Professional Documents
Culture Documents
Crashing PT
Crashing PT
Uploaded by
ansylaeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Crashing PT
Crashing PT
Uploaded by
ansylaeCopyright:
Available Formats
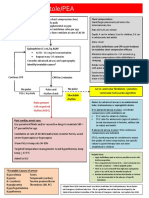
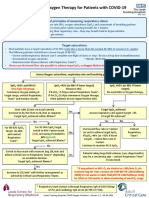
Pearls for the Crashing Medical Patient
General impression of crashing medical patient
New onset ALOC (motor GCS <6), airway issues, respiratory distress, signs of shock
Do not initiate movement of the patient
consider calling for additional resources
Place NPA/OPA as indicated/tolerated
Apply monitors (including waveform capnography)
Assess respiratory status - Intervene ASAP
Respiratory distress Respiratory failure
Increased work of breathing
Poor respiratory effort
Inability to speak full sentances
Unable to speak
Accessory muscle use
Loss of muscle tone
SpO2 <90 on room air
Unable to sit up
SpO2 < 90 despite O2
Altered mental status
Increasing EtCO2
High flow oxygen by nonrebreather or CPAP
If asthma/wheezing/anaphylaxis/acute pulmonary edema - treat Immediate PPV with BVM
per appropriate AG 2-person, elevate the head of bed, 100% O2
2 NPA +/- OPA
No Improvement or persistent hypoxia
Advanced airway measures (SGA, ETI, surgical airway if
unable to oxygenate / ventilate)
Goal = SPO2 > 94 (move to circulatory assessment / transport if persistent hypoxia despite maximum airway management)
Assess circulatory status
BP <90 with signs of shock
Unstable bradycardia General medical /cardiogenic Unstable tachycardia
Transcuteous pacing Fluids per protocol Cardioversion
Push dose epinephrine (14 years or older only) IV/IO Okay to initiate patient extrication and
10-20 mcg boluses (1-2mL) every 2 minutes transport
Preparation: mix 1mL of 1 mg/10 mL (CARDIAC) epinephrine with 9mL
NS. This results in 10 mcg/mL concentration.
Titrate to effect, goal SBP 90 mmHg
Goal = SBP >90 mmHg or initiation of vasorpressors Revised 10/2019
Movement of the patient should be minimized until goals are met or treatment optimized
Trending vital signs is important - a single set does not verify stability
Patient movement increases risks of poor BVM
You might also like
- 2021 ACLS Study GuideDocument20 pages2021 ACLS Study GuideShane Brown86% (14)
- Nursing Care Plan 6 Impaired Gas ExchangeDocument9 pagesNursing Care Plan 6 Impaired Gas Exchangedbryant0101100% (12)
- Filing # 120208791 E-Filed 01/25/2021 07:26:55 PMDocument67 pagesFiling # 120208791 E-Filed 01/25/2021 07:26:55 PMthe next miami100% (1)
- Sample Scoping ReportDocument92 pagesSample Scoping ReportEm Mar0% (1)
- Project Proposal On Dairy FarmDocument26 pagesProject Proposal On Dairy Farmvector dairy88% (8)
- MD 11fgnDocument3 pagesMD 11fgnMcDonnell Douglas MD-110% (7)
- RFH COVID-19 ICU Resource Pack FULL PDFDocument15 pagesRFH COVID-19 ICU Resource Pack FULL PDFQuique GarciaNo ratings yet
- Vasopressors and InotropesDocument31 pagesVasopressors and InotropesReza Prakosa SedyatamaNo ratings yet
- Tesla Motors Expansion StrategyDocument26 pagesTesla Motors Expansion StrategyVu Nguyen75% (4)
- RSI & Status Asthmaticus: Drug Dose Onset/duration Cons ProsDocument2 pagesRSI & Status Asthmaticus: Drug Dose Onset/duration Cons ProsAfina Abdul AzizNo ratings yet
