Professional Documents
Culture Documents
10 1017@s1049023x20000345
10 1017@s1049023x20000345
Uploaded by
eder kroeff cardosoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1017@s1049023x20000345
10 1017@s1049023x20000345
Uploaded by
eder kroeff cardosoCopyright:
Available Formats
SPECIAL REPORT
Profile of Chest Injuries and Oxygen Therapy in
Trauma Patients with Acute Respiratory Failure
after the Jiangsu Tornado in China: A Retrospective
Study
Gen hua Mu;1 Zhong qian Lu;1 Xing Li;1 Ping fa Chen;1 Lei He;1 Yun hao Sun;2 Shan shan Hou;3
Yi jun Deng1
Abstract
Note: Mu and Lu contributed equally to the Background: The aim of this study was to analyze the profile of chest injuries, oxygen
work and should be considered co-first authors. therapy for respiratory failure, and the outcomes of victims after the Jiangsu tornado, which
1. Emergency and Critical Care Center, The occurred on June 23, 2016 in Yancheng City, Jiangsu Province, China.
Fourth Affiliated Hospital of Nantong Methods: The clinical records of 144 patients referred to Yancheng City No.1 People’s
University, Yancheng, China Hospital from June 23 through June 25 were retrospectively investigated. Of those patients,
2. Department of Thoracic and Cardiovascular 68 (47.2%) sustained major chest injuries. The demographic details, trauma history, details
Surgery, The Fourth Affiliated Hospital of of injuries and Abbreviated Injury Scores (AIS), therapy for respiratory failure, surgical pro-
Nantong University, Yancheng, China cedures, length of intensive care unit (ICU) and hospital stay, and mortality were analyzed.
3. Pharmacy Department, The Fourth Results: Of the 68 patients, 41 (60.3%) were female and 27 (39.7%) were male. The average
Affiliated Hospital of Nantong University, age of the injured patients was 57.1 years. Forty-six patients (67.6%) suffered from poly-
Yancheng, China trauma. The mean thoracic AIS of the victims was calculated as 2.85 (SD = 0.76). Rib frac-
ture was the most common chest injury, noted in 56 patients (82.4%). Pulmonary contusion
Correspondence: was the next most frequent injury, occurring in 12 patients (17.7%). Ten patients with severe
Gen hua Mu, MD chest trauma were admitted to ICU. The median ICU stay was 11.7 (SD = 8.5) days. Five
Emergency and Critical Care Center patients required intubation and ventilation, one patient was treated with noninvasive
The Fourth Affiliated Hospital of Nantong positive pressure ventilation (NPPV), and four patients were treated with high-flow nasal
University cannula (HFNC). Three patients died during hospitalization. The hospital mortality was
No. 66 Renmin South Road 4.41%.
Yancheng 224005, China Conclusions: Chest trauma was a common type of injury after tornado. The most frequent
E-mail: mugenhua2009@163.com thoracic injuries were rib fractures and pulmonary contusion. Severe chest trauma is usually
associated with a high incidence of respiratory support requirements and a long length of
Co-correspondence: stay in the ICU. Early initiation of appropriate oxygen therapy was vital to restoring normal
Yi jun Deng, MD, PhD respiratory function and saving lives. Going forward, HFNC might be an effective and
E-mail: dengyj2003@163.com well-tolerated therapeutic addition to the management of acute respiratory failure in chest
trauma.
Conflicts of interest/funding: This study was
Mu GH, Lu ZQ, Li X, Chen PF, He L, Sun YH, Hou SS, Deng YJ. Profile of chest
supported by the Medical Technology Deve-
injuries and oxygen therapy in trauma patients with acute respiratory failure after the
lopment Project of Yancheng City, China
(YK2017008). The authors declare that they have
Jiangsu tornado in China: a retrospective study. Prehosp Disaster Med. 2020;00(00):1–6.
no competing interests.
Keywords: acute respiratory failure; chest injury;
oxygen therapy; rib fractures; tornadoes Introduction
An EF4 tornado with hailstones struck the northern part of Yancheng City, Jiangsu
Abbreviations: Province, China at 2:30PM on June 23, 2016. This tornado was one of the largest natural
AIS: Abbreviated Injury Scale disasters to strike mainland China in half a century. The affected area was approximately
ARF: acute respiratory failure 17,000 km2 and more than 1.6 million people were affected, in which the Funing and
CT: computed tomography Sheyang districts were almost destroyed by the tornado. Official records reported that
ED: emergency department 99 people died and 846 were injured, including 152 critically.1 Immediately after the
FiO2: fraction of inspired oxygen
HFNC: high-flow nasal cannula
ICU: intensive care unit Received: August 09, 2019 doi:10.1017/S1049023X20000345
IPPV: invasive positive-pressure ventilation Revised: November 17, 2019 © World Association for Disaster and
NPPV: noninvasive positive pressure ventilation Accepted: November 25, 2019 Emergency Medicine 2020.
PaO2: partial pressure of oxygen
Month 2020 Prehospital and Disaster Medicine
Downloaded from https://www.cambridge.org/core. The University of Reading, on 23 Mar 2020 at 22:53:07, subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms.
https://doi.org/10.1017/S1049023X20000345
2 Chest Injuries after Jiangsu Tornado
tornado, a large number of casualties were sent to the Fourth injuries, and 46 patients (67.6%) suffered from polytrauma. The
Affiliated Hospital of Nantong University (Yancheng, China) mean AIS of the victims with chest injuries was calculated as 2.85
by car and ambulance. This hospital is located approximately (SD = 0.76). There were 16 patients (23.5%) with minor to moder-
50 kilometers away from the disaster area and was not affected ate chest injuries (thoracic AIS = 1, thoracic AIS = 2); 43 patients
by the tornado; it served as the largest back-up hospital in the after- (63.2%) with serious chest injuries (thoracic AIS = 3); eight patients
math of the disaster. (11.8%) with severe injuries (thoracic AIS = 4); and one patient with
It is known that chest injuries cause one of every four trauma critical chest injuries (thoracic AIS = 5). The most common cause of
deaths, and respiratory failure is the most common complication chest injury was flying/falling bricks and wood (24 cases; 35.3%),
associated with chest injuries.2,3 Nevertheless, there are very few followed by falling/tripping during escape (19 cases; 27.9%),
reports on the epidemiology of chest injuries resulting from major collapses of walls or roof (16 cases; 23.5%), and picked up/blown by
tornadoes. To better understand the chest injuries after the tor- tornado (nine cases; 13.2%).
