Professional Documents
Culture Documents
CPH Reviewer
CPH Reviewer
Uploaded by
rinzuuu980 ratings0% found this document useful (0 votes)
1 views3 pagesOriginal Title
CPH REVIEWER
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
0 ratings0% found this document useful (0 votes)
1 views3 pagesCPH Reviewer
CPH Reviewer
Uploaded by
rinzuuu98Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
Download as docx, pdf, or txt
You are on page 1of 3
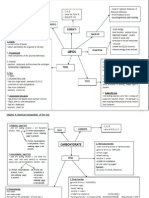
LEGEND: TOPIC KEYWORD
CPH REVIEWER – RENZO DIZON -not sick or contagious
-10% develop TB disease over life time
Communicable Diseases -infection detected by TB skin test
Human Body’s Immune System TB SKIN TEST (PPD – Purified
- a system of biological structures and processes Protein Derivative)
within an organism that protects against diseases
by identifying and killing pathogens and tumor
cells.
- It detects a whole variety of agents, including
viruses and parasitic worms.
- Detection can be complicated as pathogens can
evolve rapidly and adapt.
- protects organisms from infections.
-Human infection occurs when bacteria, fungi, Controlling Spread of Infectiion:
parasites, or viruses enter the human body and The Reactive Approach
start to multiply. Diagnosis is importance – establish the
occurrence of disease based on signs and Active TB Disease
Bacterium symptoms. -Usually involves lung infection
- single-celled microorganisms, which can exist as - Presumptive vs. Definitive -cough > 3 weeks, fever, weight loss, night sweats
either independent (free-living) or parasitic -Use of physical exam, lab tests -treatable with antibiotics
(dependent on another organism). -Case definition -contagious until appropriately treated
-start treatment of sick person immediately
Virus according to protocol. Preventing Spread of TB
- microorganism smaller than a bacterium, which (Early Diagnosis and Prompt Treatment) -Patients with TB should delay court appearance
cannot grow or reproduce apart from a living until appropriate duration of therapy.
cell. Identify the source of infection – where did the -Patients with TB are no longer contagious after
- Invades living cells and uses them to keep itself sick person get the infection? 2-3 weeks of appropriate therapy (should be
alive or multiply. cleared by doctor).
Identify the mode of transmission – how did the
sick person get infected? TB other name: Koch’s Pulmonary
Controlling the Spread of infections: MOT: Airborne droplet
Proactive Approach -Direct invasion through mucus
Identify Risk Groups – people who are -breaks in skin (rare)
susceptible to acquire communicable diseases
Period of communicability: as long as viable
Identify risk -is the community at risk of exposure bacteria are discharged from sputum
to various communicable diseases? Signs/Symptoms (S/S) – early weight loss,
listlessness, vague chest pain, pleurisy anorexia,
Preventive measures to address: fever, night sweats
Parasite 1. Identified reservoir of infectious diseases Prevention- BCG & health education
- organism that lives in or on and takes its 2. Community’s defense against infection Diagnosis (Dx): PPD (Purified Protein Derivative)
nourishment from another organism (Herd Immunity, Barriers on routes of Tuberculin exposure
- Parasitic diseases include infections by transmission) -chest x-ray cavitary lesion
protozoa, helminths, and arthropods. 3. Screening of presumed healthy population -sputum-confirmatory
Management: MDT
Factors affecting risk of infections: Communicable Diseases: r-orange urine (rifampicin)
- age Pathognomonic: a sign or symptom that is so i-neuritis and hepatitis (Isoniazid)
-heredity characteristic of disease and can be used to make p-hyperuricemia (Pyrazinamide)
-level of stress a diagnosis. e-impairment of vision (Ethambutol)
-nutritional status _______________________________________ s-8th cranial nerve damage (Streptomycin)
Current medical therapy Pulmonary Tuberculosis DOTS (Direct Observed Treatment Short Course) -
-pre-existing disease Causative Agent: Mycobacterium Tuberculosis to detect and cure TB patients.
