Professional Documents
Culture Documents
Transient Loss of Consciousness in Adults and Young People
Transient Loss of Consciousness in Adults and Young People
Uploaded by
Azka SamalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Transient Loss of Consciousness in Adults and Young People
Transient Loss of Consciousness in Adults and Young People
Uploaded by
Azka SamalCopyright:
Available Formats
G Rogers and N O’Flynn
NICE guideline:
transient loss of consciousness
(blackouts) in adults and young people
Greg Rogers and Norma O’Flynn
INTRODUCTION GUIDANCE
Transient loss of consciousness (TLoC) is loss of Initial assessment
consciousness with complete recovery. It is commonly The guidance most relevant to GPs is likely to
described by the patient as a blackout. TLoC is very concern those areas related to initial assessment in
common and people who experience it may present to order to determine whether the person has had TLoC,
GPs during surgery hours or out of hours, or they may the possible causes of it, and the appropriate next
be referred from the ambulance services or the steps.
emergency department. There are a number of
potential causes of TLoC: History. Ask the person who has had the suspected
TLoC, as well as any witnesses, to describe what
• uncomplicated faint or situational syncope; happened before, during, and after the event. Try to
• orthostatic hypotension; contact, by telephone, any witnesses who are not
• dysfunction of the nervous system (epilepsy); present at the consultation. Record details about:
• dysfunction of the cardiovascular system
(syncope); or • circumstances of the event;
• dysfunction of the psyche (psychogenic attacks). • person’s posture immediately before TLoC;
• presence or absence of any prodromal symptoms
The diagnosis of the underlying cause is often (such as sweating or feeling warm/hot) and
inaccurate, inefficient, and delayed, and movement during event (for example, jerking of the
misdiagnosis is common. NICE guideline CG1091 limbs and duration);
aims to define the appropriate pathways for the • appearance (for example, whether eyes were open
assessment of patients who experience TLoC, in or shut) and colour of the person during the event;
order to obtain the correct underlying diagnosis • any biting of the tongue (record whether the side or
quickly, efficiently, and cost-effectively, and to tailor a the tip of the tongue was bitten);
management plan to suit their true diagnosis. The • injury occurring during the event (record site
guideline includes advice on the management of and severity);
uncomplicated faint/situational syncope and • duration of the event (onset to regaining
orthostatic hypotension, as well as on detailed consciousness);
testing and assessment of those people considered • presence or absence during the recovery period of
to have a cardiovascular cause for their TLoC. confusion or weakness down one side; and
• current medication that may have contributed to
G Rogers, MSc, FRCGP, GP, The Bethesda Medical Centre, TLoC (for example, diuretics).
Margate. N O’FLynn, PhD, MRCGP, clinical director,
National Clinical Guideline Centre for Acute and Chronic Ask also about details of any previous TLoC,
Conditions, Royal College of Physicians, London.
including number of episodes and frequency, as well as
Address for correspondence the person’s medical history and any family history of
Dr Norma O’Flynn, National Clinical Guideline Centre for cardiac disease (for example, personal history of heart
Acute and Chronic Conditions, Royal College of Physicians, disease and family history of sudden cardiac death).
11 St Andrews Place, Regents Park, London NW1 4LE.
E-mail: norma.oflynn@rcplondon.ac.uk
Examination. Perform examination as clinically
Submitted: 3 September 2010; indicated. For example:
final acceptance: 7 September 2010.
• check and record vital signs (such as pulse rate,
©British Journal of General Practice 2011; 61: 40–42. respiratory rate, and temperature) and lying and
standing blood pressure, if clinically appropriate;
DOI: 10.3399/bjgp11X548965
• examine for other cardiovascular and neurological
40 British Journal of General Practice, January 2011
NICE Guideline
signs, such as cardiac murmurs or neurological
Box 1. Electrocardiogram ‘red flags’ that should prompt
deficit, where relevant. specialist cardiovascular assessment within 24 hours.