nado, authors analyzed the injury patterns, therapy for respiratory Rib fracture was the most common chest injury and was noted in
failure, surgical procedures, and short-term outcomes in chest- 56 patients (82.4%), including multiple rib fractures (24 patients).
injured patients referred to a back-up hospital. Pulmonary contusion was the next most frequent injury, occurring
in 12 patients (17.7%). Twenty-one patients suffered intrathoracic
Patients and Methods damage, including pneumothorax (nine), hemothorax or hemop-
The present study retrospectively investigated the medical records neumothorax (eight), and mediastinal emphysema or hematoma
of 144 patients admitted to the Fourth Affiliated Hospital of (four). Chest drainage was performed in 11 patients within the first
Nantong University with tornado-related injuries during the first 12 hours. One patient underwent a thoracotomy due to massive
three days after the 2016 Jiangsu tornado. Descriptive statistics thoracic hemorrhage. One patient was diagnosed with a diaphrag-
were used to analyze the demographics, causes of injury, the injury matic rupture and underwent urgent laparotomy and repair of the
patterns, treatments, hospital stays, and prognosis of patients after diaphragm. The profiles of the chest injuries are listed in Table 1.
the tornado. An electronic database with information on tornado-
related injuries from patients admitted to the hospital from June 23 Management of Acute Respiratory Failure
through 25, 2016 was produced based on patient files available at Ten patients with severe chest injuries were admitted to the inten-
the hospital. The research variables were discussed with the medical sive care unit (ICU; Table 2). All subjects with ARF were managed
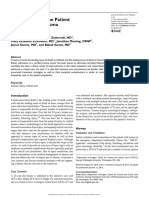
and statistical experts. A data entry manual was developed; the according to protocol (Figure 1). Five of them required intubation
quality of the data entry process was checked by researchers. and ventilation. The first was a 29-year-old woman. She was
Injury diagnoses were attributed following the International injured by a collapsed house and was sent directly from the scene
Classification of Diseases (ICD)-10 (version 2010). All injuries to the emergency department (ED). Multiple rib fractures and a
were classified with respect to the Abbreviated Injury Scale hemothorax were noted. A chest tube was inserted and a massive
(AIS) 2005 and according to their severity. The severity index blood transfusion was given. Massive bleeding with approximately
ranges from one to six, with one being a minor injury and six being 1800mL in the chest bottle was noted upon arrival to the ICU.
maximal injury.4 Of the 144 patients, 68 (47.2%) were diagnosed A thoracotomy was performed immediately. She was successfully
with a major chest injury for further evaluation or surgery. These weaned from ventilation after surgery and was discharged from
patients were examined by two thoracic surgeons. The diagnosis the ICU three days later. The second patient was a 2-year-old girl
of superficial trauma, comprising lacerations and contusions, was who was injured by a collapsing wall. Loss of consciousness was
made from the physical examination. Rib fractures, pneumothorax, noted at the scene. She was transferred to the ED after endotra-
hemothorax, and mediastinal injury were diagnosed from chest cheal intubation in a field hospital. The Glasgow Coma Scale
radiographs, computed tomography (CT) scans, or magnetic res- was E2V1M2. Brain CT revealed a brain contusion, subarachnoid
onance imaging (MRI). The diagnosis of acute respiratory failure hemorrhage, and diffuse brain swelling. A decompressive craniec-
(ARF) was made by a partial pressure of oxygen (PaO2)<60mmHg tomy was performed immediately. However, she died of brain
and/or a partial pressure of carbon dioxide (PaCO2)>50mmHg in herniation 20 hours later. The third patient presenting with hypo-
blood gas analysis. xemia was a 67-year-old man. A chest CT revealed multiple rib
All data collected via medical records were entered into an fractures, pneumothorax, and diaphragmatic rupture. Urgent lapa-
Access database and converted into Excel files (version 2016 rotomy and repair of the diaphragm were undertaken, and blunt
for Windows; Microsoft Inc.; Redmond, Washington USA). hepatic trauma was noted. He was discharged from the ICU seven
Descriptive statistics were calculated for all numerical variables, days later. Another two elderly patients with multiple rib fractures
including the means and standard deviations; percentages were cal- and pulmonary contusions needed intubation and mechanical ven-
culated for all categorical variables. Excel software was used for the tilation for severe hypoxemia. These two patients developed acute
statistical analysis. respiratory distress syndrome (ARDS) and serious complications
The study protocol was approved by the Ethics Committee of during their hospitalization. One died of pneumonia and septic
The Fourth Affiliated Hospital of Nantong University. Due to the shock on day eight, and the other died of multiple organ dysfunc-
retrospective nature of the study, informed consent was waived. tion syndrome (MODS) on day 30.
A 65-year-old woman was diagnosed with multiple rib fractures
Results and hemopneumothorax. Chest tube drainage was performed, and
Profile of Chest Injuries pain management was administered. Subsequently, she was treated
Of the 68 patients, 41 (60.3%) were female and 27 (39.7%) were with noninvasive positive pressure ventilation (NPPV) for moder-
male. The average age of the injured patients was 57.1 years (range ate hypoxemia. The PaO2/fraction of inspired oxygen (FiO2) ratio
two years to 89 years). Twenty-eight (41.2%) patients were aged gradually increased, and she was successfully weaned from NPPV
60 years or older. Twenty-two patients (32.4%) had isolated thoracic eight days later.