-immunization status Reservoir: humans
Definition: Chronic Infection of lungs
STAGES OF AN INFECTIOUS PROCESS: - chronic coughing for two weeks LEPROSY
I. Incubation Period -weight loss, night sweats, unexplained fever CA: Mycobacterium Leprae, Hansen's Bacillus
- the silent stage and ends when the first signs -blood-stained sputum MOT: prolonged skin-skin contact (common) and
and symptoms of disease appear. Period of communicability: droplets
II. Prodromal Period It depends on the number of bacilli discharges, IP = years to decades
- first onset signs and symptoms occur (malaise, the virulence of bacilli, ventilation, exposure to Chronic disease of the skin and peripheral nerves
runny nose, etc.) the sun or UV light, and opportunities for S/S EARLY
III. Illness period/Acute Stage (Pathognomonic aerosolization by coughing, sneezing, talking, or 1. change in skin color (either reddish or white)
Sign) sneezing. 2. loss of sensation on the skin lesion
-the disease reaches its highest point 3. decrease or loss of sweating and hair growth
IV. Declining Period Latent TB infection: on skin lesion
-Symptoms starts to subside -Person infected with TB bacteria 4. thickened and/or painful nerves
V. Convalescence Period -bacteria kept dormant in persons immune 5. pain and redness in the eyes
-Symptoms vanished, pathogen eliminated system 6. nasal obstruction or bleeding
LEGEND: TOPIC KEYWORD
LATE S/S: quartan-febrile paroxysm: q48H-72H Dx:
1. Lagopthalmos: -inability to close the eyelids ACUTE FEBRILE ILLNESS WITH NO IDENTIFIABLE
completely MOT: Bite from infected anopheles mosquito FOCUS OF INFECTION
2. Madarosis: absence or loss of Blood Transfusion Internal and external sign of bleeding
eyelashes/eyebrows IP (Incubation Period) 5-6 days Torniquet Test or Rumpel Lead Test
3. Clawing of fingers and toes Dx: blood extraction (extract blood at the height Platelet count
4. contractures - permanent shortening of of fever) PT (Prothrombin Time)
muscle or joint Manifestations: APTT (Activated Partial Thromboplastin Time)
5. Saddle nose- sinking of the nosebridge Fever, chills, profuse sweating-convulsion Bleeding time
6. gynecomastia -enlargement of breast in males Anemia, fluid and electrolyte imbalance, Coagulation time
7. Chronic ulcers hepatomegaly, splenomegaly, rigor, headache,
DX: Lepromin Test - ID injection and diarrhea. Notes:
Slit Skin Smear Blackwater Fever - hemolysis and -any condition associated with bleeding is
Prevention: hemoglobinuria enough cause for alarm
-avoid MOT Management: -for fever don't give asa
-BCG vaccination, good personal hygiene, Chloroquine and Primaquine drug of choice -rapid replacements of fluids is the most
adequate nutrition, Health Education Chloroquine for pregnant women important treatment
Management: For resistant plasmodium-use chemo drug -give oresol/hydrite
Multidrug therapy (MDT- two or more drugs -vit c to promote capillary integrity
RA 4073 (home meds) NOTES: -blood transfusion
-Paucibacillary (Tuberculoid and indeterminate) -travelers to malaria endemic area should follow -iv crystalloids (plain lrs, plain 0.9 nss)
Dapsone/ Rifampicin preventive measures (chemoprophylaxis -dextran (colloids)
Non-infectious types -chloroquine may be taken 1 week before -platelets
Duration of tx: 6-9 months entering endemic area) -fresh frozen plasma
-Multibacilary (Lepromatous and borderline) -soaking of mosquito net in an insecticide -cryoprecipitate
Dapsone/ Rifampicin/Clofazimine solution -whole blood
Infectious types -bio ponds for fish -no known immunization (vaccine currently
