). S2 – S4. S2 – S4.
Acts on: Function: controls Function: innervate
❖ -receptors in urethra & bladder motor function pelvic floor, urethra,
bladder neck urethral contraction & external anal
tone promotes closure. emptying. sphincter.
❖ -receptors in bladder
body detrusor tone.
Rawan Khandaqji Rawan Khandaqji
Obstetrics & Gynecology
Introduction Urge Incontinence
o Definition: involuntary leakage of urine. o Presentation: involuntary leakage of urine accompanied by urgency.
o Epidemiology: o Triggers:
Undetected & undertreated despite its impact on individuals. Running water.
Prevalence in women is high. Hand washing.
In older women prevalence is 17-55%. Cold weather exposure.
In younger & middle-aged women prevalence is 12-42%. o Etiology:
Idiopathic.
Bladder infection.
Classification Bladder inflammation.
Bladder stones.
Bladder cancer.
Stress Incontinence NS diseases (MM).
DM.
o Most common type.
o Pathophysiology: detrusor over activity.
o Definition: involuntary leakage of urine when intra-abdominal pressure
exceeds urethral sphincter closure Symptoms Stress Incontinence Urge Incontinence
mechanisms. Urgency No Yes
o Etiology: Frequency No Yes
Pregnancy, vaginal delivery Leakage with intra-
Yes No
abdominal pressure
most common cause.
Ability to reach toilet on time Yes No
age collagen. Nocturia Seldom Usually
estrogen.
Severe sphincter dysfunction.
Familial. Overflow Incontinence
o Triggers: o Definition: involuntary, continuous, urinary leakage or dribbling and
Sneezing. incomplete bladder emptying.
Coughing. o Etiology:
Laughing. DM.
o Pathophysiology: In female rare mostly due to damage to neurons.
Vesical pressure = detrusor pressure + abdominal pressure. o Pathophysiology:
Normally in coughing for example intra-abdominal pressure is Impaired detrusor contractility or bladder outlet obstruction.
transmitted equally to bladder & urethral sphincter & urethra Bladder is over-distended:
remain fixed in place. Could lead to stress incontinence
Problem in levator ani muscle pressure transmitted mainly to May provoke an uninhibited contraction of detrusor
bladder mobilization of urethra. muscle incontinence.
o Associated Conditions: genital prolapse. o Diagnosis: PVR.
o Treatment: surgery.
Rawan Khandaqji Rawan Khandaqji
Obstetrics & Gynecology
Fistula
Alarm Symptoms
o Presentation: continuous leakage of urine from vagina clothes always
❖ Sudden onset of incontinence.
wet. ❖ Presence of abdominal or pelvic pain.
o Diagnosis: ❖ Hematuria.
Taking sample of the fluid. ❖ Changes in gait or new lower extremity weakness.
CT with contrast. ❖ Cardiopulmonary or neurologic symptoms.
❖ Mental status changes.
o Physical Exam:
Pelvic exam:
Inspection: vaginal mucosa for signs of atrophy
(thinning, pallor, loss of rugae), and inflammation
Palpation: bimanually masses or tenderness.
Assess for prolapse.
Bladder stress test: ask the patient, with a full bladder,
to stand, relax, and give a single vigorous cough
Investigations:
Urine analysis.
Postvoid residual volume (PVR):
❖ PVR of < 50 mL adequate emptying.
❖ PVR > 200 mL inadequate detrusor
weakness or bladder outlet obstruction.
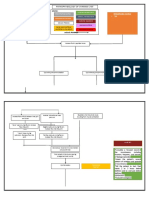
Approach Urodynamic testing:
❖ Group of tests used to assess function of
o History:
urinary tract.
Urinary symptoms.
❖ Cystometry: measure pressure and volume of
How affecting quality of life.
fluid in bladder during filling, storage, &
Associated symptoms depression, anxiety, work impairment,
voiding.
social isolation, sexual dysfunction.