Prehospital and Disaster Medicine Vol. 00, No. 00
Downloaded from https://www.cambridge.org/core. The University of Reading, on 23 Mar 2020 at 22:53:07, subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms.
https://doi.org/10.1017/S1049023X20000345
Mu, Lu, Li, et al 3
Type of Injury Number of Percentage
Patients
Rib Fracture 56 82.35
Pulmonary Contusion 12 17.65
Pneumothorax 9 13.24
Clavicle Fracture 8 11.76
Hemothorax or Hemopneumothorax 8 11.76
Mediastinal Emphysema or Hematoma 4 5.88
Sternal Fracture 2 2.94
Diaphragmatic Rupture 1 1.47
Mu © 2020 Prehospital and Disaster Medicine
Table 1. Profile of Chest Injuries in 68 Patients after Tornado, China
Note: It was noted that 58 patients (85.29%) had more than one type of chest injury.
Trauma patient with acute respiratory failure
Need for endotracheal intubation
Yes No
IPPV PaO2 persistently (> 2 hours) <60 mmHg or
SpO2<90% with face mask O2ı10 L/min
No Yes
Pursue HFNC If intolerance NPPV
Face Mask
Clinical improvement and patients could
No persistently achieve PaO2>65 mmHg or
SpO2>92% while breathing oxygen at FiO2
0.60
Yes Yes
Pursue Pursue
HFNC NPPV
Mu © 2020 Prehospital and Disaster Medicine
Figure 1. Oxygen Therapy Protocol of Patients with Acute Respiratory Failure Used in ICU.
Abbreviations: HFNC, high-flow nasal cannula; ICU, intensive care unit; IPPV, invasive positive-pressure ventilation; NPPV,
noninvasive positive pressure ventilation.
There were four patients with mild or moderate hypoxemia hemopneumothorax only seen on CT. A HFNC was introduced
treated with high-flow nasal cannula (HFNC). A 55-year-old at a flow rate of 40L/minute and an FiO2 of 0.8; NPPV was
woman was diagnosed with multiple rib fractures, a pelvic frac- not used due to abdominal distention caused by a retroperitoneal
ture, and lumbar fracture. She presented with breathlessness and hematoma. The PaO2/FiO2 ratio gradually increased, and HFNC
hypoxemia at the ED. The PaO2/FiO2 ratio further deteriorated was discontinued on day 10. A 78-year-old woman with a history
despite the delivery of a maximal dose of oxygen via a nonre- of emphysema was diagnosed with multiple rib fractures and a
breathing face mask. A trial of NPPV was not tolerated. The clavicle fracture. Moderate hypoxemia was noted when she was
patient was treated using HFNC at a flow rate of 50L/minute, transferred to the ED; she was treated with HFNC due to an
with an FiO2 of 0.8; continuous analgesia was administered. intolerance to NPPV. The PaO2/FiO2 ratio gradually increased,
The PaO2/FiO2 ratio increased gradually, and HFNC was and she was discharged from the ICU on day 10. An 82-year-
replaced by oxygen delivery through a nasal cannula on day old man injured by a collapsing wall was diagnosed with multiple
12. A 65-year-old man was thrown by the wind. Multiple rib rib fractures, pulmonary contusions, and facial lacerations.
fractures and hemopneumothorax were noted. The treating clini- The combination of injuries weakened the patient’s ability to
cians did not insert a chest drain due to the small size of the clear secretions, and impaired ventilation and oxygen exchange.
Month 2020 Prehospital and Disaster Medicine
Downloaded from https://www.cambridge.org/core. The University of Reading, on 23 Mar 2020 at 22:53:07, subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms.
https://doi.org/10.1017/S1049023X20000345
4 Chest Injuries after Jiangsu Tornado
Treatment with HFNC was introduced at a flow rate of 40L/minute Mechanical ventilation is an essential means of life support for
with an FiO2 of 0.6. Hypoxemia slowly resolved, and HFNC was patients with respiratory failure caused by chest trauma. The choice
discontinued on day 19. of mechanical ventilation depends on the type of injury and the
The median hospital stay for 68 patients with chest injuries was requirements for further surgery.22 In present study, five of ten
24.88 (SD = 11.5) days (range one to 65): 22.1% of patients were patients with severe chest injuries were treated with invasive
hospitalized for one to 14 days, 44.1% were hospitalized for positive-pressure ventilation (IPPV). However, mechanical venti-
15-28 days, and 33.8% were hospitalized for more than 28 days. lation was a double-edged sword, and there were many complica-
The median ICU stay was 11.7 (SD = 8.5) days (range one to tions while saving lives, including ventilator-induced lung injury
30). Three patients died during hospitalization. The hospital (VILI) and ventilator-associated pneumonia (VAP).23 Ventilation
mortality was 4.41%. in patients after chest trauma is challenging because of the difficulty
in achieving a balance between sufficient ventilation and the avoid-
Discussion ance of further harm to the lungs. The magnitude, location,
The Jiangsu tornado was one of the deadliest tornadoes to occur in and type of lung or chest injury require a gradually adapted therapy
China in half a century. The severity of the tornado caused a large tailored to individual patient needs.