-Duration of tx: 24–30 months -on stream clearing (to expose the breeding underway)
stream to sunlight)
-vectors peak biting at night 9pm-3am MEASLES
CHICKEN POX -planting of neem tree (repellent effect) AKA: 7 Day Fever, Hard Red Measle
AKA: Varicella -zooprophylaxis (deviate mosquito bites from CA: Rubeola virus
CA: Herpes Zoster Virus; Varicella Zoster Virus man to animals) MOT = droplets and airborne
MOT: direct contact, Droplet spread -infected mother can continue breast feeding PC 4 days before and 5 days after rash
IP: 2-3 weeks commonly 14-21 days HIGHLY CONTAGIOUS
Period of communicability: one day IP 7-14 days
before rash and 6 days after first crop of vesicles Rashes: maculopapular, cephalocaudal (hairline
and behind the ears to trunk and limbs),
HIGHLY CONTAGIOUS desquamation, pruritus
-An acute infectious disease of sudden onset PS koplik's spot
with slight fever, mild constitutional Characteristic: photophobia (typical complaint)
symptoms and eruption, which are maculo- Fever: high fever
papular for a few hours, vesicular for 3-4 days
and leaves granular scabs. GERMAN MEASLES
- Lesions are more on covered than on exposed AKA: Rotheln Disease, 3 Day Measles
parts of the body and may appear on scalp and CA: Rubella
mucous membrane of URT Rashes: Maculopapular, Diffuse/not confluent,
No desquamation, spreads from the face
Susceptibility/Resistance/ Occurrence DENGUE FEVER downwards
-Universal among those not previously -mosquito-borne infection that causes a severe PS forschheimer's
attacked, severe in adults flu-like illness, and sometimes a potentially lethal Characteristic: cervical lymphadenopathy
-second attacks : rare, 70% have the disease by complication called dengue called dengue Fever: low grade fever
the time they are 15 y/o hemorrhagic fever. CX rare; CX to pregnant women:
Rashes: Maculopapulovesicular (covered areas), -about two fifths of the world’s population are Ist tri-congenital anomalies
Centrifugal, starts on face and trunk now at risk. 2nd tri-abortion
and spreads to entire body 3rd tri-pre mature delivery
Leaves a pitted scar (pockmark) AKA H-Fever, Dandy Fever, Breakbone Disease
DX: Tzanck smear (scraping of ulcer for staining) Acute Febrile Disease
DIPHTHERIA
CA: DENGUE VIRUS TYPE 1,2,3,4, and
CA; Corynebacterium diphtheriae
MALARIA Chikungunya virus
Klebsloeffler's bacillus (bacteria)
King of Tropical Diseases MOT: Bite of Aedes aegypti, Aedes albopictus
MOT = droplets and airborne
CA: Protozoan plasmodium Culex fatigans (day biting, stagnant water)
HIGHLY CONTAGIOUS
plasmodium ovale - dormant (liver) IP (Incubation Period) 1 week
IP 2-5 days
plasmodium vivax - benign S/S
Dx: throat swab, (Schick test - susceptibility to
plasmodium malariae - mild but resistant Hyperpyrexia without focal of infection
diphtheria toxin & Moloney - sensitivity to
plasmodium falciparum - malignant (cerebral TRIAD: fever, rashes and muscle pain (myalgia)
diphtheria toxoid)
malaria) Bleeding to hypovolemic shock
S/sx:
P.VIVAX AND OVALE MAY HAVE RECCURENCE ASA (Aspirin) is contraindicated
sore throat, fever, "Bull-neck"
OF SYMPTOMS Watchout for bleeding
(Pseudomembrane-gray exudate, foul breath,
tertian-febrile paroxysm: q24H-48H PLATELET is being attacked
massive swelling of tonsils and uvula, thick
speech, cervical lymphadenopathy, swelling of
submandibular and anterior neck)
obstruction of respiratory tract
Resp Acidosis with hypoxemia
Management: Diphtheria antitoxin (Skin test),
Penicillin, erythromycin, rifampicin, clindamycin
Notes:
-observe cns, cardiac and kidney complications
-pseudomembranous may lead to resp.