Electrocardiogram. It is recommended that everyone • Inappropriate persistent bradycardia
has a 12-lead electrocardiogram (ECG) recorded using • Any ventricular arrhythmia (including ventricular ectopic beats)
automated interpretation. If any of the following • Long QT (corrected QT >450 ms) and short QT (corrected QT <350 ms)
abnormalities are present, referral within 24 hours for intervals
specialist cardiovascular assessment is recommended: • Brugada syndromea
• Ventricular pre-excitation (part of Wolff-Parkinson-White syndrome)
• conduction abnormality (for example, complete • Left or right ventricular hypertrophy
right- or left-bundle branch block or any degree of • Abnormal T wave inversion
heart block); • Pathological Q waves
• evidence of delayed atrioventricular conduction,
• Atrial arrhythmia (sustained)
including bundle branch block;
• Paced rhythm
• evidence of a long or short QT interval; or a
An inherited ion channel disorder, characterised by abnormal ST segment elevation in leads
• any ST segment or T wave abnormalities.
V1 to V3 on electrocardiogram. This predisposes the individual to ventricular arrhythmia and
sudden cardiac death and may present with syncope.
If an automated ECG is not available, an ECG needs
to be taken and interpreted by a trained and competent
health professional who can identify the ‘red flags’ • unusual posturing;
listed in Box 1. • prolonged jerking of limbs (note that brief
The possibility of underlying problems that are either seizure-like activity can often occur during
causing or contributing to TLoC should not be uncomplicated faints);
forgotten; relevant examinations and investigations • confusion following the event;
may be required (for example, into blood glucose or • prodromal déjà vu (whereby an unfamiliar situation
haemoglobin levels). feels familiar or is recognised) or jamais vu (whereby
a familiar situation feels totally unfamiliar or is not
Differential diagnosis and management recognised).
Cardiological causes. TLoC can occur due to an
underlying cardiological problem. Referral for The episode may not be related to epilepsy if any of
cardiovascular assessment within 24 hours is the following features are present:
recommended if any of the following apply:
• prodromal symptoms that, on other occasions, have
• an ECG abnormality; been abolished by sitting or lying down;
• heart failure (history or physical signs); • sweating before the episode or pallor during the
• TLoC occurs during exertion; episode; or
• family history of sudden cardiac death in people aged • prolonged standing that appeared to precipitate the
<40 years and/or an inherited cardiac condition; TLoC.
• new or unexplained breathlessness;
• a heart murmur. Uncomplicated faint, situational syncope, and
orthostatic hypotension. Uncomplicated faint
TLoC occurring during exercise indicates that a (uncomplicated vasovagal syncope) should be
cardiac arrhythmic cause is probable; it should be diagnosed when there are no features that suggest an
distinguished from TLoC that occurs shortly after alternative diagnosis (note that brief seizure activity can
stopping exercise, when a vasovagal cause is more occur during uncomplicated faints and is not
likely. necessarily diagnostic of epilepsy). Features
suggestive of uncomplicated faint include:
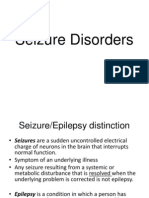
Epilepsy. People who present with features that are
strongly suggestive of epileptic seizures will require • posture (prolonged standing or similar episodes that
referral to a specialist in epilepsy. Features to note are: have been prevented by lying down);
• provoking factors (such as pain or a medical
• a bitten tongue; procedure); and
• head turning to one side during TLoC; • prodromal symptoms (such as sweating or feeling
• no memory of abnormal behaviour that was warm/hot before TLoC).
witnessed before, during, or after TLoC by
someone else; These are known as ‘the three Ps’.
British Journal of General Practice, January 2011 41
G Rogers and N O’Flynn
Situational syncope should be diagnosed when there • For people with suspected carotid sinus syncope
are no features from the initial assessment that suggest and for those with unexplained syncope who are
an alternative diagnosis and syncope is clearly and aged ≥60 years, carotid sinus massage is the first-
consistently provoked by straining during micturition line investigation.
(usually while standing) or by coughing or swallowing. • For people with suspected vasovagal syncope for
If a diagnosis of uncomplicated faint or situational whom recurrent episodes of TLoC adversely affect
syncope is made, no further immediate management is their quality of life or represent a high risk of injury, a
required. The mechanism of the syncope, possible tilt test is recommended. This will assess whether
triggers, and avoidance strategies should be discussed the syncope is accompanied by a severe
and patients reassured. The guideline recommends cardioinhibitory response (usually asystole).
that if the presentation is not to the GP, a copy of the • An ambulatory ECG is recommended for all people
patient report form and the ECG record should be taken with unexplained syncope (including after negative
to the GP or sent to the GP. If an ECG has not been carotid sinus massage test in those for whom this is
recorded, the GP should arrange one within 3 days. appropriate). A tilt test is not recommended before
Orthostatic hypotension should be suspected on the ambulatory ECG.