number of tornado-related deaths in China.5,6 After the tornado, a Noninvasive positive pressure ventilation has been increasingly
large number of patients were sent to the hospital within a short used to manage ARF of various etiologies, such as exacerbations of
period of time, placing great demands on medical resources. chronic obstructive pulmonary disease (COPD), cardiogenic pul-
Injuries to the thorax during the tornado were common and monary edema, or chest trauma.24 Gonzalo Hernandez, et al25
presented a major challenge to the emergency medical staff. reported that noninvasive mechanical ventilation can reduce intu-
In the present study, of the 144 trauma patients treated in this bation compared with the oxygen mask in severe thoracic trauma-
hospital, 68 patients (47.2%) sustained chest injuries, compatible related hypoxemia. However, its use should be restricted to patients
with reports by Millie, et al from the 1998 tornado disaster in rural without pneumothorax or mediastinal emphysema, severe abdomi-
Georgia (USA).7 Chest injury is also associated with high morbid- nal distention, or maxillofacial injury.26 In addition, NPPV failure
ity.8,9 Brown, et al8 reported that 18.0% of all trauma deaths involve has been experienced often because of mask intolerance or inad-
a chest injury, making it second only to multiple injuries and head equate cooperation.26 In this study, two of three patients with mod-
injuries in the Oklahoma (USA) tornado in 1999. Rib fractures erate hypoxemia could not tolerate NPPV and were then treated
were the most frequent pathology observed in 82.4% of patients, with HFNC.
and pulmonary contusion was the second most frequent pathology In recent years, HFNC as a new respiratory support therapy has
observed in 33.3% of patients. The incidence of rib fractures in the been introduced, and HFNC can deliver up to 100% humidified
current study was much higher than in previous studies.7-10 The and heated, blended gas at flow rates of up to 60L/minute into
reason can be attributed to a higher proportion of elderly patients the nares. This HFNC therapy can reduce the work of breathing
who are prone to fractures due to osteoporosis and the loss of by decreasing oxygen demands, improving the expectoration of
muscle mass. Bulger, et al11 compared patients who were at least secretions, and recruiting alveoli by supplying a small amount of
65 years old to a matched cohort of 18-to-64-year-olds who sus- positive end expiratory pressure.27 Previous studies demonstrated
tained chest trauma with rib fractures. The elderly group had twice that HFNC therapy was well-tolerated and useful for early oxy-
the mortality and thoracic morbidity. The risk of pneumonia genation during acute hypoxemic respiratory failure.28-30 However,
and respiratory failure increases with age from as young as 45 years there were no previously published clinical studies evaluating its
and particularly over the age of 65 years.12-14 This is likely associ- efficacy and tolerability in the management of chest trauma-related
ated with increased comorbidities and the loss of physical reserves hypoxemia. In reviewing four cases of chest trauma treated with
that is observed in the elderly.15 HFNC, it was found that HFNC could be an effective therapy
In previous reports, 84.0% to 94.0% of rib fracture patients had to patients with chest injuries, and it may be a useful alternative
significant associated injuries.16,17 The most common associated to NPPV in victims with mask intolerance. Nevertheless, whether
thoracic injuries are pneumothorax, hemothorax, and pulmonary HFNC could reduce the requirement for both invasive and non-
contusion.17,18 In the present study, pneumothorax developed in invasive ventilation of patients with thoracic injury needs to be con-
eight patients (13.2%), followed by hemothorax or hemopneumo- firmed by further clinical research.
thorax (11.8%). Consequently, the majority of these patients had to
be treated with tube thoracostomy. It is vital to identify the pres- Study Limitations
ence of a major pneumothorax and/or hemothorax as an urgent The current study has some limitations that are worth noting. This
chest tube may be required to decompress the pleura and improve was a single hospital study, but didn’t include persons treated in
lung inflation.19 local hospital affected by the tornado. Therefore, it is not represen-
Patients with multiple rib fractures or a flail segment have been tative of the total casualties in tornado. In the study, most epi-
shown to have a higher incidence of underlying lung injury.20 The demiological data of patients rely on the medical records, but
combination of chest wall and lung injury significantly reduces pul- detailed medical records of small proportion of hospitalized
monary function, resulting in a higher incidence of patients requir- patients were often incomplete, especially during chaotic disaster
ing respiratory support and a long length of stay in the ICU,21 as conditions. In addition, though the data analysis has been under-
demonstrated in this study. Respiratory function should be sup- taken by a single individual, the patient files were originally regis-
ported with oxygen therapy to treat hypoxia and reduce the work tered by many different doctors. This type of data is very inclined to
of breathing. The amount and type of oxygen therapy needs be individual variation and clinical interpretation bias which is diffi-
selected according to the respiratory status and injury severity of cult to avoid. Finally, case numbers for ARF were small, resulting
the patient. in limited statistical power.
Prehospital and Disaster Medicine Vol. 00, No. 00
Downloaded from https://www.cambridge.org/core. The University of Reading, on 23 Mar 2020 at 22:53:07, subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms.
https://doi.org/10.1017/S1049023X20000345
Mu, Lu, Li, et al 5
Conclusion be learned from the Jiangsu tornado experience that could be used
Chest trauma was a common type of injury and presented a major to improve all levels of performance in future tornado management.
challenge in emergency medical support during the Jiangsu
Authors’ Contributions
tornado. Most patients (67.6%) with chest injuries suffer from
Mu and Lu contributed equally to the work and should be consid-
multiple injury; the most frequent thoracic injuries were fracture
ered co-first authors. Mu, Lu, and Deng contributed substantially to
of the ribs and pulmonary contusion. Severe chest trauma is usually
study conception and design. Mu, Chen, He, and Sun contributed
associated with a high incidence of respiratory support require-
to data acquisition. Lu, Li, and Hou contributed to data analysis and
ments and a long length of stay in the ICU. The clinical assessment
interpretation. Mu drafted the article. Mu, Lu, Li, Chen, and Deng
must be accurate and repeated regularly to determine the needs of
critically revised the manuscript for important intellectual content.
the patient. Early initiation of appropriate oxygen therapy, which
All authors read and approved the final manuscript.
includes IPPV, NPPV, or HFNC, is vital to restore normal respi-
ratory function and save lives. Going forward, HFNC might be Acknowledgments
an effective and well-tolerated therapeutic addition to the manage- The authors thank all participating staff at The Fourth Affiliated
ment of ARF in chest trauma. Therefore, there are many lessons to Hospital of Nantong University for their assistance.