❖ Uroflowmetry: measures the rate of urine flow.
Caffeine intake.
❖ Technique:
Medications.
Chronic disorders. Catheter inserted into bladder vesical pressure
Voiding dairies: Intravesical & rectal catheters measure detrusor & abdominal pressure
Fill bladder with water or normal saline
Provocative maneuvers (Valsalva, running water) determining if they cause leakage
Bladder is completely full begin voiding measurements are made of pressure,
volume, and flow rate.
Rawan Khandaqji Rawan Khandaqji
Obstetrics & Gynecology
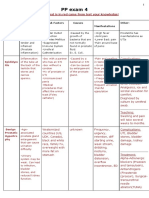
❖ Normal values: o Treatment:
Residal urine < 50 ml Stress Incontinence
1st disere to void 150-250 ml ❖ Reduce factors that worsen the problem obesity,
Strong desire to void > 250 ml smoking, medication, excessive fluid intake…etc
Bladder compliance 400-600 ml Non-Surgical ❖ Pelvic floor exercise & biofeedback.
Flow rate during voiding > 15 ml/sec ❖ Estrogen therapy in postmenopausal.
Detrusor pressure during voiding < 50 cm ❖ Electrical stimulation of pelvic floor muscle.
Overactive bladder ❖ Anterior vaginal colporrhaphy.
Urgency or leakage + Detrusor contraction that patient can’t suppress. ❖ Retropubic bladder neck suspension operations.
Surgical
Stress urinary incontinence ❖ Tension-free vaginal tape.
Leakage with in abdominal pressure (coughing, Valsalva) + No in true detrusor ❖ Periurethral injections.
pressure. Urge Incontinence
❖ Cut down volume of fluid consumed (1-1.5 L/day).
Conservative
❖ Avoid caffeine based drinks.
Vesical ❖ Void on a timed schedule, starting with a relatively
Bladder training
Filling pressure. Detrusor pressure frequent interval.
Phase By bladder remain at 0 or slightly. ❖ Antimuscarinic drugs.
Medications
catheter. ❖ Estrogen.
Abdominal Intra-vesical therapy ❖ Botulinum toxin.
Sharp rises & falls. ❖ In refractory cases.
pressure. Surgery
Cough No in detrusor ❖ Cystoplasty, urinary diversion.
By rectal
pressure. Overflow Incontinence
catheter.
Leak at this stage pure stress incontinence. Medical ❖ Bethanechol.
detrusor pressure Treat underlying ❖ Myomectomy or hysterectomy in the case of fibroid,
Voiding Vesical – cause removal of the urethral stricture
(bladder contract to
Phase abdominal. Intermittent self-
empty)
catheterization
o Prevention:
Lifestyle changes:
Weight loss.
Smoking cessation.
Increasing physical activity.
Improving diet.
Pelvic floor muscle exercises.
Management of conditions associated with incontinence.
Specific medications and surgical procedures may adversely
affect continence.