basis of the initial assessment when there are no
features suggesting an alternative diagnosis and the Appropriate advice for people who experience TLoC
history is typical. If these criteria are met, measure the is also included in the guidance. This involves advising
patient’s lying and standing blood pressure (with them that they must not drive while waiting for a
repeated measurements while standing for 3 minutes). specialist assessment and explaining the fact that they
If clinical measurements do not confirm orthostatic will need to report to the Driver and Vehicle Licensing
hypotension despite a suggestive history, refer the Agency following diagnosis. Consideration of safety at
person for further specialist cardiovascular work may also be required. In addition, patients should
assessment. If orthostatic hypotension is confirmed, be told what to do if they have another event before
likely causes or contributing factors, such as diuretics, assessment is completed.
should be considered.
CONCLUSION
Further assessment and referral From a general practice perspective, the
The outcome from the initial assessment will be that all recommendation that all people who have a TLoC
people with TLoC who do not have a firm diagnosis of episode should have an ECG is likely to be the biggest
uncomplicated faint, situational syncope, orthostatic change from current practice. The recommendation
hypotension, or symptoms suggestive of epilepsy that an automated ECG should be carried out is based
should have a specialist cardiovascular assessment by on evidence assessing automated interpretation
the most appropriate local service. The aim is to versus clinician-read ECGs, and evidence that
categorise the TLoC as either caused by suspected clinicians who were not regularly interpreting ECG
structural heart disease, suspected cardiac arrhythmia, traces were likely to be less accurate than those who
suspected neurally mediated, or unexplained. Specific were experienced in this interpretation. Details of the
guidance is given as to appropriate further evidence, together with discussions of the guideline
investigation, depending on the suspected cause. The development group, can be found in the full guideline.
following tests are likely during specialist assessment:
Funding body
This work was undertaken by the National Clinical Guideline
• An ambulatory ECG is required to diagnose a Centre for Acute and Chronic Conditions, which received
suspected cardiac arrhythmia. The type chosen will funding from the National Institute for Health and Clinical
Excellence (NICE). The views expressed in this publication are
depend, in particular, on the frequency of TLoC and those of the authors and not necessarily those of NICE.
will require, for example, 24- or 48-hour monitoring Competing interests
or external or implantable event recorders. Greg Rogers is a GP and was a member of the guideline
• People with structural heart disease may have development group that formulated the guidance. Norma
O’Flynn is clinical director at the National Clinical Guideline
several mechanisms for syncope and so should have Centre (NCGC) where the guideline was developed. The
investigations for arrhythmia, as well as NCGC is funded by NICE.
consideration of orthostatic hypotension and neurally Discuss this article
Contribute and read comments about this article on the
medicating syncope, in addition to cardiac imaging. Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
• TLoC during exercise requires urgent (within
7 days) exercise testing, unless there is a possible REFERENCE
1. National Institute for Health and Clinical Excellence. Transient loss of
contraindication (such as suspected aortic stenosis consciousness (‘blackouts’) management in adults and young people. NICE
or hypertrophic cardiomyopathy). The patient should clinical guideline 109. London: NICE, 2010.
http://guidance.nice.org.uk/CG109/NICEGuidance/pdf/English (accessed
refrain from exercise until further assessment. 29 Nov 2010).