- High-Flow Nasal Cannula-Protocol For Initiation, Titration and WeaningDocument3 pagesHigh-Flow Nasal Cannula-Protocol For Initiation, Titration and WeaningMahmoud khedrNo ratings yet
- Management of Acute Exacerbation in Children: Dr. Raghvendra Singh Senior Resident K.S.C.HDocument18 pagesManagement of Acute Exacerbation in Children: Dr. Raghvendra Singh Senior Resident K.S.C.HDr Amit BishnoiNo ratings yet
- CC Final Study Guide 1Document21 pagesCC Final Study Guide 1api-402814755No ratings yet
- Rapid Sequence Intubation: Mask and MonitoringDocument6 pagesRapid Sequence Intubation: Mask and MonitoringHatim DziauddinNo ratings yet
- Airway ManagementDocument4 pagesAirway ManagementEllamae DerupeNo ratings yet
- Asystole/PEA: Epinephrine 0.1 ML/KG ASAPDocument1 pageAsystole/PEA: Epinephrine 0.1 ML/KG ASAPAlejandro MusaNo ratings yet
- Comprehensive Life Support Tutorial Case 1: Question/Action Information Note/Reference TipsDocument3 pagesComprehensive Life Support Tutorial Case 1: Question/Action Information Note/Reference Tipshyukkie minnieNo ratings yet
- DR Lily - Resp Distress in Newborn Infants PDFDocument45 pagesDR Lily - Resp Distress in Newborn Infants PDFM Ilham MNo ratings yet
- Increasing and Decreasing Repspiratory Support PDFDocument1 pageIncreasing and Decreasing Repspiratory Support PDFÖzgür Barışcan KayaNo ratings yet
- Postanesthesia Care: Dhany BudipratamaDocument36 pagesPostanesthesia Care: Dhany BudipratamaAbu Bakr Ar RaziNo ratings yet
- WB COVID19 Latest Treatment ProtocolDocument1 pageWB COVID19 Latest Treatment ProtocolRahul AwasthiNo ratings yet
- Bronchiolitis: See AlsoDocument6 pagesBronchiolitis: See AlsoJuleides De LeonNo ratings yet
- Status Asthmaticus: Triwahju AstutiDocument41 pagesStatus Asthmaticus: Triwahju AstutirianiNo ratings yet
- NIV and HFNCDocument16 pagesNIV and HFNCMarceline GarciaNo ratings yet
- Asma 1Document8 pagesAsma 1punkgatitNo ratings yet
- Chapter 36V3Document25 pagesChapter 36V3عباس أحمد الشيخ جعفرNo ratings yet
- Case 4Document11 pagesCase 4Shakshi RainaNo ratings yet
- Post Arrest CareDocument23 pagesPost Arrest CareMohamed RasoolNo ratings yet
- NPPVDocument29 pagesNPPVStephanie SusavageNo ratings yet
- 01 - Bronchial AsthmaDocument6 pages01 - Bronchial AsthmaFrank VaronaNo ratings yet
- GINA AlgorithmDocument6 pagesGINA AlgorithmMarcela YolinaNo ratings yet
- Emergencies-Pulmonary OedemaDocument1 pageEmergencies-Pulmonary OedemaMaimoona AimanNo ratings yet
- Nursing Intervention Respiratory Status: Ventilation Respiratory Status: Airway Patency Vital Sign StatusDocument12 pagesNursing Intervention Respiratory Status: Ventilation Respiratory Status: Airway Patency Vital Sign StatusSepti MemorisaNo ratings yet
- Respiratory Rules 2013Document20 pagesRespiratory Rules 2013kawaiiriceNo ratings yet
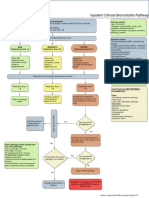
- Bronchiolitis Pathway InpatientDocument1 pageBronchiolitis Pathway Inpatientd'Agung NugrohoNo ratings yet
- Supplementary Material 1a Acute AsthmaDocument3 pagesSupplementary Material 1a Acute AsthmaJanela Chriselle B. TICARNo ratings yet
- Asthma: Treatment and ManagementDocument54 pagesAsthma: Treatment and ManagementEndah susantiNo ratings yet