References
1. Lyu HM, Wang GF, Cheng WC, Shen SL. Tornado hazards on June 23 in Jiangsu 16. Sirmali M. A comprehensive analysis of traumatic rib fractures: morbidity, mortality
Province, China: preliminary investigation and analysis. Natural Hazards. and management. Eur J Cardiothorac Surg. 2003;24(1):133–138.
2017;85(1):597–604. 17. Karadayi S, Nadir A, Sahin E, Celik B, Arslan S, Kaptanoglu M. An analysis of 214
2. LoCicero J, Mattox KL. Epidemiology of chest trauma. Surg Clin North Am. cases of rib fractures. Clinics. 2011;66(3):449–451.
1989;69(1):15–19. 18. Novakov I. The incidence of pulmonary contusion in blunt thoracic trauma: self-
3. Veysi VT, Nikolaou VS, Paliobeis C, Efstathopoulos N, Giannoudis PV. Prevalence of experience study. Chest. 2014;145(Suppl 3):47A.
chest trauma, associated injuries and mortality: a level I trauma center experience. 19. Roberts DJ, Leigh-Smith S, Faris PD, et al. Clinical presentation of patients with ten-
International Orthopaedics. 2009;33(5):1425–1433. sion pneumothorax: a systematic review. Annals of Surgery. 2015;261(6):1068–1078.
4. Gennarelli TA, Wodzin E. AIS 2005: a contemporary injury scale. Injury. 20. Battle CE, Evans PA. Predictors of mortality in patients with flail chest: a systematic
2006;37(12):1083–1091. review. Emerg Med J. 2015;32(12):961–965.
5. Deng Q, Lv Y, Xue C, Kang P, Dong J, Zhang L. Pattern and spectrum of tornado 21. Amital A, Shitrit D, Fox BD, et al. Long-term pulmonary function after recovery from
injury and its geographical information system distribution in Yancheng, China: a pulmonary contusion due to blunt chest trauma. Israel Medical Association Journal.
cross-sectional study. BMJ Open. 2018;8(6):e021552. 2009;11(11):673–676.
6. Jia H, Pan D. Tornado disaster impacts and management: learning from the 2016 tor- 22. Richter T, Ragaller M. Ventilation in chest trauma. J Emerg Trauma Shock. 2011;4(2):
nado catastrophe in Jiangsu Province, China. Natural Hazards. 2017;89(1):457–471. 251–259.
7. Millie M, Senkowski C, Stuart L, Davis F, Ochsner G, Boyd C. Tornado disaster in 23. Rico FR, Cheng JD, Gestring ML, Piotrowski ES. Mechanical ventilation strategies
rural Georgia: triage response, injury patterns, lessons learned. Am Surg. 2000;66(3): in massive chest trauma. Crit Care Clinics. 2007;23(2):299–315.
223–228. 24. Duggal A, Perez P, Golan E, Tremblay L, Sinuff T. Safety and efficacy of noninvasive
8. Brown S, Archer P, Kruger E, Mallonee S. Tornado-related deaths and injuries ventilation in patients with blunt chest trauma: a systematic review. Crit Care.
in Oklahoma due to the 3 May 1999 tornadoes. Weather Forecasting. 2002;17(3): 2013;17(4):R142.
343–353. 25. Hernandez G, Fernandez R, Lopez-Reina P, et al. Noninvasive ventilation reduces
9. Daley WR, Brown S, Archer P, et al. Risk of tornado-related death and injury in intubation in chest trauma-related hypoxemia: a randomized clinical trial. Chest.
Oklahoma, May 3, 1999. Am J Epidemiol. 2005;161(12):1144–1150. 2010;137(1):74–80.
10. Niederkrotenthaler T, Parker EM, Ovalle F, et al. Injuries and post-traumatic stress 26. Carron M, Freo U, Zorzi M, Ori C. Predictors of failure of noninvasive ventilation in
following historic tornados: Alabama, April 2011. PLOS One. 2013;8(12):e83038. patients with severe community-acquired pneumonia. J Crit Care. 2010;25(3):540.
11. Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. 27. Nishimura M. High-flow nasal cannula oxygen therapy in adults. J Intensive Care.
J Trauma. 2000;48(6):1040–1046. 2015;3(1):15.
12. Battle C, Hutchings H, Evans PA. Outcomes in older blunt chest wall trauma patients: 28. Papazian L, Corley A, Hess D, et al. Use of high-flow nasal cannula oxygenation in
a retrospective study. Critical Care. 2012;16(Suppl 1):453. ICU adults: a narrative review. Intensive Care Med. 2016;42(9):1336–1349.
13. Holcomb JB, McMullin NR, Kozar RA, Lygas MH, Moore FA. Morbidity from rib 29. Gaunt KA, Spilman SK, Halub ME, Jackson JA, Lamb KD, Sahr SM. High-flow
fractures increases after age 45. J Am Col Surg. 2003;196(4):549–555. nasal cannula in a mixed adult ICU. Respiratory Care. 2015;60(10):1383–1389.
14. Ng S, Seethala R, Yang Y, et al. Risk factors for respiratory failure in elderly patients 30. Simon M, Braune S, Frings D, Wiontzek AK, Klose H, Kluge S. High-flow nasal
with traumatic rib fractures. Crit Care Med. 2012;40(12):53–54. cannula oxygen versus non-invasive ventilation in patients with acute hypoxaemic
15. Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at respiratory failure undergoing flexible bronchoscopy–a prospective randomized trial.
greater risk of death and pneumonia. J Trauma. 2003;54(3):478–485. Crit Care. 2014;18(6):712.