42 British Journal of General Practice, January 2011
You might also like
- Closed Legal MemoDocument8 pagesClosed Legal Memogaming accountNo ratings yet
- Top Tung Acupuncture Points (PDFDrive)Document28 pagesTop Tung Acupuncture Points (PDFDrive)shaukijameel50% (4)
- Status Epilepticus: MD Neurologist, Epilepsy and General Neurology, Comprehensive Epilepsy ProgramDocument28 pagesStatus Epilepticus: MD Neurologist, Epilepsy and General Neurology, Comprehensive Epilepsy ProgramHayley JuniorNo ratings yet
- Syncope in Adults - Clinical Manifestations and Initial Diagnostic Evaluation - UpToDateDocument21 pagesSyncope in Adults - Clinical Manifestations and Initial Diagnostic Evaluation - UpToDateBruno FernandesNo ratings yet
- Yncope Earning Bjectives: EfinitionDocument5 pagesYncope Earning Bjectives: EfinitionmuhammadridhwanNo ratings yet
- Syncope - Approach To The Patient Dynamed 2020 PDFDocument76 pagesSyncope - Approach To The Patient Dynamed 2020 PDFHeriberto Moreno HernandezNo ratings yet
- TIA NeneDocument13 pagesTIA NenekenNo ratings yet
- Syncope 3Document19 pagesSyncope 3Pratyush PrateekNo ratings yet
- Acute Stroke Management by Carlos L Chua PDFDocument61 pagesAcute Stroke Management by Carlos L Chua PDFHynne Jhea EchavezNo ratings yet
- SyncopeDocument14 pagesSyncopemaithamNo ratings yet
- Fainting and Blacking Out (Near-Syncope and Syncope) .: - o o o o o o oDocument3 pagesFainting and Blacking Out (Near-Syncope and Syncope) .: - o o o o o o oLILY MAINNo ratings yet
- EpilepsyDocument41 pagesEpilepsyaboubakarylwabukobaNo ratings yet
- Neurological EmergenciesDocument11 pagesNeurological Emergenciespunit lakraNo ratings yet
- Acute Ischemic StrokeDocument44 pagesAcute Ischemic Strokext202003495No ratings yet
- Syncope:: Definition, Epidemiology, and ClassificationDocument5 pagesSyncope:: Definition, Epidemiology, and Classificationangela_karenina_1No ratings yet
- Long QT Syndrome: Diagnosis and Management: BackgroundDocument8 pagesLong QT Syndrome: Diagnosis and Management: BackgroundArizkie AlfiNo ratings yet
- ENLS Sub-Arachnoid Hemorrhage ProtocolDocument22 pagesENLS Sub-Arachnoid Hemorrhage ProtocolFransiskus MikaelNo ratings yet
- SyncopeDocument78 pagesSyncopeDiego BaghinoNo ratings yet
- Emergency Presentation of Neurosurgical ConditionsDocument5 pagesEmergency Presentation of Neurosurgical ConditionsMuhammad Azhary LazuardyNo ratings yet
- Epilepsy/Seizure: Presented by Mirjana Milutinovic, M.D. Professor SJSMDocument47 pagesEpilepsy/Seizure: Presented by Mirjana Milutinovic, M.D. Professor SJSMAbanoub AwadallaNo ratings yet
- Tremors in Primary CareDocument67 pagesTremors in Primary CareAmir MahmoudNo ratings yet
- Podział Diagnostyka PDFDocument9 pagesPodział Diagnostyka PDFMagda KupczyńskaNo ratings yet
- Essential Tremor - Practice Essentials, Background, EtiologyDocument6 pagesEssential Tremor - Practice Essentials, Background, EtiologydilaNo ratings yet
- Chapter 40 - SyncopeDocument8 pagesChapter 40 - SyncopeJonalyn MejellanoNo ratings yet
- Guide To ECT 2015Document25 pagesGuide To ECT 2015Diana CalderónNo ratings yet
- Chapter 23the Multiply & Severely Injured PatientDocument19 pagesChapter 23the Multiply & Severely Injured PatientWahyuNo ratings yet
- Syncope: UCI Internal Medicine Core Curriculum - Mini LectureDocument15 pagesSyncope: UCI Internal Medicine Core Curriculum - Mini LecturechandanNo ratings yet
- Syncope in Adults - Clinical Manifestations and Initial Diagnostic EvaluationDocument26 pagesSyncope in Adults - Clinical Manifestations and Initial Diagnostic EvaluationRaúl MartínezNo ratings yet
- Transient Ischemic Attacks: Part I. Diagnosis and EvaluationDocument10 pagesTransient Ischemic Attacks: Part I. Diagnosis and EvaluationAndi SaputraNo ratings yet
- Seizure DisordersDocument26 pagesSeizure DisordersMolly NguyenNo ratings yet