- 3 Combined AHA BLS ACLS Updates CombinedDocument5 pages3 Combined AHA BLS ACLS Updates Combinedamanrup randhawa100% (1)
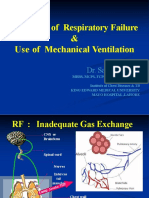
- Overview of Respiratory Failure & Use of Mechanical VentilationDocument89 pagesOverview of Respiratory Failure & Use of Mechanical VentilationsheharyarNo ratings yet
- Nueva Ecija University of Science and Technology: Case 7Document7 pagesNueva Ecija University of Science and Technology: Case 7jomariNo ratings yet
- Niv HFNCDocument15 pagesNiv HFNCFrank VaronaNo ratings yet
- Seven Ps For RSI BOARDDocument2 pagesSeven Ps For RSI BOARDJames BrownNo ratings yet
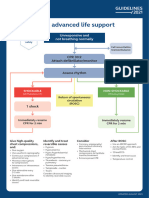
- 8-Adult Advanced Life Support Algorithm 2021Document1 page8-Adult Advanced Life Support Algorithm 2021khaledNo ratings yet
- Aclspediatric BradycardiaDocument2 pagesAclspediatric BradycardiasalamredNo ratings yet
- Adult Advanced Life Support Algorithm 2021 Aug 2023Document1 pageAdult Advanced Life Support Algorithm 2021 Aug 2023cknihilnewNo ratings yet
- NCP - Or-Rotation 2Document12 pagesNCP - Or-Rotation 2Vian RiveraNo ratings yet
- DR Sujata: Professor Dept - of Anaesthesiology &critical Care Ucms & GTB HospitalDocument53 pagesDR Sujata: Professor Dept - of Anaesthesiology &critical Care Ucms & GTB HospitalMiniNo ratings yet
- RahpoDocument3 pagesRahpoassouma16052002No ratings yet
- A (ACLS) - 2015: Dvanced Cardiac Life SupportDocument52 pagesA (ACLS) - 2015: Dvanced Cardiac Life SupportNajmussaqibNo ratings yet
- AIIMS COVID Doc 1.6.1-1Document1 pageAIIMS COVID Doc 1.6.1-1mbhangaleNo ratings yet
- HFOV High-Frequency-Oscillatory-VentilationDocument22 pagesHFOV High-Frequency-Oscillatory-VentilationJZNo ratings yet
- PRIORITY 2: Impaired Gas Exchange Related To Excessive or Thick Secretions Tree Secondary To PneumoniaDocument4 pagesPRIORITY 2: Impaired Gas Exchange Related To Excessive or Thick Secretions Tree Secondary To PneumoniaElay Pedroso100% (1)
- Tutorial 6 - SedationDocument4 pagesTutorial 6 - SedationSNo ratings yet
- Pediatrics-Respiratory Disorders of The Newborn: Diseases Clinical Manifestations Diagnosis & Prognosis ManagementDocument9 pagesPediatrics-Respiratory Disorders of The Newborn: Diseases Clinical Manifestations Diagnosis & Prognosis ManagementJonathan ZumakpehNo ratings yet
- ICU One Pager ARDS v1.1Document1 pageICU One Pager ARDS v1.1Michael LevitNo ratings yet
- Oxygen TherapyDocument2 pagesOxygen TherapyPhilip MusonyeNo ratings yet
- Adult ALS-A3Document1 pageAdult ALS-A3jbruunsNo ratings yet
- BipapDocument26 pagesBipapالغائب الحاضرNo ratings yet
- Guidance On Oxygen Therapy For Patients With COVID-19: General Principles of Assessing Respiratory StatusDocument1 pageGuidance On Oxygen Therapy For Patients With COVID-19: General Principles of Assessing Respiratory StatusAsh mohamedNo ratings yet
- ICU One Pager Intubation ChecklistDocument4 pagesICU One Pager Intubation ChecklistCarlos Hernandez CamposNo ratings yet
- Drug-Assisted Intubation (Dai) : Expanded Scope Practice (NR)Document1 pageDrug-Assisted Intubation (Dai) : Expanded Scope Practice (NR)MEKSELINA KALENDERNo ratings yet