Rawan Khandaqji Rawan Khandaqji
You might also like
- Concept Map On AppendicitisDocument6 pagesConcept Map On Appendicitisitalisayan_rondario80% (5)
- Shannon Hanchett Autopsy ReportDocument1 pageShannon Hanchett Autopsy ReportOKCFOXNo ratings yet
- Nursing Care Plan CholecystectomyDocument2 pagesNursing Care Plan Cholecystectomyderic87% (23)
- Nursing Care Plan Abruptio PlacentaeDocument2 pagesNursing Care Plan Abruptio Placentaederic93% (29)
- Concept Map of Acute PancreatitisDocument2 pagesConcept Map of Acute Pancreatitissalome carpioNo ratings yet
- Neurogenic BladderDocument11 pagesNeurogenic BladderRoy LiemNo ratings yet
- Jurnal OG 1Document6 pagesJurnal OG 1Wa Ode Meutya ZawawiNo ratings yet
- Catheterization HANDOUTSDocument9 pagesCatheterization HANDOUTSYalc LapidNo ratings yet
- CatheterizationDocument11 pagesCatheterizationSJ MNo ratings yet
- 4.physiology of Micturition PDFDocument20 pages4.physiology of Micturition PDFNaimish VermaNo ratings yet
- Nursing Care Plan Abrubtio PlacentaDocument2 pagesNursing Care Plan Abrubtio PlacentaLei Ortega0% (1)
- Mechanism of MicturitionDocument4 pagesMechanism of MicturitionGerardLum100% (2)
- Lec15 - Renal SystemDocument3 pagesLec15 - Renal SystemGeorge Constante Valiente-SebastianNo ratings yet
- L4 MicturitionDocument26 pagesL4 MicturitionAlimahtabNo ratings yet
- Nursing Care Plan Ectopic PregnancyDocument2 pagesNursing Care Plan Ectopic PregnancyLei Ortega94% (36)
- INTUSSUSCEPTIONDocument1 pageINTUSSUSCEPTIONMaecy PasionNo ratings yet
- Web of Caution (WOC) Ca. ServiksDocument3 pagesWeb of Caution (WOC) Ca. ServiksAndreas Panda BanjalNo ratings yet
- Pathophysiology of Benign Prostatic HyperplasiaDocument1 pagePathophysiology of Benign Prostatic HyperplasiaErika BernardinoNo ratings yet
- Normal KUB-IVP: GUT ViewboxDocument17 pagesNormal KUB-IVP: GUT ViewboxtabatchNo ratings yet
- Impaired Urinary EliminationDocument2 pagesImpaired Urinary EliminationSiafei RabeNo ratings yet
- Seminar 15 - UTIDocument41 pagesSeminar 15 - UTIBONG AIKCHINGNo ratings yet
- PerineumDocument7 pagesPerineumapi-3812135No ratings yet
- Nursing Care Plan Risk For Uterine InfectionDocument4 pagesNursing Care Plan Risk For Uterine Infectionderic97% (30)
- Pathophysiology of Ovarian CystDocument3 pagesPathophysiology of Ovarian CystLuayon FrancisNo ratings yet
- Testicular Torsion, Peds Cases NotesDocument1 pageTesticular Torsion, Peds Cases NotesdzalhcNo ratings yet
- Fisiologi DefekasiDocument9 pagesFisiologi DefekasiAmirullah AbdiNo ratings yet
- Urinary IncontinenceDocument1 pageUrinary IncontinenceZiyad100% (1)
- Testicular Torsion: Journal ReadingDocument14 pagesTesticular Torsion: Journal ReadingRizkiYudaPurnomoNo ratings yet
- MicturitionDocument7 pagesMicturitionOsama MohamedNo ratings yet
- Bladder IrrigationDocument3 pagesBladder IrrigationMyfanway Am-isNo ratings yet
- Abdominal Inury 2Document8 pagesAbdominal Inury 2Chol Koryom CholNo ratings yet
- Chap 23Document25 pagesChap 23Ghazian AdliNo ratings yet
- Physiology of Micturition Reflex PDFDocument37 pagesPhysiology of Micturition Reflex PDFVanathy KarunamoorthyNo ratings yet
- Ipm 2Document3 pagesIpm 2Fritzienico BaskoroNo ratings yet
- PP Exam 4: Everything That Is in Red Came From Test Your Knowledge!Document15 pagesPP Exam 4: Everything That Is in Red Came From Test Your Knowledge!netanya DoanNo ratings yet