- Enls V 4 0 Protocol Coma FinalDocument16 pagesEnls V 4 0 Protocol Coma Finalsucipto suciptoNo ratings yet
- Therapy (LLL)Document432 pagesTherapy (LLL)Biruk DesalegnNo ratings yet
- Evaluation and Management of Premature Ventricular ComplexesDocument11 pagesEvaluation and Management of Premature Ventricular ComplexesjahangirealamNo ratings yet
- SyncopeDocument3 pagesSyncopeJesily JoyNo ratings yet
- Pre-Extern Tutorial, 2013Document70 pagesPre-Extern Tutorial, 2013Surat TanprawateNo ratings yet
- ASN 2016 UPDATE Flash DriveDocument119 pagesASN 2016 UPDATE Flash DrivethisarNo ratings yet
- Aes PPT Pooja KumariDocument27 pagesAes PPT Pooja KumariAbhilasha Singh PanwarNo ratings yet
- NeurologyDocument37 pagesNeurologyDevangkumar PatelNo ratings yet
- First Seizure-RCEMDocument2 pagesFirst Seizure-RCEMalsadiqbr5No ratings yet
- Seizure Disorders: Brian Elliott, Dawn Garcia, Jenna Jordan, Dawn Miller, Reis, Michelle SimonsDocument26 pagesSeizure Disorders: Brian Elliott, Dawn Garcia, Jenna Jordan, Dawn Miller, Reis, Michelle SimonsAnastasiafynnNo ratings yet
- Stroke GuidelineDocument15 pagesStroke GuidelinePetrik Aqrasvawinata FsNo ratings yet
- TGA CaseDocument43 pagesTGA CaseGuan-Ying WuNo ratings yet
- Approach To The Comatose PatientDocument29 pagesApproach To The Comatose PatientsteffiwpNo ratings yet
- J American Geriatrics Society - 2022 - GaliziaDocument4 pagesJ American Geriatrics Society - 2022 - GaliziaVitor LopesNo ratings yet
- CBL Os TraumaDocument35 pagesCBL Os TraumaKirthiga15No ratings yet
- Emergency Neurological Life Support - Subarachnoid HemorrhageDocument9 pagesEmergency Neurological Life Support - Subarachnoid HemorrhageIsabel VillalobosNo ratings yet
- Stroke MX at A Glance (May 2020)Document27 pagesStroke MX at A Glance (May 2020)Rye CalderonNo ratings yet
- Avc Isquêmico - Acute Ischemic Stroke Enls 2015Document9 pagesAvc Isquêmico - Acute Ischemic Stroke Enls 2015Fernanda SomeraNo ratings yet
- Crise Convulsiva Provocada - ManejoDocument11 pagesCrise Convulsiva Provocada - Manejorafael rocha novaesNo ratings yet
- SyncopeDocument6 pagesSyncopeDodi TambunNo ratings yet
- Acute Ischaemic StrokeDocument37 pagesAcute Ischaemic StrokeDr. Sarthak MishraNo ratings yet
- Various TopicsDocument8 pagesVarious TopicsLindsay WeissNo ratings yet
- Osce PalpitationshistoryDocument3 pagesOsce PalpitationshistoryEvan O'FlahertyNo ratings yet
- MED SPEC Lecture 3 Adult Critical Care and Trauma 2Document7 pagesMED SPEC Lecture 3 Adult Critical Care and Trauma 28Niellyn Marientes M BeltranNo ratings yet
- Seminar ON Seizure: Presented To Presented byDocument35 pagesSeminar ON Seizure: Presented To Presented byShitaljit IromNo ratings yet
- Stroke, Epilepsy and TB Practical CasesDocument12 pagesStroke, Epilepsy and TB Practical CasesMustahedinNo ratings yet
- Transient Ischemic AttacksDocument10 pagesTransient Ischemic AttacksfabianounifenasNo ratings yet
- Current Guidelines in The Management of Ischaemic Stroke3Document35 pagesCurrent Guidelines in The Management of Ischaemic Stroke3Princewill SmithNo ratings yet
- Diagnosis and Management of Idiopathic Normal-Pressure HydrocephalusDocument11 pagesDiagnosis and Management of Idiopathic Normal-Pressure HydrocephalusPablo Sousa Casasnovas100% (1)
- Nanda, A, Niranjan NS, Transient Ischemic Attack. Medscape. 2013Document6 pagesNanda, A, Niranjan NS, Transient Ischemic Attack. Medscape. 2013rahmatNo ratings yet
- Approach PalpitationDocument6 pagesApproach PalpitationAfien MuktiNo ratings yet
- Postural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated ConditionsFrom EverandPostural Tachycardia Syndrome: A Concise and Practical Guide to Management and Associated ConditionsNicholas GallNo ratings yet
- Fphar 13 889226Document15 pagesFphar 13 889226Azka SamalNo ratings yet