Month 2020 Prehospital and Disaster Medicine
Downloaded from https://www.cambridge.org/core. The University of Reading, on 23 Mar 2020 at 22:53:07, subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms.
https://doi.org/10.1017/S1049023X20000345
https://doi.org/10.1017/S1049023X20000345
Downloaded from https://www.cambridge.org/core. The University of Reading, on 23 Mar 2020 at 22:53:07, subject to the Cambridge Core terms of use, available at https://www.cambridge.org/core/terms.
Prehospital and Disaster Medicine
6
Patient Sex/Age Chest Injuries Associated Injuries Emergency Operations Oxygen ICU Stay (d) Result
Therapy
1 Female/29 Multiple rib fractures, Clavicle Fracture of right fibula Exploratory thoracotomy IPPV 3 Alive
fracture, Hemothorax
2 Female/2 Pulmonary contusion Severe craniocerebral injury Decompressive craniectomy IPPV 1 Dead
3 Male/67 Multiple rib fractures, Hepatic blunt trauma Repair of diaphragm IPPV 7 Alive
Pneumothorax, Pulmonary
contusion, Diaphragmatic
rupture
4 Female/87 Multiple rib fractures, Pulmonary Upper limb injury, Lumbar Thoracic closed drainage IPPV 30 Dead
contusion, Clavicle fracture fracture
5 Male/71 Multiple rib fractures, Pulmonary Thoracic vertebral fracture IPPV 8 Dead
contusion
6 Female/65 Multiple rib fractures, Skull fracture, Radius/Femoral Thoracic closed drainage NPPV 17 Alive
Hemopneumothorax fractures
7 Female/55 Multiple rib fractures Pelvic fracture, Lumbar fracture HFNC 12 Alive
8 Female/65 Multiple rib fractures, Retroperitoneal hematoma HFNC 10 Alive
Hemopneumothorax
9 Female/78 Multiple rib fractures, Clavicle Eyelid trauma, Lumbar/ Upper HFNC 10 Alive
fracture limb fractures
10 Male/82 Multiple rib fractures, Pulmonary Facial laceration, Femoral HFNC 19 Alive
contusion fracture
Mu © 2020 Prehospital and Disaster Medicine
Chest Injuries after Jiangsu Tornado
Table 2. Details of 10 Patients Admitted to the Intensive Care Unit
Abbreviations: HFNC, high-flow nasal cannula; IPPV, invasive positive-pressure ventilation; NPPV, noninvasive positive pressure ventilation.
Vol. 00, No. 00
You might also like
- Katherine Byrne, Tuberculosis and The Victorian: Literary ImaginationDocument5 pagesKatherine Byrne, Tuberculosis and The Victorian: Literary ImaginationMaria Eliza GiuboruncaNo ratings yet
- Winters PreviewDocument265 pagesWinters PreviewcqpresscustomNo ratings yet
- InstallationDirective C13 IvecoDocument60 pagesInstallationDirective C13 Ivecoblaktion0% (1)
- Traumatic Diaphragmatic Hernia Anaesthetic ConsideDocument3 pagesTraumatic Diaphragmatic Hernia Anaesthetic ConsideHalim SudonoNo ratings yet
- Pulmonary Contusion in Mechanically Ventilated Subjects After Severe TraumaDocument5 pagesPulmonary Contusion in Mechanically Ventilated Subjects After Severe TraumaFauzan KurniawanNo ratings yet
- 2016 Bilateral Subpectoral Interfascial Plane Catheters For Analgesia For Sternal Fractures A Case ReportDocument3 pages2016 Bilateral Subpectoral Interfascial Plane Catheters For Analgesia For Sternal Fractures A Case ReportDaniela Alejandra Bravo RomeroNo ratings yet
- Fernandez Bustamante2016Document10 pagesFernandez Bustamante2016Has HurNo ratings yet
- 1 s2.0 S000709122200366X MainDocument12 pages1 s2.0 S000709122200366X MainTlally Itzel Zamora CastroNo ratings yet
- Wiring CostaDocument4 pagesWiring CostaKulo YitnoNo ratings yet
- Huge Mediastinal Ancient Schwannoma Causing AcuteDocument6 pagesHuge Mediastinal Ancient Schwannoma Causing AcuteBarbara SouzaNo ratings yet
- Daniel Pramandana Lumunon, Raihanita Zahra: ReferensiDocument1 pageDaniel Pramandana Lumunon, Raihanita Zahra: Referensiabdul hamidNo ratings yet
- Towards Prevention of Acute Lung Injury: Frequency and Outcomes of Emergency Department Patients At-Risk - A Multicenter Cohort StudyDocument12 pagesTowards Prevention of Acute Lung Injury: Frequency and Outcomes of Emergency Department Patients At-Risk - A Multicenter Cohort StudysiputamaliaputriNo ratings yet
- 2022-10# (PEERJ) RR in ECMODocument17 pages2022-10# (PEERJ) RR in ECMOjycntuNo ratings yet
- Jurnal Flail Chest.Document6 pagesJurnal Flail Chest.Dessy Christiani Part IINo ratings yet
- 2020 Neuropsicología de Las AfasiasDocument17 pages2020 Neuropsicología de Las AfasiasConsuelo SepulvedaNo ratings yet
- Difficult Intubation and Anesthetic Management in An Adult Patient With Undiagnosed Congenital Tracheal Stenosis: A Case ReportDocument6 pagesDifficult Intubation and Anesthetic Management in An Adult Patient With Undiagnosed Congenital Tracheal Stenosis: A Case ReportBianca CaterinalisendraNo ratings yet
- Dsi Vs Rsi in TraumaDocument7 pagesDsi Vs Rsi in TraumaAbhi JeetNo ratings yet
- 頸椎損傷患者之呼吸照護經驗Document8 pages頸椎損傷患者之呼吸照護經驗s0874057物治系No ratings yet