obstruction
-isolation until 2 negative culture at 24 hour
interval
-f&e resuscitation
-parents or siblings who have never immunized
should receive a dose of diph.anti-toxin
-attention to nasopharyngeal discharge
-antibiotics-penicillin, erythromycin if allergic to
penicillin
MUMPS
CA: Mumps virus/filtrable virus
AKA: Parotitis
MOT = droplets and airborne (secretion of the
mouth and nose)
HIGHLY CONTAGIOUS
IP 12-16 days
Unilateral or bilateral parotitis
-ice collar
Stimulating foods cause severe pain
Bilateral orchitis and oophoritis
-Active spermatogenesis
-Sterility
Steroids
Supporter
You might also like
- Epidemiology Exam Questions and AnswersDocument107 pagesEpidemiology Exam Questions and Answersdimitrios82% (34)
- Nursing Assistant A Nursing Process Approach 11Th Edition Acello Solutions Manual Full Chapter PDFDocument67 pagesNursing Assistant A Nursing Process Approach 11Th Edition Acello Solutions Manual Full Chapter PDFhelgasophie7478k0100% (9)
- Concept Communicable DiseasesDocument421 pagesConcept Communicable DiseasesJoric Magusara93% (14)
- Heat Stress Poster 2 - 260520153053Document2 pagesHeat Stress Poster 2 - 260520153053TomNo ratings yet
- Positive Behavior SupportsDocument10 pagesPositive Behavior Supportsapi-491244141No ratings yet
- Concept Communicable DiseasesDocument425 pagesConcept Communicable DiseasesRjhay14100% (2)
- Communicable Disease Nursing 2020Document421 pagesCommunicable Disease Nursing 2020Kenneth Myro GarciaNo ratings yet
- Infectious Process: "All Contagious Diseases Are Communicable But Not All Communicable Diseases Are Contagious"Document8 pagesInfectious Process: "All Contagious Diseases Are Communicable But Not All Communicable Diseases Are Contagious"Micah TuringanNo ratings yet
- Concept Communicable DiseasesDocument477 pagesConcept Communicable DiseasesrimeoznekNo ratings yet
- Chapter 1 Communicable Diseases 2ND Sem 2022 2023Document10 pagesChapter 1 Communicable Diseases 2ND Sem 2022 2023Lovelyn Cantollas EugenioNo ratings yet
- Communicable Disease Prevention and ControlDocument197 pagesCommunicable Disease Prevention and Controldennisjamesbartz100% (1)
- Communicable Nursing - LecturervDocument329 pagesCommunicable Nursing - LecturervCarl WaletNo ratings yet
- Communicable DiseasesDocument32 pagesCommunicable DiseasesPatty RomeroNo ratings yet
- Theory PointersDocument89 pagesTheory Pointerslala byuNo ratings yet
- LONG Communicable Disease NursingDocument33 pagesLONG Communicable Disease NursingSK PatacboNo ratings yet
- Communicable DiseasesDocument164 pagesCommunicable DiseasesJasmin Jacob33% (3)
- Infectious Diseases 2Document12 pagesInfectious Diseases 2Jean GolezNo ratings yet
- Communicable DiseaseDocument7 pagesCommunicable DiseasePatricia LoanzonNo ratings yet
- Epidemiology Exam Questions and AnswersDocument107 pagesEpidemiology Exam Questions and AnswersilerioluwaibitoyeNo ratings yet
- Control of Communicable DiseaseDocument4 pagesControl of Communicable DiseaseBianca CordovaNo ratings yet
- Communicable DiseaseDocument98 pagesCommunicable DiseasePeach BubbleNo ratings yet
- Prefinals MPDocument7 pagesPrefinals MPJireh Joy TangaraNo ratings yet
- Pathology Week-14Document9 pagesPathology Week-14taysi tafriNo ratings yet
- MODULE 1 and 2 RevisedDocument50 pagesMODULE 1 and 2 RevisedMaricar RosasNo ratings yet
- Communicable Disease Nursing Ca1 July 2018 5Document461 pagesCommunicable Disease Nursing Ca1 July 2018 5Jordz PlaciNo ratings yet
- Care of Patients With Infectious DiseasesDocument3 pagesCare of Patients With Infectious DiseasesMutya XDNo ratings yet
- CHN Final TopicsDocument52 pagesCHN Final TopicsMary Ann SacramentoNo ratings yet
- Communicable DiseaseDocument5 pagesCommunicable DiseaseLordson Gem P. IbonNo ratings yet
- Communicable DiseaseDocument41 pagesCommunicable DiseaseMrz AlzNo ratings yet