- Benign Prostatic HyperplasiaDocument5 pagesBenign Prostatic Hyperplasiatabangin_hilario100% (1)
- Clinical Course Discussion: Oregon Health & Science University, Portland, OregonDocument1 pageClinical Course Discussion: Oregon Health & Science University, Portland, OregonperjadanutNo ratings yet
- 6 SURGERY II 6 - Pediatric UrologyDocument6 pages6 SURGERY II 6 - Pediatric UrologyDeann RoscomNo ratings yet
- Nursing Care Plan For Peritonitis NCPDocument2 pagesNursing Care Plan For Peritonitis NCPyamie sulongNo ratings yet
- Case Study: Lower Gastrointestinal Bleeding Secondary To DiverticulitisDocument14 pagesCase Study: Lower Gastrointestinal Bleeding Secondary To DiverticulitisKevin Cloyd BragasNo ratings yet
- Fluid and ElectrolytesDocument21 pagesFluid and ElectrolytesKc Cabanilla LizardoNo ratings yet
- SABISTON AnoDocument24 pagesSABISTON AnosantigarayNo ratings yet
- Fecal Elimination, Hayam?Document5 pagesFecal Elimination, Hayam?Aryam SNo ratings yet
- Shoulder 1 PDFDocument3 pagesShoulder 1 PDFRyan Joseph GaholNo ratings yet
- Normal Deviation: Imbalanced Nutrtion: Less Than Body Requirements R/T Gastrointestinal ObstructionDocument1 pageNormal Deviation: Imbalanced Nutrtion: Less Than Body Requirements R/T Gastrointestinal ObstructionMaecy PasionNo ratings yet
- Bladder Innervation Physiology of Micturition Voiding DysfunctionDocument77 pagesBladder Innervation Physiology of Micturition Voiding DysfunctionKoushik Sharma AmancharlaNo ratings yet
- Chapter-7-Pathophysiology Nephrotic SyndromeDocument3 pagesChapter-7-Pathophysiology Nephrotic SyndromeCxarina RamirezNo ratings yet
- The Perfect Ic Diet Cookbook The Complete Nutrition Guide To Healing Chronic Pelvic Pain And Managing Symptoms Of Interstitial Cystitis With Delectable And Nourishing RecipesFrom EverandThe Perfect Ic Diet Cookbook The Complete Nutrition Guide To Healing Chronic Pelvic Pain And Managing Symptoms Of Interstitial Cystitis With Delectable And Nourishing RecipesNo ratings yet
- Dictionary of Veterinary Terms: Vet-Speak Deciphered for the Non VeterinarianFrom EverandDictionary of Veterinary Terms: Vet-Speak Deciphered for the Non VeterinarianNo ratings yet
- Conquering Incontinence: A new and physical approach to a freer lifestyleFrom EverandConquering Incontinence: A new and physical approach to a freer lifestyleNo ratings yet
- Female Arousal and Orgasm: Anatomy, Physiology, Behaviour and EvolutionFrom EverandFemale Arousal and Orgasm: Anatomy, Physiology, Behaviour and EvolutionNo ratings yet
- The Perfect Pancreatitis Diet Cookbook; The Complete Nutrition Guide To Managing And Healing Pancreatitis With Delectable And Nourishing Recipes;From EverandThe Perfect Pancreatitis Diet Cookbook; The Complete Nutrition Guide To Managing And Healing Pancreatitis With Delectable And Nourishing Recipes;No ratings yet
- Drug Study of FluoxetineDocument2 pagesDrug Study of FluoxetineLance De GuzmanNo ratings yet
- Genetics and Oral HealthDocument16 pagesGenetics and Oral Healthsalah jerbiNo ratings yet
- 63c18da748714 Basic Geriatric Nursing 7th Edition Williams Test Bank px8nzf PDFDocument108 pages63c18da748714 Basic Geriatric Nursing 7th Edition Williams Test Bank px8nzf PDFerickomusiq7100% (1)