- Stroke Severity Versus Dysphagia Screen As Driver For Post-Stroke PneumoniaDocument7 pagesStroke Severity Versus Dysphagia Screen As Driver For Post-Stroke PneumoniaAnonymous nhN9Gr4No ratings yet
- Burns 3: Pathophysiology, Research Challenges, and Clinical Management of Smoke Inhalation InjuryDocument10 pagesBurns 3: Pathophysiology, Research Challenges, and Clinical Management of Smoke Inhalation InjuryEduardo ChanonaNo ratings yet
- Impact On Survival On Interval Between Surgery andDocument10 pagesImpact On Survival On Interval Between Surgery andZamekile LukheleNo ratings yet
- Post-Extubation Dysphagia: The Truth Is Hard To SwallowDocument2 pagesPost-Extubation Dysphagia: The Truth Is Hard To SwallowRaka dewiNo ratings yet
- Prone Position in Management of COVID-19 Patients A CommentaryDocument3 pagesProne Position in Management of COVID-19 Patients A CommentaryJoseLuisNo ratings yet
- Bag-Mask Ventilation During Tracheal Intubation of Critically Ill AdultsDocument11 pagesBag-Mask Ventilation During Tracheal Intubation of Critically Ill AdultsRitmaNo ratings yet
- BMJ Open 2015 ZhangDocument10 pagesBMJ Open 2015 ZhangLuis CordovaNo ratings yet
- NehshebajakaDocument14 pagesNehshebajakanuraenikhasanah98No ratings yet
- Rib Fixation Who What WhenDocument5 pagesRib Fixation Who What Whenfatimah putriNo ratings yet
- J Nucl Med 2018 Kim 543Document2 pagesJ Nucl Med 2018 Kim 543nabilaoctafNo ratings yet
- Jurnal KMB Diva - 015Document10 pagesJurnal KMB Diva - 015Setiaty PandiaNo ratings yet
- RETIC StudyDocument14 pagesRETIC StudyHelena GomesNo ratings yet
- MC Sparr On 2016Document10 pagesMC Sparr On 2016Matias FlammNo ratings yet
- Spontaneous Breathing During Mechanical Ventilation: A Two-Edged SwordDocument2 pagesSpontaneous Breathing During Mechanical Ventilation: A Two-Edged SwordKhanh Ha NguyenNo ratings yet
- J Bjoms 2019 12 008Document5 pagesJ Bjoms 2019 12 008Muhammad Abdul GhonyNo ratings yet
- Blunt Bronchial InjuriesDocument3 pagesBlunt Bronchial InjuriesaizatamlikhaNo ratings yet
- Jurnal THT Kea 3Document5 pagesJurnal THT Kea 3RiaNo ratings yet
- Medi 98 E18430Document2 pagesMedi 98 E18430Anonymous tG35SYROzENo ratings yet
- The Effect of The Duration of Pre-Oxygenation Before Endotracheal Suction On Hemodynamic SymptomsDocument7 pagesThe Effect of The Duration of Pre-Oxygenation Before Endotracheal Suction On Hemodynamic SymptomsnurharyantidarmaningtyasNo ratings yet
- Regional Versus General Anesthesia in Surgical Patients With Chronic Obstructive Pulmonary Disease: Does Avoiding General Anesthesia Reduce The Risk of Postoperative Complications?Document8 pagesRegional Versus General Anesthesia in Surgical Patients With Chronic Obstructive Pulmonary Disease: Does Avoiding General Anesthesia Reduce The Risk of Postoperative Complications?mluthfidunandNo ratings yet
- Jurnal 3Document8 pagesJurnal 3WIANI FITRINo ratings yet
- Jurnal 2Document3 pagesJurnal 2zahroNo ratings yet
- Assessment of Postoperative Anaesthetic Incidents in The Recovery RoomDocument5 pagesAssessment of Postoperative Anaesthetic Incidents in The Recovery RoomIJAR JOURNALNo ratings yet
- 1 s2.0 S1053077022009168 MainDocument8 pages1 s2.0 S1053077022009168 MainOttofianus Alvedo Hewick KalangiNo ratings yet
- Management of Pneumothorax in Emergency Medicine Departments: Multicenter TrialDocument6 pagesManagement of Pneumothorax in Emergency Medicine Departments: Multicenter TrialYuliana WiralestariNo ratings yet
- Penetrating Chest Trauma With Massive Hemothorax by A Small StoneDocument2 pagesPenetrating Chest Trauma With Massive Hemothorax by A Small Stoneputri firda erlinaNo ratings yet
- Acute Injuries of The Trachea and Major BronchiDocument1 pageAcute Injuries of The Trachea and Major BronchiaryopraditoNo ratings yet
- NPPEDocument8 pagesNPPEjijocasoNo ratings yet
- Damage Control Management y Polytrauma PatientDocument324 pagesDamage Control Management y Polytrauma PatientMauri ParadedaNo ratings yet
- Transverse Striation Needling For 30 Cases of Cervical SpondylosisDocument5 pagesTransverse Striation Needling For 30 Cases of Cervical SpondylosisMamdouh ASNo ratings yet
- Zias2008 Article PostTracheostomyAndPostIntubatDocument9 pagesZias2008 Article PostTracheostomyAndPostIntubatcar19No ratings yet
- Rehabilitacion Pulmonar en La UciDocument19 pagesRehabilitacion Pulmonar en La UcimavhelllinaNo ratings yet
- Late Stabilization Surgery in Flail Chest and Pulmonary ContusionDocument3 pagesLate Stabilization Surgery in Flail Chest and Pulmonary ContusionSukma PranataNo ratings yet
- Critical Care For The Patient With Multiple TraumaDocument12 pagesCritical Care For The Patient With Multiple TraumaSyifa Aulia AzizNo ratings yet
- Operative Stabilization of Flail Chest Injuries: Review of Literature and Fixation OptionsDocument7 pagesOperative Stabilization of Flail Chest Injuries: Review of Literature and Fixation OptionsTommysNo ratings yet