- Ca2 CDNDocument17 pagesCa2 CDNcrix crixNo ratings yet
- Communicable Disease NursingDocument428 pagesCommunicable Disease NursingRellie Castro100% (5)
- Human MonkeypoxDocument8 pagesHuman Monkeypoxlakshay kumarNo ratings yet
- Asepsis and Infection PreventionDocument31 pagesAsepsis and Infection PreventionPamela Ria HensonNo ratings yet
- ST STDocument4 pagesST STChlodette Eizl M. LaurenteNo ratings yet
- Tuberculosi 1Document5 pagesTuberculosi 1Corine FabulaNo ratings yet
- Infectios DiseasesDocument183 pagesInfectios DiseasesAnonymous eson90No ratings yet
- Communicable Disease Day 1Document7 pagesCommunicable Disease Day 1JolensNo ratings yet
- TuberculosisDocument35 pagesTuberculosisAmr KhayyalNo ratings yet
- Introduction of MicroparasitoryDocument36 pagesIntroduction of MicroparasitoryEben Alameda-PalapuzNo ratings yet
- Week 10 Basic Concept of Comm DiseasesDocument10 pagesWeek 10 Basic Concept of Comm Diseasesjmmacar19No ratings yet
- Health and DiseaseDocument32 pagesHealth and DiseaseAlejandro GonzalezNo ratings yet
- Communicable Disease NursingDocument50 pagesCommunicable Disease NursingChernobyle Tolentino BattadNo ratings yet
- MPH 5203 Communicable DiseasesDocument134 pagesMPH 5203 Communicable DiseasesOLIVIERNo ratings yet
- Chapter 43: Nursing Care of A Family When A Child Has An Infectious DisorderDocument12 pagesChapter 43: Nursing Care of A Family When A Child Has An Infectious DisorderAlyssaGrandeMontimorNo ratings yet
- Lec5 MP Bacteria and DiseaseDocument51 pagesLec5 MP Bacteria and DiseasePriya ManobalNo ratings yet
- Parasitology Note 1Document9 pagesParasitology Note 1UNKNOWN ANGELNo ratings yet
- MLSP111 TransesDocument9 pagesMLSP111 Transesrd timolaNo ratings yet
- Basic Concepts of Nursing Notes Edited by Lovely Jovellanos 1Document4 pagesBasic Concepts of Nursing Notes Edited by Lovely Jovellanos 1Love Jovellanos ÜNo ratings yet
- Community Health Nursing Doh Related Programs: Epi - Types of VaccinesDocument32 pagesCommunity Health Nursing Doh Related Programs: Epi - Types of VaccinesAngelaNo ratings yet
- Communicable DiseaseDocument1 pageCommunicable DiseaseJULIUS CEZAR QUINAYNo ratings yet
- Module 1Document40 pagesModule 1Rohan RalliNo ratings yet
- Community Health Nursing Doh Related Programs: Epi - Types of VaccinesDocument32 pagesCommunity Health Nursing Doh Related Programs: Epi - Types of VaccinesAngelaNo ratings yet
- COMMUNICABLE-DISEASE-NURSING-DAY1.pdf - PDF ExpertDocument24 pagesCOMMUNICABLE-DISEASE-NURSING-DAY1.pdf - PDF ExpertFrances Sofia DuranNo ratings yet
- Chapter 14: Host Parasite RelationshipsDocument10 pagesChapter 14: Host Parasite RelationshipsNurul WidyawatiNo ratings yet
- Infectious DiseaseDocument5 pagesInfectious DiseaseResa Fela AfianaNo ratings yet
- CD HandoutDocument20 pagesCD HandoutiandameNo ratings yet
- CD CompiledDocument39 pagesCD CompiledGeraldine MaeNo ratings yet
- Public Health (Midterm)Document24 pagesPublic Health (Midterm)Beshoy YousefNo ratings yet
- 1 Introduction To EpidemiologyDocument39 pages1 Introduction To EpidemiologySarahLiyana100% (2)
- Fundamentals of Infectious Diseases - UpdatedDocument56 pagesFundamentals of Infectious Diseases - UpdatedamilaNo ratings yet
- PH Part 1Document64 pagesPH Part 1Jimmy SadsadNo ratings yet
- Contagious Diseases: The Science, History, and Future of Epidemics. From Ancient Plagues to Modern Pandemics, How to Stay Ahead of a Global Health CrisisFrom EverandContagious Diseases: The Science, History, and Future of Epidemics. From Ancient Plagues to Modern Pandemics, How to Stay Ahead of a Global Health CrisisNo ratings yet
- COVID-19 LEGACY: SARS-CoV-2 clinical trials, vaccines trials and bioethicsFrom EverandCOVID-19 LEGACY: SARS-CoV-2 clinical trials, vaccines trials and bioethicsNo ratings yet