- Scenario Title: Community Acquired Pneumonia Learning Outcomes: 1. Assessment and Recognition of The Signs and Symptoms of PneumoniaDocument6 pagesScenario Title: Community Acquired Pneumonia Learning Outcomes: 1. Assessment and Recognition of The Signs and Symptoms of PneumoniaDud AccNo ratings yet
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsFrom EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNo ratings yet
- WWTP (Grit Chamber) - TDocument22 pagesWWTP (Grit Chamber) - TsarfaNo ratings yet
- OtooDocument11 pagesOtooStefania DavidNo ratings yet
- Shadow Presentation Photography IdeasDocument28 pagesShadow Presentation Photography IdeasagharizwanaliNo ratings yet
- CMA Pre Exam Test PDFDocument28 pagesCMA Pre Exam Test PDFVinay YerubandiNo ratings yet
- Nile International Freight ServicesDocument19 pagesNile International Freight ServicessameerhamadNo ratings yet
- Practical File AI - Class 10Document3 pagesPractical File AI - Class 10pawankvs2008No ratings yet
- Bluetooth 4.2 SpecificationDocument2,772 pagesBluetooth 4.2 SpecificationScott PooleNo ratings yet
- Free Iptv Ex - Yu Streams 11.07.14Document51 pagesFree Iptv Ex - Yu Streams 11.07.14bajra123No ratings yet
- Instructional Methods For Teaching Social Studies: A Survey of What Middle School Students Like and Dislike About Social Studies InstructionDocument4 pagesInstructional Methods For Teaching Social Studies: A Survey of What Middle School Students Like and Dislike About Social Studies InstructionShally GuptaNo ratings yet
- NLC English 7 Enhancement LP v.1Document85 pagesNLC English 7 Enhancement LP v.1patric maturan100% (1)
- Class 12 CS ProjectDocument27 pagesClass 12 CS ProjectKs100% (3)
- Tce Exam SNV S3Document9 pagesTce Exam SNV S3koubi enactaNo ratings yet
- Fruit Processing: Ömer Utku Çopur and Canan Ece TamerDocument28 pagesFruit Processing: Ömer Utku Çopur and Canan Ece TamerTan Hau VoNo ratings yet
- Structural Analysis of Complex Networks 2011Document501 pagesStructural Analysis of Complex Networks 2011kemalihsan_17959No ratings yet
- Engleza Maritima 4: 2a-SMCP External ROUTINE Communication - READING Comprehension-Book1Document5 pagesEngleza Maritima 4: 2a-SMCP External ROUTINE Communication - READING Comprehension-Book1dark959595No ratings yet
- Rapidraw Honey AnalysisDocument5 pagesRapidraw Honey AnalysistaufiqridzNo ratings yet
- National Security Act of 1947 PDFDocument142 pagesNational Security Act of 1947 PDFMax TaylorNo ratings yet
- Digital NativesDocument10 pagesDigital NativesJonathan Blanco Sa RiyadhNo ratings yet
- Anderson Distribution of The Correlation CoefficientDocument14 pagesAnderson Distribution of The Correlation Coefficientdauren_pcNo ratings yet
- First AId Notes - UpdatedDocument54 pagesFirst AId Notes - UpdatedewawireNo ratings yet
- How To Calculate Quantity of Bricks in WallDocument5 pagesHow To Calculate Quantity of Bricks in Wallواثق كريم نعيمNo ratings yet
- 3.3.2.3 Lab - Configuring Rapid PVST, PortFast, and BPDU GuardDocument9 pages3.3.2.3 Lab - Configuring Rapid PVST, PortFast, and BPDU Guardsebastian ruiz100% (1)
- Ge 4.500HP PDFDocument3 pagesGe 4.500HP PDFCarlos FiorilloNo ratings yet
- Color Powder Color ChartDocument4 pagesColor Powder Color ChartArif RusyanaNo ratings yet
- Ict Dos and DontsDocument5 pagesIct Dos and DontsLouwellaEredianoIbabaoNo ratings yet