- P Nemo ThorakDocument5 pagesP Nemo ThoraklukmanNo ratings yet
- Treatment of Benign Tracheal Stenosis Using Endoluminal Spray CryotherapyDocument6 pagesTreatment of Benign Tracheal Stenosis Using Endoluminal Spray CryotherapyVania Dwi AndhaniNo ratings yet
- Fraktur FemurDocument11 pagesFraktur FemurYusuf BrilliantNo ratings yet
- Early Intervention Can Improve Clinical Outcome of Acute Interstitial PneumoniaDocument9 pagesEarly Intervention Can Improve Clinical Outcome of Acute Interstitial PneumoniaHerbert Baquerizo VargasNo ratings yet
- 19 (3.6)Document13 pages19 (3.6)JOHAN STEVEN COSME ARANZAZUNo ratings yet
- 325 FullDocument5 pages325 FullDuolingo Leal CarreroNo ratings yet
- AtelectasiaDocument9 pagesAtelectasiapattoxoxoNo ratings yet
- Effect of Endobronchial Coils Vs Usual Care On Exercise Tolerance in Patients With Severe Emphysema The RENEW Randomized Clinical TrialDocument12 pagesEffect of Endobronchial Coils Vs Usual Care On Exercise Tolerance in Patients With Severe Emphysema The RENEW Randomized Clinical TrialCésarNo ratings yet
- Intermediate Care Units and Their Role in Medical WardsDocument2 pagesIntermediate Care Units and Their Role in Medical WardsJHNo ratings yet
- From Thoracic Surgery to Interventional Pulmonology: A Clinical GuideFrom EverandFrom Thoracic Surgery to Interventional Pulmonology: A Clinical GuideJ. Francis Turner, Jr.No ratings yet
- Visvesvaraya Technological University, BELGAUM-590 014: "Online Movie Ticket Management System"Document53 pagesVisvesvaraya Technological University, BELGAUM-590 014: "Online Movie Ticket Management System"Ashutosh pandeyNo ratings yet
- SyntaxDocument9 pagesSyntaxVeronicaTurtusanNo ratings yet
- TOS JRMSU 2nd SemDocument24 pagesTOS JRMSU 2nd SemCris Ann PausanosNo ratings yet
- Art AppreciationDocument10 pagesArt AppreciationJasmine EnriquezNo ratings yet
- Bluetooth Car Using ArduinoDocument13 pagesBluetooth Car Using ArduinoRainy Thakur100% (1)
- Table of Specifications Grade 5Document3 pagesTable of Specifications Grade 5rene balayoNo ratings yet
- Fire Catalog Alco-LiteDocument14 pagesFire Catalog Alco-LiteForum PompieriiNo ratings yet
- Cronin 1992Document15 pagesCronin 1992Marcela GonzálezNo ratings yet
- ACC 30 Research PaperDocument29 pagesACC 30 Research PaperPat RiveraNo ratings yet
- UGEB2362 Course Outline 2023-24Document5 pagesUGEB2362 Course Outline 2023-24Suki PunNo ratings yet
- A) JU4H UF14Document54 pagesA) JU4H UF14Eric Ruiz Lopez50% (2)
- Data Flow DiagramsDocument3 pagesData Flow DiagramsHaco Chinedu ObasiNo ratings yet
- Review of Related LiteratureDocument4 pagesReview of Related Literatureimmanuel AciertoNo ratings yet
- Diesel Engine Crankshaft DisassemblyDocument15 pagesDiesel Engine Crankshaft DisassemblyAnshar NaraNo ratings yet
- Full Data AnalysisDocument627 pagesFull Data AnalysisMyMinecrafter97No ratings yet
- AP06-EV04 - Taller en Idioma Inglés Sobre Sistema de Distribución.Document8 pagesAP06-EV04 - Taller en Idioma Inglés Sobre Sistema de Distribución.juanze rodriguezNo ratings yet
- Case Study 3 Cynar Plastics To Fuel FINALDocument8 pagesCase Study 3 Cynar Plastics To Fuel FINALtalhaNo ratings yet
- Designing Steam Reformers For Hydrogen Production: Keep These Important Factors in Mind When Designing, Revamping or TroubleshootingDocument7 pagesDesigning Steam Reformers For Hydrogen Production: Keep These Important Factors in Mind When Designing, Revamping or TroubleshootingdjinxdNo ratings yet
- Class XII Applied Mathematics 2023-24 (K R Mangalam School)Document7 pagesClass XII Applied Mathematics 2023-24 (K R Mangalam School)GouriJayanNo ratings yet
- Module 2 Year 4Document16 pagesModule 2 Year 4mioraffandyNo ratings yet
- People Vs OandasanDocument2 pagesPeople Vs OandasanAdoha Lei T Blanco100% (1)
- Metric System Common Measure Conversion Factor Common UseDocument4 pagesMetric System Common Measure Conversion Factor Common UseMarielle ChuaNo ratings yet
- Neonatal Questions and Controversies Neurology 4th Edition Perlman Jeffrey M Inder Terrie Jeffrey M Perlman Terrie InderDocument70 pagesNeonatal Questions and Controversies Neurology 4th Edition Perlman Jeffrey M Inder Terrie Jeffrey M Perlman Terrie Inderclaude.moore690100% (12)
- Page 5 of 48: Assignment On Garment Manufacturing - Quality Control PDFDocument50 pagesPage 5 of 48: Assignment On Garment Manufacturing - Quality Control PDFShivangi RajouriyaNo ratings yet
- IBPS Clerk Prelims Maha Mock-2 QuestionsDocument24 pagesIBPS Clerk Prelims Maha Mock-2 Questionsfoxunderfire0% (1)
- Volume Kerja English Year 4Document6 pagesVolume Kerja English Year 4kamiliamawaddahNo ratings yet
- Drug StudyDocument7 pagesDrug StudydivineNo ratings yet