- Effect of Beta Blockers On Stroke Outcome A Meta AnalysisDocument12 pagesEffect of Beta Blockers On Stroke Outcome A Meta AnalysisAzka SamalNo ratings yet
- Clinical Drug - Drug Interaction of Cardiovascular Drugs and Their Case ReportDocument3 pagesClinical Drug - Drug Interaction of Cardiovascular Drugs and Their Case ReportAzka SamalNo ratings yet
- SlidesDocument36 pagesSlidesAzka SamalNo ratings yet
- Pharmaceutics 13 01586Document19 pagesPharmaceutics 13 01586Azka SamalNo ratings yet
- Pharmacologic Treatment Option For Non Insulin DependentDocument6 pagesPharmacologic Treatment Option For Non Insulin DependentAzka SamalNo ratings yet
- Profil N Appropriate Use of Antibiotic Among Children in A General Hospital in Southern BrazilDocument7 pagesProfil N Appropriate Use of Antibiotic Among Children in A General Hospital in Southern BrazilAzka SamalNo ratings yet
- Business PlanDocument7 pagesBusiness PlanddddddaaaaeeeeNo ratings yet
- Tugas PPT Jurnal (Anindya Septiawati-20090310091)Document6 pagesTugas PPT Jurnal (Anindya Septiawati-20090310091)Anindya SeptiawatiNo ratings yet
- Managemen OMADocument8 pagesManagemen OMAHefieNo ratings yet
- Cardiac CatheterizationDocument2 pagesCardiac Catheterizationjacallis50% (2)
- Icknield Newsletter December 2023Document20 pagesIcknield Newsletter December 202322hzamanNo ratings yet
- 7b. Orientation Module 2Document4 pages7b. Orientation Module 2Fuad AddaieNo ratings yet
- Myra Estrin LevineDocument24 pagesMyra Estrin LevineLeonardo Balondo DulaNo ratings yet
- Agesim PaperDocument10 pagesAgesim PaperadilNo ratings yet
- Mechanick 2020 AACE TOS ASMBS GuidelinesDocument73 pagesMechanick 2020 AACE TOS ASMBS GuidelinesCláudia NevesNo ratings yet
- Preboard 2 Maternal and Child and CHNDocument27 pagesPreboard 2 Maternal and Child and CHNDavid Lopez100% (3)
- Articles CSPCDocument61 pagesArticles CSPCStephanieNo ratings yet
- Complications in Children With Percutaneous Endoscopic Gastrostomy (PEG) PlacementDocument5 pagesComplications in Children With Percutaneous Endoscopic Gastrostomy (PEG) PlacementHenry BarberenaNo ratings yet
- Bed BathDocument11 pagesBed Bathramtenki sreelekha100% (1)
- Senior Resource Guide: Allegheny CountyDocument148 pagesSenior Resource Guide: Allegheny CountyDaniel MalloyNo ratings yet
- Job Description - PANCoDocument3 pagesJob Description - PANCoMr_PaintpotsNo ratings yet
- Link L8 U2 Extra Vocabulary WsDocument1 pageLink L8 U2 Extra Vocabulary WsBartosz WesołowskiNo ratings yet
- Risk Management PlanDocument29 pagesRisk Management Plan01095902062ahmedNo ratings yet
- Socio Economic Impact COVID 19 Mozambique UN Mozambique March 2020Document18 pagesSocio Economic Impact COVID 19 Mozambique UN Mozambique March 2020ildoNo ratings yet
- Master Rotation Plan - Final-F B. SC NursingDocument10 pagesMaster Rotation Plan - Final-F B. SC NursingRumela ChakrabortyNo ratings yet
- Charles BabbageDocument3 pagesCharles BabbageElgen B. AgravanteNo ratings yet
- UnfinishedDocument46 pagesUnfinishedSkyerexNo ratings yet
- Community Medicine Module Book PDFDocument37 pagesCommunity Medicine Module Book PDFLiya SuwarniNo ratings yet
- Legend Vaidhya NarayanamurthyDocument2 pagesLegend Vaidhya Narayanamurthyanbarasu86No ratings yet
- Psychological First AidDocument14 pagesPsychological First Aidbreton_nadja226980% (5)
- NCC Presentation Poster Draft JabDocument1 pageNCC Presentation Poster Draft JabJabraan JNo ratings yet
- Perio MedicineDocument90 pagesPerio MedicineAnsh Veer ChouhanNo ratings yet
- What Is Gateway?: Gateway Mental Health AssociationDocument1 pageWhat Is Gateway?: Gateway Mental Health AssociationGateway ProjectNo ratings yet
- Guilford County 10 Year Plan To End HomelessnessDocument2 pagesGuilford County 10 Year Plan To End HomelessnessAbrarNo ratings yet