- Disorders of Parathyroid GlandsDocument52 pagesDisorders of Parathyroid GlandsDr. Akash GuptaNo ratings yet
- CheatsheetsDocument2 pagesCheatsheetsprosie392No ratings yet
- SCP Infection ControlDocument7 pagesSCP Infection ControlNoreen PunjwaniNo ratings yet
- Belize Medical Fitness CertificateDocument2 pagesBelize Medical Fitness CertificateSea BlackNo ratings yet
- OceanofPDF - Com Why Charlie Brown Why - Charles M SchulzDocument70 pagesOceanofPDF - Com Why Charlie Brown Why - Charles M SchulzKarabo LetsholoNo ratings yet
- Nursing Worksheet Template 1 1Document2 pagesNursing Worksheet Template 1 1api-651287771No ratings yet
- Flagellates LabDocument4 pagesFlagellates LabWilliam RamirezNo ratings yet
- Large: Primary Adrenocortical Deficiency Pernicious AnemiaDocument28 pagesLarge: Primary Adrenocortical Deficiency Pernicious Anemiawaqasmumtaz12No ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument15 pagesDr. Ali's Uworld Notes For Step 2 CKBoogy WoogyNo ratings yet
- Surgical Treatment of Gastric Cancer Then and NowDocument8 pagesSurgical Treatment of Gastric Cancer Then and NowConstantin BudinNo ratings yet
- Department of Education Division of Leyte Taberna National High SchoolDocument6 pagesDepartment of Education Division of Leyte Taberna National High SchoolSheila May Tapales TabonNo ratings yet
- PESTEL AnalysisDocument7 pagesPESTEL AnalysiszenerdiodeNo ratings yet
- Rs Foreign Body AspirationDocument50 pagesRs Foreign Body AspirationDr.P.NatarajanNo ratings yet
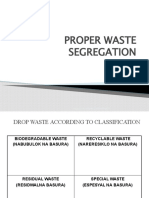
- Solid Waste ManagementDocument40 pagesSolid Waste ManagementMark Jacartny TuyongNo ratings yet
- Full Download PDF of Medical Secrets 6th Edition Mary P. Harward - Ebook PDF All ChapterDocument69 pagesFull Download PDF of Medical Secrets 6th Edition Mary P. Harward - Ebook PDF All Chapterphakhijayahr100% (7)
- Midterm Psych NSG Nclex Test BanksDocument19 pagesMidterm Psych NSG Nclex Test BanksAliza AlyyNo ratings yet
- Varicose Vein - Management, DVT: BY Anandhu Lal Anjali P K AnjusjDocument108 pagesVaricose Vein - Management, DVT: BY Anandhu Lal Anjali P K AnjusjAsif AbbasNo ratings yet
- Eü Szaknyelvi AngolDocument44 pagesEü Szaknyelvi AngolKissné Makai KataNo ratings yet
- Smoking, Mental Illness, and Public Health: FurtherDocument24 pagesSmoking, Mental Illness, and Public Health: FurtherIndriani BaharuddinNo ratings yet
- Minimally Invasive Gynecologic SurgeryDocument25 pagesMinimally Invasive Gynecologic SurgerySamir CastilloNo ratings yet
- DR Suraya Hani Kamsani Paediatrics Dept Hosp SegamatDocument25 pagesDR Suraya Hani Kamsani Paediatrics Dept Hosp Segamatshk229No ratings yet
- Government of Rajasthan Finance Department Rules DivisionDocument2 pagesGovernment of Rajasthan Finance Department Rules DivisionSadanand PariharNo ratings yet
- Werewolf - Curse of The Otolleys BurgerDocument7 pagesWerewolf - Curse of The Otolleys BurgerVictor LewisNo ratings yet
- 10 Penyakit Terbanyak Di Rawat Jalan Di Puskesmas Provinsi Dki Jakarta TW I Tahun 2019Document9 pages10 Penyakit Terbanyak Di Rawat Jalan Di Puskesmas Provinsi Dki Jakarta TW I Tahun 2019Klinik pratama Iqra' medical centreNo ratings yet
- Wound Management in Urgent CareDocument93 pagesWound Management in Urgent CareFahmi RizalNo ratings yet
- Microbiology and ParasitologyDocument55 pagesMicrobiology and ParasitologyJade BuriNo ratings yet