- Biology Form 4 Chapter 4 Chemical Composition Oft He CellDocument18 pagesBiology Form 4 Chapter 4 Chemical Composition Oft He CellAngie Kong Su MeiNo ratings yet
- Wound Healing Properties of Root Extract of Harungana Madagascariensis On Wistar Rat ModelDocument6 pagesWound Healing Properties of Root Extract of Harungana Madagascariensis On Wistar Rat ModelInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Catch It Right - A Case Report On Occlusal SplintDocument6 pagesCatch It Right - A Case Report On Occlusal SplintSkAliHassanNo ratings yet
- Tim Dosen: Nur Rachmat, Bpo Cica Trimandasari N, Amd Op Muhammad Syaifuddin, Amd OpDocument11 pagesTim Dosen: Nur Rachmat, Bpo Cica Trimandasari N, Amd Op Muhammad Syaifuddin, Amd OpAdi NugrohoNo ratings yet
- Minscat Bongabong Campus, To Be Placed On 'Localized Lockdown' Due To Coronavirus ThreatDocument5 pagesMinscat Bongabong Campus, To Be Placed On 'Localized Lockdown' Due To Coronavirus ThreatFranz Chavez GarciaNo ratings yet
- The Tourism Industry and The Impact of Covid-19 Scenarios and ProposalsDocument34 pagesThe Tourism Industry and The Impact of Covid-19 Scenarios and ProposalsAMMAR MUSTAQIM BIN ABDUL BOSTANINo ratings yet
- Omega 3 PaperDocument22 pagesOmega 3 PaperDr. Bushra SumraNo ratings yet
- AcuPulse Versatility SupplementDocument16 pagesAcuPulse Versatility SupplementSD DSNo ratings yet
- B.inggris3 7A Group Task10 Group 6Document7 pagesB.inggris3 7A Group Task10 Group 6Rosita DamayantiNo ratings yet
- EM00000453 CareFusion - 3100B High Frequency Oscillatory Ventilator Operator's ManualDocument100 pagesEM00000453 CareFusion - 3100B High Frequency Oscillatory Ventilator Operator's ManualHobi's WaifuNo ratings yet
- Added Sugars and Periodontal Disease in Young Adults: An Analysis of NHANES III DataDocument6 pagesAdded Sugars and Periodontal Disease in Young Adults: An Analysis of NHANES III DataNavaneethan GnanadesiganNo ratings yet
- Theory of Cultural Care and DiversityDocument16 pagesTheory of Cultural Care and DiversityJunne Rafaela NovalNo ratings yet
- Emergency Medicine Pharmacist ServicesDocument15 pagesEmergency Medicine Pharmacist ServicesalfinadyaNo ratings yet
- 2023 Guideline Diagnosis Management AFIB Slide SetDocument46 pages2023 Guideline Diagnosis Management AFIB Slide SetMARIAM BANONo ratings yet
- Detailed Lesson Plan in MapehDocument5 pagesDetailed Lesson Plan in MapehNel LovedorialNo ratings yet
- Baby Massage Guide Au 2011Document8 pagesBaby Massage Guide Au 2011dianNo ratings yet
- Ujang RDocument20 pagesUjang Rrode sihombingNo ratings yet
- Care For The Child Under Photo TherapyDocument36 pagesCare For The Child Under Photo Therapylamiaa80% (10)
- CASEST1Document4 pagesCASEST1allyNo ratings yet
- dm2022 0304Document2 pagesdm2022 0304Charlemagne Sabio GalamgamNo ratings yet
- Accumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaDocument5 pagesAccumulation of Alpha-Fluoro-Beta-Alanine and Fluoro Mono Acetate in A Patient With 5-Fluorouracil-Associated HyperammonemiaJana NgNo ratings yet
- IPSGDocument29 pagesIPSGShermaida Basirul100% (1)
- الذهبي ٦ Corrected by Yes We Can 2021Document30 pagesالذهبي ٦ Corrected by Yes We Can 2021Salma HelmyNo ratings yet
- Nurse Patient Nurse: Tugas Sir Jon. Admission Patient DialogueDocument7 pagesNurse Patient Nurse: Tugas Sir Jon. Admission Patient DialogueIndry LabungasaNo ratings yet
- Veterinary HelminthologyDocument54 pagesVeterinary HelminthologyAli KipkoechNo ratings yet
- Immunization: DR Shahbaz Ahmad Professor Community Medicine Independent Medical College FaisalabadDocument67 pagesImmunization: DR Shahbaz Ahmad Professor Community Medicine Independent Medical College FaisalabadPriya bhattiNo ratings yet
- Past Life RegressionDocument8 pagesPast Life RegressionGabriel AndradeNo ratings yet